Abstract
Background
The European Renal Association – European Dialysis and Transplant Association (ERA-EDTA) Registry collects data on kidney replacement therapy (KRT) via national and regional renal registries in Europe and countries bordering the Mediterranean Sea. This article summarizes the 2018 ERA-EDTA Registry Annual Report, and describes the epidemiology of KRT for kidney failure in 34 countries.
Methods
Individual patient data on patients undergoing KRT in 2018 were provided by 34 national or regional renal registries and aggregated data by 17 registries. The incidence and prevalence of KRT, the kidney transplantation activity and the survival probabilities of these patients were calculated.
Results
In 2018, the ERA-EDTA Registry covered a general population of 636 million people. Overall, the incidence of KRT for kidney failure was 129 per million population (p.m.p.), 62% of patients were men, 51% were ≥65 years of age and 20% had diabetes mellitus as cause of kidney failure. Treatment modality at the onset of KRT was haemodialysis (HD) for 84%, peritoneal dialysis (PD) for 11% and pre-emptive kidney transplantation for 5% of patients. On 31 December 2018, the prevalence of KRT was 897 p.m.p., with 57% of patients on HD, 5% on PD and 38% living with a kidney transplant. The transplant rate in 2018 was 35 p.m.p.: 68% received a kidney from a deceased donor, 30% from a living donor and for 2% the donor source was unknown. For patients commencing dialysis during 2009–13, the unadjusted 5-year survival probability was 42.6%. For patients receiving a kidney transplant within this period, the unadjusted 5-year survival probability was 86.6% for recipients of deceased donor grafts and 93.9% for recipients of living donor grafts.
Keywords: dialysis, epidemiology, kidney failure, kidney transplantation, survival analysis
INTRODUCTION
This article summarizes the European Renal Association – European Dialysis and Transplant Association (ERA-EDTA) Registry’s 2018 Annual Report, providing the most recent data on the epidemiology of kidney replacement therapy (KRT) for kidney failure in Europe, and countries bordering the Mediterranean Sea [1]. In total, 51 national or regional renal registries from 34 countries provided data to the ERA-EDTA Registry, of which 34 renal registries from 18 countries provided individual patient data, and another 17 renal registries provided aggregated data from 17 countries (Supplementary Appendix S1). In total, these registries cover a general population of 636 million people, which is lower than the 694 million people covered in the 2017 Annual Report [2], as this year Croatia, Georgia, Poland and Sfax region (Tunisia) could not be included. When excluding Israel, the remaining countries cover a general population of 627 million people, representing 74.2% of the total 2018 European general population. On the other hand, compared with our 2017 Annual Report, Montenegro and the Valencian region (Spain) are now included with individual patient data.
This article presents the 2018 incidence and prevalence of KRT, kidney transplantation activity and both patient and graft survival in Europe. More information on the methods used to analyse the data, as well as the complete results, can be found in the ERA-EDTA Registry 2018 Annual Report [1].
RESULTS
Incidence of KRT
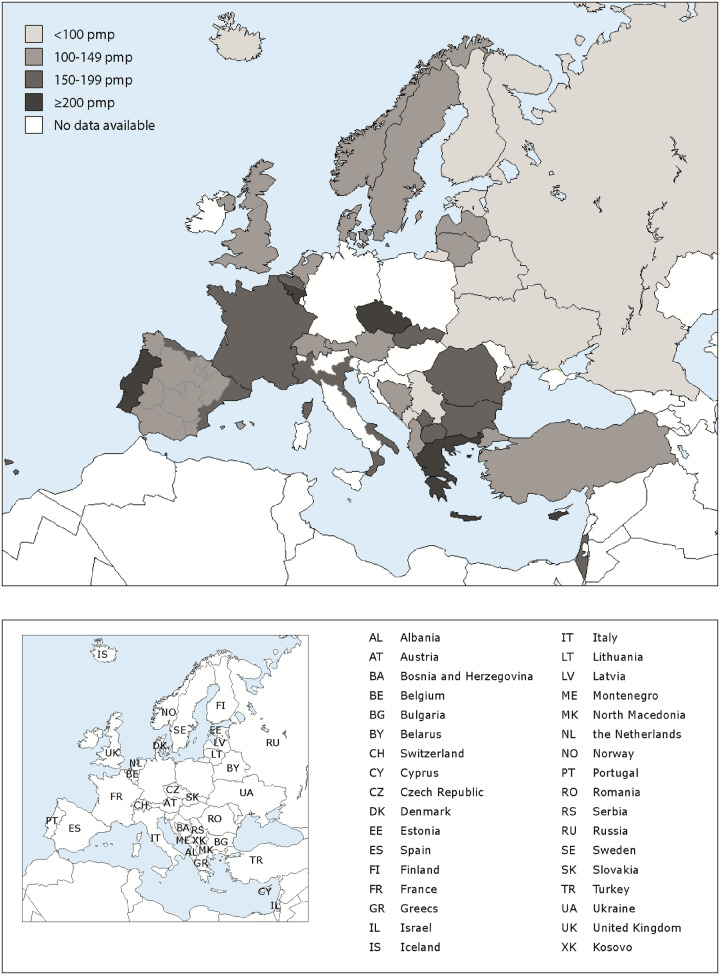
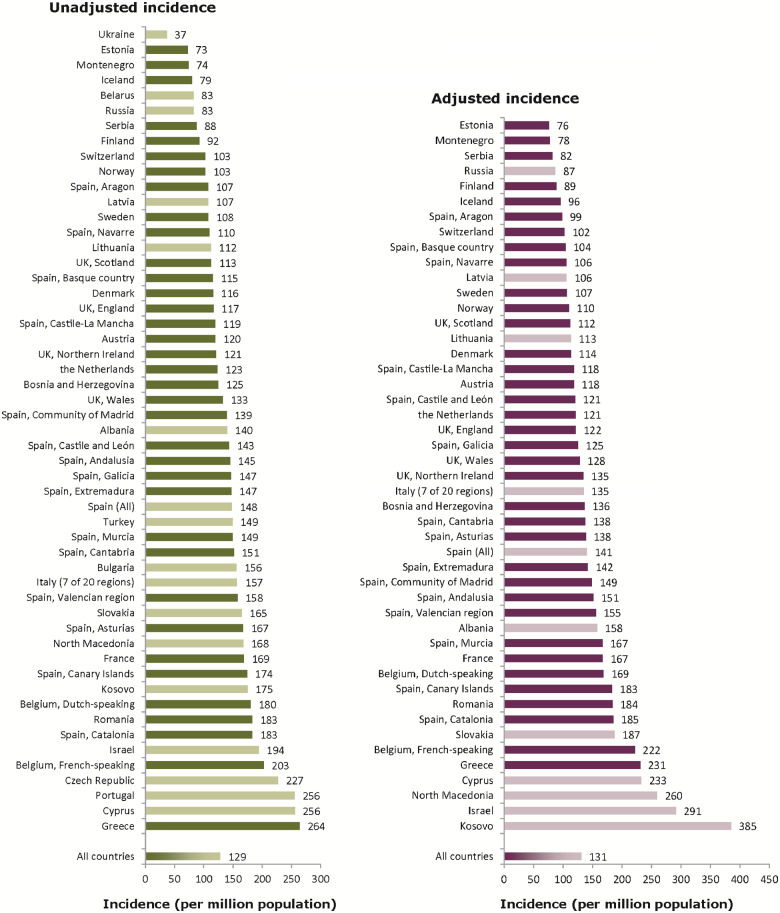
In 2018, 81 714 individuals out of a population of 636 million people started KRT for kidney failure, resulting in an overall unadjusted incidence of 129 per million population (p.m.p.; Table 1). The unadjusted incidence ranged from 37, 73 and 74 p.m.p. in Ukraine, Estonia and Montenegro, respectively, to 256 p.m.p. in Portugal and Cyprus and 264 p.m.p. in Greece (Table 1 and Figures 1 and 2). Of the patients starting KRT, 62% were men, 51% were aged ≥65 years and 20% had diabetes mellitus (DM) as cause of kidney failure (Figure 3). The median age of the patients starting KRT was 66.5 years, and differed by almost 20 years between Ukraine (55.0 years) and the Dutch-speaking part of Belgium (74.4 years; Table 1). The majority (84%) of patients started KRT with haemodialysis (HD), another 11% started with peritoneal dialysis (PD) and 5% of patients received a pre-emptive kidney transplant (Figure 4). While the distribution of initial treatment modalities was similar for men and women, there were considerable differences between age groups, with decreasing proportions of patients receiving either PD or a pre-emptive transplant with increasing age (Figure 4). In addition, compared with patients without DM as cause of kidney failure, those with DM as cause of kidney failure more often started KRT on HD (85% versus 80%), and less frequently received a pre-emptive kidney transplant (2% versus 6%). Among the incident patients receiving KRT at Day 91 after the onset of treatment, 82% were receiving HD, 13% were receiving PD and 5% were living with a functioning kidney transplant (Figure 5). When compared with Day 1, the percentage of patients receiving HD decreased, a finding that was particularly evident in the younger age groups.
