Background:
Facial transplantation (FT) is recognized as the ultimate reconstruction for severely disfigured patients. The substantial cost of these procedures in a nationalized health system has not been extensively published. The first Canadian FT performed in May 2018 was a great opportunity to address this subject and evaluate the viability of such a program.
Methods:
A detailed patient chart review was performed and a cost per unit approach was used to estimate the procedure cost. The preoperative, operative, and the postoperative periods up to 1-year after the surgery were analyzed. Financial support from private sponsors and Hospital Fund donations were considered. The literature on international FT and national solid organ transplantation was reviewed.
Results:
The overall 1-year cost was estimated at $440,224 (2018 CAD). The costs are explained by a long hospital length of stay, costly immunosuppressive therapy, and high immunosuppression-related complications. Those findings are consistent with international FT literature. The societal impact of the surgery was minimized with a $36,921 (2018 CAD) grant obtained from an external contributor. Interestingly, the hospital foundation sustained a 794% increase in donations ($1,787,148; 2019 CAD) the year following the surgery.
Conclusion:
Our experience confirmed that the combination of private funding, with positive goodwill and hospital donations, is a workable model for innovative surgery in the setting of a nationalized health system with financial restrictions.
INTRODUCTION
A facial vascularized composite allotransplant (VCA) is the penultimate reconstructive procedure performed on the severely disfigured. Since the first facial transplant in 2005, successful facial transplantations (FTs) have been performed over 45 times worldwide.1 Facial VCAs have added significant and invaluable quality-adjusted life years in this specific patient population.2,3 There has been wide media coverage of the successes in FT and the general public has ideologically supported the research and development of this reconstructive domain. However, the question always remains: How much do face transplants cost? and who pays for such a procedure? These questions are even more important in the setting of a publicly funded National Health System such as the one that we have in Canada. Few cost analyses on face transplantation were performed to this date, and none has yet addressed this question specifically.
The first Canadian face transplant, performed in May 2018, offered a great opportunity to examine the finances of facial VCA through a detailed cost analysis of all capital expenditures on materials, personnel, and infrastructure used from the work-up of the patient up to a year postoperatively. A detailed patient chart review and a cost per unit approach were required to obtain a realistic reflection of the transplantation cost.
Due to the limited cost analysis available in the literature, the results obtained in this study were compared with those published in the solid organ transplant literature, in addition to those published on facial VCA. The supposition was that, although costly, facial VCA is sustainable in the setting of a National Health System through the combination of private financial/material support with public funding and inferring potential savings from free goodwill marketing and hospital foundation donations.
First Canadian Facial VCA
On May 11, 2018, a Montreal team including 6 plastic surgeons, 2 oto-rhino-laryngologists, and 1 maxillofacial surgeon performed the first Canadian face transplantation. The recipient was a 64-year-old man severely disfigured by an accidental gun-shot wound in 2012, who had undergone 5 reconstructive procedures and who still suffered physically from chronic pain, severe speech impairment, the inability to masticate, breathe, and swallow normally, and who suffered from social stigmatization (Fig. 1). Following the face transplant, the patient remained in the ICU for 13 days and was hospitalized for another 47 days without major complication (Fig. 2). Weekly skin biopsies revealed an acute immunological rejection on postoperative day 57 that was successfully treated with intravenous and oral corticosteroids. More details on the procedure and the postoperative management are discussed in the article “Face Transplant: Current Update and First Canadian Experience” accepted for publication in Plastic and Reconstructive Surgery Journal.
Fig. 1.

Preoperative image of the patient immediately before the FT.
Fig. 2.

Postoperative image of the patient 2 years after the surgery.
METHODOLOGY
Patient medical records were reviewed from the initial evaluation in 2015 up to 1 year after the face transplant surgery. To obtain an accurate cost estimate, hospitalization, surgery, investigation, laboratory, medication, and health care professional costs were examined in detail.
Hospitalization costs were based on the LOS in the ICU and the ward. The daily cost of each unit, provided by the Government Health department reports,4 covered the direct and indirect costs. Direct expenses are defined as medical supplies, nursing and nursing assistant time, and admitting physician fees, whereas indirect fees represent the overhead cost. Surgery costs included the operation theater cost, material used, virtual surgical planning, anesthesiologists and surgeons’ fees, and donor mask fabrication.
