Abstract
COVID-19 had led to severe clinical manifestations. In the current scenario, 98 794 942 people are infected, and it has responsible for 2 124 193 deaths around the world as reported by World Health Organization on 25 January 2021. Telemedicine has become a critical technology for providing medical care to patients by trying to reduce transmission of the virus among patients, families, and doctors. The economic consequences of coronavirus have affected the entire world and disrupted daily life in many countries. The development of telemedicine applications and eHealth services can significantly help to manage pandemic worldwide better. Consequently, the main objective of this paper is to present a systematic review of the implementation of telemedicine and e-health systems in the combat to COVID-19. The main contribution is to present a comprehensive description of the state of the art considering the domain areas, organizations, funding agencies, researcher units and authors involved. The results show that the United States and China have the most significant number of studies representing 42.11% and 31.58%, respectively. Furthermore, 35 different research units and 9 funding agencies are involved in the application of telemedicine systems to combat COVID-19.
Keywords: Telemedicine, e-Health, COVID-19, Literature, Systems
Introduction
COVID-19 is an acute respiratory disease considered the third documented propagation of an animal coronavirus in humans [1, 2]. This virus has become a pandemic with severe clinical manifestations. In the current situation, 98 794 942 people are infected, and it has responsible for 2 124 193 deaths around the world as reported by World Health Organization on 25 January 2021 [3]. This large-scale pandemic imposes extraordinary demands on the world’s health systems, attacks vulnerable populations, and threatens global communities in an unprecedented way [4]. Researchers are working hard to detect the virus, provide treatments, and develop vaccines [5]. However, the technologies and systems to address disease emergence, stop its propagation and prevent disease are vitally important [6, 7].
Telemedicine and eHealth represent the contribution of a new technology that combines the exchange of knowledge between health professionals and gives patients access to quality services [8]. Its applications improve the availability of various medical services and health care despite geographic and economic barriers such as home health control, ensuring that elderly patients can lead independent lives and reducing direct and indirect costs. They also help patients with minor diseases to get the supportive care they need while minimizing their exposure to other patients with acute conditions [9, 10].
Telemedicine has become a critical technology for providing medical care to patients by trying to reduce transmission of the virus among patients, families, and doctors. In the case of hospitals, strict limitations on visitors have meant that some consultation programs of palliative care for inpatient are doing family meetings and consultations virtually [11]. Using eHealth apps helps to mitigate the propagation of COVID-19 and preserve the lives of medical personnel. The use of virtual platforms for medical care reduces the saturation of emergency patients during the pandemic [12, 13]. These virtual platforms can be used by smartphones or webcam computers and allow clinicians to effectively detect patients with early signs of COVID-19 before they arrive at the hospital [14, 15].
The economic consequences of coronavirus have affected the entire world and disrupted daily life in many countries. The development of telemedicine applications and eHealth services can significantly help to manage pandemic worldwide better [16]. Hence, in this study, we present a systematic review of the literature regarding the current situation on telemedicine and mobile health applications to face the current pandemic scenario. Therefore, the main objective of this paper is to present a systematic review of the application of telemedicine and e-health systems to combat COVID-19. Furthermore, the main contribution of this paper is to present a comprehensive description of the state of the art in this field considering the domain areas, organizations, funding agencies, researcher units and authors involved.
The paper has the following structure: Section 2 describes the methods applied in the review. Section 3 states the results of the relevant articles found. Finally, in Sect. 4, the results achieved are discussed, and in Sect. 5, the conclusions of this paper are presented.
Methods
The proposed literature review aims to present a systematic information extraction from the application of mobile health applications regarding the current pandemic public challenge of COVID-19. This systematic review has been conducted on 15/5/2020, and the papers have been selected by common agreement of all authors. Taking into account the proliferation of a high number of publications regarding this topic as preprints or in non-indexed journals and conferences, this paper reviews the documents published in peer-reviewed journals indexed in the journal citation reports (JCR). This indexation is considered as the most relevant index available. Moreover, the Web of Science database includes the most relevant journals of the most reputable publishers.
Furthermore, the authors aim to find the common objectives, outcomes and limitations of the applications of mobile health to face the current pandemic scenario. A biometric analysis is conducted to make a summary about the countries, regions, domains and authors who are employing mobile health solutions to promote health and well-being and combat the critical new virus.
The methods used in this literature review includes multiple steps that start with the definition of the keywords used to search the relevant papers. Second, the research objectives have been formulated. Consequently, the extracted documents from the Web of Science selection have been selected based on the title and abstract. The relevant studies have been selected for full review, and several have been excluded since do not meet the inclusion criteria. The final selection of papers that met the selection criteria have been analysed for data extraction.
