Abstract
The COVID-19 pandemic accelerated adoption of telemedicine visits into American medicine. It is commonly believed that, within a matter of weeks, telemedicine was widely and successfully implemented and that medicine is forever changed. The experience on the ground, however, is more nuanced, with both positive and negative experiences for patients and clinicians. Advanced models of team-based care with in-room support (aTBC) have developed over the past decade, with strategic delegation of tasks to uptrained support staff, allowing physicians to provide undivided attention to their patients and greater access to care for their populations. Herein, we describe our initial experiences with telemedicine in the context of many years practicing in aTBC models. Our experience demonstrates that when implementing telemedicine visits, it is important to avoid a reflex reversion to the outmoded model of the physician alone in the room with the patient and instead bring forth the safety, quality, and satisfaction advantages associated with aTBC. We provide a practical “how-to” guide for implementing telemedicine visits; outline logistical details of representative video and audio visits from our own practices; describe new opportunities for family engagement, care coordination, and comanagement across specialties; and outline a research agenda going forward to further knowledge of the risks and benefits and optimal application of health care on a telemedicine platform.
Abbreviations and Acronyms: aTBC, advanced team-based care; CMS, Centers for Medicare and Medicaid Services; EHR, electronic health record; MA, medical assistant
Adoption of telemedicine has been accelerated by necessity with the onset of COVID-19. The common narrative is that COVID-19 happened, and within a matter of weeks, telemedicine was widely implemented, all is rosy, and medicine is forever changed. New subthemes, however, are emerging that offer an opportunity for a more nuanced view, including the importance of accommodating patient choice, appropriately matching encounter type to visit platform, acknowledging hazards associated with care delivered remotely, and adapting existing models of advanced team-based care with in-room support (aTBC)1, 2, 3, 4, 5, 6 to the virtual environment.
From the vantage point of the first few months of virtual visits as a new normal, and in the context of extensive professional experience with aTBC, we share our (J.J. and K.H.) initial experience with telemedicine visits (see representative case examples in Appendix 1, available online at http://www.mayoclinicproceedings.org); outline models available for team-based care within telemedicine; provide a guide for the types of patient encounters best suited to each visit type; share logistical pearls; and suggest a research agenda for moving forward.
Telemedicine Timeline
Before COVID, a neglible fraction of visits were virtual. In mid-March 2020, the Centers for Medicare and Medicaid Services (CMS) implemented waivers that facilitated adoption of telemedicine visits.7 These waivers addressed credentialing, payment parity, and sites of service that qualified for audio or video visits (ie, lifting the geographic restrictions that previously confined telemedicine to rural areas and allowing that virtual visits can now be provided from either the physician’s workplace or home). These changes are to last for the duration of the emergency declaration or beyond. Many commercial payers have followed suit.8
Delivery organizations also made changes. For example, some organizations that had previously delivered telemedicine visits primarily for urgent-care needs, using a third-party vendor and requiring credit-card payment up front, made these visits more palatable for patients by no longer requiring payment before the visit and now support virtual visits across multiple specialties. To increase capacity, some organizations used multiple virtual-visit platform venues including personal smart phones, technology embedded within their electronic health record (EHR) platforms and 1 or more third-party technology vendors.
