Abstract
Background
Closely spaced birth increases the risk of adverse maternal and child health outcomes. In Ethiopia, the prevalence of short birth spacing was highly variable across studies. Besides, contraceptive use, educational status, and duration of breastfeeding were frequently mentioned factors affecting short birth spacing. Therefore, this meta-analysis aimed to estimate the pooled prevalence of short birth spacing and its association with contraceptive use, educational status, and duration of breastfeeding among reproductive-age women in Ethiopia.
Methods
International databases: Google Scholar, PubMed, CINAHL, Cochrane library, HINARI, and Global Health were searched systematically to identify articles reporting the prevalence of short birth spacing and its association with contraceptive use, educational status, and duration of breastfeeding among reproductive-age women in Ethiopia. The data were analyzed by STATA/SE version-14 statistical software. The random-effect model was used to estimate the pooled prevalence of short birth spacing and the log odds ratio was used to determine the association. Moreover, egger’s test and I-squared statistics were used to assess publication bias and heterogeneity respectively.
Results
After reviewing 511 research articles, a total of nine articles with 5,682 study participants were included in this meta-analysis. The pooled prevalence of short birth spacing in Ethiopia was 46.9% [95% CI: (34.7, 59.1)]. Significant heterogeneity was observed between studies (I2 = 98.4, p <0.001). Not using contraceptives [OR = 3.87, 95% CI: (2.29, 6.53)] and duration of breastfeeding < 24 months [OR = 16.9, 95%CI: (2.69, 106.47)] had a significant association with short birth spacing.
Conclusions
Although a minimum inter-pregnancy interval of two years was recommended by the World Health Organization (WHO), significant numbers of women still practiced short birth spacing in Ethiopia. Duration of breastfeeding and non-use of contraceptives were factors significantly associated with short birth spacing. So, efforts should be made to improve breastfeeding practice and contraceptive utilization among women in Ethiopia.
Introduction
Maternal mortality remains the major public health challenge to the global population. Reports indicated that an estimated 303,000 maternal deaths occurred worldwide and among this, 99% of deaths were from developing countries [1]. The scenario is worst in sub-Saharan Africa (SSA) in which 546 deaths per 100,000 live births were documented as compared to 216 maternal deaths per 100,000 live births worldwide [2, 3]. The recent national health survey data showed that an estimated 412 maternal deaths per 100,000 live births occurred in Ethiopia [4].
Birth spacing, also known as the birth interval is the duration of time between two successive live births [5–7]. World Health Organization (WHO) recommends a minimum inter-pregnancy interval of two years or an inter-birth interval of thirty-three months or more to ensure the maximum health benefits for the mothers and the newborns [8, 9]. Spacing the child for a minimum of two years reduces infant mortality by 50% [10]. There is a significant variation in the practice of birth spacing across developing and developed countries [11]. Women from developing regions usually have short birth spacing than their actual preference [12]. Data from 52 developing countries indicated that over two-thirds of births happened within 30 months since the preceding live birth [13]. Like many other developing countries, short birth spacing is also the problem of Ethiopian in which 41.5% of women practiced short birth spacing [14].
Short birth spacing has been linked with different adverse pregnancy and childbirth outcomes such as low birth weight [15–18], preterm birth [15–20], congenital anomalies [21, 22], autism [23–27], small size for gestational age [15, 20], and neonatal, infant and child mortality [5, 15, 20, 28–31]. Moreover, women with short birth spacing are at high risk of developing hypertensive disorders of pregnancy, anemia, third-trimester bleeding, premature rupture of membranes, and puerperal endometritis [9, 10, 32, 33]. Beyond the maternal and child health implications, closely spaced birth increases population growth, decelerates one’s country economic development, decreases women's productivity, and increases the demand for natural resources [9].
Reducing maternal and neonatal mortality is one of the key targets of Sustainable Development Goals (SDGs) particularly SDG 3 which aimed to reduce the global Maternal Mortality Ratio (MMR) to less than 70 per 100,000 live births and to decrease neonatal mortality below 12 per 1000 live births by the year 2030 [34]. The Ethiopian government is also implementing Health Sector Transformation Plan (HSTP) IV which aimed to reduce MMR from 420 to 199 per 100,000 live births and under five-year, infant and neonatal mortality rates from 64, 44 and 28 to 30, 20 and 10 per 1,000 live births respectively [35]. Optimal birth spacing is an important concept largely used for maternal and child health advocacy, designing family planning policies, and monitoring and evaluation of policies, strategies, and programs related to maternal and child health.
In Ethiopia, different studies were conducted on childbirth spacing [36–44] and a wide range of maternal and service-related factors like maternal educational status [39, 42, 43], contraceptive use [38, 39, 41–44], duration of breastfeeding [39, 42, 43] residence [38, 41], sex of the index child [39, 42], survival status of the index child [38], religion [40], and unwanted pregnancy [40] were identified. However, the prevalence of short birth spacing varies from region to region ranging from 23.3% to 59.9% [39, 40]. In addition to this, there is no country-level study assessing short birth spacing and associated factors among women of childbearing age in Ethiopia. Moreover, maternal educational status, contraceptive use, and duration of breastfeeding are frequently mentioned and clinically important factors affecting short birth spacing even though they have controversial findings across the included articles. Therefore, this meta-analysis aimed to estimate the pooled prevalence of short birth spacing and its association with maternal educational status, contraceptive use, and duration of breastfeeding among reproductive-age women in Ethiopia.
The result of this study will serve as an input for program designers and policymakers to design evidence-based interventions related to child spacing. It will also have paramount importance for future researchers interested in related topics.
