Abstract
A 49-year-old male was evaluated in our hospital for chronic cough, cervical lymphadenopathy, and a testicular mass. As a part of the management, he underwent a cervical lymph node biopsy, which showed metastatic deposits from papillary carcinoma thyroid. Subsequently, he underwent orchidectomy for suspected testicular malignancy, but the biopsy showed discrete granulomatous inflammation consistent with sarcoidosis. This was followed by total thyroidectomy with neck node dissection. Nodal histopathological examination, this time, revealed a single node containing both malignancy and granulomas. Prior to the thyroid surgery, he underwent a mediastinoscopic sampling of the mediastinal nodes, which also showed granulomatous inflammation consistent with sarcoidosis. Sarcoidosis affecting the genitourinary system is a rare entity. The coexistence of sarcoidosis and thyroid malignancy poses a diagnostic challenge. A thorough review of the literature was done, and there are no reports from India on the above association. This is a unique case, which could possibly suggest an association between sarcoidosis and malignancy and highlights the importance of obtaining a tissue diagnosis in such cases.
KEY WORDS: Genitourinary, papillary carcinoma of thyroid, sarcoidosis
INTRODUCTION
Sarcoidosis is a granulomatous disease of unknown origin that primarily affects lungs and the lymphatic system. Extrapulmonary involvement is common, and any organ may be involved, but genitourinary involvement is uncommon (<1%).[1] Genitourinary sarcoid can be easily mistaken for malignancy, especially when a patient has a unilateral, palpable mass which is painless. Distinguishing genitourinary sarcoid from primary testicular sarcoid is very difficult, as neither conventional imaging nor fluorodeoxyglucose–positron-emission tomography scans are diagnostic. Serum markers such as beta-human chorionic gonadotropin and alpha-fetoprotein may be helpful in distinguishing but not 100% reliable.[2]
Sarcoidosis is a chronic inflammatory disease and is being increasingly reported to be associated with malignancies, even though the exact frequency has not yet been established. They can occur together or in sequence. Therefore, it is important for clinicians to be aware of the simultaneous occurrence of sarcoidosis and metastatic malignancy, especially when the biopsy shows a granulomatous reaction.
CASE REPORT
A 42-year-old male presented to our hospital with complaints of dry cough of 6-month duration and loss of weight and appetite for the past 2 months. He had no history of fever, chest pain, or breathlessness. His comorbidities include Type II diabetes mellitus, hypertension, and dyslipidemia. He did not have any symptoms suggestive of respiratory ailments or tuberculosis in the past. He had no history of close contact with tuberculosis. He was a nonsmoker, and there was no pet, bird, or chemical exposure, and review of his medications history did not reveal any possible agent which could cause cough.
On examination, his vital signs were normal. He was moderately built and nourished and had clubbing of fingers and toes. A right supraclavicular node was palpable, and it was firm and nontender. Examination of the respiratory system was essentially normal, and other system examinations were unremarkable, except for a painless unilateral right-sided scrotal swelling, which was not noted by the patient so far.
A chest radiograph showed bilateral hilar prominence without lung parenchymal involvement. A computed tomography chest [Figure 1] revealed multiple enlarged mediastinal lymph nodes such as upper and lower paratracheal, subcarinal, and bilateral hilar. The lung window did not reveal any lung parenchymal lesions. His total lymphocyte count was normal (6700 cells/mm3). Liver function tests and well as renal function tests were normal. Serum calcium was 10 mg/dl (normal: 8.6–10.2 mg/dl). In view of chronicity and nature of symptoms and enlarged cervical and mediastinal lymph nodes, the differential diagnoses that were considered were tuberculosis, sarcoidosis, and lymphoma. Sputum smear examination for acid-fast bacillus and CBNAAT was negative. A tuberculin test was done, and it did not show any induration after 48 h. The patient was referred to general surgeon for cervical node biopsy. Urology consultation was sought for the testicular mass. Since he was a middle-aged male with painless scrotal swelling, the possibility of malignancy had to be ruled out. A magnetic resonance imaging of the abdomen and pelvis was taken, which revealed multiple enlarged paraaortic and iliac nodes in addition to the testicular mass. The radiological features favored a testicular tumor.
Figure 1.