Investigations included radiology and pathology analysis ordered. Laboratory tests were individually numbered. Hourly rate of operating room utilization, unitary cost of laboratory, pathology, and radiological tests were obtained from the hospital accounting department. Physician fees were extracted from to the Provincial Specialist Physician Billing Manual.5
Specialized medication such as immunosuppressive drugs, antibiotics, antivirals, and antifungals were counted in the medication group. Each medication cost was retrieved according to the Provincial Medication List establishing the maximal authorized selling price.6
Health care professional category had 2 components: out-patient clinic visits and professional assessments.5 The cost of these evaluations was established based on the hourly wage, or billing, of each health professionals employed by the hospital and salary were provided by the accounting department. Each hospitalization episode (transplantation and complication readmissions) and the out-patient period were examined separately. In-patient, out-patient, preoperative, transplantation, and postoperative costs were individually analyzed.
PubMed literature of solid organ transplant and face transplantation costs was reviewed. To allow for an easy comparison between our cost and those reported in the literature, numbers were adjusted according to medical inflation and then converted to Canadian Dollar (CAD) as of May 2018.7 The inflation rate was reflected by the Health Consumer Price Index of each respective country and obtained from their official statistical data website.8–11 For easier understanding, costs in the following text will be displayed in inflation-adjusted CAD with the original prices mentioned in parenthesis.
RESULTS
From the preoperative period up to 1 year after the transplantation, the combined cost estimate was $440,224. The preoperative period accounted for 6% of the overall cost, with a total of $24,926. The transplantation episode, lasting 60 days, was the most important part of the overall cost with 54% or $237,427. The postoperative period counted itself for $177,841 and 40% of the total (Fig. 3).
Fig. 3.
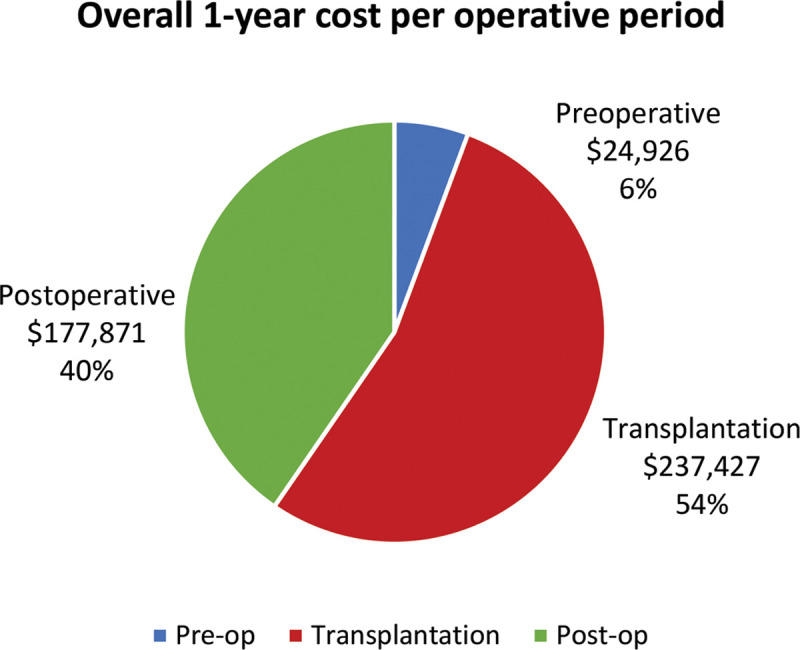
Pie diagram displaying the overall 1-year cost of the facial transplantation by medical periods.
Preoperative Cost
Of the $24 926 preoperative cost, surgical preparation and cadaver dissection were the most expensive, with 3 sessions at $7500 each, amounting to a total of $22,500. This training cost, fully sponsored by an external contributor (Johnson & Johnson), was included in the overall analysis because we believe it is a key element leading to the success of the surgery that cannot be neglect. Other charges were $733 for the preoperative examinations, $313 for laboratory analysis, and $1380 for physicians and health care professionals’ evaluations.