Materials and methods
Search strategy
A systematic search was conducted on Google Scholar, PubMed, CINAHL, Cochrane library, HINARI, and Global Health to find both published and unpublished research articles. Besides, Addis Ababa Digital Library was also searched to identify unpublished papers. Grey literatures were identified through the input of content experts and the review of reference lists. The searching was carried out from April 1 up to May 30, 2020, and articles published from 1990 up to May 30, 2020, were included in the review. The Endnote software was used for managing articles and removing duplicates identified by our search strategy. The search strategy includes the following keywords: "proportion", "magnitude", "prevalence", "incidence", "Birth spacing", "child spacing", "birth interval", "suboptimal birth intervals", "short birth spacing", "suboptimal child spacing", "optimal birth spacing", "inter-birth interval", "risk factors", "predictors", "factors", "determinants", "associated factors", "married women", "women", "women of childbearing age", "Ethiopia" independently and in combination using “OR” or “AND” Boolean operators (see S1 File). This systematic review and meta-analysis was organized according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA-2009) checklist [45] (see S1 Table). The protocol of this systematic review and meta-analysis was registered in the international prospective register of systematic reviews (PROSPERO) with a specific registration number: CRD42020160922.
Inclusion and exclusion criteria
Studies conducted in Ethiopia, studies involving women of childbearing age, all types of observational studies (Cross-sectional, case-control, and cohort), published and unpublished articles, full-text articles, articles published from 1990 up to May 30, 2020, and articles written in the English language were included in this study. Whereas relevant articles with full texts of which unavailable after two email contacts of the corresponding authors were excluded.
Outcome measurement
This review measured two main outcomes. The first outcome was the overall pooled prevalence of short birth spacing which was computed by dividing the number of women with short birth spacing to the total sample size multiplied by 100. The second outcome was the association between the duration of breastfeeding, contraceptive use, maternal educational status, and short birth spacing.
Data extraction
Three authors (YD, BK, and MY) independently extracted all the necessary data using a standardized data extraction format. The remaining two authors (MA and BA) solved the disagreement raised at the time of data extraction. The corresponding author of the research article was also contacted for clarification and additional information. Data extraction form includes author name, region, study area, publication year, study design, study setting, sample size, response rate, and the number of women with short birth spacing. For the associated factors, frequencies in the form of two by two tables were extracted, and the log odds ratio for each factor was calculated accordingly.
Quality assessment
BK and MY independently assessed the quality of each research article using the Newcastle-Ottawa quality assessment scale (NOS) [46]. The mean score was taken to solve the disagreements between the two authors.
The quality assessment tool has three subdivisions. The first segment deals with the methodological quality, the second subdivision mainly focuses on the comparability of the study, and the third section deals with the statistical analysis and the outcome of the research article. Finally, studies scoring ≥6 out of 10 scales were considered as high-quality research articles.
Data analysis
The relevant data were extracted using a Microsoft Excel spreadsheet and exported into STATA/SE version-14 statistical software for analysis. The heterogeneity between the included articles was assessed by using a p-value for the I2 test [47]. The random-effect model was used to estimate the Der Simonian and Laird’s pooled effect as a result of significant heterogeneity between the studies. Besides, subgroup analysis by residence, sample size, and the cutoff point used to measure the outcome variable was done to decrease the random variations among the point estimates of original articles.
Univariate meta-regression analysis was also done by taking sample size, publication year, and response rate as covariates. Moreover, the presence of publication bias was assessed using both the funnel plot and Egger’s test at a 5% significant level [48].
The point estimates with their 95% confidence interval were presented using the forest plot and the log odds ratio was used to determine the association between short birth spacing and maternal educational status, contraceptive use, and duration of breastfeeding.
Results
Study selection
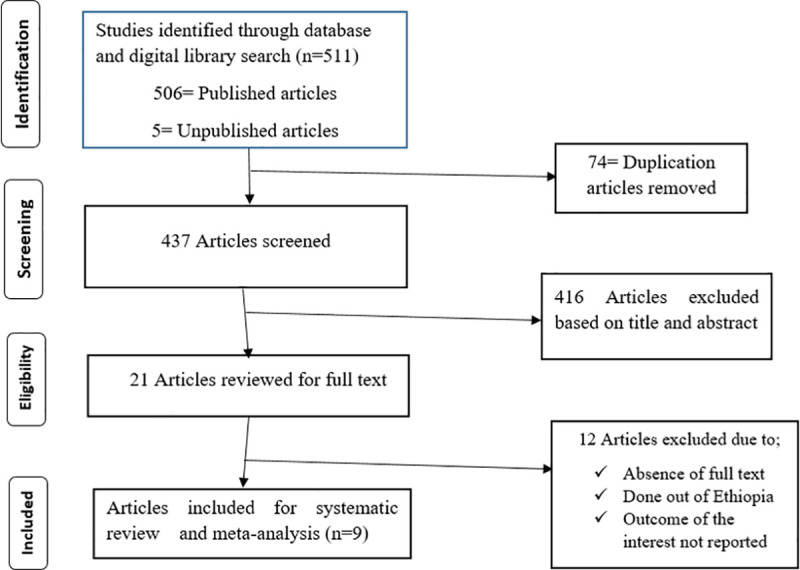
A total of five hundred eleven (511) published and unpublished studies were identified through electronic databases (Google Scholar, PubMed, CINAHL, Cochrane library, Hinari, and Global Health) and digital library search. Of these identified articles, 502 of them were dropped as a result of duplication, by the titles and abstracts, due to the absence of full texts, and as a result of not fulfilling the eligibility criteria. Finally, 9 eligible articles were included for analysis (Fig 1).
Fig 1. PRISMA flow diagram describes the selection of studies for a systematic review and meta-analysis of short birth spacing and its association with maternal educational status, contraceptive use, and duration of breastfeeding in Ethiopia, 2020.
