Abstract
The mental health problems might have been increased owing to the COVID-19 pandemic with the commencement of the year 2020, therefore, an epidemiological survey appraising the burden of mental health issues among the general population is imperative. This cross-sectional study attempts to reveal the underlying mental health conditions, such as Post-Traumatic Stress Symptoms (PTSS), depression, and insomnia, relating to the pandemic situation, and to further examine the combined effects of gender and age on the COVID-19 related mental health consequences. An online survey was conducted among 2,992 adults in China from February 1st 2020 to February 10th 2020. The study uses binary logistic regression to analyze the potential factors associated with PTSD, depression, and insomnia. The results indicate that the prevalence of PTSS, depression, and insomnia are 19.5, 26.9, and 19.6% respectively during the COVID-19. Men and women show different rates of PTSS and depression, whereas no insomnia is found in both males and females. The females above 50 years of age have a lower level of depressive symptoms (OR = 0.448, 95%CI: 0.220–0.911, Cohen's d = −0.443) as compared with females aged 18–25; while the highest effect sizes for PTSS (OR = 2.846, 95%CI: 1.725–4.695, Cohen's d = 0.537) and the depression (OR = 2.024, 95%CI: 1.317–3.111, Cohen's d = 0.314) are seen in males aged 26 to 30. Besides gender, education, living conditions, direct exposure to COVID-19, the post mental and the physical health condition is related to PTSS, depression, and insomnia. Our study suggests that high-risk groups, especially those having two or more related factors and young men, should be the focus of mental health intervention.
Keywords: PTSD, depression, insomnia, age, gender, China
Introduction
Detected by the end of 2019, Corona Virus Disease, known as COVID-19, has become a global pandemic now after affecting millions of people worldwide. The outbreak and the spread of COVID-19 caused multiple challenges relating not only to political management, economic growth, and healthcare delivery on the macro-level but also to the psychological well-being of individuals (1, 2).
Recently, anxiety, depression, insomnia, denial, anger, and fear among medical workers in Wuhan can be observed, associated with excessive work burden and intensive dangers of contagious infection (3, 4). However, as a new form of a stressor for mental health (5), the COVID-19 pandemic affects populations beyond healthcare workers. Unlike natural disasters that have specific regional impacts in a given time (6), the impact of this global crisis is profound and lasting. The social risks in the COVID-19 pandemic are not as recognizable as those in wars or international mass conflicts (7). One meta-analysis study suggests over one-in-five people experienced post-traumatic stress symptoms (PTSS) and psychological stress (8). Another systematic review indicates that the general population in many countries reported a relatively high prevalence of depression, posttraumatic stress disorder, psychological distress during the COVID-19 pandemic (9). Thus, it is rational to assume that this epidemic is sweeping across the population, and an epidemiological survey of the general population is essential for evaluating the actual mental health burden of the COVID-19 crisis.
For mental health studies, gender and age are primarily considered as demographic variables and get less attention as such. Neither gender nor age is the main area to focus on within most mental health studies. As early as Freud, gender differences were recognized in mental health because women were believed to be stunted in both ego and superego development, further resulting in passivity as a gender characteristic (10). This idea was later criticized by Rosenfield and Smith, claiming that there were no differences in the overall rates of psychopathy between genders, but admitted that males and females differ in the type of psychopathology experiences (11). Females develop more internalizing disorders, even though they are less subjected to potentially traumatic events (12). However, male counterparts have higher rates of externalizing problems. The variation in the extent of gender differences on mental health varies between trauma types (13). However, it should be noted that the evidence during the pandemic context is lacking.
Moreover, as noted by gender-roles theory, males and females show differences in the age distribution of mental health issues during their life course (14). Additionally, gender is found to be a significant biomarker of brain development and behavioral development throughout the lifespan so that it has further interactions with the mental health of individuals (15). But, how exactly gender and age affect mental health under traumatic circumstances is not clear. Taking post-traumatic stress disorder (PTSD) as an internalizing disorder, Kessler's study demonstrates that there is no age difference for men across age groups, despite a tendency for PTSD symptoms to decline as women get older (16). On the contrary, another study suggests that females of 25–35 and males between 45 and 55 years might suffer the highest level of PTSS (17), possibly due to changes in sympathetic or noradrenergic systems (18). Besides, the study of Norris shows that women aged between 55 and 64 years old are most possibly to suffer PTSD symptoms (19). Some other studies claim that it is more likely for individuals aged between 18 and 24 years to get PTSD symptoms (20). The inconsistency in these studies could be attributed to methodological or cultural differences, and this situation, therefore, suggests urgency for more evidence highlighting how epidemics in a social setting may affect the mental health risk evaluation as an important factor.
Influenced by ancient Confucian traditions and current market expansion, “males are considered the main breadwinners while females are the primary caretakers” in China (21). Chinese men as the primary supporter for the family may undergo more stress facing higher psychological symptoms owing to the economic ebb and the higher COVID-19 related mortality rate (22). According to the life course theory, there is an inverted U-shape between mental health symptoms and age. The highest symptoms may be in young adulthood and decrease after midlife (23). The stress about the job, parenting young children, and marriage is very common in early adulthood but it diminishes with time, however, health problems are a major cause of stress in late adulthood (24). Therefore, Chinese young adults with jobs and married status may have the highest psychological symptoms during the pandemic. Combining the gender role theory and life course theory, we expect that young males may have higher financial stress regarding supporting their family as compared with young females.
During the COVID-19 crisis, especially with social distancing measures and policies to slow the spreading speed, PTSD, depression, and insomnia are the three most prevalent psychiatric disorders affecting the individuals' mental health (25, 26). In addition to gender and age relationship with PTSS, depression, and insomnia, previous studies on pandemics have found other potential factors including the personal characteristics, the traumatic exposure, the individuals' physical health and the psychological states, and so on (9). However, the significance of those factors varies in different psychiatric studies. One study estimates the prevalence of PTSD which is 7% in COVID-19 hard-hit areas in China, while gender, exposure history, and sleep quality also matter (27). Other studies suggest a 16.5–17.7% prevalence of depression, while the predictions from gender, age, educational levels, and professions are significant (28, 29). However, none of these studies focus on the related factors of PTSS, depression, insomnia simultaneously. To identify the shared factors and the specific factors of PTSS, depression, and insomnia, this study, therefore, attempts to discuss three typical symptoms in unison to allocate the limited resources more effectively.
For the reasons discussed above, the objectives of this study are (1) to estimate the prevalence of PTSD symptoms, depression, and insomnia among the general population during the COVID-19 outbreak; (2) to examine the combined effect of gender and age on PTSD symptoms, depression, and insomnia respectively; (3) to figure out the shared factors and the specific factors which are associated with PTSS, depression, and insomnia. Based on the reviewed literature, three hypotheses are proposed for the current study. First, we expected that males may have higher symptoms of PTSD, depression, and insomnia than females in china during the COVID-19 outbreak. Second, we assumed that young adults may experience higher PTSS, depression, and insomnia symptoms. Third, we proposed that age may have a significant interaction effect with the gender on PTSS, depression, and insomnia. Lastly, we expected that there exist other factors like the living conditions, the direct exposure to COVID-19, the post mental, and the physical health condition associated with PTSS, depression, and insomnia.
Methods
Data Source, Procedure, and Participants
This survey was conducted online from February 1st to February 10th in 2020, and all questionnaires were given out and retrieved through a web-based platform (https://www.wjx.cn/app/survey.aspx). In total, 2,992 participants across 31 Chines provinces participated in the survey. A snowball sampling was used to select participants and Chinese citizens aged ≥ 18 years old were invited. To reach more subjects from groups with high exposure to COVID-19 and low social-economic status, we sent out questionnaires to some specific citizens. After excluding 134 questionnaires of low quality (excluding criteria including finishing in shorter than 10 min or having some logical problem et al.), we finally got 2,858 subjects, including medical workers (N = 421, 14.7%), nonprofessional employees (N = 259, 9.1%), social service workers (N = 230, 8.0%), teachers and faculties (N = 648, 22.7%), workers and farmers (N = 388, 13.6%), students (N = 424, 14.8%), unemployed and others (N = 488, 17.1%). All participants gave their consent and joined this research voluntarily after being informed about the nature of the study. This study was approved by the Ethics Committee of the Peking University Medical Center.
