Abstract
Background
Poor handover and inadequate transmission of clinical information between shifts can result in patient harm. This study was designed to evaluate the impact of implementing a handover protocol on the quality of information exchanged in the trauma handover meetings in a UK district general hospital.
Methods
A prospective single centre observational study was performed at an acute NHS trust, using the define, measure, analyse, improve and control (DMAIC) methodology. Ten consecutive weekday trauma meetings, involving 43 patients, were observed to identify poor practices in handover. This data was used in conjunction with the Royal College of Surgeon's recommendations for effective handover (2007) to create a standard operating protocol (SOP). Following the implementation of the SOP, a further eight consecutive weekday trauma meetings, involving a further 47 patients, were observed. The data collection was performed by five trained independent observers. The data was analysed using t-test for quantitative variables and chi-square or Fisher's exact tests for categorical variables.
Results
An improvement in the trauma handover was demonstrated in multiple aspects of trauma handover including patient's past medical history, date of injury, results, diagnosis, consent, mark and starvation status (all p < 0.001). Subgroup analyses showed that handover of neck of femur patients including information on baseline mobility (p = 0.04), Nottingham Hip Fracture Score (p = 0.01), next of kin discussion (p = 0.075) and resuscitation status (p = 0.001) all improved following our interventions.
Conclusion
These results demonstrate that the implementation of a well-structured handover protocol can improve the transmission of critical information in trauma meetings.
Keywords: Trauma orthopaedics handover quality improvement femur
Highlights
-
•
Poor handover of clinical information results in patient harm.
-
•
A research method has been proposed to assess the clinical handover process.
-
•
A handover protocol improved the transfer of patient information.
-
•
A significant improvement in the handover of neck-of-femur patients was observed.
-
•
The protocol can be utilised by other similarly structured orthopaedic departments.
1. Introduction
1.1. Problem description
Handover is defined as the transfer of professional responsibility and accountability for the aspects of a patient's care to another person [1] including information such as the patient's history, current medical state and management plan [2]. The handover period is recognised as a vulnerable period in a patient's journey [3] in which inadequate transfer of information can result in patient harm [4]. It has been suggested that trauma patients specifically are at a greater risk of mortality as a result of poor communication [5]. A greater emphasis has been placed on the handover process since the implementation of the European Working Time Directive [6], meaning working patterns have moved towards shift work; therefore, multiple teams and specialities can be involved in the care of a given patient. As a result, the handover process needs to be efficient and effective [1]. As well as improving patient safety, the handover process is important from an individual's professional perspective especially in an increasingly litigious health culture [7]. Furthermore, the handover process should be regularly reviewed as part of clinical governance according to the Royal College of Surgeons' England guidelines on handover [8].
In trauma and orthopaedics specifically, effective communication in handover is critical, especially due to a high turnover of patients. If key clinical information is missed, this can result in significant delays in the deliverance of appropriate care. For example, for the handover of a patient who has sustained a neck-of-femur (NOF) fracture, specific clinical information including the patient's baseline mobility, Abbreviated Mental Test Score (AMTS) and Nottingham Hip Fracture Score (NHFS) [9] assist in the formation of the management plan. If this information is missed, the information cannot be discussed as part of the multidisciplinary team (MDT) approach in the handover meeting. Therefore, improper management plans may be formulated and the opportunity to discuss a patient's management may be missed, ultimately resulting in adverse patient outcomes especially for NOF patients with a known one-month mortality of 10% [10].
This study was performed at a cross-site district general hospital in the United Kingdom serving a population of 530,000 people with approximately 40,000 admissions per year [11]. The morning handover meeting occurs at 08:00 and is split into two: the handover of trauma patients going to theatre (trauma handover) and other patients who have been admitted under the orthopaedic department (admissions handover). The meetings are attended by many members of the MDT including trauma and orthopaedic consultants, registrars, junior doctors, anaesthetic consultants and trauma co-ordinators. Often, more members are present in the handover meeting; therefore, the handover process needs to be efficient. Previous qualitative assessments of the handover process at our institution have identified poor handover practices particularly in relation to NOF fracture and acutely unwell trauma patients.
1.2. Available knowledge
The Royal College of Surgeons’ England has set out the minimum standards for safe handover [8]; however, compliance with these standards can prove challenging. Previous studies have sought to develop standardised handover proformas in a bid to improve compliance with these guidelines [12] and in turn improving patient safety and communication amongst team members [13,14]. For example, one study by Ferran et al. [15] improved the handover of outstanding jobs from 31% to 100% using a standardised proforma in an orthopaedic department. However, implementations of proformas alone is not sufficient to guarantee effective handover of critical information. Furthermore, as members of the team change due to rotation, long-term change is difficult to maintain. This was recognised in a study by Sato and Yeung [14].
