Graphical Abstract
Training in nephrology requires both medical skills and the mastering of technical invasive procedures such as central venous catheter (CVC) placement and percutaneous kidney biopsy (KB). The French Nephrology Residency Teaching Program, published in 2020, encourages the development of simulation-based learning techniques [1, 2]. However, only a small minority of universities currently offer these training methods.
We surveyed nephrology residents, fellows and young nephrologists aged ≤43 years about their perceptions of KB and CVC placement teaching (Supplementary data, File S1). The survey was promoted on the Club des Jeunes Néphrologues (French Young Nephrologists Association) website, by e-mail and through social networks.
We received 164 responses: 95 (57.9%) from nephrology residents (about one-third of the French total), 33 (20.1%) from fellows and 36 (22.0%) from young attending physicians, from all 13 French regions.
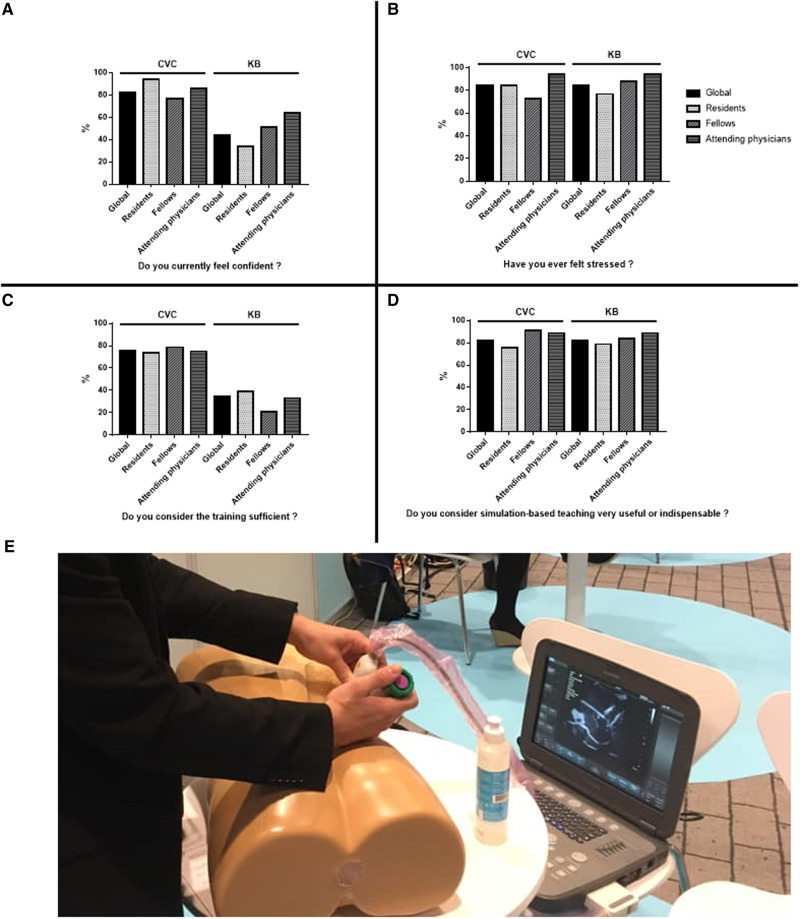
The majority of the participants (75.9%) considered teaching of CVC placement to have been sufficient during their residency and they feel confident using this technique (82.3%). However, 84.1% of the responders have experienced stress while carrying out the procedure. CVC placement is mainly ultrasound guided (65.9%). Of the participants, 53.0% considered that the successful placement between 5 and 10 CVC was necessary to be fully confident with the technique. The simulation-based teaching is considered very useful for 62.6% and mandatory for 19.6% of the participants. The most suitable simulation model for CVC placement was the mannequin for 77.0% participants (Figure 1).
FIGURE 1.
Feelings of young nephrologists about CVC placement and KB. Results of the French survey of (A) current confidence, (B) stress, (C) current training, (D) simulation-based teaching and (E) simulation-based teaching of KB on mannequin.
The answers were very different concerning the training for KB. Only 34.4% of the participants considered the teaching of KB to have been sufficient during their residency, with just 44.2% of them currently feeling confident with this procedure, with residents being the least confident (33.7%, P = 0.005). The vast majority (84%) have experienced stress during a KB. A total of 50.3% considered that performing >10 KB was necessary to be confident with the procedure. More than 80% of the participants considered a simulation-based teaching for KB to be very useful (53.4%) or mandatory (28.8%). The most suitable simulation model for KB was the mannequin for 72.8% of respondents, the cadaveric model for 23.5% and the animal model for 3.7% (Figure 1).