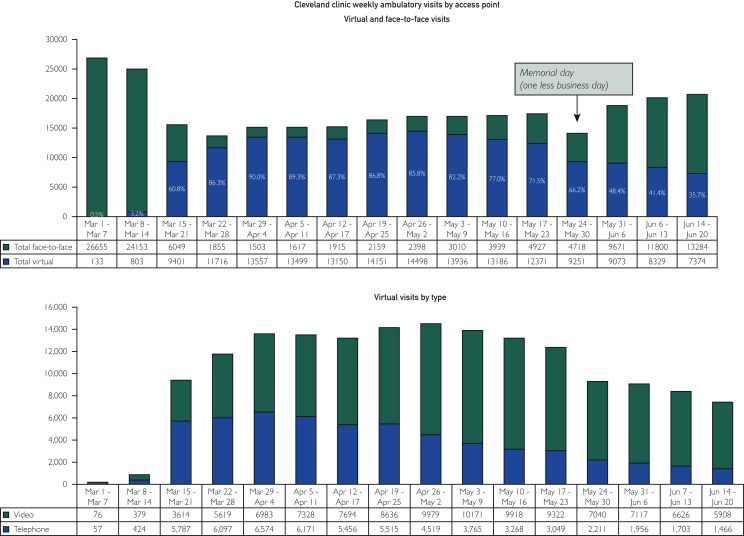
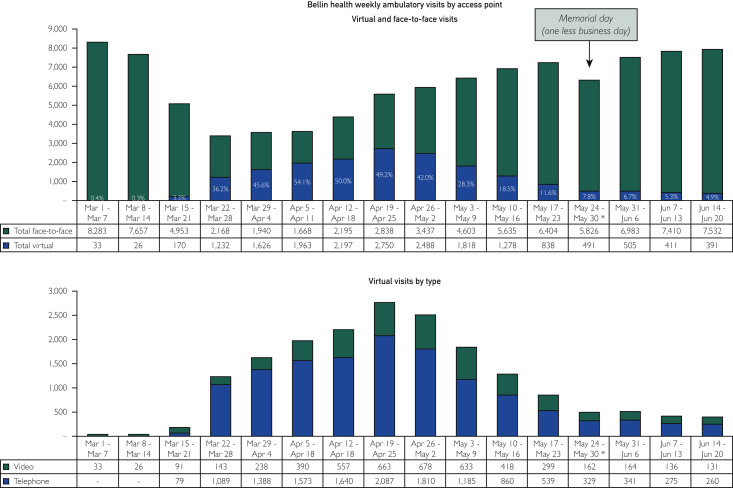
By mid-April, virtual visits in the United States had reached a peak of 14% of all visits.9 , 10 The authors’ experiences, and others,11 reflect even more rapid adoption. In the span of 6 weeks (from March 7, 2020, to April 11, 2020), the proportion of Cleveland Clinic outpatient visits that were provided virtually increased from 2% to 75% (and to 90% for primary care)12 (Figure 1 ). Similarly, at Bellin Health, in Green Bay, Wisconsin, nearly 50% of all visits were delivered virtually by the end of April 2020 (Figure 2 ).
Figure 1.
Cleveland Clinic Community Care encounters by visit type and virtual visits by type/platform.
Figure 2.
Bellin Health primary care encounters by visit type and virtual visits by type/platform.
Early Experience
Unlike the common narrative, virtual visits have not, in our experience, been an unqualified success. Although policy and payment barriers to virtual visits were quickly addressed, the technology barriers could not be removed as quickly, and reimplementation of teamwork has not been automatic. In 1 of our clinics (J.J.), approximately one-half of all planned video visits in the first several weeks failed for a combination of reasons, including technology breakdowns and limitations to patient understanding of the process.
Clinicians experienced many frustrations, including network and platform reliability issues, patient and clinician Internet and Wi-Fi limitations, insufficient device battery life, poor audio and video quality, and multiple virtual platforms, causing confusion for clinicians and patients.13 For some virtual-visit platforms, patients need a patient portal account, which only approximately one-half of our patients (J.J.) have, and some also require the patient to download a special app. Some physicians reported to us, and in the literature,14 that it could take 20 to 40 minutes of staff time to help the patient establish a connection before the video visit. Physicians in safety-net clinics might spend one afternoon calling their patients to set up for the next afternoon’s official audio or video visit (Personal communication, Dr. Mark Linzer, May 12, 2020). In addition, some physicians report that virtual visits are more superficial and less satisfying, with reduced ability to read facial and body expressions and no access to the therapeutic touch that comes with examining a patient.
