Abstract
Since the emergence of the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection in December 2019, it has rapidly spread across many countries and it has become a crucial global health concern. Furthermore, SARS-CoV-2 infection not only effect on respiratory system, but on reproductive system of human. However, there has been not any review described the transmission paths and effects of SARS-CoV-2 infection on human reproductive system, systematically. In order to describe the transmission paths of SARS-CoV-2, effect on the male/female reproductive system of SARS-CoV-2 and some successful prevention measures. We would like to review effect of SARS-CoV-2 on reproductive system. To conclude, SARS-CoV-2 infection might damage to male reproductive system via ACE2 receptor mediating and male patients were reportedly slightly more affected than women by SARS-CoV-2 infections.
Keywords: The 2019 novel coronavirus (2019-nCoV), Coronavirus disease 2019 (COVID-19), Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), Transmission, Reproductive system
1. Introduction
Since the emergence of the 2019 novel coronavirus (2019-nCoV) infection in December 2019, it has rapidly spread across many countries say, United Nations, Japan, P.R. China, etc. As of 13 December 2020, the number of 2019-nCoV cases and deaths continued to rise with 70 million cumulative cases and 1.6 million deaths globally (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c, Holshue et al., 2020, Illiano et al., 2020, National Health Commission of the People's Republic of China, 2020, Reusken et al., 2020, Tauseef et al., 2020, Wold Health Organization, 2020) (Fig. 1 ). 2019-nCoV has become a crucial global health concern (Li et al., 2020a, Li et al., 2020b, Li et al., 2020c). Initially, the World Health Organization (WHO) have been confirmed that full genome sequence data from the 2019-nCoV viruses have been shared officially with WHO in January 17, 2020 (Ceraolo and Giorgi, 2020, Dong et al., 2020a, Dong et al., 2020b, Paraskevis et al., 2020). After that, WHO announced a new name for the epidemic disease caused by 2019-nCoV: coronavirus disease (COVID-19), in 11 February 2020. Then the International Committee on Taxonomy of Viruses has renamed the 2019-nCoV as severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (Feng et al., 2020, Li et al., 2020a, Li et al., 2020b, Li et al., 2020c). In 11 March 2020; WHO announced SARS-CoV-2 as a pandemic (Muralidar et al., 2020). Additionally, several studies have revealed that SARS-CoV-2 infection not only damage to respiratory system, but other organs of human, such as heart, liver, oesophagus, kidney, bladder and ileum, and specific cell types such as type II alveolar cells, myocardial cells, proximal tubule cells of kidney, ileum and oesophagus epithelial cells, and bladder urothelial cells (Chai et al., 2020, Liang et al., 2020, Zhang et al., 2020). Furtherly, Wang’s results indicated that the virus and anti-viral drugs with certain renal toxicity could result in the kidney damage and potential pathogenicity to testicular tissues (Fan et al., 2020). Even more, an astounding case reported that on February 6, 2020, a neonate born to a pregnant woman with SARS-CoV-2 neumonia tested positive for SARS-CoV-2 infection 36 h after birth (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c). However, there has been not any review described the transmission paths and effects of SARS-CoV-2 infection on human reproductive system, systematically. In this study, we will discuss the potential transmission paths of SARS-CoV-2 infection on human reproductive system, then we will further describe effect on the male/female reproductive system of SARS-CoV-2 and some successful prevention measures.
Fig. 1.
The data on SARS-Cov-2 on 13 December 2020. (A) SARS-Cov-2 cases per 1 million population reported in the last seven days by countries, territories and areas, 7 December through 13 December 2020. (B) SARS-Cov-2 cases reported weekly by WHO Region, and global deaths, as of 13 December 2020. (Wold Health Organization, 2020).
2. The potential transmission paths of SARS-CoV-2 infection on human reproductive system
Above all, as of February 7, 2020, 44 strains of SARS-CoV-2 have been sequenced and uploaded to GenBank (Flynn et al., 2020, Luczak-Roesch, 2020). Detailed genomic and structure-based analysis of SARS-CoV-2, suggested that the novel virus is a new type of bat coronavirus and it is genetically distant from the human severe acute respiratory syndrome coronavirus (SARS-CoV) or Middle East Respiratory Syndrome coronavirus (MERS-CoV) (Benvenuto et al., 2020, Ceraolo and Giorgi, 2020). These three viruses belong to the genus Betacoronavirus of subfamily Coronavirinae of the family Coronaviridae of the order Neovirales (Rastogi et al., 2020). Then, through analyzing among the genetic distances from the SARS-CoV-2 strain to the coronaviruses residing in animal hosts, the genomic and protein data, researches established that the host identification found the most possible transmission chain was from bats to pangolins to humans (Benvenuto et al., 2020, Ji et al., 2020, Zhou et al., 2020). The most importantly, as we known, profiling the genetic evolution and dynamic spreading of SARS-CoV-2 was crucial, and some reports have suggested that SARS-CoV-2 with single stranded RNA genome were tend to evolve by accumulation of mutations, which could lead to fast transmission among hosts and cross species (Benvenuto et al., 2020, Kumar et al., 2020, Tang et al., 2020).
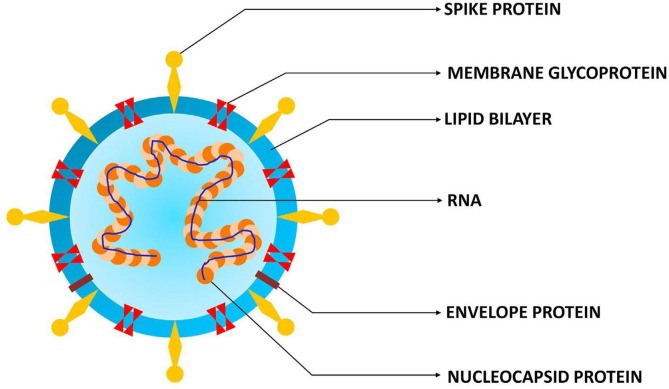