All the participants would like to use simulation models for both CVC placement and KB if available.
Concerning CVC placement, the contribution of simulation training on mannequins has been widely demonstrated in recent years in intensive care. It allows an increase in the technical performance of the trainees and faster empowerment [3–5]. Compared with standard training, mannequin training has been shown to improve accuracy of the procedure, with a decrease in the number of catheter complications [4] such as catheter-related sepsis [6].
KB has a risk of post-procedural haemorrhage, which necessitates implementation of special precautions. In reality, therefore, residents have very little opportunity for training during their internship. Performing KB also requires experience in ultrasound techniques for guiding the puncture.
The contribution of simulation to the teaching of KB has been little documented in the literature. Some articles have shown that participants in simulation teaching using a porcine KB model introduced into a turkey carcass [7, 8] performed better in KB procedures compared with those who received ‘conventional’ teaching, with a reduction of post-procedure bleeding. In nephrology, teaching by in vivo simulation in pigs and in silico on mannequins is feasible, but poorly evaluated [9, 10].
Young nephrologists are open-minded about simulation-based teaching, which has shown interesting pedagogical results in other fields [3–6]. New simulation models using mannequins are now emerging [10] (Figure 1E) and could improve technical teaching in nephrology.
In our opinion, simulation-based teaching should be extended to all nephrology residents and fellows, for better training of invasive procedures, to reduce stress and to improve patient safety.
SUPPLEMENTARY DATA
Supplementary data are available at ckj online.
Supplementary Material
ACKNOWLEDGEMENTS
We thank all those who participated in this survey. We thank Felicity Kay for the English editing.
AUTHORS’ CONTRIBUTIONS
M.B. and Y.L. designed the survey. M.B., V.M., C.B. and Y.L. promoted the survey. M.B. and S.C. interpreted the data. M.B. drafted the manuscript and made the figures and visual abstract. V.M., S.C., C.B. and Y.L. revised the manuscript critically.
CONFLICT OF INTEREST STATEMENT
None declared. The results presented in this article have not been published previously in whole or part, except in abstract form.
REFERENCES
- 1. Lohéac C, Maisons V, Bureau C. et al. [ Amending of the 3rd cycle of medical studies in France: what the nephrologists stand for]. Nephrol Ther 2020; 16: 50–58 [DOI] [PubMed] [Google Scholar]
- 2.JORF n°0066 du 17 mars 2020 texte n° 23 Arrêté du 13 février 2020 modifiant l’arrêté du 21 avril 2017 relatif aux connaissances, aux compétences et aux maquettes de formation des diplômes d’études spécialisées et fixant la liste de ces diplômes et des options et formations spécialisées transversales du troisième cycle des études de médecine NOR: ESRS2001981A. 66AD. https://www.legifrance.gouv.fr/eli/arrete/2020/2/13/ESRS2001981A/jo/texte
- 3. McGraw R, Chaplin T, McKaigney C. et al. Development and evaluation of a simulation-based curriculum for ultrasound-guided central venous catheterization. Can J Emerg Med 2016; 18: 405–413 [DOI] [PubMed] [Google Scholar]
- 4. Barsuk JH, McGaghie WC, Cohen ER. et al. Simulation-based mastery learning reduces complications during central venous catheter insertion in a medical intensive care unit. Crit Care Med 2009; 37: 2697–2701 [PubMed] [Google Scholar]
- 5. Koh J, Xu Y, Yeo L. et al. Achieving optimal clinical outcomes in ultrasound-guided central venous catheterizations of the internal jugular vein after a simulation-based training program for novice learners. Simul Healthc 2014; 9: 161–166 [DOI] [PubMed] [Google Scholar]
- 6. Barsuk JH, Cohen ER, Feinglass J. et al. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med 2009; 169: 1420–1423 [DOI] [PubMed] [Google Scholar]
- 7. Mrug M, Bissler JJ.. Simulation of real-time ultrasound-guided renal biopsy. Kidney Int 2010; 78: 705–707 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dawoud D, Lyndon W, Mrug S. et al. Impact of ultrasound-guided kidney biopsy simulation on trainee confidence and biopsy outcomes. Am J Nephrol 2012; 36: 570–574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rivera Gorrín M, Correa Gorospe C, Burguera V. et al. Teaching innovations in ultrasound-guided renal biopsy. Nefrología 2016; 36: 1–4 [DOI] [PubMed] [Google Scholar]
- 10. Sharma SG, Arthur JM, Bonsib SM. et al. An integrated pathology and ultrasonography-based simulation for training in performing kidney biopsy. Clin Nephrol 2018; 89: 214–221 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.