In our experience, patient adoption was initially motivated primarily by patients’ concern for their health (“Do I have COVID?” or “I don’t want to come to the office and risk being exposed to COVID”) rather than patients’ embrace of technology to connect with their physicians in a novel way. Over time, some of our patients were also motivated by the desire to resume care for their non-COVID issues and yet remained fearful that it was not safe to come in.
Distracted Doctoring
We experienced unexpected hazards with the early implementation of telemedicine. The “doctor-does-it-all” mentality, pervasive in our history, re-emerged, even among pioneers in aTBC. Most, if not all, of the tasks of preparing our patients and the medical record for in-office visits, which were previously completed by our practice support (medical assistants, nurses, and clerical staff), were handed back to physicians, who were now alone “in the room” with their patients. In addition, there is new work associated with establishing and maintaining a video connection. This led to significant inefficiencies, uncompleted standard workflows, cognitive overload, and frustration among patients and clinicians alike. There was an assumption that this additional work could be performed by physicians while patients continued to talk with us and that such multitasking would be without consequence. And yet, we are aware of the perils of this time-pressured divided attention: the risks of skipping steps and taking shortcuts, mistyping and clicking, incomplete ordering, documentation inaccuracies, and working in the wrong chart.
We were transforming on the fly. Initially, we did not have the standard operating procedures, robust training, and adequate experience practicing aTBC in virtual visits. Not only did the physicians and advanced-practice providers have experience gaps, so did our clinical support teams. As we develop new models of TBC for telemedicine, we are building on our experiences with aTBC for in-office visits.
In-Office Advanced Team-Based Care
In aTBC, 2 medical assistants (MAs) or nurses are paired with a physician and serve as navigators for the patient. During the office visit, the upskilled MA or nurse stays with the patient from the beginning to the end of each appointment. During the pre-visit rooming process, the nurse or MA performs agenda setting, medication review, care gap closure and updates the history, pends refills, performs pre-charting, and obtains vital signs. When the physician enters the room, the nurse or MA assists with retrieval of information and visit-note documentation, pends additional orders, and completes billing forms: all in real time per physician direction. During the post-visit, the nurse or MA reviews the visit and next steps with the patient; engages the patient in self-management support, as appropriate; and arranges for the next visit, along with specified pre-visit laboratory testing. Soon thereafter, the physician reviews and signs off on the note, orders, and billing information. Because they were present during the patients’ appointments, the MA or nurse is also able to more capably coordinate care and respond to issues that arise between visits.
This model is associated with higher-quality care, better documentation, increased access and productivity, and greater staff and physician satisfaction.2 , 15, 16, 17 Dr Hopkins’ revenue value unit-based productivity, for example, increased by 40%. With expansion to the other family physicians in his group, total practice productivity increased by approximately 20%. Access correspondingly increased. Quality metrics improved along with significant improvement in patient satisfaction scores as well as physician and support staff engagement and satisfaction.2
Advanced Team-Based Care in Telemedicine
In our view, aTBC is as important for virtual visits as it is for in-person visits. We recommend physicians and their teams develop workflows that continue the gains achieved in aTBC and avoid reversion to the unsafe “doctor-does-it-all” model. It is crucial that staff continue to provide this support whether the visit is face to face or virtual (Table 1 ). For practices that have experience with aTBC, a similar model of virtual in-room support increases staff engagement in patient care and frees the physician to give undivided attention to the patient because of the enhanced documentation and EHR support. For practices with less robust staffing, or limited experience with TBC, enhanced virtual rooming by the MA or nurse, including setting up and starting documentation before physician involvement, still provides significant improvement in efficiency and a decrease in the burden of EHR work for the physician. Care-gap closure, medication review, and updating of the medical history are examples of work that can be done during virtual rooming by the staff, even if they are unable to provide in-room support.
Table 1.