Research questions
This review aims to serve as a first situation report about the most recent mobile health applications to face the current pandemic scenario. Therefore, the authors want to answer the following research questions that will support the ongoing research activities in the mobile health domain:
RQ1: What are the different areas of research that are proposing the use of telemedicine systems regarding the current pandemic scenario?
RQ2: Which are the organizations and institutions that are working in this field?
RQ3: Which are the funding agencies that are supporting the current research in this field?
RQ4: Who are the top authors involved in the development of telemedicine in the current pandemic scenario?
RQ5: Where is the location of the studies about the application of telemedicine concerning the current pandemic scenario?
Search strategy, inclusion criteria and study selection
The current pandemic scenario has shown the crucial importance of cross-domain research and the application of mobile health. Furthermore, the present situation brings together researchers from multiple fields that joint efforts to combat COVID-19. Mobile health includes two major domain fields, such as computer science and medical field. The high proliferation of non-peer-reviewed papers concerning the current pandemic scenario is evident. However, there is a critical problem emergence from the spread of non-validated results that can also provide fake and limited outcomes for further research activities. Therefore, this systematic literature review only considers the most reputable journals included in JCR.
Moreover, the authors only consider the articles and do not have regarded as other document types such as editorial material and letters. Since the objective is to analyse the mobile health initiatives, the review papers have also been removed from our analysis. These search queries have been selected by the authors and applied in the web of science database from Clarivate Analytics. The defined keywords are “coronavirus”, COVID-19”, “SARS-CoV-2″, “telemedicine”, “eHealth”, “telehealth”, “mobile health”, and “mHeatlh”. Consequently, the search string used is: ((coronavirus or COVID-19 or SARS-CoV-2) and (telemedicine or eHealth or Telehealth or mHeatlh or mobile health)). This research has been applied, considering all the document fields. The search query has been applied in on 15th May 2020.
The inclusion criteria defined by the authors were divided into five requirements such as 1) the paper has been published after 2020; 2) the included documents are articles; 3) the selected papers propose the application of mobile health regarding the current pandemic scenario, 4) the paper is indexed in a peer-reviewed journal included in the JCR, and 5) the study does not include only a recommendation of mobile health technologies.
The search query has initially returned 85 publications. After applying the inclusion criteria, 1) the results have been reduced to 74. The inclusion criteria two have limited the considered papers to 48 since 15 are editorial material, 8 letters and 3 reviews. Furthermore, 5 documents have been removed since they do not meet the inclusion criteria 4, resulting in 43 papers. Following the abstract and title analysis, 20 papers have been removed. Finally, after full review, 4 articles have been excluded since they according to the inclusion criteria 5. The PRISMA diagram is presented in Fig. 1.
Fig. 1.
PRISMA diagram for proposed literature review
Results and discussion
Nowadays, many countries have successfully integrated telemedicine and advanced technologies into a wide range of healthcare processes including diagnosis, disease prevention, treatment and health research. The benefits of using these telemedicine and eHealth technologies in epidemics such as the current COVID-19, allow helping patients with chronic diseases who need follow-up and medical attention, reducing their exposure in hospital centres.
In this systematic review, we found a total of 19 relevant studies that base their research on the analysis of the current situation on mobile health applications to face the present pandemic scenario.
Due to the social isolation that the COVID-19 pandemic has generated, different studies focus on using telemedicine to support patients who need medical and psychological help. In [17], the authors implement a process of multidisciplinary telemedicine clinics to preserve the care model for patients with cystic fibrosis. The study was performed at the University of Virginia, with a total of 63 patients. The results achieved show that the multidisciplinary team attended 60% of patients through telemedicine. This systematic process of design and testing demonstrates that through telemedicine, viable and sustainable programs can be created and adapted to the context.
In [18], the authors show the importance of eHealth to avoid depression in patients who feel alone and maintain their life quality during serious diseases. They describe patient participation in healthcare at the individual and organizational level when it comes to eHealth urgent solutions for COVID-19. Based on case histories in public media in which patients and families share their experiences during isolation and quarantine with the virus. They analysed a list of 8 functionalities of eHealth tools in an eHealth centre in Denmark during COVID-19, demonstrating that for 7 features, patient participation can be an essential element that improves the meaning of the tool, to ensure compliance and adherence, and integrating needs.
In [19], the authors analyse the importance of telehealth applied to Mental Health. They highlight the use of telemedicine as a valuable way of meeting the physical and psychosocial needs of patients, independently of their geographical location. The main challenge that the authors describe is to provide mental health services in the context of patient isolation, highlighting the telehealth role through videoconference, email and smartphone applications. They show how the use of telehealth systems allows sharing information on symptoms of exhaustion, depression and anxiety during the COVID-19, offer the cognitive ability, treat minor symptoms, and encourage access to online self-help programs.