Measures
Depression was assessed with the help of a 20-item scale used by the Center for Epidemiological Studies Depression (CESD) to measure depressive symptoms in the general population (30). Previous studies have proved that this scale has high reliability and validity among Chinese (31). Respondents reported the frequency of each symptoms item on a four-point scale: 0 (rarely or none of the time; <1 day), 1 (some of the time; 1–2 days), 2 (much or a moderate amount of the time; 3–4 days), or 3 (most or all of the time; 5–7 days). The total score ranges from 0 to 60, with a higher score indicating a higher level of depressive symptoms. With a cut-off point at 21, respondents were divided into two categories, “depressed” or “no depressive symptoms.” Cronbach's alpha was 0.93 in this study.
PTSS was assessed by a 20-item self-report PCL-5 (PTSD Checklist for DSM-5) scale, estimating the degree to which individuals have been disturbed in the past month using PTSD symptoms (32). Respondents answered 20 items on a four-point scale rating from 0 (not at all) to 4 (extremely). Items were summed for a total score ranging from 0 to 80, with higher scores indicating a higher level of PTSS. Each item rated at least 2 (moderate) could be regarded as PTSD symptoms. And 20 items were divided into four DSM-5 PTSD symptoms clusters: intrusions (items 1–5), avoidance (items 6–7), negative alterations in mood and cognition (items 8–14), alterations in reactivity, and arousal (items 15–20). The diagnostic criteria of DSM-5 required at least 1 “intrusions-symptom,” 1 “avoidance-symptom,” 2 “negative alterations in the mood and the cognition-symptoms,” and 2 “alterations in reactivity and arousal-symptoms.” The Cronbach's alpha was 0.97 in this study.
Insomnia was estimated with The Pittsburgh Sleep Quality Index (PSQI) (33). The PSQI (Chinese Version) was translated and validated by Liu and associates (34). The PSQI is constitutive of 19 self-reported items including various factors about sleep quality consisting of estimation of sleep latency, duration, disturbances, and the severity and frequency of other sleep problems. The total PSQI scale is grouped into seven 0–3 subscales, with the total score ranging from 0 to 21 and higher scores indicating worse sleep quality. With a cut-off point at 7, respondents were divided into two categories, “insomnia” or “no insomnia.” The Cronbach's alpha in this study was 0.86.
Exposure items included Wuhan exposure (“1” refers to lived or had Wuhan travel history, “0” refers to none Wuhan travel history), prior exposure (yes, no), media exposure (frequently, sometimes, less, very less), impact on livelihood (none, some, relatively large, very large) and direct exposure to COVID-19 (“1” includes self, family, friend, and neighborhood exposure to COVID-19, “0” refers to none exposure).
Gender in this study was divided into males and females, and age was categorized as 18–25, 26–30, 31–40, 41–50, 51, and over comprehensively considering the basic age distribution and the internal variation between age groups. Also, socioeconomic covariates in this study include ethnicity (Han, else), marriage (have no spouse, have a spouse), education (junior high school and below, high school/technical school, junior college, undergraduate, postgraduate and above), job (medical workers, nonprofessional employees, social service workers, teachers and operators, students, workers and farmers, unemployed and others) and income (poor, not poor). Health-related variables contained prior and post psychological problems (yes, no), chronic diseases (yes, no), and 2-week illness (yes, no). These variables are included in the study according to previous studies (23, 24).
Statistical Analyses
Descriptive analysis was conducted to describe the characteristics of the sample. In the analyses, PTSS, depression, and insomnia were used as binary variables. χ2 or t-test was used to examine the binary correlation between independent variables with PTSS, depression, insomnia respectively. Then, three logistic regression models were used to examine the factors linked to PTSS, depression, and insomnia. Finally, another two logistic regression models were designed to examine the combined effect of gender and age on PTSS and depression. All potentially confounding variables including socio-demographic variables (consisted of ethnicity, marriage, education, job, and income), health-related factors (contained prior and post psychological problems, chronic diseases, and 2-week illness), were controlled in the above models. We set the alpha at 0.05 for statistical significance in all the tests. SPSS 22.0 was used to carry out these analyses.
Results
Descriptive Analyses
As shown in Table 1, about 95.8% of the total 2,858 participants belong to the Han ethnicity, and the proportion of men and women is nearly equal (46.4% as male and 53.6% as female). The distribution of age groups is presented as following: participants aged 31–40 years constitute the most (about 31.2%), followed by those aged 18–25 years (about 24.2%), aged 26–30 years (about 22.6%), and aged 41–50 years (about 14.0%); participants above 50 years of age contribute to merely 8.1% of the sample. Besides, 60.2% of the participants are married and nearly 60% of them are well-educated (undergraduate or above). When it comes to the traumatic exposure, there are 85.5% of participants considering themselves as being free of the Wuhan exposure and about 92.1% of the samples are out of prior traumatic exposures. However, nearly 83% of the participants are under indirect exposure to COVID-19, occasionally or frequently through media in particular. In general, the health condition of most participants is good, as the proportion for participants having the prior psychological problem, the post psychological problem, the chronic diseases, and the 2-week illness are 14.6, 29, 12, and 7% respectively. More detailed, among all 2,858 participants, 19.5% are found of PTSS, 26.9% of depression, and 19.6% of insomnia. More details could be seen in Table 1.
Table 1.
Descriptive analysis of sample characteristics.
| Total | Male | Female | P-value | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| PTSS | p < 0.001 | ||||||
| Yes | 558 | 19.5 | 334 | 25.2 | 224 | 14.6 | |
| No | 2,300 | 80.5 | 992 | 74.8 | 1,308 | 85.4 | |