Transplantation
The face transplant hospitalization totaled $237,427. The cost was, in major part, generated by the surgical, hospitalization, and medication expenses, with $83,792, $85,162, and $54,542, respectively. Details of the surgical cost estimates are provided in Table 1. Medical supplies used during the surgery and the virtual surgical planning accounted for $14,421. Although included in the surgical cost, those 2 last components were provided by external sponsor (Johnson & Johnson) and not charged to the hospital. Surgeons salary was calculated in the analysis for extrapolation reasons; however, the surgery was performed voluntarily and therefore was not billed to the national health insurance.
Table 1.
Cost of Transplantation Hospitalization by Department
| Departments | Cost ($) |
|---|---|
| Surgery (total) | 83,792 |
| Operating room | 45,000 |
| Surgeons | 12,502 |
| Anesthesiologists | 6869 |
| Material | 14,421 |
| Donor mask | 5000 |
| Hospitalization (total) | 85,162 |
| Intensive care unit | 37,128 |
| Ward | 48,034 |
| Investigations | 1 220 |
| Medication | 54,542 |
| Health professionals | 1 177 |
| Laboratory | 11,534 |
Hospital LOS engendered major costs, with $37,128 for 13 days in ICU and $48,034 for 47 days on the ward. Of the medication expenses, the use of thymoglobulin for 8 days was responsible for more than 94% of this category’s cost with $51,525. Investigation, laboratory, and health care professional costs represented a smaller amount of the global fees and are displayed in Table 1.
Postoperative Cost
The postoperative costs, totaling $177,871 and 40% overall, were distributed between in-patient and out-patient care. Of the in-patient expenses, 4 complications required hospital readmission, generating significant costs as detailed in Table 2. Hospitalization fees, directly proportional to the LOS, represented the largest expense for each episode.
Table 2.
Cost of Complication-related Hospital Readmissions over 1 Year
| 1st Readmission | 2nd Readmission | 3rd Readmission | 4th Readmission | |
|---|---|---|---|---|
| Complication | Skin fungal infection | Tacrolimus toxicity with transient acute renal failure | Peptic esophageal disease and CMV infection | Perforated diverticular disease |
| Length of stay (d) | 18 | 7 | 49 | 21 |
| Cost ($) | ||||
| Surgery | — | — | — | 6478 |
| Hospitalization | 18,396 | 7154 | 50,078 | 21,462 |
| Investigations | 591 | 26 | 644 | 929 |
| Medication | 6714 | 139 | 6678 | 11,391 |
| Health professionals | 66 | 557 | 316 | 426 |
| Laboratory | 1173 | 412 | 2113 | 1111 |
| Total | 26,940 | 8289 | 59,829 | 41,797 |
In-patient Treatment of Complications
At 3 months postoperative, a spontaneous cutaneous fungal infection (Lichtheimia) on the thigh necessitated a short hospitalization and initiation of an expensive antifungal therapy. This treatment had to be pursued on an out-patient basis for a total of 6 months. On the seventh month postoperative, a brief readmission was caused by systemic tacrolimus toxicity with transient acute renal failure. The third rehospitalization, by far the longest, lasted 49 days, occurred 8 months after the face transplantation, and accounted for 44% of readmitting costs. Refractory peptic esophageal disease combined with late discovery of cytomegalovirus infection were the main reasons for this extended LOS. At 10 months postoperative, perforated diverticular disease warranted rehospitalization and surgical management, representing 31% of the overall complication charges.
Out-patient Care
Over the 365-day period studied, the patient was out of the hospital for a total 210 days and the estimated expenses related to his medical situation were $41,017. Medication represented a largest part of the sum with 78% or $32,067, followed by health care professional (18%) and investigations (4%). Immunosuppressive therapy consisting of tacrolimus, mycophenolic acid, and prednisone represented a monthly cost estimated at $764. Nevertheless, the Lichthemia skin infection treated with antifungal medication (Posaconazole) for more than 5 months was largely responsible for the expenses of this category ($22,707).
