Abstract
Aims/Introduction
We aimed to assess the health‐related quality of life (HRQoL) and identify its predictors among type 2 diabetes patients of Bangladesh.
Materials and Methods
This nationwide cross‐sectional study assessed HRQoL among 1,806 type 2 diabetes patients using the EuroQol‐5 Dimensions Questionnaire (EQ‐5D‐5L), and the responses were further translated into a single summary crosswalk index score using the UK time trade‐off value set. The predictors were determined using multinomial logistic regression analysis.
Results
The mean EQ‐5D‐5L index score was 0.62 (standard deviation 0.25), and men scored better than women. More than half of the study participants (53.4%) were ranked as “average” HRQoL. Overall, 64% of respondents had a “problem” at least in one of the dimensions of the EQ‐5D‐5L, and the burden of reported “problems” was higher among women (70%). Among the five dimensions, the highest reported “problem” was 79.8% for anxiety/depression, 77.7% for pain/discomfort and 60.1% for mobility. However, younger participants (aged <30 years) showed a higher burden of anxiety/depression (95%) compared with the rest of the population. The specific predictors of average/good HRQoL (odds ratio >1) were being men, living in a rural area, married, literate, a monthly income >19,488 BDT, absence of comorbidity and had a duration of diabetes ≤5 years.
Conclusions
The majority of Bangladesh’s type 2 diabetes patients had an “average” HRQoL based on the EQ‐5D‐5L index score. In broad terms, the identified predictors were sex, place of residence, marital status, literacy, monthly income, comorbidity and duration of diabetes.
Keywords: Bangladesh, Health‐related quality of life, Type 2 diabetes
The majority of type 2 diabetes patients in Bangladesh have an “average” level of health‐related quality of life using EuroQol‐5 Dimensions Questionnaire and it is significantly associated with several predictors.

Introduction
Diabetes mellitus is a chronic disease with great public health importance leading to high morbidity and mortality 1 . The International Diabetes Federation report that approximately 415 million people had diabetes mellitus globally, and it will be projected to reach 642 million by 2040 or maybe even doubled by the year 2040 2 . According to a study published in the Bulletin of the World Health Organization, 9.7% of the Bangladeshi adult population (aged >35 years) have diabetes, and 22.4% are prediabetic 3 . A meta‐analysis showed the increasing trend of diabetes mellitus in Bangladesh from 4% in 1995–2000 and 5% in 2001–2005 to 9% in 2006–2010, respectively 4 . Along with the burden of mortality and morbidity, the economic impact is also substantial, and the estimated average annual cost of diabetes care for Bangladeshi patients was $ USD314, among which the average direct cost was $USD283 and the indirect cost was $USD31 5 . Another aspect of diabetes mellitus as a disease is its psychosocial burden that affects self‐care behavior, resulting in poor glycemic control, more complications and poor quality of life 5 , 6 , 7 , 8 . Although the chain of diabetes care and modalities of treatment are gradually expanding in Bangladesh, the health‐related quality of life (HRQoL) of type 2 diabetes patients is still unjustified. Thus, understanding the HRQoL among type 2 diabetes patients is gradually becoming essential and might improve the overall outcome, and reduce the associated burden in terms of cost, care and complications 8 , 9 .
The HRQoL is a dimension that measures the composite of both physical and psychosocial aspects, and is influenced by personal experience of beliefs, expectations and perceptions 10 . It has shown that the HRQoL supplements the traditional measures of disease burden, and is specifically beneficial to address self‐reported chronic diseases (diabetes, breast cancer, arthritis and hypertension) and their risk factors (body mass index, physical inactivity and smoking status) 11 . Among these chronic preventable diseases, the negative impact of diabetes mellitus on HRQoL has been reported from different high and middle‐income countries using both generic and disease‐specific tools 12 .
Several tools have been used in diabetes research to address HRQoL. Among those, the EuroQol‐5 Dimensions Questionnaire (EQ‐5D) is a preference‐based instrument due to its simplicity and reliability 13 . Its utility was also reported by the Fenofibrate Intervention and Event Lowering in Diabetes study as an independent predictor of morbidity and mortality in patients with type 2 diabetes 13 . Different Asian countries, including Japan 14 and Korea 15 , have already applied EQ‐5D to evaluate HRQoL among their population with type 2 diabetes. Like other developing countries, the measurement of diabetes‐related QoL using the EQ‐5D instrument among the Bangladeshi population is very uncommon, and is carried out among limited samples using the 3L version 16 , 17 . As per our knowledge, no nationwide study was carried out among Bangladesh’s type 2 diabetes patients using the EQ‐5D‐5L version to measure the HRQoL. Hence, for the first time, we were prompted to evaluate the HRQoL using the EQ‐5D‐5L instrument in a large sample of the type 2 diabetes population. In addition to this, we sought to determine the predictors that influenced the HRQoL of Bangladeshi type 2 diabetes populations.
Methods
Study design
The cross‐sectional study was carried out among 1,832 type 2 diabetes patients in Bangladesh aged ≥18 years. The duration of the study was 6 months from January 2018 to June 2018. The sample size was determined using the prevalence of pain/discomfort obtained from a study of Bangladesh 16 that used the EQ‐5D‐5L instrument to assess HRQoL among type 2 diabetes patients (Appendix S1). First, we used multistage clustered random sampling to select the study sites from all divisions of Bangladesh. At the last stage, a health camp was organized in urban and rural areas to conveniently recruit type 2 diabetes patients (Figure S1). We had to apply convenient sampling, as currently, there is no existing sampling frame of the type 2 diabetes population in Bangladesh. Participants who were pregnant, mentally ill, showed an unwillingness to participate or residing in hospitals, prisons, nursing homes and other such institutions were excluded from the study.