| Depression | p < 0.001 | ||||||
| <21 | 2,088 | 73.1 | 897 | 67.6 | 1,191 | 77.7 | |
| ≥21 | 770 | 26.9 | 429 | 32.4 | 341 | 22.3 | |
| Sleep quality | 0.001 | ||||||
| ≤7 | 2,297 | 80.4 | 1,030 | 77.7 | 1,267 | 82.7 | |
| >7 | 561 | 19.6 | 296 | 22.3 | 265 | 17.3 | |
| Ethnicity | 0.070 | ||||||
| Han | 2,738 | 95.8 | 1,280 | 96.5 | 1,458 | 95.2 | |
| Else | 120 | 4.2 | 46 | 3.5 | 74 | 4.8 | |
| Gender | |||||||
| Male | 1,326 | 46.4 | |||||
| Female | 1,532 | 53.6 | |||||
| Age | 0.027 | ||||||
| 18–25 | 691 | 24.2 | 309 | 23.3 | 382 | 24.9 | |
| 26–30 | 645 | 22.6 | 272 | 20.5 | 373 | 24.3 | |
| 31–40 | 891 | 31.2 | 425 | 32.1 | 466 | 30.4 | |
| 41–50 | 400 | 14.0 | 200 | 15.1 | 200 | 13.1 | |
| ≥51 | 231 | 8.1 | 120 | 9.0 | 111 | 7.2 | |
| Marriage | 0.672 | ||||||
| Not have a spouse | 1,137 | 39.8 | 552 | 41.6 | 615 | 40.1 | |
| Have a spouse | 1,721 | 60.2 | 804 | 60.6 | 917 | 59.9 | |
| Education | p < 0.001 | ||||||
| Junior high school and below | 268 | 9.4 | 127 | 9.6 | 141 | 9.2 | |
| High school/Technical school | 387 | 13.5 | 231 | 17.4 | 156 | 10.2 | |
| Junior College | 488 | 17.1 | 247 | 18.6 | 241 | 15.7 | |
| Undergraduate | 1,257 | 44.0 | 559 | 42.2 | 698 | 45.6 | |
| Postgraduate and above | 458 | 16.0 | 162 | 12.2 | 296 | 19.3 | |
| Job | p < 0.001 | ||||||
| Medical workers | 421 | 14.7 | 88 | 6.6 | 333 | 21.7 | |
| Nonprofessional employees | 259 | 9.1 | 174 | 13.1 | 85 | 5.5 | |
| Social service workers | 230 | 8.0 | 129 | 9.7 | 101 | 6.6 | |
| Teachers and operators | 648 | 22.7 | 304 | 22.9 | 344 | 22.5 | |
| Students | 424 | 14.8 | 169 | 12.7 | 255 | 16.6 | |
| Workers and farmers | 388 | 13.6 | 244 | 18.4 | 144 | 9.4 | |
| Unemployed and others | 488 | 17.1 | 218 | 16.4 | 270 | 17.6 | |
| Income | p < 0.001 | ||||||
| Poor | 327 | 11.4 | 200 | 15.1 | 127 | 8.3 | |
| Not poor | 2,531 | 88.6 | 1,126 | 84.9 | 1,405 | 91.7 | |
| Wuhan exposure | 0.002 | ||||||
| Yes | 413 | 14.5 | 163 | 12.3 | 250 | 16.3 | |
| No | 2,445 | 85.5 | 1,163 | 87.7 | 1,282 | 83.7 | |
| Impact on livelihood | 0.055 | ||||||
| None | 825 | 28.9 | 358 | 27.0 | 467 | 30.5 | |
| Some | 975 | 34.1 | 454 | 34.2 | 521 | 34.0 | |
| Relatively large | 611 | 21.4 | 284 | 21.4 | 327 | 21.3 | |
| Very large | 447 | 15.6 | 230 | 17.3 | 217 | 14.2 | |
| Prior exposure | 0.229 | ||||||
| Yes | 227 | 7.9 | 114 | 8.6 | 113 | 7.4 | |
| No | 2,631 | 92.1 | 1,212 | 91.4 | 1,419 | 92.6 | |
| Media exposure | 0.125 | ||||||
| Frequently | 1,608 | 56.3 | 759 | 57.2 | 849 | 55.4 | |
| Sometimes | 762 | 26.7 | 328 | 24.7 | 434 | 28.3 | |
| Less | 259 | 9.1 | 131 | 9.9 | 128 | 8.4 | |
| Very less | 229 | 8.0 | 108 | 8.1 | 121 | 7.9 | |
| Prior psychological problems | 0.292 | ||||||
| Yes | 418 | 14.6 | 184 | 13.9 | 234 | 15.3 | |
| No | 2,440 | 85.4 | 1,142 | 86.1 | 1,298 | 84.7 | |
| Post psychological problems | 0.003 | ||||||
| Yes | 828 | 29.0 | 348 | 26.2 | 480 | 31.3 | |
| No | 2,030 | 71.0 | 978 | 73.8 | 1,052 | 68.7 | |
| Chronic disease | 0.701 | ||||||
| Yes | 342 | 12.0 | 162 | 12.2 | 180 | 11.7 | |
| No | 2,516 | 88.0 | 1,164 | 87.8 | 1,352 | 88.3 | |
| Two-week illness | 0.359 | ||||||
| Yes | 201 | 7.0 | 87 | 6.6 | 114 | 7.4 | |
| No | 2,657 | 93.0 | 1,239 | 93.4 | 1,418 | 92.6 | |
| Mean | SD | Mean | SD | Mean | SD | ||
| Direct exposure | 0.6 | 1.2 | 0.5 | 1.1 | 0.6 | 1.3 | 0.035 |
To identify possible factors associated with mental disorders, this study further conducts binary analysis, where results are presented in Table 2. Findings indicated that PTSS, depression, and insomnia share some factors in common, including gender, age, education, profession, income, psychological health conditions, and the 2-week illness, as well as impacts of COVID-19 on livelihood and traumatic exposure experiences. However, there are some characteristics with partial significance. For example, the different marital status affects PTSS and insomnia only, and suffering from chronic diseases is related only to higher depressive symptoms. Also, people who live in Wuhan or even have been to Wuhan within 2 weeks before the outbreak of COVID-19 would reflect the higher level of insomnia, but prior exposure experiences are insignificantly related. More details are presented in Table 2.
Table 2.
Binary correlations of risk factors with PTSS, depression, sleep quality.
| PTSS N (%) | Depression N (%) | Insomnia N (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | P-value | Yes | No | P-value | >7 | ≤7 | P-value | |
| Ethnicity | |||||||||
| Han | 538 (19.6) | 2,200 (80.4) | 0.420 | 739 (27.0) | 1,999 (73.0) | 0.780 | 538 (19.6) | 2,200 (80.4) | 0.896 |
| Else | 20 (16.7) | 100 (83.3) | 31 (25.8) | 89 (74.2) | 23 (19.2) | 97 (80.8) | |||
| Gender | |||||||||
| Male | 334 (25.2) | 992 (74.8) | p < 0.001 | 429 (32.4) | 897 (67.6) | p < 0.001 | 296 (22.3) | 1,030 (77.7) | 0.001 |
| Female | 224 (14.6) | 1,308 (85.4) | 341 (22.3) | 1,191 (77.7) | 265 (17.3) | 1,267 (82.7) | |||
| Age | |||||||||
| 18–25 | 124 (17.9) | 567 (82.1) | 0.006 | 190 (27.5) | 501 (72.5) | p < 0.001 | 113 (16.4) | 578 (83.6) | 0.003 |
| 26–30 | 143 (22.2) | 502 (77.8) | 184 (28.5) | 461 (71.5) | 112 (17.4) | 533 (82.6) | |||
| 31–40 | 193 (21.7) | 698 (78.3) | 266 (29.9) | 625 (70.1) | 207 (23.2) | 684 (76.8) | |||
| 41–50 | 68 (17.0) | 332 (83.0) | 94 (23.5) | 306 (76.5) | 76 (19.0) | 324 (81.0) | |||
| ≥51 | 30 (13.0) | 201 (87.0) | 36 (15.6) | 195 (84.4) | 53 (22.9) | 178 (77.1) | |||
| Marriage | |||||||||
| Not have a spouse | 194 (17.1) | 943 (82.9) | 0.007 | 292 (25.7) | 845 (74.3) | 0.217 | 188 (16.5) | 949 (83.5) | 0.001 |
| Have a spouse | 364 (21.2) | 1,357 (78.8) | 478 (27.8) | 1,243 (72.2) | 373 (21.7) | 1,348 (78.3) | |||
| Education | |||||||||
| Junior high school and below | 45 (16.8) | 223 (83.2) | p < 0.001 | 62 (23.1) | 206 (76.9) | p < 0.001 | 52 (19.4) | 216 (80.6) | p < 0.001 |
| High school/Technical school | 111 (28.7) | 276 (71.3) | 139 (35.9) | 248 (64.1) | 99 (25.6) | 288 (74.4) | |||
| Junior College | 108 (22.1) | 380 (77.9) | 135 (27.7) | 353 (72.3) | 110 (22.5) | 378 (77.5) | |||
| Undergraduate | 240 (19.1) | 1,017 (80.9) | 337 (26.8) | 920 (73.2) | 235 (18.7) | 1,022 (81.3) | |||
| Postgraduate and above | 54 (11.8) | 404 (88.2) | 97 (21.2) | 361 (78.8) | 65 (14.2) | 393 (85.8) | |||
| Job | |||||||||