A complementary and effective strategy to slow the virus propagation and reduce the impact is to track the primary and secondary contacts of COVID-19 confirmed cases using tracking technology. For this reason, in [20], the authors present an exploratory review of the current measures implemented in the world to trace contacts of cases confirmed by COVID-19 and propose recommendations on how Nigeria can adopt this approach while adhering to the guidelines provided by the National Data Protection Regulations (NDPR). The study shows that mobile phone location data can be used effectively in Nigeria in response to COVID-19. Furthermore, the authors suggest that the government can take advantage of existing mobile technologies and infrastructure available to optimize the monitoring and surveillance of ongoing contacts of more than 9000 known contacts of confirmed cases. Moreover, taking into account the NDPR for protecting people’s data and avoid a violation of privacy right.
On the other hand, the use of videoconferencing platforms has been of great help in providing training to health personnel facing the COVID-19. The authors of [21] propose the application of the Kirkpatrick model in a training program for nurses. This application has been conducted at the department of emergency surgery during COVID-19 pandemic in China. The study includes 35 nurses who were trained according to the clinical program during the epidemic. The application of the Kirkpatrick model based on the clinical market during COVID-19 confirms that it is useful for the nurse training program of the emergency surgery department. Improving nurse knowledge and skills during the pandemic is also beneficial, serving as a positive influence on the clinical reference.
In [22], the authors analyse the effect of applying the combined mode of the micro-video of Massive Open Online Course (MOOC) during the epidemic period COVID-19 in the practice of distance teaching of interns in the emergency department. The study involved 60 interns in nursing practices at Tongji Hospital, China. The results show that compared to traditional teaching methods, the effect of the combined mode of micro-video MOOC in nursing practice is the same as that of conventional teaching methods. Still, satisfaction is more significant, so it is best suited to be used in nursing practice during the epidemic period of COVID-19, to reduce cross-infection among doctors effectively, nurses and teaching personnel.
In [23], the authors provide orientation for researchers transitioning from in-person evaluations and interventions to a synchronous videoconferencing platform. They show the challenges to consider for the implementation of videoconferencing, such as the development of protocols. These protocols will simplify the process and help reduce unexpected problems. Protocols for facilitators and personnel should include standards to promote data privacy and confidentiality. In this way, the transition to videoconferencing can help ensure continuity of research and to benefit from potentially meaningful social interaction during isolation time.
Part of the relevant studies found in the review focus on analyzing the use of telemedicine and eHealth to face pandemics such as COVID-19. In the study [24], the authors propose hospitalization services for patients with neurological diseases through teleconferencing platforms at the Medical University of South Carolina. Medical records are completed remotely by all team members as well as virtual "table rounds," and academic discussions are concluded via the teleconferencing platform each morning before clinical rounds. In this way, they can optimize the use of telehealth services in neurology and significantly help reduce virus propagation.
In [25], the authors analyse the benefits of using telehealth technology in previous epidemics and how they can influence the management of COVID-19. The authors show that to control the rapid propagation of coronavirus better and manage the COVID-19 crisis, both developed and developing countries can improve the efficiency of their health system by replacing a proportion of clinical patient encounters with a telehealth system. Hence, providing therapeutic diagnostic and follow-up services for patients with COVID-19 through telemedicine may be the right solution.
In [26], the authors show telemedicine in Italy under the management of COVID-19. The authors state a limited availability of telemedicine systems to manage locked-up patients with chronic diseases. In recent years, health authorities have ignored requests from various experts and professionals in the sector for the efficient implementation and integration of telemedicine services in the national health system. The authors show that telemedicine should not be considered as a possible option or complement to react to an emergency, but as a proactive approach to guarantee continuity of care for patients suffering from chronic diseases.
The authors of [27] present a mobile telehealth system (MTS) applied to facilitate the presentation of patient information and the discussion of cases among professionals. The MTS provides epidemiological medical personnel members with a concise interface and tracks patient information, which is stored on the hospital intranet and uses five modules to display patient information. The system uses mobile collaboration technology to present patient information and support case discussion, thus providing benefits for professionals and reducing physical contact.
In [28], the authors explore the role of Internet hospitals in the prevention and control of the COVID-19 epidemic in China. A total of 4913 online queries related to the pandemic were collected. The results show that 94.20% (n = 4628) of the consulted patients had symptoms related to the epidemic with a distribution similar to COVID-19. These hospitals have enabled essential medical support to the public during the pandemic, reduce social panic, promote social distancing and enhance the public’s self-protection capacity.
In the study [29], the authors implement an online/offline multidisciplinary quarantine observation model for epidemic prevention and control, analyzing the successful recovery of a mild and severe patient. The model allowed medical experts to monitor disease progression in both and the treatment of patients that ultimately resulted in a successful recovery. This model applies to the current COVID-19 epidemic and can actively promote the management of mild suspected or confirmed cases, the monitoring of critical incidents and self-management of discharged patients.