Models of Teamwork for Virtual Visits
| Model of teamwork | Description | Workflow | Most appropriate- use cases |
|---|---|---|---|
| Team-based care with synchronous (real-time) “in-room” support | Video or phone visit with nurse or MA present from start to finish of appointment |
|
All visit types, unless the patient requests the nurse or MA to leave during a portion of the visit. |
| Team-based care with asynchronous support | Nurse/MA present during pre-visit and sometimes also during post-visit |
|
Straightforward, single problem acute or chronic visits (ie, URI or controlled hypertension) |
APP = advanced practice provider; MA = medical assistant; URI = upper respriratory infection.
We share representative experiences implementing aTBC within both video and phone visits from our practices (Appendix 2, available online at http://www.mayoclinicproceedings.org).
Novel Visits Made Possible With Telemedicine
Technology has the potential to support novel clinical encounters in the future that bring family members, staff, and even other physicians “into the room” in a way that is not possible in purely in-office visits. For example, for complex medical and family decision making, such as end-of-life planning, a daughter from out of state could attend her mother’s visit virtually. During the shut-down phase of a contagious pandemic, all parties may be virtual; during ordinary times, the patient, staff, and physician may be in office with the out-of-state daughter joining by video.
In addition, we envision the possibility of better care coordination as we become adept at cross-specialty hybrid visits. For example, a patient and his cardiologist are considering when to schedule heart valve surgery. The patient also requires radiation therapy for prostate cancer. The cardiology team could set up an appointment with patient and family, and video conference in the oncologist, so that the family had confidence that the physicians involved in their care were all “on the same page” and that the order of interventions was optimized.
Finally, there may be circumstances in which, for efficiency or for control of infection, it is better for the nurse or MA in aTBC to perform support virtually, outside of the examination room, but still “inside the room” via video conferencing technology during an in-person appointment between the patient and physician, limiting the number of people in close physical proximity without compromising the benefits of aTBC.
Logistic Pearls
Let Patients Choose Their Visit Type
Some patients, when offered a video visit, will prefer an in-office appointment. Allowing patients to choose their visit type, within reason—making exceptions, for example, during COVID when a patient has upper respiratory symptoms or when community COVID rates are high, making an inperson visit unsafe—is a patient-centered approach. We provide guidance to help match the encounter type to the visit platform (Appendix 3, available online at http://www.mayoclinicproceedings.org).
Track Appointment Type Demand
Some physicians prefer to schedule patients into different session blocks, depending on whether the appointment is virtual or in person. In doing so, it is important for unit leaders to track appointment type demand so that this can be matched to supply. One of our organizations (K.H.) was surprised to learn that fill rates for virtual visits were lower than fill rates for in-person visits. In fact, some patients preferred to wait longer for the next available in-office visit rather than schedule a sooner video visit, a trend we are watching closely. As a result of these observations, we shifted the balance of appointment-type offerings.
Schedule Realistic Time Slots for Virtual Visits
It may take more time to accomplish the same care in a video visit compared with in-office visit, owing to the associated logistics and the limitations of communication via a 2-dimensional screen. We have learned that it is unlikely that we can do everything we would accomplish in an in-office visit in a virtual visit in the same amount of time, especially when the physician is acting solo. By contrast, as we re-engage our staff to provide full support during virtual visits, we are finding that time requirements for physicians in these visits is coming closer to the time required for in-office visits. Staff involvement in virtual visits is critical for optimal efficiency.
Support Patients in Gaining Familiarity With the Technology, and Establish Expectations
It can be helpful to have a team member call patients ahead of their first virtual visits to walk them through the process. This is also a good time to set up mutual expectations: for example, regarding the length of the visit (“We will have 15 minutes with you tomorrow, so I’d like to be sure we understand what your priorities are for that visit”) and its location (“We find it works best, when possible, if you can be in a quiet, private location where you won’t be disturbed.”) One physician reported on his early experience with telemedicine during COVID “Several minutes in, I learned the patient was having a pedicure during our visit” (Personal communication, Dr. Yul Ejnes, May 9, 2020). We’ve also had several examples of patients driving while doing a virtual visit, a practice that we do not recommend for either patient or physician.
