Abstract
Background:
Health administrative databases may provide rich sources of data for the study of outcomes following burn. We aimed to determine the accuracy of International Classification of Diseases diagnoses codes for burn in a population-based administrative database.
Methods:
Data from a regional burn center’s clinical registry of patients admitted between 2006–2013 were linked to administrative databases. Burn total body surface area (TBSA), depth, mechanism, and inhalation injury were compared between the registry and administrative records. The sensitivity, specificity, and positive and negative predictive values were determined, and coding agreement was assessed with the kappa statistic.
Results:
1215 burn center patients were linked to administrative records. TBSA codes were highly sensitive and specific for ≥10 and ≥20% TBSA (89/93% sensitive and 95/97% specific), with excellent agreement (k, 0.85/k, 0.88). Codes were weakly sensitive (68%) in identifying ≥10% TBSA full-thickness burn, though highly specific (86%) with moderate agreement (k,0.46). Codes for inhalation injury had limited sensitivity (43%) but high specificity (99%) with moderate agreement (k, 0.54). Burn mechanism had excellent coding agreement (k, 0.84).
Conclusions:
Administrative data diagnosis codes accurately identify burn by burn size and mechanism, while identification of inhalation injury or full-thickness burns is less sensitive but highly specific.
Keywords: Burns, Burn, Validation, Administrative data
1. Introduction
The care of the burn-injured patient has evolved over the past several decades, such that all but the most devastating injuries are survivable [1]. Alongside these improvements, a need to understand the long-term outcomes of burn patients has emerged to inform development of interventions to mitigate long-term morbidity following burn. However, a paucity of data regarding the long-term burden of burn exists [2,3].
Our current knowledge of outcomes after burn derives from studies hampered by small cohort sizes and loss to follow up with limited data available beyond 2 years after injury [3–5]. Many of these challenges can be overcome through population-based studies that utilize health administrative data. These data facilitate the long-term study of burn-injured individuals through the analysis of health care utilization data. Such data have been successfully utilized to study long-term mortality following major burn [6,7]. In other cohorts, these data have been used to evaluate self-harm risk, cancer risk, and to describe long-term health trajectories [7–12].
A key limitation of administrative data is the potential for misclassification bias. The identification of patients with specific conditions, such as burn, depends on the accuracy with which these conditions are coded within administrative databases. In Canadian administrative databases, diseases are coded using the tenth revision of the International Classification of Diseases (ICD-10) [13]. While the validity of these codes has been demonstrated for many conditions [14–18], the accuracy of codes for burn size, depth, body region, mechanism and inhalation injury is unknown. Prior to the use of administrative databases to study the long-term outcomes of burn-injured patients, it is important that these diagnosis codes are evaluated and proven sufficiently accurate. Therefore, the objective of this study was to determine the accuracy of ICD-10 diagnosis codes for burn and inhalation injury in a provincial health administrative database, using comprehensive clinical data from the same patients in a second regional clinical database.
2. Methods
2.1. Study design
This study is reported in accordance with the guidelines for diagnostic and validation studies of health administrative data[19]. Records derived from a clinical burn registry reflecting the acute care of burn patients admitted to the largest burn center in Canada were linked to administrative discharge data to validate ICD-10 diagnosis and external cause codes for burn. This study was approved by the Research Ethics Board of Sunnybrook Health Sciences Centre.
2.2. Data sources
Two distinct healthcare datasets were used for the study:(1) a provincial health administrative database, and (2) a comprehensive regional clinical registry. The clinical burn registry contains data regarding patient demographics, injury characteristics, and inpatient complications for all patients admitted to the burn center. Data were entered into the registry by a trained burn registrar and collected in accordance with the National Burn Repository data standard [20]. TBSA estimations were derived from the Lund and Browder chart completed by the admitting burn surgeon on admission. Presence of inhalation injury was documented on admission based on bronchoscopic evaluation performed by the admitting burn surgeon. Mechanism of injury was recorded in the medical record based on the admission history taken by the surgeon (self-reported by patient or collateral history from witnesses).
