Abstract
Background
COVID-19 outbreak has adversely affected care of breast cancer patients world-wide. There is paucity of available data on cancer management in lower-middle income countries during this pandemic, we sought to determine the institutional approach towards management of breast cancer patients and the outcomes during COVID-19 pandemic at our institution.
Materials and methods
Clinicopathological and treatment record of cancer patients who presented to the Breast Clinic from 15th March to 31st December 2020 was retrieved from the institutional database for this retrospective clinical observational study.
Results
A total of 292 patients were qualified for the analysis in which 206 patients (70.5%) underwent breast cancer surgeries. Only 10 of them (4.9%) were identified to be COVID-19 virus positive on routine pre-operative RT-PCR test before elective surgeries. All were asymptomatic, received home-based care via telecommunication and were operated at a later date when test turned out negative. None of them developed any complications post-operatively. Another group of 86 patients (29.5%) were referred for Neoadjuvant/Systemic chemotherapy in which COVID-19 infection was detected in only 4 patients (4.6%) while receiving cycles. Two patients shown symptoms of cough and fever hence hospitalised but were not candidates for Intensive Care Unit admission while other two patient were asymptomatic and isolated at home. All patients recovered well and chemotherapy was commenced again after negative RT-PCR test. No mortality was observed.
Conclusion
Despite of being a global crisis particularly for cancer patients we observed infectivity, complications and fatality much lower among breast cancer cases. Further research is needed in this regard including public and private sector hospitals for better understanding behavior of COVID-19 disease and achieve common goal to combat COVID-19 and cancer together.
Keywords: COVID-19, Breast cancer, Neoadjuvant therapy, Pandemic
Highlights
-
•
Covid 19 infectivity and its impact found much lower in our study group as compared to world-wide data.
-
•
Majority of infected cases were asymptomatic despite of inherent weak immune system.
-
•
None of the cases showed disease progression while they were off treatment because of infective status.
1. Introduction
The fatal Coronavirus Disease 2019 (COVID-19) has emanated as a global pandemic unleashing a health and economic crises unprecedented in scope and magnitude. The infecting pathogen causing this disease was a beta coronavirus or severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) having its centre of origin in Wuhan, China where the first person contracting this infection was identified on 17th November 2019 [1,2]. Since then, it has gradually afflicted other countries of the world accounting for more than 97 million cases and 2 million deaths by 24th January 2021 [3]. Pakistan is among the most affected victim of COVID-19 outbreak with limited resources to curb against severe expected outcomes, till to date 532,412 confirmed cases were reported [4]. This pandemic was an inciting panic for us because of many reasons as little is known about this disease, less understanding about appropriate treatment and unavailability of effective vaccine with evidence to affect immunocompromised cases including cancer patients more severely than others.
Pakistan is a low middle income country with limited healthcare budget and limited resources. We have been facing serious consequences after being inflicted with COVID-19 outbreak as there is a lack of adequate testing facilities for COVID-19 country wide, insufficient supply of personal protective equipment for frontline responders and limited hospital capacity including ICU beds and ventilators. Moreover, fear of COVID-19 positive detection on testing does not allow many including breast cancer patients to get their test done or to get admitted in hospital if symptomatic and bear their treatment expenses resulting in deterioration of their health and delay in receiving standard cancer treatment.
The care of breast cancer patients has been adversely affected as a result of COVID-19 pandemic worldwide. There is a paucity of local data on breast cancer management during the attack of this contagion therefore our present study is designed to determine our institutional approach towards management of breast cancer patients and their outcomes. This study will assist to curtail knowledge gaps and adds invaluable input to our breast cancer practices during COVID-19 crises.
2. Material and methods
After the attainment of Ethical exemption from the Ethics Review Committee of Aga Khan University Hospital (reference number: 2020-5418-14043) in Pakistan, a retrospective single-centre clinical observational study was conducted in breast surgery unit. The study was registered under the German Clinical Trials Register (DRKS) in accordance with the declaration of Helsinki (Registration ID: DRKS00023807,https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00023807) and was conducted according to the STROCSS statement guidelines 2019 [5].
