Abstract
BACKGROUND
In the Middle East, data on liver transplantation (LT) are limited, and reports on LT from this region are of specific value. The purpose of this study is to report our 8-year experiences and challenges with LTs in our center to improve the outcomes.
METHODS
116 patients received whole organ graft from deceased donors, and orthotopic liver transplantation was performed at Taleghani hospital, between January 2009 and July 2017. The patients were prioritized according to Model for End-Stage Liver Disease (MELD) score and Child-Pugh classification.
RESULTS
The most common postoperative complication was sepsis (16%), although the most common surgical post LT complication was postoperative bleeding. The most common cause of death was primary graft dysfunction (21.9%). Following LT, 50% of the deaths (n = 16) occurred during the first 10 days. Cumulative survival rates were 78.4%, 77.6%, and 66.7% at 1 month, 1 year, and 5 years, respectively.
CONCLUSION
This report provides invaluable experience from a region where data on LT is largely missing due to the absence of official registration programs. The data could be used to improve the LT program in the region.
Keywords: Transplantation in Iran, Transplant surgery, Liver re-transplantation, End-stage liver disease
INTRODUCTION
Irreversible liver failure is among the most common causes of death worldwide, which results in end-stage liver disease (ESLD).1 The prevalence and outcomes of ESLD vary widely according to the geographical region. In European countries and Central Asia, it was among the top 10 causes of death in 2010.1,2 Unlike other European countries, mortality rates of liver disease are increasing in England.3 According to recent reports, the number of patients who required liver transplantation (LT) has increased in the United States.4 When ESLD occurs, LT remains the only treatment option for patients.5,6 More centers are required in the world to perform LT to meet the increasing demands; therefore, experiences and reports from different regions of the world are invaluable.
In the Middle East, considering the existing socioeconomic limitations and the limited number of registration systems, data on LTs mainly lack, and reports on LTs from this region are of specific value.7,8
LT program has been launched at the organ transplantation center of Taleghani Hospital, one of the well renowned multidisciplinary hospitals affiliated to Shahid Beheshti University of Medical Sciences (SBMU) in Tehran since January 2009. This is the third approved LT center in Iran. The first LT was performed at Nemazee Hospital in Shiraz in 1993,9 and the second center, Imam Khomeini Hospital Complex, started its LT program since 200.10
MATERIALS AND METHODS
Study design
This study was conducted at Taleghani Hospital affiliated to Shahid Beheshti University of Medical Sciences, Tehran, Iran. This hospital is the second hospital in Tehran and the third hospital in Iran, which received approval for LT.
Study protocol
Between January 2009 and July 2017, a total of 116 patients with ESLD received whole organ graft from deceased donors, and orthotopic LT was performed. Patients were prioritized according to model for end stage liver disease (MELD) score.11,12 They were also classified according to their Child-Pugh classification.13
Standard hepatectomy and end-to-end cavo-caval anastomosis and the piggy-back technique with end-to-side cavo-caval anastomosis were carried out for the patients. Regarding the immunosuppressive therapy, all patients received a triple immunosuppressive regimen, which included steroids, tacrolimus, and mycophenolate mofetil, as it has been shown that introducing immunosuppressive agents such as tacrolimus efficiently increased the survival rates after LT.14,15
Data on baseline characteristics including age and sex, clinical characteristics including MELD score, Child-Pugh classification, etiology of ESLD, postoperative complications, and cause of death were recorded for each patient.
Follow-up
Patients were asked to remain within the city for the first month after discharge, and were visited on a weekly basis for the first three months. For the next three months, they were followed up every two weeks and then visited every month until the end of the first year; unless the patient developed unexpected complications.
Ethical consideration
Secrecy of data was maintained throughout the study period, and no personal data of the patients were released. The ethics committee of Shahid Beheshti University of Medical Sciences, Tehran, Iran, approved the study protocol.