| Medical workers | 66 (15.7) | 355 (84.3) | p < 0.001 | 103 (24.5) | 318 (75.5) | 0.002 | 102 (24.2) | 319 (75.8) | 0.005 |
| Nonprofessional employees | 80 (30.9) | 179 (69.1) | 96 (37.1) | 163 (62.9) | 52 (20.1) | 207 (79.9) | |||
| Social service workers | 44 (19.1) | 186 (80.9) | 57 (24.8) | 173 (75.2) | 48 (20.9) | 182 (79.1) | |||
| Teachers and operators | 131 (20.2) | 517 (79.8) | 164 (25.3) | 484 (74.7) | 127 (19.6) | 521 (80.4) | |||
| Students | 64 (15.1) | 360 (84.9) | 105 (24.8) | 319 (75.2) | 60 (14.2) | 364 (85.8) | |||
| Workers and farmers | 91 (23.5) | 297 (76.5) | 119 (30.7) | 269 (69.3) | 89 (22.9) | 299 (77.1) | |||
| Unemployed and others | 82 (16.8) | 406 (83.2) | 126 (25.8) | 362 (74.2) | 83 (17.0) | 405 (83.0) | |||
| Income | |||||||||
| Poor | 88 (26.9) | 239 (73.1) | p < 0.001 | 109 (33.3) | 218 (66.7) | 0.006 | 84 (25.7) | 243 (74.3) | 0.003 |
| Not poor | 470 (18.6) | 2,061 (81.4) | 661 (26.1) | 1,870 (73.9) | 477 (18.8) | 2,054 (81.2) | |||
| Wuhan exposure | |||||||||
| Yes | 69 (16.7) | 344 (83.3) | 0.118 | 116 (28.1) | 297 (71.9) | 0.571 | 96 (23.2) | 317 (76.8) | 0.046 |
| No | 489 (20.0) | 1,956 (80.0) | 654 (26.7) | 1,791 (73.3) | 465 (19.0) | 1,980 (81.0) | |||
| Impact on livelihood | |||||||||
| None | 90 (10.9) | 735 (89.1) | p < 0.001 | 148 (17.9) | 677 (82.1) | p < 0.001 | 131 (15.9) | 694 (84.1) | p < 0.001 |
| Some | 160 (16.4) | 815 (83.6) | 231 (23.7) | 744 (76.3) | 170 (17.4) | 805 (82.6) | |||
| Relatively large | 177 (29.0) | 434 (71.0) | 224 (36.7) | 387 (63.3) | 143 (23.4) | 468 (76.6) | |||
| Very large | 131 (29.3) | 316 (70.7) | 167 (37.4) | 280 (62.6) | 117 (26.2) | 330 (73.8) | |||
| Prior exposure | |||||||||
| Yes | 59 (26.0) | 168 (74.0) | 0.010 | 78 (34.3) | 149 (65.6) | 0.009 | 50 (22.0) | 177 (78.0) | 0.343 |
| No | 499 (19.0) | 2,132 (81.0) | 692 (26.3) | 1,939 (73.7) | 511 (19.4) | 2,120 (80.6) | |||
| Media exposure | |||||||||
| Frequently | 346 (21.5) | 1,262 (78.5) | 0.005 | 451 (28.0) | 1,157 (72.0) | 0.035 | 346 (21.5) | 1,262 (78.5) | 0.029 |
| Sometimes | 119 (15.6) | 643 (84.4) | 184 (24.1) | 578 (75.9) | 126 (16.5) | 636 (83.5) | |||
| Less | 54 (20.8) | 205 (79.2) | 82 (31.7) | 177 (68.3) | 49 (18.9) | 210 (81.1) | |||
| Very less | 39 (17.0) | 190 (83.0) | 53 (23.1) | 176 (76.9) | 40 (17.5) | 189 (82.5) | |||
| Prior psychological problems | |||||||||
| Yes | 126 (30.1) | 292 (69.9) | p < 0.001 | 204 (48.8) | 214 (51.2) | p < 0.001 | 137 (32.8) | 281 (67.2) | p < 0.001 |
| No | 432 (17.7) | 2,008 (82.3) | 566 (23.2) | 1,874 (76.8) | 424 (17.4) | 2,016 (82.6) | |||
| Post psychological problems | |||||||||
| Yes | 247 (29.8) | 581 (70.2) | p < 0.001 | 355 (42.9) | 473 (57.1) | p < 0.001 | 244 (29.5) | 584 (70.5) | p < 0.001 |
| No | 311 (15.3) | 1,719 (84.7) | 415 (20.4) | 1,615 (79.6) | 317 (15.6) | 1,713 (84.4) | |||
| Chronic disease | |||||||||
| Yes | 61 (17.8) | 281 (82.2) | 0.401 | 113 (33.0) | 229 (67.0) | 0.007 | 100 (29.2) | 242 (70.8) | p < 0.001 |
| No | 497 (19.8) | 2,019 (80.2) | 657 (26.1) | 1,859 (73.9) | 461 (18.3) | 2,055 (81.7) | |||
| Two-week illness | |||||||||
| Yes | 63 (31.3) | 138 (68.7) | p < 0.001 | 96 (47.8) | 105 (52.2) | p < 0.001 | 75 (37.3) | 126 (62.7) | p < 0.001 |
| No | 495 (18.6) | 2,162 (81.4) | 674 (25.4) | 1,983 (74.6) | 486 (18.3) | 2,171 (81.7) | |||
| Mean (SD) | P value | Mean (SD) | P value | Mean (SD) | P-value | ||||
| Direct exposure | 0.8 (1.6) | 0.5 (1.1) | p < 0.001 | 0.9 (1.6) | 0.5 (1.0) | p < 0.001 | 1.0 (1.7) | 0.5 (1.0) | p < 0.001 |
Logistic Regression Analyses
As shown in Table 3, the prevalence of PTSS is generally higher among males than females (OR = 1.824, 95%CI: 1.477–2.251, Cohen's d = 0.331). In comparison with single and above 50-year-old participants, those aged between 26 and 30 years and married possibly suffer from higher PTSS (OR = 1.796, 95%CI: 1.103, 2.925, Cohen's d = 0.323). Essential service jobs, direct exposure to COVID-19, negative impact on livelihood, post psychological problems, 2-week illness are significantly associated with a higher level of PTSS. Counter-intuitively, participants with higher education, the Wuhan contact, and sometimes media exposure are less likely to be diagnosed with PTSD.
Table 3.
Logistic regression analysis for risk factors of PTSS, depression and insomnia.
| Variables | Model 1-PTSS | Model 2-Depression | Model 3-Insomnia | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | Cohen's d | OR (95% CI) | Cohen's d | OR (95% CI) | Cohen's d | |
| Wuhan exposure (No) | ||||||
| Yes | 0.694* (0.501, 0.961) | −0.201 | 0.883 (0.668, 1.168) | −0.069 | 0.995 (0.739, 1.340) | −0.003 |
| Impact on livelihood (None) | ||||||
| Some | 1.499** (1.123, 1.999) | 0.223 | 1.393** (1.089, 1.781) | 0.183 | 1.146 (0.882, 1.490) | 0.075 |
| Relatively large | 3.054*** (2.275, 4.101) | 0.616 | 2.482*** (1.914, 3.218) | 0.051 | 1.579** (1.193, 2.089) | 0.252 |
| Very large | 2.590*** (1.879, 3.571) | 0.525 | 2.255*** (1.693, 3.003) | 0.448 | 1.632** (1.202, 2.216) | 0.270 |
| Prior exposure (No) | ||||||
| Yes | 1.204 (0.851, 1.705) | 0.102 | 1.068 (0.772, 1.477) | 0.036 | 0.789 (0.548, 1.134) | −0.131 |
| Direct exposure | 1.186** (1.069, 1.315) | 0.094 | 1.187** (1.077, 1.308) | 0.095 | 1.257*** (1.138, 1.389) | 0.126 |
| Media exposure (Frequently) | ||||||
| Sometimes | 0.768* (0.601, 0.981) | −0.146 | 0.941 (0.758, 1.168) | −0.034 | 0.793 (0.625, 1.007) | −0.128 |
| Less | 0.936 (0.656, 1.333) | −0.036 | 1.298 (0.947, 1.778) | 0.144 | 0.863 (0.605, 1.231) | −0.081 |
| Very less | 0.813 (0.546, 1.210) | −0.114 | 0.915 (0.638, 1.312) | −0.049 | 0.807 (0.547, 1.191) | −0.118 |
| Ethnicity (Han) | ||||||
| Else | 0.919 (0.546, 1.545) | −0.047 | 1.005 (0.918, 1.101) | 0.003 | 0.969 (0.590, 1.591) | −0.017 |
| Gender (Female) | ||||||
| Male | 1.824*** (1.477, 2.251) | 0.331 | 1.698*** (1.405, 2.052) | 0.292 | 1.390** (1.131, 1.707) | 0.182 |
| Age (≥51) | ||||||
| 18–25 | 1.471 (0.846, 2.559) | 0.213 | 2.245** (1.348, 3.739) | 0.446 | 0.714 (0.432, 1.179) | −0.186 |
| 26–30 | 1.796* (1.103, 2.925) | 0.323 | 2.369*** (1.500, 3.739) | 0.476 | 0.718 (0.465, 1.106) | −0.183 |
| 31–40 | 1.419 (0.894, 2.253) | 0.193 | 2.166*** (1.407, 3.333) | 0.426 | 0.965 (0.652, 1.430) | −0.020 |
| 41–50 | 1.124 (0.679, 1.860) | 0.064 | 1.631** (1.024, 2.597) | 0.270 | 0.761 (0.493, 1.174) | −0.151 |
| Marriage (None spouse) | ||||||