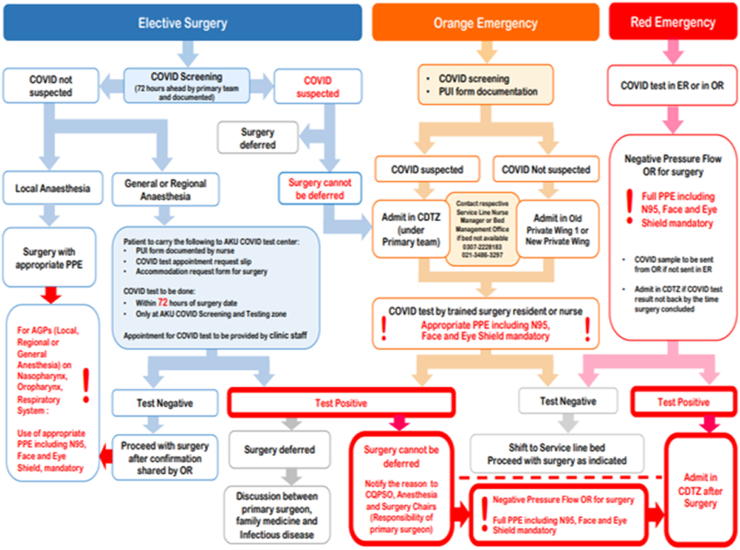
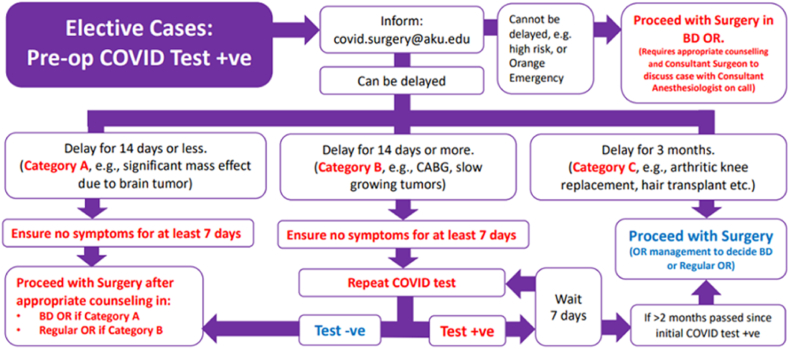
As per the inclusion criteria only cancer patients who presented to Breast Clinic from 15th March to 31st December 2020 which either underwent surgery or referred for Neoadjuvant/Systemic treatment were included. Those patients with incomplete medical records or lost to follow-up were excluded from the analysis. Information on demographic data, clinicopathological and treatment characteristics was retrieved from the prospectively maintained Institutional Breast Cancer Data base. In late March formal guidelines were designed and approved by Multidisciplinary Breast cancer team to individualized treatment during COVID-19 crises (Table 1). Late in April formal COVID-19 testing was made mandatory 72 h preoperatively for all cases, elective cases were marked blue. The algorithm was designed to clearly outline plan in those cases who found positive on COVID testing, breast surgeries were categorized in Group B (Fig. 1, Fig. 2).
Table 1.
Institutional approach to triaging of breast cancer surgery.
|
|
| |
| |
| |
| |
| |
| |
| |
|
|
| |
| |
|
|
| |
| |
| |
| |
| |
| |
| |
| |
|
Fig. 1.
COVID testing algorithm for surgery patients.
Fig. 2.
Plan for elective surgeries.