Solid Organ Transplant Cost Literature
Few studies have successfully assessed the cost of solid organ transplant in Canada. Levy et al. in 2009 reviewed the estimated cost of lung, liver, heart, and kidney transplants between 1995 and 2003 in British Columbia.12 The organ transplant program of this province is regulated and paid by a publicly funded, not-for-profit agency. This organization registers numerous details on the preoperative, operative, and postoperative care provided, from which cost estimates can be extracted accurately. The analysis of 1333 solid organ transplants were performed for the index hospitalization, the first and second year postoperative. Index hospitalization mean costs ranged from $34,851 ($27,695 CAD 2003) for kidneys to $113,180 ($89,942 CAD 2003) for lungs. Postoperative care costs of the first year after the transplant was in average between $27,120 ($21,552 CAD 2003) and $34,722 ($27,593 CAD 2003). Mean ICU LOS was between 0,1 and 11,0 days, and nursing ward stays between 10,2 and 18,0 days. Hospitalization fees represented between 50% and 70% of the overall costs of the transplantation hospitalization. The overall 1-year costs are displayed in Table 3.
Table 3.
Solid Organ Transplantation Costs in Canada and USA
| Transplantation and 1-Year Follow-up Cost | ||||||
|---|---|---|---|---|---|---|
| Levy et al | Gagnon et al | Schnitzler et al (Medicare) | ||||
| 2003 (CAD$) | 2018 (CAD$*) | 2001 (CAD$) | 2018 (CAD$*) | 2013 (USD$) | 2018 (CAD$*) | |
| Lung | 117,535 | 147,903 | — | — | 288,000 | 419,607 |
| Liver | 93,542 | 117,711 | 137,308 | 176,579 | 211,000 | 307,420 |
| Heart | 89,104 | 112,126 | — | — | 341,000 | 496,826 |
| Kidney | 49,247 | 61,971 | — | — | 114,000 | 166,094 |
| Intestine | — | — | — | — | 426,000 | 620,669 |
| Pancreas | — | — | — | — | 142,000 | 206,890 |
*Medical inflation included.
Older studies also evaluated specific solid organ transplantation costs in Canada. Gagnon et al published in 2004 the cost estimate related to liver transplant and obtained $127,399 ($99,066 CAD 2001) for the transplant hospitalization and $49,179 ($38,242 CAD 2001) for the first follow-up year13 (Table 3).
In the United States, a report on solid organ transplantation by the Scientific Registry of Transplant Recipients is issued annually. In 2018, Schnitzler et al published in this report a cost analysis based on the Medicare reimbursement for organ transplants made in 2013 and 2014.14 The overall 1-year costs ranged from $166,094 ($114,000 USD 2013) for kidneys to $620,669 ($426,000 USD 2013) for intestine transplants (Table 3).
Face Transplant Cost Literature
Few cost analyses on face transplant were performed at this point. Two publications from USA provided a good estimate on expenses with a detailed cost assessment distributed by sector. The first one by Siemionow et al in 2008 studied the cost of the first US face transplant relatively to the cost of the previous conventional reconstruction performed on the same patient. The face transplant represented an overall cost of $595,408 ($349,959 USD 2008) for the 1-year period. The patient spent a total of 58 days hospitalized and was readmitted 8 times for complications for a total of 36 days15 (Table 4).
Table 4.
Face Transplantation Cost Published in the Literature
| Siemionow et al | Nguyen et al | Ruëgg et al | Chenggang et al | |||||
|---|---|---|---|---|---|---|---|---|
| 2008 USD$ | 2018 CAD$* | 2010 USD$ (mean) | 2018 CAD$* | 2010 EUR € (mean) | 2018 CAD$* | 2006 USD $ | 2018 CAD $* | |
| Transplantation hospitalization cost | 232,893 | 396,236 | 228,118 | 363,761 | 129,798 | 185,948 | 80,000 | 108,474 |
| Total 1-year cost | 349,959 | 595,408 | 337,360 | 537,960 | — | — | — | — |
*Medical inflation included.
The second US article was written by Nguyen et al in 2015. They did a thorough comparison of the mean cost of their last 4 face transplants performed through 2009 to 2011 and the estimated cost that would have been generated with conventional reconstruction. They revealed an overall 1-year mean cost of $537,960 ($337,360 USD 2010) for the face transplant group16 (Table 4).