It was widely accepted that coronavirus human transmission is driven by the interactions of its spike protein (S protein) with human receptor on host cell surface (Tian et al., 2020). In detail, a coronavirus contains four structural proteins, including spike (S), envelope (E), membrane (M), and nucleocapsid (N) proteins (Dong et al., 2020a, Dong et al., 2020b) (Fig. 2 ). Among them, S protein plays the most important roles in viral attachment, fusion and entry, and it serves as a target for development of antibodies, entry inhibitors and vaccines (Rastogi et al., 2020). However, several researches have indicated that SARS-CoV and MERS-CoV RBDs recognize different receptors. SARS-CoV recognizes angiotensin-converting enzyme 2 (ACE2) as its receptor, whereas MERS-CoV recognizes dipeptidyl peptidase 4 (DPP4) as its receptor (Letko and Munster, 2020). It has detected that SARS-CoV receptor-binding domain (RBD) contains a core structure and a receptor-binding motif (RBM), and in the case of SARS-CoV, some of its critical RBM residues were adapted to human ACE2 (Ding et al., 2004, Letko and Munster, 2020). Similar to SARS-CoV, SARS-CoV-2 also recognizes ACE2 as its host receptor binding to viral S protein (Letko and Munster, 2020, Zhao et al., 2020). In order to reveal the potential cell receptor mediating mechanism of SARS-CoV-2, a number of researchers have been doing a lot of systematically studies (Beal et al., 2020, Dong et al., 2020a, Dong et al., 2020b, Zhao et al., 2020). Especially, the latest study reported by Balistreri and Simons, etc. demonstrated that Neuropilin-1 (NRP1) co-expression with ACE2 and transmembrane protease serine 2 (TMPRSS2) markedly enhanced SARS-CoV-2infection in HEK-293T cells (Cantuti-Castelvetri et al., 2020). It may be explained based on a broadly recognized hypothesis that the SARS-CoV-2 S protein mediates viral entry into host cells by first binding to a host receptor, through the sequence of SARS-CoV-2 RBD, including its RBM that directly contacts ACE2, in the S1, second, providing favorable interactions with human ACE2 through several critical residues in SARS-CoV-2 RBM, and then fusing the viral and host membranes through the S2 (Beal et al., 2020, Cantuti-Castelvetri et al., 2020, Dong et al., 2020a, Dong et al., 2020b, Drak Alsibai, 2020, Huang and Herrmann, 2020, Letko and Munster, 2020, Rastogi et al., 2020, Tai et al., 2020, Tian et al., 2020, Wan et al., 2020, Wang et al., 2020, Zhao et al., 2020, Zhou et al., 2020, Zhu et al., 2020). Meanwhile, the research of Cullen and Yamauchi, etc. suggested that there is the presence of a polybasic furin-type cleavage site, RRAR, at the S1/S2 boundary in the SARS-CoV-2 S protein but that is absent in SARS-CoV. The presence of the polybasic cleavage site in SARS-CoV-2 results in two protein units, S1 and S2, remain non-covalently associated with the serine protease TMPRSS2, further enhanced pathogenicity by priming the fusion activity of the S2 and could potentially create additional cell surface receptor binding sites (Daly et al., 2020). Proteolytic cleavage of RRAR by furin exposes a conserved carboxyterminal (C-terminal) motif RXXROH (where R is arginine and X is any amino acid; R can be substituted by lysine, K) termed the ‘C-end rule’ (CendR) in the S1 (Drak Alsibai, 2020). CendR peptides bind to NRP1 and NRP2, transmembrane receptors at the cell surface, which could regulate pleiotropic biological processes, including axon guidance, angiogenesis, and vascular permeability. NRP1 binding to the CendR peptide in the S1 is thus likely to play a role in the increased infectivity of SARS-CoV-2 compared with SARS-CoV (Daly et al., 2020). Several results have confirmed that NRP1 could represent such an ACE2 potentiating factor, however, it was also possible that SARS-CoV-2 can enter cells independently of ACE2 when viral loads were high. The reason why a number of viruses use NRPs as entry factors could be because of their high expression on epithelia facing the external environment, and their function in enabling cell, vascular, and tissue penetration. The ability to target this specific interaction may provide a route for COVID-19 therapies (Cantuti-Castelvetri et al., 2020, Esakandari et al., 2020, Harrison et al., 2020, Illiano et al., 2020, Li et al., 2020a, Li et al., 2020b, Li et al., 2020c, Yousefi et al., 2020) (Fig. 3 ).
Fig. 2.
The structure of SARS-CoV-2 (Muralidar et al., 2020).
Fig. 3.
Effects and mechanisms of SARS-CoV-2 infection in the male/female reproductive system. S1 and S2: S domain; PD: peptidase domain; RBD: receptor-binding domain. (Fan et al., 2020, Illiano et al., 2020, Khalili et al., 2020, Kumar et al., 2020, Rasmussen et al., 2020).
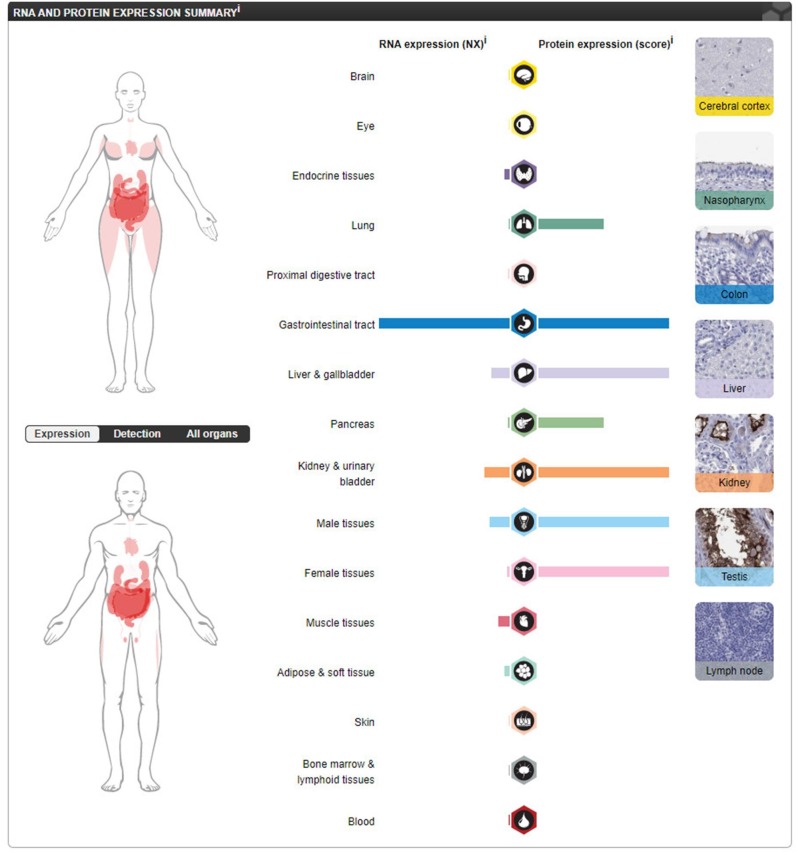
Several studies revealed that ACE2 not only expression profiled in respiratory system, concentrated in a small population of type II alveolar cells (AT2), but in another system and organ of human during the SARS-CoV-2 infection (Chai et al., 2020, Liang et al., 2020, Zhang et al., 2020). Says, the study of Meng, Zhou and Liu, etc., confirmed that ACE2 highly expressed in absorptive enterocytes such as ileum and colon. These results indicated that digestive system is a potential route for SARS-CoV-2 infection (Zhang et al., 2020). Meanwhile, Cai, Fan and Lan’s results indicated that virus could directly bind to ACE2 positive cholangiocytes but not necessarily hepatocytes. This finding suggested that the liver admages of SARS-CoV and SARS-CoV-2 patients may be result in cholangiocyte dysfunction and another causes like drug induced and systemic inflammatory response induced liver injury (Chai et al., 2020). Importantly, there are several studies confirmed that ACE2 expression profile both in male and female reproductive systems (Abhari and Kawwass, 2020, Fan et al., 2020, Verdecchia et al., 2020, Yan et al., 2020) (Fig. 4 ). Thus, we could infer that the potential transmission paths of SARS-CoV-2 infection on human reproductive system might be mediated via ACE2 receptor.
Fig. 4.
Data of ACE2 protein expression level in different human tissues from HPA portal. ACE2 protein expression level in different tissues (Fan et al., 2020).