The data was collected on a self-designed proforma by the investigators. Information regarding age, grade, type, stage of breast cancer, immunohistochemical (IHC) status of oestrogen, progesterone and Her2 neu, co-morbid illness, neo-adjuvant chemo or hormonal therapy, type of surgery, pre-operative COVID-19 testing performed or not, testing result, whether surgery was deferred on the basis of result, post-operative hospital stay, development of any COVID-19 symptoms post-operatively during hospital stay or within one week after discharge or development of any surgical complications and survival status were collected for the analysis. Patients whose neo adjuvant treatments deferred because of positive COVID-19 status were contacted by one of the authors to collect confirmed data about delay in treatment/repeat testing and number of repeat test with outcome in addition to reviewing electronic medical records as many patients had there testing done from outside AKUH.
Data was analysed using statistical package for the social sciences (SPSS) (version 23.0). The categorical variables were represented by frequencies and percentages including procedures, COVID positivity, hormonal receptor status and quantitative variables like age were reported as mean/median.
3. Results
Overall, the data analysis carried out revealed that in a study population of 292 patients, significant proportion of them were diagnosed of breast cancer at a median age of 48 years (range = 22–79 years) having diabetes mellitus (30.8%) being the most prevalent co-morbid medical ailment among them. More than half of the patients (90.1%) were identified with invasive ductal carcinoma of grade III (39.7%). Majority of patients (82.9%) presented with stage II/III disease and Luminal A was the most frequent molecular subtype seen in 35.9% of cases (Table 2).
Table 2.
Demographic and clinicopathological data of breast cancer patients (N = 292).
| Patient characteristics | Details | N (%) |
|---|---|---|
| Age at diagnosis | <25 | 2 (0.7) |
| 25–45 | 98(33.6) | |
| 46–65 | 170 (58.2) | |
| >65 | 22 (7.5) | |
| Comorbidities | Diabetes | 90 (30.8) |
| Hypertension | 115 (39.4) | |
| Ischemic Heart Disease | 4 (1.4) | |
| None | 83 (28.4) | |
| Histologic Type | Invasive Ductal Carcinoma | 263 (90.1) |
| Invasive Lobular Carcinoma | 8 (2.7) | |
| Metaplastic Carcinoma | 11 (3.8) | |
| In-situ Ductal Carcinoma | 5 (1.7) | |
| Papillary Carcinoma | 2 (0.7) | |
| Mucinous Carcinoma | 1 (0.3) | |
| Others | 2 (0.7) | |
| Histologic Grade | Grade 1 | 12 (4.1) |
| Grade 2 | 164 (56.2) | |
| Grade 3 | 116 (39.7) | |
| Molecular Subtype | Luminal A | 105 (35.9) |
| Luminal B | 80(27.3) | |
| Triple Negative | 68 (23.5) | |
| Her 2 enriched | 39 (13.3) | |
| Tumor Stage (pathological) | Stage 0 | 25 (8.5) |
| Stage I | 15 (5.2) | |
| Stage II | 106 (36.3) | |
| Stage III | 136 (46.6) | |
| Stage IV | 10 (3.4) |
Following the hospital's standard protocol, pre-operative COVID-19 RT-PCR test was made mandatory within 72 h before elective surgeries (Fig. 1). Cases were categorized in three groups according to nature of disease, breast cancer surgeries were kept in group B (Fig. 2). Over all infectivity in elective surgeries at our institution from April–July 2020 was 139/2456 (5.6%) and from August–December 2020 was 53/4631 (1.1%). A total of 206 patients were subjected to Breast cancer surgeries and infectivity observed among these group from April–July was 07/66 (10.6%) and from August–December was 03/140 (2.1%). All of these were asymptomatic hence quarantined at home. Besides this a telecommunication network was established linking these COVID-19 positive patients with their primary consultant, infectious disease specialist and nurses to monitor their health and identify any worsening symptoms prompting admission in hospital. They were retested after 14 days as per designed guidelines and if test turned out negative surgery was performed. There were 4 patients who were tested negative more than 4 weeks after first positive test hence their procedures were performed after 5 weeks. The mean hospital stay was 24 h (18–27 h). None of the patients developed any signs and symptoms of COVID-19 disease or surgical complications post-operatively. All postoperative patients were asked to visit wound clinic once in a week, breast care nurse regularly monitored their wound through teleconsultations.