Table 1.
Incidence of KRT (as count and p.m.p.) in 2018, at Day 1, by country or region, unadjusted and the mean and median age at the start of KRT, and the incidence of KRT for patients with DM as cause of kidney failure (as count and p.m.p.)
|
Country/region |
General population covered by the registry in thousands | Incidence of KRT in 2018 at Day 1 |
|||||
|---|---|---|---|---|---|---|---|
| All (n) | All (p.m.p.) | Mean age (years) | Median age (years) | DM (n) | DM (p.m.p.) | ||
| Albania | 2841 | 398 | 140 | 59.8 | 61.0 | 78 | 27 |
| Austria | 8822 | 1057 | 120 | 64.4 | 67.1 | 243 | 28 |
| Belarus | 9475 | 782 | 83 | 176 | 19 | ||
| Belgium, Dutch-speakinga | 6578 | 1186 | 180 | 71.1 | 74.4 | 241 | 37 |
| Belgium, French-speakinga | 4849 | 983 | 203 | 68.6 | 70.0 | 187 | 39 |
| Bosnia and Herzegovina | 3531 | 440 | 125 | 62.0 | 64.0 | 127 | 36 |
| Bulgaria | 7000 | 1091 | 156 | 317 | 45 | ||
| Cyprus | 876 | 224 | 256 | 69.0 | 73.0 | 86 | 98 |
| Czech Republicb | 9983 | 2265 | 227 | ||||
| Denmark | 5850 | 679 | 116 | 63.2 | 66.8 | 174 | 30 |
| Estonia | 1322 | 96 | 73 | 57.3 | 58.5 | 20 | 15 |
| Finland | 5516 | 509 | 92 | 61.1 | 64.1 | 161 | 29 |
| France | 66 966 | 11 296 | 169 | 67.6 | 70.5 | 2503 | 37 |
| Greece | 10 733 | 2833 | 264 | 70.9 | 73.5 | 682 | 64 |
| Iceland | 353 | 28 | 79 | 59.7 | 59.6 | 5 | 14 |
| Israel | 8883 | 1723 | 194 | 65.4 | 68.1 | 780 | 88 |
| Italy (7 of 20 regions) | 21 427 | 3355 | 157 | 68.6 | 71.6 | 559 | 26 |
| Kosovo | 1688 | 295 | 175 | 62.0 | 65.0 | 112 | 66 |
| Latvia | 1312 | 141 | 107 | 62.3 | 66.0 | 28 | 21 |
| Lithuania | 2809 | 316 | 112 | 59.9 | 60.4 | 46 | 16 |
| Montenegroa | 622 | 46 | 74 | 56.5 | 60.1 | 10 | 16 |
| North Macedonia | 2022 | 339 | 168 | 62.9 | 64.0 | 104 | 51 |
| Norway | 5312 | 546 | 103 | 63.8 | 67.9 | 92 | 17 |
| Portugal | 10 309 | 2634 | 256 | 811 | 79 | ||
| Romania | 19 064 | 3487 | 183 | 62.5 | 64.5 | 424 | 22 |
| Russiab | 133 570 | 11 070 | 83 | 56.3 | 61.0 | 1838 | 14 |
| Serbia | 6284 | 552 | 88 | 61.0 | 63.6 | 124 | 20 |
| Slovakiab | 5444 | 898 | 165 | 64.5 | 66.0 | 325 | 60 |
| Spain (All) | 46 723 | 6918 | 148 | 64.8 | 68.2 | 1702 | 36 |
| Spain, Andalusia | 8419 | 1221 | 145 | 62.5 | 65.5 | 319 | 38 |
| Spain, Aragon | 1317 | 141 | 107 | 66.8 | 69.8 | 33 | 25 |
| Spain, Asturias | 1028 | 172 | 167 | 67.2 | 68.5 | 53 | 52 |
| Spain, Basque country | 2174 | 251 | 115 | 65.2 | 68.4 | 61 | 28 |
| Spain, Canary Islands | 2192 | 382 | 174 | 64.3 | 66.4 | 136 | 62 |
| Spain, Cantabriaa | 581 | 88 | 151 | 69.4 | 72.1 | 12 | 21 |
| Spain, Castile and Leóna | 2409 | 345 | 143 | 66.3 | 69.4 | 81 | 34 |
| Spain, Castile-La Manchaa | 2034 | 243 | 119 | 66.7 | 69.5 | 67 | 33 |
| Spain, Catalonia | 7600 | 1392 | 183 | 65.8 | 69.6 | 275 | 36 |
| Spain, Community of Madrid | 6578 | 915 | 139 | 65.6 | 69.2 | 241 | 37 |
| Spain, Extremadura | 1073 | 158 | 147 | 64.5 | 66.4 | 41 | 38 |
| Spain, Galicia | 2702 | 397 | 147 | 65.3 | 67.9 | 103 | 38 |
| Spain, Murcia | 1479 | 221 | 149 | 62.1 | 65.4 | 54 | 37 |
| Spain, Navarrea | 647 | 71 | 110 | 67.4 | 70.4 | 16 | 25 |
| Spain, Valencian region | 4964 | 783 | 158 | 66.2 | 70.0 | 166 | 33 |
| Sweden | 10 175 | 1095 | 108 | 64.2 | 68.1 | 280 | 28 |
| Switzerland | 8514 | 875 | 103 | 65.5 | 69.3 | 192 | 23 |
| The Netherlands | 16 025 | 1975 | 123 | 63.9 | 67.2 | 380 | 24 |
| Turkeyc | 82 004 | 12 232 | 149 | 954 | 54 | ||
| Ukraine | 42 216 | 1563 | 37 | 52.8 | 55.0 | 370 | 9 |
| UK, Englanda,d | 55 977 | 6530 | 117 | 62.0 | 64.0 | 1761 | 31 |
| UK, Northern Irelanda | 1882 | 228 | 121 | 64.3 | 67.2 | 48 | 26 |
| UK, Scotland | 5438 | 613 | 113 | 60.2 | 62.1 | 180 | 33 |
| UK, Walesa | 3139 | 416 | 133 | 63.4 | 65.9 | 125 | 40 |
| All countries | 635 534 | 81 714 | 129 | 63.5 | 66.5 | 16 245 | 29 |
When cells are left empty, the data are unavailable and could not be used for the calculation of the summary data.
Patients <20 years are not reported. The true incidence counts are therefore slightly higher than the counts reported here.
Data include dialysis patients only.
Data on incidence by cause of kidney failure (DM) is based on 2642 dialysis patients (21.6% of total).
The incidence is underestimated by ∼2% due to one centre not submitting data since 2014.
