Abstract
COVID-19 is one of the biggest health crises that the world has seen. Whilst measures to abate transmission and infection are ongoing, there continues to be growing numbers of patients requiring chronic support, which is already putting a strain on health care systems around the world and which may do so for years to come. A legacy of COVID-19 will be a long-term requirement to support patients with dedicated rehabilitation and support services. With many clinical settings characterized by a lack of funding and resources, the need to provide these additional services could overwhelm clinical capacity. This position statement from the Healthy Living for Pandemic Event Protection (HL-PIVOT) Network provides a collaborative blueprint focused on leading research and developing clinical guidelines, bringing together professionals with expertise in clinical services and the exercise sciences to develop the evidence base needed to improve outcomes for patients infected by COVID-19.
Keywords: COVID-19, Rehabilitation, Integrated roles, Sports medicine, Exercise sciences
List of abbreviations
| AACVPR | American Association of Cardiovascular and Pulmonary Rehabilitation |
| ACC | American College of Cardiology |
| ACCP | American College of Chest Physicians |
| AHA | American Heart Association |
| ARDS | Acute Respiratory Distress Syndrome |
| ATS | American Thoracic Society |
| BASES | British Association for Sport and Exercise Sciences |
| ERS | European Respiratory Society |
| ESC | European Society of Cardiology |
| HL-Pivot | Healthy Living for Pandemic Event Protection |
| ICU | Intensive Care Unit |
| IL | Interleukin |
| MOST | The Multiphase Optimization Strategy |
| NK | Natural Killer Cells |
| PPE. | Personal Protective Equipment |
| SARS | Severe Acute Respiratory Syndrome |
| TNF-α | Tumor-Necrosis Factor |
| VO2max | Maximal Oxygen Uptake |
Introduction
The COVID-19 pandemic has revealed inequalities in health, wellbeing, and economic status across communities. Whilst emergency approaches taken by governments worldwide have attempted to increase service capacity, the unprecedented demand has outstripped additional increases in personnel and infrastructure, leading to the curtailment of routine services to meet service demand necessitated by the widespread transmission and prolonged morbidity caused by COVID-19. Transmission rates globally have fluctuated over the past months. Currently, countries, particularly in the northern hemisphere, are experiencing a second peak in infections; therefore, the threat of further future waves remains. While collective efforts towards the development of a vaccine, effective treatments and anti-body tests are all global priorities, it remains likely that COVID-19 and its impact will be present in society for some time. Alongside the threat of sustained transmission, there is an urgent need to consider the complexity and chronic care needs of those most seriously affected by COVID-19 to ensure that it does not widen the exposed health inequalities.
Post-acute COVID-19 or ‘long-COVID’ is a colloquial term being used to describe patients reporting persistent symptoms and illness for longer than would be typically expected, despite clinical resolution of infection.1 Long-COVID is a multi-system disease associated with a broad range of symptoms, including fever, fatigue, shortness of breath, chest pain, headaches, neurocognitive difficulties, muscle pains and weakness, depression and other mental health conditions.2 Whilst the medical implications of COVID-19 are not understood in their entirety, it is evident that the duration and severity of persisting symptom profiles do not follow a universal trend and could last for several weeks to months, or even longer.3 The categorization of an individual patient's needs is broad but has been eloquently described by Greenhalgh et al.,4 who categorize those requiring intensive support, as 1) prolonged intensive care unit (ICU) stays; 2) serious and potentially life threatening sequelae (e.g., thromboembolic complications); and 3) those with a non-specific clinical picture (e.g., fatigue and breathlessness). Recent data suggests that >50% of patients that are hospitalized5 and 10% of all COVID-19 infections4 will experience musculoskeletal and neurological de-conditioning requiring rehabilitative support. This provides a significant challenge to clinical services to support those recovering from COVID-19 that are being discharged into community settings with existing and newly acquired co-morbidities.
The pandemic and its legacy present a unique opportunity to forge impactful alliances between clinical and non-clinical support mechanisms. The need to adopt a truly multidisciplinary and collaborative approach that brings together medicine and clinical services alongside those that are aligned with disciplines such as the exercise sciences, engineering, software, and digital technologists can be unified to extend the knowledge base and support the delivery of bespoke services, leading to improved patient outcomes. The Healthy Living for Pandemic Event Protection (HL-PIVOT) network is a recently formed team of professionals with various backgrounds and expertise that share the unifying goal of promoting human resilience and enhancing quality of life through healthy living medicine.6 In this position statement, we highlight the opportunities for integrated practice between professionals from the exercise science and clinical domains to form an alliance in the treatment of post-COVID-19 patients.
The need for bespoke cardiorespiratory rehabilitation programs
Before COVID-19, cardiac and pulmonary rehabilitation was a key aspect of post-acute management and long-term risk reduction for a large population of patients with clinically confirmed cardiovascular or pulmonary disease. Such individualized treatment plans aimed to 1) address the variety of underlying factors that contribute to the patient's disease; 2) implement a comprehensive intervention for secondary prevention of future events, and 3) promote a healthier community overall. The physiological benefits of structured rehabilitation programs have been well-described, with countless trials demonstrating improvements in mortality, hospital readmission rates, functional status, return-to-work time, and quality of life.7, 8, 9 Furthermore, the impact extends far beyond physical recovery, with ample evidence to support psychological benefits in participants, including reduced rates of depression, anxiety and confusion.10 The myriad of high-quality evidence is reflected in international guidelines put forward by the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), the American Thoracic Society (ATS), the European Respiratory Society (ERS), the American College of Chest Physicians (ACCP), the American Heart Association (AHA), and the American College of Cardiology (ACC), the European Society of Cardiology (ESC), among others.9 , 11, 12, 13
The short-term cardiac and pulmonary sequelae of the SARS-CoV-2 virus show similarities with cardiopulmonary complications previously described with Severe Acute Respiratory Syndrome, Middle Eastern Respiratory Syndrome and Influenza A virus subtype H1N1.14 , 15 Whilst data indicates that fewer patients are getting fibrosis (mostly limited to those ventilated who were on intensive care units) than in SARS there are increasing reports of chronic pulmonary emboli and cryptogenic organizing pneumonia.16 Cardiac injury during acute infection has been identified in one-third of hospitalized patients,17 , 18 occasionally measurable by a precipitous rise in troponin or echocardiographic or electrocardiographic abnormalities,14 with data suggesting that cardiac troponin I values are significantly increased in patients with severe SARS-CoV-2 infection and may help in identifying a subset of patients with possible cardiac injury and thereby predict the progression of COVID-19 towards a worse clinical picture.19 The presentation of cardiac injury will vary from acute coronary syndrome and myocardial infarction to cardiogenic shock, arrhythmia, heart failure, and fulminant myocarditis.20 Furthermore, myocardial injury was associated with increased in-hospital mortality.21 , 22 Pulmonary complications most commonly reported with COVID-19 are superimposed bacterial pneumonia and Acute Respiratory Distress Syndrome (ARDS)14; many of these patients may have significant changes in pulmonary function that persist for weeks after recovery, if not lifelong.23 The long-term impact of these prolonged hospitalizations remains to be fully realized. It has been understood that patients are at high risk of significant physical and cognitive impairments after an ICU stay, including critical illness polyneuropathy, critical illness myopathy, and post-intensive care syndrome.24 Furthermore, these patients are at high risk of lasting loss of independence and inability to return to work, which carries significant societal implications.25 The impact on mental health will also undoubtedly be substantial; ARDS is specifically associated with approximately one-quarter of patients reporting post-traumatic stress disorder, one-third suffering from depression, and nearly one-half carrying a diagnosis of generalized anxiety.24
Early evidence for pulmonary rehabilitation in COVID-19 patients is promising, revealing statistically significant improvements in quality of life, respiratory function, and anxiety.26 As lung damage is likely reversible in the majority of hospitalized cases,27 rehabilitation services must be employed early to promote a rapid return to gainful employment and resumption of activities of daily living. The role of inspiratory muscle training as an adjunct to pulmonary rehabilitation should also be considered and the importance here is eloquently described in the context of COVID-19 and future pandemics by Severin et al.28 There is additional evidence to support the use of cardiac rehabilitation in COVID-recovered patients whose underlying cardiac conditions have been exacerbated.29 Beyond this, there is an ongoing need to continue rehabilitation services for those with non-COVID-related indications for referral, with added protective measures to prevent viral spread among these high-risk individuals.