A total of 74 patients received Neoadjuvant chemotherapy, 2 were kept on Neoadjuvant Hormonal Treatment while Stage IV disease was identified in 10 patients and referred subsequently for primary systemic treatment. Out of which only 4 patients (4.6%) were tested positive for COVID-19 infection; two were symptomatic and both were treated in hospital as developed cough and low grade fever however none of them developed any serious complications or shifted to ICU. One was 75 years old lady with no comorbid while another was 53 years old having comorbid including diabetes, hypertension and recent cardiac bypass surgery, both recovered well. The treatment commenced after 4 weeks when symptoms resolved and were tested negative for COVID-19. Other two patients were completely asymptomatic and tested only because of positive exposure history hence kept in isolation for a week subsequently chemotherapy was commenced again. None of these individuals shown disease progression while kept off chemotherapy during this time period (Table 3).
Table 3.
Treatment Data and COVID-19 status of Breast Cancer Patients (N = 292).
| Patient characteristics | Details | N (%) |
|---|---|---|
| Pre-operative COVID-19 test Result (n = 206) | Positive | 10 (4.9) |
| Negative | 196 (95.1) | |
| Surgical Procedure (n = 206) | Modified Radical Mastectomy | 94 (45.6) |
| Simple Mastectomy + Sentinel node biopsy | 25 (12.1) | |
| Oncoplastic Conservative Surgery + Sentinel node biopsy | 66 (32.1) | |
| WLE and Axillary Sampling | 9 (4.4) | |
| Others (Reconstruction, Axillary Clearance) | 12 (5.8) | |
| Systemic Treatment (n = 86) | Neo adjuvant Chemotherapy | 74 (86.1) |
| Systemic Chemotherapy | 10 (11.6) | |
| Hormonal Treatment | 2 (2.3) | |
| COVID 19 status in patients on Neoadjuvant/Systemic Chemotherapy. (n = 86) | Positive | 4 (4.6) |
| Negative | 82 (95.4) |
4. Discussion
Pakistan reported first case of COVID-19 on 26th February 2020 who travelled from Iran, till that Pakistan has not designed any concrete policy to tackle this epidemic so as our institution [4]. However standard preventive measures were undertaken since early March. Late in March exponential increase in infectivity was a call to design robust policy in order to avoid perilous contagion spread in hospital, hence strategy was designed as per standard guidelines following worldwide [6]. Following that integrated multidisciplinary comprehensive breast cancer care guidelines were also designed incorporating recommendations from all the stakeholders. Mammographic screening, cancer surveillance services, elective non-cancer surgeries and reconstructive surgeries had been temporarily suspended in the beginning. Non-urgent clinic appointments were deferred while videoconferencing and telehealth facilities were increasingly used amidst this unfurling health crises. Monitoring all patients and staff for the suspected COVID-19 infection and inquiring regarding travel history had been made mandatory before entering clinic or operation theatre. Specially designed negative pressure air flow system were assigned to handle COVID-19 cases or emergency cases whose COVID-19 status were not known which further controlled the situation within institution. Literature shown that guidelines have been efficaciously followed by every cancer care institute worldwide and literature search had shown promising results as a study conducted by Fregatti in Italy unravelled that if necessary preventive measures were fulfilled, neither patients nor health care workers tested positive for COVID-19 after breast surgery [7]. American College of Surgeons, ESMO and other cancer care organizations issued essential guidelines on the treatment strategies of breast cancer patients in order to deliver standardized quality care by mitigating exposure to COVID-19 among patients and health care professionals without jeopardizing the health of them at the crucial time when health care resources are allocated to participate more in ensuing COVID-19 outbreak response [8,9].