1.3. Rationale
Multiple previous qualitative assessments have been performed in the department but poor practices in handover continues that team members were still unaware of. Using the COM-B behaviour change model [16], highlighting the current shortcomings whilst also educating the team about the importance of handover would theoretically result in behaviour change.
1.4. Specific aims
The aims of this study therefore are as follows:
-
•
To assess the handover of trauma patients going to theatre, including a focus on whether relevant information was handed over from the theatre team ranging from patient's past medical history to starvation status.
-
•
To continue to assess the handover of admissions patients as per the Royal College of Surgeons' guidelines.
-
•
To examine the handover of NOF fracture patients, such as the handover of pre-operative scores and resuscitation status.
-
•
To determine if unwell patients were being handed over from the admissions list or patients already on the ward.
Our secondary aims included to determine the attendance of team members at the exact handover start time and calculating the length of the trauma and admission handovers respectively.
2. Methods
2.1. Context
The study focused on the morning weekday handover at 08:00, as the weekday meetings are busier than the weekend handover meetings and involve more team members, thereby placing our interventions under greater scrutiny. The study was performed between October and December 2019 approaching the winter months, with the intention to assess whether the effect of the intervention is maintained through busier times of the year.
2.2. Interventions
The development of a standard operating protocol (SOP) was the main intervention utilised in the study. The protocol provided information to team members with regards to how the handover meeting should be structured and reinforced key information that should be communicated in the meeting [APPENDIX 1]. The content of the protocol was developed using a combination of the Royal College of Surgeon's guidelines [8], the information submitted to the National Hip Fracture Database [17] and expert knowledge. In addition, visual aids in the form of two posters [Appendix 2, Appendix 3] created by the lead author were utilised to further assist team members in the handover process. The SOP was approved by the senior management group. This was then introduced to the team members in the form of presentations and also distributed electronically via email. The posters were then placed on the wall in the handover room to further support the SOP.
2.3. Study of the interventions
The following timeline shows the structure of the project utilising the define, measure, analyse, improve and control (DMAIC) methodology [18] for quality improvement:
2.3.1. D: Define
To identify and understand the current deficiencies in the handover process, the first cycle of data collection pre-intervention was performed for 10 consecutive morning weekday handovers.
2.3.2. M: Measure
The content of the handover was assessed utilising a handover proforma, varying from basic demographic information such as the age of the patient to the past medical history and consent, mark and starvation status. The parameters assessed were deemed to be of clinical significance as determined by the authors.
2.3.3. A: Analyse
The raw data was tabulated, and quantitative analysis was performed by two independent observers. Quantitative analysis of the data was performed independently by two authors to ensure no mistakes were made. As there were no differences in data analysis, a third independent observer was not required.
2.3.4. I: Improve
Following the first data collection cycle, the SOP was introduced, and posters were inserted in the handover room to reinforce the SOP. The information was left to circulate for four weeks in order to provide team members sufficient time to digest the information. The time period was also felt to be a more stringent test of the effectiveness of the interventions rather than performing the second data collection cycle immediately after the introduction of the interventions.
The second data collection was cycled was then performed after four weeks with eight consecutive weekday trauma meetings observed using the same method as defined in the ‘measure’ section.
2.3.5. C: Control
Following the second data collection cycle, the SOP was kept as part of the long-term plan to improve the handover process. Further suggestions, as mentioned in the ‘discussion’ section, were also implemented.
2.4. Outcome measures
The primary outcome measure was improvement in compliance with the handover SOPs. This was assessed using a handover assessment proforma [APPENDIX 4] created by the lead author. The assessment proforma consisted of a checklist of items identified as crucial to effective information transfer in the SOP. This checklist was completed by one of five independent observers who were physically present in the handover meetings. The observers assessed the content of the written and verbal handover and scored each item as ‘handed over’ or ‘not handed over’.
The secondary outcome measures included the attendance of team members and calculating the length of the handover.
2.5. Analysis
Statistical analysis was performed using SPSS version 20 (IBM; Armonk, NY). Significant differences between groups were identified by independent t-tests for continuous variables and χ2 tests for categorical variables with Fisher's exact correction if a subgroup had less than 10 data points. P values < 0.05 were considered statistically significant.