We recommend that all patients admitted to hospital be screened for any evidence of cardiac involvement of COVID-19. Current practice generally supports screening with serial electrocardiogram and troponin measurements, though there is limited data on the topic. Additionally, echocardiography at the time of admission and, as appropriate, for hemodynamic changes alongside ultrasound to help in the identification of cardiac manifestations30 may be considered for patients at increased risk of cardiac involvement. Those who develop significant cardiac injury that persists up to the time of discharge, or those with significant cardiac complications during hospitalization (e.g., acute coronary syndrome, arrhythmia, heart failure, myocarditis, pericarditis, cardiogenic shock, or resuscitated sudden cardiac death) certainly qualify for enrolment in cardiac rehabilitation or combined cardiopulmonary rehabilitation.
We advocate for early initiation of rehabilitation during admission with exclusion criteria for those trending towards critical illness. Multiple parameters have been suggested, but it is generally agreed upon that active fever (Temperature > 38 °C), hemodynamic instability (e.g., hypotension, tachycardia, bradycardia), peripheral oxygenation less than 90%, a respiratory rate greater than 40, or desaturation (>4% from baseline) with attempted activity should prompt modification or discontinuation of rehabilitation.31, 32, 33 In-hospital rehabilitation may be tailored to the patient's clinical condition. Assessment of muscle strength, nutritional needs, frailty, and current understanding of the disease process is reasonable.12 Additionally, early evaluation for poor balance, dysphagia, sleep disturbance, and mental health complications could be considered.34 , 35 For those with severe COVID-19 requiring mechanical ventilation, passive range of motion, joint mobilization, and stretching may prevent rapid deconditioning while the patient remains sedated.12 When able, physical activities such as sitting up, sit to stand, transfer to chair, and walking in place with the assistance of a physiotherapist or occupational therapist may be initiated with careful monitoring of oxygenation levels and symptoms throughout the intervention. Maintaining isolation in this setting with the use of personal protective equipment (PPE) is key to protecting health care workers and avoiding further virus propagation. Early initiation will therefore require both initial assessment and frequent re-assessment of the patient's individual needs, their overall trajectory, and availability of hospital resources (including staff and PPE). Evidence suggests that outpatient rehabilitation is most efficacious when initiated 1 to 3 weeks after the index event, with longer delay times associated with less overall benefit.12 , 36 It has also been suggested that participation in the first three weeks of an exercise program is important in the development of adherence.10 Therefore, referral should be placed by the discharge provider near the end of the index hospitalization or by primary care physicians or other specialists at the first follow-up visit within one week of discharge. Establishing contact during the hospitalization by a healthcare provider and providing information as done for cardiac rehabilitation, could also be beneficial, considering the safety of the healthcare provider.37
It is broadly felt that limiting contact between health care providers and those undergoing post-acute rehabilitation will reduce the risk of nosocomial spread and preserve PPE.33 We recommend that patient-clinician contact be limited to monitored exercise training, and, whenever possible, for interactions to occur primarily via telecommunication at this time (see below for more details). While some have advocated for home-based rehabilitation to be explored as a solution to isolation requirements, this is unlikely to currently be a feasible option. As many of the patients enrolled in rehabilitation were recently critically ill and warrant careful monitoring with frequent reassessments during exercise, we propose that rehabilitation centres instead focus on implementing safe and effective sanitation methods and protocols for the appropriate distancing of patients in attendance. Such interventions as limiting group class sizes, restricting the presence of family members or caregivers, providing masks, requiring hand sanitation before entry, preventing participant aggregation at the entrance and exit of the facility, and moving tasks that do not require supervision (such as education) to an online platform are fairly easily employed and will confer increased safety to patients and providers alike.38 For those low-risk patients who have demonstrated the ability to exercise safely during several sessions of centre-based rehabilitation, it is reasonable to consider transitioning to a hybrid model that incorporates home sessions, provided that they have: 1) demonstrated consistency and reliability; 2) developed a good understanding of the exercise techniques; 3) access to facilities or exercise equipment outside of the rehabilitation centre; 4) adequate social support, and 5) not experienced any adverse events during exercise for the first portion of the program.
Whilst the need for evidence-based and efficacious rehabilitative programs is obvious in the post-COVID-19 period, the volume of patients requiring support will place unprecedented demand for health care services globally. Servicing this demand, which affects all areas of clinical spaces, may overwhelm health care systems who alongside COVID-19 are attempting to continue to provide routine services in settings that are commonly under-resourced at this time.39 A possible solution is to bring the collective expertise of exercise sciences into the clinical fold, to design and deliver interventions and address patients physical and mental health needs.
The need for cross disciplinary approaches Incorporating Exercise Science
There is a need to enhance and develop the role of Exercise Scientists in the treatment and management of COVID-19. Before the pandemic, a taskforce for lung health was established in England in response to the increasing prevalence and rising associated costs of respiratory disease.40 In 2018, this task force published a framework that prioritized the accurate diagnosis, availability of high-quality treatments and a skilled and knowledgeable workforce. Given the shortage of appropriately skilled clinical personnel, a possible solution is to integrate professionals with suitable training from exercise science backgrounds into the system.41 Academics, researchers, and students from exercise science have a broad theoretical and practical knowledge base and understand the integration of the bodies systems at rest and during physical exertion that can be applied to both sport performance and health and disease42 as part of multidisciplinary approaches. As a result of the Pandemic, it is timely to (re)consider a cross disciplinary approach to the promotion and the prescription of exercise in the context of COVID-19. To reflect on cross disciplinary approaches which incorporate Exercise Science the following 4 subsections consider the impact insights and inputs from Exercise Science could have on i) reducing the severity of COVID-19; ii) tackling mental health issues during the Pandemic; iii) increasing the resources available to health care systems and iv) how integration could be achieved.
