Abstract
The pandemic outbreak of coronavirus disease 2019 (COVID-19) is raising global anxiety and fear of both real and perceived health threat from the virus. Overwhelming evidence shows infected patients experiencing neuropsychiatric complications, suggesting that the “psychoneuroimmunity” model might be beneficial in understanding the impact of the virus. Therefore, this Special Issue on “Immunopsychiatry of COVID-19 Pandemic” was launched immediately after the pandemic was declared, with the first paper accepted on the March 25th, 2020. A total of ninety-three papers were accepted, the last one was on the July 10th, 2020 when the initial acute phase started declining. The papers of this Special Issue have illuminated the social impact, psychopathology, neurological manifestation, immunity responses, and potential treatments and prevention on COVID-19. For example, anxiety disorders, mood disorders, and suicidal ideation are most common psychiatric manifestations. COVID-19 infection can have central and/or peripheral nervous system symptoms, including headache, sleep disorders, encephalopathy, and loss of taste and smell. A “three-steps” Neuro-COVID infection model (neuro-invasion, clearance and immune response) was established. The current therapeutic interventions for COVID-19 include supportive intervention, immunomodulatory agents, antiviral therapy, and plasma transfusion. Psychological support should be implemented, improving the psychological wellbeing, as well as to enhance psychoneuroimmunity against COVID-19.
Keywords: Coronavirus disease 2019, COVID-19, Psychoneuroimmunity, Brain, Behavior, Immunity
The pandemic outbreak of coronavirus disease 2019 (COVID-19) is raising global anxiety and fear about the real and perceived health threat from the virus. Overwhelming evidence shows infected patients experiencing neuropsychiatric complications on top of the predominant target of respiratory system (Kim and Su, 2020), suggesting the psychoneuroimmunity model might be beneficial (Lazzari et al., 2020). As the awareness and preparedness against the COVID-19 is now at fullest deployment, early on there was an insufficient understanding of how to mitigate morbidity issues, like autoimmune, neurocognitive, and mental health needs (Vindegaard and Benros, 2020). Therefore, we made an immediate call for the Special Issue of Brain, Behavior, and Immunity on the “Immunopsychiatry of COVID-19 Pandemic”, covering from the biopsychosocial impacts to patients and the care providers, as well as the basic and clinical research.
The COVID-19 caused government lockdown the city to control the pandemic; accurate screening and diagnosis tool for medical staff were urgently needed, as well as the sufficient mental support. The researchers have illuminated the social impact, psychopathology, neurological manifestation, immunity responses of COVID-19, trying to find the potential treatment and prevention. Therefore, this Special Issue on “Immunopsychiatry of COVID-19 Pandemic” was launched immediately after the pandemic was declared, with the first paper accepted on the March 25th, 2020. A total of ninety-three papers were accepted, the last one was on the July 10th, 2020 when the initial acute phase started declining. In this editorial, we reviewed and summarized all the published articles related to this special issue, connecting the efforts of all researchers who have contributed to COVID-19 research.
1. Lockdown
Is lockdown a necessary measure and what is the immunopsychiatry impacts? During the lockdown, emulation suicides, economic crisis, and recession, all had negative psychological impact on individuals, increasing the suicide rate and depressive features, further worsening stigma (Guo et al., 2020, Hao et al., 2020, Mamun and Ullah, 2020, Meda and Slongo, 2020). Furthermore, Zhu et al., recommended that centralized isolation was not only convenient to get timely treatment and interventions, but effective to cut off transfection (Zhu et al., 2020a). Controversially, a relative high prevalence of mental illnesses was found in the quarantined individuals, due to the impacts on daily life, rather than the control measure of quarantine (Zhu et al., 2020b), and social isolation strategies decreased the likelihood of clinically dysfunctional coronavirus anxiety, even when the individuals were under stressful event (Milman et al., 2020).
To improve mental health during the lockdown, Chen et al., used the online questionnaire and reported physical exercise might be beneficial (Chen et al., 2020a), while a family-centered approach might have the potential benefits to optimize the psychological management (Liu et al., 2020a). In addition, Ren and his colleagues’ found that it is necessary to make the information open, transparent and timely (Ren et al., 2020), although the intensity of exposure to media COVID-19 information was positively associated with the individuals’ distress (Yao, 2020). Applying health belief such as encouraging lifestyle modification also helped stress appraisal and coping strategies (Mukhtar, 2020).
2. Screening, diagnosis and medical staff
Screening tools or effective diagnostic instruments are urgently needed, because the COVID-19 pandemic and mitigation efforts carry a mental health toll among medical staff, patients, and general population (Ransing et al., 2020). It is very important to continue tracking the development of vicarious traumatization in medical staff as well as the general public (Ghaffari et al., 2020, Li et al., 2020b). For example, Joob et al., reported that traumatization was caused among the Thailand medical staff by high workload, lack of protective devices, non-effective infection control system, and direct insult by patients (Joob and Wiwanitkit, 2020). In addition, the impact of COVID-19 on different people such as African Americans, individuals with low cognitive function, and elite athletes, suggested that the COVID-19 is a heterogeneous disease; therefore, a standard screening tool is urgently needed (Ajilore and Thames, 2020, Batty et al., 2020, Lassale et al., 2020, Mehrsafar et al., 2020, Sominsky et al., 2020).