| Have a spouse | 1.368** (1.022, 1.831) | 0.173 | 1.212 (0.931, 1.577) | 0.106 | 1.050 (0.789, 1.398) | 0.027 |
| Education (Postgraduate and above) | ||||||
| Junior high school and below | 1.540 (0.933, 2.540) | 0.238 | 1.251 (0.807, 1.939) | 0.123 | 1.471 (0.912, 2.371) | 0.213 |
| High school/Technical school | 2.373** (1.573, 3.581) | 0.476 | 1.818** (1.268, 2.607) | 0.330 | 2.028*** (1.364, 3.016) | 0.390 |
| Junior College | 1.940** (1.305, 2.885) | 0.365 | 1.379 (0.979, 1.943) | 0.177 | 1.901** (1.304, 2.773) | 0.354 |
| Undergraduate | 1.679** (1.193, 2.363) | 0.286 | 1.309 (0.985, 1.739) | 0.148 | 1.351 (0.978, 1.867) | 0.166 |
| Job (Medical workers) | ||||||
| Nonprofessional employees | 1.721* (1.129, 2.621) | 0.299 | 1.421 (0.967, 2.089) | 0.194 | 0.643* (0.421, 0.982) | −0.243 |
| Social service workers | 1.488 (0.938, 2.358) | 0.219 | 1.175 (0.777, 1.777) | 0.089 | 0.978 (0.641, 1.492) | −0.012 |
| Teachers and operators | 1.335 (0.927, 1.921) | 0.159 | 1.032 (0.747, 1.426) | 0.017 | 0.757 (0.544, 1.054) | −0.153 |
| Students | 1.231 (0.752, 2.017) | 0.115 | 1.030 (0.669, 1.587) | 0.016 | 0.647 (0.402, 1.042) | −0.240 |
| Workers and farmers | 1.346 (0.890, 2.037) | 0.164 | 1.290 (0.890, 1.871) | 0.140 | 0.804 (0.546, 1.182) | −0.120 |
| Unemployed and others | 1.036 (0.699, 1.535) | 0.019 | 1.108 (0.787, 1.559) | 0.057 | 0.629* (0.438, 0.903) | −0.256 |
| Income (Not poor) | ||||||
| Poor | 1.276 (0.953, 1.709) | 0.134 | 1.098 (0.834, 1.447) | 0.052 | 1.377* (1.028, 1.846) | 0.176 |
| Prior psychological problems (No) | ||||||
| Yes | 1.316 (0.992, 1.745) | 0.151 | 1.930*** (1.498, 2.486) | 0.363 | 1.572** (1.199, 2.062) | 0.249 |
| Post psychological problems (No) | ||||||
| Yes | 2.026*** (1.609, 2.552) | 0.389 | 2.168*** (1.762, 2.668) | 0.427 | 1.658*** (1.321, 2.080) | 0.279 |
| Chronic disease (No) | ||||||
| Yes | 0.741 (0.528, 1.039) | −0.165 | 1.204 (0.904, 1.602) | 0.102 | 1.412* (1.058, 1.884) | 0.190 |
| Two-week illness (No) | ||||||
| Yes | 1.554* (1.074, 2.248) | 0.243 | 1.829*** (1.303, 2.566) | 0.333 | 1.766** (1.249, 2.497) | 0.314 |
The values of coefficients and 95% confidence interval in bold represent statistically significant at 0.05 level.
p <0.05,
p <0.01,
p <0.001.
Factors correlated with depression are mostly similar to those for PTSS, however, a few differences ought to be noted. Firstly, significant differences exist between all age groups. Take people aged over 51 as a reference, those aged 18–50 are more likely to be depressed. In detail, the Cohen's d effect size is highest in the 26–30 age group, followed by the 18–25 age group and 31–40 age group, while is lowest in the 41–50 age group. And the Cohen's d values of all these age groups are over 0.2 and below 0.5, indicating a medium association with depression. Secondly, participants with prior psychological problems, high school/technical school education, post psychological problems, and 2-week illness incline to a higher level of depression. And the Cohen's d effect sizes of all these variables are medium (over 0.2 and below 0.5).
When it comes to insomnia, there exists a significant gender variation in the PTSS prevalence (OR = 1.390, 95%CI: 1.131–1.707, Cohen's d = 0.182), but no age differences. Compared with medical workers who are intensively exposed, individuals in essential service jobs and those being unemployed are less possibly to experience PTSS, and both the Cohen's d effect sizes of them were medium. And people suffering from chronic diseases may be more prone to have high insomnia symptoms (OR = 1.412, 95%CI: 1.058–1.884, Cohen's d = 0.190), although Cohen's d effect size is small.
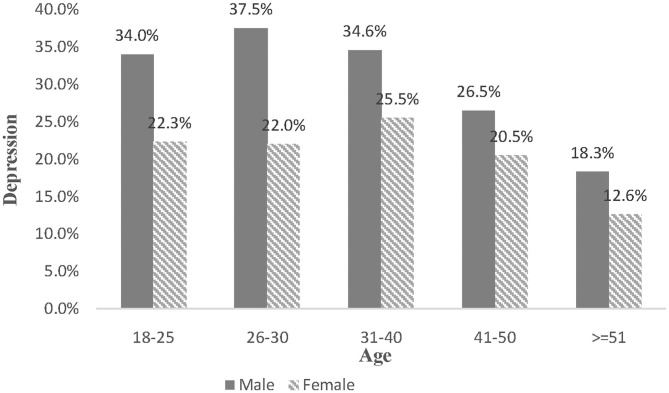
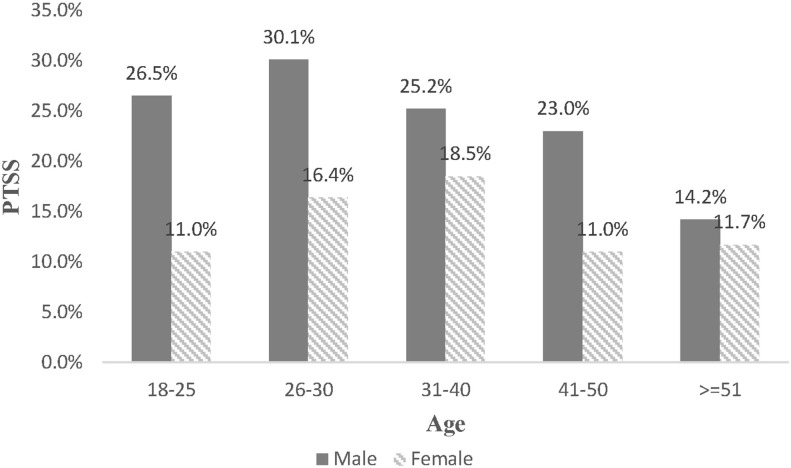
Since age has an insignificant association with insomnia, this study further examines the combined effect of gender and age on PTSS and depression. Although no significant differences are found among other age groups, men aged 18–50 may experience a high degree of PTSS, compared with females aged 18–25 years old. At the same time, the age distribution of depressive prevalence is different (see Figure 2). Despite no differences exist between females aged 18–25 and other groups, those aged over 50 years old are less likely to suffer depression (OR = 0.448, 95%CI: 0.220–0.911, Cohen's d = −0.443). In comparison with young women, young men are more likely to develop depression. For example, compared with women aged 18–25, the prevalence of depression for men at the same age is higher (OR = 1.766, 95%CI: 1.219–2.560, Cohen's d = 0.314), peaking during their late 20s (OR = 2.024, 95%CI: 1.317–3.111, Cohen's d = 0.389) and then declining. For more details, Table 4 is demonstrated below. Sensitivity analysis was conducted by linear regression, and the results were consisted with the above (more detail can be seen in Figures 1, 2 and Table 5).
Figure 2.
The combine effect of gender and age on depression.
Table 4.
Logistic regression analysis for the combined effect of gender and age on PTSS and depressive symptoms.
| Model 4-PTSS | Model 5-Depression | |||
|---|---|---|---|---|
| Variables | OR (95% CI) | Cohen's d | OR (95% CI) | Cohen's d |
| Gender*age [Female (18–25)] | ||||
| Female (26–30) | 1.505 (0.904, 2.505) | 0.225 | 0.971 (0.630, 1.495) | −0.016 |
| Female (31–40) | 1.403 (0.835, 2.359) | 0.187 | 1.004 (0.645, 1.563) | 0.002 |
| Female (41-50) | 0.863 (0.450, 1.655) | −0.081 | 0.861 (0.506, 1.466) | −0.083 |
| Female (≥51) | 1.118 (0.521, 2.401) | 0.061 | 0.448* (0.220, 0.911) | −0.443 |
| Male (18–25) | 2.647*** (1.711, 4.097) | 0.537 | 1.766** (1.219, 2.560) | 0.314 |
| Male (26–30) | 2.846*** (1.725, 4.695) | 0.577 | 2.024** (1.317, 3.111) | 0.389 |
| Male (31–40) | 1.962** (1.181, 3.259) | 0.372 | 1.620* (1.050, 2.500) | 0.266 |
| Male (41–50) | 1.880* (1.050, 3.364) | 0.348 | 1.101 (0.658, 1.843) | 0.053 |
| Male (≥51) | 1.323 (0.644, 2. 717) | 0.154 | 0.777 (0.411, 1.467) | −0.139 |
The combine effect of gender and age was not significant in logistic regression analysis for insomnia, thus the results are not presented in this table; all confounding variables were controlled in the above models. The values of coefficients and 95% confidence interval in bold represent statistically significant at 0.05 level.
p < 0.05,
p < 0.01,
p < 0.001.