FIGURE 1:
Incidence of KRT (p.m.p.) in 2018, at Day 1, by country or region, unadjusted. The incidence for Czech Republic, Russia and Slovakia only includes patients receiving dialysis. For England (UK), the incidence is underestimated by 2% (Table 1).
FIGURE 2:
Unadjusted (left panel) and adjusted (right panel) incidence of KRT p.m.p. in 2018, at Day 1, by country or region. Registries providing individual patient data are shown as dark bars, and registries providing aggregated data as light bars. Adjustment of incidence was performed by standardizing to the age and sex distribution of the EU27 population. The incidence for Czech Republic, Russia and Slovakia only includes patients receiving dialysis. For England (UK), the incidence is underestimated by 2% (Table 1).
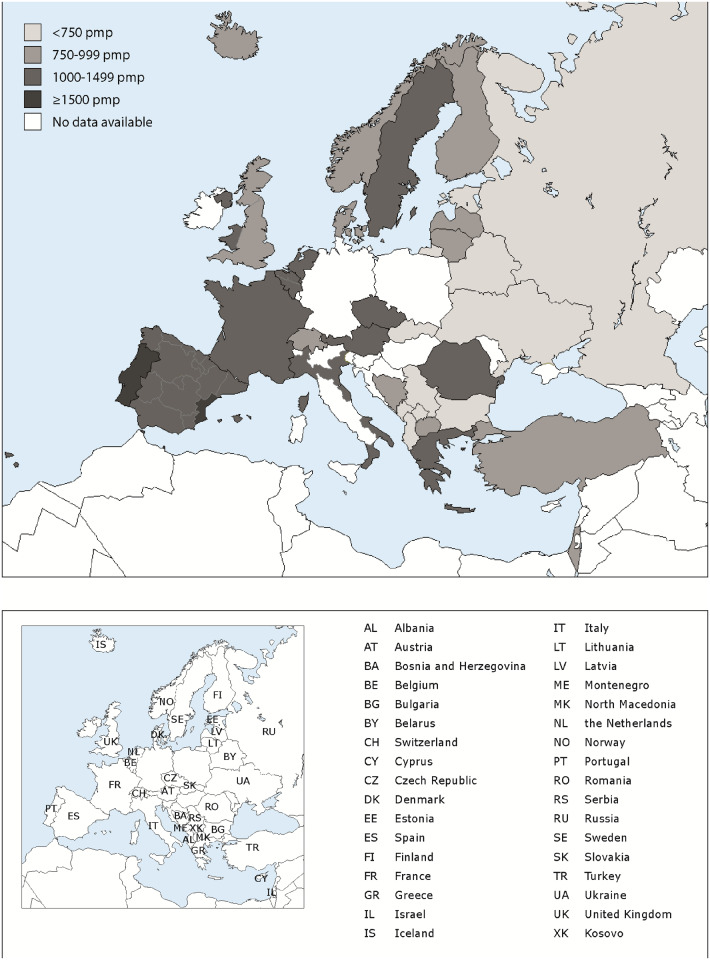
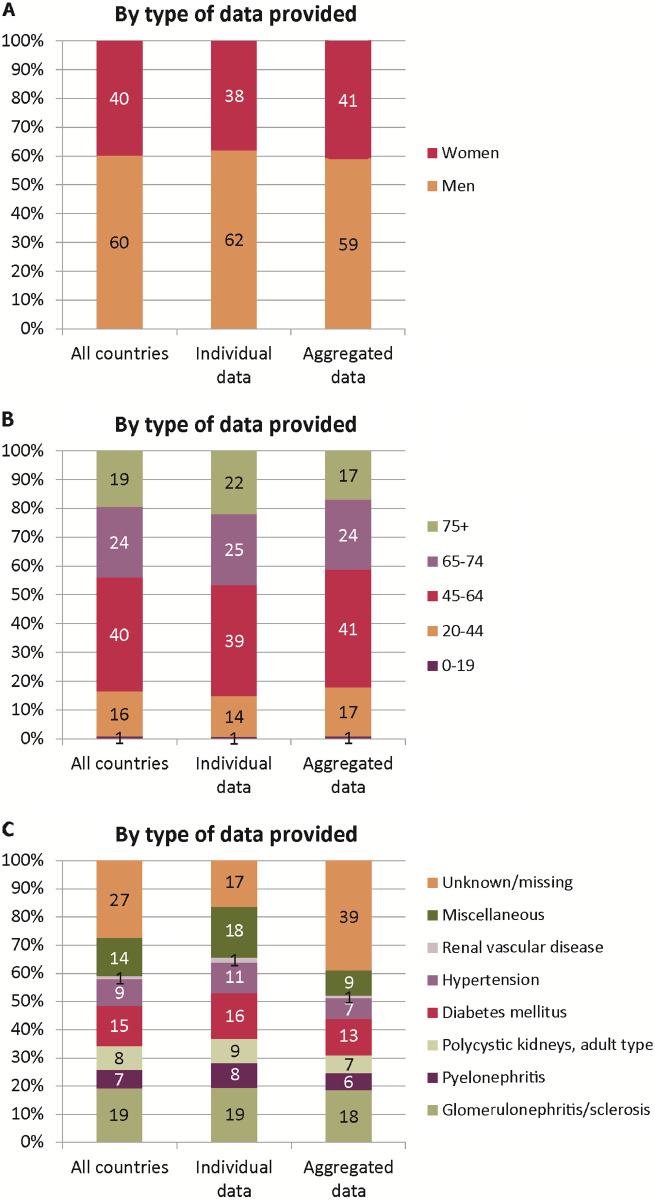
FIGURE 3:
(A) Sex, (B) age and (C) cause of kidney failure distribution by type of data provided for incident patients accepted for KRT in 2018, at Day 1. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 4:
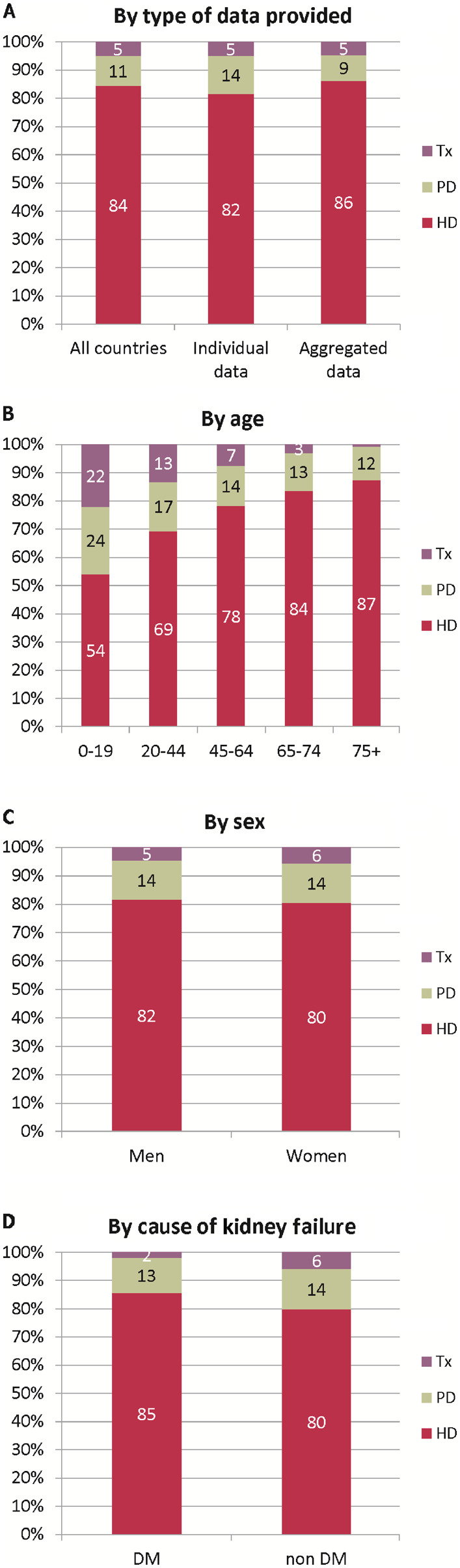
Treatment modality distribution, at Day 1, by (A) type of data provided, (B) age, (C) sex and (D) cause of kidney failure (DM and non-DM) for incident patients accepted for KRT in 2018. Parts (B), (C) and (D) are only based on the data from registries providing individual patient data. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data. Tx, kidney transplant
FIGURE 5:
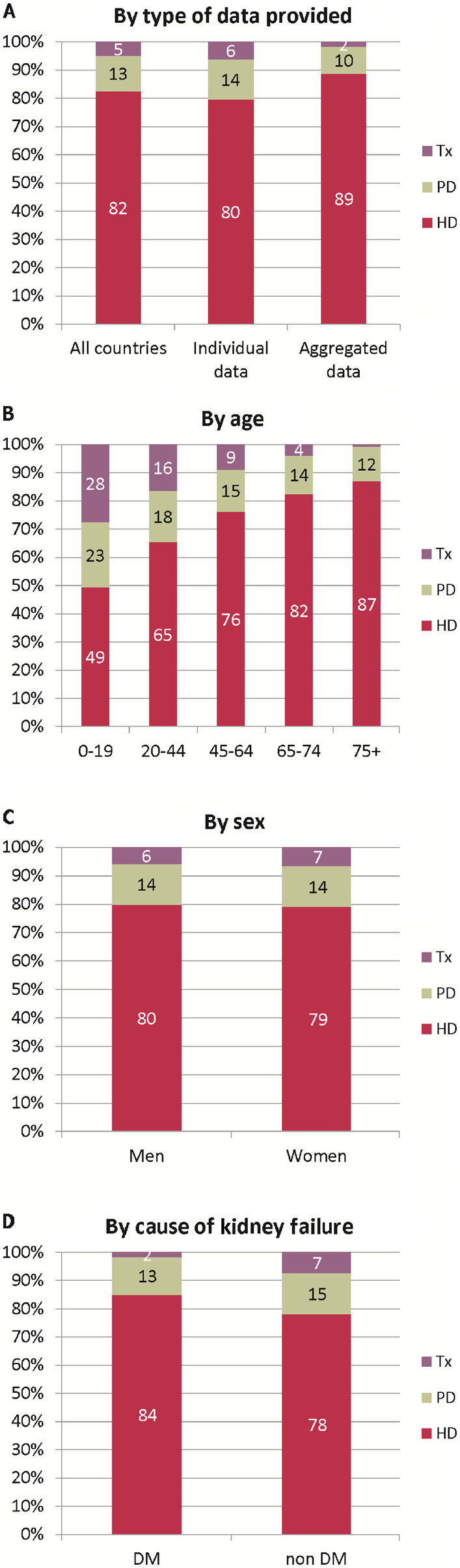