The work has been reported in line with the Standards for Quality Improvement Reporting Excellence (SQUIRE) criteria.
2.6. Ethical considerations
All of the collected patient data was anonymised. Ethical approval was gained by the local audit department at Sandwell Hospital, SWBH NHS Trust.
3. Results
3.1. Handover attendance on-time
The attendance at the exact start point of the handover meeting was recorded, as shown in Table 1. Handover attendance was greater than 75% in all groups before and after our interventions. However, despite these interventions the attendance was noted to be poor in three groups: the day admissions registrar, the trauma registrar and anaesthetic team. A small increase was seen in on-time handover attendance in the day admissions registrar and anaesthetic team groups; however, the trauma registrar attendance on-time actually halved to 50%.
Table 1.
Handover attendance of team members on time pre-intervention and post-intervention.
| Handover Team Member | Pre-Intervention Attendance on time (%) | Post-Intervention Attendance on time (%) |
|---|---|---|
| Day Admissions Consultant | 100 | 75 |
| Day Admissions Registrar | 33.3 | 62.5 |
| Trauma Consultant | 100 | 100 |
| Trauma Registrar | 100 | 50 |
| Day Senior House Officer | 100 | 87.5 |
| Day Foundation Year 1 Doctor | 90 | 75 |
| Anaesthetist | 10 | 37.5 |
| Trauma Co-Ordinator | 100 | 100 |
| Night Registrar | 90 | 100 |
| Night Foundation Year 1 Doctor | 80 | 100 |
The percentage of handovers starting on time increased slightly from 30% to 50% with an average delay of handover start time reduced by a delay of 8.7 min to 4.0 min.
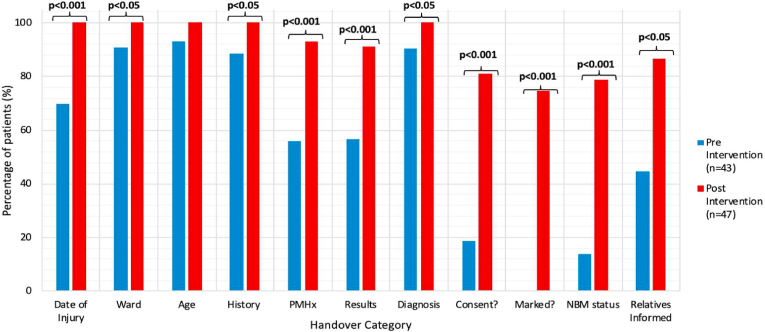
3.2. Trauma Handover
Fig. 1 summarises the results for the categories assessed in the trauma handover part of the handover meeting. 43 patients were included in the pre-intervention group and 47 patients were included in the post-intervention group. In both groups, the NOF admissions were included. In all categories assessed, the percentage of information handed over increased. This increase was statistically significant (p < 0.05) in all categories except for the handover of a patient's age. The greatest increase was shown in the handover of the consent, mark and starvation status. For example, the handover of ‘mark’ status, increased from 0% to 74% (p < 0.001).
Fig. 1.
Percentage of trauma patients in whom each item was handed over pre-intervention and post-intervention.
The length of the trauma handover increased from 19.5 min ± 5.8 min to 23.8 ± 8.4 min; however, this difference was not statistically significant (p = 0.26).
3.3. Admissions Handover
Table 2 demonstrates the categories assessed with regards to the handover of admissions patients. 146 patients were included in the pre-intervention group and 81 patients in the post-intervention group. In most categories assessed, the percentage of information handed over pre-intervention was ≥97%. After the introduction of the interventions, the percentage of information handed over increased in groups that were <97%. These groups included the handover of past medical history (84.2%–96.2%, p = 0.07), results (82.7%–96.2%, p = 0.003), diagnosis (96.6%–100%, p = 0.06) and outstanding tasks (93.8%–100%, p = 0.11).
Table 2.
A table summarising the percentage of information handed over in each handover category pre-intervention and post-intervention for admissions patients.
| Admissions Handover Category | Pre-Intervention Information Handed Over (%) | Post-Intervention Information Handed Over (%) |
|---|---|---|
| Date of Admission | 100 | 100 |
| Named Consultant | 97.9 | 100 |
| Hospital Location | 97.3 | 100 |
| Patient Identifiable Number | 100 | 100 |
| Age | 99.3 | 100 |
| Name | 100 | 100 |
| History of Injury | 97.9 | 98.8 |
| Past Medical History | 84.2 | 96.2 |
| Results | 82.7 | 96.2 |
| Diagnosis | 96.6 | 100 |
| Outstanding Tasks | 93.8 | 100 |
The length of the admissions handover increased from 19.7 ± 8.5 min to 24.3 ± 8.6 min; however, this difference was not statistically significant (p = 0.28).
