Abstract
Introduction:
Monteggia fracture dislocations are a relatively rare entity and they represent less than 2% of forearm fractures, the diagnosis can be missed in up to 50% of the time. The gold standard of treatment in adults has been open reduction and internal fixation, and closed reduction and cast immobilization in pediatrics.
Case Report:
We present three cases series of neglected Monteggia fractures in a 5-, 4-, and 9-year-old patients. The patients presented 10, 20, and 25 days post-injury, respectively. Each case was treated differently with the last case requiring open reduction and annular ligament reconstruction. All the three cases showed excellent results on follow-up.
Conclusion:
To avoid missing these injuries, each patient should undergo a comprehensive clinical approach and adequate radiological imaging. Various treatment methods exist for neglected Monteggia fracture and each option should be exhausted to salvage the radial head starting with the less invasive approaches.
Keywords: Monteggia, fracture dislocation, neglected
Learning Point of the Article:
Monteggia fractures in children should be managed in a timley fashion as missing them can lead to dreadful complications, time till management and age directly correlate with the outcomes of these fractures.
Introduction
Monteggia fractures represent a unique entity of forearm fractures, they were first described by Rang Monteggia [1], and they represent a proximal ulna shaft fracture with associated proximal radial head dislocation. However, some authors subsequently described Monteggia fractures as any ulna shaft fracture – not only proximal – with associated radioulnar dislocation [2]. Bado has classified Monteggia fractures into four types, type 1 is an ulna shaft fracture with anterior radial head dislocation, type 2 is an ulna shaft fracture with posterior radial head dislocation, type 3 is an ulna shaft fracture with anterior lateral head dislocation, and type 4 is an ulna shaft fracture with fracture of the radius and a dislocation in any direction [3]. A variant of this fracture in pediatrics is plastic deformation of the ulna without a fracture and radial head dislocation [4]. Monteggia fractures represent approximately 1.7 of all forearm fractures [3] and are considered relatively rare injury with a high likelihood of the injury being missed especially if it’s a pediatric Monteggia variant [4]. Classically, the treatment of Monteggia fractures in adults is open reduction of the ulna and internal fixation with the radial head spontaneously reducing [5]. In pediatrics, on the other hand, it has been closed reduction and splinting with some author’s recommending internal fixation regardless of the age depending on the fracture pattern of the ulna [6, 7]. There have been few reports of neglected Monteggia fractures in pediatrics, therefore, we present a case series of three neglected cases who have been treated differently.
Case 1
History
A 5-year-old medically free female presented to us after falling down 10 days ago. She went to the Emergency Room immediately following her fall complaining of the left arm pain, she was discharged on a splint and paracetamol with the diagnosis of a greenstick fracture of her left ulna by the ER physician (Fig. 1, 2). The pain has shown little improvement and she refused to move her arm completely. She had no other complaints on systemic review.
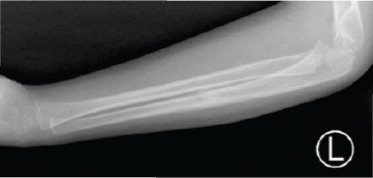
Figure 1.

XR of Case 1 on initial visit to ER.
Figure 2.

XR of Case 1 on initial visit to ER clearly showing a Monteggia fracture.
Physical examination
The child was generally well and she was holding her left elbow in a flexed position, the left forearm and elbow showed mild swelling, she was uncooperative with the range of motion examination, and she was guarding her left arm. Distal neurovascular examination was intact.
Diagnosis
On reviewing her X-rays at the time of diagnosis, the lateral elbow X-ray has clearly shown a radial head dislocation with a proximal ulna fracture, the anteroposterior (AP) X-ray was poor quality and did not show any fracture (Fig. 2), on repeating the forearm X-ray, a complete fracture of the ulna shaft was noted (Fig. 3).
Figure 3.