Characteristics of the included studies
A total of 9 research articles published from 2011 up to 2019 were included in this meta-analysis. Among the 9 articles, 6 of them were cross-sectional [36–41], 2 of them were case-control [42, 43] and the remaining 1 study was a retrospective follow-up study [44]. This meta-analysis included 4 studies from Oromia region [36, 38, 39, 43], 2 studies from Amhara region [37, 44], 2 studies from SNNP region [41, 42] and 1study from Tigray region [40] with a sample size ranged from 314 [39] to 811 [38, 41]. From the 9 articles, 6 studies with a total of 3,797 women of childbearing age were included to estimate the pooled prevalence of short birth spacing in Ethiopia. The lowest prevalence of short birth spacing (23.3%) was reported from a study done in the Tselemti district, Tigray region [40] whereas the highest prevalence of short birth spacing (59.9%) was observed from a study done in Serbo town, Oromia region [39]. (Table 1).
Table 1. Descriptive summary of nine studies included in the meta-analysis of short birth spacing and associated factors among women of childbearing age in Ethiopia, 2020.
| Authors | Publication year | Region | Study Area | Study Design | Sample size | Response rate | Prevalence (%) | Quality score |
|---|---|---|---|---|---|---|---|---|
| Shallo and Gobena [36] | 2019 | Oromia | Dodota woreda | cross-sectional | 647 | 98 | 49.1 | 7 |
| Ejigu et al. [37] | 2019 | Amhara | Debre Markos | cross-sectional | 411 | 98.3 | 40.9 | 6 |
| Tsegaye et al. [38] | 2017 | Oromia | Illubabor zone | cross-sectional | 811 | 98.2 | 51.2 | 8 |
| Ayane et al [39] | 2019 | Oromia | Serbo town | cross-sectional | 314 | 100 | 59.9 | 6 |
| Gebrehiwot et al [40] | 2019 | Tigray | Tselemti | cross-sectional | 803 | 99.6 | 23.3 | 7 |
| Yohannes et al [41] | 2011 | SNNP | Lemo district | cross-sectional | 811 | 96.1 | 57 | 8 |
| Hailu et al [42] | 2016 | SNNP | Arba Minch | Case-control | 636 | 100 | -- | 7 |
| Begna et al [43] | 2013 | Oromia | Yaballo Woreda | Case-control | 636 | 97.5 | -- | 8 |
| Tessema et al. [44] | 2013 | Amhara | Dabat district | Retrospective follow up | 613 | 99.5 | -- | 6 |
SSNP; Southern Nations, Nationalities, and Peoples.
Prevalence of short birth spacing in Ethiopia
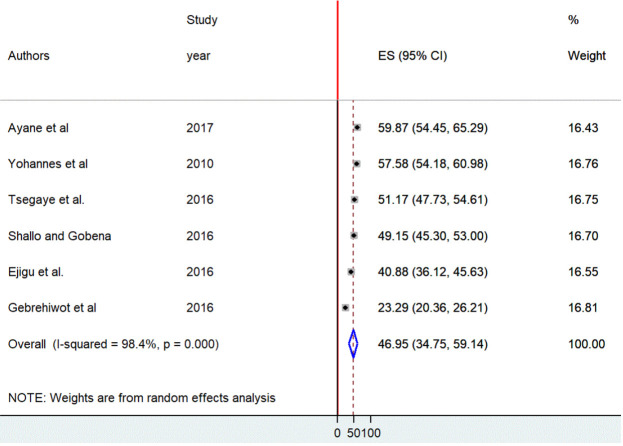
The pooled prevalence of short birth spacing from the six included studies [36–41] in Ethiopia was 46.9%, [95% CI: (34.7, 59.1)]. A random-effect meta-analysis model was used to estimate the pooled prevalence as a result of substantial heterogeneity among the included studies (I2 = 98.4, p <0.001) (Fig 2).
Fig 2. Forest plot of the pooled prevalence of short birth spacing among reproductive-age women in Ethiopia, 2020.
To identify the possible source of heterogeneity, univariate meta-regression was conducted using sample size, publication year, and response rate as a factor, but neither of them were not a significant source of heterogeneity (Table 2).
Table 2. Univariate meta-regression analysis to determine factors related to the heterogeneity of the prevalence of short birth spacing in Ethiopia, 2020.
| Variables | Coefficient | P-value |
|---|---|---|
| Sample size | -0.0412 | 0.357 |
| Response rate | -1.3660 | 0.890 |
| Year of publication | -2.7533 | 0.546 |
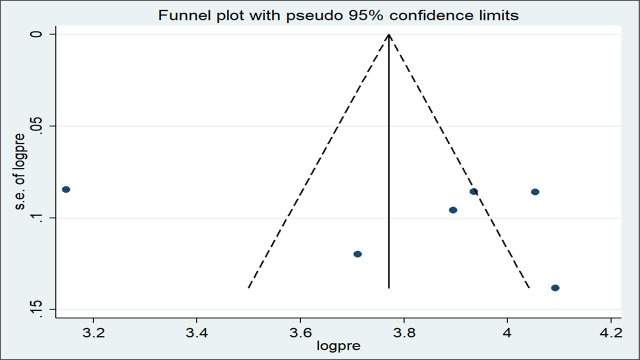
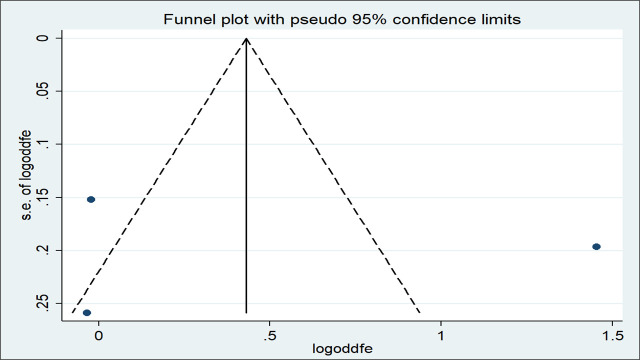
Besides, the funnel plot was visually inspected for symmetry and there was an asymmetrical distribution of the effect estimates (Fig 3). To confirm this, egger’s test was used and the test statistic showed the absence of significant publication bias (p = 0.606).