Treatment modality distribution, at Day 91, by (A) type of data provided, (B) age, (C) sex and (D) cause of kidney failure (DM and non-DM) for incident patients accepted for KRT in 2018. Parts (B), (C) and (D) are only based on the data from registries providing individual patient data. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data. Tx, kidney transplant
Prevalence of KRT
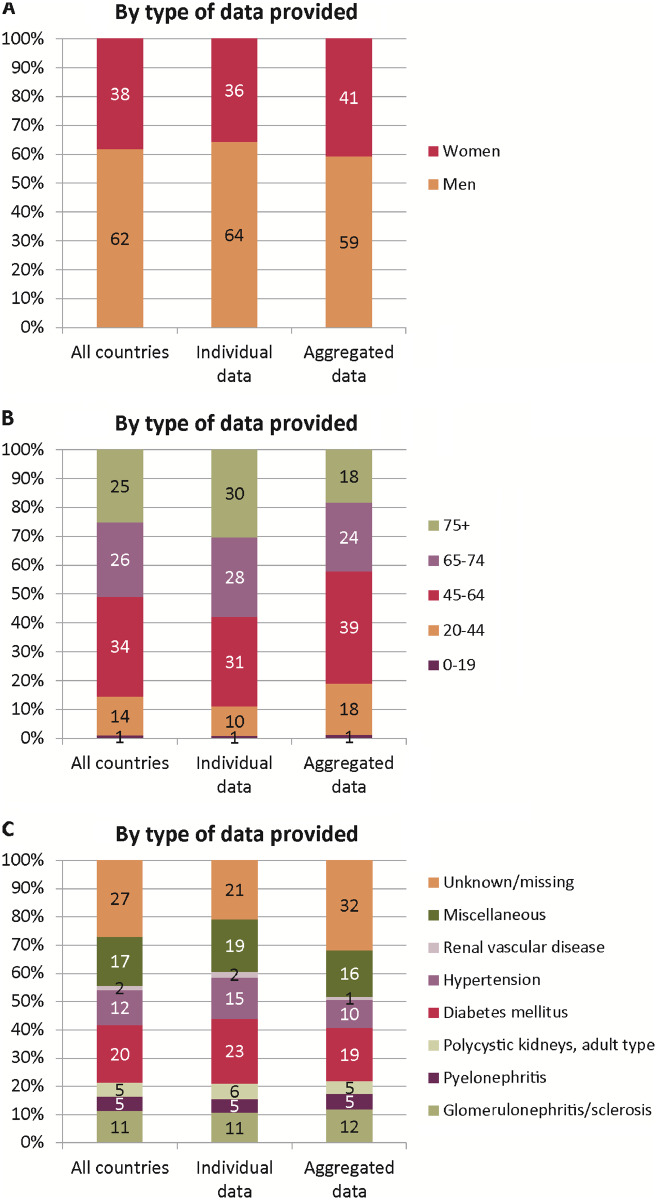
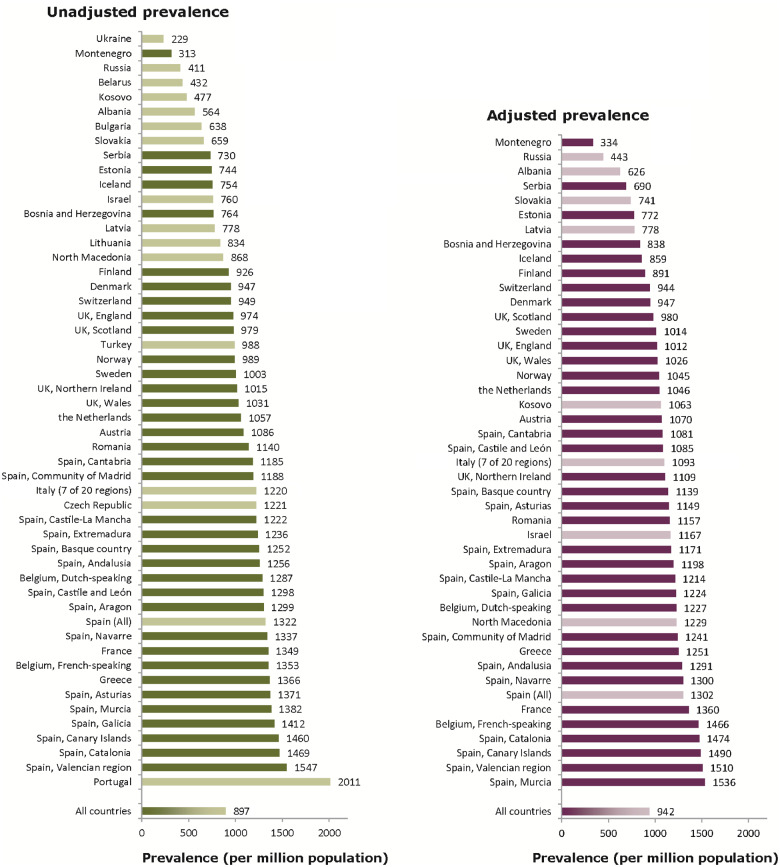
On 31 December 2018, 569 678 patients were receiving KRT for kidney failure, corresponding to an overall unadjusted prevalence of 897 p.m.p. (Table 2). Among the individual countries or regions the unadjusted prevalence ranged from 229, 313 and 411 p.m.p. in Ukraine, Montenegro and Russia, respectively, to 1469, 1547 and 2011 p.m.p. in Catalonia (Spain), Valencian region (Spain) and Portugal, respectively (Table 2 and Figures 6 and 7). Of the prevalent patients, 60% were men, 43% were aged ≥65 years and 15% had DM as cause of kidney failure (Figure 8). The median age of prevalent patients receiving KRT was 63.0 years, ranging from 52.0 years in Albania and Ukraine to 68.6 years in Israel (Table 2). Of the prevalent patients, 57% were receiving HD and 5% were receiving PD, while 38% were living with a kidney transplant (Figure 9). Compared with prevalent patients with a cause of kidney failure other than DM, those with DM as cause of kidney failure were less likely to be living with a functioning kidney transplant (51% versus 29%).