3. Effect of SARS-CoV-2 on male reproductive system
3.1. Dose SARS-CoV-2 affect the male reproductive system
As mentioned above, ACE2 has recently been demonstrated as a receptor in SARS-CoV-2 infection. On the one hand, as a pivotal role in the cardiovascular system by generating the vasoconstrictor peptide angiotensin II (Ang II), the metallopeptidase angiotensin-converting enzyme (ACE) is a constitutive product of adult-type leydig cells and the expression of ACE2 by leydig cells suggests a regulatory role for the enzyme in steroidogenesis via limiting testosterone inhibition by Ang II (Batiha et al., 2020, Li et al., 2020a, Li et al., 2020b, Li et al., 2020c, Muñoz et al., 2014, Reis et al., 2010, Verdecchia et al., 2020, Zou et al., 2020). On the other hand, Reis’ study suggested that the testicular samples of infertile men with impaired spermatogenesis expressed ACE2 mRNA at lower concentrations than samples with full spermatogenesis (Reis et al., 2010). These results implied that ACE2 plays an important role in male reproductive system and SARS-CoV-2 infection might damage to male reproductive system via ACE2 receptor mediating.
3.2. Testicle
As we known, the spikes of SARS-CoV-2 infected the cell via interacted with ACE2 on the cell membrane (Hoffmann et al., 2020). Nevertheless, ACE2 not only expression in the lung, but extensively expresses in spermatogonia, sertoli and leydig cell in testicle (Fan et al., 2020, Groner et al., 2021, Vishvkarma and Rajender, 2020, Wang and Xu, 2020). Indeed, it has detected that testicle might be infected by SARS-CoV-2, which probably lead to further reproductive system diseases (Cheng et al., 2020, Fan et al., 2020, Fraietta et al., 2020, Guo et al., 2020, Hoffmann et al., 2020, Illiano et al., 2020, Verdecchia et al., 2020, Wang and Xu, 2020, Yang et al., 2020, Zou et al., 2020). Similarly, it was well known that viruses could enter the testicular cells and cause viral orchitis, and even could result in male infertility and testicular tumor (Illiano et al., 2020, Xu et al., 2006, Yang et al., 2020). Previous researches have also investigated that SARS-CoV damage to the testicle in SARS patients and risk to spermatogenesis (Xu et al., 2006). Meanwhile, the cases of secondary infection also provided that testicle might be the potential host for SARS-CoV-2. In detail, Wang’s study indicated that the results of using the online datasets to analyze ACE2 expression in different human organs suggested that ACE2 highly expresses in renal tubular cells, leydig cells, testicular cells and cells in seminiferous ducts in testicle (Fan et al., 2020). Then, Gene ontology analyses revealed that GO categories associated with SARS-CoV-2 reproduction and transmission were highly enriched in ACE2-positive spermatogonia but were down-regulated in male gamete generation related terms. Cell-cell junction and immunity related GO terms were increased but mitochondria and reproduction related GO terms were decreased in ACE2-positive leydig and sertoli cells. ACE2-positive cells possessed higher abundance of transcripts associated with SARS-CoV-2 reproduction and transmission and lower abundance of transcripts related with male gametogenesis. ACE2 expression in human testicle suggested that SARS-CoV-2 could infect the male gonad and risk male reproductive dysfunction (Wang and Xu, 2020). In summary, there were evidences that the testicle was susceptible to SARS-CoV-2 infection, and it was important to reveal the mechanism of SARS-CoV-2 infection in testicle.
Then, several articles have implied the possible mechanisms of SARS-CoV-2 infecting to testicle mediated by ACE2 reporter (Cardona Maya et al., 2020, Fan et al., 2020, Fraietta et al., 2020). On the one hand, studies suggested that the SARS-CoV-2 infection into cells was mediated by the binding of the S protein to the ACE2 receptors, as which a transmembrane type I glycoprotein uses a single extracellular catalytic domain to remove one single amino acid from the octapeptide angiotensin II to generate angiotensin 1–7 and converts angiotensin I into angiotensin 1–9. The first step that SARS-CoV-2 entry process is that the N-terminal portion of the protein unit S1 bind to the ACE2 peptidase domain (PD) through the RBD and facilitates viral attachment to the surface of target cells. The second step that the polybasic furin-type cleavage site promotes the protein cleavage between the S1 and S2 units by the TMPRSS2, a member of the Hepsin/TMPRSS subfamily and contiguous to ACE2 receptor, at the S1/S2 and the S2′ site and then the proteolytic cleavage of RRAR by furin exposes CendR in the S1, and CendR could bind to NRP1, an ACE2 potentiating factor, enhancing the mediating capacity of ACE2. It was the most crucial that the process driven by the S2 allows fusion of viral and cellular membranes with subsequent entry of the virus into cell and infection of other cells via replication releasing (Beal et al., 2020, Cantuti-Castelvetri et al., 2020, Daly et al., 2020, Dong et al., 2020a, Dong et al., 2020b, Drak Alsibai, 2020, Huang and Herrmann, 2020, Letko and Munster, 2020, Rastogi et al., 2020, Tai et al., 2020, Tian et al., 2020, Wan et al., 2020, Wang et al., 2020, Zhao et al., 2020, Zhou et al., 2020, Zhu et al., 2020) (Fig. 3). On the other hand, ACE2 is also a crucial component of the renin-angiotensin system (RAS). The classical RAS, ACE-Ang II-AT1R regulatory axis and the ACE2-Ang 1–7-MasR counter-regulatory axis, play an essential role in maintaining homeostasis in humans. In the COVID-19 infection process, ACE2 receptors are saturated by binding with the virus to giving rise to the increased availability of angiotensin II. However, this process could be blocked by the conversion of angiotensin II into angiotensin (1–7) via ACE2. Next, angiotensin (1–7) binds to the ART2 and MAS receptors, which in the testicles, specifically in leydig and sertoli cells (Douglas et al., 2004, Glowacka et al., 2011, Green et al., 2018, Grive et al., 2019, Guo et al., 2018, Guo et al., 2017, Lukassen et al., 2018, Muñoz et al., 2014, Omolaoye et al., 2020, Reis et al., 2010, Verdecchia et al., 2020) (Fig. 3).
3.3. Semen
Furthermore, it has been confirmed that SARS-CoV-2 could be spread by human-to-human transmission, mainly through respiratory droplets and contact (Mohseni et al., 2020). Several results suggested that the SARS-CoV-2 have been found in the semen and testicle in men infected by SARS-CoV-2 at both acute and recovery phases. Thus, it supported that the SARS-CoV-2 can be sexually transmitted by men (Karia et al., 2020, Karia and Nagraj, 2020). Due to the imperfect blood-testicle/deferens/epididymis barriers, SARS-CoV-2 might be seeded to the male reproductive tract, especially in the presence of systemic local inflammation (Kayaaslan et al., 2020, Khalili et al., 2020). Even more, the virus cannot replicate in the male reproductive system, it might persist and possibly resulting from the privileged immunity of testicle. Nevertheless, the presence of viruses in semen may be commonplace, and traditional non-sexually transmitted viruses might be assumed to be appear in genital secretions (Li et al., 2020a, Li et al., 2020b, Li et al., 2020c). These results suggested that SARS-CoV-2 was detected in the semen of recovering patients and sexual transmission might be a critical part of the prevention of transmission (Kayaaslan et al., 2020, Khalili et al., 2020, Li et al., 2020a, Li et al., 2020b, Li et al., 2020c). Indeed, abstinence or condom use might be considered as preventive for these patients. In conclusion, researchers found results that male patients were reportedly slightly more affected than women by both SARS-CoV and SARS-CoV-2 infections (Holtmann et al., 2020, Karia et al., 2020, Karia and Nagraj, 2020, Kayaaslan et al., 2020, Khalili et al., 2020, Li et al., 2020a, Li et al., 2020b, Li et al., 2020c, Ma et al., 2020, Paoli et al., 2020, Vishvkarma and Rajender, 2020).