The medical staff, as well as the volunteer medical staff, were at high risk of mental health problems during the COVID-19 pandemic, and the majority of mental health workers lacked professional training for psychological crisis intervention (Li et al., 2020a). Non-infectious disease specialists have experienced varying, but increased levels of depression, anxiety and insomnia during this COVID-19 pandemic, which could be reduced by sufficient levels of protective equipment and workplace training (Liu et al., 2020b). The targeted psychological intervention measures should be developed to improve the mental health of non-medical workers on the front-line of COVID-19 epidemic, especially the females and younger individuals (Fang et al., 2020). Thus, expanding the availability of well-prepared mental health professionals is needed (Yang et al., 2020), and all medical staff must have complete and accurate knowledge on COVID-19; using telepsychiatry for practice (Kinoshita et al., 2020) and the internet and television for public health education is helpful (Ko et al., 2020). Rapid mental health interventions could improve the medical staff’s mental health and physical health perceptions (Kang et al., 2020). In the United States, a National Suicide Prevention Lifeline was activated (Montemurro, 2020).
3. Psychopathology
The first longitudinal study on the mental health of general population was reported by Wang et al., during the COVID-19 pandemic in China; they focused on mental illnesses and the impact of quarantine and lockdown, suggesting that governments should focus on effective methods of disseminating COVID-19 knowledge and teaching correct containment methods (Wang et al., 2020). Then, the first data available on the Italian population showed that affective temperament and attachment style predict psychological impact during the COVID-19 pandemic (Moccia et al., 2020).
Anxiety disorders, mood disorders, and suicidal ideation were the most common psychiatric manifestations during the COVID-19 pandemic (Nalleballe et al., 2020); even the convalescent COVID-19 patients had high self-reported depression (Yuan et al., 2020). Too much or repetitive COVID-19 thinking could induce anxiety and cause clinical dysfunction (Lee, 2020). Poor sleep quality among COVID-19 patients was also associated with a slow recovery and an increased need for intensive care (Zhang et al. 2020a). Among patients with mental disorders, the COVID-19 pandemic appeared to disrupt daily routines, cut social ties, and increase financial worries and fears of the future (Frank et al., 2020).
The predictive models created by Gonzalez-Sanguino et al., showed that the greatest protector was spiritual well-being, while loneliness was the strongest predictor of mental illnesses (Gonzalez-Sanguino et al., 2020); physical health, mental health, and job satisfaction of healthcare staff were other potential predictors (Zhang et al., 2020b). Geographical variation was also present: compared with China, Jahanshahi et al., reported that the Iranian adults have more distress (Jahanshahi et al., 2020); in Croatia, during the earthquake co-occurring with COVID-19 pandemic, more people showed mental illnesses than the infection; furthermore, mental illnesses might impede recovery process (Marko et al., 2020). Timely identification of psychological distress and precise classifying of the mental health needs will facilitate development of targeted psychological interventions (Zhang et al., 2020c).
4. Neurological manifestation
COVID-19 infection can have a wide variety of central and/or peripheral nervous system symptoms, including headache, sleep disorders, encephalopathy, seizures, acute cerebrovascular disease, impaired consciousness, dizziness, loss of taste and smell neuroleptic malignant syndrome and anti-NMDA receptor encephalitis (Kajani et al., 2020, Nalleballe et al., 2020, Panariello et al., 2020), as well as neuropsychiatric sequelae such as mood changes, psychosis, neuromuscular dysfunction, or demyelinating processes (Troyer et al., 2020). COVID-19 patients frequently presented with subjective neurological symptoms in their early stage of the disease; cutaneous hyperesthesia was also reported (Krajewski et al., 2020, Liguori et al., 2020). Several COVID-19 cases with delirium or meningoencephalitis were also reported (Duong et al., 2020, Hosseini et al., 2020), and the COVID-19 virus was detected in cerebrospinal fluid by PCR in a case with encephalitis (Duong et al., 2020, Huang et al., 2020).
In some cases, the central and/or peripheral nervous system dysfunction by COVID-19 was similar to Guillain-Barré syndrome; thus, plasma therapy was applied in severely affected patients. Several COVID-19 patients with pneumonia had fair clinical response to plasma therapy; however, among COVID-19 patients with Guillain-Barré syndrome, the effect of plasma therapy has not yet been reported (Coen et al., 2020, Gupta et al., 2020).
5. Immunity, biochemistry and physiology
COVID-19 is highly contagious because most persons lack immunity against this novel virus. Horn et al., proposed an immunopsychiatry model of COVID-19 (Horn et al., 2020). To link the neurological complication and the immunopsychiatry model, Wu et al., reviewed the possible neuro-invasion mechanisms among COVID-19 and other coronaviruses infections (Sun et al., 2020, Wu et al., 2020a), suggesting matrix metalloproteases and the host proteases might involve in this neuroinvasion (Bongetta et al., 2020, Vavougios, 2020a). In addition, gastrointestinal dysfunction, such as diarrhea, as well as olfactory and gustatory impairments, might be caused by neuroinvasion by COVID-19 (Esposito et al., 2020, Vavougios, 2020b). Furthermore, massive infiltration of immune cells in the olfactory epithelium and lamina propria of infected animals in the early stage of infection was found (Bryche et al., 2020), indicating why anosmia could be an early indicator (De Santis, 2020). The above findings support that the virus enters the brain through axons of olfactory bulb neurons and the angiotensin converting enzyme 2 (ACE2) receptor may play an important role in this (Bostanciklioglu, 2020). Furthermore COVID-19 may induce potential pain sensation (Su et al., 2020). However, currently no obvious pathological evidence was found to support viral infection in nerve tissue, and only short-term effects of COVID-19 on nervous system were reported (Wu et al., 2020b). A potential “three-steps” Neuro-COVID infection model (neuroinvasion, clearance and immune response) was also proposed (Panciani et al., 2020).