Fig 3. Funnel plot with 95% confidence limits of the pooled prevalence of short birth spacing among reproductive-age women in Ethiopia, 2020.
Subgroup analysis
Subgroup analysis by residence, sample size, and the cutoff point used to measure the outcome variable was carry out to identify the possible source variation between studies. The analysis showed that residence (both rural and urban) was one of the sources of severe heterogeneity (I2 = 98.4, P = 0.000) (Fig 4). However, severe heterogeneity still existed in the subgroup analysis of studies by sample size and the cutoff point used to measure the outcome variable.
Fig 4. Forest plot of the pooled prevalence of short birth spacing by the area of residence (rural versus both urban and rural) in Ethiopia, 2020.
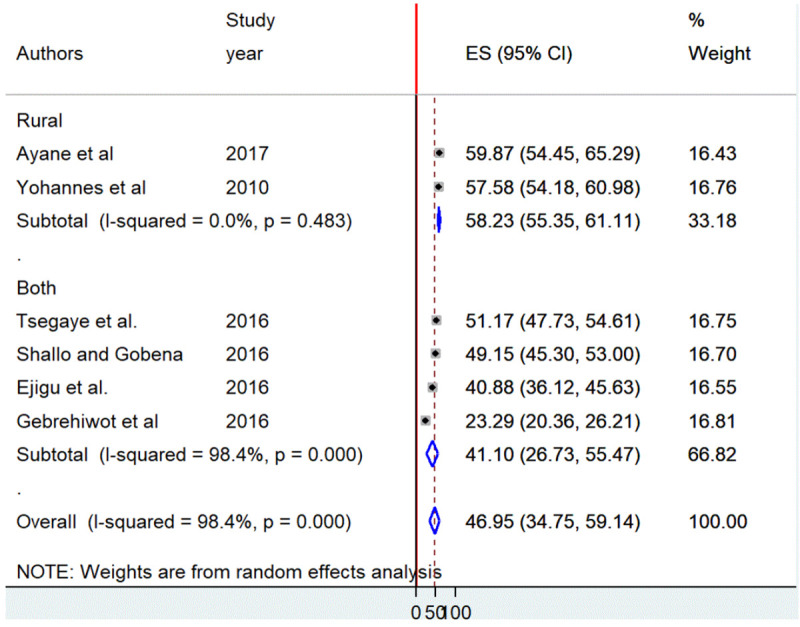
The highest prevalence of short birth spacing (58.2%) was observed among studies conducted in rural settings (58.2%) as compared to both (41.1%) (Table 3).
Table 3. Subgroup prevalence of short birth spacing in Ethiopia, 2020 (n = 6).
| Variables | Characteristics | Included studies | Sample size | Prevalence (95% CI) |
|---|---|---|---|---|
| Residence | Rural and urban | 4 | 2,672 | 41.1 (26.7,55.5) |
| Rural | 2 | 1,125 | 58.2 (55.3,61.1) | |
| Sample size | ≤700 | 3 | 1,372 | 49.9 (40.1, 59.7) |
| >700 | 3 | 2,425 | 44 (22.4,65.6) | |
| Short birth spacing cut off point | <33 months | 3 | 1,861 | 37.7 (20.9,54.5) |
| <36 months | 3 | 1,936 | 56 (50.8, 61.1) |
Factors associated with short birth spacing
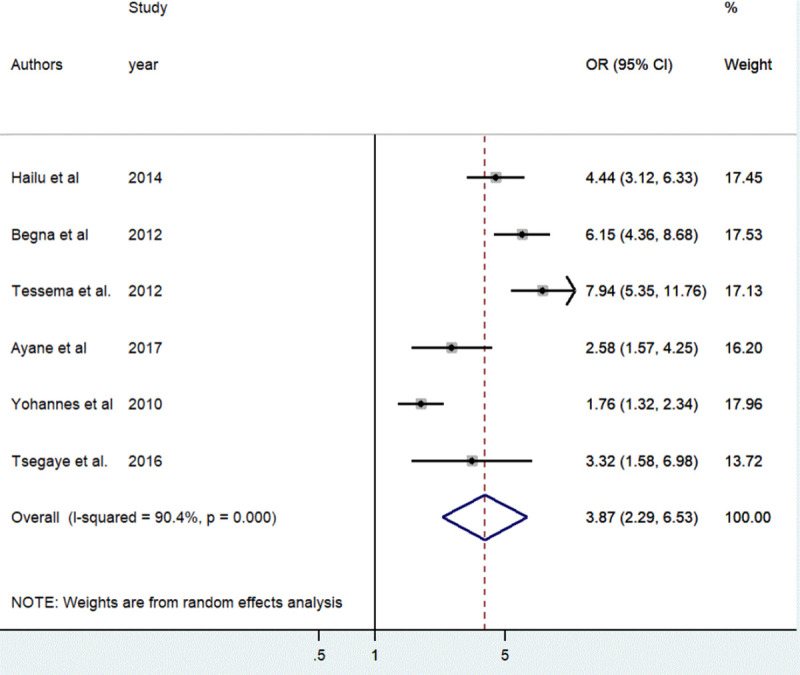
The association between contraceptive non-utilization and short birth spacing was determined based on the result of six studies [38, 39, 41–44]. The result indicated women who had never used contraception before the conception of the last child were 3.87 times more likely to have short birth spacing as compared to women who utilized contraceptive methods [OR = 3.87, 95%, CI: (2.29, 6.53)]. The random effect meta-analysis model was used to examine the association due to the presence of significant heterogeneity (I2 = 90.4%, p<0.001) (Fig 5).
Fig 5. The pooled odds ratio of the association between contraceptive use and short birth spacing in Ethiopia, 2020.