To determine the accuracy of burn diagnosis codes in administrative data, the burn registry was linked to the Registered Persons Database (RPDB). The RPDB contains demographic information on all residents of Ontario, and is linked by unique identifier to the Discharge Abstract Database (DAD), a population-based administrative database that records all discharges from acute care hospitals in the province of Ontario after the year 1991. Diagnoses responsible for admission are coded in the DAD according to a modification of the 10th revision of the International Classification of Diseases, and each admission can contain up to 25 recorded diagnoses. The Canadian Institute for Health Information coding standards require that data abstractors assign burn diagnosis codes according to each affected body area, along with codes reflecting the TBSA and external cause of injury[21]. These data were made available through the Institute of Clinical and Evaluative Sciences (ICES). ICES is a prescribed entity under the Province of Ontario’s privacy law and holds a large proportion of the administrative health data collected in Ontario. These datasets were linked using unique encoded identifiers and analyzed at ICES.
2.3. Validation cohort
We used the clinical registry to identify all patients aged 16 years and older who were admitted to the burn center for the treatment of acute burn between January 1, 2006 and December 31, 2013. Patients were excluded if data regarding their burn extent, presence of inhalation injury, or mechanism of injury were missing in the clinical burn registry. The TBSA estimation, % full-thickness burn estimation, mechanism of burn, and diagnosis of inhalation injury from the burn registry were considered the reference standard.
2.4. Administrative data and record linkage
Once the validation cohort was assembled, each patient record was linked to administrative data through both deterministic and probabilistic linkage. Deterministic linkage was performed based on hospital health record number and date of birth. Where deterministic linkage was not possible, probabilistic linkage on patient name was used.
2.5. Validation
The ICD-10 diagnosis codes related to the identification of burn, characterization of burn extent, depth and mechanism, and identification of inhalation injury were defined a priori and used to derive case definitions for validation (Table 1).
Table 1 –
Case definitions for validation.
| ICD-10CAa Diagnosis code(s) | |
|---|---|
| ≥10% TBSAb | T31.10-T31.99 |
| ≥20% TBSAb | T31.20-T31.99 |
| Inhalation injury | T27.0-T27.3 |
| TBSAb | |
| 0–10 | T31.0 |
| 11–20 | T31.1 |
| 21–30 | T31.2 |
| 31–40 | T31.3 |
| 41–50 | T31.4 |
| 51–60 | T31.5 |
| 61–70 | T31.6 |
| 71–80 | T31.7 |
| 81–90 | T31.8 |
| >90 | T31.9 |
| ≥10% full-thickness TBSAb | T31.12, T31.22–23, T31.32–34, T31.42–45, T31.52–56, T31.62–67, T31.72–78, T31.82–89, T31.92–99 |
| Burn mechanism | |
| Flame | X00-X09 |
| Contact | X10-X19 |
| Electrical | W85-W87 |
ICD-10CA, International Statistical Classification of Diseases and Related Health Problems, 10th revision, Canada.
TBSA, total body surface area.
We compared case definitions derived from the DAD to those derived from the reference standard. Diagnoses were coded as binary variables for each patient; for example, inhalation injury was coded as present or absent in the clinical registry and as positive or negative based on DAD diagnoses. For each case definition, each patient was classified as true positive (registry present, DAD positive), true negative (registry absent, DAD negative), false positive (registry absent, DAD positive), and false negative (registry present, DAD negative).
We sought to determine whether the administrative data were accurate in identifying patients with ≥10% TBSA, ≥20% TBSA, ≥10% full-thickness burn, and inhalation injury, as compared to the clinical registry. These TBSA cutoffs were chosen as they identify patients who meet criteria for referral to a burn center (≥10% TBSA) [22] and major burn (≥20% TBSA). This was assessed in two ways: (1) by determining the agreement for each case definition between the clinical registry and administrative data using the kappa coefficient, and (2) by calculating the sensitivity, specificity, and positive and negative predictive values (PPV, NPV). Accuracy in burn mechanism between the clinical registry and administrative data was assessed by exact agreement. For each mechanism (flame, electrical, contact), coding agreement was assessed using the kappa coefficient. To understand how accurately TBSA estimates are coded, we evaluated agreement between TBSA estimates within each decile of % TBSA between the clinical registry and administrative data using the kappa coefficient.