The essential requirements to ensure the use of telemedicine systems in COVID-19 pandemic are discussed in [30]. The authors show the benefits of telemedicine by highlighting its ability to quickly deploy a large number of providers, deliver medical services when local clinics or hospitals are damaged or cannot meet demand; and decrease the risk of contagious diseases by contact.
In [31], the authors describe the implementation of capabilities by UW Medicine Information Technology Services (ITS) to support the clinical response to the COVID-19 pandemic and provide recommendations for consideration by the Health systems. They analyze the management of control processes to quickly update Electronic Health Records (EHR) with new clinical and laboratory workflows. Therefore, the authors' recommendations include establishing a hospital incident command structure that provides for close integration with IT, optimize emergency communication for personnel and patients, preparing human resources, security and equipment to support the transition of all staff not essential for teleworking.
In the study [32], the authors review the transition from a new LGBTQ clinic to telemedicine and the implications for providing HIV prevention and care services during COVID-19. Open Door Health (ODH) is the first clinic dedicated to providing primary and sexual healthcare to the LGBTQ community in Rhode Island. It offers phone calls when patients have technological challenges with videoconferencing and completes pre-appointment documentation on the patient portal with electronic medical records. Moreover, this provider includes consent forms, demographic information, and social and medical histories. Both patients and providers report high levels of satisfaction with telemedicine, and providers can overcome most obstacles in providing clinical services.
In countries such as Afghanistan where war and social conflict have been going on for many years, the use of telemedicine platforms would allow better management of the COVID-19 pandemic [33]. Healthcare workers need consultation and support on a global scale, creating small consultation networks using mobile apps could deliver better health outcomes. Telemedicine in countries like this could help provide clinical services, drug testing and vaccines that are currently being developed worldwide.
Based on the situation we are going through with COVID-19, integrated healthcare providers such as HealthPartners with based in Minnesota have reinforced their telemedicine infrastructure to deal with the pandemic [34]. This organization is currently providing hospital medications coverage outside the hours of patient care in five rural hospitals and critical access; for this, they use commercial telemedicine carts in hospitals and home laptop computers provided by the company. They have also increased capacity at two large tertiary care hospitals by adding webcams to existing mobile workstations and purchasing new laptops for new telemedicine providers. The main barriers found in this process include cost and equipment testing.
In the study [35], the authors show the use of telehealth in postoperative visits to minimize patient exposure during the pandemic. The study presents a medical case in which they use a passive and self-extracting drainage dressing after a neck dissection to facilitate the discharge process during the day and the postoperative follow-up through telehealth. The results were favourable since the patient removed the bandage and drainage at home during a telehealth visit on postoperative day 4, healing without any sign of infection.
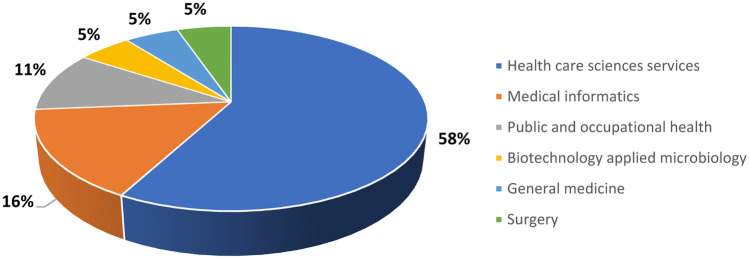
Table 1 shows the research domain area of the analysed proposals on the application of telemedicine systems. Moreover, Fig. 2 presents the percentage of the papers for each research domain area.
Table 1.
Category of the research domain area
Fig. 2.
Percentage category of the research domain area
In total, 58% of the analysed literature have been published in health care sciences services journals (N = 12). Moreover, 16% (3) of the selected papers have been published in medical informatics journals and 11% (2) in the public and occupational health domain. Finally, biotechnology applied microbiology, general medicine and surgery count with one published paper each.
The results of our review show us the leading research organizations found in the literature that are involved in the fight against COVID-19, as well as the funding agencies that support the research (See Table 2 and Table 3).
Table 2.