Consider Simulated “Practice Visits” for Clinical Teams
At one of our organizations (K.H.) we held simulated “practice virtual visits” among our team, with one of us serving as the patient. This allowed physicians and support staff to experience the virtual platform from both sides. We learned to navigate the platform and troubleshoot technical problems. We are considering offering patients a “practice virtual visit” to let them test drive the platform technology before the actual visit.
Have a Backup Plan for Technology Failures
Having technical support available in real time and on site in the office is valuable at go live. It is important to have a backup plan if the technology fails or user error prevents an adequate connection. Our default backup (K.H.) was initially a phone call, now it is Apple FaceTime, Google Duo, or Doximity Dialer, rather than a phone call.
Help the Patient Assist With the Physical Examination
Until we have accessories for smart phones and computers that assist in the virtual physical examinations, we can enlist the help of the patient: for example, to check patients' pulses, show them how to feel the radial artery pulse, and then ask them to count out loud every time they feel a beat. For dermatologic concerns, ask the patient to send pictures ahead of the appointment. (It is difficult to see skin lesions by video camera, and patients often have difficulty aiming the camera and optimizing the lighting.) For neurologic examinations, patients can be asked to do tasks associated with daily living, such as putting on their shoes, during the visit. There are, however, some aspects of the physical examination that are not feasible or may be unsafe to perform virtually.
The specific needs for physical examination can be anticipated in the pre-visit phone call or portal message, which, if done the day before, allows patients time to practice taking their pulse, to send in a picture of the skin lesion, or ensure that the camera is adjusted so that the activity of interest can be viewed.
Respect Boundaries for Patients
Some patients may find it intrusive to have their physician and team peer into their home or to have their family members or coworkers overhear confidential conversations. During an initial pre-visit setup call, the patient can be instructed on the use of artificial backgrounds, if desired.
Respect Boundaries for Physicians
Physicians may be concerned about breeches of their own privacy when conducting visits from home, wondering about the risk of patients inadvertently achieving access to personal information. What else might they see or hear that physicians would rather they not?
Some Suggestions
Choose a quiet location, with a low likelihood for audible and visual distractions. Check for adequacy of Internet and Wi-Fi signals. Have chargers available for any devices and equipment, as well as a backup power source. Consider using the “Do Not Disturb” feature on your device. Be aware of what may be visible through your camera in the background and that sound and audio connections with the patient may be active before or after you think they are. Use virtual backgrounds and headphones. Understand the potential for unintended consequences of doing virtual visits from a personal device (potential access to your phone number, email address, device IP one address, or other personal information).
Scheduling Tips
When telemedicine is delivered from home, there is a risk that the physician will feel “on the clock” most of the time. We suggest maintaining a weekly schedule of telemedicine sessions, just as one would have for in-office visits, rather than handling visits in random fashion at any time.
Some physicians schedule virtual visits and in-person visits within the same schedule block. This allows patients the flexibility to convert from 1 visit type to the next at the last minute and provides the physician some variety in the course of their days. It also requires staying precisely on time or developing a system in which the assistant calls the patient within a prespecified window of time when the team is ready to begin that patient’s appointment.
An alternative approach is to cohort all in-person visits and all virtual visits into specific time blocks. This allows the physician and the team to focus on particlur visit types within a certain block of time, which may enhance efficiency. It may even allow the physician and team to manage these visits off site (ie, from home), if desired. By limiting the number of staff members in the clinic at any given time, this can also be helpful with maintaining safe physical distancing in the office.