For our purposes, accuracy of 80% or greater and a kappa coefficient of 0.60 or greater were considered targets for validation [23,24]. Based on prior studies of the validity of other diagnoses codes in the same database, we expected these codes to have sensitivity in excess of 75% and specificity in excess of 90% [14,15,18,25–27].
2.6. Statistical analysis
Descriptive statistics were used to describe the validation cohort. Means and standard deviations, or medians and interquartile ranges were calculated for continuous variables, as appropriate. For discrete variables, absolute frequencies were measured. Sensitivity, specificity, PPV, NPV, accuracy (% exact agreement) and the kappa coefficient were calculated for each case definition. Agreement was considered excellent where kappa was greater than 0.81; substantial where kappa ranged between 0.61–0.80 and moderate where kappa was between 0.41–0.60 [28]. All analyses were conducted on de-identified data using SAS Version 9.4 (Cary, NC).
3. Results
We identified 1252 patients in the burn registry meeting inclusion criteria. Of these, 17 were excluded prior to linkage due to missing data. We were able to deterministically link 89% (n=1099) patients to administrative data; the remaining 11% (n=136) were linked probabilistically (Fig. 1).
Fig. 1 –
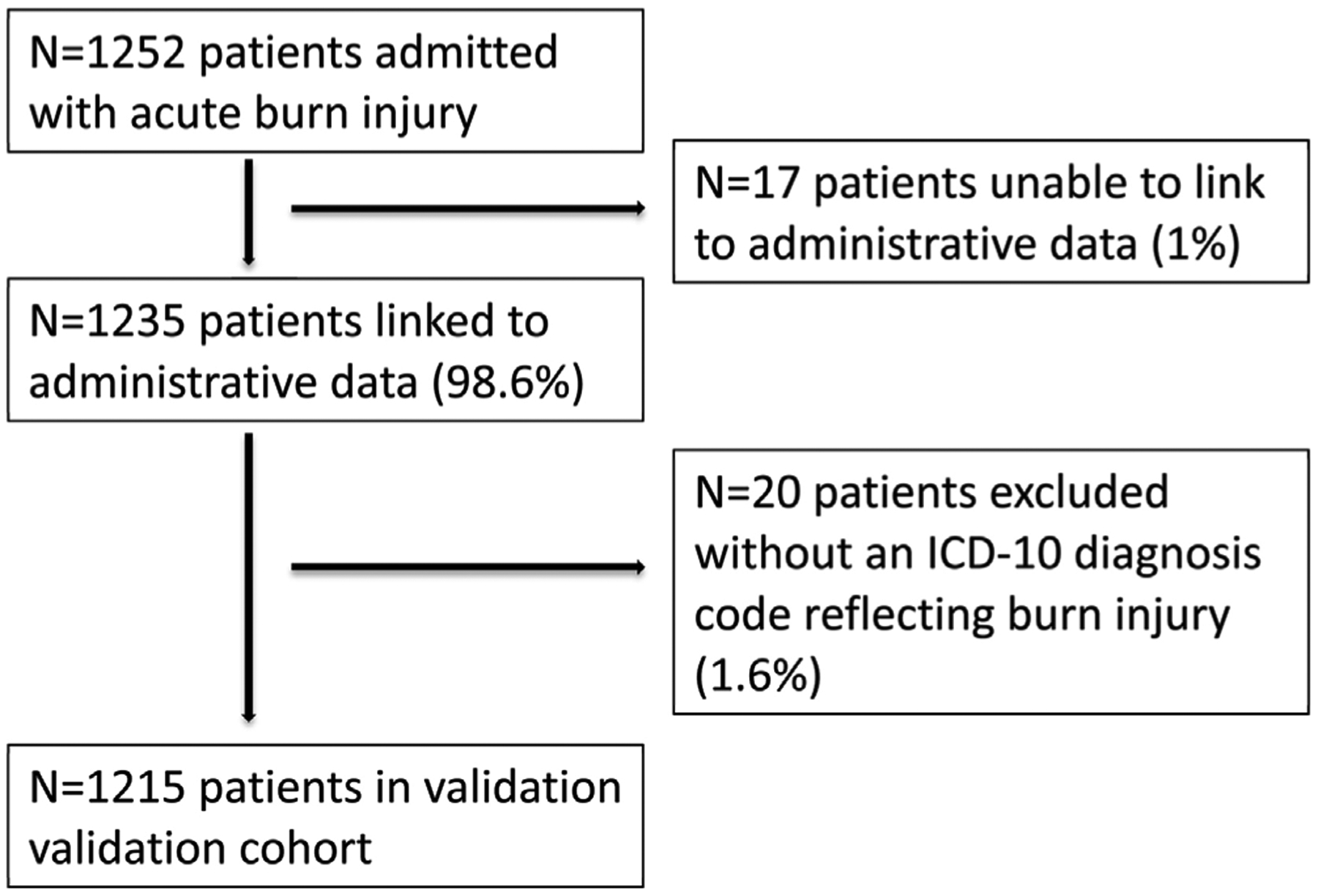
Derivation and linkage of validation cohort. ICD-10, International Classification of Diseases, 10th edition.
The patient and injury characteristics of the validation cohort are presented in Table 2. Most patients (73%, n=890) were men, and the median age of patients was 50 years. The median TBSA was 7.8%, with the most frequent mechanism being flame burns (61%, n=731).