Increasing physical capacity to prevent disease severity
The role of exercise promotion is well established as a preventative approach to numerous chronic health conditions, and exercise has been shown to provide profound preventive and therapeutic effects for physical health alongside the well-documented benefits to mental wellbeing.43 , 44 However, immunomodulation induced by exercise is dependent on the duration, intensity, and frequency of exercise. Prolonged periods of high-intensity exercise (i.e., >2-h, >80% of maximal oxygen uptake - VO2max) depresses immune function, whereas shorter, moderate-intensity exercise (i.e., 45–60 min, 50–70% VO2max) is beneficial, particularly in those within at-risk groups. The evidence from this novel virus suggests that the immunopathology of the SARS-CoV-2 infection involves the innate and adaptive immune system.45 Following infection, neutrophil count is increased, and natural killer (NK) cells are reduced leading to the advent of leukopenia based upon a reduced percentage of monocytes, eosinophils, and basophils.46 In relation to the adaptive immune response, there have been observed reductions in TCD4+ and TCD8+ lymphocytes which coincides with upregulation of B lymphocytes and the detection of high levels of IgG in the plasma 7–10 days after SARS-CoV-2 infection. Proinflammatory cytokines (e.g., tumor-necrosis factor (TNF)-α, interleukin (IL)-6, IL-1β, IL-8, IL-17, and IL-2) are also elevated in an abnormal manner.47 These abnormal elevations lead to crosstalk activation of the neuroendocrine-immune system, with a consequent release of glucocorticoids which impair the immune response and lead to clinical complications such as multiple organ failure.48 This is particularly an issue in the lungs where a cytokine-induced infiltration of neutrophils and macrophages can provoke the formation of hyaline membranes and fracture of the alveolar wall,47 leading to chronic complaints and irreversible lung damage. There is a clear role for the exercise sciences to work alongside the clinical sector to apply this knowledge and implement widespread exercise programs for the larger population, most notably in those considered vulnerable or ‘at risk’. Such interventions could prime the body's immune response in the event of a positive diagnosis, reducing the possibility of an intense clinical intervention and lasting, multisystem complications in the weeks, months and years following COVID-19 infection.
Addressing the broader mental health crisis
The physical health of patients is an important consideration but previous epidemics (e.g., SARS-1) have demonstrated significant reductions in mental health and wellbeing in patients, health care workers and broader society.41 COVID-19 has seen the introduction of national lockdowns around the world that have restricted movement, resulted in large population groups switching to remote working and having their leisure activities significantly curtailed. Whilst national lockdowns are being replaced with localized restrictions enforced relative to spikes in transmission, the results of lockdowns and social distancing measures will inevitably have a lasting impact on physical and mental health. Evidence already demonstrates that regular structured exercise and psychological interventions from exercise science are effective in improving people's mental health and can address broader health and wellbeing issues like those elicited by COVID-19 [42,43]. Therefore, adopting interprofessional health responses that combine clinical and allied health practice to support broad rehabilitative processes are needed and of great importance.
The need for a clinical response to the acute and long-term physical impacts of COVID-19 is largely understood. However, what is now becoming apparent is the need to consider other aspects than just the physical.49 , 50 Both the disease itself and the lockdown measures taken to combat it may have significant impacts on the mental and social wellbeing of people, as well as their physical wellbeing.51 As people live with the impacts of the disease for longer clinicians are increasingly understanding the need for interprofessional health responses, bringing medicine and allied health practice together in rehabilitative processes.52 Beyond the biological impacts, models such as the biopsychosocial framework consider the interaction of the psychological and social impacts in those that have contracted the virus, and those living within imposed measures to control transmission. The biopsychosocial model provides a lens through which this topic can be approached to appreciate the complex and inter-related facets of ‘health.’ This thematic approach allows for a fuller understanding of the various aspects of wellbeing during a pandemic, and the complicated way in which they in turn influence each other. A greater understanding of this complexity will enable the accurate targeting of services and resources and aid in improving the advice given. National approaches using this framework emphasize the need for integrated and holistic approaches to meet the broad needs of the population who are experiencing difficulty with the imposed disease control measures.51 To date, data collected from >13,000 participants from the United Kingdom highlight the biological, psychological, and social determinants that must be considered in response to the increasing global challenge. A range of biological issues was reported in relation to worsening health conditions (blood pressure, diabetes, and epidermal conditions). There were reports related to the progression of health issues, due to curtailed clinical services. Of additional interest were psychological issues such as stress, anxiety, and social issues such as overeating and reduced levels of physical activity which were of greater significance in those with existing health conditions. Psychological issues included new or elevated stress, anxiety, depression, panic attacks, and obsessive behaviours which were unpinned by long-term low-level and multifaceted worry and post-traumatic stress disorder. Countering the development of lasting psychological disorders is paramount to mitigating against a COVID-19 legacy. Whilst there is efficacy in adopting self-help strategies such as mindfulness, nature connectedness and socialization with friends and family some of these approaches have been impeded due to imposed restrictions. Interestingly here, the interaction with pre-existing biological conditions could exacerbate important psychological distress and health conditions in the post-COVID-19 period. The social perspective was the most complex, including a matrix of negative impact from the disease control measures such as isolation and loneliness, loss of meaningful activities, loss of physical contact, loss or changes to education and employment, additional emotional burden caring for children, parents, and or community members. Adopting digital and technology solutions could alleviate some of these issues and will be a key tool in any recovery planning (in both broader welfare and targeted rehabilitation). Considering the complexity and interaction, biopsychosocial perspectives are critical to support people suffering from COVID-19 or the imposed control measures instilled to mitigate against sustained transmission. Interventions must extend beyond clinical settings to support individuals and communities, where depressive and anxiety symptoms have been reported.53
Expert facilities and infrastructure
Alongside the need for multidisciplinary collaborations and a shared knowledge base is the need to make available sports facilities and equipment that can be utilized to support the delivery of rehabilitation programs and clinical recovery approaches. Housed within universities and applied performance centres, exercise scientists are extensive and well-funded. Some of these have been specifically developed with health and wellbeing in mind and could be used with very little adaptation for clinical services. 54 (p19) Others were created to meet the needs of elite high-performance athletes but with care could be transformed to meet the needs of clinical groups. Whilst these facilities differ between institutions normally, they include laboratory spaces that can provide physiological, biomechanical, and psychological support. University-based exercise physiology laboratories have been established for some time and teach students a range of skills from blood sampling to aerobic capacity and muscle function to body composition assessment. It is possible to utilize this space, and staff expertise, to conduct physiological assessments (e.g., cardiopulmonary exercise testing) under the supervision of a clinician, to monitor recovery and develop rehabilitation strategies to ultimately improve patient outcomes. Biomechanics laboratories have been used for sports research for many decades. More recently, these spaces have been used in health research to examine, for example, gait and balance in patients with neuromuscular disorders. Biomechanics laboratories and the techniques used could assist in helping regain balance and return to walking in patients who have spent time in ICU as a result of COVID-19.55 Additionally, many Sport and Exercise Psychologists work without the need for a lab in areas such as motivation, perfectionism, self-esteem, and attitudes. Some of this work has applications that are relevant to addressing the COVID-19 pandemic, for example, developing interventions to help patients to adhere to rehabilitation programs. In addition, some universities have Sport and Exercise Psychology Laboratories. Whilst it is hard to generalize about the resources in these labs many will have: 1) advanced statistical and mathematical modelling software; 2) psychometric inventories; 3) interview and focus group rooms; 4) test apparatus for motor control and learning; 5) eye-tracking systems; and 6) systems for the assessment of stress and anxiety. Alongside the more specialist facilities, most universities have fitness facilities for their students and many of these are open to the public, some of which already host cardiac rehabilitation classes. These facilities normally include cardiovascular and strength training equipment as well as spaces for people to work on their flexibility and balance. They often offer both individual and group-based exercise programs as well as interventions designed to promote exercise adherence.