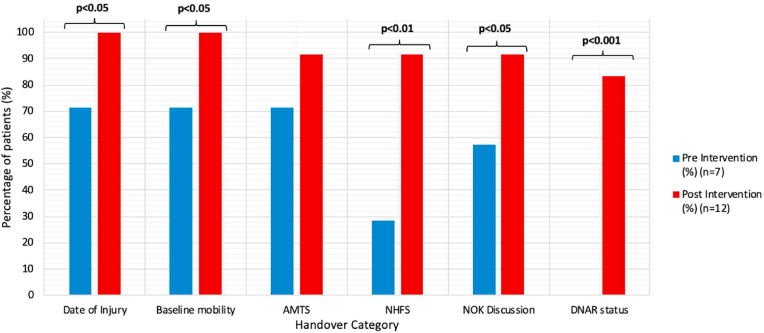
3.4. NOF handover
Fig. 2 shows the information handed over with regards to NOF patients specifically. 7 patients were included in the pre-intervention group and 12 patients were included in the post-intervention group. As shown, in all categories assessed, the percentage of information handed over increased. This increase was statistically significant in all categories except for handover of AMTS score (71.4%–91.7%, p = 0.24). The greatest increase was demonstrated in the handover of resuscitation status, which increased from 0% to 83.3% (p < 0.001).
Fig. 2.
A graph showing the percentage of information handed over for NOF patients for each NOF specific handover category pre-intervention and post-intervention.
3.5. Handover of unwell patients
The percentage of unwell patients handed over actually decreased from 80% pre-intervention to 75% post-intervention. Unwell patients were specifically asked about in handover only 10% of the time pre-intervention and 12.5% post-intervention.
3.6. Missing data
In the pre-intervention data collection, data for ‘results’ was missing for six patients in the trauma pre-intervention group with one patient's ‘diagnosis’ data missing. For the admissions pre-intervention group, data for ‘results’ was missing for seven patients with one patient's ‘diagnosis’ data missing.
For the post-intervention data collection, data for ‘past medical history’ was missing for three patients in the admissions post-intervention group with data for ‘results’ missing for three patients. For the trauma post-intervention group, data for ‘past medical history’ was missing for three patients with ‘results’ data missing for one patient and ‘diagnosis’ data missing for one patient.
4. Discussion
4.1. Summary
Our results have demonstrated that with the implementation of a SOP, reinforced by visual aids, the handover of trauma admissions and theatre lists including NOF fracture patients improved significant across all items except patient's age and cognitive status where relevant.
5. Interpretation
The handover of admissions patients continues to be successful. This is because in our department, an electronic handover proforma has already been created with headings as per the Royal College of Surgeon's guidelines [8]. Therefore, if the handover is utilised correctly and information is included for each category on the electronic handover proforma, this ensures that the information is handed over either written or verbally. However, an improvement was still demonstrated in all categories, which suggests that the implementation of the SOP helped reinforce good values and acted as a reminder for how the handover meeting should be conducted.
The total handover length increased slightly; however, this increase was not statistically significant and is a valuable trade-off for improved patient safety. Over time, with more practice and reduced delays, the authors hypothesise that the overall handover duration should decrease.
Shahrami et al. [19] introduced a handover checklist to facilitate the handover of trauma patients and reduce the numbers of missing patients from the handover meeting. Our study demonstrated some similarities; for example, both our study and this study demonstrated an improvement in the handover of the patient's ‘history’ or ‘mechanism of injury’ using our respective interventions. However, our study showed a statistically significant improvement in the handover of ‘diagnosis.’ In addition, our study focused on specifics for theatre such as ‘consent’ status and an added focus on NOF patients. To our knowledge, our study conducted is one of few studies with a focus on the handover of trauma patients and specifically NOF patients. We have created a set criterion that should be handed over for NOF patients to facilitate improved decision-making and care of NOF patients, which can be utilised by other trauma and orthopaedic departments.
From this study, we have demonstrated that clinicians want to improve the handover process, as it improves patient care. For example, for a NOF patient, having the background information including AMTS and NHFS scores helps the decision-making process, as a patient's management plan can therefore be discussed in the handover. This therefore improves patient-specific care but also can help facilitate teaching and discussion. Although there was no data collected to substantiate these claims, informal feedback from colleagues has suggested that these interventions have helped improved satisfaction amongst those attending the handover and has promoted patient-centered care.