Statistical Analysis
Data analysis was done using the Statistical Software for Social Sciences software (SPSS Inc., Chicago, IL, USA), for Windows, version 25. Kaplan-Meier method was used to calculate the cumulative survival rate.
RESULTS
During the study period, 120 LTs, including four re-transplantations, were done for 116 recipients at our center. All patients received transplant organs from brain-dead deceased donors.
Of the 116 patients who underwent LT, 54% were female, and 46% were male. The median age at the LT time was 34 years and 40 years, respectively.
The mean and the median MELD score was 25.35 ± 5.70 SD and 26.00 (21, 29 IQR). In total, 58.6% had a MELD score ≥ 25, 38.8% had a MELD score from 16 to 24, and the remaining patients had a MELD score ≤ 15. Moreover, most of the patients (87.1%) were classified as Child-Pugh class C.
The main cause of LT was cryptogenic cirrhosis (29.3%) and primary sclerosing cholangitis (29.3%) followed by autoimmune hepatitis (25.9%). While primary sclerosing cholangitis was the most common indication for LT among men (45.3%), autoimmune hepatitis was the most common cause of LT among women (46.0%) (Table 1).
Table 1 . Baseline and clinical characteristics of the patients with liver transplantation* .
| Variables |
Males (n = 53) |
Females (n = 63) |
Total |
| Age mean ± SD | 40.38 ± 12.77 | 35.78 ± 11.56 | 37.88 ± 12.29 |
| MELD | n (%) | n (%) | n (%) |
| ≤ 15 | 1 (1.9) | 2 (3.2) | 3 (2.6) |
| 16 – 24 | 19 (35.8) | 26 (41.3) | 45 (38.8) |
| ≥ 25 | 33 (62.3) | 35 (55.6) | 68 (58.6) |
| Child-Pugh classification | |||
| Class A | - | 1 (1.6) | 1 (0.9) |
| Class B | 9 (17) | 5 (7.9) | 14 (12.1) |
| Class C | 44 (83) | 57 (90.5) | 101 (87.1) |
| Indication for LT | |||
| Cryptogenic cirrhosis | 12 (19.0) | 22 (41.5) | 34 (29.3) |
| Primary sclerosing cholangitis | 10 (15.9) | 24 (45.3) | 34 (29.3) |
| Autoimmune hepatitis | 29 (46.0) | 1 (1.9) | 30 (25.9) |
| Primary biliary cirrhosis | 6 (9.5) | - | 6 (5.2) |
| Wilson's disease | 2 (3.2) | 2 (3.8) | 4 (3.4) |
| Alcoholic cirrhosis | - | 3 (5.7) | 3 (2.6) |
| Budd-Chiari syndrome | - | 1 (1.9) | 1 (0.9) |
| Congenital hepatic fibrosis | 1 (1.6) | - | 1 (0.9) |
| Epitheloid hemangioendothelioma | 1 (1.6) | - | 1 (0.9) |
| Primary hyperoxaluria | 1 (1.6) | - | 1 (0.9) |
| Secondary sclerosing cholangitis | 1 (1.6) | - | 1 (0.9) |
| Total | 63 (100) | 53 (100) | 116 (100) |
MELD: Model for end-stage liver disease
*All plus-minus values are means and standard deviations unless stated otherwise.
In general, the most common postoperative complication was sepsis (16%), although the most common surgical post LT complication was postoperative bleeding (Table 2).