Integrating the knowledge and skills of the exercise sciences
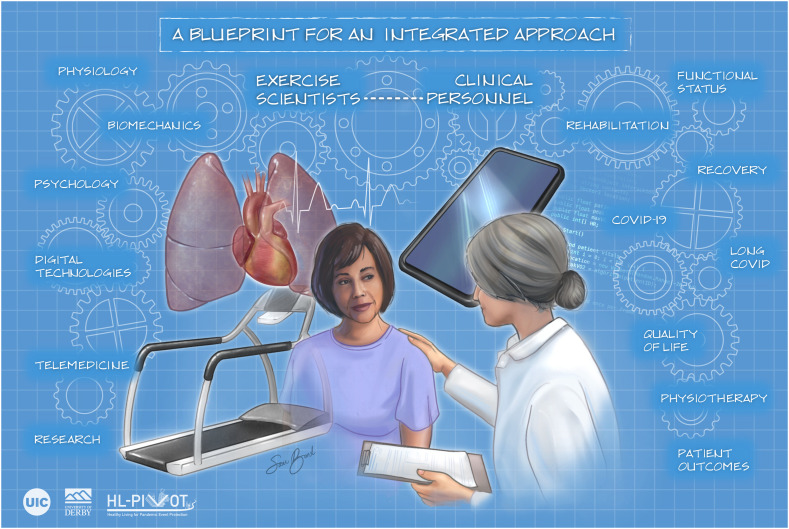
In Fig. 1 , we provide a blueprint that demonstrates how well placed the exercise sciences are to support and have a critical role to play here. The specialist has the skills, knowledge and competencies to design, promote and deliver general physical activity counselling and clinical exercise prescription for a range of populations including older adults,56 from the healthy to those with chronic and complex diseases.57 For some, the recovery from COVID-19 will be a lengthy process with the reality that some may never return to their pre-COVID status. Rehabilitation resources within many health care sectors around the world are scarce, therefore, incorporating these skills sets into healthcare settings could assist in preventing overburdening of clinical settings and assist in the design and delivery of interventions to address mental and physical patient needs.42 These collaborative approaches offer a cohesive approach to understand COVID-19 via targeted research, enhance recovery52 and provide much needed capacity. However, for this to be effective and to achieve the associated broad impacts, a greater understanding of the possibilities is needed from international governments, clinical commissioners, and policymakers. Therefore, health and social care policy makers, commissioners and managers need to engage with national (e.g., the British Association for Sport and Exercise Sciences (BASES)) and international (e.g., the American College Sports Medicine (ACSM) and the European College of Sports Science (ECSS)) organizations to establish what the exercise sciences sector can offer and formulate a blueprint to achieve a collaborative approach that helps meet the needs of the world's population.
Fig. 1.
A blueprint highlighting the opportunities for integrated working between the exercise sciences and clinical partners.
Software and digital technologists
For patients in isolation who do not have significant symptoms, there is an increasing amount of useful information and communication technologies to increase physical activity levels. These technologies are capable of reaching a considerable number of individuals at the same time. One of the primary potentialities of information and communication technology is the possibility of immediate interventions (Just-in-time interventions), i.e., allowing users to engage more dynamically. To date, the evidence for these technologies, specifically in patients with and after COVID-19, is scarce or even non-existent. However, it is reasonable to speculate that these tools will be even more essential post-COVID-19, as the landscape of clinical outpatient care changes from mainly in-person visits to a greater reliance on telemedicine and remote monitoring.58 According to recent recommendations from the American College of Sports Medicine,59 five categories of technologies present more consistent scientific evidence, and we believe that they could be implemented in the context of the current pandemic.60 These include wearable activity monitors, physical activity interventions offered by telephone or through websites, computer-tailored print interventions and interventions using mobile phone text messaging.
Mobile health (mHealth) can be described as the public health strategy supported by mobile devices, such as mobile phones, health monitoring devices like wearable, flexible and unobtrusive devices, personal digital assistants like tablet computers, and other wireless devices.61 In addition to video visits or virtual consultants, mHealth can track the contacts of infected people and provide support and care for patients with suspected or confirmed COVID-19 and those who require other routine clinical services. Wearable devices have enormous potential both in the prevention and care of patients with COVID-19. These devices can be used for respiratory monitoring (e.g., peripheral O2 saturation, respiratory rate, auscultation), cardiovascular monitoring with measures of rhythm/variability of heart rate and blood pressure, for monitoring symptoms such as cough, for measuring blood pressure, body temperature and, within the scope of this text, to monitor physical activity and encourage a physically more active lifestyle.61
To our knowledge, there are no clinical trials that have evaluated the effects of mobile technologies on patients with COVID-19. However, a cohort study showed that using a smartphone application for physical activity was positively associated with the change in habitual physical activity in MET/min/week. Physical activity decreased less with the increase in the frequency of use of the application. Also, a potential independent of gamification has been identified among all functionalities.62 Unfortunately, the effects of using technologies to increase the level of physical activity in adults have been investigated in advisedly and only in the short term. The dynamic context of smartphone applications, for example, demands dynamic and adaptive interventions. Therefore, the efficiency of conventional randomised clinical trials is questionable. The Multiphase Optimization Strategy (MOST) could be used post-pandemic to identify the best combination and intensity of favourable behaviour changes concerning physical activity.63
Apps for physical activity and fitness have also been developed to date with little or no scientific basis, exploring a minimal number of available behaviour change techniques. For smartphone applications, a maximum of 8 techniques64 was identified, and for activity trackers, there is evidence of using a maximum of 20 behaviour change techniques,65 considering almost a hundred available techniques.66 As for cardiorespiratory fitness, Muntaner-Mas et al.67 identified only six applications with sufficient scientific basis and validation studies. Critical physiological variables, such as heart rate and blood pressure, have been neglected in these applications.67
For this type of technology to make a difference inside or outside the pandemic context, applications must be developed scientifically, with a more significant number of behavioural techniques, greater exploration of gamification, and interaction with the built and natural environment. Also, there is already artificial intelligence and data mining technology capable of making the user experience increasingly personalized and interactive. Accordingly, Sporrel et al.68 described an application with innovative features proposed by a consortium between Brazilian and Dutch researchers. Although more research is needed to achieve the objectives mentioned above, the study68 showed a rational and feasible direction for smartphone applications' future development to increase adults' activity and physical fitness levels.
Therefore, considering the need for social distance, technologies can be promising to maintain and increase the level of activity and physical fitness of adults recovering from COVID-19 or in asymptomatic individuals and playing an essential role in uninfected adults. The use of technologies for physical activity and fitness could be encouraged through social media and mass campaigns. The World Health Organization has highlighted mass campaigns as a critical strategy for reducing the prevalence of worldwide physical inactivity69 and has shown to be effective in increasing physical exercise.70 In the case of social networks, the evidence is based on studies of questionable methodological quality.71 However, it has been recommended by the American College of Sports Medicine as promising to encourage a more physically active lifestyle.59 In the urgent moment we are challenging, with an almost absolute absence of specific evidence for patients with COVID-19, it is rational to propose using the technologies highlighted above to mitigate the pandemic's negative impact on physical activity and fitness.