Despite the overwhelming positive results, there were some differences between our observed and anticipated outcomes. Overall our results showed that unwell patients were not being handed over. This is perhaps because there was no set criterion for what an ‘unwell’ patient was; the definition for an ‘unwell’ patient therefore varied between observers. For example, some observers felt that an ‘unwell’ patient was anyone deteriorating on early warning scores; however, for others it was a patient for whom there was a clinical concern even if the observations were normal. Despite this, our results suggest that if there are no ‘unwell’ patients, this is also not being mentioned. In addition, attendance on time varied significantly between groups, although it must be acknowledged that extenuating circumstances may result in delays and attendance. Despite this, the full results regarding the handover attendance were not presented to colleagues to demonstrate the punctuality differences of different groups. Having presented the full results to colleagues within the department and highlighting these deficiencies in attendance on time, theoretically this should improve in the future.
6. Limitations
There were three limitations that were identified from the study: the generalisability of the data, blinding and only two data collection cycles being completed. The generalisability of the data can be questioned for larger teaching hospitals. Our study was performed in a district general hospital and larger hospitals may have a different structure for their handover meeting in line with their hospital structure and patient population. Therefore, these hospitals not be able to implement our structure to the handover meeting. In addition, due to the low number of NOF patients included in the study with 19 in total, the validity of our conclusions may be questioned. However, the improvements were still statistically significant and therefore suggests our interventions will be successful for other hospitals. Due to the nature of the study, blinding was difficult to perform as one data observer was present in each handover meeting that was not part of the immediate team. Therefore, the study could have been impacted by the Hawthorne effect. However, steps had been taken to minimise this as mentioned earlier such as having only one observer present. Only two data collection cycles were performed for this study; however, this study was deemed as an additional study to the previous work performed at the hospital and the aim will be to perform a further cycle in 12–24 months to assess whether a long-term impact has been achieved.
Missing data points were also present in this study. However, the fast speed of the handover meeting due to the volume of patients meant that occasionally, data was missed. In addition, having two data collectors would have minimised missing these data points. However, limited observers were available, and the handover room can only fit 10 to 15 people; therefore, the risk of the Hawthorne effect with having two observers present as compared to one would have been greater. On balance therefore it was deemed that one observer would be satisfactory. Furthermore, only 8 handover meetings were observed in the post-intervention group and similarly this was due to the limited number of observers available. Replication of the data in future could be hindered if the standards of team members slip; this will be minimised if senior staff commit to the changes to facilitate long-term change.
The assessment proforma was deemed to be a simple and cost-effective method to evaluate the handover process. In addition, as the project was conducted across multiple weekday meetings, different team members would be present on different days; therefore, any conclusions drawn from the study could assume that uniform change was implemented across the department.
7. Conclusions
Our results demonstrate that the introduction of a well-structured SOP is an effective method to improve the transmission of information during trauma meetings, thereby improving surgical decision-making and overall patient care. Future data collection cycles will be required in the next 24 months to help facilitate long-term change. The SOP can be utilised by other district general hospitals in other orthopaedic departments to help structure their handover meetings.
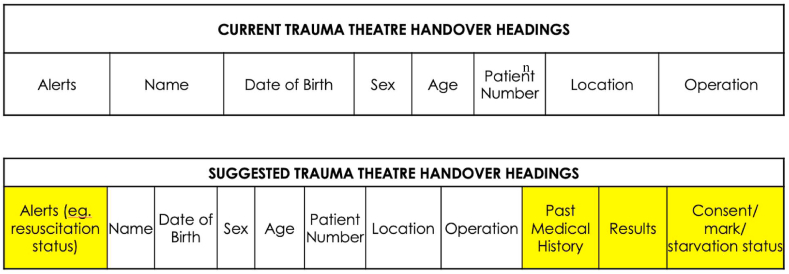
Future work will include a new structure for the electronic handover sheet for the trauma handover as demonstrated in Fig. 3, as the use of a similar structure in the admissions handover proforma sheet has been highly effective. A checklist will be implemented for future handover meetings [APPENDIX 5]; this will help ensure that ‘unwell’ patients are included in each handover meeting and the checklist will reinforce the SOP further. Following on from previous studies, the next data collection cycle will include questionnaires to include qualitative data to assess the satisfaction within the surgical team.