From a neurological point of view, the hypercoagulation and aneurysm instability partially due to systemic COVID-19 inflammation might induce severe brain hemorrhage, with a case with concomitant subarachnoid hemorrhage and COVID-19 reported (Muhammad et al., 2020), and the physicians and medical staff should pay attention to potential risk of thromboembolic complications among COVID-19 patients (Mongan et al., 2020). The COVID-19 patients could present with cerebrovascular accidents to minimize their mortality and morbidity; therefore, timely assessment and hyperacute treatment should be performed (Avula et al., 2020).
6. Massive inflammation and related neuropsychiatric manifestations
Almost all individuals with COVID-19 present with lung involvement; the clinical immune responses of COVID-19 are similar to SARS-CoV and MERS-CoV. Higher levels of inflammatory markers were found in blood, and the serum levels of several inflammatory cytokines are positively associated with disease severity; moreover, the severe COVID-19 cases are more likely to have hyperinflammation and/or cytokine storm (Chen et al., 2020b, Zhou et al., 2020). COVID-19 affects central and/or peripheral nervous system both directly and indirectly (Jasti et al., 2020). Early studies from Wuhan showed neutrophilia, lymphopenia, and increased systemic inflammatory proteins such as Interleukin 6 and C-Reactive protein are associated with severe COVID-19 infection and unfavorable outcomes (Chen et al., 2020c). COVID-19 directly binds to ACE2 and induced anosmia, ageusia, and central respiratory failure. Through the massive inflammation, The COVID-19 indirectly induced stroke, toxic-metabolic encephalopathy, acute inflammatory demyelinating polyneuropathy/Guillain Barre syndrome, and other neuropsychiatric manifestations, such as psychosis, insomnia, and mood changes (Oxley et al., 2020, Xiang et al., 2020, Zhao et al., 2020).
7. Treatment and prevention
The Special Issue described potential therapeutic interventions for COVID-19, including supportive intervention, immunomodulatory agents, antiviral therapy, and convalescent plasma transfusion (Chen et al., 2020d, Zhang et al., 2020d). Immunomodulatory medications for rheumatoid arthritis and other targets, such as CCL2, CCR5 or EGFR inhibitors, may have the potential to treat severe COVID-19 patients (Ray et al., 2020). Immunoglobulin A vaccination inducing a local protective immunity within the mucosa where pathogenic infection is initiated may have potential benefit (Chao et al., 2020). Cannabinoids was found as a plausible option to be added as an adjunct on COVID-19 patients with lung inflammation (Byrareddy and Mohan, 2020). Supportive intervention such as Ayurveda could positively influence immunity (Golechha, 2020, Rajkumar, 2020); recognizing the uniqueness of each individual would also help them adapt and promote mental health (Zhai and Du, 2020). Moreover, Qiu et al., summarized the recent systemic supportive interventions to maintain mental wellness in public population, isolated patients, and frontline medical staff (Qiu et al., 2020).
The internet media such as Facebook, Google, and Twitter have been growing rapidly in the past decade and have become relevant to potential disease prevention. Google related methods were performed to investigate the population interest and the COVID-19 disease spreading, suggesting the importance of public awareness of “hand washing”, “COVID-19 symptoms”, “social distancing” and “lock down” and medical therapeutic direction (Lin et al., 2020, Springer et al., 2020a, Springer et al., 2020b). More online information seeking was related to insomnia, rather than depression and suicide (Misiak et al., 2020). In Twitter, Bhat et al., performed sentiment analysis, and found that even though users are quarantined, yet they are hopeful (Bhat et al., 2020).
An unhealthy lifestyle was identified as a risk factor for COVID-19 hospitalization, suggesting that adopting simple lifestyle changes can have potential benefit (Hamer et al., 2020); physical activity could also help maintain emotional stability, counteract the negative effects of isolation, and improve immune competency (Simpson and Katsanis, 2020). Healthy foods and eating habits might have the potential to reduce susceptibility to severe complications (Butler and Barrientos, 2020). Specific nutritional interventions (e.g. omega-3 polyunsaturated fatty acids) have immunomodulation effects and may potentially improve the immunity to counteract both physical and mental impact of COVID-19 (Chang et al., 2020). In addition, Tan et al., found that the psychoneuroimmunity prevention measures in China had the potential to maintain the low prevalence of psychiatric symptoms among the workforce who returned to work (Tan et al., 2020).
The history of face mask and its related information was reviewed (Goh et al., 2020); face mask restrictions have the potential to protect against the COVID-19 and increase the level of perceived self-protection, as well as the level of social solidarity, improving mental health wellbeing (Szczesniak et al., 2020).