XR showing complete fracture of the ulna shaft.
Treatment
The patient was admitted for further treatment and consented for closed reduction under general anesthesia with the possibility of internal fixation versus open reduction and internal fixation. Intraoperatively, the patient was placed supine with the left arm on the arm board and was draped with strict aseptic technique due to the possibility of converting to open reduction. The traction-countertraction method was used to obtain reduction and slight pressure on the radial head to reduce it in place. The radial head was reduced and after a trial of range of motion and intraoperative fluoroscopy it was found to be stable, the patient was placed in an above elbow cast in slight hyperflexion to maintain reduction (Fig. 4, 5).
Figure 4.

XR of Case 1 following closed reduction and cast application.
Figure 5.

XR of Case 1 following closed reduction and cast application.
Follow-up
The patient was kept for 24 h postoperatively to monitor the neurovascular status, she was discharged and given follow-ups at 2, 4, and 6 weeks. The cast was removed 6 weeks post-operative (Fig. 6, 7) and the patient experienced slight elbow stiffness as expected. The patient was not given a formal physical therapy referral and the family was instructed with home exercises and where educated to advocate the patient to use his injured limb, at 12 weeks, the patient had full range of motion of the left arm and elbow and was discharged.
Figure 6.

Case 1 XR after cast removal.
Figure 7.
Case 1 XR after cast removal.
Case 2
History
A 4-year-old medically free girl came to our clinic for routine follow-up 3 weeks after falling on her right elbow. She came to the Emergency Room complaining of elbow pain and swelling after falling from the couch, she was seen by the oncall junior orthopedic resident and discharged on above elbow splint with the diagnosis of proximal ulna fracture, (Fig. 8, 9) show her X-rays on presentation.
Figure 8.

Case 8 XR showing a Monteggia fracture.
Figure 9.

Case 2 XR showing inadequate imaging.
Physical examination
The splint was removed and the patient looked generally well on examination, she was guarding her right limb making the examination difficult, but she showed no obvious swelling or deformity. Distal neurovascular examination was intact.
Diagnosis
On reviewing the X-rays at her initial visit to the Emergency Room, it was clear that the patient sustained a Monteggia fracture dislocation (Fig. 8). The AP X-ray was also of poor quality and they also did not remove her bracelet (Fig. 9). Repeat X-rays have shown the same diagnosis with the radial head dislocated.
Treatment
The patient was admitted for further treatment and consented for closed reduction under general anesthesia with the possibility of internal fixation versus open reduction and internal fixation. Intraoperatively, closed reduction was unsuccessful although various methods have been used, subsequently, a trial of antegrade percutaneous pinning of the ulna was attempted and closed reduction was achieved with the radial head reduced and stable (Fig. 10, 11). However, range of motion was limited, particularly extension which was attributed to the time the radial head remained dislocated and splinted. Finally, the patient was placed in an above elbow splint in slight hyperflexion.
Figure 10.

Case 2 intraoperative XR.
Figure 11.

Case 2 intraoperative XR after splint application.
Follow-up
The patient was kept for 24 h postoperatively to monitor the neurovascular status, she was discharged and given follow-ups at 3, 6, and 12 weeks. At the 3 weeks follow-up, the K-wires were removed and the fracture showed radiographic union (Fig. 12, 13). A formal supervised physical therapy protocol was initiated to overcome the patient’s elbow stiffness which consisted of flexion and extension exercises with the proper motivation for her age which included reaching for toys to play with them while being advocated by the parents not to use the uninjured limb, and at the 6-month follow-up, the patient showed near full range of motion and was discharged from our service.
Figure 12.
Case 2 after K-wire removal.
Figure 13.

Case 2 after K-wire removal.
Case 3
History
A 9-year-old medically free boy presented to our emergency 25 days after sustaining an open ulna fracture following a motorbike accident. The patient was seen at a peripheral primary healthcare center, the wound was small as per the family description, it was cleaned and covered and his X-ray showed and ulna fracture which his was given an above elbow splint and due to the unavailability of an orthopedic surgeon, he was asked to visit a higher center.
Physical examination
The patient was thin and below the 50th percentile for his weight, he was uncomfortable and the local examination showed a small 1 cm healed scar on the surface of the ulna with a mild deformity. Wrist and shoulder examination were intact but his elbow range of motion was limited to 70–110° of flexion. His distal neurovascular examination was intact.
Diagnosis
On reviewing his X-ray at presentation, it showed a proximal ulna fracture with associated radial head dislocation (Fig. 14, 15).
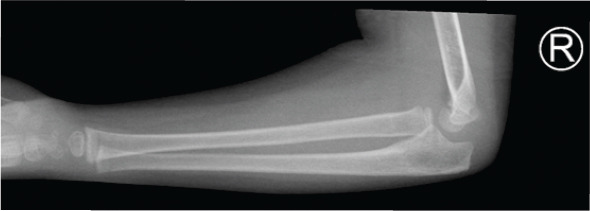
Figure 14.