Table 2.
Prevalence of KRT (as count and p.m.p.) on 31 December 2018, by country or region, unadjusted and the mean and median age on 31 December 2018 and the prevalence of KRT for patients DM as cause of kidney failure (as count and p.m.p.)
|
Country/region |
General population covered by the registry in thousands | Prevalent patients on KRT in 2018 |
|||||
|---|---|---|---|---|---|---|---|
| All (n) | All (p.m.p.) | Mean age (years) | Median age (years) | DM (n) | DM (p.m.p.) | ||
| Albania | 2841 | 1602 | 564 | 51.3 | 52.0 | 322 | 113 |
| Austria | 8822 | 9577 | 1086 | 62.0 | 63.4 | 1756 | 199 |
| Belarus | 9475 | 4096 | 432 | 541 | 57 | ||
| Belgium, Dutch-speakinga | 6578 | 8466 | 1287 | 66.4 | 68.4 | 1435 | 218 |
| Belgium, French-speakinga | 4849 | 6559 | 1353 | 65.2 | 66.9 | 1164 | 240 |
| Bosnia and Herzegovina | 3531 | 2699 | 764 | 59.9 | 61.6 | 539 | 153 |
| Bulgaria | 7000 | 4464 | 638 | ||||
| Cyprus | 876 | ||||||
| Czech Republic | 9983 | 12 194 | 1221 | ||||
| Denmark | 5850 | 5541 | 947 | 59.1 | 60.7 | 938 | 160 |
| Estonia | 1322 | 983 | 744 | 58.3 | 59.0 | 176 | 133 |
| Finland | 5516 | 5106 | 926 | 59.6 | 62.1 | 1286 | 233 |
| France | 66 966 | 90 358 | 1349 | 63.2 | 65.3 | 14 881 | 222 |
| Greece | 10 733 | 14 665 | 1366 | 65.4 | 67.5 | 2757 | 257 |
| Iceland | 353 | 266 | 754 | 56.3 | 57.5 | 30 | 85 |
| Israelb | 8883 | 6747 | 760 | 66.6 | 68.6 | 3121 | 351 |
| Italy (7 of 20 regions) | 21 427 | 26 131 | 1220 | 62.8 | 65.0 | 2916 | 136 |
| Kosovo | 1688 | 805 | 477 | 62.9 | 66.0 | 240 | 142 |
| Latvia | 1312 | 1020 | 778 | 55.5 | 57.0 | 103 | 79 |
| Lithuania | 2809 | 2342 | 834 | ||||
| Montenegroa | 622 | 195 | 313 | 57.0 | 59.5 | 28 | 45 |
| North Macedonia | 2022 | 1756 | 868 | 58.8 | 60.0 | 304 | 150 |
| Norway | 5312 | 5256 | 989 | 60.0 | 62.2 | 724 | 136 |
| Portugal | 10 309 | 20 730 | 2011 | 68.0 | 68.5 | 3670 | 356 |
| Romania | 19 064 | 21 738 | 1140 | 62.6 | 64.3 | 2220 | 116 |
| Russia | 133 570 | 54 953 | 411 | 56.8 | 59.0 | 7913 | 59 |
| Serbia | 6284 | 4589 | 730 | 60.0 | 62.4 | 808 | 129 |
| Slovakiab | 5444 | 3589 | 659 | 64.1 | 66.0 | 1202 | 221 |
| Spain (All) | 46 723 | 61 773 | 1322 | 59.9 | 63.1 | 10 014 | 214 |
| Spain, Andalusia | 8419 | 10 577 | 1256 | 60.9 | 62.2 | 1675 | 199 |
| Spain, Aragon | 1317 | 1710 | 1299 | 63.8 | 65.2 | 307 | 233 |
| Spain, Asturias | 1028 | 1409 | 1371 | 63.9 | 65.1 | 252 | 245 |
| Spain, Basque country | 2174 | 2723 | 1252 | 62.2 | 64.4 | 328 | 151 |
| Spain, Canary Islands | 2192 | 3200 | 1460 | 61.8 | 63.1 | 886 | 404 |
| Spain, Cantabriaa | 581 | 689 | 1185 | 63.4 | 64.7 | 97 | 167 |
| Spain, Castile and Leóna | 2409 | 3126 | 1298 | 65.4 | 66.5 | 552 | 229 |
| Spain, Castile-La Manchaa | 2034 | 2485 | 1222 | 63.3 | 64.1 | 405 | 199 |
| Spain, Catalonia | 7600 | 11 162 | 1469 | 63.3 | 65.0 | 1609 | 212 |
| Spain, Community of Madrid | 6578 | 7816 | 1188 | 62.3 | 63.8 | 1406 | 214 |
| Spain, Extremadura | 1073 | 1326 | 1236 | 62.4 | 62.8 | 207 | 193 |
| Spain, Galicia | 2702 | 3816 | 1412 | 63.1 | 64.5 | 649 | 240 |
| Spain, Murcia | 1479 | 2043 | 1382 | 62.4 | 63.3 | 299 | 202 |
| Spain, Navarrea | 647 | 865 | 1337 | 63.2 | 65.0 | 128 | 198 |
| Spain, Valencian region | 4964 | 7679 | 1547 | 63.5 | 65.5 | 1095 | 221 |
| Sweden | 10 175 | 10 206 | 1003 | 60.3 | 62.4 | 1836 | 180 |
| Switzerland | 8514 | 8077 | 949 | 62.5 | 64.5 | 1220 | 143 |
| The Netherlands | 16 542 | 17 493 | 1057 | 60.8 | 62.8 | 2336 | 141 |
| Turkeyc | 82 004 | 81 055 | 988 | 3043 | 338 | ||
| Ukraine | 42 216 | 9659 | 229 | 50.7 | 52.0 | 1511 | 36 |
| UK, Englanda,d | 55 977 | 54 520 | 974 | 59.0 | 59.6 | 9645 | 172 |
| UK, Northern Irelanda | 1882 | 1909 | 1015 | 59.3 | 59.5 | 283 | 150 |
| UK, Scotland | 5438 | 5324 | 979 | 57.1 | 58.5 | 901 | 166 |
| UK, Walesa | 3139 | 3235 | 1031 | 59.6 | 60.7 | 561 | 179 |
| All countries | 636 051 | 569 678 | 897 | 61.1 | 63.0 | 80 424 | 148 |
When cells are left empty, the data are unavailable and could not be used for the calculation of the summary data.
Patients <20 years are not reported. The true prevalent counts are therefore slightly higher than the counts reported here.
Data on prevalence include dialysis patients only.
Data on the prevalence by cause of kidney failure (DM) is based on 8904 dialysis patients (11.0% of total).
The prevalence is underestimated by ∼1% due to one centre not submitting data since 2014.
FIGURE 6:
Prevalence of KRT (p.m.p.) on 31 December 2018 by country or region. The prevalence for Israel and Slovakia only includes patients receiving dialysis. For England (UK), the prevalence is underestimated by 1% (see Table 2).