Data collection procedures
Data were collected using a pre‐tested interviewer‐administered semistructured questionnaire based on the objectives. We segregated the overall data collection procedures into three phases. In the first phase, a face‐to‐face interview was carried out to collect information (personal, sociodemographic, comorbidities/complications, cost of diabetes management and HRQoL) using the questionnaire. The annual cost of diabetes management was calculated as a direct cost and indirect cost. Direct costs consisted of direct medical and non‐medical costs. To estimate the total direct cost, we added both of the components. Indirect healthcare cost was calculated using the human capital approach. Data on indirect costs covered in the present study included the cost for loss of productivity and loss of time (during traveling, waiting in clinic and consultation, hospitalization). The detailed methodology of direct and indirect cost calculation for type 2 diabetes patients in Bangladesh was previously described in two other studies 5 , 18 . Diabetes‐related QoL was measured using the generic instrument “EuroQoL (EQ‐5D‐5L)”, which was merged with the questionnaire and administered by the interviewers. In the second phase, anthropometric and blood pressure measurements were carried out following the methods described in “Non‐Communicable Disease Risk Factors Survey Bangladesh 2010” 19 . The anthropometric measurements included height, weight, waist circumference, hip circumference and their derivatives, such as body mass index and waist‐to‐hip ratio. These parameters were measured by trained male and female assistants while maintaining adequate privacy. In the third phase, capillary blood glucose measurement (fasting or 2 h after breakfast) was carried out using a standard glucometer with aseptic precautions. Glycemic status was defined as controlled when fasting glucose was <6.1 mmol/L and 2 h post‐meal was <7.8 mmol/L 20 .
Assessment of HRQoL using EQ‐5D‐5L
The HRQoL was assessed using an adapted and translated Bengali (local language) version of the EQ‐5D‐5L. This generic instrument is a descriptive version with five dimensions, such as mobility, self‐care, usual activities, pain/discomfort and anxiety/depression. Each dimension has five levels: no problem, slight problems, moderate problems, severe problems and extreme problems. Again, we generated a score of HRQoL using the EQ‐5D‐5L crosswalk index, and ranked the score using percentiles as “poor,” “average” and “good” (Table S1). We did this, as currently there is no classification system of the EQ‐5D‐5L to show the HRQoL of a population. The EQ‐5D‐5L generated value sets in several countries to calculate the preference‐based index considering a scale of 0.0 as being dead and 1.0 as full health. As there is no value set for Bangladesh, we used the time trade‐off method carried out in the UK, in which −0.59 is the worst possible health status 21 . We chose the UK value set, as it was previously also applied by another Bangladeshi study to assess HRQoL using the EQ‐5D instrument 17 .
Ethical consideration
All participants gave their informed written consent for inclusion before they participated in the study. The study was approved by the Ethical Review Committee of Bangladesh University of Health Sciences (identification number: BUHS/BIO/EA/18/001) on 19 April 2018.
Statistical analysis
All 1,832 responses were reviewed thoroughly for consistency and completeness. A total of 26 responses were found incomplete or inconsistent, and hence the final analysis comprised 1,806 responses. The data were entered in the pre‐designed Microsoft Office Excel format (Microsoft Corporation, Redmond, WA, USA), which was imported later into the Statistical Package for Social Science software version 20.0 for Windows (SPSS Inc., Chicago, IL, USA). All the estimates of precision were presented at a 95% confidence interval (CI), as appropriate. Descriptive analysis included the mean, standard deviation, median and interquartile range, frequencies and percentages.
The predictors of HRQoL were determined using multinomial logistic regression analysis. To find the factors that influenced the HRQoL, first, we ran univariate analysis considering the EQ‐5D‐5L index score as a dependent variable. Variables that showed a significant association (P < 0.05) with the dependent variable in the univariate analysis were identified. These statistically significant variables were examined as independent variables against the dependent variable in the multinomial logistic regression analysis. For multinomial logistic regression analysis, we calculated odds ratios (OR) and 95% CI for each independent variable. In the regression table, predictors that had OR >1 were presented for each category of HRQoL. We ensured the presence of no multicollinearity using the variance inflation factor to run the regression analysis. The statistical tests were considered significant (2‐sided) at a level of P < 0.05.
Results
Sociodemographic and diabetes‐related information
A total of 1,806 type 2 diabetes patients were included in the present study. Their mean (standard deviation) age and duration of diabetes were 50.8 (±11.7) years and 5.6 (±5) years, respectively. The majority of the participants were women (61.8%), living in urban areas (61.7%), married (91.3%) and illiterate (39.6%). More than half of the respondents (56.3%) were homemakers, and nearly half (48.2%) belonged to the lower‐middle‐income group. Most of the type 2 diabetes patients had uncontrolled glycemic status (88.7%), and nearly one‐quarter (19.5%) had diabetes‐related comorbidities (Table 1).
Table 1.