Table 2 –
Patient and injury characteristics of validation cohort.
| Patient characteristics | |
| Median age, years (IQRa) | 50 (35–62) |
| Male (%) | 890 (73) |
| Injury characteristics | |
| Median % TBSAb (IQR) | 7.8 (3.1–16.5) |
| Median % full-thickness TBSAb (IQRa) | 0.5 (0–5) |
| Inhalation injury (%) | 195 (16) |
| Mechanism (%) | |
| Flame | 731 (61) |
| Contact | 385 (32) |
| Electrical | 90 (7) |
| Median APACHEc II Score (IQRa) | 3 (1–7) |
| In-hospital mortality (%) | 12 (1) |
IQR, interquartile range.
TBSA, total body surface area.
APACHE, acute physiology and chronic health evaluation.
In the burn registry, the prevalence of ≥10% TBSA burn was 41% (n=502); the prevalence of ≥20% TBSA burn was 20% (n=245). 17% of patients had ≥10% TBSA full-thickness burns. The prevalence of inhalation injury was 16% (n=196).
3.1. Burn size
The diagnosis codes in the administrative data identified both ≥10% TBSA and ≥20% TBSA with high sensitivity and specificity (Table 3). In identifying patients with ≥10% TBSA, administrative data were 89% sensitive and 95% specific; for ≥20% TBSA, administrative data were 93% sensitive and 97% specific. Agreement between the clinical registry and administrative data in discriminating between ≥10/20% and <10/20% TBSA injury was excellent (k=0.85 and 0.88 respectively). Accuracy (exact agreement) between TBSA estimates within each decile of % TBSA was 87%. Coding agreement by TBSA decile ranged from moderate to excellent (k, 0.58–0.86), and generally increased with increasing burn size (Table 4).