Use the Flexibility of Virtual Care to Your Advantage
There may be times when physicans may have minor illnesses or may be off work because of exposure. The flexility of virtual visits allows the physician to provide patient care from home, avoiding significant disruptions and delays in care.
Research Agenda
There is a paucity of evidence about the safety, efficacy, and unintended consequences of this new mode of clinical interaction with patients. Likewise, we are only beginning to explore some of the novel opportunities for enhanced connection and communication. Our first few months’ experience with telemedicine has raised more questions than answers about the pros and cons of virtual visits (Appendix 4, available online at http://www.mayoclinicproceedings.org). We believe it is important to approach telemedicine with an open mind; to not assume equivalency of efficacy, safety, and strength of relationships resulting from in-office vs virtual visits; and to consider new opportunities this platform brings. In Table 2 , we outline questions that can inform a research agenda, with an emphasis on optimizing workflows and teamwork, overcoming logistic hurdles, and understanding the impact of remote care on quadruple aim18 , 19 outcomes of quality, cost, and patient and care-team experience.
Table 2.
Research Agenda for Telemedicine in Ambulatory Care
| Research question | |
|---|---|
| Logistic | What types of visit are most appropriate for in person vs virtual care? (See Appendix 3 for initial guidance) |
| How does the total time vary for in-person vs video visit for comparable care? | |
| Does a pre-visit call for technology support improve the completion rate of virtual visits? | |
| Does a pre-visit call for agenda setting and information gathering (ie, photos of skin lesions) improve patient and physician satisfaction with the visit? | |
| How does aTBC (ie, MA/nurse drafts visit note and pends orders in real-time during visit) affect productivity, completeness of intended care, patient satisfaction, staff satisfaction, physician satisfaction, and total time per visit? | |
| If the nurse/MA is not in the room for a virtual visit, how are handoffs between staff and physician best accomplished? | |
| What are the implications for space requirements for clinics when many visits are virtual? | |
| What are the differences in care elements between virtual vists and in-office visits? Can these differences inform efficiencies for either visit type? | |
| Quality | Are there demonstrable quality differenes between in-office and virtual visits? |
| Does the appropriateness of medical decision making and accuracy of diagnosis vary by in-office vs virtual visits? | |
| What is the impact of tele-fragmentation (ie, in which outside vendors provided clinical services via telemedicine but do not provide in-office care) on continuity, quality, satisfaction, and overall costs of care? | |
| Technology | How can technology be optizmized to support virtual care? |
| Trust | How does telemedicine impact trust, including patient trust in physician and team, physician trust in patient, physician trust in team members? |
| Can intentional practices to improve presence (See Stanford “Presence 5”18) improve the quality of care provided virtually? | |
| Costs and financing | What are the differences in costs vs revenue for virtual care when delivered with and without aTBC with in-room support? |
| Does the payment model (FFS vs capitated) affect the number and type of visits recommended by the physician or chosen by the patient? | |
| Do physicians order more or less tests during virtual visits vs in-person visits? |
aTBC = advanced team-based care; FFS = fee for service; MA = medical assistant.
Conclusion
The adoption of telemedicine has been accelerated during the COVID-19 pandemic, and yet its appropriate role in patient care is not yet clearly established. Our intial experience suggests that telemedicine, implemented without attention to workflow, risks eliminating—rather than enhancing—teamwork and, by returning to a solo-hero model, risks introducing new hazards. These early days also suggest novel opportunities to bring family members from afar or other clinicians involved in the patient’s care “into the room” and thus improve patient and family centeredness and enhance care coordination.
Footnotes
Dr Sinsky is employed by the American Medical Association. The opinions expressed in this article are those of the authors and should not be interpreted as American Medical Association policy.
Grant Support: The authors report no grant support for this article.
Potential Competing Interests: The authors report no competing interests.