A 2012 French study by Ruëgg et al. reviewed the expenses of 5 face transplants realized between 2007 and 2010. The focus was on the preoperative period and index hospitalization. Their mean cost was $185,948 (129,798 € EUR 2010) for the combined preoperative and transplant hospitalization period.17 It is worth mentioning here that in the index hospitalization, postoperative medication, laboratory, and radiological examinations were not considered in their analysis (Table 4).
Chenggang et al published in 2008 their first partial face transplant accomplished in 2006. The overall cost was briefly mentioned without details on the method and was estimated as $108,474 ($80,000 USD 2008) with $814 ($600 USD 2006) monthly cost for immunosuppressants18 (Table 4).
DISCUSSION
Our first experience with face transplant generated an estimated overall 1-year cost of $440,224, mainly associated with in-patient care and hospitalization fees. This final cost estimate appears to be closer to what was reported in the US literature by Siemionow and Nguyen et al.15,16 When put in relation with the cost of other US solid organ transplants, they were similar to that of heart and small intestine transplants.14
The comparison of cost between countries and different health care systems is quite inaccurate due to the countless differences that exist. Health coverage, funding resources, administrative costs of care, medical supply and pharmaceutical costs, and physician and nurse salaries are a few features that vary among different nations.19–24 Those differences added to dramatic methodology disparities within published articles and can explain why our results differ from European and Asian cost analysis.
Nevertheless, data regarding solid organ transplant cost in Canada, though limited, are available. When compared with the published Canadian literature, our transplant hospitalization cost, representing the largest percent of expenditure (54%), was costlier than that of other solid organ transplants. Lung transplants had the highest index hospitalization cost [$113,180 ($89,942 CAD 2003)],12 and liver transplantation had a cost of $127,399 ($99,066 CAD 2001).13
Despite the inherent differences between face and solid organ transplantation, it is interesting to evaluate the source of the cost differences. Length-of-stay (LOS), immunosuppressive induction and maintenance therapy, and immunosuppression-related complication rates seem to explain the cost gap between conventional organ transplantation and FT.
In our analysis of the Canadian cost, it is clear that the hospital LOS was the most expensive component. The mean hospital LOS for liver and lung transplant was, respectively, 23.5 and 28.8 days.12 Our face transplant LOS was 60 days, which is similar to that of the first USA transplant in 2008 (58 days).15 This LOS was also comparable with the most experienced VCA team in France, with mean total hospital stay of 65,4 days.17 Hospital LOS for an FT seems to be twice as long as the most expensive solid organ transplants reported in the Canadian literature. This significant cost will be reduced with more VCA experience because we would transition the patients out of the hospital and into rehabilitation centers sooner.
At 1-year postoperative interval, 4 complications and subsequent hospitalizations accounted for a cost of $136,854. This complication rate is in the range of previously published literature on facial transplantation.25 A part of this high rate of postoperative complications could be explained by aggressive immunosuppression and subsequent viral, fungal, and bacterial infections. The high complication rate and associated costs have led us to re-evaluate our immunosuppressive protocol and will be altered for future VCAs.
Although rigorous in their cost analysis, Canadian published papers are not without limitations. For example, Levy et al were unable to access data regarding medication different than immunosuppressant.12 In our analysis, antibiotics, antifungals, and antivirals largely represented hospital and out-patient costs, with $50,418 or 11% overall. There is a significant possibility that missing data in previously cited retrospective Canadian studies led to an underestimation of overall costs.
Another aspect that is not often considered in the balance of the cost analysis is the value of innovation. As mentioned by Dahlborg et al, surgical innovation such as face and hand transplants can improve hospital goodwill and improve faith in the public health care system and thereby draw scientists, researchers, patients, and funding.26 They demonstrated a net increase in advertising value equivalent of their transplant program accordingly with the realization of surgical innovative procedure. In our experience, instead of measuring the advertisement worth generated by the media coverage of the surgery, we analyzed the donation collected at the Hospital Fund for the year following the procedure. Donation totaled $1,787,148, a substantial increase of 794% compared with the $225,101 annual average of the 4 previous years.27 The FT surgery being the only major event of that year, it is reasonable to consider that it has had a significant effect on the donation growth. Donation itself would have covered 4 face transplantations based on our actual cost estimated for a 1-year period.