Telemedicine and remote support programs
Among the many consequences of the COVID-19 pandemic has been an urgent acceleration of reliance on remote health care, commonly termed “telehealth”. Telehealth has been defined as “the investigation, monitoring and management of patients and education of patients and staff, using systems which allow access to expert advice and patient information, no matter where the patient or relevant information is located”.72 While telehealth had been expanding rapidly prior to COVID-19, it accounted for only ~19% of health care encounters globally in 2019, a number that is projected to increase roughly 4-fold going forward largely due to the COVID-19 pandemic.73 Greater reliance on telehealth has been necessary as COVID-19 mandated social distancing to reduce staff exposure, preserve PPE, and minimize the impact of patient surges on facilities. Potential positive effects of this transition to greater use of telehealth include improved convenience and access to care, better patient outcomes, and more efficient provision of care.74 For the exercise professional involved in prevention and rehabilitation programs, this sudden, obligatory transformation in healthcare has provided an opportunity to rise to the occasion, to embrace alternative methods of providing rehabilitative services and strengthen their role as allied healthcare providers. Given the rapid changes in technology and reimbursement patterns for rehabilitation, the argument has been made that COVID-19 merely accelerated a process that was already underway.75 , 76
COVID-19 has brought an urgent acceleration of this transformation to telehealth; indeed, there is a “new normal” that has created opportunities for preventive and rehabilitative services to evolve through innovative, technology-driven models of delivery. While patients are less often seen in person or a group setting, the Exercise Scientist is well-equipped to function not only to provide exercise guidance but also to be a health counsellor/navigator as they guide the patient through an individualized plan that optimizes their health. With a little imagination, the ability to exercise at home can be facilitated in numerous ways, including calisthenics, yoga, chair exercises, encouraging walking, gardening, or other household activities, or when it is safe, joining an exercise program at a senior centre. Telehealth can be utilized to monitor real time exercise sessions to ensure patient safety. Additionally, telehealth can be used for patient feedback, exercise progression and post-exercise review of data by an exercise professional. Although new technologies applied to rehabilitation have several caveats to consider (see below), there have been numerous recent innovative efforts to provide activity surveillance and case-management through computer programs designed for this purpose, in addition to guidance through video chat, text/messaging using smartphones or use of wrist-worn devices.77, 78, 79 Real-time monitoring of physiological data can be obtained (e.g., heart rate, respiratory rate, accelerometery) and many devices provide education and motivational support. Simple apps or trackers are commonplace due to their incorporation into technological devices (e.g., mobile phone and watches) which reduces the barrier for both patients and health professionals to monitor progress; in addition to facilitating accountability, many of these tools provide a reference for counselling and optimizing compliance. Application of an exercise program through telehealth, monitored by an exercise professional, has the potential to counter many of the personnel, organizational, cost, and transportation barriers that deter participation in regular exercise for individuals with cardiovascular and pulmonary disease.
In recent years the use of telemedicine in the context of prevention/rehabilitation has expanded beyond cardiovascular and pulmonary disease to monitor and treat conditions that include cancer, diabetes, kidney disease, post-surgical interventions, and many others.80 Relative to usual care, exercise programs using telehealth are convenient, scalable, and cost-effective.76 , 81 Telehealth improves access to care, can be delivered at home on a personalized schedule, and provides an opportunity for social support and the promotion of healthy behaviours.76 , 78 When compared to traditional hospital-based cardiac rehabilitation programs, innovative technologies applying remote monitoring via telehealth in selected populations have reported superior compliance and results that are similar in terms of achieving functional improvement, management of risk factors, and improved quality of life. Longer follow-up studies have also reported similar mortality and re-hospitalization rates between traditional in-hospital and telehealth programs.8 , 82 Some studies have shown that patient dropout rates were lower and the degree of responsiveness and patient preference were higher using telehealth compared to traditional rehabilitation.82 The application of telehealth is consistent with a recent American Heart Association Presidential Advisory calling for the reengineering of community exercise programs to enhance access, adherence, and effectiveness of health care.83 , 84 Finally, telehealth provides an opportunity to incorporate the “Inclusive Chronic Disease Model” of care,85 which endeavours to expand the utilization of services yet reduce costs by restructuring health care delivery through utilization of non-physician, allied health professionals.
The priorities needed to support the development of efficacious support programs
Whilst the benefits of exercise across various health conditions is well established, there is more to be done to further advance the exercise sciences within the context of the “new normal” during and following the COVID-19 pandemic. This, however, requires a clear roadmap to ensure a steady pace of development in this area.
Clinical research
Advancements on the benefits of exercise has grown immensely over the last years. Data from PubMed has shown a rising trend in the number of studies related to exercises with the initial studies being reported from the 1800s. However, from the 1950s, there has been a steep rise in the number of studies with approximately >38,800 studies to date. These studies have spanned the areas of chronic, non-communicable diseases, physical activity, sports, and exercise through various models of delivery. More research into alternate models of delivery, the use of digital health technology, artificial intelligence and machine learning still requires a lot more research. The need for remote monitoring and technology driven assessment and prescription methods is paramount and requires validation and field testing. Furthermore, implementation research, large scale population studies and exercise studies across various resource settings should become a priority as this would greatly enhance the application and relevance of exercise-based interventions.
Trans disciplinarity in research is key and is required for advancement. The integration of sports engineers, software and digital technologists, architectural and design experts, social workers, and public health scientists are some key strategic relations that could foster and spearhead research in this area. Researcher-industry partnerships to facilitate community wide dissemination of innovations are important and should be a priority to ensure a public health impact and to reach a mass audience. Integrating with basic science research to establish the cellular and molecular basis for responses to a healthy lifestyle is crucial to strengthening the physiological and cellular basis for healthy living interventions through both animal and translational research.
Health policy and systems
Many healthcare systems and policies across the world are not favourable towards exercise specialists or those working to promote healthy living. The need for policy and health systems to accommodate exercise specialists is still lacking in most countries. Considering the impact of COVID on long term sequelae, there is a growing need for post-acute care rehabilitation. In this scenario, this would be the opportune time to emphasize the need for exercise scientists and healthy living specialists to play a vital role in the post-COVID rehabilitation interventions, that should be a global priority. Facilitating dialogues with the Government agencies for policy creation should be a priority. Altering the healthcare system and health care policy to promote interdisciplinarity models of care which include exercise specialists should be considered to further facilitate healthy living. Introducing reimbursement strategies for rehabilitation and healthy living interventions would facilitate the wider reach of exercise specialists. All these are possible only with strong advocacy campaigns by professional bodies and the scientific community.
Education and capacity building
Considering the need to utilize non-physician health workers and allied health professionals for the success of the “inclusive chronic disease model”,85 it is imperative that there be strong initiatives building capacity in these areas. Apart from mainstream university based education programs that work towards creating competent professionals in the exercise sciences and allied health, there is the need to re-structure these specialities such that they achieve greater impact on the healthcare needs of those with chronic disease and recovering from COVID-19. Programs like the Healthy Living Practitioner86 appears to be both timely and relevant in the current context with enormous global relevance. Raising the professional bar through doctoral programs is also key and is being initiated through the Doctor of Clinical Exercise Physiology program that is being rolled out in the USA.
With all these priorities, it is important also for funding agencies, professional bodies, and governments to understand the need for further advances in exercise sciences to be better prepared to deal with the immediate and the lasting impact of the COVID pandemic. These implications of exercise advancement transcend all borders and societies and will generate evidence that will be beneficial to the world at large.