Breast cancer patients can easily become a victim of this virulent virus as compared to general population owing to their inherently fragile immune system as a consequence of their disease and anti-tumour therapies [10]. Our experience had shown that 10 out of 206 (4.9%) breast cancer cases operated during the study time period found positive of COVID-19 virus, this rate was almost doubled in comparison to other elective surgeries apart from cancer 2.7% (192/7087) endorsing that cancer patients are at much higher risk than general population though all virus infected breast cancer patients were asymptomatic and none developed any sinister complication post-operatively. A large proportion of patients were also referred for Neoadjuvant treatment according to designed institutional guidelines including stage II- IV cases, 4 patients became positive during this treatment, and fortunately they recovered well without any complication. On contrary, figures reported from multiple cancer institutes worldwide showed much higher infectivity rate and complications with increased mortality as study published from Wuhan reported incidence of infection among cancer cases (0.79%) found to be much higher than the overall incidence of COVID‐19 cases over the same time period (0.37%) [10]. Likewise, another case series from China reported that cancer cases were associated with higher rate of complications including ICU admissions, invasive ventilation or mortality (39% with cancer vs. 8% without cancer) [11]. Data by Vuagnat et al. from the Institut Curie hospitals, Paris revealed that out of 76 breast cancer patients having suspicion of COVID-19, 59 turned out to be positive [12].
Our data had shown that overall mortality rate in our institution among breast cancer cases affected with SARS-CoV-2 virus was 0%, again fatality rate from other institutions reported was up to 5.6% among cancer cases [13]. Onder et al. from Italy reviewed demographics of cases succumbed to COVID-19 and found 20.3% were cancer patients (72 cancer patients out of 355 deaths). They attributed different factors responsible for such high death rate among cancer cases including frequent hospital visits, immunocompromised state, and advanced age, co morbid or poor functional status [14].
Our results endorsed the fact that infectivity and mortality rate in Pakistan is comparatively much less than other nations of the world as a result of this contagion. The anecdotal evidence from India has also proven the fact that despite of high viral load and infectivity among community mortality rate is much lower. Several theories had been put forward to explain this odd response to COVID-19, this may be attributed because the virus responsible for infecting people here must had undergone mutation rendering it less virulent or might population have robust levels of immunity against it due to life time exposure to high microbial load like dengue, malaria, typhoid or universal BCG vaccination all being a source to develop innate and adaptive immunity. The cross immunity or genetic diversity in immune responses, ACE 2 gene lays on the X-chromosome has additional advantage allowing females to be potentially heterozygous or environmental factors like high temperature and high humidity in Karachi could be the reason for lower susceptibility to COVID-19 [15,16].
5. Limitations
Understanding the fact that there are certain limitations of this study as being a single center experience having small sample size which might not be a true representative of the entire population plus the number of surgeries performed in the COVID-19 era decreased significantly as compared to pre-COVID-19. The management guidelines outlined in our study can be of great source of help to other institutions who are providing cancer care during the attack of this contagion in the presence of finite health care resources and workforce. More research is needed in this regard including other institutions from public and private sector for better understanding behavior of COVID-19 disease and achieve common goal to tackle COVID-19 and cancer together.
6. Conclusion
Timely planning, multidisciplinary management and implementation of health policies kept infectivity and fatality rate among breast cancer cases and in general population much lower than one would expect in a low middle income country with high constraints to allocate health resources properly nationwide during COVID-19 pandemic.
Ethical approval
This research was approved by the Ethical Review Committee of Aga Khan University Hospital (Reference number: 2020-5418-14043).
Sources of funding
The authors have no funding resources to be declared.
Author contribution
Study Conception: LMV.
Data Collection: LMV, DJ, NA, AA.
Analysis: DJ.
Investigation: LMV, NA, AA.
Writing: LMV, DJ.
Critical review and revision: all authors.
Final approval of the article: all authors.
Accountability for all aspects of the work: all authors.
Registration of research studies
1Name of the registry: German Clinical Trials Register (DRKS).
2Unique Identifying number or registration ID: DRKS00023807.