FIGURE 7:
Unadjusted (left panel) and adjusted (right panel) prevalence (p.m.p.) of KRT on 31 December 2018 by country or region. Registries providing individual patient data are shown as dark bars, and registries providing aggregated data as light bars. Adjustment of the prevalence was performed by standardizing to the age and sex distribution of the EU27 population. The prevalence for Israel and Slovakia only includes patients receiving dialysis. For England (UK), the prevalence is underestimated by 1% (see Table 2).
FIGURE 8:
(A) Sex, (B) age and (C) cause of kidney failure distribution, by type of data provided for prevalent patients on KRT on 31 December 2018. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 9:
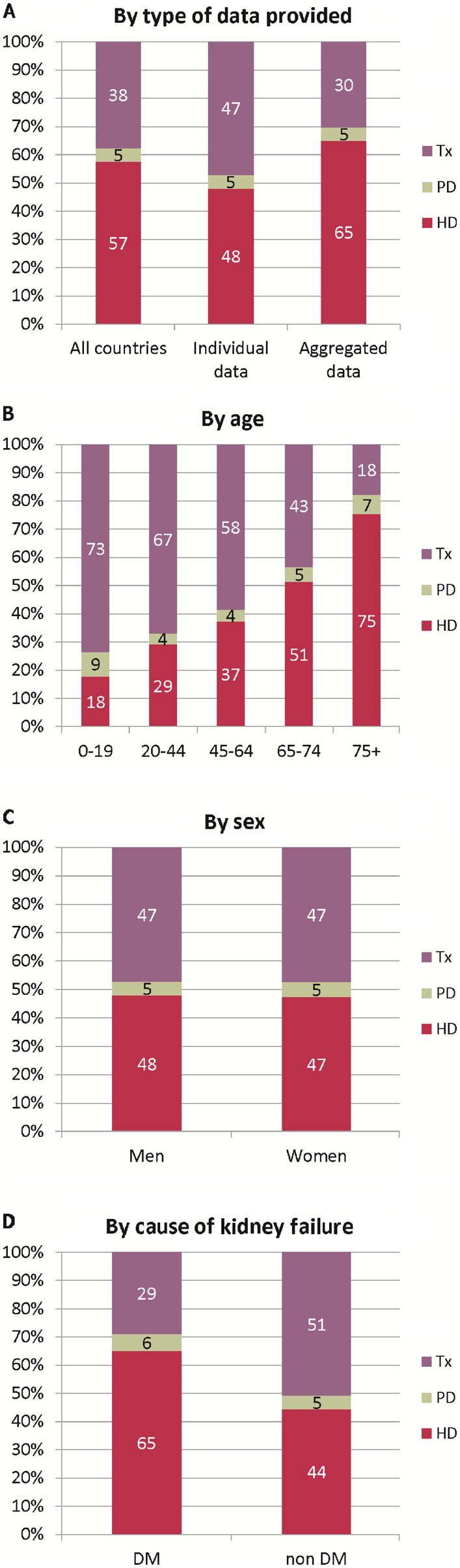
Treatment modality distribution by (A) type of data provided, (B) age, (C) sex and (D) cause of kidney failure (DM and non-DM) for prevalent patients on KRT on 31 December 2018. Parts (B), (C) and (D) are only based on the data from registries providing individual patient data. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data. Tx, kidney transplant
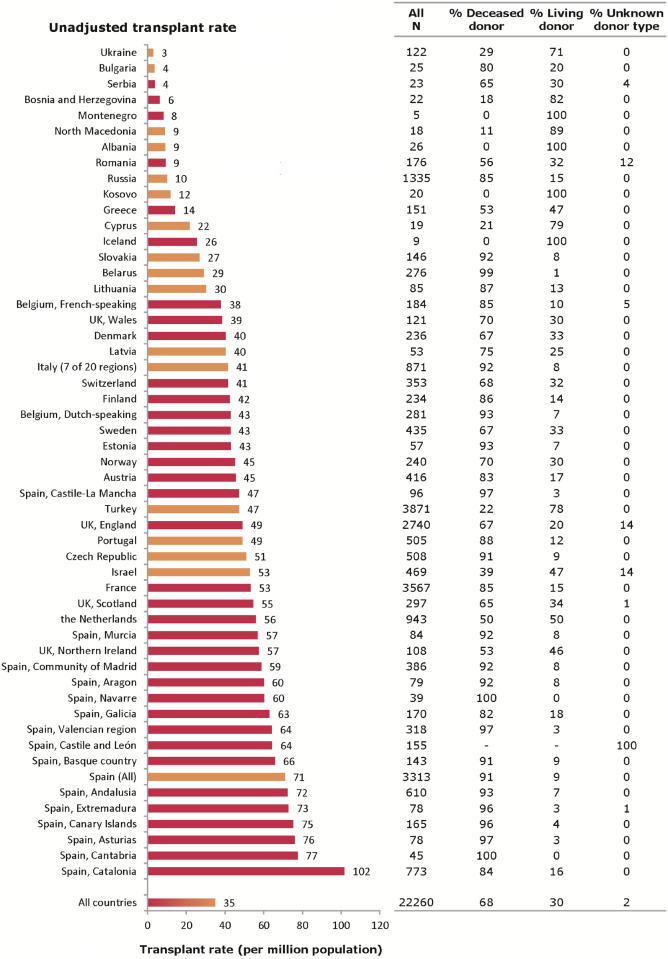
Kidney transplantation
In 2018, a total of 22 260 kidney transplantations were performed, corresponding to an overall unadjusted transplant rate of 35 p.m.p. (Figure 10). In the individual countries or regions, the unadjusted kidney transplant rates ranged from 3 p.m.p. in Ukraine and 4 p.m.p. in Bulgaria and Serbia, to 76, 77 and 102 p.m.p. in Asturias (Spain), Cantabria (Spain) and Catalonia (Spain), respectively. Overall, the unadjusted deceased donor kidney transplant rate was more than twice that of living donor transplants (24 p.m.p. versus 10 p.m.p.; 68% versus 30%; Figures 11 and 12). The highest unadjusted rates of deceased donor kidney transplants were observed in several Spanish regions (>70 p.m.p.; Figure 12), whereas the highest unadjusted rates of living donor transplants were observed in Northern Ireland (27 p.m.p.), the Netherlands (28 p.m.p.) and Turkey (37 p.m.p.; Figure 12).
FIGURE 10:
Kidney transplants performed in 2018, presented as counts and p.m.p. (unadjusted) by country or region. Registries providing individual patient data are shown as red bars, and registries providing aggregated data as orange bars. The total count for Austria is based on residents and non-residents. For Romania, Serbia and England (UK), the overall kidney transplant rate is underestimated by 30, 15 and 7%, respectively.
FIGURE 11:

Donor-type distribution for kidney transplants performed in 2018, by type of data provided. See Supplementary Appendix A1 for a list of countries and regions providing individual patient data or aggregated data.
FIGURE 12:
Deceased donor (A) and living donor (B) kidney transplants performed in 2018 p.m.p., by country or region, unadjusted. Registries providing individual patient data are shown as dark bars and registries providing aggregated data as light bars. The total count for Austria is based on residents and non-residents. For Romania and England (UK), the kidney transplant rate is underestimated by 30 and 7%, respectively. For Serbia, the transplant rate is underestimated by 16% for deceased donor transplants and by 12% for living donor transplants.