The need and impact of an integrated approach
COVID-19 has presented an unprecedented challenge to global healthcare systems, economies, and broader society. Whilst vaccine trials and knowledge to support efficacious treatments are nearing completion, social distancing and restricted social activity are likely to remain in place for the foreseeable future. Whilst most people that contract COVID-19 will be either asymptomatic or have mild symptoms at most, those admitted to hospitals are likely to experience extended periods of morbidity in the months following discharge. In the most severe cases (i.e., those requiring prolonged stays in ICUs) patients will experience irreversible damage to their lungs and other organs which could result in profound disability. These extraordinary circumstances will create additional requirements for healthcare providers to support patients during their rehabilitation and to restore functional status in the coming months and years. With many healthcare settings suffering from chronic underfunding and insufficient resource, this additional and unforeseen pressure will challenge the capacity of clinical services even further. The synergies and complementary knowledge, skillsets and facilities contained within the disciplines of the exercise sciences can create a unique opportunity to promote collaborative working, ease pressure on clinical staff and services and realize the widespread impact that is not limited to improving patient outcomes and the health and wellbeing agenda.
Conclusion
Whilst the opportunity for effective collaboration is apparent, key government agencies and policymakers must seize the opportunity and engage professional bodies from the exercise sciences (e.g., American College of Sports Medicine, European College Sport Sciences and the British Association of Sport and Exercise Sciences) and clinical services (e.g., American Pharmacists Association and National Health Service, UK). This is essential to develop and formalize a blueprint that encourages effective collaborative and cross disciplinary approaches that utilizes a substantial resource in response to this and future health crisis.
Disclosure
The authors have no conflicts of interests/financial relationships to declare.
Declaration of Competing Interest
None.
References
- 1.Mahase E. Covid-19: what do we know about “long covid”? BMJ. 2020:370. doi: 10.1136/bmj.m2815. [DOI] [PubMed] [Google Scholar]
- 2.Dasgupta A., Kalhan A., Kalra S. Long term complications and rehabilitation of COVID-19 patients. JPMA. 2020;70(5):S131–S135. doi: 10.5455/JPMA.32. [DOI] [PubMed] [Google Scholar]
- 3.How Long Does COVID-19 Last? 2020. https://covid.joinzoe.com/post/covid-long-term Accessed September 10.
- 4.Greenhalgh T., Knight M., Buxton M., Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020:370. doi: 10.1136/bmj.m3026. [DOI] [PubMed] [Google Scholar]
- 5.Thomas P., Baldwin C., Bissett B., et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. April 2020;66(2):73–82. doi: 10.1016/j.jphys.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arena R., Lavie C.J., Network H.-P. The global path forward-healthy living for pandemic event protection (HL-PIVOT) Progr Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.05.008. Published online. (S0033–0620) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomas R.J., Brewer L.C. Strengthening the evidence for cardiac rehabilitation benefits. JAMA Cardiol. 2019;4(12):1259–1260. doi: 10.1001/jamacardio.2019.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson L., Oldridge N., Thompson D.R., et al. Exercise-based cardiac rehabilitation for coronary heart disease: cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67(1):1–12. doi: 10.1016/j.jacc.2015.10.044. [DOI] [PubMed] [Google Scholar]
- 9.Thomas R.J., Balady G., Banka G., et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J Am Coll Cardiol. 2018;71(16):1814–1837. doi: 10.1016/j.jacc.2018.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Duncan K., Pozehl B., Hertzog M., Norman J.F. Psychological responses and adherence to exercise in heart failure. Rehabil Nurs. 2014;39(3):130–139. doi: 10.1002/rnj.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Balady G.J., Williams M.A., Ades P.A., et al. Core components of cardiac rehabilitation/secondary prevention programs: 2007 update: a scientific statement from the american heart association exercise, cardiac rehabilitation, and prevention committee, the council on clinical cardiology; the councils on cardiovascular nursing, epidemiology and prevention, and nutrition, physical activity, and metabolism; and the American association of cardiovascular and pulmonary rehabilitation. Circulation. 2007;115(20):2675–2682. doi: 10.1161/CIRCULATIONAHA.106.180945. [DOI] [PubMed] [Google Scholar]
- 12.Spruit M.A., Rochester C., Pitta F., et al. Pulmonary rehabilitation, physical activity, respiratory failure and palliative respiratory care. Thorax. 2019 doi: 10.1136/thoraxjnl-2018-212044. Published online March 14. thoraxjnl-2018-212044. [DOI] [PubMed] [Google Scholar]
- 13.Ries A.L., Bauldoff G.S., Carlin B.W., et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest. 2007;131(5):4S–42S. doi: 10.1378/chest.06-2418. [DOI] [PubMed] [Google Scholar]
- 14.Cho H.J., Heinsar S., Jeong I.S., et al. ECMO use in COVID-19: lessons from past respiratory virus outbreaks—a narrative review. Crit Care. 2020;24(1):1–8. doi: 10.1186/s13054-020-02979-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chan K.S., Zheng J.P., Mok Y.W., et al. SARS: prognosis, outcome and sequelae. Respirology. 2003;8:S36–S40. doi: 10.1046/j.1440-1843.2003.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen L., Tang R., Chen H., et al. Pulmonary vasculature: a target for COVID-19. Am J Respir Crit Care Med. 2020;203(2):260–261. doi: 10.1164/rccm.202009-3564LE. (ja) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lala A., Johnson K.W., Januzzi J.L., et al. Prevalence and impact of myocardial injury in patients hospitalized with COVID-19 infection. J Am Coll Cardiol. 2020;76(5):533–546. doi: 10.1016/j.jacc.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lavie C.J., Sanchis-Gomar F., Lippi G. American College of Cardiology Foundation; Washington DC: 2020. Cardiac Injury in COVID-19–Echoing Prognostication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lippi G., Lavie C.J., Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Progr Cardiovasc Dis. 2020;63(3):390–391. doi: 10.1016/j.pcad.2020.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi S., Qin M., Cai Y., et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Giustino G., Croft L.B., Stefanini G.G., et al. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol. 2020;76(18):2043–2055. doi: 10.1016/j.jacc.2020.08.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bavishi C., Bonow R.O., Trivedi V., Abbott J.D., Messerli F.H., Bhatt D.L. Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Progr Cardiovasc Dis. September–October 2020;63(5):682–689. doi: 10.1016/j.pcad.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fumagalli A., Misuraca C., Bianchi A., et al. Pulmonary function in patients surviving to COVID-19 pneumonia. Infection. 2020:1–5. doi: 10.1007/s15010-020-01474-9. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sheehy L.M. Considerations for postacute rehabilitation for survivors of COVID-19. JMIR Public Health Surveill. 2020;6(2) doi: 10.2196/19462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stam H., Stucki G., Bickenbach J. Covid-19 and post intensive care syndrome: a call for action. J Rehabil Med. 2020;52(4):1–4. doi: 10.2340/16501977-2677. [DOI] [PubMed] [Google Scholar]