Sociodemographic and diabetes‐related information of the study participants
| Variables | n (%) | 95% CI |
|---|---|---|
| Age (years) † | 50.8 ± 11.7 | |
| Age categories (years) | ||
| <30 | 24 (1.3) | 0.8–1.8 |
| 30–39 | 268 (14.8) | 13.2–16.4 |
| 40–49 | 468 (25.9) | 23.9–27.9 |
| 50–59 | 567 (31.4) | 29.3–33.5 |
| ≥60 | 479 (26.5) | 24.5–28.5 |
| Sex | ||
| Men | 689 (38.2) | 36–40.4 |
| Women | 1,117 (61.8) | 59.6–64 |
| Area of residence | ||
| Urban | 1,114 (61.7) | 59.5–63.9 |
| Rural | 692 (38.3) | 36.1–40.5 |
| Educational status | ||
| Illiterate | 715 (39.6) | 37.3–41.9 |
| Primary | 364 (20.2) | 18.3–22.1 |
| Secondary | 530 (29.3) | 27.2–31.4 |
| Higher education | 197 (10.9) | 9.5–12.3 |
| Marital status | ||
| Married | 1,648 (91.3) | 90–92.6 |
| Others | 158 (8.7) | 7.4 (10) |
| Occupational status | ||
| Unemployed | 73 (4) | 3.1–4.9 |
| Service holder | 237 (13.1) | 11.5–14.7 |
| Farmer | 84 (4.7) | 3.7–5.7 |
| Businessmen | 263 (14.6) | 13–16.2 |
| Self‐employed | 55 (3) | 2.2–3.8 |
| Housewife | 1,017 (56.3) | 54–58.6 |
| Retired | 77 (4.3) | 3.4–5.2 |
| Monthly household income (BDT) ‡ | 18,000 (10,000–26,000) | |
| Monthly household income groups (BDT) § | ||
| <4,907 (low income) | 53 (2.9) | 2.1–3.7 |
| 4,907–19,488 (lower‐middle income) | 870 (48.2) | 45.9–50.5 |
| 19,489–60,252 (upper‐middle income) | 831 (46) | 43.7–48.3 |
| >60,252 (high income) | 52 (2.9) | 2.1–3.7 |
| Duration of diabetes (years) † | 5.6 ± 5 | |
| Glycemic status ¶ | ||
| Controlled | 204 (11.3) | 9.8–12.8 |
| Uncontrolled | 1,602 (88.7) | 87.2–90.2 |
| Yearly direct cost of diabetes care ‡ | 15,702 (8,213–25,793) | |
| Yearly indirect cost of diabetic care ‡ | 366 (125–854) | |
| Presence of comorbidities | 352 (19.5) | 17.7–21.3 |
Total n = 1,806.
Mean and standard deviation.
Median with interquartile range.
According to the 2006 per capita gross national income and the World Bank calculation.
Based on plasma glucose level pre‐meal (fasting) <6.1 mmol/L and 2 h post‐meal <7.8 mmol/L.
HRQoL among type 2 diabetes patients
More than half of the type 2 diabetes population (53.4%) of Bangladesh had “average” HRQoL, and just 21.6% had “good” HRQoL (Figure 1). The median EQ‐5D‐5L index score was 0.65 (interquartile range 0.53–0.77). This score was higher among men and those living in a rural area (Tables S2;S3). Pain/discomfort (77.7%) and anxiety/depression (79.8%) showed a higher burden than other dimensions. Overall, 64% of respondents had a “problem” at any of the dimensions of EQ‐5D‐5L, and the burden of reported “problems” was higher among women (70%) than their male counterparts. The total proportion of reported levels of health status for no problem, slight problem, moderate problem, severe problem and extreme problem were 36.1, 35.3, 19.5, 7.6 and 1.54%, respectively (Table 2). The burden of anxiety/depression was higher among patients with aged <30 years (Table S4).
Figure 1.
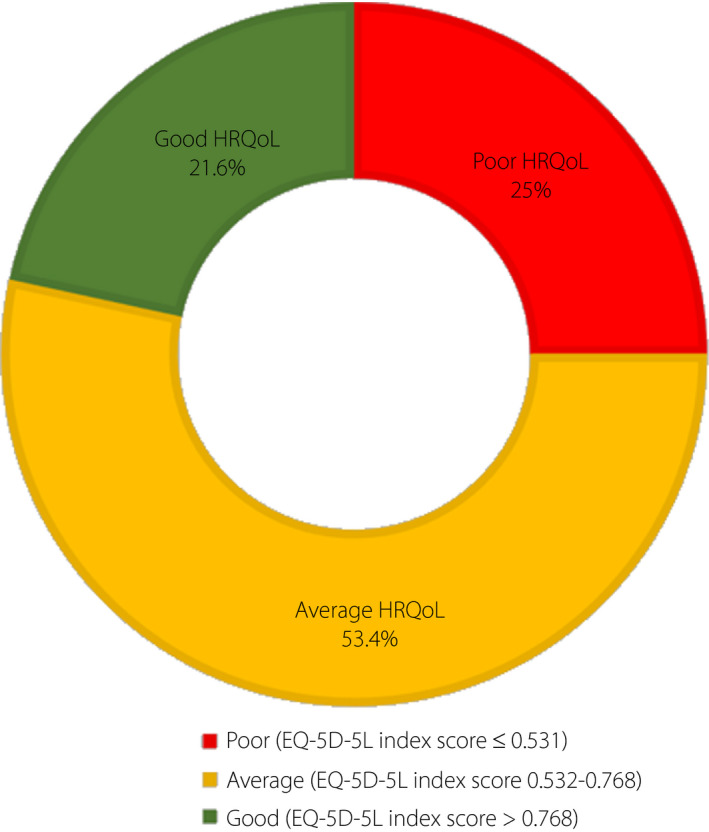
Levels of health‐related quality of life among type 2 diabetes patients in Bangladesh. Here, the EuroQol‐5 Dimensions Questionnaire (EQ‐5D‐5L) index score was categorized using percentiles of “poor” (score ≤25th percentile, ≤0.531), “average” (score >25th percentile and ≤75th percentile, 0.532–0.768) and “good” (score >75th percentile, >0.768).