Table 2 . Post liver transplantation complications .
| Complication | n (%) |
| Sepsis | 13 (16) |
| Post-transplantation bleeding | 11 (13) |
| Respiratory failure | 11 (13) |
| Primary non-function | 8 (10) |
| Acute respiratory distress syndrome | 7 (9) |
| Graft rejection | 5 (6) |
| Hepatic artery thrombosis | 4 (5) |
| Wound infection | 4 (5) |
| Renal failure | 4 (5) |
| Biliary stricture | 3 (4) |
| Spontaneous bacterial peritonitis | 2 (2) |
| Pulmonary hemorrhage | 2 (2) |
| Intra-abdominal collection | 2 (2) |
| Arrhythmia | 2 (2) |
| Intestinal obstruction | 1 (1) |
| Disseminated herpes infection | 1 (1) |
| Biliary leakage | 1 (1) |
| Hemothorax | 1 (1) |
| Total | 82 (100) |
The most common cause of death was primary graft dysfunction (21.9%) followed by pneumonia (15.6%) and sepsis (12.5%). Following LT, 50% of the deaths (n=16) occurred during the first 10 days [median (IQR) time of death was of 10.50 (2.25, 33.25) days]. Moreover, 3 out of the 16, died on the same day of the LT. Overall, 19.83% (n: 23) of the total patients died in less than one month after LT that is defined as early death (Table 3).
Table 3 . Causes of death after liver transplantation .
| Cause of death | n (%) |
| Primary graft dysfunction | 7 (21.9) |
| Pneumonia | 5 (15.6) |
| Sepsis | 4 (12.5) |
| Fungal infection | 3 (9.4) |
| Heart failure | 2 (6.3) |
| Pulmonary emboli | 2 (6.3) |
| Acute respiratory distress syndrome | 1 (3.1) |
| Arrhythmia | 1 (3.1) |
| Brain tumor | 1 (3.1) |
| Cerebrovascular accident | 1 (3.1) |
| Refractory hyperkalemia | 1 (3.1) |
| Renal failure | 1 (3.1) |
| Respiratory failure | 1 (3.1) |
| Steven-Johnson syndrome | 1 (3.1) |
| Sudden cardiac arrest | 1 (3.1) |
| Total | 32 (100) |
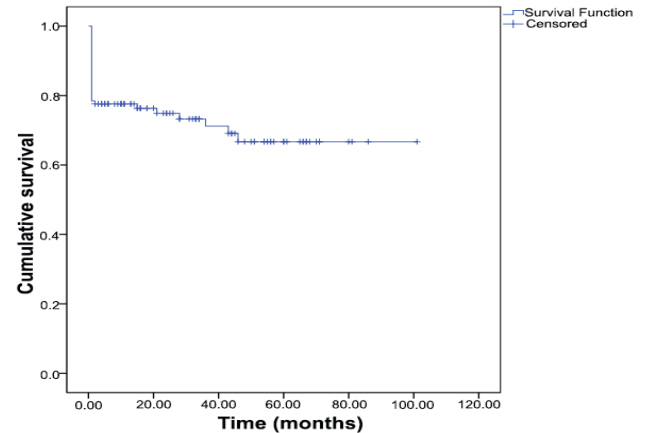
Cumulative survival rates were 78.4%, 77.6%, and 66.7% at 1 month, 1 year, and 5 years, respectively (Figure 1).
Fig.1 .
Cumulative survival rates
DISCUSSION
LT has been recognized as the standard care for ESLD, either due to acute or chronic liver failure since 1963.16 In this study, we report our first experience with 116 LTs at Taleghani Transplant Center from January 2009 to May 2017. We found that most of the patients in our center had a MELD score of more than 25, and were categorized as class C according to the Child-Pugh classification.
Among different treatment choices, LT is the last line treatment modality for patients suffering from multiple diseases that eventually lead to ESLD, including chronic hepatocellular disease, chronic cholestatic disease, metabolic liver disease, and inborn errors of metabolism.6
In our study, the most common cause of liver transplantation was cryptogenic cirrhosis and primary sclerosing cholangitis. The most common complication was sepsis, followed by post-transplant bleeding. The most common cause of death was primary graft dysfunction.