- 26.Liu K., Zhang W., Yang Y., Zhang J., Li Y., Chen Y. Respiratory rehabilitation in elderly patients with COVID-19: A randomized controlled study. Complement Ther Clin Pract. 2020:101166. doi: 10.1016/j.ctcp.2020.101166. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu C., Ye L., Xia R., et al. Chest CT and clinical follow-up of discharged patients with COVID-19 in Wenzhou City, Zhejiang, China. Ann Am Thorac Soc. 2020;17(10):1231–1237. doi: 10.1513/AnnalsATS.202004-324OC. (ja) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Severin R., Arena R., Lavie C.J., Bond S., Phillips S.A. Respiratory muscle performance screening for infectious disease management following COVID-19: a highly pressurized situation. Am J Med. September 2020;133(9):1025–1032. doi: 10.1016/j.amjmed.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mureddu G.F., Ambrosetti M., Venturini E., et al. Cardiac rehabilitation activities during the COVID-19 pandemic in Italy. Position Paper of the AICPR (Italian Association of Clinical Cardiology, Prevention and Rehabilitation) Monaldi Archiv Chest Dis. 2020;90(2) doi: 10.4081/monaldi.2020.1439. [DOI] [PubMed] [Google Scholar]
- 30.Khanji M.Y., Ricci F., Patel R.S., et al. The role of hand-held ultrasound for cardiopulmonary assessment during a pandemic. Progr Cardiovasc Dis. September–October 2020;63(5):690–695. doi: 10.1016/j.pcad.2020.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao H.-M., Xie Y.-X., Wang C. Recommendations for respiratory rehabilitation in adults with coronavirus disease 2019. Chin Med J (Engl) 2020;133(13):1595–1602. doi: 10.1097/CM9.0000000000000848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vitacca M., Carone M., Clini E.M., et al. Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration. 2020:1–7. doi: 10.1159/000508399. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang T.J., Chau B., Lui M., Lam G.-T., Lin N., Humbert S. Physical medicine and rehabilitation and pulmonary rehabilitation for COVID-19. Am J Phys Med Rehabil. 2020;99(9):769–774. doi: 10.1097/PHM.0000000000001505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Vitacca M., Lazzeri M., Guffanti E., et al. 2020. Italian Suggestions for Pulmonary Rehabilitation in COVID-19 Patients Recovering From Acute Respiratory Failure: Results of a Delphi Process. Published online. [DOI] [PubMed] [Google Scholar]
- 35.Kiekens C., Boldrini P., Andreoli A., et al. Rehabilitation and respiratory management in the acute and early post-acute phase.“Instant paper from the field” on rehabilitation answers to the Covid-19 emergency. Eur J Phys Rehabil Med. 2020;56(3):323–326. doi: 10.23736/S1973-9087.20.06305-4. (06305–4) [DOI] [PubMed] [Google Scholar]
- 36.Johnson D.A., Sacrinty M.T., Gomadam P.S., et al. Effect of early enrollment on outcomes in cardiac rehabilitation. Am J Cardiol. 2014;114(12):1908–1911. doi: 10.1016/j.amjcard.2014.09.036. [DOI] [PubMed] [Google Scholar]
- 37.Santiago de Araújo Pio C., Beckie T.M., Varnfield M., et al. Promoting patient utilization of outpatient cardiac rehabilitation: a Joint International Council and Canadian Association of Cardiovascular Prevention and Rehabilitation Position Statement. J Cardiopulm Rehabil Prev. 2020;40(2):79–86. doi: 10.1097/HCR.0000000000000474. [DOI] [PubMed] [Google Scholar]
- 38.Smith A., de Oliverira R., Faghy M., Ross M., Maxwell N. The BASES position stand on the “reopening” of sport and exercise science departments in higher education after lockdown. Br Assoc Sport Exer Sci. 2020:1–14. Published online. [Google Scholar]
- 39.The LRM NHS staff shortages threaten the future of respiratory health. Lancet Respir Med. 2019;7(1):1. doi: 10.1016/S2213-2600(18)30512-5. [DOI] [PubMed] [Google Scholar]
- 40.The Battle for Breath - The Economic Burden of Lung Disease. British Lung Foundation; March 9, 2017. https://www.blf.org.uk/policy/economic-burden Published. Accessed February 26, 2020. [Google Scholar]
- 41.Soan E.J., Street S.J., Brownie S.M., Hills A.P. Exercise physiologists: essential players in interdisciplinary teams for noncommunicable chronic disease management. J Multidiscip Healthc. 2014;7:65. doi: 10.2147/JMDH.S55620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Price O.J., Sylvester K.P., Hull J.H. Respiratory physiology and exercise science: time to bridge the gap? BMJ Open Respir Res. 2019;6(1) doi: 10.1136/bmjresp-2019-000442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mikkelsen K., Stojanovska L., Polenakovic M., Bosevski M., Apostolopoulos V. Exercise and mental health. Maturitas. 2017;106:48–56. doi: 10.1016/j.maturitas.2017.09.003. [DOI] [PubMed] [Google Scholar]
- 44.Adams V., Reich B., Uhlemann M., Niebauer J. Molecular effects of exercise training in patients with cardiovascular disease: focus on skeletal muscle, endothelium, and myocardium. Am J Physiol. 2017;313(1):H72–H88. doi: 10.1152/ajpheart.00470.2016. [DOI] [PubMed] [Google Scholar]
- 45.Leandro C.G., e Silva W.T.F., Lima-Silva A.E. Covid-19 and exercise-induced immunomodulation. Neuroimmunomodulation. 2020:1. doi: 10.1159/000508951. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cao X. COVID-19: immunopathology and its implications for therapy. Nat Rev Immunol. 2020;20(5):269–270. doi: 10.1038/s41577-020-0308-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sarzi-Puttini P., Giorgi V., Sirotti S., et al. COVID-19, cytokines and immunosuppression: what can we learn from severe acute respiratory syndrome? Clin Exp Rheumatol. 2020;38(2):337–342. [PubMed] [Google Scholar]
- 48.Mehta P., McAuley D.F., Brown M., et al. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet (London, England) 2020;395(10229):1033. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Holmes E.A., O’Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Patel J.A., Nielsen F.B.H., Badiani A.A., et al. Poverty, inequality and COVID-19: the forgotten vulnerable. Public Health. 2020;183:110. doi: 10.1016/j.puhe.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stuart K., Faghy M.A., Bidmead E., et al. A biopsychosocial framework for recovery from COVID-19. Int J Soc Soc Policy. 2020;40(No. 9/10):1021–1039. [Google Scholar]
- 52.Faghy M.A., Ashton R.E., Maden-Wilkinson T.M., et al. Integrated sports and respiratory medicine in the aftermath of COVID-19. Lancet Respir Med. 2020;8(9):852. doi: 10.1016/S2213-2600(20)30307-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gritti A., Salvati T., Russo K., Catone G. COVID-19 pandemic: a note for psychiatrists and psychologists. JPS J. 2020;4(1):63–77. doi: 10.23823/jps.v4i1.70. [DOI] [Google Scholar]