Fig. 3.
A comparison between the headings included in the current handover of trauma patients going to theatre and the suggested new highlighted headings.
Funding
No funding was obtained for this study. Only the listed authors were involved in the design of the study, the data collection, the interpretation of the data and the decision to submit for publication.
CRediT authorship contribution statement
Salman Sadiq: Conceptualization, Methodology, Validation, Formal analysis, Investigation, Resources, Writing - original draft, Visualization, Project administration. Muaaz Tahir: Conceptualization, Methodology, Investigation, Resources, Writing - review & editing, Supervision, Project administration. Intesar Nur: Investigation, Resources, Writing - original draft. Diya Baker: Investigation. Sherif Elerian: Investigation. Angus Bruce: Investigation, Writing - review & editing. Atul Malik: Conceptualization, Writing - review & editing, Supervision, Project administration.
Declaration of competing interest
The authors declare that there are no conflicts of interest.
Acknowledgements
We would like to thank the trauma and orthopaedics department at Sandwell Hospital, SWBH NHS Trust, for allowing us to conduct the study.
APPENDIX
Appendix 1. The standard operating protocol (SOP) utilised as the primary intervention to improve the handover of trauma and orthopaedic patients
STANDARD OPERATING PROTOCOL FOR TRAUMA HANDOVER - SANDWELL HOSPITAL, SWBH NHS TRUST.
THE GOLDEN PATIENTS.
-
1.
The Golden patient will have to be decided before the end of the operating session on the prior day by the on-call consultant or the trauma consultant. This will be communicated to the theatre team and the anaesthetist for the following day.
-
2.
The day on-call registrar would let the on-call team and the trauma team know if there were to be a change in the Golden patient before he hands over at 8pm.
-
3.
If the night registrar where to decide to change the Golden patient, he would communicate this with the on-call between 7 and 8 before the beginning of the trauma meeting.
THE HANDOVER.
-
1.
The trauma handover would begin at 8am.
-
2.The trauma handover would be divided into 3 parts:
-
(a)Handover of theatre patients.
-
(b)Handover of the night take.
-
(c)Handover of any acutely deteriorated patients overnight. Any mortality or post-op complications ie; infection.
-
(a)
-
3.
The trauma handover would be attended by the day on-call team, the trauma theatre team, the night registrar, the theatre team and the trauma anaesthetist.
The first part of the meeting would consist of discussion of patients who are on the Trauma list. The handover would consist of adequate history and clinical examination, relevant aspects of consenting, marking, discussion with the patients and relatives where appropriate, DNACPR where relevant. Following this handover, the trauma team would depart to review these patients.
-
4.
The second part of the handover would consist of the intake from the previous night, which would be handed over by the night on-call registrar detailing all the findings of these patients.
-
5.
The final handover part would consist of any acutely deteriorated patients, post-operative complications and any mortality overnight.
PRE-OPERATIVE CHECK.
Confirmation of trauma list:
-
1.
the trauma team would return back from their ward round between 8.30 and 8.40 to hand over a signed list to the SCP's to confirm the order of the side and the procedure to the SCP's to formulate a final list. The final list would be handed over to the theatre team and anaesthetist before the beginning of the team brief for the trauma theatre.
Appendix 2. Handover Protocol Poster 1 - Summary of SOP
HANDOVER PROTOCOL (1)
For ALL patients going to theatre, ensure the following is handed over:
-
•
Golden Patient
-
•
Date of injury AND mechanism of injury
-
•
Past Medical History
-
•
Examination findings
-
•
Investigation results
-
•
Consent status
-
•
Mark status
-
•
Starvation status
-
•
Discussion with relatives if appropriate
Appendix 3. Handover Protocol Poster 2 - Summary of SOP
HANDOVER PROTOCOL (2)
For ALL NOF patients, ensure the following is ALSO handed over:
-
•
Date of Injury
-
•
Baseline Mobility
-
•
AMTS AND NHFS
-
•
NOK discussion
-
•
Resuscitation status
Other Handover Tips.
-
•
Ensure handover starts at 08:00
-
•
Night team please handover any: unwell patients, mortalities, post-operative complications
Appendix 4. Handover Proforma used for Data Collection
HANDOVER QIP PROFORMA DATA COLLECTION.