Figure 1.
The combine effect of gender and age on PTSS.
Table 5.
Sensitivity analysis for the combined effect of gender and age on PTSS and depressive symptoms.
| Model 6-PTSS | Model 7-Depression | |||
|---|---|---|---|---|
| Variables | Coef. (Sta.Err) | Beta | Coef. (Sta.Err) | Beta |
| Gender*age [Female (18–25)] | ||||
| Female (26–30) | 0.521 (1.384) | 0.010 | −0.492 (0.920) | −0.014 |
| Female (31–40) | −0.372 (1.456) | −0.008 | −0.564 (0.968) | −0.017 |
| Female (41–50) | −2.026 (1.711) | −0.029 | −1.622 (1.138) | −0.035 |
| Female (≥51) | −3.401 (2.025) | −0.037 | –3.151 (1.346)* | −0.052 |
| Male (18–25) | 4.502 (1.251)*** | 0.079 | 1.766 (0.832)* | 0.047 |
| Male (26–30) | 5.017 (1.458)*** | 0.083 | 3.545 (0.969)*** | 0.089 |
| Male (31–40) | 2.266 (1.460) | 0.045 | 2.066 (0.971)* | 0.063 |
| Male (41–50) | 0.7225 (1.715) | 0.010 | 0.379 (1.140) | 0.008 |
| Male (≥51) | −1.976 (1.985) | −0.022 | −2.313 (1.320) | −0.040 |
The combined effect of gender and age was not found significant in logistic regression analysis for insomnia, thus the results are not presented in this table; All confounding variables were controlled in the above models. The values of coefficients and 95% confidence interval in bold represent statistically significant at 0.05 level.
p < 0.05,
p < 0.001.
Discussion
This study attempted to reveal the mental health conditions among the population during the initial stage of the COVID-19 pandemic, and further to identify the combined effect of gender and age on the COVID-19 related mental health effects. Most importantly, this study found that the prevalence of PTSS, depression, and insomnia were 19.5, 26.9, and 19.6% respectively. Although no significant combined effect of gender and age was found in insomnia, PTSS, and depression closely related to gender-age interaction. Men in the late 20s were with relatively high PTSD symptoms, while the lowest prevalence of depression was found in women in the early 50s. At the same time, men aged 26–30 were more likely to get PTSS and depression. Besides, other factors related to PTSS, depression, and insomnia, in common or in particular, were confirmed either. Our findings identified factors associated with higher mental health symptoms so that they could be used to formulate psychological interventions to improve the mental health of vulnerable populations during the COVID-19 pandemic.
This study suggests that the public should pay greater attention to mental health conditions, as about one-fifth of the population (or over) has shown psychological symptoms. In the absence of traumatic events, the all-age prevalence for PTSS, depression, and insomnia in China are <1, 3.99, and 15% respectively (34–36). With the presence of disaster, the sweeping extent of the mental disorders also varies across traumatic types. An early review concludes the prevalence of PTSD at 5–10% among the general population after disasters (37), and later studies underline it as 8% in the Wenchuan earthquake (38), 8.6% after the flood (39), and <4% after terrorist attacks (40). The uncertain possibility of being infected leads to more PTSD symptoms among the general population, as 27% of individuals in Ebola-affected countries meet levels of clinical concerns for PTSD (41). Due to its huge disease burden in the general population, depression is the most prevalent mental disorder during the COVID-19 pandemic, and the number of people getting depression increases faster than after Hurricane Ike (42) and the 9–11 attack (43). It has to be noted that we estimate a slightly higher prevalence of PTSS and depression than prior studies, which were conducted about 10 days ahead (27, 28). Apart from the variance in sample distribution, the possible reason goes to the accumulative exposure under this pandemic. Communities continued to lockdown and almost all citizens were required to keep social distancing, especially people who could not return to their workplaces at the end of the New Year Holiday. Taking all the above comparisons, it is reasonable for this study to suggest that more attention is needed for mental health conditions under the COVID-19 pandemic.
Moreover, this study indicates an interesting reversal in the gender distribution of mental disorders. As noted by most trauma studies, women have higher incidence rates of mental health problems like PTSS and depression than their male counterparts (44, 45), explained partially by physiological differences or distinguished psychological mechanism (46). On the contrary, the evidence from this study supports that males are more possibly diagnosed with psychological disorders under the pandemic situation. An analogous conclusion could be seen in recent literature on COVID-19 (22) since the traditional gender roles and division is still prevalent in China (47). Chinese men as families' pillars have to take more psychological pressures for ensuring adequate supplies and the safety of the family during the COVID-19 pandemic, such as taking on family affairs with high exposure risk. In the meantime, the lack of strategies for men to cope with stress exacerbates their mental health disorders in COVID-19 scenarios. Previous studies find that men incline to reduce their pressure by resolving problems caused by stressors, while women turn to psychological adaptation (11, 48). However, with a universal lockdown policy, men who worry about their income could hardly find a way to solve the problem and thus experiencing high financial and living stress. Based on the prevalence of traditional gender role attitudes in China and the males' special strategy coping with stress, it is reliable for this study to claim that men express more mental health symptoms than women during the COVID-19 outbreak in China, therefore, releasing pressures on income and living is important to improve mental health.
Furthermore, a combined effect of gender and age is found upon PTSS and depression, indicating a different life-course expectation between men and women. Accordingly, previous studies show that women aged 26–30 may have the greatest depression and PTSD symptoms for the role burden and role conflict (49). For example, the responsibilities for taking care of families and troubles to balance work and family serve as a major source of psychological stress for young women. Greater psychological symptoms are assumed for women aged over 50, and the reasons are that changes in their reproductive ability, hormonal levels, and sympathetic responses tend to be risky (50). However, this study finds that them having the lowest level of depression. Perhaps, elderly women have stronger social support, lighter economic worries, and are under minimal media exposure. Comparatively, men suffer more from PTSD and depression in their early life in consideration of the family role and economic responsibility (51). Their mental health should be recognized as a social issue, with special attention paid to social problems such as unemployment, the familial disruption. Because of the similarities in the age distribution of psychological symptoms, we confirm that the income disruption raises the greatest negativity for both males and females, and figure out the age groups which should be concerned with priority. And the results also indicated that the gender difference in PTSS and depression could be amplified in young adulthood during the COVID-19, which partly supported our hypothesis. According to life course theory, younger adults usually enter into more new roles and statuses such as beginning marriage and becoming parents than elders, most of them have relative higher job strain and financial stress than older people who would exit from these roles and status (24). Therefore, young adults with these role transitions naturally suffer more financial pressure induced by the COVID-19 pandemic and lockdown, compare to older people. By combining the above explanation about gender difference that Chinese males as breadwinners usually had to bear most of these economic pressures, it could explain that the gender variation in PTSS and depression was magnified in the young adults. Therefore, policymakers should pay attention to these young males who suffer greater pressure because of their social roles and financial burden during this crisis.
Also, this study identifies the shared factors and the specific factors linked to PTSS, depression, and insomnia. Consistent with prior studies (52, 53), people with lower socioeconomic status and poorer health conditions, under more traumatic exposure, are found with greater vulnerabilities to PTSS, depression, and insomnia. Social support can help individuals mitigate PTSS and depression (54, 55). However, living with spouses may lead to greater mental health symptoms and it could be attributed to two aspects. On the one hand, married people are concerned not only for their own health but also for the health of their spouse in a pandemic, indicating an approximately 2-fold higher prevalence in mental disorders (56). Also, negative emotions may spread across individuals in a context full of unknown fears (57). On the other hand, married individuals have more concerns about the health of their families than their single counterparts (47). Besides, the significant variance in insomnia is not found in different age groups, while it is found in PTSS and depression. Possibly, greater hyper-arousal and sleep reactivity of young adults during the trauma counteracts the natural increasing prevalence of insomnia with age (58). The findings of this study implicate that interventions to improve mental health conditions of the population could be adapted with the types of psychopathologies and different sub-groups. It should be noted that health-related behaviors are also demonstrated to correlate with mental health conditions in the period of COVID-19 confinement, specifically, mental health symptoms could be mitigated by physical activity (59) or exacerbated through longer screen time (60). Also a study found that physical activity decreased while screen exposure time increased during the COVID-19 confinement (61). So we should consider reducing individuals' psychological symptoms by increasing their health-related behaviors in the mental health program during the lockdown and further control the variables related to health-related behaviors in future relevant studies.