4. Effect of SARS-CoV-2 on female reproductive system
4.1. Ovary
As we known, SARS-CoV-2 enter host cells via ACE2 receptors (Li et al., 2020a, Li et al., 2020b, Li et al., 2020c). Researches indicated that the expression of ACE2 mRNA transcripts was abundant in the ovaries of childbearing age and postmenopausal women (Yan et al., 2020). Therefore, it was implied that the female reproductive system may be at risk of SARS-CoV-2 infection. To confirm that several researchers used single cell sequencing to analyze the expression of ACE2, TMPRSS2, cathepsin B and L (CTSB and CTSL, respectively) in human ovarian cells and found that the expression of ACE2 was very low in stromal cells and perivascular cells of the ovarian cortex, TMPRSS2 was not expressed in different types of ovarian cells, CTSB and CTSL were expressed in all tested ovarian cell types. No co-expression of ACE2/CTSB or ACE2/CTSL was observed in all cell types of ovary. Because ACE2 needed the co-expression of protease TMPRSS2 or CTSB/L, which causes the S protein on its surface to enter the host cell. ACE2 was expressed in less than 5% of ciliated cells, secretory cells and leukocytes. On the contrary, the expression levels of protease TMPRSS2 and CTSL/B were different in different fallopian tube cells, and the expression of CTSL was not detected in any fallopian tube cells. No co-expression of ACE2, TMPRSS2 or CTSB was observed in any fallopian tube cells. The ciliated cells in the fallopian tube were essential for the lumen movement of oocytes and spermatozoa (Goad et al., 2020). These results showed that SARS-CoV-2 was unlikely to infect ovarian cells or affect oogenesis and early fertilization events (Goad et al., 2020, Segars et al., 2020).
4.2. Uterus
Above all, the ability of SARS-CoV-2 to damage tissue depended on its ability to enter and infect cells in the tissue (Bilal et al., 2020, Henarejos-Castillo et al., 2020). After getting the entry path of cells, SARS-CoV-2 would affect the renin-angiotensin system and down-regulate the expression of ACE2, and up-regulate the pro-inflammatory response through angiotensin Ⅱ (Chadchan et al., 2020). Recently, a novel entry path for SARS-CoV-2 into the cell has revealed, which is using Basigin (BSG), also known as CD147 or EMMPRIN, instead of ACE2 as the receptor. S protein of SARS-CoV-2 bind to ACE2 into the host cell, resulting in the fusion of the virus with the cell membrane and endocytosis. Transmembrane protease TMPRSS2 could cleave S protein. TMPRSS4 itself increases viral infectivity, at least in intestinal epithelial cells. The expression of CTSB and CTSL were observed in SARS-CoV-2-infected TMRPSS2-cell line, indicating that CTSB and CTSL have partial activity to cleave S protein. Furin is another protease that cleaves S protein, which exists in the epithelium of several oral mucosa tissues together with ACE2. MX dynamin-like GTPase1 (MX1) could regulate neutrophil infiltration and facilitate virus infection through S protein modification of neutrophil elastase. A study based on the human protein map (HPA) found that ACE transcripts were low in the endometrium and were not expressed in protein form. The expression of TMPRSS4 and furin RNA was also low and the protein level was moderate, while CTSB, MX1 and BSG had moderate RNA expression and high protein expression. However, several results indicated that TMPRSS4, CTSL, CTSB, furin, MX1 and BSG were highly expressed in the whole stages of endometrium, and proteases such as CTSL, CTSB, furin could be co-expressed with TMPRSS4, cutting S protein at different sites, thus increasing infectivity. The expression of ACE2 was low. TMPRSS4 was expressed in all menstrual cycles, especially during menstruation, which cleaves S protein and enables SARS-CoV-2 to bind to ACE2, to infect cells, even if the expression of ACE2 was low (Abhari and Kawwass, 2020, Henarejos-Castillo et al., 2020). Especially, Diaz-Gimeno’s study also found that from the proliferative phase to the middle secretory stage of the endometrium, especially in the early secretory stage, there was a positive correlation between age and ACE2, which mean that older women may be more likely to be infected with SARS-CoV-2 (Henarejos-Castillo et al., 2020) (Fig. 4).
Nevertheless, in myometrium, the expression of ACE2 was low in 1% of fibroblasts, but no expression of TMPRSS2 was observed in any cell type of normal myometrium. CTSB and CTSL may promote the entry of SARS-CoV-2 into cells without the participation of TMPRSS2. CTSB and CTSL were expressed in myeloid cells, endothelial cells, lymphoendothelial cells, T cells, NK cells and fibroblasts in the myometrium. However, no co-expression of CTSB or CTSL and ACE2 was found in these cells. These findings suggested that SARS-CoV-2 was less likely to infect smooth muscle cells in the myometrium, and SARS-CoV-2 infection was unlikely to cause myometrial inflammation and potential preterm delivery (Henarejos-Castillo et al., 2020).
4.3. Maternal-fetal transmission
The ways of SARS-CoV-2 transmission has been indicated as follows: 1, it can be transmitted through respiratory tract, 2, fecal-oral transmission and 3, pollutant transmission 4, inhalation of small aerosols diffused in the air. So far, there was no definite answer to whether SARS-CoV-2 can be transmitted vertically and the mechanism by which it occurs (Schwartz and Graham, 2020). Several studies have shown that 70 pregnant women with SARS-CoV-2 had symptoms including fever (84%), cough (28%) and dyspnea (18%). Obstetrical complications included preterm delivery (39%), intrauterine growth restriction abortion (10%) and abortion (2%). Amniotic fluid, umbilical cord blood, throat swabs and milk of newborns were collected from 9 pregnant women infected with SARS-CoV-2 in Wuhan. All results indicated that there was no direct evidence of vertical transmission of SARS-CoV-2 (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c). But a study showed that ACE2 was expressed in placental barrier cells suggesting the possibility of vertical transmission (Singh et al., 2020). Another study suggested that ACE2 had transient overexpression and increased activity during pregnancy, especially in the placenta (Schwartz and Graham, 2020). These studies implied that there may be vertical transmission of SARS-CoV-2. As we known, ACE2 receptors were widely distributed in maternal-fetal interface cells and special cell types of fetal organs. In the maternal-fetal interface, the expression of ACE2 was increased in these cells, including stromal cells of uterine decidua, perivascular cells, cytotrophoblast cells and plasmoditrophoblast cells in placenta (Mauvais-Jarvis et al., 2020). Previous clinical studies have not observed evidence of vertical transmission of SARS-CoV-2 in cases, and this phenomenon still needed to be studied more carefully in clinical practice (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c). Schwartz's research confirmed this study, they tested the newborn samples, including RT-PCR tests and placental SARS-CoV-2 tests, which showed negative results. Therefore, there was no evidence that SARS-CoV-2 virus was transmitted to the fetus through intrauterine or transplacental transmission in infected pregnant women (Schwartz and Graham, 2020). According to a significant report that there was a pregnant woman who had a fever for 8 h. According to her typical symptoms and CT images before admission, she was diagnosed as SARS-CoV-2 pneumonia. Throat swabs of newborns 30 h after birth were collected after emergency caesarean section, and still no direct evidence of intrauterine infection was provided. In addition, tissue samples in the uterus, such as amniotic fluid, cord blood or placenta, were not directly tested to confirm that SARS-CoV-2 infection in newborns was caused by intrauterine transmission (Schwartz, 2020). Therefore, we have been not sure whether intrauterine SARS-CoV-2 infection occurs. When considering whether there was vertical transmission of SARS-CoV-2, the following questions should be considered: 1. Whether this vertical transmission was related to pregnancy. 2. Whether vaginal delivery increased the risk of mother-to-child transmission during delivery. 3. The risk of infection in pregnant women and the impact of the time or mode of delivery on pregnancy outcomes needed to be assessed. 4. Whether SARS-CoV-2 could damage the placenta was an important part of vertical transmission, which should further investigation (Bilal et al., 2020, Egloff et al., 2020).