Table 3 –
Estimates of diagnostic accuracy of administrative data.
| Sensitivity (%, 95%CIa) | Specificity (%, 95% CIa) | Positive predictive value (%, 95% CIa) | Negative predictive value (%, 95% CIa) | |
|---|---|---|---|---|
| ≥10% TBSAb | 89 (86–92) | 95 (93–97) | 93 (90–95) | 93 (91–95) |
| ≥20% TBSAb | 93 (89–96) | 97 (95–98) | 88 (84–92) | 98 (97–99) |
| ≥10% full-thickness TBSAb | 68 (61–74) | 86 (83–88) | 49 (43–55) | 93 (91–95) |
| Inhalation injury | 43 (36–50) | 99 (98–100) | 93 (88–98) | 90 (88–92) |
| Burn mechanism | ||||
| Flame | 93 (87–92) | 91 (88–93) | 94 (92–95) | 85 (82–88) |
| Contact | 89 (85–92) | 93 (91–95) | 86 (82–89) | 95 (93–96) |
| Electrical | 76 (65–84) | 99 (99–100) | 93 (85–98) | 98 (97–99) |
CI, confidence interval.
TBSA, total body surface area.
Table 4 –
Prevalence and accuracy of specific injury characteristics.
| Prevalence (%) | Accuracy (%) | Kappa (95%CIa) | Agreement | ||
|---|---|---|---|---|---|
| Burn registry | Administrative data | ||||
| ≥10% TBSAb | 41 | 40 | 93 | 0.85 (0.82–0.88) | Excellent |
| ≥20% TBSAb | 20 | 21 | 96 | 0.88 (0.84–0.91) | Excellent |
| ≥10% full-thickness TBSAb | 17 | 23 | 83 | 0.46 (0.40–0.52) | Moderate |
| Inhalation injury | 16 | 7 | 90 | 0.54 (0.47–0.61) | Moderate |
| Mechanism | 88 | 0.84 (0.81–0.87) | Excellent | ||
| Flame | 61 | 60 | 92 | ||
| Contact | 32 | 34 | 93 | ||
| Electrical | 7 | 6 | 98 | ||
| %TBSAb | 87 | ||||
| 0–10 | 58 | 60 | 92 | 0.83 (0.80–0.86) | Excellent |
| 11–20 | 21 | 19 | 92 | 0.74 (0.70–0.79) | Substantial |
| 21–30 | 9 | 10 | 96 | 0.77 (0.70–0.83) | Substantial |
| 31–40 | 4 | 4 | 98 | 0.77 (0.68–0.87) | Substantial |
| 41–50 | 3 | 3 | 99 | 0.73 (0.60–0.86) | Substantial |
| 51–60 | 2 | 2 | 99 | 0.72 (0.57–0.86) | Substantial |
| 61–70 | 1 | 2 | 99 | 0.58 (0.38–0.78) | Moderate |
| 71–80 | 0.9 | 0.8 | 99.5 | 0.70 (0.47–0.93) | Substantial |
| 81–90 | 0.3 | 0.7 | 99.7 | 0.67 (0.36–0.97) | Moderate |
| >90 | 0.7 | 0.5 | 99.8 | 0.86 (0.66–1) | Excellent |
CI, confidence interval.
TBSA, total body surface area.
We also evaluated the sensitivity of diagnosis codes to identify patients with full-thickness burns of ≥10% TBSA. These codes were moderately sensitive (68%) and highly specific (86%), with moderate agreement between the burn registry and administrative data (k, 0.46).
3.2. Inhalation injury
The administrative data diagnoses codes were poorly sensitive (43%) but highly specific (99%) for inhalation injury. Agreement between the clinical registry and administrative data was moderate (k=0.54).
3.3. Burn mechanism
We first sought to determine overall agreement between the clinical registry and administrative data for burn mechanism, and then to determine coding accuracy for flame, contact, and electrical burns. An external cause of injury code was missing in the administrative data for 9 patients (0.7%). Among the remaining patients, overall agreement was excellent (k, 0.84). Diagnoses codes were highly sensitive for flame and contact burns (93% and 89%), while moderately sensitive for electrical burns (76%). Specificity for all 3 mechanisms was excellent (91–99%, Table 3).