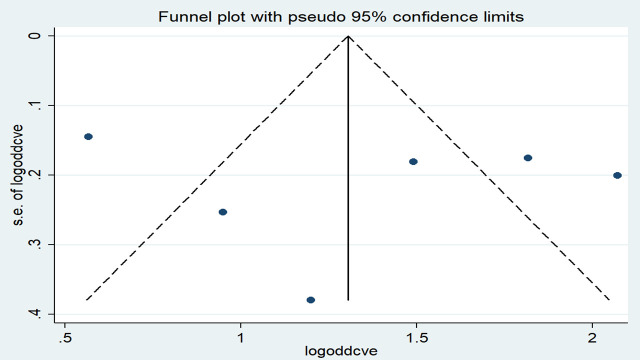
The effect estimates were distributed symmetrically on the funnel plot indicating the absence of publication bias (Fig 6). The result of Egger’s tests also revealed the absence of publication bias (p-value = 0.684).
Fig 6. Funnel plot with 95% confidence limits of the pooled odds ratio of contraceptive use among women in Ethiopia, 2020.
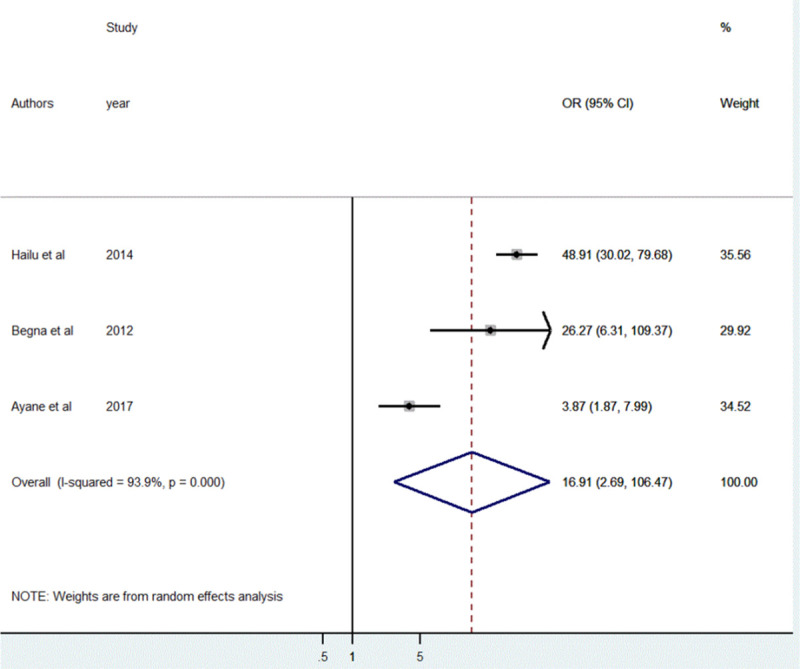
A total of three studies [39, 42, 43] were included to identify the association between the duration of breastfeeding and short birth spacing. The result of the random-effect meta-analysis showed the odds of practicing short birth spacing was 16.9 higher among women who breastfeed their child less than 24 months as compared to women who breastfeed ≥ 24 months [OR = 16.9, 95%CI: (2.69, 106.47)]. High heterogeneity was observed between the included studies (I2 = 93.9%, p<0.001) (Fig 7).
Fig 7. The pooled odds ratio of the association between the duration of breastfeeding and short birth spacing in Ethiopia, 2020.
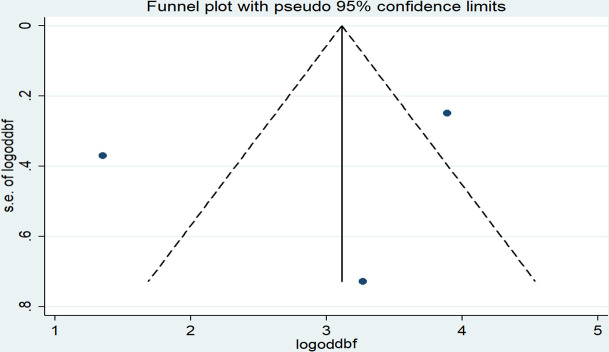
The results of Egger’s tests showed the absence of publication bias (P = 0.748) even though a slight asymmetrical distribution of the effect estimates was observed on the funnel plot (Fig 8).
Fig 8. Funnel plot with 95% confidence limits of the pooled odds ratio of the duration of breastfeeding among women in Ethiopia, 2020.
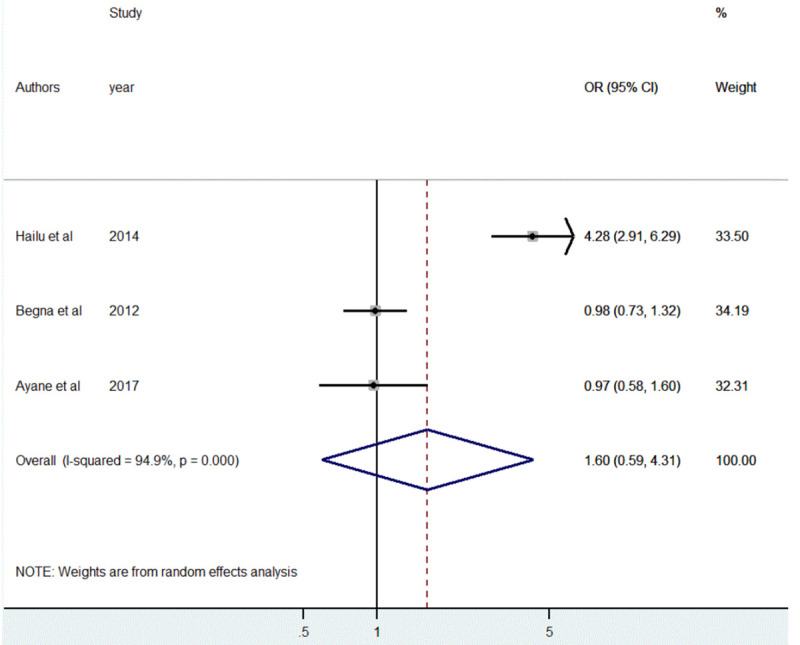
The association between the educational status of the mother and short birth spacing was also assessed based on the results of three studies [39, 42, 43]. But, pooled estimate showed non-significant association [OR = 1.60, 95%CI: (0.59, 4.31)]. The included articles showed significant heterogeneity (I2 = 94.9%, p<0.001) (Fig 9).