5. Successful solutions of controlling and prevention
From the above, China played a critical role in control and prevent the SARS-CoV-2 (Chen et al., 2020a, Chen et al., 2020b, Chen et al., 2020c, Feng et al., 2020, National Health Commission of the People's Republic of China, 2020). In order to control and prevent the further epidemic outbreaks of coronavirus into people, Chinese government has been implementing several strong initiatives. These primary initiatives were fruitful and effective to prevent spreading of epidemic outbreaks of coronavirus (Feng et al., 2020, Prasse et al., 2020, Wu et al., 2020). Especially, a medical team that composed of the military medical universities went to Wuhan and started the treatment work during the dates of Chinese traditional lunar new year holiday (Gao and Fan, 2020, Zhang, 2020). For countries outside China, Chinese government had sent 29 medical expert groups to 27 countries, meanwhile the government has provided or was providing assistance to 150 countries and four international organizations to control and prevent the SARS-CoV-2, as of May 31 (The Xinhua News Agency, 2020). After that, the monitoring of passing tourists has been increased at airports, ports and other transportation arteries, mainly including temperature detection and symptom screening recently, to avoid the occurrence of imported cases (Feng et al., 2020). At present, China’s epidemic control was relatively stable, and its various measures were worth studying and have been copied by other countries (Feng et al., 2020, National Health Commission of the People's Republic of China, 2020, Prasse et al., 2020, Wu et al., 2020).
Indeed, the effects of SARS-CoV-2 on the male/female reproductive system should be study in long term, such as the effects on fetal development. However, no much clinical/experimental data were reported at present. The reason might be that firstly, the most researchers preferred to focus on the studies of the damages to respiratory system than reproductive system, primarily; secondly, the time is not so long enough since the start of the pandemic, as a result that not any data of fetal development could be detected; thirdly, despite some results implied that SARS-CoV-2 infection might damage to male reproductive system via ACE2 receptor mediating, the potential cell receptor mediating mechanisms of SARS-CoV-2 have not been detected very clearly. With the studies of effects of SARS-CoV-2 on the male/female reproductive system become increasingly further deeper and the more effective vaccine could be manufactured, we would control and prevent the SARS-CoV-2 infection in the male/female reproductive system more and more efficient.
CRediT authorship contribution statement
Nengzhuang Wang: Conceptualization, Methodology, Software, Validation, Investigation, Data curation, Writing - original draft, Visualization, Project administration. Lina Qin: Conceptualization, Methodology, Software, Validation, Investigation, Data curation, Writing - original draft. Long Ma: Conceptualization. Hongli Yan: Supervision, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
We thank Reproductive Medicine Center of the First Affiliated Hospital of China Naval Military Medical University, for all artistic support related to this work.
Funding agencies
This research was supported by National Key Research and Development Program of China (2018YFC1004900), and National Key Research and Development Program of China (2018YFC1005002).
References
- Abhari S., Kawwass J.F. Endometrial susceptibility to SARS CoV-2: explained by gene expression across the menstrual cycle? Fertil. Steril. 2020;114:255–256. doi: 10.1016/j.fertnstert.2020.06.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batiha O., Al-Deeb T., Al-Zoubi E., Alsharu E. Impact of COVID-19 and other viruses on reproductive health. Andrologia. 2020;52 doi: 10.1111/and.13791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beal J., Mitchell T., Wyschogrod D., Manthey J., Clore A. Highly distinguished amino acid sequences of 2019-nCoV (Wuhan coronavirus) bioRxiv. 2020 2020.2001.2031.929497. [Google Scholar]
- Benvenuto D., Giovanetti M., Salemi M., Prosperi M., De Flora C., Junior Alcantara L.C., Angeletti S., Ciccozzi M. The global spread of 2019-nCoV: a molecular evolutionary analysis. Pathog. Glob. Health. 2020;114:64–67. doi: 10.1080/20477724.2020.1725339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilal M.Y., Katara G., Dambaeva S., Kwak-Kim J., Gilman-Sachs A., Beaman K.D. Clinical molecular genetics evaluation in women with reproductive failures. Am. J. Reprod. Immunol. 2020;e13313 doi: 10.1111/aji.13313. [DOI] [PubMed] [Google Scholar]
- Cantuti-Castelvetri L., Ojha R., Pedro L.D., Djannatian M., Franz J., Kuivanen S., van der Meer F., Kallio K., Kaya T., Anastasina M., Smura T., Levanov L., Szirovicza L., Tobi A., Kallio-Kokko H., Österlund P., Joensuu M., Meunier F.A., Butcher S.J., Winkler M.S., Mollenhauer B., Helenius A., Gokce O., Teesalu T., Hepojoki J., Vapalahti O., Stadelmann C., Balistreri G., Simons M. Neuropilin-1 facilitates SARS-CoV-2 cell entry and infectivity. Science. 2020 doi: 10.1126/science.abd2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cardona Maya W.D., Du Plessis S.S., Velilla P.A. SARS-CoV-2 and the testis: similarity with other viruses and routes of infection. Reprod. Biomed. Online. 2020;40:763–764. doi: 10.1016/j.rbmo.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceraolo C., Giorgi F.M. Genomic variance of the 2019-nCoV coronavirus. bioRxiv. 2020 doi: 10.1002/jmv.25700. 2020.2002.2002.931162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chadchan S.B., Maurya V.K., Popli P., Kommagani R. The SARS-CoV-2 receptor, angiotensin converting enzyme 2 (ACE2) is required for human endometrial stromal cell decidualization. bioRxiv. 2020 doi: 10.1093/biolre/ioaa211. 2020.06.23.168252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai X., Hu L., Zhang Y., Han W., Lu Z., Ke A., Zhou J., Shi G., Fang N., Fan J., Cai J., Fan J., Lan F. Specific ACE2 expression in cholangiocytes may cause liver damage after 2019-nCoV infection. bioRxiv. 2020 2020.2002.2003.931766. [Google Scholar]