Supplemental online material can be found online at http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Funk K.A., Davis M. Enhancing the role of the nurse in primary care: the RN “co-visit” model. J Gen Intern Med. 2015;30(12):1871–1873. doi: 10.1007/s11606-015-3456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hopkins K., Sinsky C.A. Team-based care: saving time and improving efficiency. Fam Pract Manag. 2014;21(6):23–29. [PubMed] [Google Scholar]
- 3.Jerzak J., Siddiqui G., Sinsky C.A. Advanced team-based care: how we made it work. J Fam Pract. 2019;68(7):E1–E8. [PubMed] [Google Scholar]
- 4.Sinsky C.A., Bodenheimer T. Powering-up primary care teams: advanced team care with in-room support. Ann Fam Med. 2019;17(4):367–371. doi: 10.1370/afm.2422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sinsky C. Improvement happens: an interview with Christine Sinsky, MD. Interview by Richard L. Kravitz. J Gen Intern Med. 2010;25(5):474–477. doi: 10.1007/s11606-010-1281-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sinsky C.A., Sinsky T.A., Althaus D., Tranel J., Thiltgen M. ‘Core teams’: nurse-physician partnerships provide patient-centered care at an Iowa practice. Health Affairs. 2010;29(5):966–968. doi: 10.1377/hlthaff.2010.0356. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare COVID-19 emergency declaration blanket waivers for health care providers. 2020. https://wwwcmsgov/files/document/covid19-emergency-declaration-health-care-providers-fact-sheetpdf
- 8.American Academy of Family Physicians COVID-19 private payer frequently asked questions. 2020. https://wwwaafporg/dam/AAFP/documents/practice_management/COVID-19/payer-faqspdf
- 9.Mehrotra A Chernew M., Linetsky D., Hatch H., Cutler D. The impact of the COVID-19 pandemic on outpatient visits: a rebound emerges, to the point (blog). Commonwealth Fund; May 19, 2020. https://doiorg/1026099/ds9e-jm36
- 10.Mehrotra A Chernew M., Linetsky D., Hatch H., Cutler D., Schneider E.C. The impact of the COVID-19 pandemic on outpatient visits: changing patterns of care in the newest COVID-19 hot spots. https://wwwcommonwealthfundorg/publications/2020/aug/impact-covid-19-pandemic-outpatient-visits-changing-patterns-care-newest 2020.
- 11.Baum A., Kaboli P.J., Schwartz M.D. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. https://doi.org/10.7326/M20-3026 Ann Intern Med. 2020 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 12.Cleveland Clinic COVID-19 Response, Digital Health Playbook. 2020. https://myclevelandclinicorg/-/scassets/files/org/landing/preparing-for-coronavirus/covid-response-digital-health-playbookashx?la=en
- 13.Lam K., Lu A.D., Shi Y., Covinsky K.E. Assessing telemedicine unreadiness among older adults in the United States during the COVID-19 pandemic. JAMA Intern Med. 2020;180(10):1389–1391. doi: 10.1001/jamainternmed.2020.2671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nabhan C. The virtual visit. JAMA Cardiol. 2020;5(10):1089–1090. doi: 10.1001/jamacardio.2020.2706. [DOI] [PubMed] [Google Scholar]
- 15.Anderson P., Halley M.D. A new approach to making your doctor-nurse team more productive. Fam Pract Manag. 2008;15(7):35–40. [PubMed] [Google Scholar]
- 16.Jerzak J. December 2016. Restoring joy in practice through team based care. Presentation at the Institute for Healthcare Improvement. [Google Scholar]
- 17.Lyon C., English A.F., Chabot Smith P. A team-based care model that improves job satisfaction. Fam Pract Manag. 2018;25(2):6–11. [PubMed] [Google Scholar]
- 18.Zulman D.M., Verghese A. Tele-presence 5. https://medstanfordedu/presence/initiatives/stanford-presence-5/tele-presence-5html. 2020
- 19.Bodenheimer T., Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014;12(6):573–576. doi: 10.1370/afm.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.