The association between the MELD score and post LT survival benefit is controversial. A systematic review has been conducted over 37 LT studies; the results showed that in 15 studies, there was no relationship between MELD score and post-transplantation survival rate. The other 22 studies identified an association between post-transplantation lower survival rates and higher MELD score.17 Out of the total 116 patients included in this study, 58.6% (n: 68) had a MELD score ≥ 25 at the time of transplantation. Patients with lower MELD scores had significantly better post LT survival output than those with higher MELD scores (p= 0.017). This study supports those investigations that showed an association between lower MELD score and better post-transplantation survival.18,19
It is well documented that elderly patients who underwent LT had a higher mortality rate than younger recipients,20 and younger ones had significantly better post-transplantation survival.21 The results of our study are also in favor of other studies that identified a better survival rate in younger patients.
Most of the cases that were referred to this center included old patients with high MELD scores and serious comorbidities that required emergency transplantation. The higher mortality rate and the more complications developed after LT in this period could be attributed to the general patients’ physical and medical conditions as well as inadequate facilities and human resource insufficiency.
The LT program at our center had many limitations that have been considered to improve the overall performance of the center and eventually have increased patients’ benefits through better post-transplantation outcomes. It takes time and needs financial supports to overcome the insufficient infrastructures (e.g., preoperative care unit, postoperative care unit, and specific intensive care unit), shortage of nursing services, and trained staff to improve the performance of the LT center.
Patients with viral hepatitis were not considered as LT candidates in this center due to the limitations in postoperative treatment and follow-up that are specially required for these patients.
A precise and thorough evaluation of the LT candidates before transplantation, knowledge, and experience of the surgical and anesthesiology team, critical post-transplantation care, and follow-up play a critical role in increasing the benefits of LT.
CONCLUSION
This report provides invaluable experience from a region where data on LT is largely missing due to the absence of official registration programs, which could be used to improve the LT program in the region.
Acknowledgments
The authors would like to thank Dr. Seyed Ali Malek-Hosseini, for his valuable review and suggestions. We would also appreciate Dr. Saman Nikeghbalian for his precious appraisal and recommendations. The authors also like to thank Dr. Peyman Arasteh for his critical appraisal and valuable comments on the paper. The authors declare no conflicts of interest regarding this work. This study was conducted in the Department of Hepato-Pancreato-Biliary/Transplant Surgery, Taleghani Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Please cite this paper as: Nejatollahi SMR, Marashi SA, Janatmakan F, Vosoghian M, Hasanzadehkiabi M, Fazel I. A Single-Center Report on Liver Transplantation: First Experiences from Shahid Beheshti University of Medical Sciences. Middle East J Dig Dis 2020;12:252-256. doi: 10.34172/mejdd.2020.190.
Footnotes
ETHICAL APPROVAL There is nothing to be declared.
CONFLICT OF INTEREST The authors declare no conflict of interest related to this work.
References
- 1.Mokdad AA, Lopez AD, Shahraz S, Lozano R, Mokdad AH, Stanaway J. et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: A systematic analysis. BMC Med. 2014;12:145. doi: 10.1186/s12916-014-0145-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kotzeva M, Kraszewska K, Velasco Dujo S, Mear C. European social statistics (eurostat pocketbooks). 2013 ed. luxembourg: European union, 2013. https://annazavaritt.blog.ilsole24ore.com/wp-content/uploads/sites/54/files/eurostat-social-stats-2013-complete-edition.pdf. Updated 2013.
- 3. Public Health England. Public health profiles. october 2019. https://fingertips.phe.org.uk © Crown copyright. Updated 2019.