Limitations and Implications
It has to be noted that there are several limitations to this study. First, this study is based on a cross-sectional survey, indicating that only correlations rather than causal relationships between variables could be revealed. More longitudinal studies are needed to focus on causal relationships. Second, the representativeness of this sample to the general population may be biased. Since this study was conducted online and the elderly who did not have a smartphone might be excluded, the proportion of elderly respondents in this study is lower than it should be in the normal situation. With the adoption of snow-ball sampling, there may be a selection bias, leading to the underrepresentation of the general public and overrepresentation of individuals with specific status such as medical workers, students, and faculties. Overall, a community-based survey could be implemented in the future to avoid these limitations. Thirdly, PTSS, depression, and Insomnia are based on self-report scales. We used PCL-5 without a Criterion A component to assess PTSD symptoms. Clinical diagnosis should be used to increase the veracity of future research in this area.
Despite these limitations, this study is one of the few studies that focus on the interaction effect of age and gender on PTSS, depression, and insomnia among the Chinese general population during the early period of the COVID-19 outbreak. The findings of this study can help to examine the factors associated with the greatest mental health symptoms and provide implications for formulating psychological interventions. On one hand, mental health intervention programs, available psychological support resources, and the necessary economic grant should focus on groups with several special features, especially those who are likely to show two or more kind of mental health problems, such as people with post psychological problems, being male, suffering large impact on livelihood and with high exposure risks. On the other hand, young men take excessive stress because of their social roles and financial burden, which contribute more to mental health problems than exposure experiences. Thus, policy efforts must guarantee people's return to a safe and prejudice-free working environment and work efficiently with the necessary protective equipment.
Conclusion
This study estimates that more or less one-fifth of the population have psychological symptoms during the COVID-19 outbreak. It has to be noted that males, especially young males suffer more from PTSS and depression. Additionally, people with lower socioeconomic status, poorer health conditions, and under extra traumatic exposure were found to be more susceptible to PTSS, depression, and insomnia. These findings are much supportive to screening the significant reasons linked with more mental health symptoms in current and future pandemic.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Peking University Medical Center. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JG designed the study and conceived the manuscript. CL, DL, MF, JG, and YZ drafted the manuscript. XW, JFA, MS, and YW were involved in revising the manuscript. All authors were involved in writing the manuscript and approve of its final version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors wish to thank all those who kindly volunteered to participate in the study.
Footnotes
Funding. This work was supported by the National Social Science Fund of China (Number: 20VYJ042) to JG.
References
- 1.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kickbusch I, Leung G. Response to the emerging novel coronavirus outbreak. BMJ. (2020) 368:M406. 10.1136/bmj.m406 [DOI] [PubMed] [Google Scholar]
- 3.Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiat. (2020) 7:E14. 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu S, Yang L, Zhang C, Xiang YT, Liu Z, Hu S, et al. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiat. (2020) 7:E17–8. 10.1016/S2215-0366(20)30077-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. (2020) 63:1–2. 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ravila G, Rose A, Fils-Aime Jr, Therosme T, Affricot E, Valentin C, et al. Development of a comprehensive, sustained community mental health system in post-earthquake Haiti, 2010-2019. Global Mental Health. (2020) 7:E6. 10.1017/gmh.2019.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaniasty K. Social support, interpersonal, and community dynamics following disasters caused by natural hazards. Curr Opin Lipidol. (2019) 32:105–9. 10.1016/j.copsyc.2019.07.026 [DOI] [PubMed] [Google Scholar]
- 8.Cooke JE, Eirich R, Racine N, Madigan S. Prevalence of posttraumatic and general psychological stress during COVID-19: a rapid review and meta-analysis. Psychiatry Res. (2020) 292:113347. 10.1016/j.psychres.2020.113347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freud A. The widening scope of indications for psychoanalysis: discussion. J Am Psychoanal Ass. (1954) 2:607–20. 10.1177/000306515400200404 [DOI] [PubMed] [Google Scholar]
- 11.Rosenfield S, Smith D. Gender and Mental Health: Do Men and Women Have Different Amounts or Types of Problems? A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York, NY: Cambridge University Press; (2012). p. 256–67. [Google Scholar]
- 12.Perkonigg A, Kessler RC, Storz S, Wittchen HU. Traumatic events and post-traumatic stress disorder in the community: prevalence, risk factors and comorbidity. Acta Psychiat Acand. (2000) 101:46–59. 10.1034/j.1600-0447.2000.101001046.x [DOI] [PubMed] [Google Scholar]
- 13.Ditlevsen D. The Trauma Type Related Variance of Gender Differences in PTSD Prevalence: A Meta-analysis of 15 Danish and 3 Icelandic Convenience Samples. Aarhus: Institute of Psychology; (2009). [Google Scholar]
- 14.Lengua LJ, Stormshak EA. Gender, gender roles, and personality: gender differences in the prediction of coping and psychological symptoms. Sex Roles. (2000) 43:787–820. 10.1023/A:1011096604861 [DOI] [Google Scholar]
- 15.Wang J, Korczykowski M, Rao H, Fan Y, Pluta J, Gur RC, et al. Gender difference in neural response to psychological stress. Soc Cogn Affect Neur. (2007) 2:227–39. 10.1093/scan/nsm018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiat. (1995) 52:1048–60. 10.1001/archpsyc.1995.03950240066012 [DOI] [PubMed] [Google Scholar]
- 17.Ditlevsen DN, Elklit A. The combined effect of gender and age on post traumatic stress disorder: do men and women show differences in the lifespan distribution of the disorder? Ann Gen Psychiatr. (2010) 9:32. 10.1186/1744-859X-9-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rasmusson A, Friedman M. Gender issues in the neurobiology of PTSD. In: Kimerling R, Ouimette P, Wolfe J, editors. Gender and PTSD. New York, NY: The Guilford Press; (2002). p. 43–75. [Google Scholar]
- 19.Norris FH, Kaniasty K, Conrad ML, Inman GL, Murphy AD. Placing age differences in cultural context: a comparison of the effects of age on PTSD after disasters in the United States, Mexico, and Poland. J Clin Geropsychol. (2002) 8:153–73. 10.1023/A:1015940126474 [DOI] [Google Scholar]
- 20.Creamer M, Parslow R. Trauma exposure and posttraumatic stress disorder in the elderly: a community prevalence study. Am J Geriat Psychiat. (2008) 16:853–6. 10.1097/01.JGP.0000310785.36837.85 [DOI] [PubMed] [Google Scholar]
- 21.Yang J. The continuity and change of chinese gender norms in the past 20 years. Shandong Soc Sci. (2017) 11:60−71. [Google Scholar]
- 22.Ren Z, Zhou Y, Liu Y. The psychological burden experienced by Chinese citizens during the COVID-19 outbreak: prevalence and determinants. BMC Public Health. (2020) 20:1–10. 10.1186/s12889-020-09723-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Umberson D, Liu H, Reczek C. Stress and health behaviour over the life course. Adv Life Course Res. (2008) 13:19–44. 10.1016/S1040-2608(08)00002-6 [DOI] [Google Scholar]
- 24.Pearlin LI. The study of coping: an overview of problems and directions. In: Eckenrode J, editor. The Social Context of Coping. New York, NY: Plenum; (1991). p. 261–76. [Google Scholar]
- 25.Altena E, Baglioni C, Espie CA, Ellis J, Gavriloff D, Holzinger B, et al. Dealing With Sleep Problems During Home Confinement Due to the COVID-19 Outbreak: Practical Recommendations From a Task Force of the European CBT-I Academy. (2020). Available online at: https://sci-hub.tw/downloads-ii/2020-04-06/c9/10.1111@jsr.13052.pdf#view=FitH (accessed January 20, 2020). [DOI] [PubMed]
- 26.Bansal P, Bingemann TA, Greenhawt M, Mosnaim G, Nanda A, Oppenheimer J, et al. Clinician Wellness During the COVID-19 Pandemic: Extraordinary Times and Unusual Challenges for the Allergist/Immunologist. (2020). Available online at: https://www.jaci-inpractice.org/article/S2213-2198(20)30327-5/pdf (accessed January 20, 2020). [DOI] [PMC free article] [PubMed]
- 27.Liu N, Zhang F, Wei C, Jia Y, Shang Z, Sun L, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiat Res. (2020) 287:112921. 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the general population in China. Int J Env Res Pub HE. (2020) 17:1729. 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang Y, Di Y, Ye J, Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. (2020) 26:13–22. 10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- 30.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. (1997) 1:385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- 31.Cheng ST, Chan CM. The center for epidemiologic studies depression scale in older Chinese: thresholds for long and short forms. Int J Geriatr Psych. (2005) 20:465–70. 10.1002/gps.1314 [DOI] [PubMed] [Google Scholar]
- 32.Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL-5). (2013). Available online at: www.ptsd.va.gov (accessed January 20, 2020).