Fig 9. The pooled odds ratio of the association between maternal educational status and short birth spacing in Ethiopia, 2020.
The presence of publication bias was assessed using both funnel plots and Egger’s test. The effect estimates were distributed asymmetrically on the funnel plot indicating the presence of publication bias (Fig 10). But Egger’s test objectively confirmed the absence of publication bias (p = 0.876).
Fig 10. Funnel plot with 95% confidence limits of the pooled odds ratio of maternal educational status in Ethiopia, 2020.
Discussion
Although WHO recommended optimal birth spacing to ensure the health of the mother and the newborn [8], 46.9%, [95% CI: (34.7, 59.1)] of reproductive age women practiced short birth spacing in Ethiopia. The finding of this study is in line with the Ethiopian Demographic and Health Survey (EDHS) report (41.5%) [14] and a study done in Tanzania (48.4%) [49]. But, the pooled prevalence of short birth spacing was higher than the studies conducted in Nepal (23%) [50], Bangladesh (24.6%) [18], and Iran (28.5%) [6]. This discrepancy could be due to variation in maternal socio-demographic characteristics, methodological variation (data analysis, study design, and sampling of study participants), the difference in economic status, lifestyle difference, and the difference in the health service utilization. Furthermore, varied study settings (urban and rural) and the difference in the methods applied to measure the outcome variable may have paramount importance for the variation of the findings.
Even if the increasing birth interval was the primary intervention area of the national government, practically, short birth spacing among reproductive-age women was still quite common. Babies delivered from those mothers who practice short birth spacing might experience low birth weight, small for gestational age, preterm birth, and congenital anomalies. Mothers are also at high risk of developing different adverse pregnancy outcomes [15–33]. So, the clinician needs to be aware of different risk factors and should give special emphasis to them in addition to increasing family planning utilization and duration of breastfeeding among women of reproductive age women.
In this study, the result of subgroup analysis by residence (both urban and rural versus rural) indicated, the practice of short birth spacing was significantly higher in rural settings (58.2%) as compared to both (41.1%). This finding is in agreement with the recent EDHS report which indicated that rural women had a high prevalence of short birth spacing than urban women [4]. Access to the health facility, educational, and employment opportunities among women living in urban areas could be responsible for the variation by residence.
Contraceptive non-utilization had a significant association with short birth spacing. This is consistent with studies conducted in Jordan, Manipur, Egypt, Southeastern Nigeria, and Mbarara Hospital [51–55]. The objective of the family planning program is not only to limit the family size but also adequately space the children by delaying pregnancy. Whenever women use contraceptive methods, they are deliberately avoiding short birth spacing and unwanted pregnancy [9].
The duration of breastfeeding also had a significant association with short birth spacing. The finding is in line with studies conducted in Jordan and Southeastern Nigeria [51, 52]. During breastfeeding, a high amount of prolactin hormone is produced as a result of nipple stimulation. The prolactin hormone inhibits ovulation by reducing the release of the gonadotrophic hormone and resulted in post-partum amenorrhea and thereby lengthen the interval between births. On the other hand, a woman with a short duration of breastfeeding might experience short birth spacing as a result of a decreased level of prolactin concentration in the body [56].
Limitations of the study
This systematic review and meta-analysis considered only articles written in English language. Besides, most of the articles included in the analysis were cross-sectional studies and had a small sample size, these might affect the pooled estimates. Conducting meta-analysis with low numbers of studies is another potential limitation of this study which decreases statistical power, permits large standard errors, and leads to publication bias. Moreover, regions may be under-represented since the included studies were from only four regions of Ethiopia.
Conclusions
A significant number of Ethiopian women practiced short birth spacing though a minimum inter-pregnancy interval of two years was recommended by WHO. Duration of breastfeeding and non-use of contraceptives were factors affecting short birth spacing. Based on the finding, Health care providers should counsel women about the importance of optimal birth spacing, breastfeeding, and contraceptive utilization during their antenatal care, delivery, and postnatal care follow-up. Health extension workers should provide house to house education to improve contraceptive utilization and breastfeeding practice in the community.
Supporting information
(DOCX)
(DOC)
(XLSX)
Acknowledgments
The authors would like to acknowledge Wollo and Addis Ababa University Library for providing an available online database.