8. Conclusion
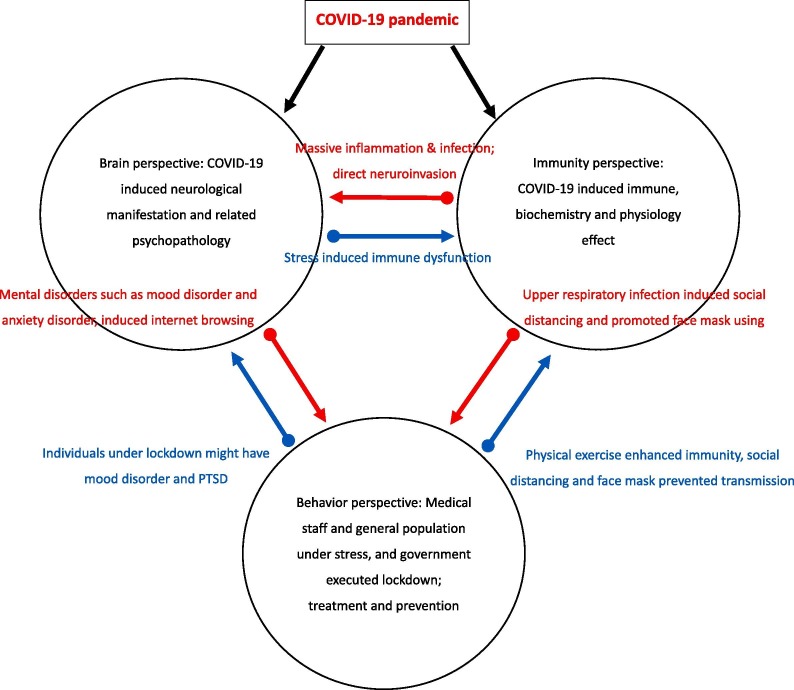
We linked the psychoneuroimmunity model to the three frontlines: Brain, Behavior, and Immunity, and described the detail below. Brain involves both psychology and neurology. The medical staff, as well as the general population, felt anxious and low mood under the stress of COVID-19. The direct neuroinvasion of COVID-19 induced headache, sleep disorder, olfactory and gustatory impairments, and more severe encephalopathy. In addition to neuroinvasion, the COVID-19 infection triggered the immunity, causing massive inflammation of lung and brain; the former is the main death cause of COVID-19 and the latter can induce brain hemorrhage. The hypercoagulation and aneurysm instability partially due to systemic COVID-19 inflammation might be the potential cause of mental illnesses. During the COVID-19 pandemic, the individuals performed specific behavioral patterns to relieve stress and anxiety; they were more likely to browse internet to seek health information such as face mask and hand washing. Healthy lifestyle and psychological intervention were recommended to boost the immune system against COVID-19. Furthermore, the government locked down the cities. Though lockdown seems to be positive against COVID-19, it had a deep impact on both the general populations’ social interaction and psychological wellbeing. The connection between Brain, Behavior, and Immunity showed in Fig. 1 .
Fig. 1.
The connection between the psychoneuroimmunity model and the three frontlines: Brain, Behavior, and Immunity.
COVID-19 therapy involves prevention, symptomatic treatments, and supportive care. Besides the targeted vaccinations that have been made available just recently, a healthy lifestyle and psychological interventions have the potential to improve psychoneuroimmunity. Although social distancing or wearing masks might help us to prevent infection, quality interpersonal connection should be fostered not only among the medical staff but also the general population, to improve the psychological wellbeing and also to enhance psychoneuroimmunity against COVID-19.
Acknowledgement
The authors of this work were supported by the following grants: MOST 106-2314-B-039-027-MY3, 108-2320-B-039-048, 108-2813-C-039-133-B, 108-2314-B-039-016, 109-2320-B-038-057-MY3, 109-2320-B-039-066, and 110-2321-B-006-004 from the Ministry of Science and Technology, Taiwan; ANHRF109-31 from An Nan Hospital, China Medical University, Tainan, Taiwan; CMRC-CMA-3 from Higher Education Sprout Project by the Ministry of Education (MOE), Taiwan; CMU108-SR-106 from the China Medical University, Taichung, Taiwan; and CMU104-S-16-01, CMU103-BC-4-1, CRS-108-048, DMR-108-216, DMR-109-102, DMR-109-244, DMR-HHC-109-11 and DMR-HCC-109-12 from the China Medical University Hospital, Taichung, Taiwan. Prof Pariante is funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. Prof Pariante has received research funding from Johnson & Johnson as part of a research program on depression and inflammation, and from the Medical Research Council (UK) and the Wellcome Trust for research on depression and inflammation as part of two large consortia that also include Johnson & Johnson, GSK and Lundbeck; however, the present paper is independent from this funding.