Research organizations involved in the study of telemedicine applied to COVID-19 pandemic
| Organization | References | % |
|---|---|---|
| Huazhong University of Science Technology | [21, 22, 29] | 15.79% |
| University of Queensland | [19, 25, 30] | 15.79% |
| University of Southern Denmark | [19, 30] | 10.53% |
| Acibadem Hospitals Group | [33] | 5.26% |
| Brown University | [32] | 5.26% |
| Fac Hlth | [18] | 5.26% |
| Hans Christian Andersen Childrens Hosp | [30] | 5.26% |
| Harvard Medical School | [30] | 5.26% |
| Healthpartners Institute for Education Research | [34] | 5.26% |
| Istanbul Medeniyet University | [33] | 5.26% |
| Italian Inst Telemed | [26] | 5.26% |
| Kerman University of Medical Sciences | [25] | 5.26% |
| Medical University of South Carolina | [24] | 5.26% |
| Rhode Isl Publ Hlth Inst | [32] | 5.26% |
| Rigshospitalet | [18] | 5.26% |
| Seattle Children S Hospital | [31] | 5.26% |
| Sechenov First Moscow State Medical University | [26] | 5.26% |
| Serat Hosp | [33] | 5.26% |
| State University System of Florida | [23] | 5.26% |
| Tallinn University of Technology | [20] | 5.26% |
| Tehran University of Medical Sciences | [25] | 5.26% |
| Tianjin Normal University | [19] | 5.26% |
| Uc San Diego Health | [35] | 5.26% |
| University of California San Diego | [35] | 5.26% |
| University of Copenhagen | [18] | 5.26% |
| University of Malta | [20] | 5.26% |
| University of South Florida | [23] | 5.26% |
| University of Virginia | [17] | 5.26% |
| University of Washington | [31] | 5.26% |
| Uw Med | [31] | 5.26% |
| Xiamen University | [28] | 5.26% |
| Yale University | [23] | 5.26% |
| Zhejiang University | [21] | 5.26% |
| Zhengzhou University | [27] | 5.26% |
| Zoenet Hlth Co Ltd | [28] | 5.26% |
Table 3.
Funding agencies that are supporting the study of telemedicine applied to COVID-19 pandemic
| Funding Agencies | References | % |
|---|---|---|
| National Health and Medical Research Council of Australia | [19, 30] | 10.53% |
| Cystic Fibrosis Foundation Care Center Grant | [17] | 5.26% |
| Cystic Fibrosis Learning Network Grant | [17] | 5.26% |
| Huazhong University of Science and Technology | [29] | 5.26% |
| National Institutes of HeUSAh Nih USA | [23] | 5.26% |
| Nih National Cancer Institute Nci | [23] | 5.26% |
| Nih National Institute of Mental Health Nimh | [23] | 5.26% |
| Special Project for COVID 19 Prevention and Control Of Xiamen City | [28] | 5.26% |
| United States Department of Health Human Services | [23] | 5.26% |
| Vertex Pharmaceuticals | [17] | 5.26% |
According to Table 2, 35 different organizations are involved in the application of telemedicine systems to combat COVID-19. The three top organizations who are researching telemedicine applied to the COVID-19 pandemic scenario are the Huazhong University of Science Technology, the University of Queensland, and the University of Southern Denmark. On the one hand, the Huazhong University of Science Technology and the University of Queensland are responsible for 15.79% of the analysed studies (N = 3). One the other hand, University of Southern Denmark is involved in two studies and represents 10.53%. Finally, it must be noted that the collaboration of different institutions has conducted in most of the analysed papers.
The funding agencies that are supporting the study of telemedicine applied to COVID-19 pandemic are presented in Table 3.
In total, ten different agencies are supporting the research on telemedicine solutions applied to the COVID-19 pandemic. The National Health and Medical Research Council of Australia is involved in two research works. Moreover, the research work presented by the authors of [23] is supported by four agencies, and the study proposed by [17] involves three different agencies.
Furthermore, Table 4 highlight the authors with more than two research papers in the telemedicine, considering the analysed literature.
Table 4.
Top authors in the relevant papers
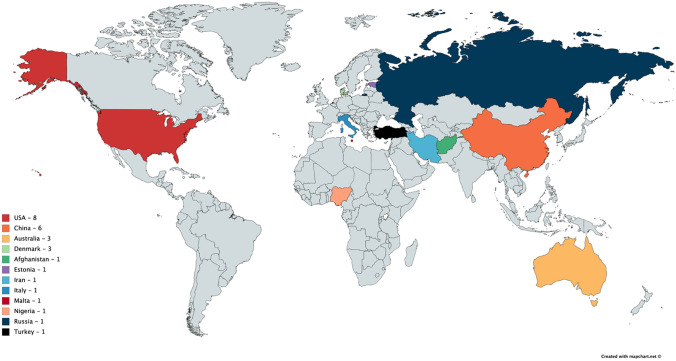
According to Table 4, Huang SF is involved in three different studies. Moreover, Cheng J, Smith AC, Snoswell CL, Xiao YR and Zhou T collaborate in more than one research study. Figure 3 presents graphical information about the countries of the authors involved in the analysed studies.
Fig. 3.
