The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation is the most commonly used equation for estimating glomerular filtration rate (GFR). Recently the European Kidney Function Consortium (EKFC) formula with an extended age range from 2 to 90 years was published [1]. In the study validation cohort, it predicted measured GFR in adults with low bias and greater accuracy and precision than the CKD-EPI equation [1].
Here we provide a systematic and comprehensive graphical comparison between the EKFC and CKD-EPI equations. This analysis is not about their abilities to predict measured GFR; instead we are focusing on the practical implications of using the EKFC equation instead of the CKD-EPI equation.
This is an entirely mathematical comparison between the EKFC [1] and CKD-EPI (non-black) equations [2]. We created contour plots (Figure 1) for absolute and relative differences across the age range 18–90 years (x-axis) and CKD-EPI values from 1 to 104 mL/min/1.73 m2 (y-axis). Absolute differences were calculated by subtracting CKD-EPI values from EKFC values. For relative differences we divided these results by the CKD-EPI values. To plot the findings as a function of CKD-EPI values, we solved the CKD-EPI equation for creatinine and used this term for calculating EKFC values. Within the same coordinate system, we drew region plots (Figure 2) with coloured areas, where corresponding EKFC and CKD-EPI values would result in discordant attribution of Kidney Disease: Improving Global Outcomes (KDIGO) GFR categories (G1, 2, 3a, 3b, 4 and 5) [3]. All analyses were done for females and males. We used Mathematicaversion 12.1.1.0 (Wolfram Research, Champaign, IL, USA) for our calculations.
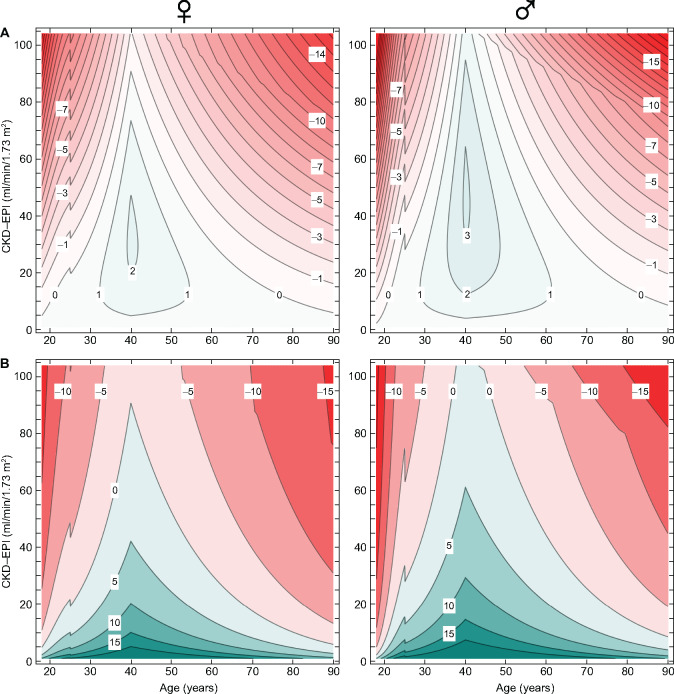
FIGURE 1:
Contour plots of absolute and relative differences between the EKFC and CKD-EPI equations as a function of age (x-axis) and CKD-EPI estimated GFR values (y-axis). Areas where EKFC eGFR is higher than CKD-EPI are shaded in green and areas where EKFC eGFR is lower are in red. (A) Absolute differences (EKFC − CKD-EPI, in mL/min/1.73 m2) for females and males. Contours are drawn for every 1 mL/min/1.73 m2 difference. (B) Relative differences [100 × (EKFC − CKD-EPI)/CKD-EPI, in percent] for males and females. Contours are drawn for every 5% difference.