Table 2.
Sex‐wise distribution of reported problems using five dimensions of the EuroQol‐5 Dimensions Questionnaire
| Dimensions | Men | Women | Total | |||
|---|---|---|---|---|---|---|
| n (%) | 95% CI | n (%) | 95% CI | n (%) | 95% CI | |
| Mobility | 351 (50.9) | 48.6–53.2 | 749 (67.1) | 64.9–69.2 | 1,100 (60.9) | 58.6–63.2 |
| Self‐care | 238 (34.5) | 32.3–36.7 | 627 (56.1) | 53.8–58.4 | 865 (47.9) | 45.6–50.2 |
| Usual activities | 284 (41.2) | 38.9–43.5 | 681 (61) | 58.8–63.2 | 965 (53.4) | 51.1–55.7 |
| Pain/discomfort | 483 (70.1) | 70–72.2 | 920 (82.4) | 80.6–84.2 | 1,403 (77.7) | 75.8–79.6 |
| Anxiety/depression | 509 (73.9) | 81.9–75.9 | 933 (83.5) | 81.8–85.2 | 1,442 (79.8) | 77.9–81.7 |
Total n = 1,806. CI, confidence interval.
Predictors of HRQoL among type 2 diabetes patients
Table 3 shows the predictors of HRQoL among the study population. Seven factors were identified that showed high odds (>1) for average/good HRQoL: area of residence (average, OR 2.028; good, OR 2.149), sex (average, OR 1.754; good, OR 3.765), education status (average, OR 1.565; good, OR 3.013), marital status (average, OR 1.281), monthly income (average, OR 1.442; good, OR 1.785), comorbidity (average, OR 1.438; good, OR 2.405) and duration of diabetes (average, OR 1.346; good, OR 1.184).
Table 3.
Predictors of health‐related quality of life among the type 2 diabetes population of Bangladesh
| HRQoL | Predictors | B | P‐value | OR | 95% CI for OR | ||
|---|---|---|---|---|---|---|---|
| Lower limit | Upper limit | ||||||
| Average | Area of residence | ||||||
| Rural area | 0.707 | <0.001* | 2.028 | 1.567 | 2.625 | ||
| Urban area |
Ref. |
||||||
| Sex | |||||||
| Men | 0.562 | <0.001* | 1.754 | 1.337 | 2.301 | ||
| Women |
Ref. |
||||||
| Education status | |||||||
| Literate | 0.147 | 0.002* | 1.565 | 1.173 | 2.089 | ||
| Illiterate |
Ref. |
||||||
| Marital status | |||||||
| Married | 0.200 | 0.214 | 1.281 | 0.866 | 1.895 | ||
| Others |
Ref. |
||||||
| Monthly income (BDT) | |||||||
| >19,488 | 0.366 | 0.003* | 1.442 | 1.135 | 1.831 | ||
| ≤19,488 |
Ref. |
||||||
| Comorbidity | |||||||
| Absent | 0.297 | 0.010* | 1.438 | 1.089 | 1.898 | ||
| Present |
Ref. |
||||||
| Duration of diabetes | |||||||
| ≤5 years | 0.297 | 0.017* | 1.346 | 1.055 | 1.718 | ||
| >5 years |
Ref. |
||||||
| Good | Area of residence | ||||||
| Rural area | 0.765 | <0.001* | 2.149 | 1.564 | 2.953 | ||
| Urban area |
Ref. |
||||||
| Sex | |||||||
| Men | 1.326 | <0.001* | 3.765 | 2.719 | 5.213 | ||
| Women |
Ref. |
||||||
| Education status | |||||||
| Literate | 1.103 | <0.001* | 3.013 | 1.950 | 4.657 | ||
| Illiterate |
Ref. |
||||||
| Monthly income (BDT) | |||||||
| >19,488 | 0.579 | <0.001* | 1.785 | 1.327 | 2.402 | ||
| ≤19,488 |
Ref. |
||||||
| Comorbidity | |||||||
| Absent | 0.878 | <0.001* | 2.405 | 1.631 | 3.548 | ||
| Present |
Ref. |
||||||
| Duration of diabetes | |||||||
| ≤5 years | 0.169 | 0.277 | 1.184 | 0.873 | 1.606 | ||
| >5 years |
Ref. |
||||||
Total n = 1,806. Statistically significant. BDT, Bangladesh Taka; CI, confidence interval; HRQoL, health‐related quality of life; OR, odd ratio; Ref, reference.
Overall, the odds for average/good HRQoL were higher among those who were men, living in a rural area, married, literate, had a monthly income of >19,488 BDT, did not have a comorbidity and had a duration of diabetes ≤5 years.
Discussion
One of the major goals of clinicians is to improve the physical and mental well‐being of a patient. To achieve this end‐point, they have to rely on unstructured conversations to explore subjective symptoms and extract laboratory data in clinical settings. In this regard, the measurement of HRQoL will add an alternative and cost‐effective dimension to subjective symptoms and the investigations. Although HRQoL has benefits over objective measures of health, data related to this issue are not well‐documented in Bangladesh. This is the first nationwide study in Bangladesh that detected the majority of the type 2 diabetes population of Bangladesh as having “average” HRQoL, and it was significantly influenced by several sociodemographic and diabetes‐related predictors.