DATE:
CONSULTANT:
-
(1a)
AT EXACTLY 08:00, WHO IS PRESENT FROM THE FOLLOWING:
| Member of Staff | Present? (tick) | |
|---|---|---|
| DAY TEAM | On-Call Admissions Consultant | |
| On-Call Admissions Registrar | ||
| Trauma Consultant | ||
| Trauma Registrar | ||
| SHO | ||
| FY1 | ||
| Anaesthetist- Consultant or Registrar | ||
| Trauma Co-Ordinator | ||
| NIGHT TEAM | Night Registrar | |
| Night FY1 |
-
(1b)AT 08:00
-
•Did handover start at exactly 08:00?
-
•
If not, state at what time handover officially started:
-
(2a)
TRAUMA HANDOVER - note start time + tick if present (either written/verbally)
| Date of Admission | Consultant | Ward | Patient Identifiable Number | Age | Name | History of Injury | |
|---|---|---|---|---|---|---|---|
| Case 1 | |||||||
| Case 2 | |||||||
| Case 3 | |||||||
| Case 4 | |||||||
| Case 5 | |||||||
| Case 6 |
| Past Medical History | Results | Diagnosis | Pending investigations | If Pending Investigations - Are They Requested? | Consent? | Marked? | Starvation status? | If appropriate, have relatives been informed? | |
|---|---|---|---|---|---|---|---|---|---|
| Case 1 | |||||||||
| Case 2 | |||||||||
| Case 3 | |||||||||
| Case 4 | |||||||||
| Case 5 | |||||||||
| Case 6 |
| If unwell, mention of general clinical status? | If unwell, is resuscitation plan mentioned? | If NO for any of these questions, have reasons been stated why? | |
|---|---|---|---|
| Case 1 | |||
| Case 2 | |||
| Case 3 | |||
| Case 4 | |||
| Case 5 | |||
| Case 6 |
| NECK OF FEMUR FRACTURE SPECIFIC | ||||||
|---|---|---|---|---|---|---|
| Case No. | Date of Injury | Baseline mobility | AMTS | NHFS | Next of Kin discussion | Resuscitation status |
| Case 1 | ||||||
| Case 2 | ||||||
| Case 3 | ||||||
| Case 4 | ||||||
| Case 5 | ||||||
-
(2b)
How long did the trauma handover take (to closest minute):
-
(3a)
ADMISSIONS HANDOVER - note start time + tick if present (either written/verbally)
| Date of Admission | Consultant | Ward | Bed number | Patient Identifiable Number | Age | Name | History/Exam Findings | Past Medical History | Results | |
|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | ||||||||||
| Case 2 | ||||||||||
| Case 3 | ||||||||||
| Case 4 | ||||||||||
| Case 5 | ||||||||||
| Case 6 | ||||||||||
| Case 7 | ||||||||||
| Case 8 | ||||||||||
| Case 9 | ||||||||||
| Case 10 |
| Diagnosis | If unwell, is there a mention of general clinical status? (eg.stable/unstable) | If unwell, is resuscitation plan mentioned? | Pending investigations | |
|---|---|---|---|---|
| Case 1 | ||||
| Case 2 | ||||
| Case 3 | ||||
| Case 4 | ||||
| Case 5 | ||||
| Case 6 | ||||
| Case 7 | ||||
| Case 8 | ||||
| Case 9 | ||||
| Case 10 |
-
(3b)
How long did the admissions handover take (to the closest minute):
-
(4)AFTER MAIN HANDOVER
-
•Is a question asked about whether there are any unwell patients overnight/currently under T + O care?
-
•
Appendix 5. A Proposed Handover Checklist for the handover of Trauma and Orthopaedic patients
HANDOVER CHECKLIST.
At 08:00:
| Member of Staff | Present? | |
|---|---|---|
| DAY TEAM | On-Call Admissions Consultant | |
| On-Call Admissions Registrar | ||
| Trauma Consultant | ||
| Trauma Registrar | ||
| Senior House Officer | ||
| Foundation Year 1 Doctor | ||
| Anaesthetist- Consultant or Registrar | ||
| Trauma Co-Ordinator | ||
| NIGHT TEAM | Night Registrar | |
| Night Foundation Year 1 Doctor |
Everyone should introduce themselves.
08:00–08:10 Trauma Handover including:
-
-
Consent status.
-
-
Mark status.
-
-
Starvation status.
-
-
Resuscitation status.
-
-
Next of kin informed?
-
-
For NOF patients include date of injury, baseline mobility, AMTS, NHFS
08:10–08:40 Admissions Handover.
08:40–09:00 Any unwell patients on the ward either overnight or currently under Trauma & Orthopaedics care?