References
- Ajilore O., Thames A.D. The fire this time: the stress of racism, inflammation and COVID-19. Brain Behav. Immun. 2020;88:66–67. doi: 10.1016/j.bbi.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avula A., Nalleballe K., Narula N., Sapozhnikov S., Dandu V., Toom S., Glaser A., Elsayegh D. COVID-19 presenting as stroke. Brain Behav. Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batty G.D., Deary I.J., Luciano M., Altschul D.M., Kivimäki M., Gale C.R. Psychosocial factors and hospitalisations for COVID-19: Prospective cohort study based on a community sample. Brain Behav. Immun. 2020;89:569–578. doi: 10.1016/j.bbi.2020.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat M., Qadri M., Beg N.U., Kundroo M., Ahanger N., Agarwal B. Sentiment analysis of social media response on the Covid19 outbreak. Brain Behav. Immun. 2020;87:136–137. doi: 10.1016/j.bbi.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bongetta D., Calloni T., Colombo E.V., Versace A., Assietti R. Do matrix metalloproteases mediate the SARS-CoV-2-related damage to the central nervous system? Brain Behav. Immun. 2020;88:35. doi: 10.1016/j.bbi.2020.05.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostanciklioglu M. SARS-CoV2 entry and spread in the lymphatic drainage system of the brain. Brain Behav. Immun. 2020;87:122–123. doi: 10.1016/j.bbi.2020.04.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryche B., St Albin A., Murri S., Lacôte S., Pulido C., Ar Gouilh M., Lesellier S., Servat A., Wasniewski M., Picard-Meyer E., Monchatre-Leroy E., Volmer R., Rampin O., Le Goffic R., Marianneau P., Meunier N. Massive transient damage of the olfactory epithelium associated with infection of sustentacular cells by SARS-CoV-2 in golden Syrian hamsters. Brain Behav. Immun. 2020;89:579–586. doi: 10.1016/j.bbi.2020.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M.J., Barrientos R.M. The impact of nutrition on COVID-19 susceptibility and long-term consequences. Brain Behav. Immun. 2020;87:53–54. doi: 10.1016/j.bbi.2020.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrareddy S.N., Mohan M. SARS-CoV2 induced respiratory distress: can cannabinoids be added to anti-viral therapies to reduce lung inflammation? Brain Behav. Immun. 2020;87:120–121. doi: 10.1016/j.bbi.2020.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang J.-P.-C., Pariante C.M., Su K.-P. Omega-3 fatty acids in the psychological and physiological resilience against COVID-19. Prostaglandins Leukot. Essent. Fatty Acids. 2020;161 doi: 10.1016/j.plefa.2020.102177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chao Y.X., Rotzschke O., Tan E.K. The role of IgA in COVID-19. Brain Behav. Immun. 2020;87:182–183. doi: 10.1016/j.bbi.2020.05.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen F., Zheng D., Liu J., Gong Y., Guan Z., Lou D. Depression and anxiety among adolescents during COVID-19: a cross-sectional study. Brain Behav. Immun. 2020;88:36–38. doi: 10.1016/j.bbi.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen G., Wu D., Guo W., Cao Y., Huang D., Wang H., Wang T., Zhang X., Chen H., Yu H. Clinical and immunological features of severe and moderate coronavirus disease 2019. J. Clin. Investig. 2020;130(5) doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J., Yu T., Zhang X., Zhang L.i. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S.-J., Wang S.-C., Chen Y.-C. Novel antiviral strategies in the treatment of COVID-19: a review. Microorganisms. 2020;8(9):1259. doi: 10.3390/microorganisms8091259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coen M., Jeanson G., Culebras Almeida L.A., Hubers A., Stierlin F., Najjar I., Ongaro M., Moulin K., Makrygianni M., Leemann B., Kronig I., Bertrand J., Reny J.L., Schibler M., Serratrice J. Guillain-Barre syndrome as a complication of SARS-CoV-2 infection. Brain Behav. Immun. 2020;87:111–112. doi: 10.1016/j.bbi.2020.04.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Santis G. SARS-CoV-2: A new virus but a familiar inflammation brain pattern. Brain Behav. Immun. 2020;87:95–96. doi: 10.1016/j.bbi.2020.04.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong L., Xu P., Liu A. Meningoencephalitis without respiratory failure in a young female patient with COVID-19 infection in Downtown Los Angeles, early April 2020. Brain Behav. Immun. 2020;87:33. doi: 10.1016/j.bbi.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito G., Pesce M., Seguella L., Sanseverino W., Lu J., Sarnelli G. Can the enteric nervous system be an alternative entrance door in SARS-CoV2 neuroinvasion? Brain, Beh., Immu. 2020;87:93–94. doi: 10.1016/j.bbi.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang X., Zhang J., Teng C., Zhao K., Su K.-P., Wang Z., Tang W., Zhang C. Depressive symptoms in the front-line non-medical workers during the COVID-19 outbreak in Wuhan. J. Affect. Disord. 2020;276:441–445. doi: 10.1016/j.jad.2020.06.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank A., Fatke B., Frank W., Forstl H., Holzle P. Depression, dependence and prices of the COVID-19-Crisis. Brain Behav. Immun. 2020;87:99. doi: 10.1016/j.bbi.2020.04.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaffari M.E., Mortezapour A., Heidarimoghadam R. Letter to Editor: Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020;87:25–26. doi: 10.1016/j.bbi.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goh Y., Tan B.Y.Q., Bhartendu C., Ong J.J.Y., Sharma V.K. The face mask: How a real protection becomes a psychological symbol during Covid-19? Brain Behav. Immun. 