Finally, our project is not without potential bias. Indeed, the retrospective nature of this study and the cost per unit approach can potentially underestimate certain costs. Furthermore, the cost of potential failure, although very rare, is not considered and would potentially represent more than twice the amount of expenditure spent for the surgery. Our analysis, however, gives us a good starting point on how to minimize the cost for eventual future VCA. Namely, reducing immunosuppression-related complications with a less aggressive therapy, and a shorter hospital stay. Moreover, with the success of this first FT, we were able to show the university, the government, and the public the positive benefits of such a procedure on multiple levels. In fact, the government has recently allocated a fixed budget for VCA research and development at our center, a first in the country.
CONCLUSIONS
This study demonstrates that successful face transplantation comes with certain inherent costs that are not seen with conventional transplants. It is widely accepted that the single facial transplant is less costly than the multiple conventional reconstructive procedures required to have poorer results, and it is also widely accepted that the social and physical benefits of the transplant outweigh the financial costs. This study has clearly demonstrated the precise cost of a face transplant in a publicly funded health care system with a 1-year follow-up. By combining private funding for materials and equipment, with positive goodwill and hospital donations for research and development, we have displayed a workable model for innovative surgery in the current climate of health care funding restrictions.
PATIENT CONSENT
The patient provided written consent for the use of his image.
Footnotes
Published online 25 January 2021.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. A research grant was donated by Johnson & Johnson to support the operation of the patient.
REFERENCES
- 1.Devauchelle B, Badet L, Lengelé B, et al. First human face allograft: early report. Lancet. 2006;368:203–209. [DOI] [PubMed] [Google Scholar]
- 2.Wo L, Bueno E, Pomahac B. Facial transplantation: worth the risks? A look at evolution of indications over the last decade. Curr Opin Organ Transplant. 2015;20:615–620. [DOI] [PubMed] [Google Scholar]
- 3.Cugno S, Sprague S, Duku E, et al. Composite tissue allotransplantation of the face: decision analysis model. Can J Plast Surg. 2007;15:145–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ministère de la Santé et des Services Sociaux du Québec. MSSS direction des politiques de financement et de l’allocation des ressources. Available at http://msssa4.msss.gouv.qc.ca/fr/document/d26ngest.nsf/93715d5d9d8780c9852565700049834e/e52bf6a9cdb55194852585420063f284?OpenDocument&Highlight=0,prix,journ%C3%A9e. Published April 2019. Accessed March 30, 2020.
- 5.Régie de l’Assurance Maladie du Québec. Manuel des médecins spécialistes – rénumération à l’acte. Available at https://www.ramq.gouv.qc.ca/SiteCollectionDocuments/professionnels/manuels/150-facturation-specialistes/manuel-specialistes-remuneration-acte-M93-li1.html. Published March 6, 2020. Accessed March 30, 2020.
- 6.Régie de l’assurance maladie du Québec. Liste des médicaments. Available at https://www.ramq.gouv.qc.ca/SiteCollectionDocuments/liste_med/2018/liste_med_2018_05_24_fr.pdf. Published May 24, 2018. Accessed March 30, 2020.
- 7.Bank of Canada (2020). Daily exchange rates lookup. Available at https://www.bankofcanada.ca/rates/exchange/daily-exchange-rates-lookup/?series%5B%5D=FXUSDCAD&lookupPage=lookup_daily_exchange_rates_2017.php&startRange=2010-04-26&rangeType=range&rangeValue=&dFrom=2018-05-11&dTo=2018-05-11&submit_button=Submit. Published May 11, 2018. Accessed April 29, 2020.
- 8.U.S. Bureau of Labor Statistics. CPI for all urban consumers – U.S. city average, medical care. Available at https://data.bls.gov/cgi-bin/surveymost?cu. Published 2008, 2010, 2013 and 2018. Accessed April 29, 2020.