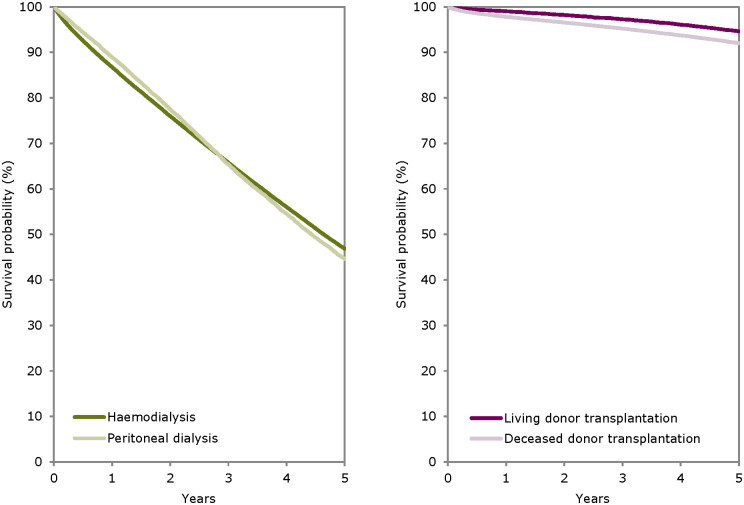
Survival of patients receiving KRT
For patients commencing KRT in the period 2009–13, the 5-year unadjusted patient survival probability was 51.1% [95% confidence interval (95% CI) 51.0–51.2; Table 3]. For patients starting KRT with dialysis in this period, the unadjusted 5-year patient survival probability was 42.6% (95% CI 42.5–42.7). Adjusted analyses for patient survival on HD and PD revealed higher survival probabilities in the first 3 years for those receiving PD (Figure 13). For patients receiving a kidney transplant in the period 2009–13, living donor transplant recipients experienced a higher adjusted 5-year patient survival than recipients of deceased donor transplants: 94.7% (95% CI 94.3–95.2) versus 92.0% (95% CI 91.7–92.3; Figure 13), as well as a higher adjusted 5-year graft survival: 87.1% (95% CI 86.4–87.8) versus 81.1% (95% CI 80.6–81.5; Table 3). A description of the adjustments made and the countries and regions included in these analyses can be found in Table 3.
Table 3.
The survival probabilities at 1, 2 and 5 years by treatment modality and cohort, from Day 1 of the start of KRT, dialysis or from the day of kidney transplantation
| Survival probabilities as percentage (95% CIs) |
|||||||
|---|---|---|---|---|---|---|---|
| Cohort: 2009–13 | Cohort: 2012–16 | ||||||
| Survival type | 1 year | 2 years | 5 years | 1 year | 2 years | ||
| Patient survival on KRT | |||||||
| Unadjusted | 84.3 (84.2–84.5) | 74.3 (74.2–74.5) | 51.1 (51.0–51.2) | 85.1 (85.0–85.3) | 75.1 (75.0–75.3) | ||
| Adjusteda | 87.0 (86.9–87.2) | 77.9 (77.6–78.1) | 53.1 (52.8–53.4) | 87.5 (87.4–87.7) | 78.3 (78.1–78.5) | ||
| Patient survival on dialysis | |||||||
| Unadjusted | 83.3 (83.1–83.4) | 71.8 (71.7–72.0) | 42.6 (42.5–42.7) | 84.1 (83.9–84.2) | 72.6 (72.4–72.7) | ||
| Adjusteda | 85.5 (85.3–85.6) | 75.1 (74.9–75.3) | 46.4 (46.1–46.8) | 86.3 (86.1–86.5) | 76.0 (75.8–76.3) | ||
| Patient survival after first kidney transplantation (deceased donor) | |||||||
| Unadjusted | 96.1 (95.9–96.3) | 94.0 (93.8–94.2) | 86.6 (86.3–86.9) | 96.3 (96.1–96.4) | 94.1 (93.9–94.3) | ||
| Adjustedb | 97.8 (97.7–97.9) | 96.5 (96.4–96.7) | 92.0 (91.7–92.3) | 98.0 (97.8–98.1) | 96.8 (96.6–96.9) | ||
| Graft survival after first kidney transplantation (deceased donor) | |||||||
| Unadjusted | 90.7 (90.5–91.0) | 87.6 (87.3–87.9) | 77.5 (77.2–77.9) | 91.2 (90.9–91.4) | 88.0 (87.7–88.3) | ||
| Adjustedb | 92.4 (92.1–92.6) | 89.7 (89.4–90.0) | 81.1 (80.6–81.5) | 93.0 (92.7–93.2) | 90.4 (90.1–90.7) | ||
| Patient survival after first kidney transplantation (living donor) | |||||||
| Unadjusted | 98.9 (98.7–99.1) | 97.9 (97.6–98.2) | 93.9 (93.5–94.3) | 98.9 (98.7–99.1) | 98.0 (97.8–98.3) | ||
| Adjustedb | 99.1 (98.9–99.2) | 98.2 (98.0–98.5) | 94.7 (94.3–95.2) | 99.1 (98.9–99.2) | 98.3 (98.1–98.5) | ||
| Graft survival after first kidney transplantation (living donor) | |||||||
| Unadjusted | 96.5 (96.2–96.8) | 94.7 (94.3–95.1) | 87.8 (87.2–88.3) | 96.7 (96.4–97.0) | 95.1 (94.8–95.5) | ||
| Adjustedb | 96.3 (95.9–96.6) | 94.4 (94.0–94.9) | 87.1 (86.4–87.8) | 96.5 (96.2–96.8) | 94.8 (94.4–95.2) | ||
The findings are based on data from the following renal registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque country), Spain (Cantabria), Spain (Castile and León), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Community of Madrid), Spain (Extremadura), Spain (Galicia), Spain (Valencian region), Sweden, the Netherlands, UK (England/Northern Ireland/Wales) and UK (Scotland). Unadjusted survival probabilities were calculated using the Kaplan–Meier method, and adjusted survival probabilities using the Cox regression model.
Analyses were adjusted using fixed values: age (67 years), sex (63% men) and cause of kidney failure (24% DM, 19% hypertension/renal vascular disease, 11% glomerulonephritis and 46% other causes).
Analyses were adjusted using fixed values: age (50 years), sex (63% men) and cause of kidney failure (14% DM, 10% hypertension/renal vascular disease, 23% glomerulonephritis and 53% other causes).
FIGURE 13:
Survival of patients starting HD and PD between 2009 and 2013 from Day 91 (A) and patients receiving a first kidney transplant from a living or deceased donor between 2009 and 2013 (B). Survival on dialysis was censored for kidney transplantation, and adjusted using fixed values for age (67 years), sex (63% men) and cause of kidney failure (24% DM, 19% hypertension/renal vascular disease, 11% glomerulonephritis and 46% other causes). Survival after kidney transplantation was adjusted using fixed values for age (50 years), sex (63% men) and cause of kidney failure (14% DM, 10% hypertension/renal vascular disease, 23% glomerulonephritis and 53% other causes). These figures are based on the data from the following registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque country), Spain (Cantabria), Spain (Castile and León), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Extremadura), Spain (Galicia), Spain (Community of Madrid), Spain (Valencian region), Sweden, the Netherlands, UK (England/Northern Ireland/Wales) and UK (Scotland).
Expected remaining lifetime
Patients receiving dialysis between 2014 and 2018 are expected to live only half of the estimated expected remaining lifetime of patients living with a functioning kidney transplant in the same period (Figure 14). When compared with the general population, the life expectancy of patients on dialysis was ∼70% shorter, while for kidney transplant recipients it was ∼40% shorter.