In the current study, more than three‐quarters of the diabetes patients had problems in anxiety/depression (80%) and pain/discomfort (78%) dimensions individually. These findings were higher than the study of Saleh et al. 17 , where anxiety/depression was 74%, and pain/discomfort was 73%, respectively. However, the similarity was that both studies reflected a higher burden in the psychological aspect (anxiety/depression) than other dimensions. Contradictory to the current study and Saleh et al., another Bangladeshi case–control study 16 among the type 2 diabetes population reported a higher burden among the pain/discomfort dimension. The finding of the current study was also inconsistent and contradictory to some extent with the results of other Asian countries, including Japan 14 , Korea 15 , Singapore 22 , Indonesia 23 , Brunei 24 , China 25 , Thailand 26 and Iran 27 . As for the Asian countries, the toll of the problem was also higher for the pain/discomfort dimension in other parts of the world, including South Australia 28 , Canada 29 , Germany 30 , Spain 31 and Italy 32 . However, these developed countries assessed their HRQoL among the general population instead of among those who had diabetes. Although in the current study, the reported problem was higher in anxiety/depression, the pain/discomfort dimension also showed a substantial burden, as in other countries, and the difference of reported problems was negligible for the Bangladeshi type 2 diabetes population (80% in anxiety/depression vs 78% in pain/discomfort).
The present study reported that 36% of the respondents had “no problem,” and 64% had “problems” in at least one of the dimensions of the EQ‐5D‐5L. This reported “problem” was much higher than the two other Bangladeshi studies of Saleh et al. 17 and Safita et al. 12 , 16 , where the overall reported problem was 54.5 and 30.8%, respectively. The same contradictory findings were also observed among other Asian countries, where the reported problem was 19.3, 21.3, 13, 33.4, 33.4, 25.7 and 41.2% for Japan 14 , Korea 15 , Singapore 23 , Indonesia 23 , Brunei 24 , Thailand 26 and Iran 27 , respectively.
Other than reporting the burden of “problems” at each dimension, we also generated an index value or score using the responses. In the present study, the mean and median EQ‐5D‐5L crosswalk index score was 0.62 (standard deviation 0.25) and 0.65 (interquartile range 0.53–0.77), respectively. This continuous score also coincides with our categorized proportion of HRQoL that detected more than half of the study population had “average” HRQoL. However, other Asian countries, including Japan 14 , Korea 15 , Singapore 22 , Indonesia 23 , Iran 27 and China 33 , reported a much higher mean index score as 0.86, 0.92, 0.77, 0.89, 0.70 and 0.88, respectively, reflecting health status near to full health and better than Bangladesh. Other than reporting the mean index value, we have found only one study of Asia that reported HRQoL based on different ranks or categories, as in the present study (poor/average/good), and their findings were consistent with us as “perfect health” (21%), “slight/moderate” (51%) and “severe/extreme” (28%) 34 .
In the above discussion, country‐to‐country variation was observed for HRQoL among the type 2 diabetes population. The population‐based variation of HRQoL is due to its time dependency, and it is suggested to measure HRQoL repeatedly to obtain a reliable estimation. Explanations also include discontinuation of follow up by patients, the quality of diabetes care and the availability of access to support services that could bring change in the HRQoL 17 . Another reason for the population‐wide variation of HRQoL is the mode of administration of responses. It was shown that face‐to‐face interviews, postal surveys and participant‐administered responses differed from each other and results varied significantly. In this regard, face‐to‐face interviews influence survey results from two opposite aspects: the first is that persons with ill‐health could be easier to reach than with a postal survey 35 ; and the second aspect is that respondents answer questions more optimistically than any other methods 36 . A study with face‐to‐face interviews in Beijing showed that the Chinese population generally reported a smaller proportion of problems in EQ‐5D dimensions than Spain, the UK, the USA and Canada, and a slightly smaller proportion than Japan 37 . This difference was especially predominant in the pain/discomfort and anxiety/depression dimensions, as seen in the current study. In our discussion, we compared the countries that also used a different mode of administration of responses. The Asian countries – Japan 14 , Korea 15 , Indonesia 23 , Brunei 24 and Thailand 26 – used the participant‐administered format.
In contrast, Singapore 22 used the interviewer‐administered format, and Iran 27 used a mixed approach to complete the questionnaire. This might be the cause of the difference in findings between Bangladesh and other countries. Two other factors that might influence the result: one is the ceiling effect 37 and another is ethnicity 38 . Although the impact of ethnicity was beyond the scope of the current study, we briefly analyzed the ceiling effect (the proportion of respondents reporting “no problems” for all dimensions) and floor effect (the proportion of respondents reporting the worst level for all dimensions) of EQ‐5D‐5L. In the present study, no ceiling effect and floor effect were detected based on the criteria used by McHorney and Tarlov 39 . As a result, possibly, the tool has the capability to discriminate between individuals at either extreme of the scale.
In the present study, we identified that the anxiety/depression was higher among young diabetes populations compared with other age groups, and this was supported by an Iranian study that showed depression was significantly higher among younger type 2 diabetes patients compared with older patients 40 .The possible explanation is that in younger populations, the fear of future complications of diabetes is greater. Among sexes, we found that women had a lower index score than men, and it was a significant predictor of HRQoL. Findings among other native and Asian countries were also in agreement with the current report 14 , 15 , 17 , 22 , 23 , 24 , 25 , 27 . From Bangladesh’s perspective, the relatively better social life and high physical activity of men might contribute to a high satisfaction level about HRQoL among them. Besides this, women tend to be more expressive and are more likely to complain about their poor quality of life. In this regard, previous studies showed that men were more confident about glycemic control, reported a higher quality of life and were less likely to develop depression or anxiety compared with women 41 .