List of abbreviations
- EDHS
Ethiopia Demographic and Health Survey
- HSTP
Health Sector Transformation Plan
- NOS
Newcastle-Ottawa quality assessment Scale
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- SSA
Sub-Saharan Africa
- SDG
Sustainable Development Goals
- WHO
World Health Organization
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.World Health Organization: Global health observatory (GHO) data. Life expectancy. World Health Organization, Geneva: Available: http://www.who.int/gho/mortality_burden_disease/life_tables/situation_trends_text/en/ Accessed 2016, 20. [Google Scholar]
- 2.World Health Organization: World health statistics 2016: monitoring health for the SDGs sustainable development goals: World Health Organization; 2016. [Google Scholar]
- 3.Alkema L, Chou D, Hogan D, Zhang S, Moller A-B, Gemmill A et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet 2016, 387(10017):462–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Central Statistical Agency (CSA) and ICF. Ethiopia Demographic and Health Survey 2016. Addis Ababa and Rockville: CSA and ICF; 2016. [Google Scholar]
- 5.Rutstein SO: Effects of preceding birth intervals on neonatal, infant and under‐five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. International Journal of Gynecology & Obstetrics 2005, 89:S7–S24. 10.1016/j.ijgo.2004.11.012 [DOI] [PubMed] [Google Scholar]
- 6.Fallahzadeh H, Farajpour Z, Emam Z: Duration and determinants of birth interval in Yazd, Iran: a population study. Iranian Journal of reproductive medicine 2013, 11(5):379 [PMC free article] [PubMed] [Google Scholar]
- 7.Central Statistical Authority. Ethiopia Demographic and Health Survey, Addis Ababa, Ethiopia ICF International Calverton, Maryland, USA: 2011. [Google Scholar]
- 8.World Health Organization: Report of a WHO technical consultation on birth spacing: Geneva, Switzerland 13–15 June 2005 In.: World Health Organization; 2007. [Google Scholar]
- 9.United States Agency for International Development. Strengthening family planning policies and programs in developing countries USAID, Washington, DC, USA: 2005. [Google Scholar]
- 10.DaVanzo J, Razzaque A, Rahman M, Hale L, Ahmed K, Khan MA et al. The effects of birth spacing on infant and child mortality, pregnancy outcomes, and maternal morbidity and mortality in Matlab, Bangladesh. Technical Consultation and Review of the Scientific Evidence for Birth Spacing 2004. [Google Scholar]
- 11.Setty-Venugopal V, Upadhyay UD: Birth spacing: three to five saves lives. 2002. 12134554 [Google Scholar]
- 12.Abdel-Tawab NG, Loza S, Zaki A: Helping Egyptian women achieve optimal birth spacing intervals through fostering linkages between family planning and maternal/child health services. 2008. [Google Scholar]
- 13.Rutstein SO: Further Evidence of the Effects of Preceding Birth Intervals on Neonatal, Infant, and Under-Five-Year Mortality and Nutritional Status in Developing Countries: Evidence from the Demographic and Health Surveys: Macro International; 2008. [DOI] [PubMed] [Google Scholar]
- 14.Ethiopian Demographic and Health survey: Addis Ababa. Ethiopia and Calverton, Maryland, USA: central statistics agency and ORC macro 2011, 2011.
- 15.Grisaru-Granovsky S, Gordon E-S, Haklai Z, Samueloff A, Schimmel MM: Effect of interpregnancy interval on adverse perinatal outcomes—a national study. Contraception 2009, 80(6):512–518. 10.1016/j.contraception.2009.06.006 [DOI] [PubMed] [Google Scholar]
- 16.Adam I, Ismail MH, Nasr AM, Prins MH, Smits LJ: Low birth weight, preterm birth, and short interpregnancy interval in Sudan. The Journal of Maternal-Fetal & Neonatal Medicine 2009, 22(11):1068–1071. [DOI] [PubMed] [Google Scholar]
- 17.Conde‐Agudelo A, Rosas‐Bermudez A, Castaño F, Norton MH: Effects of birth spacing on the maternal, perinatal, infant, and child health: a systematic review of causal mechanisms. Studies in family planning 2012, 43(2):93–114. 10.1111/j.1728-4465.2012.00308.x [DOI] [PubMed] [Google Scholar]
- 18.De Jonge HC, Azad K, Seward N, Kuddus A, Shaha S, Beard J et al. Determinants and consequences of short birth interval in rural Bangladesh: a cross-sectional study. BMC pregnancy and childbirth 2014, 14(1):427 10.1186/s12884-014-0427-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nerlander LM, Callaghan WM, Smith RA, Barfield WD: Short interpregnancy interval associated with preterm birth in US adolescents. Maternal and child health journal 2015, 19(4):850–858. 10.1007/s10995-014-1583-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kozuki N, Lee AC, Silveira MF, Victora CG, Adair L, Humphrey J et al. The associations of birth intervals with small-for-gestational-age, preterm, and neonatal and infant mortality: a meta-analysis. BMC public health 2013, 13(S3): S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kwon S, Lazo-Escalante M, Villaran M, Li C: Relationship between interpregnancy interval and birth defects in Washington State. Journal of Perinatology 2012, 32(1):45–50. 10.1038/jp.2011.49 [DOI] [PubMed] [Google Scholar]
- 22.Chen I, Jhangri GS, Chandra S. Relationship between interpregnancy interval and congenital anomalies. American journal of obstetrics and gynecology. 2014; 210(6):564 10.1016/j.ajog.2014.02.002 [DOI] [PubMed] [Google Scholar]
- 23.Cheslack-Postava K, Liu K, Bearman PS: Closely spaced pregnancies are associated with increased odds of autism in California sibling births. Pediatrics 2011, 127(2):246–253. 10.1542/peds.2010-2371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Conde-Agudelo A, Rosas-Bermúdez A, Kafury-Goeta AC: Birth spacing and risk of adverse perinatal outcomes: a meta-analysis. Jama 2006, 295(15):1809–1823. 10.1001/jama.295.15.1809 [DOI] [PubMed] [Google Scholar]
- 25.Cheslack-Postava K, Suominen A, Jokiranta E, Lehti V, McKeague IW, Sourander A et al. Increased risk of autism spectrum disorders at short and long interpregnancy intervals in Finland. Journal of the American Academy of Child & Adolescent Psychiatry 2014, 53(10):1074–1081. e1074. 10.1016/j.jaac.2014.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durkin MS, DuBois LA, Maenner MJ: Inter-pregnancy intervals and the risk of autism spectrum disorder: results of a population-based study. Journal of autism and developmental disorders 2015, 45(7):2056–2066. 10.1007/s10803-015-2368-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Conde-Agudelo A, Rosas-Bermudez A, Norton MH: Birth spacing and risk of autism and other neurodevelopmental disabilities: a systematic review. Pediatrics 2016, 137(5). 10.1542/peds.2015-3482 [DOI] [PubMed] [Google Scholar]