4. Discussion
We conducted a retrospective validation study of the accuracy of burn diagnosis codes in a health administrative database in Ontario, Canada. Our findings demonstrate that diagnoses codes were highly sensitive and specific for burn size and mechanism, while burn depth and inhalation injury were less sensitive and specific. The high accuracy of diagnoses codes for burn extent and burn mechanism suggests that administrative data can be reliably used to identify cohorts of burn-injured patients on the basis of either TBSA or mechanism. The diagnoses codes had the greatest sensitivity and specificity in discriminating between greater and less than 20% TBSA injury, with lower but strong agreement below this threshold. We observed greater reliability with increasing deciles of % TBSA, consistent with prior studies demonstrating that the accuracy of burn size estimations increases with increasing burn extent[29].
The diagnoses codes for inhalation injury had poor sensitivity; despite high specificity, only 43% of patients with inhalation injury were identified as such in the administrative data. The significant difference in prevalence of inhalation injury between the burn registry and administrative data (16% vs. 7%) suggests that inhalation injury is not coded as commonly during routine medical records abstraction for administrative purposes. This may reflect low clinical suspicion and confirmatory diagnostic testing, poor documentation of inhalation injury in the medical record, or incomplete coding of inhalation injury as a secondary diagnosis by the data abstractor. As a result, these codes cannot be reliably used to identify burn-injured patients with inhalation injury.
We found that diagnoses codes for ≥10% full-thickness burns were weakly sensitive and highly specific, with moderate agreement. The characterization of patients based on the extent of full-thickness burn is limited by the nature of ICD-10 diagnosis codes for burn depth. This is expressed in deciles, such that both 0% and 9% full-thickness have the same diagnosis code; this same code is used when burn depth is unspecified. As a result, for patients with <10% TBSA, it is impossible to discriminate between patients with and without full-thickness burns. This limits the ability of researchers to distinguish patients with potentially significant functional burns that will very likely undergo surgery, i.e. full-thickness burns to the face, feet, or hands, from those with more minor burns.
A key limitation of this work is its generalizability to administrative databases in other settings. Furthermore, data derived from the largest regional burn center in Canada were used as the reference standard. Diagnoses codes in administrative data are assigned based on abstraction from the medical record. Therefore, the accuracy of TBSA estimations in administrative data depends on the accuracy of estimations in the medical record. While we demonstrated high accuracy of these codes in our study, this reflects comparison to estimations performed by expert burn surgeons. TBSA estimations have previously been demonstrated to vary widely, even among burn surgeons [30–32]. It is reasonable to assume that TBSA estimations might be less accurate outside of regional burn centers. This will be a limitation of future studies utilizing health administrative data to identify burn-injured patients, and might result in misclassification of patients based on their burn extent. To the best of our knowledge, this is the first validation study of burn diagnosis codes, limiting our ability to compare our results to studies in other settings.
5. Conclusion
This validation study linked a clinical burn registry to population-based health administrative database in order to assess the validity of diagnoses codes for burn size, depth, mechanism, and inhalation injury. We have demonstrated that diagnosis codes for TBSA and burn mechanism are highly sensitive and specific, with excellent reliability between the administrative data and burn registry. Our findings suggest that patients with major burn can be reliably identified in administrative data. This should encourage investigators to consider the potential advantages of using health administrative data to further contribute to our understanding of burn and its impact at both the patient and health care system levels.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. Dr Nathens is supported by the DeSouza Chair in Trauma Research. Dr Jeschke is supported by: Canadian Institutes of Health Research #123336 and CFI Leader’s Opportunity Fund Project # 25407, NIH RO1 GM087285-01. Dr Fowler’s work was supported by a personnel award from the Heart and Stroke Foundation, Ontario Provincial Office. Dr Karanicolas is supported by a CIHR New Investigator Award.
Footnotes
Disclaimer
This study was supported by the Institute for Clinical Evaluative Sciences (ICES), which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI.
Conflicts of interest
None reported.