Different sociodemographic predictors were identified in the present study that showed significant associations with higher odds for average/good HRQoL among the Bangladeshi type 2 diabetes population. The same findings were also reported by other studies for place of residence (rural) 17 , 27 , sex (men) 16 , 17 , 27 , levels of education (literate) 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 33 , marital status (married) 6 , 42 , 43 and monthly income (high) 16 . It has reported that people with diabetes living in an urban area, especially in bigger cities 27 , have relatively lower HRQoL 17 , 27 . From Bangladesh’s perspective, the comparatively better HRQoL among rural people of the current study (Tables S2 and S3) could be explained by their dietary habits and lifestyle factors. Still, in Bangladesh, the rural population has access to fresh fruits, vegetables and fish compared with the urban population. Besides this, countrywide exploration of mass media also plays an important role in providing information to maintain a healthy life. Again, root‐level distribution of community healthcare services gradually is improving the HRQoL of the rural population 17 . Regarding sex, several studies reported that men with diabetes have an advantage over women with diabetes in HRQoL 6 . This is because men report comparatively lower disease impact 44 and more treatment satisfaction 45 than women do. To explore the sex difference, the previous study attempted to adjust age, educational level, living and marital status, physical activity, and some chronic disease conditions, such as obesity, diabetes and hypertension. However, these parameters did not fully explain the sex difference in HRQoL 46 .
In the present study, educated type 2 diabetes patients showed higher odds for average/good HRQoL in them. Previous studies showed that education level had a linear association with HRQoL. People with higher education levels are able to maintain a comparatively good HRQoL and their judgment of decisions impacts positively on diabetes care. This could be due to their better understanding of the disease process, its effect on them and their best effort to continue lifelong diabetes treatment 27 . The current study identified marriage as a predictor of hrqol, and this finding is similar to the previous studies that reported those who were not married were significantly more likely than those who were married to report psychological symptoms and subsequently low HRQoL 43 .
In the present study, two disease‐specific predictors were detected that showed a significant association with higher odds in relation to average/good HRQoL. One of them was the duration of diabetes, and the other was the absence of comorbidities. In the current study, participants who had lived with type 2 diabetes for ≤5 years had better HRQoL compared with those who had lived with it for >5 years. Previous studies 17 , 27 , 47 also reported this negative impact on HRQoL. Again, the findings of the present study about the impact of comorbidities on HRQoL are also supported by two other studies of Asia 34 , 48 . In this regard, Rubin and Peyrot stated in their review that the association of HRQoL and comorbidities are very consistent, and so strong that inconsistent findings with regard to the association between other variables and quality of life might be explained by the frequent omission of this factor as a possible confounding variable 6 .
The current study had several limitations. First, our study was a cross‐sectional study in design; it only provides an association and not causation. Second, we used the UK crosswalk index score to estimate the score for the Bangladeshi type 2 diabetes population; to our knowledge, a specific set of EQ‐5D‐5L for the Bangladeshi population has not been developed. Third, we did not assess the impact of behavioral risk factors, such as physical inactivity, tobacco use or alcohol intake, that might also have had an impact on HRQoL. Fourth, we used an interviewer‐administered questionnaire that might overestimate the problems in different dimensions due to the optimistic response of the participants, mentioned in detail earlier. Finally, because of the lack of a sampling frame of the type 2 diabetes population in Bangladesh, we had to apply the convenience sampling technique during sample recruitment, which might be associated with selection bias.
Despite of these limitations, this is the first nationwide study that simultaneously reported the EQ‐5D‐5L index score and levels of HRQoL for the type 2 diabetes population of Bangladesh. These findings are crucial, as evidence on this issue is lacking and dispersed. Furthermore, the current findings of HRQoL were a completely patient‐reported outcome that will help policymakers to identify different health problems related to diabetes, and thereby to remodel the chain of diabetes care effectively. Again, significant predictors were also identified in a large sample of the diabetes population that should be considered in clinical practice. We believe the present findings are generalizable and robust, providing direction for the future to improve the care of diabetes patients in Bangladesh.
In conclusion, the current study identified that most of the type 2 diabetes population of Bangladesh has an “average” HRQoL affecting both physical and mental well‐being. The substantial burden of anxiety/depression and pain/discomfort demand the involvement of mental health counsellors and physiotherapist in the management of diabetes patients. Furthermore, the identification of several predictors of the EQ‐5D‐5L index score could guide and facilitate the efforts aimed at improving the HRQoL of Bangladeshi type 2 diabetes patients.
Disclosure
The authors declare no conflict of interest.
Supporting information
Figure S1 | Sampling technique.
Table S1 | Levels/ranks of health‐related quality of life using the EuroQol‐5 Dimensions Questionnaire crosswalk index score among type 2 diabetes patients of Bangladesh, n = 1,806.
Table S2 | EuroQol‐5 Dimensions Questionnaire index score according to sex and area of residence, n = 1,806.
Table S3 | Area‐based distribution of reported problems using five dimensions of the EuroQol‐5 Dimensions Questionnaire, n = 1,806.
Table S4 | Proportion of the diabetes population that reported five levels of health status according to dimensions of the EuroQol‐5 Dimensions Questionnaire and age groups, n = 1,806.
Appendix S1 | Sample size estimation.
Acknowledgment
This study was supported by a grant (Invitation Ref No: DGHS/LD/NCDC/Procurement plan/GOB(Service)/2017‐18/LI/SP–05/1531) from the Noncommunicable Diseases Control Program, Directorate General of Health Services (DGHS), Ministry of Health & Family Welfare, Government of the People’s Republic of Bangladesh.