Case 3 XR on initial presentation.
Figure 15.

Case 3 XR on initial presentation.
Treatment
The patient was admitted and the social services were informed to rule out non-accidental injury or neglect and they concluded that there was no concern or suspicion and the family was undereducated with 14 kids and came from a low socioeconomic status. The patient was consented for closed reduction under general anesthesia with the possibility of internal fixation versus open reduction and internal fixation. Although closed reduction would be likely unsuccessful, it was attempted regardless to ovoid open reduction. After failure of closed reduction, an antegrade flexible nail was inserted, and the proximal and distal segment were manipulated and the radial head was still irreducible, open reduction was performed using the Kocher interval and removal of the interposed soft tissue was performed along with annular ligament repair. Two antegrade flexible nails were inserted to optimize the stability and provide more rigid fixation. Although the reduction was found to be stable, intraoperative range of motion was found to be significantly limited, especially extension. The patient was placed then in an above elbow splint in slight hyperflexion to maintain the reduction (Fig. 16, 17).
Figure 16.

Case 3 post-operative XR.
Figure 17.

Case 3 post-operative XR.
Follow-up
The patient was kept for 48 h postoperatively to monitor the neurovascular status and to discuss with the family the intraoperative findings, he was discharged and given follow-ups at 2, 6, and 8 weeks. At the 8 weeks follow-up, the patient was readmitted as a day surgery case and the flexible nails were removed and the fracture showed radiographic union (Fig. 18, 19). A formal supervised physical therapy protocol was initiated to overcome the patient’s elbow stiffness which included flexion and extension exercises, and at the 6-month follow-up, the patient showed drastic improvement in range of motion but still not acceptable for his age, the patient continued formal physical therapy for 6 months in the form of weight-assisted exercises and at 1 year, he showed a 30–120 flexion and extension arc and near full pronosupination.
Figure 18.

Case 3 XR at radiographic union.
Figure 19.