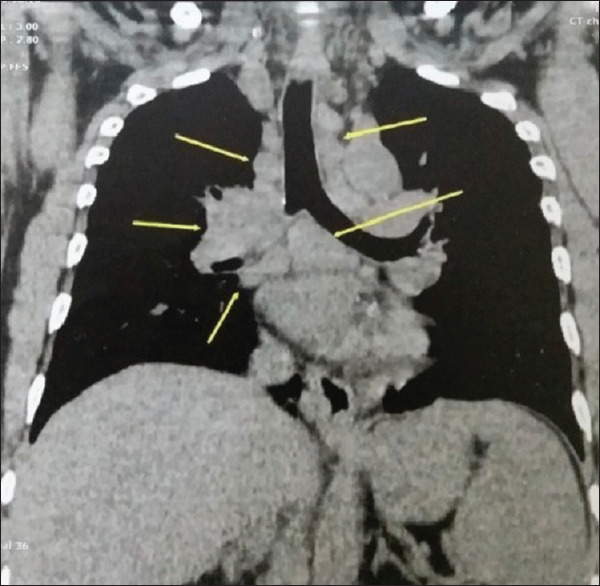
Computed tomography thorax sagittal image, mediastinal window showing enlarged paratracheal, subcarinal, and hilar lymph nodes (arrows)
Cervical lymph node biopsy was done, and biopsy unexpectedly revealed metastasis from papillary carcinoma of the thyroid. Serum angiotensin-converting enzyme value was 160 U/L (normal: 8–52 U/L). Urinary calcium was 870 mg/dl (normal: 50–150 mg/dl), and serum calcium was 10 (normal: 8.6–10.2 mg/dl). After multidisciplinary discussion, it was decided to go for high inguinal orchidectomy for scrotal swelling since malignancy was of prime consideration. Histopathological examination of the orchidectomy specimen [Figure 2] showed discrete noncaseating granulomas, which on reticulin staining showed reticulin-positive fibers permeating the areas of inflammation. Since the patient also had multiple mediastinal nodes, in the background of thyroid malignancy, it was decided to do a mediastinoscopic sampling of the nodes to rule out metastasis from the thyroid malignancy. The histopathological examination of mediastinal nodes revealed discrete noncaseating granuloma, and reticulin staining was also positive.
Figure 2.
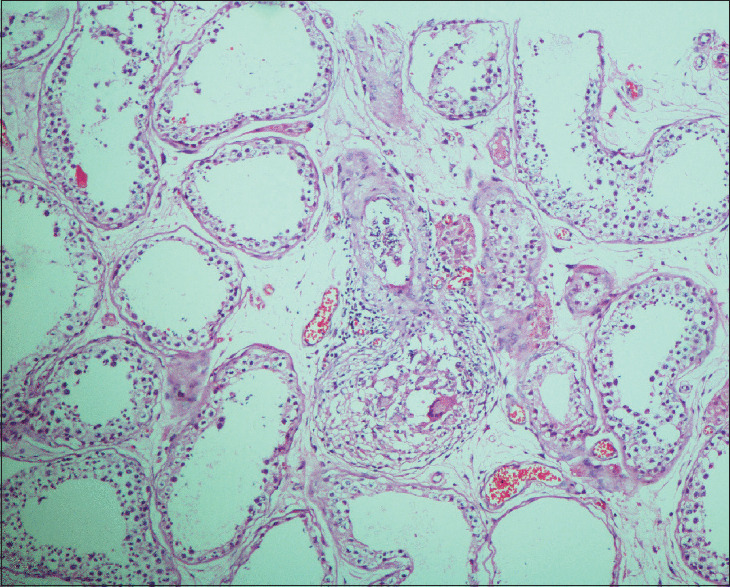
Orchidectomy specimen showing seminiferous tubules with interstitium showing epithelioid cell granuloma H and E, ×200
The final diagnosis was sarcoidosis with multisystem involvement such as lymph nodes, renal and genital involvement, and coexisting with papillary carcinoma of the thyroid. A multi-disciplinary discussion in the tumor board was held, and it was decided to proceed with total thyroidectomy and block dissection of the neck. Histopathological examination of the thyroid tissue confirmed the diagnosis of papillary carcinoma of the thyroid. Adding more twists and turns to the clinical scenario, the histopathological examination of cervical nodes revealed some nodes having metastatic deposits from thyroid, some showed discrete granulomas, awhile some other nodes showed both metastatic deposits as well as epithelioid cell granulomas in the same tissue [Figure 3]. The patient subsequently underwent radiotherapy and was then started on oral prednisolone with an initial dose of 40 mg once daily, which was slowly tapered off by 1 year. At follow-up a year later, he was healthy and had a complete radiological resolution of the mediastinal nodes.
Figure 3.