- 9.National Bureau of Statistics of China. Annual data, consumer price indices by category. Available at http://www.stats.gov.cn/tjsj/ndsj/2018/indexeh.html. Published 2006 and 2018. Accessed April 29, 2020.
- 10.International Monetary Fund. IMF data: Access to macroeconomic and financial data, consumer price index (CPI). Available at https://data.imf.org/?sk=4FFB52B2-3653-409A-B471-D47B46D904B5&sId=1485878802128. Published 2010 and 2018. Accessed April 29, 2020.
- 11.Statistics Canada. Table 18-10-0004-08 consumer price index, monthly, percentage change, not seasonally adjusted, Canada, provinces, Whitehorse and Yellowknife — Health and personal care. 10.25318/1810000401-eng. 2001, 2003 and 2018. Accessed April 29, 2020. [DOI]
- 12.Levy AR, Sobolev B, James D, et al. The costs of change: direct medical costs of solid organ transplantation in British Columbia, Canada, 1995–2003. Value Health. 2009;12:282–292. [DOI] [PubMed] [Google Scholar]
- 13.Gagnon YM, Levy AR, Iloeje UH, et al. Treatment costs in Canada of health conditions resulting from chronic hepatitis B infection. J Clin Gastroenterol. 2004;38(10 suppl 3):S179–S186. [DOI] [PubMed] [Google Scholar]
- 14.Schnitzler MA, Skeans MA, Axelrod DA, et al. OPTN/SRTR 2016 Annual Data Report: economics. Am J Transplant. 2018;18suppl 1):464–503. [DOI] [PubMed] [Google Scholar]
- 15.Siemionow M, Gatherwright J, Djohan R, et al. Cost analysis of conventional facial reconstruction procedures followed by face transplantation. Am J Transplant. 2011;11:379–385. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen LL, Naunheim MR, Hevelone ND, et al. Cost analysis of conventional face reconstruction versus face transplantation for large tissue defects. Plast Reconstr Surg. 2015;135:260–267. [DOI] [PubMed] [Google Scholar]
- 17.Rüegg EM, Hivelin M, Hemery F, et al. Face transplantation program in France: a cost analysis of five patients. Transplantation. 2012;93:1166–1172. [DOI] [PubMed] [Google Scholar]
- 18.Chenggang Y, Yan H, Xudong Z, et al. Some issues in facial transplantation. Am J Transplant. 2008;8:2169–2172. [DOI] [PubMed] [Google Scholar]
- 19.Brown LD. Comparing health systems in four countries: lessons for the United States. Am J Public Health. 2003;93:52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Duffin J. The impact of single-payer health care on physician income in Canada, 1850-2005. Am J Public Health. 2011;101:1198–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papanicolas I, Woskie LR, Jha AK. Health care spending in the United States and other high-income countries. JAMA. 2018;319:1024–1039. [DOI] [PubMed] [Google Scholar]
- 22.Petch J, Dhalla IA, Henry DA, et al. Public payments to physicians in Ontario adjusted for overhead costs. Healthc Policy. 2012;8:30–36. [PMC free article] [PubMed] [Google Scholar]
- 23.Pozen A, Cutler DM. Medical spending differences in the United States and Canada: the role of prices, procedures, and administrative expenses. Inquiry. 2010;47:124–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ridic G, Gleason S, Ridic O. Comparisons of health care systems in the United States, Germany and Canada. Mater Sociomed. 2012;24:112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shanmugarajah K, Hettiaratchy S, Clarke A, et al. Clinical outcomes of facial transplantation: a review. Int J Surg. 2011;9:600–607. [DOI] [PubMed] [Google Scholar]
- 26.Dahlborg EJ, Diaz-Siso JR, Bueno EM, et al. The value of innovation: face and hand transplantation programs at Brigham and Women’s Hospital. Plast Reconstr Surg. 2014;134:178e–179e. [DOI] [PubMed] [Google Scholar]
- 27.Fondation de l’Hôpital Maisonneuve-Rosemont. Rapport annuel 2019. Available at https://www.fondationhmr.ca/fr/la-fondation/rapports-annuels-et-etats-financiers/. Accessed June 20, 2020.