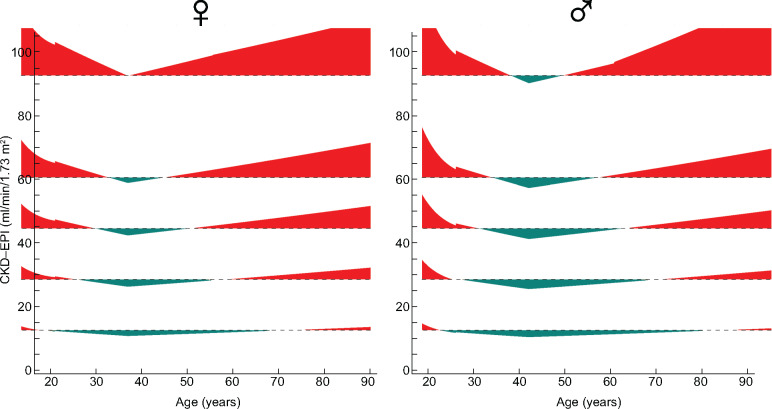
FIGURE 2:
Region plot showing discordant KDIGO GFR categories (G1, 2, 3a, 3b, 4 and 5) [3] between the EKFC and CKD-EPI equations as a function of age (x-axis) and CKD-EPI estimated GFR values (y-axis). Areas where the EKFC GFR category is lower than the CKD-EPI (i.e. kidney function is better) are colored green and areas where the EKFC GFR category is higher are colored red. In the white areas, KDIGO GFR categories are the same for both equations.
The resulting graphs are shown in Figures 1 and 2. We want to comment on several important aspects. Absolute differences (Figure 1A) between the two formulas are very small with CKD-EPI values <30 mL/min/1.73 m2. They remain well below 5 mL/min/1.73 m2 for almost all patients with CKD-EPI values <45 mL/min/1.73 m2. The biggest absolute differences are observed in very young and old patients with well-preserved kidney function. Here, EKFC values are significantly lower than their CKD-EPI counterparts. Although the relative differences (Figure 1B) are generally still <15%, there are huge areas where KDIGO GFR categories according to the EKFC equation are higher than with the CKD-EPI equation (Figure 2).
Our graphs provide a comprehensive comparison between the EKFC and CKD-EPI formulas across their complete age and kidney function range. Differences are shown as a function of CKD-EPI values (Figure 1), so eGFR changes resulting from using the EKFC equation instead of the CKD-EPI equation are very easy to grasp. Figure 2 depicts the impact on KDIGO GFR categorization in the same framework.
We clearly demonstrate that for most patients with impaired kidney function, the differences between these two equations are minor and generally smaller than the imprecision of these formulas for the true, measured GFR [1]. We predict that, for example, for drug dose adaptions, the choice of formula will not lead to clinically significant differences. Larger discrepancies are observed in older adults with well-preserved kidney function. Irrespective of whether the EKFC equation is more correct in predicting measured GFR, the systematically lower EKFC values in this age group could lead to more patients being diagnosed with CKD. As recently suggested [4], it would be necessary to redefine ‘normal’ in this age group to avoid inappropriate increases in CKD diagnoses by the new formula.
The extended age range and smooth transition of eGFR from paediatric to adult age make the EKFC equation an attractive alternative to the CKD-EPI equation. Substituting the EKFC equation for the CKD-EPI equation will not lead to significantly different eGFRs for the majority of adult patients, but the oftentimes higher KDIGO GFR category in older adults with the EKFC equation should be kept in mind.
FUNDING
S.S. was supported by a grant of the Fundação Pesquisa e Desenvolvimento Humanitario. The funder had no role in study design, analysis and interpretation of data, writing the article or the decision to submit the article for publication.
AUTHORS’ CONTRIBUTIONS
F.B. provided the research idea and data analysis. S.S. contributed to supervision. Each author contributed important intellectual content during manuscript drafting and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved.
CONFLICT OF INTEREST STATEMENT
F.B. has no relevant financial interests or other potential conflicts of interest. S.S. receives financial support and travel expenses as a speaker from Baxter and Fresenius. He is a medical advisor for Peripal and Versantis. These are not related to the current study. S.S. has no potential conflicts of interest.
REFERENCES
- 1. Pottel H, Björk J, Courbebaisse M. et al. Development and validation of a modified full age spectrum creatinine-based equation to estimate glomerular filtration rate: a cross-sectional analysis of pooled data. Ann Intern Med 2020; doi:10.7326/M20-4366 [DOI] [PubMed] [Google Scholar]
- 2. Levey AS, Stevens LA, Schmid CH. et al. A new equation to estimate glomerular filtration rate. Ann Intern Med 2009; 150: 604–612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kidney Disease: Improving Global Outcomes CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013; 3: 1–150 [DOI] [PubMed] [Google Scholar]
- 4. Delanaye P, Jager KJ, Bökenkamp A. et al. CKD: a call for an age-adapted definition. J Am Soc Nephrol 2019; 30: 1785–1805 [DOI] [PMC free article] [PubMed] [Google Scholar]