REFERENCES
- [1].Roberts G, Lloyd M, Parker M, Martin R, Philp B, Shelley O, et al. The Baux score is dead. Long live the Baux score: a 27-year retrospective cohort study of mortality at a regional burns service. J Trauma Acute Care Surg 2012;72:251–6, doi: 10.1097/TA.0b013e31824052bb. [DOI] [PubMed] [Google Scholar]
- [2].Brych SB, Engrav LH, Rivara FP, Ptacek JT, Lezotte DC, Esselman PC, et al. Time off work and return to work rates after burns: systematic review of the literature and a large two-center series. J Burn Care Rehabil 2001;22:401–5. [DOI] [PubMed] [Google Scholar]
- [3].van Baar ME, Essink-Bot ML, Oen IMMH, Dokter J, Boxma H, van Beeck EF. Functional outcome after burns: a review. Burns 2006;32:1–9, doi: 10.1016/j.burns.2005.08.007. [DOI] [PubMed] [Google Scholar]
- [4].Druery M, Brown T, Muller M. Long term functional outcomes and quality of life following severe burn injury. Burns 2005;31:692–5. [DOI] [PubMed] [Google Scholar]
- [5].Wasiak J, Lee SJ, Paul E, Mahar P, Pfitzer B, Spinks A, et al. Predictors of health status and health-related quality of life 12 months after severe burn. Burns 2014;40:568–74, doi: 10.1016/j.burns.2014.01.021. [DOI] [PubMed] [Google Scholar]
- [6].Duke JM, Boyd JH, Randall SM, Wood FM. Long term mortality in a population-based cohort of adolescents, and young and middle-aged adults with burn injury in western Australia: a 33-year study. Accid Anal Prev 2015;85:118–24, doi: 10.1016/j.aap.2015.09.011. [DOI] [PubMed] [Google Scholar]
- [7].Duke JM, Boyd JH, Rea S, Randall SM, Wood FM. Long-term mortality among older adults with burn injury: a population-based study in Australia. Bull World Health Organ 2015;93:400–6, doi: 10.2471/BLT.14.149146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Lone NI, Gillies MA, Haddow C, Dobbie R, Rowan KM, Wild SH, et al. Five year mortality and hospital costs associated with surviving intensive care. Am J Respir Crit Care Med 2016; 194:198–208, doi: 10.1164/rccm.201511-2234OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ou S-M, Chu H, Chao P-W, Lee Y-J, Kuo S-C, Chen T-J, et al. Long-term mortality and major adverse cardiovascular events in sepsis survivors: a nationwide population-based study. Am J Respir Crit Care Med 2016;194:209–17, doi: 10.1164/rccm.201510-2023OC. [DOI] [PubMed] [Google Scholar]
- [10].Duke JM, Bauer J, Fear MW, Rea S, Wood FM, Boyd J. Burn injury, gender and cancer risk: population-based cohort study using data from Scotland and western Australia. BMJ Open 2014;4: e003845, doi: 10.1136/bmjopen-2013-003845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hill AD, Fowler RA, Pinto R, Herridge MS, Cuthbertson BH, Scales DC. Long-term outcomes and healthcare utilization following critical illness — a population-based study. Crit Care 2016;20:76, doi: 10.1186/s13054-016-1248-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Bhatti JA, Nathens AB, Thiruchelvam D, Grantcharov T, Goldstein BI, Redelmeier DA. Self-harm emergencies after bariatric surgery: a population-based cohort study. AMA Surg 2016;151:226–32, doi: 10.1001/jamasurg.2015.3414. [DOI] [PubMed] [Google Scholar]
- [13].ICD-10-CA | CIHI n.d. https://www.cihi.ca/en/data-and-standards/standards/classification-and-coding/icd-10-ca [Accessed May 18 May 2016].