Countries of the authors involved in the analysed studies
Table 5 presents the countries of the authors involved in the analysed studies. The United States and China have the most significant number of studies found in the literature and that have been relevant to our review; with 42.11% and 31.58%, respectively. In total, 12 different countries have work on the application of telemedicine systems on this pandemic scenario. However, countries such as Brazil, United Kingdom, Spain, France, Germany and India that are in the top of the most affected locations considering the number of total deaths originated by the COVID-19 are not presented in any of the analysed research studies.
Table 5.
Countries of the studies included in the review
| Country | References | Total | % |
|---|---|---|---|
| USA | [17, 23, 24, 30–32, 34, 35] | 8 | 42.11% |
| China | [19, 21, 22, 27–29] | 6 | 31.58% |
| Australia | [19, 25, 30] | 3 | 15.79% |
| Denmark | [18, 19, [30] | 3 | 15.79% |
| Afghanistan | [33] | 1 | 5.26% |
| Estonia | [20] | 1 | 5.26% |
| Iran | [25] | 1 | 5.26% |
| Italy | [26] | 1 | 5.26% |
| Malta | [20] | 1 | 5.26% |
| Nigeria | [20] | 1 | 5.26% |
| Russia | [26] | 1 | 5.26% |
| Turkey | [33] | 1 | 5.26% |
It has been proven the interest of the international community on COVID-19 topic. Also, the applicability of telemedicine and e-health systems on COVID-19 issue or similar pandemic situations is very promising. However, there are some limitations related for instance the quality of the open data available for research. An important challenge concerning cleaning and reliable data is denoted. Finally, a recent study related to risks of emergency use authorizations for medical products during outbreak situations states the limitation regarding the need for an evidence-based regulatory framework [36].
Conclusions
This paper presents a state-of-the-art analysis of telemedicine and e-health systems that have emerged in the current pandemic scenario. Furthermore, the authors have shown a comprehensive on the domain areas, organizations, funding agencies, researcher units and authors involved in this field. This systematic review paper has been carried following the PRISMA guidelines. In total, this review includes 19 research proposals from 12 different countries have work on the application of telemedicine systems on this pandemic scenario. The authors have systematically analysed the included studies and answered the following research questions:
RQ1: What are the different areas of research that are proposing the use of telemedicine systems regarding the current pandemic scenario? The definition and implementation of telemedicine systems involve a cross-domain research approach that includes healthcare sciences services, medical informatics, public and occupational health, biotechnology applied microbiology, general medicine and surgery.
RQ2: Which are the organizations and intuitions that are working in this field? In total, 35 different organizations are involved in the application of telemedicine systems to combat COVID-19.
RQ3: Which are the funding agencies that are supporting the current research in this field? In total, ten different agencies are supporting the research on telemedicine solutions applied to the COVID-19 pandemic.
RQ4: Who are the top authors involved in the development of telemedicine in the current pandemic scenario? Huang SF is involved in three different studies. Moreover, Cheng J, Smith AC, Snoswell CL, Xiao YR and Zhou T collaborate in more than one research study.
RQ5: What location of the studies about the application of telemedicine concerning the current pandemic scenario? The use of telemedicine systems involves 12 different countries. Moreover, the United States and China have the most significant number of studies representing 42.11% and 31.58%, respectively
Nevertheless, this systematic review has limitations. This literature review only considers the most reputable journals included in JCR since there is a significant spread of non-peer-reviewed papers that can also provide fake and limited outcomes for further research activities.
In summary, the application of telemedicine and e-health systems involves a cross-domain research approach and is used by numerous authors from distinct locations. Furthermore, telemedicine plays a critical role to ensure continuous access to healthcare in lockdown scenarios. Consequently, it is necessary to ensure the quality and privacy of these architectures to offer efficient methods and approaches for enhanced public health and well-being.
Acknowledgments
This study was supported by the grants HAZITEK and IT-905-16 from Basque Country Government.
Declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Susel Góngora Alonso, Email: susel.gongora@uva.es.
Goncalo Marques, Email: goncalosantosmarques@gmail.com.
Isidro Barrachina, Email: isidrosanjose@telefonica.net.
Begonya Garcia-Zapirain, Email: mbgarciazapi@deusto.es.
Jon Arambarri, Email: jon.arambarri@uneatlantico.es.
Javier Cabo Salvador, Email: jcabo@telefonica.net.
Isabel de la Torre Díez, Email: isator@tel.uva.es.