J Diabetes Investig 2021; 12: 277–285
References
- 1. Wee H‐L, Cheung Y‐B, Li S‐C, et al The impact of diabetes mellitus and other chronic medical conditions on health‐related Quality of Life: is the whole greater than the sum of its parts? Health Qual Life Outcomes 2005; 3: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogurtsova K, Fernandes JDR, Huang Y, et al IDF diabetes atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 2017; 128: 40–50. [DOI] [PubMed] [Google Scholar]
- 3. Akter S, Rahman MM, Abe SK, et al Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: a nation‐wide survey. Bull World Health Organ 2014; 92: 204–213A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saquib N, Saquib J, Ahmed T, et al Cardiovascular diseases and Type 2 Diabetes in Bangladesh: a systematic review and meta‐analysis of studies between 1995 and 2010. BMC Public Health 2012; 12, 434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Afroz A, Habib SH, Chowdhury HA, et al Healthcare cost of type 2 diabetes mellitus in Bangladesh: a hospital‐based study. Int J Diabetes Dev Ctries 2015; 36: 235–241. [Google Scholar]
- 6. Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev 1999; 15: 205–218. [DOI] [PubMed] [Google Scholar]
- 7. Glasgow RE, Osteen VL. Evaluating diabetes education: are we measuring the most important outcomes? Diabetes Care 1992; 15: 1423–1432. [DOI] [PubMed] [Google Scholar]
- 8. Rosenthal MJ, Fajardo M, Gilmore S, et al Hospitalization and mortality of diabetes in older adults: a 3‐year prospective study. Diabetes Care 1998; 21: 231–235. [DOI] [PubMed] [Google Scholar]
- 9. Glasgow RE, Ruggiero L, Eakin EG, et al Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care 1997; 20: 562–567. [DOI] [PubMed] [Google Scholar]
- 10. Rwegerera GM, Moshomo T, Gaenamong M, et al Health‐related quality of life and associated factors among patients with diabetes mellitus in Botswana. Alexandria J Med 2018; 54: 111–118. [Google Scholar]
- 11. NTIS . Measuring Healthy Days: Population Assessment of Health‐Related Quality of Life. NTIS. Available from: https://ntrl.ntis.gov/NTRL/dashboard/searchResults/titleDetail/PB2002104934.xhtml (Accessed May 13, 2019).
- 12. Glasziou P, Alexander J, Beller E, et al Which health‐related quality of life score? A comparison of alternative utility measures in patients with type 2 diabetes in the ADVANCE trial. Health Qual Life Outcomes 2007; 5, 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clarke PM, Hayes AJ, Glasziou PG, et al Using the EQ‐5D index score as a predictor of outcomes in patients with type 2 diabetes. Med Care 2009; 47: 61–68. [DOI] [PubMed] [Google Scholar]
- 14. Sakamaki H, Ikeda S, Ikegami N, et al Measurement of HRQL using EQ‐5D in patients with type 2 diabetes mellitus in Japan. Value Health 2006; 9: 47–53. [DOI] [PubMed] [Google Scholar]
- 15. Lee WJ, Song K‐H, Noh JH, et al Health‐related quality of life using the EuroQol 5D questionnaire in Korean patients with type 2 diabetes. J Korean Med Sci 2012; 27: 255–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Safita N, Islam SMS, Chow CK, et al The impact of type 2 diabetes on health related quality of life in Bangladesh: results from a matched study comparing treated cases with non‐diabetic controls. Health Qual Life Outcomes 2016; 141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Saleh F, Ara F, Mumu SJ, et al Assessment of health‐related quality of life of Bangladeshi patients with type 2 diabetes using the EQ‐5D: a cross‐sectional study. BMC Res Notes 2015; 81–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Afroz A, Chowdhury HA, Shahjahan M, et al Association of good glycemic control and cost of diabetes care: experience from a tertiary care hospital in Bangladesh. Diabetes Res Clin Pract 2016; 120: 142–148. [DOI] [PubMed] [Google Scholar]
- 19. Non‐Communicable Disease Risk Factor Survey Bangladesh 2010. Available from: https://www.who.int/ncds/surveillance/steps/2010_STEPS_Report_Bangladesh.pdf. (Accessed December 4, 2017).
- 20. Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1, Diagnosis and classification of diabetes mellitus. World Health Organization, 1999. Available from: https://apps.who.int/iris/handle/10665/66040. [Google Scholar]
- 21. EQ‐5D instruments . EQ‐5D. Available from: https://euroqol.org/eq‐5d‐instruments/eq‐5d‐5l‐about/valuation‐standard‐value‐sets/crosswalk‐index‐value‐calculator/ (Accessed December 4, 2017).
- 22. Shim YT, Lee J, Toh MPHS, et al Health‐related quality of life and glycaemic control in patients with Type 2 diabetes mellitus in Singapore. Diabetic Med. 2012; 29: e241–e248. [DOI] [PubMed] [Google Scholar]
- 23. Arifin B, Idrus LR, Asselt ADIV, et al Health‐related quality of life in Indonesian type 2 diabetes mellitus outpatients measured with the Bahasa version of EQ‐5D. Qual Life Res 2019; 28: 1179–1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Koh D, Abdullah AMKB, Wang P, et al Validation of Brunei’s Malay EQ‐5D questionnaire in patients with type 2 diabetes. PLoS One 2016; 11(11): e0165555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Sun S, Chen J, Johannesson M, et al Population health status in China: EQ‐5D results, by age, sex and socio‐economic status, from the National Health Services Survey 2008. Qual Life Res 2010; 20: 309–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pattanaphesaj J, Thavorncharoensap M. Measurement properties of the EQ‐5D‐5L compared to EQ‐5D‐3L in the Thai diabetes patients. Health Qual Life Outcomes 2015; 13: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Javanbakht M, Abolhasani F, Mashayekhi A, et al Health‐related quality of life in patients with type 2 diabetes mellitus in Iran: a national survey. Primary Care Diabetes 2013; 7: 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mccaffrey N, Kaambwa B, Currow DC, et al Health‐related quality of life measured using the EQ‐5D–5L: South Australian population norms. Health Qua Life Outcomes 2016; 14, 133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. EQ‐5D Population Norms . APERSU. Available from: https://apersu.ca/about‐eq‐5d/norms/ (Accessed May 29, 2019).