- [14].Hussain MA, Mamdani M, Saposnik G, Tu JV, Turkel-Parrella D, Spears J, et al. Validation of carotid artery revascularization coding in Ontario health administrative databases. Clin Invest Med 2016;39:E73–8. [DOI] [PubMed] [Google Scholar]
- [15].Widdifield J, Ivers NM, Young J, Green D, Jaakkimainen L, Butt DA, et al. Development and validation of an administrative data algorithm to estimate the disease burden and epidemiology of multiple sclerosis in Ontario, Canada. Mult Scler 2015;21:1045–54, doi: 10.1177/1352458514556303. [DOI] [PubMed] [Google Scholar]
- [16].Welk B, Loh E, Shariff SZ, Liu K, Siddiqi F. An administrative data algorithm to identify traumatic spinal cord injured patients: a validation study. Spinal Cord 2014;52:34–8. [DOI] [PubMed] [Google Scholar]
- [17].Lam NN, McArthur E, Kim SJ, Knoll GA. Validation of kidney transplantation using administrative data. Can J Kidney Heal Dis 2015;2:20, doi: 10.1186/s40697-015-0054-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Benchimol EI, Guttmann A, Mack DR, Nguyen GC, Marshall JK, Gregor JC, et al. Validation of international algorithms to identify adults with inflammatory bowel disease in health administrative data from Ontario, Canada. J Clin Epidemiol 2014;67:887–96. [DOI] [PubMed] [Google Scholar]
- [19].Benchimol EI, Manuel DG, To T, Griffiths AM, Rabeneck L, Guttmann A. Development and use of reporting guidelines for assessing the quality of validation studies of health administrative data. J Clin Epidemiol 2011;64:821–9, doi: 10.1016/j.jclinepi.2010.10.006. [DOI] [PubMed] [Google Scholar]
- [20].National Burn Data Standard n.d. http://ameriburn.org/NBDS_Final_061615.pdf [Accessed 29 February 2016].
- [21].Canadian Coding Standards for Version 2015 ICD-10-CA and CCI. n.d.
- [22].American Burn Association Burn Center Referral Criteria n.d. http://www.ameriburn.org/BurnCenterReferralCriteria.pdf [Accessed 29 June 2015].
- [23].Cicchetti DV. The precision of reliability and validity estimates re-visited: distinguishing between clinical and statistical significance of sample size requirements. J Clin Exp Neuropsychol 2001;23:695–700, doi: 10.1076/jcen.23.5.695.1249. [DOI] [PubMed] [Google Scholar]
- [24].Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. [PubMed] [Google Scholar]
- [25].Han T, Kim J, Yang M, Han K, Han S, Jung J, et al. A retrospective analysis of 19,157 burns patients: 18-year experience from Hallym Burn Center in Seoul, Korea. Burns 2005;31:465–70. [DOI] [PubMed] [Google Scholar]
- [26].Kurdyak P, Lin E, Green D, Vigod S. Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatry 2015;60:362–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Gershon AS, Wang C, Guan J, Vasilevska-Ristovska J, Cicutto L, To T. Identifying individuals with physcian diagnosed COPD in health administrative databases. COPD 2009;6:388–94. [DOI] [PubMed] [Google Scholar]
- [28].Viera A, Garrett J. Understanding interobserver agreement: the kappa statistic. Fam Med 2005;37:360–3. [PubMed] [Google Scholar]
- [29].Harish V, Raymond AP, Issler AC, Lajevardi SS, Chang L-Y, Maitz PKM, et al. Accuracy of burn size estimation in patients transferred to adult Burn Units in Sydney, Australia: an audit of 698 patients. Burns 2015;41:91–9, doi: 10.1016/j.burns.2014.05.005. [DOI] [PubMed] [Google Scholar]
- [30].Saffle JR, Edelman L, Morris SE. Regional air transport of burn patients: a case for telemedicine? J Trauma 2004;57:57–64 discussion 64. [DOI] [PubMed] [Google Scholar]
- [31].Harris LJ, Graetz I, Podila PSB, Wan J, Waters TM, Bailey JE. Characteristics of hospital and emergency care super-utilizers with multiple chronic conditions. J Emerg Med 2016;50:e203–14, doi: 10.1016/j.jemermed.2015.09.002. [DOI] [PubMed] [Google Scholar]
- [32].Parvizi D, Kamolz LP, Giretzlehner M, Haller HL, Trop M, Selig H, et al. The potential impact of wrong TBSA estimations on fluid resuscitation in patients suffering from burns: things to keep in mind. Burns 2014;40:241–5. [DOI] [PubMed] [Google Scholar]