Any post-operative complications or mortalities overnight?
Handover any other tasks to relevant team members.
Handover Bleeps.
On-Call Admissions Consultant to prioritise tasks.
References
- 1.handover Safe. Safe patients Guidance on clinical handover for clinicians and managers. https://www.rcpch.ac.uk/sites/default/files/2018-02/bma_handover_college_tutors.pdf (acccessed June 28, 2020)
- 2.McFarlane A. The impact of standardised perioperative handover protocols. J. Perioperat. Pract. 2018;28:258–262. doi: 10.1177/1750458918775555. [DOI] [PubMed] [Google Scholar]
- 3.Philibert I., Barach P. The European HANDOVER Project: a multi-nation program to improve transitions at the primary care - inpatient interface. BMJ Qual. Saf. 2012;21 doi: 10.1136/bmjqs-2012-001598. [DOI] [PubMed] [Google Scholar]
- 4.Acute care toolkit 1: handover - RCP london. https://www.rcplondon.ac.uk/guidelines-policy/acute-care-toolkit-1-handover (accessed June 28, 2020)
- 5.Gruen R.L., Jurkovich G.J., McIntyre L.K., Foy H.M., Maier R.V. Patterns of errors contributing to trauma mortality: lessons learned from 2594 deaths. Ann. Surg. 2006;244:371–378. doi: 10.1097/01.sla.0000234655.83517.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doctors and the European working time directive. https://www.bma.org.uk/pay-and-contracts/working-hours/european-working-time-directive-ewtd/doctors-and-the-european-working-time-directive (accessed June 28, 2020)
- 7.Birks Y., Aspinal F., Bloor K. 2018. Understanding the Drivers of Litigation in Health Services. [Google Scholar]
- 8.Handover Safe. The Royal College of Surgeons of England; 2007. Guidance from the Working Time Directive Working Party.https://www.rcseng.ac.uk/search/#SearchTerm=handover (accessed June 28, 2020) [Google Scholar]
- 9.Wiles M.D., Moran C.G., SahotaI O., Moppett K. Nottingham Hip Fracture Score as a predictor of one year mortality in patients undergoing surgical repair of fractured neck of femur. Br. J. Anaesth. 2011;106(4) doi: 10.1093/bja/aeq405. https://bjanaesthesia.org/article/S0007-0912(17)33250-6/abstract [DOI] [PubMed] [Google Scholar]
- 10.National Institute For Health And Clinical Excellence Guideline title Hip fracture: the management of hip fracture in adults. 2009. www.sign.ac.uk/guidelines/fulltext/56/index.html
- 11.About Us (removed detail for manuscript).
- 12.Din N., Ghaderi S., O'Connell R., Johnson T. Strengthening surgical handover: developing and evaluating the effectiveness of a handover tool to improve patient safety. BMJ Qual. Improv. Reports. 2012;1 doi: 10.1136/bmjquality.u492.w164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones H.G., Watt B., Lewis L., Chaku S. Structured handover in general surgery: an audit of current practice. J. Patient Saf. 2019;15:7–10. doi: 10.1097/PTS.0000000000000201. [DOI] [PubMed] [Google Scholar]
- 14.Sato T., Yeung E. Handover practice in acute surgical admissions. Bull. Roy. Coll. Surg. Engl. 2014;96:150–152. doi: 10.1308/rcsbull.2014.96.5.150. [DOI] [Google Scholar]
- 15.Ferran N.A., Metcalfe A.J., O'Doherty D. Standardised proformas improve patient handover: audit of trauma handover practice. Patient Saf. Surg. 2008;2:24. doi: 10.1186/1754-9493-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The COM-B theory of change model (V3) https://www.researchgate.net/publication/314086441_The_COM-B_Theory_of_Change_Model_V3 (n.d.) (accessed June 28, 2020)
- 17.NHFD 2019 annual report. https://www.nhfd.co.uk/20/hipfractureR.nsf/docs/2019Report
- 18.University of Bedfordshire . DMAIC Model; 2020. The Lean Six Sigma Company.https://www.theleansixsigmacompany.co.uk/dmaic-model/ [Google Scholar]
- 19.Shahrami A., Nazemi-Rafi M., Hatamabadi H., Amini A., Haji Aghajani M. Impact of education on trauma patients' handover quality; a before-after trial. Arch. Acad. Emerg. Med. 2019;7:e7. http://www.ncbi.nlm.nih.gov/pubmed/30847442 [PMC free article] [PubMed] [Google Scholar]