- 4.Fayek SA, Quintini C, Chavin KD, Marsh CL. The current state of liver transplantation in the united states: Perspective from american society of transplant surgeons (ASTS) scientific studies committee and endorsed by ASTS council. Am J Transplant. 2016;16:3093–104. doi: 10.1111/ajt.14017. [DOI] [PubMed] [Google Scholar]
- 5.Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F. et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–9. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 6.Riordan SM, Williams R. Perspectives on liver failure: Past and future. Semin Liver Dis. 2008;28:137–41. doi: 10.1055/s-2008-1073113. [DOI] [PubMed] [Google Scholar]
- 7.Ghods AJ. Current status of organ transplant in islamic countries. Exp Clin Transplant. 2015;13:13–17. [PubMed] [Google Scholar]
- 8.Shaheen FA, Souqiyyeh MZ. Current obstacles to organ transplant in middle eastern countries. Exp Clin Transplant. 2015;13:1–3. [PubMed] [Google Scholar]
- 9.Malek Hosseini SA, Lahsaee M, Zare S, Salahi H, Dehbashi N, Firoozi MS. et al. Report of the first liver transplants in iran. Transplant Proc. 1995;27:2618. [PubMed] [Google Scholar]
- 10.Jafarian A, Nassiri-Toosi M, Najafi A, Salimi J, Moini M, Azmoudeh-Ardalan F. et al. Establishing a liver transplantation program at tehran university of medical sciences, iran: A report of ten years of experience. Arch Iran Med. 2014;17:81–3. [PubMed] [Google Scholar]
- 11.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL. et al. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–70. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 12.Wiesner R, Edwards E, Freeman R, Harper A, Kim R, Kamath P. et al. Model for end-stage liver disease (MELD) and allocation of donor livers. Gastroenterology. 2003;124:91–6. doi: 10.1053/gast.2003.50016. [DOI] [PubMed] [Google Scholar]
- 13.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–9. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 14.Iwatsuki S, Starzl TE, Todo S, Gordon RD, Esquivel CO, Tzakis AG. et al. Experience in 1,000 liver transplants under cyclosporine-steroid therapy: A survival report. Transplant Proc. 1988;20:498–504. [PMC free article] [PubMed] [Google Scholar]
- 15.Jain A, Kashyap R, Dodson F, Kramer D, Hamad I, Khan A. et al. A prospective randomized trial of tacrolimus and prednisone versus tacrolimus, prednisone and mycophenolate mofetil in primary adult liver transplantation: A single center report. Transplantation. 2001;72:1091–7. doi: 10.1097/00007890-200109270-00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Starzl TE, Marchioro TL, Vonkaulla KN, Hermann G, Brittain RS, Waddell WR. Homotransplantation of the liver in humans. Surg Gynecol Obstet. 1963;117:659–76. [PMC free article] [PubMed] [Google Scholar]
- 17.Klein KB, Stafinski TD, Menon D. Predicting survival after liver transplantation based on pre-transplant MELD score: A systematic review of the literature. PLoS One. 2013;8:e80661. doi: 10.1371/journal.pone.0080661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patkowski W, Zieniewicz K, Skalski M, Krawczyk M. Correlation between selected prognostic factors and postoperative course in liver transplant recipients. Transplant Proc. 2009;41:3091–3102. doi: 10.1016/j.transproceed.2009.09.038. [DOI] [PubMed] [Google Scholar]
- 19.Guo Z, He X, Wu L, Ju W, Hu A, Tai Q. et al. Model for end-stage liver disease versus the child-pugh score in predicting the post-transplant 3-month and 1-year mortality in a cohort of chinese recipients. Surg Today. 2010;40:38–45. doi: 10.1007/s00595-009-4114-6. [DOI] [PubMed] [Google Scholar]
- 20.Chen HP, Tsai YF, Lin JR, Liu FC, Yu HP. Recipient age and mortality risk after liver transplantation: A population-based cohort study. PLoS One. 2016;11:e0152324. doi: 10.1371/journal.pone.0152324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su F, Yu L, Berry K, Liou IW, Landis CS, Rayhill SC. et al. Aging of liver transplant registrants and recipients: Trends and impact on waitlist outcomes, post-transplantation outcomes, and transplant-related survival benefit. Gastroenterology. 2016;150:441–53. doi: 10.1053/j.gastro.2015.10.043. [DOI] [PubMed] [Google Scholar]