2020;88:1–5. doi: 10.1016/j.bbi.2020.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golechha M. Time to realise the true potential of Ayurveda against COVID-19. Brain Behav. Immun. 2020;87:130–131. doi: 10.1016/j.bbi.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Sanguino C., Ausin B., Castellanos M.A., Saiz J., Lopez-Gomez A., Ugidos C., Munoz M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Q., Zheng Y., Shi J., Wang J., Li G., Li C., Fromson J.A., Xu Y., Liu X., Xu H., Zhang T., Lu Y., Chen X., Hu H., Tang Y., Yang S., Zhou H., Wang X., Chen H., Wang Z., Yang Z. Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: a mixed-method study. Brain Behav. Immun. 2020;88:17–27. doi: 10.1016/j.bbi.2020.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A., Paliwal V.K., Garg R.K. Is COVID-19-related Guillain-Barre syndrome different? Brain Behav. Immun. 2020;87:177–178. doi: 10.1016/j.bbi.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamer M., Kivimaki M., Gale C.R., Batty G.D. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: a community-based cohort study of 387,109 adults in UK. Brain Behav. Immun. 2020;87:184–187. doi: 10.1016/j.bbi.2020.05.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn S.R., Weston S.J., Fisher P.A. Identifying causal role of COVID-19 in immunopsychiatry models. Brain Behav. Immun. 2020;88:6–8. doi: 10.1016/j.bbi.2020.05.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosseini A.A., Shetty A.K., Sprigg N., Auer D.P., Constantinescu C.S. Delirium as a presenting feature in COVID-19: Neuroinvasive infection or autoimmune encephalopathy? Brain Behav. Immun. 2020;88:68–70. doi: 10.1016/j.bbi.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y.H., Jiang D., Huang J.T. SARS-CoV-2 detected in cerebrospinal fluid by PCR in a Case of COVID-19 encephalitis. Brain Behav. Immun. 2020;87:149. doi: 10.1016/j.bbi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahanshahi A.A., Dinani M.M., Madavani A.N., Li J., Zhang S.X. The distress of Iranian adults during the Covid-19 pandemic - More distressed than the Chinese and with different predictors. Brain Behav. Immun. 2020;87:124–125. doi: 10.1016/j.bbi.2020.04.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jasti M., Nalleballe K., Dandu V., Onteddu S. A review of pathophysiology and neuropsychiatric manifestations of COVID-19. J. Neurol. 2020;1 doi: 10.1007/s00415-020-09950-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joob B., Wiwanitkit V. Traumatization in medical staff helping with COVID-19 control. Brain Behav. Immun.. 2020;87:10. doi: 10.1016/j.bbi.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kajani R., Apramian A., Vega A., Ubhayakar N., Xu P., Liu A. Neuroleptic malignant syndrome in a COVID-19 patient. Brain Behav. Immun. 2020;88:28–29. doi: 10.1016/j.bbi.2020.05.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., Yao L., Bai H., Cai Z., Xiang Yang B., Hu S., Zhang K., Wang G., Ma C., Liu Z. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S.W., Su K.P. Using psychoneuroimmunity against COVID-19. Brain Behav. Immun. 2020;87:4–5. doi: 10.1016/j.bbi.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinoshita S., Cortright K., Crawford A., Mizuno Y., Yoshida K., Hilty D., Guinart D., Torous J., Correll C.U., Castle D.J. Changes in telepsychiatry regulations during the COVID-19 pandemic: 17 countries and regions’ approaches to an evolving healthcare landscape. Psychol. Med. 2020:1–33. doi: 10.1017/S0033291720004584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko N.Y., Lu W.H., Chen Y.L., Li D.J., Wang P.W., Hsu S.T., Chen C.C., Lin Y.H., Chang Y.P., Yen C.F. COVID-19-related information sources and psychological well-being: an online survey study in Taiwan. Brain Behav. Immun. 2020;87:153–154. doi: 10.1016/j.bbi.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krajewski P.K., Szepietowski J.C., Maj J. Cutaneous hyperesthesia: a novel manifestation of COVID-19. Brain Behav. Immun. 2020;87:188. doi: 10.1016/j.bbi.2020.05.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassale C., Gaye B., Hamer M., Gale C.R., Batty G.D. Ethnic disparities in hospitalisation for COVID-19 in England: The role of socioeconomic factors, mental health, and inflammatory and pro-inflammatory factors in a community-based cohort study. Brain Behav. Immun. 2020;88:44–49. doi: 10.1016/j.bbi.2020.05.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. How much “Thinking” about COVID-19 is clinically dysfunctional? Brain Behav. Immun. 2020;87:97–98. doi: 10.1016/j.bbi.2020.04.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Yu H., Bian G., Hu Z., Liu X., Zhou Q., Yu C., Wu X., Yuan T.F., Zhou D. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav. Immun. 2020;87:140–141. doi: 10.1016/j.bbi.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Liu C., Yang C. Vicarious traumatization: a psychological problem that cannot be ignored during the COVID-19 pandemic. Brain Behav. Immun. 2020;87:74. doi: 10.1016/j.bbi.2020.04.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liguori C., Pierantozzi M., Spanetta M., Sarmati L., Cesta N., Iannetta M., Ora J., Mina G.G., Puxeddu E., Balbi O., Pezzuto G., Magrini A., Rogliani P., Andreoni M., Mercuri N.B. Subjective neurological symptoms frequently occur in patients with SARS-CoV2 infection. Brain Behav. Immun. 2020;88:11–16. doi: 10.1016/j.bbi.2020.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Y.H., Liu C.H., Chiu Y.C. Google searches for the keywords of “wash hands” predict the speed of national spread of COVID-19 outbreak among 21 countries. Brain Behav. Immun. 