- 28.Hussaini KS, Ritenour D, Coonrod DV: Interpregnancy intervals and the risk for infant mortality: a case-control study of Arizona infants 2003–2007. Maternal and child health journal 2013, 17(4):646–653. 10.1007/s10995-012-1041-8 [DOI] [PubMed] [Google Scholar]
- 29.Kozuki N, Walker N: Exploring the association between short/long preceding birth intervals and child mortality: using reference birth interval children of the same mother as a comparison. BMC public health 2013, 13(S3): S6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fotso JC, Cleland J, Mberu B, Mutua M, Elungata P: Birth spacing and child mortality: an analysis of prospective data from the Nairobi urban health and demographic surveillance system. Journal of biosocial science 2013, 45(6):779–798. 10.1017/S0021932012000570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dadi AF: Short birth intervals less than 2 years double under-one mortality in Ethiopia: evidence from a meta-analysis. Science 2014, 2(6):589–595. [Google Scholar]
- 32.Van Lerberghe W: The World Health Report 2005: Make every mother and child count: World Health Organization; 2005. [Google Scholar]
- 33.Grundy E, Kravdal Ø: Do short birth intervals have long-term implications for parental health? Results from analyses of complete cohort Norwegian register data. J Epidemiol Community Health 2014, 68(10):958–964. 10.1136/jech-2014-204191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sustainable development goals. Transforming our world: 2015, 2030:338–350. [Google Scholar]
- 35.Federal Ministry of Health: Health sector transformation plan (HSTP)-2015/16–2019/20 Ethiopia Ministry of Health; 2015. [Google Scholar]
- 36.Yadeta D, Seifadin A: Duration of Birth Interval and Associated Factors among Married Women in Dodota Woreda, Arsi Zone, Ethiopia Haramaya University; 2016. [Google Scholar]
- 37.Ejigu AG, Yismaw AE, Limenih MA: The effect of sex of the last child on short birth interval practice: the case of northern Ethiopian pregnant women. BMC research notes 2019, 12(1):75 10.1186/s13104-019-4110-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tsegaye D, Shuremu M, Bidira K: Practice of child spacing and its associated factors among women of childbearing age (15 to 49 years) in Illubabor zone, South West Ethiopia. International Journal of Nursing and Midwifery 2017, 9(7):102–108. [Google Scholar]
- 39.Ayane GB, Desta KW, Demissie BW, Assefa NA, Woldemariam EB: Suboptimal child spacing practice and its associated factors among women of childbearing age in Serbo town, JIMMA zone, Southwest Ethiopia. Contraception and Reproductive Medicine 2019, 4(1):4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gebrehiwot SW, Abera G, Tesfay K, Tilahun W: Short birth interval and associated factors among women of childbearing age in northern Ethiopia, 2016. BMC women's health 2019, 19(1):85 10.1186/s12905-019-0776-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yohannes S, Wondafrash M, Abera M, Girma E: Duration and determinants of the birth interval among women of childbearing age in Southern Ethiopia. BMC pregnancy and childbirth 2011, 11(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hailu D, Gulte T: Determinants of short Interbirth interval among reproductive age mothers in Arba Minch District, Ethiopia. International journal of reproductive medicine 2016, 2016 10.1155/2016/6072437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Begna Z, Assegid S, Kassahun W, Gerbaba M: Determinants of the interbirth interval among married women living in rural pastoral communities of southern Ethiopia: a case-control study. BMC pregnancy and childbirth 2013, 13(1):116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tessema GA, Zeleke BM, Ayele TA: Birth interval and its predictors among married women in Dabat District, Northwest Ethiopia: A retrospective follow up study. African journal of reproductive health 2013, 17(2):39–45. [PubMed] [Google Scholar]
- 45.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Newcastle-Ottawa Scale customized for cross-sectional studies. In. available from https://static-content.springer.com/esm/…/12889_2012_5111.
- 47.Rücker G, Schwarzer G, Carpenter JR, Schumacher M: Undue reliance on I 2 in assessing heterogeneity may mislead. BMC medical research methodology 2008, 8(1):79 10.1186/1471-2288-8-79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Egger M, Smith GD, Schneider M, Minder C: Bias in meta-analysis detected by a simple, graphical test. Bmj 1997, 315(7109):629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Exavery A, Mrema S, Shamte A, Bietsch K, Mosha D, Mbaruku G et al. Levels and correlates of non-adherence to WHO recommended inter-birth intervals in Rufiji, Tanzania. BMC pregnancy and childbirth 2012, 12(1):152 10.1186/1471-2393-12-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Karkee R, Lee AH: Birth spacing of pregnant women in Nepal: a community-based study. Frontiers in Public Health 2016, 4:205 10.3389/fpubh.2016.00205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dim C, Ugwu E, Iloghalu E: Duration and determinants of the inter-birth interval among women in Enugu, south-eastern Nigeria. Journal of Obstetrics and Gynaecology 2013, 33(2):175–179. 10.3109/01443615.2012.747494 [DOI] [PubMed] [Google Scholar]
- 52.Youssef RM: Duration and determinants of interbirth interval: a community-based survey of women in southern Jordan. EMHJ-Eastern Mediterranean Health Journal, 11 (4), 559–572, 2005 2005. [PubMed] [Google Scholar]
- 53.Mayanja Ronald M, Mubiru Musa M, Masembe Sezalio M, Nkonwa Innocent M: Factors Associated with Short Births Intervals among Women Delivering at Mbarara Hospital. Age, 15(19):20–30. [Google Scholar]
- 54.Baschieri A, Hinde A: The proximate determinants of fertility and birth intervals in Egypt: An application of calendar data. Demographic Research 2007, 16:59–96. [Google Scholar]
- 55.Singh SN, Singh SN, Narendra R: Demographic and socio-economic determinants of birth interval dynamics in Manipur: A survival analysis. Online Journal of Health and Allied Sciences 2011, 9(4). [Google Scholar]
- 56.Labbok M: Breastfeeding, fertility, and family planning. Glob Libr women's med 2018. [Google Scholar]