- 54.Faghy M.A., Sylvester K.P., Cooper B.G., Hull J.H. Cardiopulmonary exercise testing in the COVID-19 endemic phase. Br J Anaesth. 2020;125(4):447–449. doi: 10.1016/j.bja.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Koukourikos K., Tsaloglidou A., Kourkouta L. Muscle atrophy in intensive care unit patients. Acta Inform Med. 2014;22(6):406–410. doi: 10.5455/aim.2014.22.406-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Jiménez-Pavón D., Carbonell-Baeza A., Lavie C.J. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people. Progr Cardiovasc Dis. 2020;63(3):386–388. doi: 10.1016/j.pcad.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brownie S., Hill A.P., Rossiter R. 2014. Primary Health Service Options for Affordable and Accessible Non-communicable Disease and Related Chronic Disease Prevention and Management. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Greiwe J., Nyenhuis S.M. Wearable technology and how this can be implemented into clinical practice. Curr Allergy Asthma Rep. 2020;20:1–10. doi: 10.1007/s11882-020-00927-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.King A.C., Whitt-Glover M.C., Marquez D.X., et al. Physical activity promotion: highlights from the 2018 physical activity guidelines advisory committee systematic review. Med Sci Sports Exerc. 2019;51(6):1340–1353. doi: 10.1249/MSS.0000000000001945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ding X.-R., Clifton D., Nan J.I., et al. Wearable sensing and telehealth technology with potential applications in the coronavirus pandemic. IEEE Rev Biomed Eng. 2020;14:48–70. doi: 10.1109/RBME.2020.2992838. [DOI] [PubMed] [Google Scholar]
- 61.Istepanian R., Jovanov E., Zhang Y.T. Introduction to the special section on M-health: beyond seamless mobility and global wireless health-care connectivity. IEEE Trans Inf Technol Biomed. 2004;8(4):405–414. doi: 10.1109/titb.2004.840019. [DOI] [PubMed] [Google Scholar]
- 62.Yang Y., Koenigstorfer J. Determinants of physical activity maintenance during the Covid-19 pandemic: a focus on fitness apps. Transl Behav Med. 2020;10(4):835–842. doi: 10.1093/tbm/ibaa086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Collins L.M., Murphy S.A., Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5):S112–S118. doi: 10.1016/j.amepre.2007.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schoeppe S., Alley S., Rebar A.L., et al. Apps to improve diet, physical activity and sedentary behaviour in children and adolescents: a review of quality, features and behaviour change techniques. Int J Behav Nutr Phys Act. 2017;14(1):83. doi: 10.1186/s12966-017-0538-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mercer K., Li M., Giangregorio L., Burns C., Grindrod K. Behavior change techniques present in wearable activity trackers: a critical analysis. JMIR Mhealth Uhealth. 2016;4(2) doi: 10.2196/mhealth.4461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Chia G.L.C., Anderson A., McLean L.A. Behavior change techniques incorporated in fitness trackers: content analysis. JMIR Mhealth Uhealth. 2019;7(7) doi: 10.2196/12768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Muntaner-Mas A., Martinez-Nicolas A., Lavie C.J., et al. A systematic review of fitness apps and their potential clinical and sports utility for objective and remote assessment of cardiorespiratory fitness. Sports Med. 2019;49(4):587–600. doi: 10.1007/s40279-019-01084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Sporrel K., De Boer R.D.D., Wang S., et al. The design and development of a personalized physical activity application based on behavior change principles, incorporating the views of end-users and applying empirical data-mining. Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.528472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.NCDs . WHO; 2020. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World.http://www.who.int/ncds/prevention/physical-activity/global-action-plan-2018-2030/en/ Accessed November 13,2020. [Google Scholar]
- 70.Abioye A.I., Hajifathalian K., Danaei G. Do mass media campaigns improve physical activity? A systematic review and meta-analysis. Archiv Public Health. 2013;71(1):20. doi: 10.1186/0778-7367-71-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ferrer D.A., Ellis R. A review of physical activity interventions delivered via Facebook. J Phys Activ Health. 2017;14(10):823–833. doi: 10.1123/jpah.2016-0534. [DOI] [PubMed] [Google Scholar]
- 72.Geisthoff U.W., Federspil P.A., Sittel C., Plinkert P.K. Telemedicine: interaction between clinic and general practice. HNO. 2002;50(9):812–821. doi: 10.1007/s00106-002-0684-y. [DOI] [PubMed] [Google Scholar]
- 73.Consumer Sentiment in the US During the Coronavirus Crisis. McKinsey; 2020. https://www.mckinsey.com/business-functions/marketing-and-sales/our-insights/survey-us-consumer-sentiment-during-the-coronavirus-crisis Accessed September 18. [Google Scholar]
- 74.Chindhy S., Taub P.R., Lavie C.J., Shen J. Current challenges in cardiac rehabilitation: strategies to overcome social factors and attendance barriers. Expert Rev Cardiovasc Ther. 2020:1–13. doi: 10.1080/14779072.2020.1816464. Published online. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ehrman J.K. Clinical Exercise Physiology Association; 2020. Editor’s Perspective: The Clinical Exercise Physiologist in the Time of Covid-19. [Google Scholar]
- 76.Drwal K.R., Forman D.E., Wakefield B.J., El Accaoui R.N. Cardiac rehabilitation during COVID-19 pandemic: highlighting the value of home-based programs. Telemed e-Health. 2020;26(11):1322–1324. doi: 10.1089/tmj.2020.0213. [DOI] [PubMed] [Google Scholar]
- 77.Hannan A.L., Harders M.P., Hing W., Climstein M., Coombes J.S., Furness J. Impact of wearable physical activity monitoring devices with exercise prescription or advice in the maintenance phase of cardiac rehabilitation: systematic review and meta-analysis. BMC Sports Sci Med Rehabil. 2019;11(1):14. doi: 10.1186/s13102-019-0126-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lear S.A. The delivery of cardiac rehabilitation using communications technologies: the “virtual” cardiac rehabilitation program. Can J Cardiol. 2018;34(10):S278–S283. doi: 10.1016/j.cjca.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 79.Babu A.S., Arena R., Ozemek C., Lavie C.J. COVID-19: a time for alternate models in cardiac rehabilitation to take centre stage. Can J Cardiol. 2020;36(6):792–794. doi: 10.1016/j.cjca.2020.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tuckson R.V., Edmunds M., Hodgkins M.L. Telehealth. New Engl J Med. 2017;377(16):1585–1592. doi: 10.1056/NEJMsr1503323. [DOI] [PubMed] [Google Scholar]
- 81.Russo J.E., McCool R.R., Davies L. VA telemedicine: an analysis of cost and time savings. Telemed e-Health. 2016;22(3):209–215. doi: 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
- 82.Dalal H.M., Taylor R.S. BMJ Publishing Group Ltd and British Cardiovascular Society; 2016. Telehealth Technologies Could Improve Suboptimal Rates of Participation in Cardiac Rehabilitation. [DOI] [PubMed] [Google Scholar]
- 83.Balady G.J., Ades P.A., Bittner V.A., et al. Referral, enrollment, and delivery of cardiac rehabilitation/secondary prevention programs at clinical centers and beyond: a presidential advisory from the American Heart Association. Circulation. 2011;124(25):2951–2960. doi: 10.1161/CIR.0b013e31823b21e2. [DOI] [PubMed] [Google Scholar]
- 84.Ghram A., Briki W., Mansoor H., Al-Mohannadi A.S., Lavie C.J., Chamari K. Home-based exercise can be beneficial for counteracting sedentary behavior and physical inactivity during the COVID-19 pandemic in older adults. Postgr Med. 2020 doi: 10.1080/00325481.2020.1860394. Published online. [DOI] [PubMed] [Google Scholar]
- 85.Ribisl P.M. The inclusive chronic disease model: reaching beyond cardiopulmonary patients. Clin Invest Med. 2001;24(3):S10. [Google Scholar]
- 86.Arena R., Lavie C.J., Hivert M.-F., Williams M.A., Briggs P.D., Guazzi M. Who will deliver comprehensive healthy lifestyle interventions to combat non-communicable disease? Introducing the healthy lifestyle practitioner discipline. Expert Rev Cardiovasc Ther. 2016;14(1):15–22. doi: 10.1586/14779072.2016.1107477. [DOI] [PubMed] [Google Scholar]