2020;87:30–32. doi: 10.1016/j.bbi.2020.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Li X., Chen Q., Li Y., Xie C., Ye M., Huang J. Illness perception, mood state and disease-related knowledge level of COVID-19 family clusters, Hunan, China. Brain Behav. Immun. 2020;88:30–31. doi: 10.1016/j.bbi.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu T., Zheng Z., Sha X., Liu H., Zheng W., Su H., Xu G., Su K.-P., So K.-F., Lin K. Psychological impact in non-infectious disease specialists who had direct contact with patients with COVID-19. BJPsych open. 2020;7(1) doi: 10.1192/bjo.2020.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty? – the forthcoming economic challenges for a developing country. Brain Behav. Immun. 2020;87:163–166. doi: 10.1016/j.bbi.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marko C., Kosec A., Brecic P. Stay home while going out - Possible impacts of earthquake co-occurring with COVID-19 pandemic on mental health and vice versa. Brain Behav. Immun. 2020;87:82–83. doi: 10.1016/j.bbi.2020.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meda N., Slongo I. Caution when linking COVID-19 to mental health consequences. Brain Behav. Immun. 2020;87:152. doi: 10.1016/j.bbi.2020.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrsafar A.H., Gazerani P., Moghadam Zadeh A., Jaenes Sanchez J.C. Addressing potential impact of COVID-19 pandemic on physical and mental health of elite athletes. Brain Behav. Immun. 2020;87:147–148. doi: 10.1016/j.bbi.2020.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milman E., Lee S.A., Neimeyer R.A. Social isolation as a means of reducing dysfunctional coronavirus anxiety and increasing psychoneuroimmunity. Brain Behav. Immun. 2020;87:138–139. doi: 10.1016/j.bbi.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misiak B., Szcześniak D., Koczanowicz L., Rymaszewska J. The COVID-19 outbreak and Google searches: Is it really the time to worry about global mental health? Brain Behav. Immun. 2020;87:126–127. doi: 10.1016/j.bbi.2020.04.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mongan D., Cannon M., Cotter D.R. COVID-19, hypercoagulation and what it could mean for patients with psychotic disorders. Brain Behav. Immun. 2020;88:9–10. doi: 10.1016/j.bbi.2020.05.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav. Immun. 2020;87:23–24. doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhammad S., Petridis A., Cornelius J.F., Hanggi D. Letter to editor: Severe brain haemorrhage and concomitant COVID-19 Infection: a neurovascular complication of COVID-19. Brain Behav. Immun. 2020;87:150–151. doi: 10.1016/j.bbi.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhtar S. Mental health and emotional impact of COVID-19: Applying Health Belief Model for medical staff to general public of Pakistan. Brain Behav. Immun. 2020;87:28–29. doi: 10.1016/j.bbi.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nalleballe K., Reddy Onteddu S., Sharma R., Dandu V., Brown A., Jasti M., Yadala S., Veerapaneni K., Siddamreddy S., Avula A., Kapoor N., Mudassar K., Kovvuru S. Spectrum of neuropsychiatric manifestations in COVID-19. Brain Behav. Immun. 2020;88:71–74. doi: 10.1016/j.bbi.2020.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., De Leacy R.A., Shigematsu T., Ladner T.R., Yaeger K.A. Large-vessel stroke as a presenting feature of Covid-19 in the young. N. Engl. J. Med. 2020;382(20) doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panariello A., Bassetti R., Radice A., Rossotti R., Puoti M., Corradin M., Moreno M., Percudani M. Anti-NMDA receptor encephalitis in a psychiatric Covid-19 patient: a case report. Brain Behav. Immun. 2020;87:179–181. doi: 10.1016/j.bbi.2020.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panciani P.P., Saraceno G., Zanin L., Renisi G., Signorini L., Battaglia L., Fontanella M.M. SARS-CoV-2: “Three-steps” infection model and CSF diagnostic implication. Brain Behav. Immun. 2020;87:128–129. doi: 10.1016/j.bbi.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J.Y., Zhou D.S., Liu J., Yuan T.F. Mental wellness system for COVID-19. Brain Behav. Immun. 2020;87:51–52. doi: 10.1016/j.bbi.2020.04.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. Ayurveda and COVID-19: Where psychoneuroimmunology and the meaning response meet. Brain Behav. Immun. 2020;87:8–9. doi: 10.1016/j.bbi.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ransing R., Ramalho R., Orsolini L., Adiukwu F., Gonzalez-Diaz J.M., Larnaout A., Pinto da Costa M., Grandinetti P., Bytyçi D.G., Shalbafan M., Patil I., Nofal M., Pereira-Sanchez V., Kilic O. Can COVID-19 related mental health issues be measured? Brain Behav. Immun. 2020;88:32–34. doi: 10.1016/j.bbi.2020.05.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ray P.R., Wangzhou A., Ghneim N., Yousuf M.S., Paige C., Tavares-Ferreira D., Mwirigi J.M., Shiers S., Sankaranarayanan I., McFarland A.J., Neerukonda S.V., Davidson S., Dussor G., Burton M.D., Price T.J. A pharmacological interactome between COVID-19 patient samples and human sensory neurons reveals potential drivers of neurogenic pulmonary dysfunction. Brain Behav. Immun. 2020;89:559–568. doi: 10.1016/j.bbi.2020.05.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren Y., Zhou Y., Qian W., Li Z., Liu Z., Wang R., Qi L., Yang J., Song X., Zeng L., Zhang X. Letter to the Editor “a longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 2020;87:132–133. doi: 10.1016/j.bbi.