- 33.Daniel JB, Charles FR, Timothy HM, Susan RB, David JK. The pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 2:193–213. 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 34.Cao XL, Wang SB, Zhong BL, Zhang L, Ungvari GS, Ng CH, et al. The prevalence of insomnia in the general population in China: a meta-analysis. PLoS ONE. (2017) 12:e0170772 10.1371/journal.pone.0170772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Phillips MR, Zhang J, Shi Q, Song Z, Wang Z. Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey. Lancet. (2009) 373:2041–53. 10.1016/S0140-6736(09)60660-7 [DOI] [PubMed] [Google Scholar]
- 36.Ren XW, Yu SC, Dong WL, Yin P, Xu XH, Zhou MG. Burden of depression in China, 1990-2017: findings from the global burden of disease study 2017. J Affect Disorders. (2020) 268:95–101. 10.1016/j.jad.2020.03.011 [DOI] [PubMed] [Google Scholar]
- 37.Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. (2002) 65:207–39. 10.1521/psyc.65.3.207.20173 [DOI] [PubMed] [Google Scholar]
- 38.Jia Z, Tian W, Liu W, Cao Y, Yan J, Shun Z. Are the elderly more vulnerable to psychological impact of natural disaster? A population-based survey of adult survivors of the 2008 Sichuan earthquake. BMC Public Health. (2010) 10:172. 10.1186/1471-2458-10-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu A, Tan H, Zhou J, Li S, Yang T, Wang J, et al. An epidemiologic study of posttraumatic stress disorder in flood victims in Hunan China. Can J Psychiat. (2006) 51:350–4. 10.1177/070674370605100603 [DOI] [PubMed] [Google Scholar]
- 40.Garcia-Vera MP, Sanz J, Gutierrez S. A systematic review of the literature on posttraumatic stress disorder in victims of terrorist attacks. Psychol Rep. (2016) 119:328–59. 10.1177/0033294116658243 [DOI] [PubMed] [Google Scholar]
- 41.Jalloh MF, Li W, Bunnell RE, Ethier KA, O'Leary A, Hageman KM, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. Brit Med J. (2018) 3:e000471. 10.1136/bmjgh-2017-000471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tracy M, Norris F, Galea S. Differences in the determinants of posttraumatic stress disorder and depression after a mass traumatic event. Depress Anxiety. (2011) 28:666–75. 10.1002/da.20838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Galea S, Ahern J, Resnick H, Kilpatrick D, Bucuvalas M, Gold J, et al. Psychological sequelae of the September 11 terrorist attacks in New York City. New Engl J Med. (2002) 346:982–7. 10.1056/NEJMsa013404 [DOI] [PubMed] [Google Scholar]
- 44.Laila F, Souha F, Carmen H. Correction to: PTSD and gender: could gender differences in war trauma types, symptom clusters and risk factors predict gender differences in PTSD prevalence? Arch Women Mental Health. (2018) 21:1–9. 10.1007/s00737-018-0874-6 [DOI] [PubMed] [Google Scholar]
- 45.Hung M, Bounsanga J, Tang P, Chen W, Cheng C. The factor structure of the hospital anxiety and depression scale in orthopedic trauma patients. J Clin Med. (2015) 7:453–9. 10.14740/jocmr2140w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Howard LM, Ehrlich AM, Gamlen F, Oram S. Gender-neutral mental health research is sex and gender biased. Lancet Psychiat. (2016) 4:9. 10.1016/S2215-0366(16)30209-7 [DOI] [PubMed] [Google Scholar]
- 47.Pineles SL, Hall AA, Rasmusson AM. Gender and PTSD: different pathways to a similar phenotype. Curr Opin Lipidol. (2017) 14:44–8. 10.1016/j.copsyc.2016.11.002 [DOI] [PubMed] [Google Scholar]
- 48.Hori M, Kamo Y. Gender differences in happiness: the effects of marriage, social roles, and social support in East Asia. Appl Res Qual Life. (2018) 13:839–57. 10.1007/s11482-017-9559-y [DOI] [Google Scholar]
- 49.Mcbride AB. Mental health effects of women's multiple roles. J Nurs Scholarship. (2010) 20:41–7. 10.1111/j.1547-5069.1988.tb00028.x [DOI] [PubMed] [Google Scholar]
- 50.Seib C, Lee K, Humphreys J, Anderson D. Predictors of mental health in midlife and older Australian women: a multilevel investigation. Health Care Women Int. (2016) 37:1263–76. 10.1080/07399332.2015.1080262 [DOI] [PubMed] [Google Scholar]
- 51.Rice TR, Shah LD, Trelles P, Lin SK, Christensen DS, Walther A, et al. Mental health of the male adolescent and young man: the copenhagen statement. World J Pediatrics. (2018) 3:224–32. 10.1007/s12519-018-0155-5 [DOI] [PubMed] [Google Scholar]
- 52.Chen NH, Wang PC, Hsieh MJ, Huang CC, Kao KC, Chen YH, et al. Impact of severe acute respiratory syndrome care on the general health status of healthcare workers in Taiwan. Infect Cont Hosp Epidemiol. (2007) 28:75–9. 10.1086/508824 [DOI] [PubMed] [Google Scholar]
- 53.Guo J, Guan L, Liu C, Fu M, Wang X. Depression among Chinese older adults: a perspective from hukou and health inequities. J Affect Disord. (2017) 223:115–20. 10.1016/j.jad.2017.07.032 [DOI] [PubMed] [Google Scholar]
- 54.Gros DF, Flanagan JC, Korte KJ, Mills AC, Brady KT, Back SE. Relations among social support, PTSD symptoms, and substance use in veterans. Psychol Addict Behav. (2016) 30:764–70. 10.1037/adb0000205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hakulinen C, Pulkki-Råback L, Jokela M, Ferrie JE, Aalto AM, Virtanen M, et al. Structural and functional aspects of social support as predictors of mental and physical health trajectories: Whitehall II cohort study. J Epidemiol Community Health. (2016) 70:710–5. 10.1136/jech-2015-206165 [DOI] [PubMed] [Google Scholar]
- 56.Lu YC, Chang YY, Shu BC. Mental symptoms in different health professionals during the SARS attack: a follow-up study. Psychiat Quart. (2009) 80:107–16. 10.1007/s11126-009-9095-5 [DOI] [PubMed] [Google Scholar]
- 57.Qian M, Ye D, Zhong J, Xu K, Zhang L, Huang Z, et al. Behavioural, cognitive and emotional responses to SARS: differences between college students in Beijing and Suzhou. Stress Health. (2005) 21:87–98. 10.1002/smi.1043 [DOI] [Google Scholar]
- 58.Altena E, Chen IY, Daviaux Y, Ivers H, Philip P, Morin CM. How hyperarousal and sleep reactivity are represented in different adult age groups: results from a large cohort study on insomnia. Brain Sci. (2017) 7:41. 10.3390/brainsci7040041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.López-Bueno R, Calatayud J, Ezzatvar Y, Casajús JA, Smith L, Andersen LL, et al. Association between current physical activity and current perceived anxiety and mood in the initial phase of COVID-19 confinement. Front Psychiatry. (2020) 11:729. 10.3389/fpsyt.2020.00729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee Smith LJ, Trott M, Yakkundi A, Butler L, Barnett Y, Armstrong NC, et al. The association between screen time and mental health during COVID-19: a cross sectional study. Psychiatry Res. (2020) 292:113333. 10.1016/j.psychres.2020.113333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.López-Bueno R, Calatayud J, Casaña J, Casajús JA, Smith L, Tully MA, et al. COVID-19 confinement and health risk behaviors in Spain. Front Psychol. (2020) 11:1426. 10.3389/fpsyg.2020.01426 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.