- Chen H., Guo J., Wang C., Luo F., Yu X., Zhang W., Li J., Zhao D., Xu D., Gong Q., Liao J., Yang H., Hou W., Zhang Y. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395:809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W., Peter W.H., Frederick G.H., George F.G. A novel coronavirus outbreak of global health concern. Lancet UK. 2020 doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z.M., Fu J.F., Shu Q. New coronavirus: new challenges for pediatricians. World J. Pediatr. 2020;16:222. doi: 10.1007/s12519-020-00346-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng H., Wang Y., Wang G.Q. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J. Med. Virol. 2020;92:726–730. doi: 10.1002/jmv.25785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly J.L., Simonetti B., Klein K., Chen K.-E., Williamson M.K., Antón-Plágaro C., Shoemark D.K., Simón-Gracia L., Bauer M., Hollandi R., Greber U.F., Horvath P., Sessions R.B., Helenius A., Hiscox J.A., Teesalu T., Matthews D.A., Davidson A.D., Collins B.M., Cullen P.J., Yamauchi Y. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020 doi: 10.1126/science.abd3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y., He L., Zhang Q., Huang Z., Che X., Hou J., Wang H., Shen H., Qiu L., Li Z., Geng J., Cai J., Han H., Li X., Kang W., Weng D., Liang P., Jiang S. Organ distribution of severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) in SARS patients: implications for pathogenesis and virus transmission pathways. J. Pathol. 2004;203:622–630. doi: 10.1002/path.1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong N., Yang X., Ye L., Chen K., Chan E.W.-C., Yang M., Chen S. Genomic and protein structure modelling analysis depicts the origin and infectivity of 2019-nCoV, a new coronavirus which caused a pneumonia outbreak in Wuhan, China. bioRxiv. 2020 2020.2001.2020.913368. [Google Scholar]
- Dong R., Pei S., Yin C., He R.L., Yau S.S. Analysis of the hosts and transmission paths of SARS-CoV-2 in the COVID-19 outbreak. Genes (Basel) 2020;11 doi: 10.3390/genes11060637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douglas G.C., O'Bryan M.K., Hedger M.P., Lee D.K., Yarski M.A., Smith A.I., Lew R.A. The novel angiotensin-converting enzyme (ACE) homolog, ACE2, is selectively expressed by adult Leydig cells of the testis. Endocrinology. 2004;145:4703–4711. doi: 10.1210/en.2004-0443. [DOI] [PubMed] [Google Scholar]
- Drak Alsibai K. Expression of angiotensin-converting enzyme 2 and proteases in COVID-19 patients: a potential role of cellular FURIN in the pathogenesis of SARS-CoV-2. Med. Hypotheses. 2020;143 doi: 10.1016/j.mehy.2020.109893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egloff C., Vauloup-Fellous C., Picone O., Mandelbrot L., Roques P. Evidence and possible mechanisms of rare maternal-fetal transmission of SARS-CoV-2. J. Clin. Virol. 2020;128 doi: 10.1016/j.jcv.2020.104447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esakandari H., Nabi-Afjadi M., Fakkari-Afjadi J., Farahmandian N., Miresmaeili S.M., Bahreini E. A comprehensive review of COVID-19 characteristics. Biol. Proc. Online. 2020;22:19. doi: 10.1186/s12575-020-00128-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan C., Li K., Ding Y., Lu W.L., Wang J. ACE2 Expression in kidney and testis may cause kidney and testis damage after 2019-nCoV infection. medRxiv. 2020 doi: 10.3389/fmed.2020.563893. 2020.2002.2012.20022418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng W., Zong W., Wang F., Ju S. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a review. Mol. Cancer. 2020;19:100. doi: 10.1186/s12943-020-01218-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn J.A., Purushotham D., Choudhary M.N.K., Zhuo X., Fan C., Matt G., Li D., Wang T. Exploring the coronavirus epidemic using the new WashU Virus Genome Browser. bioRxiv. 2020 2020.2002.2007.939124. [Google Scholar]
- Fraietta R., Pasqualotto F.F., Roque M., Taitson P.F. SARS-COV-2 and male reproductive health. JBRA Assist. Reprod. 2020;24:347–350. doi: 10.5935/1518-0557.20200047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao L., Fan X. In: Ministry of National Defense of the People's Republic of China Wu Han, China. Simeng Z., editor. 2020. The medical team from the Naval Military Medical University started treatment at the intensive care unit of Hankou Hospital in Wuhan. [Google Scholar]
- Glowacka I., Bertram S., Muller M.A., Allen P., Soilleux E., Pfefferle S., Steffen I., Tsegaye T.S., He Y., Gnirss K., Niemeyer D., Schneider H., Drosten C., Pohlmann S. Evidence that TMPRSS2 activates the severe acute respiratory syndrome coronavirus spike protein for membrane fusion and reduces viral control by the humoral immune response. J. Virol. 2011;85:4122–4134. doi: 10.1128/JVI.02232-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goad J., Rudolph J., Rajkovic A. Female reproductive tract has low concentration of SARS-CoV2 receptors. bioRxiv. 2020 doi: 10.1371/journal.pone.0243959. 2020.06.20.163097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green C.D., Ma Q., Manske G.L., Shami A.N., Zheng X., Marini S., Moritz L., Sultan C., Gurczynski S.J., Moore B.B., Tallquist M.D., Li J.Z., Hammoud S.S. A comprehensive roadmap of murine spermatogenesis defined by single-cell RNA-Seq. Dev. Cell. 2018;46 doi: 10.1016/j.devcel.2018.07.025. 651–667 e610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grive K.J., Hu Y., Shu E., Grimson A., Elemento O., Grenier J.K., Cohen P.E. Dynamic transcriptome profiles within spermatogonial and spermatocyte populations during postnatal testis maturation revealed by single-cell sequencing. PLoS Genet. 2019;15 doi: 10.1371/journal.pgen.1007810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groner M.F., de Carvalho R.C., Camillo J., Ferreira P.R.A., Fraietta R. Effects of Covid-19 on male reproductive system. Int. Braz. J. Urol. 2021;47:185–190. doi: 10.1590/S1677-5538.IBJU.2021.99.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Grow E.J., Mlcochova H., Maher G.J., Lindskog C., Nie X., Guo Y., Takei Y., Yun J., Cai L., Kim R., Carrell D.T., Goriely A., Hotaling J.M., Cairns B.R. The adult human testis transcriptional cell atlas. Cell Res. 2018;28:1141–1157. doi: 10.1038/s41422-018-0099-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Grow E.J., Yi C., Mlcochova H., Maher G.J., Lindskog C., Murphy P.J., Wike C.L., Carrell D.T., Goriely A., Hotaling J.M., Cairns B.R. Chromatin and single-Cell RNA-seq profiling reveal dynamic signaling and metabolic transitions during human spermatogonial stem cell development. Cell Stem Cell. 2017;21 doi: 10.1016/j.stem.2017.09.003. 533–546 e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo J., Nie X., Giebler M., Mlcochova H., Wang Y., Grow E.J., DonorConnect, Kim R., Tharmalingam M., Matilionyte G., Lindskog C., Carrell D.T., Mitchell R.T., Goriely A., Hotaling J.M., Cairns B.R. The dynamic transcriptional cell atlas of testis development during human puberty. Cell Stem Cell. 2020;26 doi: 10.1016/j.stem.2019.12.005. 262–276 e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison A.G., Lin T., Wang P. Mechanisms of SARS-CoV-2 transmission and pathogenesis. Trends Immunol. 2020;41:1100–1115. doi: 10.1016/j.it.2020.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henarejos-Castillo I., Sebastian-Leon P., Devesa-Peiro A., Pellicer A., Diaz-Gimeno P. SARS-CoV-2 infection risk assessment in the endometrium: viral infection-related gene expression across the menstrual cycle. Fertil. Steril. 2020;114:223–232. doi: 10.1016/j.fertnstert.2020.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann M., Kleine-Weber H., Schroeder S., Kruger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.H., Nitsche A., Muller M.A., Drosten C., Pohlmann S. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181 doi: 10.1016/j.cell.2020.02.052. 271–280 e278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G., Cohn A., Fox L., Patel A., Gerber S.I., Kim L., Tong S., Lu X., Lindstrom S., Pallansch M.A., Weldon W.C., Biggs H.M., Uyeki T.M., Pillai S.K., Washington State-nCo V.C.I.T. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtmann N., Edimiris P., Andree M., Doehmen C., Baston-Buest D., Adams O., Kruessel J.S., Bielfeld A.P. Assessment of SARS-CoV-2 in human semen-a cohort study. Fertil. Steril. 2020;114:233–238. doi: 10.1016/j.fertnstert.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Q., Herrmann A. Fast assessment of human receptor-binding capability of 2019 novel coronavirus (2019-nCoV) bioRxiv. 2020 2020.2002.2001.930537. [Google Scholar]