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson R.J., Katsanis E. The immunological case for staying active during the COVID-19 pandemic. Brain Behav. Immun. 2020;87:6–7. doi: 10.1016/j.bbi.2020.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sominsky L., Walker D.W., Spencer S.J. One size does not fit all – patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity of disease matters. Brain Behav. Immun. 2020;87:1–3. doi: 10.1016/j.bbi.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer S., Menzel L.M., Zieger M. Google Trends provides a tool to monitor population concerns and information needs during COVID-19 pandemic. Brain Behav. Immun. 2020;87:109–110. doi: 10.1016/j.bbi.2020.04.073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Springer S., Menzel L.M., Zieger M. Google Trends reveals: focus of interest in the population is on treatment options rather than theories about COVID-19 animal origin. Brain Behav. Immun. 2020;87:134–135. doi: 10.1016/j.bbi.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su S., Cui H., Wang T., Shen X., Ma C. Pain: a potential new label of COVID-19. Brain Behav. Immun. 2020;87:159–160. doi: 10.1016/j.bbi.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun T., Guan J., You C. The neuroinvasive potential of severe acute respiratory syndrome coronavirus 2. Brain Behav. Immun. 2020;88:59. doi: 10.1016/j.bbi.2020.05.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szczesniak D., Ciulkowicz M., Maciaszek J., Misiak B., Luc D., Wieczorek T., Witecka K.F., Rymaszewska J. Psychopathological responses and face mask restrictions during the COVID-19 outbreak: results from a nationwide survey. Brain Behav. Immun. 2020;87:161–162. doi: 10.1016/j.bbi.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Zhang Z., Lai A., Ho R., Tran B., Ho C., Tam W. Is returning to work during the COVID-19 pandemic stressful? a study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020;87:34–39. doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavougios G.D. Host proteases as determinants of coronaviral neurotropism and virulence. Brain Behav. Immun. 2020;87:27. doi: 10.1016/j.bbi.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavougios G.D. Potentially irreversible olfactory and gustatory impairments in COVID-19: Indolent vs. fulminant SARS-CoV-2 neuroinfection. Brain Behav. Immun. 2020;87:107–108. doi: 10.1016/j.bbi.2020.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Xu X., Yang L., Liu C., Yang C. Nervous system damage after COVID-19 infection: presence or absence? Brain Behav. Immun. 2020;87:55. doi: 10.1016/j.bbi.2020.04.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang Y.-T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Tong J., Meng F., Feng Q., Ma H., Shi C., Yuan J., Yang S., Liu L., Xu L., Xi Y., Li W., Rohlof H., Zhao X., Kang C. Characteristics and challenges of psychological first aid in China during the COVID-19 outbreak. Brain Behav. Immun. 2020;87:113–114. doi: 10.1016/j.bbi.2020.04.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H. The more exposure to media information about COVID-19, the more distressed you will feel. Brain Behav. Immun. 2020;87:167–169. doi: 10.1016/j.bbi.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan B., Li W., Liu H., Cai X., Song S., Zhao J., Hu X., Li Z., Chen Y., Zhang K., Liu Z., Peng J., Wang C., Wang J., An Y. Correlation between immune response and self-reported depression during convalescence from COVID-19. Brain Behav. Immun. 2020;88:39–43. doi: 10.1016/j.bbi.2020.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhai Y., Du X. Loss and grief amidst COVID-19: a path to adaptation and resilience. Brain Behav. Immun. 2020;87:80–81. doi: 10.1016/j.bbi.2020.04.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Lu H., Zeng H., Zhang S., Du Q., Jiang T., Du B. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav. Immun. 2020;87:49–50. doi: 10.1016/j.bbi.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Xie B., Hashimoto K. Current status of potential therapeutic candidates for the COVID-19 crisis. Brain Behav. Immun. 2020;87:59–73. doi: 10.1016/j.bbi.2020.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J., Xu D., Xie B., Zhang Y., Huang H., Liu H., Chen H., Sun Y., Shang Y., Hashimoto K., Yuan S. Poor-sleep is associated with slow recovery from lymphopenia and an increased need for ICU care in hospitalized patients with COVID-19: a retrospective cohort study. Brain Behav. Immun. 2020;88:50–58. doi: 10.1016/j.bbi.2020.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S.X., Liu J., Afshar Jahanshahi A., Nawaser K., Yousefi A., Li J., Sun S. At the height of the storm: healthcare staff's health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav. Immun. 2020;87:144–146. doi: 10.1016/j.bbi.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao H., Shen D., Zhou H., Liu J., Chen S. Guillain-Barré syndrome associated with SARS-CoV-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y.i., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S., Wu Y., Zhu C.Y., Hong W.C., Yu Z.X., Chen Z.K., Chen Z.L., Jiang D.G., Wang Y.G. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav. Immun. 2020;87:56–58. doi: 10.1016/j.bbi.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y.a., Wang C., Dong L.i., Xiao M. Home quarantine or centralized quarantine, which is more conducive to fighting COVID-19 pandemic? Brain Behav. Immun. 2020;87:142–143. doi: 10.1016/j.bbi.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]