References
- 1.Portnoy J, Waller M, Elliott T. Telemedicine in the Era of COVID-19. J Allergy Clin Immunol: In Practice. 2020. [DOI] [PMC free article] [PubMed]
- 2.Tolone S, Gambardella C, Brusciano L, Genio G, Del Lucido FS, Docimo L. Telephonic triage before surgical ward admission and telemedicine during COVID-19 outbreak in Italy. Effective and easy procedures to reduce in-hospital positivity. Int J Surg. 2020;78, 123–125. 10.1016/j.ijsu.2020.04.060. [DOI] [PMC free article] [PubMed]
- 3.WHO, (Accessed on 25 Jan) https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 4.Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diabetes Metab Syndr: Clin Res Rev. 2020;14:273–276. doi: 10.1016/j.dsx.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohammed MA, Abdulkareem KH, Al-Waisy AS, Mostafa SA, Al-Fahdawi S, Dinar AM, Alhakami W, Baz A, Al-Mhiqani MN, Alhakami H, Arbaiy N, Maashi MS, Mutlag AA, Garcia-Zapirain B, de la Torre Diez I. Benchmarking Methodology for Selection of Optimal COVID-19 Diagnostic Model Based on Entropy and TOPSIS Methods. IEEE Access. 2020;1–1. 10.1109/ACCESS.2020.2995597.
- 6.Ding XR, Clifton D, Ji N, Lovell NH, Bonato P, Chen W, Yu X, Xue Z, Xiang T, Long X, Xu K, Jiang X, Wang Q, Yin B, Feng G, Zhang Y. Wearable Sensing and Telehealth Technology with Potential Applications in the Coronavirus Pandemic. IEEE Rev Biomed Eng. 2020 doi: 10.1109/RBME.2020.2992838. [DOI] [PubMed] [Google Scholar]
- 7.Smith WR, Atala AJ, Terlecki RP, Kelly EE, Matthews CA. Implementation Guide for Rapid Integration of an Outpatient Telemedicine Program during the COVID-19 Pandemic. J Am Coll Surg. 2020 doi: 10.1016/j.jamcollsurg.2020.04.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abo-Zahhad M, Ahmed SM, Elnahas O. A wireless emergency telemedicine system for patients monitoring and diagnosis. Int J Telemed App. 2014;4 . 10.1155/2014/380787. [DOI] [PMC free article] [PubMed]
- 9.De la Torre Díez I, Góngora Alonso S, Hamrioui Sofiane, López-Coronado Miguel, Motta Cruz E. Systematic Review about QoS and QoE in Telemedicine and eHealth Services and Applications. J Med Syst. 2018;42, 182. [DOI] [PubMed]
- 10.Kamsu-Foguem B, Foguem C. Telemedicine and mobile health with integrative medicine in developing countries. Health Policy Technol. 2014;3:264–271. doi: 10.1016/j.hlpt.2014.08.008. [DOI] [Google Scholar]
- 11.Calton B, Abedini N, Fratkin M. Telemedicine in the Time of Coronavirus. J Pain Symptom Manage. 2020 doi: 10.1016/j.jpainsymman.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc. 2020 doi: 10.1093/jamia/ocaa072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang C, Xu X, Cai Y, Ge Q, Zeng G, Li X, Zhang W, Ji C, Yang L. Mining the Characteristics of COVID-19 Patients in China: Analysis of Social Media Posts Corresponding Author : J Med Internet Res. 2020;22, e19087. 10.2196/19087. [DOI] [PMC free article] [PubMed]
- 14.Moazzami B, Razavi-Khorasani N, Dooghaie Moghadam A, Farokhi E, Rezaei N. COVID-19 and telemedicine: Immediate action required for maintaining healthcare providers well-being. J Clin Virol. 2020;126:104345. doi: 10.1016/j.jcv.2020.104345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gadzinski AJ, Andino JJ, Odisho AY, Watts KL, Gore JL, Ellimoottil C. Telemedicine and eConsults for Hospitalized Patients During COVID-19. Urology. 2020 doi: 10.1016/j.urology.2020.04.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh RP, Javaid M, Kataria R, Tyagi M, Haleem A, Suman R. Significant applications of virtual reality for COVID-19 pandemic. Diabetes Metab Syndr: Clin Res Rev. 2020;14:661–664. doi: 10.1016/j.dsx.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Compton M, Soper M, Reilly B, Gettle L, List R, Bailey M, Bruschwein H, Somerville L, Albon D. A Feasibility Study of Urgent Implementation of Cystic Fibrosis Multidisciplinary Telemedicine Clinic in the Face of COVID-19 Pandemic: Single-Center Experience. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0091. [DOI] [PubMed] [Google Scholar]
- 18.Pappot N, Taarnhoj GA, Pappot H. Telemedicine and e-Health Solutions for COVID-19: Patients’ Perspective. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0099. [DOI] [PubMed] [Google Scholar]
- 19.Zhou X, Snoswell CL, Harding LE, Bambling M, Edirippulige S, Bai X, Smith AC. The Role of Telehealth in Reducing the Mental Health Burden from COVID-19. Telemedicine and e-Health. 2020;26:377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