- Illiano E., Trama F., Costantini E. Could COVID-19 have an impact on male fertility? Andrologia. 2020;52 doi: 10.1111/and.13654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ji W., Wang W., Zhao X., Zai J., Li X. Cross-species transmission of the newly identified coronavirus 2019-nCoV. J. Med. Virol. 2020;92:433–440. doi: 10.1002/jmv.25682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karia R., Gupta I., Khandait H., Yadav A., Yadav A. COVID-19 and its modes of transmission. SN Comprehen. Clin. Med. 2020:1–4. doi: 10.1007/s42399-020-00498-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karia R., Nagraj S. A review of viral shedding in resolved and convalescent COVID-19 patients. SN Comprehen. Clin. Med. 2020:1–10. doi: 10.1007/s42399-020-00499-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kayaaslan B., Korukluoglu G., Hasanoglu I., Kalem A.K., Eser F., Akinci E., Guner R. Investigation of SARS-CoV-2 in semen of patients in the acute stage of COVID-19 infection. Urol. Int. 2020;104:678–683. doi: 10.1159/000510531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalili M.A., Leisegang K., Majzoub A., Finelli R., Panner Selvam M.K., Henkel R., Mojgan M., Agarwal A. Male fertility and the COVID-19 pandemic: systematic review of the literature. World J. Mens Health. 2020;38:506–520. doi: 10.5534/wjmh.200134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar M., Taki K., Gahlot R., Sharma A., Dhangar K. A chronicle of SARS-CoV-2: Part-I – epidemiology, diagnosis, prognosis, transmission and treatment. Sci. Total Environ. 2020;734 doi: 10.1016/j.scitotenv.2020.139278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letko M., Munster V. Functional assessment of cell entry and receptor usage for lineage B beta-coronaviruses, including 2019-nCoV. bioRxiv. 2020 doi: 10.1038/s41564-020-0688-y. 2020.01.22.915660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Jin M., Bao P., Zhao W., Zhang S. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.8292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Li W., Song B., Wu H., Tang D., Wang C., He X., Cao Y. SARS-CoV-2 and the reproductive system: assessment of risk and recommendations for infection control in reproductive departments. Syst. Biol. Reprod. Med. 2020;66:343–346. doi: 10.1080/19396368.2020.1817627. [DOI] [PubMed] [Google Scholar]
- Li H., Zhou Y., Zhang M., Wang H., Zhao Q., Liu J. Updated approaches against SARS-CoV-2. Antimicrob. Agents Chemother. 2020;64:e00483–00420. doi: 10.1128/AAC.00483-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W., Feng Z., Rao S., Xiao C., Xue X., Lin Z., Zhang Q., Qi W. Diarrhoea may be underestimated: a missing link in 2019 novel coronavirus. Gut. 2020;69:1141. doi: 10.1136/gutjnl-2020-320832. [DOI] [PubMed] [Google Scholar]
- Luczak-Roesch M. Networks of information token recurrences derived from genomic sequences may reveal hidden patterns in epidemic outbreaks: a case study of the 2019-nCoV coronavirus. medRxiv. 2020 2020.2002.2007.20021139. [Google Scholar]
- Lukassen S., Bosch E., Ekici A.B., Winterpacht A. Single-cell RNA sequencing of adult mouse testes. Sci. Data. 2018;5 doi: 10.1038/sdata.2018.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma L., Xie W., Li D., Shi L., Ye G., Mao Y., Xiong Y., Sun H., Zheng F., Chen Z., Qin J., Lyu J., Zhang Y., Zhang M. Evaluation of sex-related hormones and semen characteristics in reproductive-aged male COVID-19 patients. J. Med. Virol. 2020 doi: 10.1002/jmv.26259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauvais-Jarvis F., Klein S.L., Levin E.R. Estradiol, progesterone, immunomodulation, and COVID-19 outcomes. Endocrinology. 2020;161 doi: 10.1210/endocr/bqaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohseni A.H., Taghinezhad S.S., Xu Z., Fu X. Body fluids may contribute to human-to-human transmission of severe acute respiratory syndrome coronavirus 2: evidence and practical experience. Chin. Med. 2020;15:58. doi: 10.1186/s13020-020-00337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muñoz M.C., Burghi V., Miquet J.G., Giani J.F., Banegas R.D., Toblli J.E., Fang Y., Wang F., Bartke A., Dominici F.P. Downregulation of the ACE2/Ang-(1–7)/Mas axis in transgenic mice overexpressing GH. J. Endocrinol. 2014;221:215–227. doi: 10.1530/JOE-13-0497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muralidar S., Ambi S.V., Sekaran S., Krishnan U.M. The emergence of COVID-19 as a global pandemic: understanding the epidemiology, immune response and potential therapeutic targets of SARS-CoV-2. Biochimie. 2020;179:85–100. doi: 10.1016/j.biochi.2020.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Commission of the People's Republic of China, 2020. Update on COVID-19 as of 24:00, 24 September. in www.nhc.gov.cn/xcs/yqfkdt/202009/7ad4cad835e444a9aa478322a7b3c9ef.shtml. [DOI] [PMC free article] [PubMed]
- Omolaoye T.S., Adeniji A.A., Cardona Maya W.D., du Plessis S.S. SARS-COV-2 (Covid-19) and male fertility: where are we? Reprod. Toxicol. 2020;99:65–70. doi: 10.1016/j.reprotox.2020.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paoli D., Pallotti F., Colangelo S., Basilico F., Mazzuti L., Turriziani O., Antonelli G., Lenzi A., Lombardo F. Study of SARS-CoV-2 in semen and urine samples of a volunteer with positive naso-pharyngeal swab. J. Endocrinol. Invest. 2020 doi: 10.1007/s40618-020-01261-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paraskevis D., Kostaki E.G., Magiorkinis G., Panayiotakopoulos G., Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. bioRxiv. 2020 doi: 10.1016/j.meegid.2020.104212. 2020.2001.2026.920249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prasse B., Achterberg M.A., Ma L., Van Mieghem P. Network-based prediction of the 2019-nCoV epidemic outbreak in the Chinese Province Hubei. Appl. Network Sci. 2020;5 doi: 10.1007/s41109-020-00274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am. J. Obstet. Gynecol. 2020;222:415–426. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rastogi Y.R., Sharma A., Nagraik R., Aygun A., Sen F. The novel coronavirus 2019-nCoV: its evolution and transmission into humans causing global COVID-19 pandemic. Int. J. Environ. Sci. Technol. (Tehran) 2020:1–8. doi: 10.1007/s13762-020-02781-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis A.B., Araujo F.C., Pereira V.M., Dos Reis A.M., Santos R.A., Reis F.M. Angiotensin (1–7) and its receptor Mas are expressed in the human testis: implications for male infertility. J. Mol. Histol. 2010;41:75–80. doi: 10.1007/s10735-010-9264-8. [DOI] [PubMed] [Google Scholar]