Case 3 XR at radiographic union.
Discussion
Monteggia first named this fracture after he himself had missed the injury in 1814 [1], and although rare, these fractures are missed at up to 50% of the time [8]. To avoid missing these injuries, a thorough comprehensive assessment should be initiated starting with the emergency physician assessment followed by an orthopedic assessment and in our experience, pediatric injuries are the most common missed injuries, especially elbow fractures and dislocations. Therefore, when it comes to pediatric injuries a senior or attending orthopedic should be involved in the clinical assessment and the radiologic evaluations, if not achievable, a close follow-up no longer than 1 week should be provided with all precautions being taken just in case an injury is present. As seen in Case 3, there was a 25-day delay to final diagnosis and treatment which may have played a role in increasing the difficulty of intraoperative reduction, necessity of annular ligament reconstruction, and prolonged post-operative rehabilitation to achieve acceptable range of motion. In one case series, it has been shown that ages above 10 years old and intervals more than 12 months were associated with worse outcomes and increased complications [9].
All the cases in this series had one thing in common which is inadequate radiological imaging which has aided in neglecting these injuries. Advanced imaging is not routinely indicated for acute management, the gold standard for diagnosis is plain X-rays provided that the imaging is adequate the fracture and dislocation will be evident, computed tomography and magnetic resonance imaging may be used to assess non-union or triangular fibrocartilage complex tears and interosseous membrane disruptions, respectively [10]. Inadequate radiographic imaging is an extremely common problem in the orthopedic practice, but only a few data has been reported regarding this issue. Parker in 2017 has reviewed 1531 pelvic radiographs from three different institutions and has found that 51.9% of these images were suboptimal and up to 19% necessitated repeat imaging [11]. Another report published by the British Medical Journal Quality Improvement Program to assess the adequacy of shoulder X-ray series showed that only 19.4% of anteroposterior and 57% of axillary views were adequate, therefore, a multimodality comprehensive educational package was delivered to radiographers and they found a significant reduction in the rate of inadequate and repeat imaging [12]. Thukral has given the following recommendations to optimize pediatric skeletal radiography: Optimizing the environment to be more pediatric friendly (painting walls), gaining the patient’s trust, sedatives in long or extensive studies, minimizing radiation, and proper training to deal with pediatric patients [13]. We suggest simple proper anteroposterior and lateral radiography for diagnosis, oblique views can be obtained to further asses the fracture characteristics and rotation, we do not recommend advanced imaging unless the injury is neglected and complications are suspected.
Various treatment methods have been proposed for acute Monteggia fractures in the pediatric population, with closed reduction and cast immobilization in incomplete fractures and plastic deformation being the gold standard, however, there is some controversy regarding the management of complete fractures as some authors propose internal fixation of the ulnar fracture [14].
In the case that the fracture has been neglected for a period of time, the radial head will undergo dysplastic changes that will alter the treatment regimen and possibly affect the outcome [15, 16]. With that being said, chronic or neglected Monteggia fractures have a wider spectrum of management depending on the reducibility and whether the radial head has undergone dysplastic changes. If the radial head is irreducible by close methods of after fixation of the ulna open reduction using the Boyd or the Kocher approach remains the gold standard [17]. Ulnar osteotomy has also been key procedure in restoring the anatomical relationship of the radius relative to the ulna as the main deformity is angulation of the ulna which is opposite to the dislocation and ulnar shortening [18]. Reconstruction of the annular ligament remains an area of controversy as some authors believe that it is no longer necessary after the ulnar osteotomy [19]. One study showed that there was no difference in outcomes between patients that underwent ulnar osteotomy with or without annular ligament reconstruction [20]. After undergoing ulnar osteotomy, the radial head should be tested for stability, if it remains unstable then reconstruction or repair if the annular ligament is recommended [21]. If the radial head remains unstable following ulnar osteotomy and annular ligament reconstruction, the a transcapitellar K-wire may be used [4], but if no instability exists, then studies have not shown any difference in outcomes with our without K-wires [22]. Finally, radial head excision has been previously used, and although it can improve the rotation, it has been showed to lead to valgus instability, proximal migration of the radius, elbow pain, and poor patient satisfaction and outcomes and should be avoided [22, 23].
Conclusion
Although Monteggia fractures are a relatively rare entity, each patient should undergo a comprehensive evaluation and proper and adequate radiographic views should be obtained especially in pediatric patients as suboptimal imaging can lead to dreadful results. In case that no injury is found, it is recommended that a close follow-up should be given for further evaluation possibly by a more experienced surgeon. In the case that a neglected Monteggia fracture is encountered, a wide array of surgical treatment exists including closed reduction, open reduction, internal fixation, ulnar osteotomy, and annular ligament reconstruction. Each treatment method should be used cautiously along with its specific indications.
Clinical Message.
Monteggia fractures represent a unique entity of forearm injuries, especially in children, a thorough evaluation should be done in order not to miss these injuries, in the case that they are missed or neglected, every treatment method should be exhausted to salvage the radial head starting with the less invasive options.
Biography

Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that Informed consent of the patient is taken for publication of this case report
References
- 1.Rang M. Philadelphia, PA: W.B. Saunders Company; 2000. The Story of Orthopaedic; pp. 407–8. [Google Scholar]
- 2.Speed JS, Boyd HB. Treatment of fractures of ulna with dislocation of head of radius (Monteggia fracture) JAMA. 1940;115:1699–705. [Google Scholar]
- 3.Bado JL. The Monteggia lesion. Clin Orthop Relat Res. 1967;50:71–86. [PubMed] [Google Scholar]
- 4.David-West KS, Wilson NI, Sherlock DA, Bennet GC. Missed Monteggia injuries. Injury. 2005;36:1206–9. doi: 10.1016/j.injury.2004.12.033. [DOI] [PubMed] [Google Scholar]
- 5.Reckling FW. Unstable fracture-dislocations of the forearm (Monteggia and Galeazzi lesions) J Bone Joint Surg Am. 1982;64:857–63. [PubMed] [Google Scholar]
- 6.Olney BW, Menelaus MB. Monteggia and equivalent lesions in childhood. J Pediatr Orthop. 1989;9:219–23. [PubMed] [Google Scholar]
- 7.Ring D, Waters PM. Operative fixation of Monteggia fractures in children. J Bone Joint Surg Br. 1996;78:734–9. [PubMed] [Google Scholar]
- 8.Dormans JP, Rang M. The problem of Monteggia fracture-dislocations in children. Orthop Clin North Am. 1990;21:251–6. [PubMed] [Google Scholar]
- 9.Atiç R, Yıldırım A, Yig?it S?, Aydın A. Neglected Monteggia fracture-dislocations in children. J Clin Anal Med. 2018;9:323–8. [Google Scholar]
- 10.Johnson NP, Silberman M. Treasure Island (FL): StatPearls Publishing; 2020. Monteggia Fractures. [PubMed] [Google Scholar]
- 11.Parker S, Nagra NS, Kulkarni K, Pegrum J, Barry S, Hughes R, et al. Inadequate pelvic radiographs: Implications of not getting it right the first time. Ann R Coll Surg Engl. 2017;99:534–9. doi: 10.1308/rcsann.2017.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Richards B, Riley J, Saithna A. Improving the diagnostic quality and adequacy of shoulder radiographs in a district general hospital. BMJ Qual Improv Rep. 2016;5:u209855. doi: 10.1136/bmjquality.u209855.w3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thukral BB. Problems and preferences in pediatric imaging. Indian J Radiol Imaging. 2015;25:359–64. doi: 10.4103/0971-3026.169466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ring D, Jupiter JB, Waters PM. Monteggia fractures in children and adults. J Am Acad Orthop Surg. 1998;6:215–24. doi: 10.5435/00124635-199807000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Chen WS. Late neuropathy in chronic dislocation of the radial head. Report of two cases. Acta Orthop Scand. 1992;63:343–4. doi: 10.3109/17453679209154798. [DOI] [PubMed] [Google Scholar]
- 16.Jacobsen K, Holm O. Chronic Monteggia injury in a child. Ugeskr Laeger. 1998;160:4222–3. [PubMed] [Google Scholar]
- 17.Eygendaal D, Hillen RJ. Open reduction and corrective ulnar osteotomy for missed radial head dislocations in children. Strategies Trauma Limb Reconstr. 2007;2:31–4. doi: 10.1007/s11751-007-0013-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jesse BJ, Diego LF, Scott L, Robert WW. Reconstruction of posttraumatic disorders of the forearm. J Bone Joint Surg Am. 2009;91:2730–9. doi: 10.2106/00004623-200911000-00027. [DOI] [PubMed] [Google Scholar]
- 19.Degreef I, De Smet L. Missed radial head dislocations in children associated with ulnar deformation:Treatment by open reduction and ulnar osteotomy. J Orthop Trauma. 2004;18:375–8. doi: 10.1097/00005131-200407000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Rahbek O, Deutch SR, Kold S, Søjbjerg JO, Møller-Madsen B. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J Child Orthop. 2011;5:449–57. doi: 10.1007/s11832-011-0372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bhaskar A. Missed Monteggia fracture in children:Is annular ligament reconstruction always required? Indian J Orthop. 2009;43:389–95. doi: 10.4103/0019-5413.55978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jepegnanam TS. Salvage of the radial head in chronic adult Monteggia fractures. Report of four cases. J Bone Joint Surg Br. 2006;88:645–8. doi: 10.1302/0301-620X.88B5.17346. [DOI] [PubMed] [Google Scholar]
- 23.Song KS, Ramnani K, Bae KC, Cho CH, Lee KJ, Son ES. Indirect reduction of the radial head in children with chronic Monteggia lesions. J Orthop Trauma. 2012;26:597–601. doi: 10.1097/BOT.0b013e3182548981. [DOI] [PubMed] [Google Scholar]