- 20.Ekong I, Chukwu E, Chukwu M. COVID-19 Mobile Positioning Data Contact Tracing and Patient Privacy Regulations: Exploratory Search of Global Response Strategies and the Use of Digital Tools in Nigeria. JMIR mHealth and uHealth. 2020;8. 10.2196/19139. [DOI] [PMC free article] [PubMed]
- 21.Li Z, Cheng J, Zhou T, Wang S, Huang S, Wang H. Evaluating a Nurse Training Program in the Emergency Surgery Department Based on the Kirkpatrick’s Model and Clinical Demand During the COVID-19 Pandemic. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0089. [DOI] [PubMed] [Google Scholar]
- 22.Zhou T, Huang S, Cheng J, Xiao Y. The Distance Teaching Practice of Combined Mode of Massive Open Online Course Micro-Video for Interns in Emergency Department During the COVID-19 Epidemic Period. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0079. [DOI] [PubMed] [Google Scholar]
- 23.Marhefka S, Lockhart E, Turner D. Achieve Research Continuity During Social Distancing by Rapidly Implementing Individual and Group Videoconferencing with Participants: Key Considerations, Best Practices, and Protocols. AIDS Behav. 2020 doi: 10.1007/s10461-020-02837-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al Kasab S, Almallouhi E, Holmstedt CA. Optimizing the Use Of Teleneurology During the COVID-19 Pandemic. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0109. [DOI] [PubMed] [Google Scholar]
- 25.Keshvardoost S, Bahaadinbeigy K, Fatehi F. Role of Telehealth in the Management of COVID-19: Lessons Learned from Previous SARS, MERS, and Ebola Outbreaks. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0105. [DOI] [PubMed] [Google Scholar]
- 26.Omboni S. Telemedicine During The COVID-19 in Italy: A Missed Opportunity? Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ren X, Zhai Y, Song X, Wang Z, Dou D, Li Y. The Application of Mobile Telehealth System to Facilitate Patient Information Presentation and Case Discussion. Telemedicine and e-Health. 2020 doi: 10.1089/tmj.2020.0084. [DOI] [PubMed] [Google Scholar]
- 28.Gong K, Xu Z, Cai Z, Chen Y, Wang Z. Internet Hospitals Help Prevent and Control the Epidemic of COVID-19 in China: Multicenter User Profiling Study. J Med Internet Res. 2020;22. 10.2196/18908. [DOI] [PMC free article] [PubMed]
- 29.Huang S, Xiao Y, Yan L, Deng J, He M, Lu J, Ke S. Implications for Online Management: Two Cases with COVID-19. Telemedicine and e-Health. 2020;26:487–494. doi: 10.1089/tmj.2020.0066. [DOI] [PubMed] [Google Scholar]
- 30.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, Caffery LJ. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare. 2020;1–5. 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed]
- 31.Grange ES, Neil EJ, Stoffel M, Singh AP, Tseng E, Resco-Summers K, Fellner BJ, Lynch JB, Mathias PC, Mauritz-Miller K, Sutton PR, Leu MG. Responding to COVID-19: The UW Medicine Information Technology Services Experience. App Clin Inform. 2020;11:265–275. doi: 10.1055/s-0040-1709715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rogers BG, Coats CS, Adams E, Murphy M, Stewart C, Arnold T, Chan PA, Nunn A. Development of Telemedicine Infrastructure at an LGBTQ+ Clinic to Support HIV Prevention and Care in Response to COVID-19, Providence. RI AIDS and Behavior. 2020 doi: 10.1007/s10461-020-02895-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Azizy A, Fayaz M, Agirbasli M. Do Not Forget Afghanistan in Times of COVID-19: Telemedicine and the Internet of Things to Strengthen Planetary Health Systems. OMICS: J Integr Biol. 2020 . 10.1089/omi.2020.0053. [DOI] [PubMed]
- 34.Doshi A, Platt Y, Dressen JR, Mathews BK, Siy JC. Keep Calm and Log On: Telemedicine for COVID-19 Pandemic Response. J Hosp Med. 2020;15, 302–304. 10.12788/jhm.3419. [DOI] [PubMed]
- 35.Qualliotine JR, Orosco RK. Self-removing passive drain to facilitate postoperative care via telehealth during the COVID-19 pandemic. Head & Neck. 2020;1–3. 10.1002/hed.26203. [DOI] [PMC free article] [PubMed]
- 36.Badnjević A, Pokvić LG, Džemić Z, Bečić F. Risks of emergency use authorizations for medical products during outbreak situations: a COVID-19 case study. BioMedical Engineering OnLine. 2020;19:75. doi: 10.1186/s12938-020-00820-0. [DOI] [PMC free article] [PubMed] [Google Scholar]