- 30. Hinz A, Kohlmann T, Stöbel‐Richter Y, et al The quality of life questionnaire EQ‐5D‐5L: psychometric properties and normative values for the general German population. Qual Life Res 2013; 23: 443–447. [DOI] [PubMed] [Google Scholar]
- 31. Garcia‐Gordillo MA, Adsuar JC, Olivares PR. Normative values of EQ‐5D‐5L: in a Spanish representative population sample from Spanish Health Survey, 2011. Qual Life Res 2015; 25: 1313–1321. [DOI] [PubMed] [Google Scholar]
- 32. Scalone L. Health Related Quality of Life norm data of the Italian general population: results using the EQ‐5D‐3L and EQ‐5D‐5L instruments. Epidemiology, Biostatistics and Public Health. Available from: https://ebph.it/article/view/11457. (Accessed May 5, 2019)
- 33. Pan C‐W, Sun H‐P, Zhou H‐J, et al Valuing health‐related quality of life in type 2 diabetes patients in China. Med Decis Making 2015; 36: 234–241. [DOI] [PubMed] [Google Scholar]
- 34. Alshayban D, Joseph R. Health‐related quality of life among patients with type 2 diabetes mellitus in Eastern Province, Saudi Arabia: a cross‐sectional study. PLoS One 2020; 15: e0227573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Bowling A. Mode of questionnaire administration can have serious effects on data quality. J Public Health 2005; 27: 281–291. [DOI] [PubMed] [Google Scholar]
- 36. Weinberger M, Oddone EZ, Samsa GP, et al Are health‐related quality‐of‐life measures affected by the mode of administration? J Clin Epidemiol 1996; 49: 135–140. [DOI] [PubMed] [Google Scholar]
- 37. Wang H, Kindig DA, Mullahy J. Variation in Chinese population health related quality of life: results from a EuroQol study in Beijing, China. Qual Life Res 2005; 14: 119–132. [DOI] [PubMed] [Google Scholar]
- 38. Fu AZ, Kattan MW. Racial and ethnic differences in preference‐based health status measure. Curr Med Res Opin 2006; 22: 2439–2448. [DOI] [PubMed] [Google Scholar]
- 39. Mchorney CA, Tarlov AR. Individual‐patient monitoring in clinical practice: are available health status surveys adequate? Qual Life Res 1995; 4: 293–307. [DOI] [PubMed] [Google Scholar]
- 40. Palizgir M, Bakhtiari M, Esteghamati A. Association of depression and anxiety with diabetes mellitus type 2 concerning some sociological factors. Iran Red Crescent Med J 2013; 15: 644–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Peyrot M, Rubin RR. Persistence of depressive symptoms in diabetic adults. Diabetes Care 1999; 22: 448–452. [DOI] [PubMed] [Google Scholar]
- 42. Jacobson AM, Groot MD, Samson JA. The evaluation of two measures of quality of life in patients with type I and type II diabetes. Diabetes Care 1994; 17: 267–274. [DOI] [PubMed] [Google Scholar]
- 43. Peyrot M, Rubin RR. Levels and risks of depression and anxiety symptomatology among diabetic adults. Diabetes Care 1997; 20: 585–590. [DOI] [PubMed] [Google Scholar]
- 44. Eiser C, Flynn M, Green E, et al Quality of life in young adults with type 1 diabetes in relation to demographic and disease variables. Diabetic Med 1992; 9: 375–378. [DOI] [PubMed] [Google Scholar]
- 45. Wredling R, Stålhammar J, Adamson U, et al Well‐being and treatment satisfaction in adults with diabetes: a Swedish population‐based study. Qual Life Res 1995; 4: 515–522. [DOI] [PubMed] [Google Scholar]
- 46. Hajian‐Tilaki K, Heidari B, Hajian‐Tilaki A. Are gender differences in health‐related quality of life attributable to sociodemographic characteristics and chronic disease conditions in elderly people? Int J Prev Med 2017; 8: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Reba K, Argaw Z, Walle B, et al Health‐related quality of life of patients with diagnosed type 2 diabetes in Felege Hiwot Referral Hospital, North West Ethiopia: a cross‐sectional study. BMC Res Notes 2018; 11, 544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hayek AAA, Robert AA, Saeed AA, et al Factors associated with health‐related quality of life among saudi patients with type 2 diabetes mellitus: a cross‐sectional survey. Diabetes Metab J 2014; 38: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 | Sampling technique.
Table S1 | Levels/ranks of health‐related quality of life using the EuroQol‐5 Dimensions Questionnaire crosswalk index score among type 2 diabetes patients of Bangladesh, n = 1,806.
Table S2 | EuroQol‐5 Dimensions Questionnaire index score according to sex and area of residence, n = 1,806.
Table S3 | Area‐based distribution of reported problems using five dimensions of the EuroQol‐5 Dimensions Questionnaire, n = 1,806.
Table S4 | Proportion of the diabetes population that reported five levels of health status according to dimensions of the EuroQol‐5 Dimensions Questionnaire and age groups, n = 1,806.
Appendix S1 | Sample size estimation.