FIGURE 14:
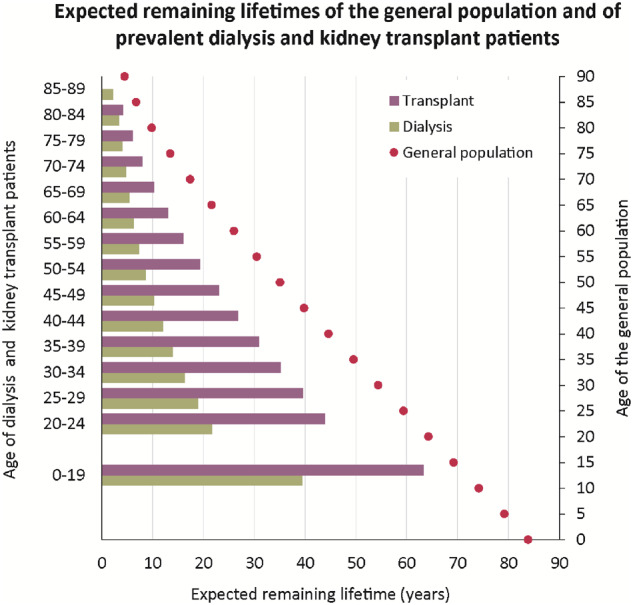
Expected remaining lifetimes of prevalent dialysis and kidney transplant patients (Cohort 2013–17) and the general population (Cohort 2013–17), by age. This figure is based on data from the following registries providing individual patient data: Austria, Belgium (Dutch-speaking), Belgium (French-speaking), Bosnia and Herzegovina, Denmark, Finland, France, Greece, Iceland, Norway, Spain (Andalusia), Spain (Aragon), Spain (Asturias), Spain (Basque Country), Spain (Cantabria), Spain (Castile and León), Spain (Castile-La Mancha), Spain (Catalonia), Spain (Extremadura), Spain (Galicia), Spain (Community of Madrid), Spain (Valencian region), Sweden, the Netherlands and the UK (all countries).
AFFILIATED REGISTRIES
Albanian Renal Registry (A. Idrizi, M. Rroji and E. Likaj); Austrian Dialysis and Transplant Registry (OEDTR) (F. Engler, J. Kerschbaum, R. Kramar, G. Mayer and the Austrian Society of Nephrology); Belarus Renal Registry (K.S. Komissarov, K.S. Kamisarau and A.V. Kalachyk); Dutch speaking Belgian Society of Nephrology (NBVN) (M. Couttenye, F. Schroven and J. De Meester); French speaking Belgian Society of Nephrology (GNFB) (J.M. des Grottes and F. Collart); Renal Registry Bosnia and Herzegovina (H. Resić, B Jakovljevic and Z. Kelava); Bulgaria (E.S. Vazelov and I. Velinova); Cyprus Renal Registry (K. Ioannou and all of the renal units providing data); Czech Republic: Registry of Dialysis Patients (RDP) (F. Lopot, I. Rychlík and J. Potucek); Danish Nephrology Registry (DNS) (K. Hommel); Estonian Society of Nephrology (Ü. Pechter, K. Lilienthal and M. Rosenberg); Finnish Registry for Kidney Diseases (P. Finne and J. Helve); France: The Epidemiology and Information Network in Nephrology (REIN) (M. Lassalle and C. Couchoud); Hellenic Renal Registry (G. Moustakas); Icelandic End-Stage Renal Disease Registry (R. Pálsson); Montenegro Renal Registry (M. Ratkovic, D. Radunović and F. Tomović); Israel National Registry of Renal Replacement Therapy (R. Dichtiar, L. Keinan-Boker and E. Golan); Italian Registry of Dialysis and Transplantation (RIDT) (A. Limido, M. Nordio and M. Postorino); Kosovo Renal Registry (H. Korca, S. Selmani and M. Tolaj-Avdiu); Latvian Renal Registry (V. Kuzema, H. Cernevskis and A. Popova); Lithuanian Renal Registry (V. Vainauskas, K. Petruliene and E. Žiginskiené); North Macedonian Renal Registry (N. Gjorgjievski, O. Stojceva and B.I. Rambabova); Norwegian Renal Registry (A.V. Reisæter and A. Åsberg); Portuguese Renal Registry (A. Galvão and A. Ferreira); Romanian Renal Registry (G. Mircescu, L. Garneata and E. Podgoreanu); Russian Renal Registry (N. Tomilina, H. Zakharova and A. Andrusev); Renal Registry in Serbia (M. Lausevic, R. Naumovic and all of the Serbian renal units and the Serbian Society of Nephrology); Slovakian Renal Registry (V. Spustová, I. Lajdová and M. Karolyova); Spain Renal Registry (B. Mahillo Durán and Spanish Regional Registries); Swedish Renal Registry (K.G. Prütz, M. Stendahl, M. Evans, S. Schön, T. Lundgren, H. Rydell and M. Segelmark); Swiss Dialysis Registry (P. Ambühl and R. Winzeler); Dutch Renal Registry (RENINE) (L. Heuveling, S. Vogelaar and M. Hemmelder); Registry of the Nephrology, Dialysis and Transplantation in Turkey (TSNNR) (G. Süleymanlar, N. Seyahi and K. Ateş); Ukrainian Renal Data System (M. Kolesnyk, O. Razvazhaieva and N. Kozliuk); UK Renal Registry (all the staff of the UK Renal Registry and of the renal units submitting data); Scottish Renal Registry (SRR) (all of the Scottish renal units); and the regional registries of Andalusia (SICATA) (P. Castro de la Nuez (on behalf of all users of SICATA), Aragon (F. Arribas Monzón), Asturias (P. Beltrán, M. Rodríguez, J.R. Quirós and RERCA Working Group), Basque country (UNIPAR) (Á. Magaz, J. Aranzabal, M. Rodrigo and I. Moina), Canary Islands (S. Trujillo Alemán, I. Santana Gil and C. Torres Medina), Cantabria (J.C. Ruiz San Millán), Castile and León (M.A. Palencia García and P. Ucio Mingo), Castile-La Mancha (G. Gutiérrez Ávila and I. Moreno Alía), Catalonia (RMRC) (J. Comas and J. Tort), Community of Madrid (M.I. Aparicio de Madre and F Tornero Molina), Extremadura [all the renal units (Nephrology and Dialysis)], Galicia (E. Bouzas-Caamaño), Renal Registry of the Region of Murcia (I. Marín Sánchez and C. Santiuste de Pablos), Navarre (M.F. Slon Roblero, J. Manrique Escola and J. Arteaga Coloma) and Valencian region (A. Bernat Hoyos and O. Zurriaga).
ERA-EDTA REGISTRY COMMITTEE MEMBERS
C. Wanner, Germany (ERA-EDTA President); Z.A. Massy, France (Chairman); P. Ambühl, Switzerland; M. Arici, Turkey; M. Evans, Sweden; P. Finne, Finland; J. Harambat, France; J. de Meester, Belgium; L. Mercadal, France; M. Nordio, Italy; S.S. Sørensen, Denmark; and E. Vidal, Italy.
ERA-EDTA REGISTRY OFFICE STAFF
K.J. Jager (Managing Director), M. Bonthuis (for the paediatric section), R. Boenink, J.R. Bosdriesz, R. Cornet, G. Guggenheim, A.L.C.J.R.M. Huijben, A. Kramer, V.S. Stel and A.J. Weerstra.
SUPPLEMENTARY DATA
Supplementary data are available at ckj online.
Supplementary Material
ACKNOWLEDGEMENTS
The ERA-EDTA Registry would like to thank the patients and staff of all the dialysis and transplant units who have contributed data via their national and regional renal registries. In addition, we would like to thank the persons and organizations listed in the paragraph ‘Affiliated Registries’ for their contribution to the work of the ERA-EDTA Registry.
FUNDING
The ERA-EDTA Registry is funded by the ERA-EDTA. This article was written by A.K. et al. on behalf of the ERA-EDTA Registry, which is an official body of the ERA-EDTA. In addition, V.S.S. reports grants from ERA-EDTA, during the conduct of the study; S.B. reports personal fees from Astra Zeneca, outside the submitted work; P.F. reports personal fees from Baxter, outside the submitted work; and K.J.J. reports grants from ERA-EDTA, during the conduct of the study.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.ERA-EDTA Registry. ERA-EDTA registry annual report 2018. Amsterdam UMC, Department of Medical Informatics, Amsterdam, the Netherlands: Amsterdam UMC, 2020 [Google Scholar]
- 2. Kramer A, Boenink R, Noordzij M. et al. The ERA-EDTA registry annual report 2017: a summary. Clin Kidney J 2020; 13: 693–709 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.