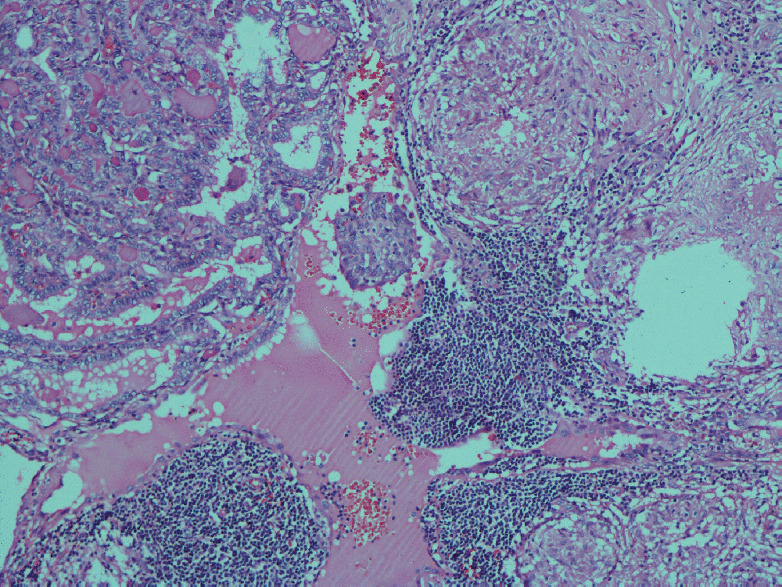
Neck node dissection specimen showing the focus of papillary cell carcinoma thyroid with adjacent tissue showing epithelioid cell granuloma H and E, ×200
DISCUSSION
Sarcoidosis commonly affects the lymph nodes, lungs, eyes, liver, bones, and skin. However, sarcoidosis of the reproductive system has been estimated to occur only in <1% of clinically diagnosed cases and 5% of autopsy cases.[1] A testicular mass has many differential diagnoses, foremost being malignancy, and sarcoidosis is an uncommon cause, as in the case described above. Imaging is central to investigating testicular lesions, but it has very low sensitivity and specificity to differentiate between genitourinary sarcoid and malignancy.[2] Histological examination, along with relevant blood tests like angiotensin-converting enzyme level estimation, remains the most reliable way to approach a case of suspected sarcoidosis (which is always a diagnosis of exclusion), and orchidectomy is the primary radical treatment for testicular mass suggestive of tumor.[2] Interestingly, there is a recognized association between sarcoidosis and testicular cancer.[3]
In 1974, Brincker and Wilbek noted a statistically significant increase of malignant tumors among sarcoid patients and speculated that immunologic deficiencies stemming from sarcoidosis may predispose the patients to malignancy.
Although there are several published cases highlighting the coexistence of malignancy and sarcoidosis, the causal relationship between these entities is still unclear.[4] On the one hand, it is possible that patients with sarcoidosis develop malignancies, and on the other hand, there are oncologic patients developing sarcoidosis and sarcoid such as reactions, especially after chemotherapy. Spiekermann et al. have reviewed the coexistence of sarcoidosis and metastatic malignancy and have shown that the most frequent cancer origin was breast, followed by malignancy of thyroid gland. Sarcoidosis occurred in 20 cases after an average of 34.4 months and in 7 cases 10.25 years before the diagnosis of malignancy. In most reported cases, sarcoidosis was diagnosed simultaneously with malignancy.[4] In a recent case report, sarcoidosis and coexistent papillary carcinoma were diagnosed in a patient presented who with hypercalcemia as the main symptom.[5]
Myeloid-derived suppressor cells may play a very important role in the pathogenic association between sarcoidosis and malignancy. Sarcoidosis has the potential to promote metastasis by inducing tumor-promoting and immune-regulating cell subsets.[6]
CONCLUSION
A literature review failed to reveal any case reports of multisystem sarcoidosis with coexisting malignancy from India. To the best of our knowledge, this is the first such case being reported from our country. This case is being reported for two unique reasons. First, the rare presentation of testicular sarcoidosis and the diagnostic dilemmas associated with this condition. Clinicians must be aware of the fact that sarcoidosis is a great mimicker of both clinical manifestations and radiological features of the primary malignancy of genitourinary tract. The second is to highlight the simultaneous occurrence of sarcoidosis with thyroid malignancy and the possible reasons for this association between sarcoidosis and malignancy. Sarcoidosis as a disease may coexist with papillary carcinoma of thyroid, and an awareness of this association is important when confronted with such a patient as ours.
The importance of getting a tissue diagnosis is very crucial in this era of evidence-based medicine. It was only because all relevant biopsies were done in our patient; we were able to establish the concurrent diagnosis of multisystem sarcoidosis and papillary carcinoma of the thyroid gland.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to acknowledge Prof. Leena Devi, Head of the Department of Pathology and Drs. Annie Belthazar, and Vidya C.S., Pathologists, for their guidance and help with histopathological examination and interpretation.
REFERENCES
- 1.Moller DR, Chen ES. Fishman's Pulmonary Diseases and Disorders. McGraw Hill Education: 2015. p. 823. [Google Scholar]
- 2.Joel J, Thomas J, Gill K, Biyani CS. Testicular sarcoidosis masquerading as testicular carcinoma. Cent European J Urol. 2014;67:261–3. doi: 10.5173/ceju.2014.03.art10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rayson D, Burch PA, Richardson RL. Sarcoidosis and testicular carcinoma. Cancer. 1998;83:337–43. doi: 10.1002/(sici)1097-0142(19980715)83:2<337::aid-cncr18>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 4.Spiekermann C, Kuhlencord M, Huss S, Rudack C, Weiss D. Coexistence of sarcoidosis and metastatic lesions: A diagnostic and therapeutic dilemma. Oncol Lett. 2017;14:7643–52. doi: 10.3892/ol.2017.7247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Riis MG, Juhl KS, Bruun JM. Concomitant sarcoidosis and papillary thyroid cancer with severe hypercalcaemia as the main symptom. BMJ Case Rep 2018. 2018 doi: 10.1136/bcr-2017-222194. pii: bcr-2017-222194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen PR, Kurzrock R. Sarcoidosis and malignancy. Clin Dermatol. 2007;25:326–33. doi: 10.1016/j.clindermatol.2007.03.010. [DOI] [PubMed] [Google Scholar]