- Reusken C., Broberg E.K., Haagmans B., Meijer A., Corman V.M., Papa A., Charrel R., Drosten C., Koopmans M., Leitmeyer K., On Behalf Of E.-L., Erli N. Laboratory readiness and response for novel coronavirus (2019-nCoV) in expert laboratories in 30 EU/EEA countries, January 2020. Euro Surveill. 2020:25. doi: 10.2807/1560-7917.ES.2020.25.6.2000082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz D.A. An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab. Med. 2020;144:799–805. doi: 10.5858/arpa.2020-0901-SA. [DOI] [PubMed] [Google Scholar]
- Schwartz D.A., Graham A.L. Potential maternal and infant outcomes from (Wuhan) coronavirus 2019-nCoV infecting pregnant women: lessons from SARS, MERS, and other human coronavirus infections. Viruses. 2020;12 doi: 10.3390/v12020194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segars J., Katler Q., McQueen D.B., Kotlyar A., Glenn T., Knight Z., Feinberg E.C., Taylor H.S., Toner J.P., Kawwass J.F., American Society for Reproductive Medicine Coronavirus C.-T.F. Prior and novel coronaviruses, coronavirus disease 2019 (COVID-19), and human reproduction: what is known? Fertil. Steril. 2020;113:1140–1149. doi: 10.1016/j.fertnstert.2020.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh B., Gornet M., Sims H., Kisanga E., Knight Z., Segars J. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and its effect on gametogenesis and early pregnancy. Am. J. Reprod. Immunol. 2020;e13351 doi: 10.1111/aji.13351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tai W., He L., Zhang X., Pu J., Voronin D., Jiang S., Zhou Y., Du L. Characterization of the receptor-binding domain (RBD) of 2019 novel coronavirus: implication for development of RBD protein as a viral attachment inhibitor and vaccine. Cell. Mol. Immunol. 2020;17:613–620. doi: 10.1038/s41423-020-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang S., Mao Y., Jones R.M., Tan Q., Ji J.S., Li N., Shen J., Lv Y., Pan L., Ding P., Wang X., Wang Y., MacIntyre C.R., Shi X. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020;144 doi: 10.1016/j.envint.2020.106039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tauseef A., Muhammad K., Fazal Mehmood K., Jin H. Are we ready for the new fatal coronavirus: scenario of Pakistan? Hum. Vacc. Immunother. Pakistan. 2020 doi: 10.1080/21645515.2020.1724000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Xinhua News Agency . 2020. White Paper: China has Provided or is Providing Assistance to 150 Countries and Four International Organizations.https://baijiahao.baidu.com/s?id=1668805905366954277&wfr=spider&for=pc in. [Google Scholar]
- Tian X., Li C., Huang A., Xia S., Lu S., Shi Z., Lu L., Jiang S., Yang Z., Wu Y., Ying T. Potent binding of 2019 novel coronavirus spike protein by a SARS coronavirus-specific human monoclonal antibody. bioRxiv. 2020 doi: 10.1080/22221751.2020.1729069. 2020.2001.2028.923011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdecchia P., Cavallini C., Spanevello A., Angeli F. The pivotal link between ACE2 deficiency and SARS-CoV-2 infection. Eur. J. Intern. Med. 2020;76:14–20. doi: 10.1016/j.ejim.2020.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vishvkarma R., Rajender S. Could SARS-CoV-2 affect male fertility? Andrologia. 2020;52 doi: 10.1111/and.13712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J. Virol. 2020;94 doi: 10.1128/JVI.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Chen W., Zhou Y.-S., Lian J.-Q., Zhang Z., Du P., Gong L., Zhang Y., Cui H.-Y., Geng J.-J., Wang B., Sun X.-X., Wang C.-F., Yang X., Lin P., Deng Y.-Q., Wei D., Yang X.-M., Zhu Y.-M., Zhang K., Zheng Z.-H., Miao J.-L., Guo T., Shi Y., Zhang J., Fu L., Wang Q.-Y., Bian H., Zhu P., Chen Z.-N. SARS-CoV-2 invades host cells via a novel route: CD147-spike protein. bioRxiv. 2020 doi: 10.1038/s41392-020-00426-x. 2020.2003.2014.988345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Xu X. scRNA-seq profiling of human testes reveals the presence of the ACE2 receptor, a target for SARS-CoV-2 infection in spermatogonia, leydig sertoli cells. Cells. 2020;9:920. doi: 10.3390/cells9040920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wold Health Organization . Wold Health Organization; New York City, USA: 2020. COVID-19 Weekly Epidemiological Update. [Google Scholar]
- Wu H., Huang J., Zhang C.J.P., He Z., Ming W.-K. Facemask shortage and the coronavirus disease (COVID-19) outbreak: reflection on public health measures. medRxiv. 2020 doi: 10.1016/j.eclinm.2020.100329. 2020.2002.2011.20020735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu J., Qi L., Chi X., Yang J., Wei X., Gong E., Peh S., Gu J. Orchitis: a complication of severe acute respiratory syndrome (SARS) Biol. Reprod. 2006;74:410–416. doi: 10.1095/biolreprod.105.044776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J., Li R.Q., Wang H.R., Chen H.R., Liu Y.B., Gao Y., Chen F. Potential influence of COVID-19/ACE2 on the female reproductive system. Mol. Hum. Reprod. 2020;26(6):367–373. doi: 10.1093/molehr/gaaa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang M., Chen S., Huang B., Zhong J.M., Su H., Chen Y.J., Cao Q., Ma L., He J., Li X.F., Li X., Zhou J.J., Fan J., Luo D.J., Chang X.N., Arkun K., Zhou M., Nie X. Pathological findings in the testes of COVID-19 patients: clinical implications. Eur. Urol. Focus. 2020;6:1124–1129. doi: 10.1016/j.euf.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yousefi B., Valizadeh S., Ghaffari H., Vahedi A., Karbalaei M., Eslami M. A global treatments for coronaviruses including COVID-19. J. Cell. Physiol. 2020;235:9133–9142. doi: 10.1002/jcp.29785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H., Kang Z., Gong H., Xu D., Wang J., Li Z., Cui X., Xiao J., Meng T., Zhou W., Liu J., Xu H. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv, 2020 2020.2001.2030.927806. [Google Scholar]
- Zhang S. Ministry of National Defense of the People's Republic of China; Wu Han, China: 2020. The Navy Medical Team is on the Move. [Google Scholar]
- Zhao Y., Zhao Z., Wang Y., Zhou Y., Ma Y., Zuo W. Single-cell RNA expression profiling of ACE2, the receptor of SARS-CoV-2. bioRxiv. 2020 doi: 10.1164/rccm.202001-0179LE. 2020.2001.2026.919985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., Chen H.D., Chen J., Luo Y., Guo H., Jiang R.D., Liu M.Q., Chen Y., Shen X.R., Wang X., Zheng X.S., Zhao K., Chen Q.J., Deng F., Liu L.L., Yan B., Zhan F.X., Wang Y.Y., Xiao G.F., Shi Z.L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J., Kim J., Xiao X., Wang Y., Luo D., Jiang S., Chen R., Xu L., Zhang H., Moise L., Gutierrez A.H., De Groot A.S., Xiao G., Schoggins J.W., Zhan X., Wang T., Xie Y. The immune vulnerability landscape of the 2019 novel coronavirus, SARS-CoV-2. bioRxiv. 2020 2020.02.08.939553. [Google Scholar]
- Zou X., Chen K., Zou J., Han P., Hao J., Han Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020;14:185–192. doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]