3Hyperlink to your specific registration (must be publicly accessible and will be checked): https://www.drks.de/drks_web/navigate.do?navigationId=trial.HTML&TRIAL_ID=DRKS00023807
Guarantor
Lubna M. Vohra Assistant Professor, Consultant Breast Surgeon, Lubna_mushtaque@hotmail.com.
Consent
Ethical Review Committee of Aga Khan University Hospital had waived documentation of informed consent due to the observational nature of the study.
Data availability
Data used in the article is available on request from the corresponding author.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The authors have no conflicts of interest to declare.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amsu.2021.01.099.
Contributor Information
Lubna M. Vohra, Email: lubna.vohra@aku.edu.
Dua Jabeen, Email: jabeen_dua@hotmail.com.
Narmeen Asif, Email: narmeen.asif@aku.edu.
Abdul Ahad, Email: abdul.ahad@aku.edu.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ma Josephine. Coronavirus: China's first confirmed Covid-19 case traced back to November 17. South China Morning Post. March 13, 2020. https://www.scmp.com/news/china/society/article/3074991/coronavirus-chinas-first-confirmed-covid-19-case-traced-back Available from:
- 3.World Health Organization WHO coronavirus disease (COVID-19) dashboard. https://covid19.who.int/ Updated January 24, 2021. Accessed January 24, 2021. Available from:
- 4.Government of Pakistan Coronavirus in Pakistan - confirmed cases. http://covid.gov.pk/ Updated January 24, 2021. Accessed January 24, 2021. Available from:
- 5.Agha R., Abdall-Razak A., Crossley E. STROCSS 2019 Guideline: strengthening the reporting of cohort studies in surgery. Int. J. Surg. 2019 Dec;72:156–165. doi: 10.1016/j.ijsu.2019.11.002. [DOI] [PubMed] [Google Scholar]
- 6.Al‐Shamsi H.O., Alhazzani W., Alhuraiji A. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID‐19) pandemic: an international collaborative group. Oncol. 2020 Jun;25(6):e936–e945. doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fregatti P., Gipponi M., Giacchino M. Breast cancer surgery during the COVID-19 pandemic: an observational clinical study of the breast surgery clinic at Ospedale Policlinico San Martino - Genoa, Italy. In Vivo. 2020 Jun;34(3 Suppl):1667–1673. doi: 10.21873/invivo.11959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dietz J.R., Moran M.S., Isakoff S.J. Recommendations for prioritization, treatment, and triage of breast cancer patients during the COVID-19 pandemic. the COVID-19 pandemic breast cancer consortium. Breast Canc. Res. Treat. 2020 Jun;181(3):487–497. doi: 10.1007/s10549-020-05644-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Azambuja E., Trapani D., Loibl S. ESMO management and treatment adapted recommendations in the COVID-19 era: breast cancer. ESMO open. 2020 May;5(Suppl 3) doi: 10.1136/esmoopen-2020-000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020 Jul;6(7):1108–1110. doi: 10.1001/jamaoncol.2020.0980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020 Mar;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vuagnat P., Frelaut M., Ramtohul T. COVID-19 in breast cancer patients: a cohort at the Institut Curie hospitals in the Paris area. Breast Cancer Res. 2020 May;22(1):55. doi: 10.1186/s13058-020-01293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. J. Am. Med. Assoc. 2020 Apr;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 14.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. J. Am. Med. Assoc. 2020 May;323(18):1775–1776. doi: 10.1001/jama.2020.4683. [DOI] [PubMed] [Google Scholar]
- 15.Gupta R., Misra A. COVID19 in South Asians/Asian Indians: heterogeneity of data and implications for pathophysiology and research. Diabetes Res. Clin. Pract. 2020 Jul;165:108267. doi: 10.1016/j.diabres.2020.108267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chinnaswamy S. SARS-CoV-2 infection in India bucks the trend: trained innate immunity? Am. J. Hum. Biol. 2020 Sep 23 doi: 10.1002/ajhb.23504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in the article is available on request from the corresponding author.