Abstract
Objectives:
The purpose of this study was to evaluate the usefulness of Hounsfield unit (HU) assessment with multislice-CT in the differentiation of radicular cysts (RCs), dentigerous cysts (DCs) and odontogenic keratocysts (OKCs).
Methods:
In total, 307 odontogenic cysts (RCs, DCs and OKCs) were included in this study. Cysts with lesion diameter <10 mm, cysts with artefacts affecting measurement of HU values, cysts involving infection and recurrent cysts were regarded as exclusion criteria. Images were acquired in three different types of CT scanners: Aquilion ONE, Discovery CT750 HD and SOMATOM Definition Flash. Differences in HU values among scanners and among types of odontogenic cysts were assessed using one-way analysis of variance; multiple comparisons were performed post hoc, using the Tukey–Kramer honestly significant difference test.
Results:
In total, 164 cysts were analysed in this study (64 RCs, 57 DCs and 43 OKCs). Regardless of the type of lesion, the Aquilion ONE scanner demonstrated a significant difference in HU value, compared with the Discovery CT750 HD scanner. Regardless of CT scanner model, HU values significantly differed between DCs and OKCs (p < 0.0001), as well as between OKCs and RCs (p < 0.0001).
Conclusions:
HU values were found to vary among CT scanners and should always be associated with other lesion imaging features while interpreting and elaboration diagnostic hypothesis. Notably, the results suggested that OKCs might be able to be differentiated from DCs and RCs by using HU values.
Keywords: Multidetector computed tomography, odontogenic cyst, odontogenic keratocyst, dentigerous cyst, radicular cyst
Introduction
Odontogenic cysts are epithelial cysts that may be developmental or inflammatory in origin.1 Developmental cysts are caused by activation of remaining odontogenic cells within alveolar bone or periodontal tissue, whereas inflammatory cysts are caused by dental inflammatory alterations.2 Odontogenic cysts comprise a diverse range of histological types; among them, the most prevalent are dentigerous cysts (DCs) and odontogenic keratocysts (OKCs) as developmental cysts, and radicular cysts (RCs) as inflammatory cysts.3,4
RCs are inflammatory cysts that arise from epithelial remnants of the periodontal ligament, due to inflammation after pulp death. In imaging examinations, RCs often appear to be radiolucent round-shaped areas with well-defined limits; they exhibit clear continuity with the apical periodontal space of teeth that contain infected or necrotic pulp.5
DCs are developmental odontogenic cysts, which comprise cystic cavities that encircle the crowns of unerupted teeth at the cementoenamel junction.6 Radiographically, DCs typically appear to be well-demarcated unilocular radiolucencies with sclerotic margins that surround tooth crowns.7
OKCs were recently reclassified as cysts8; they exhibit potentially aggressive and infiltrative behaviour with high rates of recurrence.9 Radiographically, OKCstypically appear to be unilocular or multilocular radiolucencies; similar to RCs and DCs, the OKCs exhibit well-defined borders.10
Although they exhibit similar imaging features, mainly in conventional radiographs, the aforementioned lesions require distinct treatment approaches. Further imaging examinations are needed to achieve detailed assessment of lesion characteristics (e.g., internal content, margins, three-dimensional progress limits and relationship with adjacent structures) and determine the involvement of bone tissue. CT may be taken for diagnosis of odontogenic cysts of bone lesions and subsequent treatment planning. Diagnosis of OKC especially can be informed the surgeon before surgery that careful cystectomy is necessary because of the high risk of residual cyst wall during removal. Furthermore, multislice CT allows the assessment of Hounsfield measurements of the lesions, which provides information regarding the main lesion characteristics. Image density values are measured in Hounsfield units (HUs); these are also referred to as CT numbers or Hounsfield numbers. HU assessment constitutes an effortless approach to characterize distinct tissue types on CT; it is already widely applied as a complementary diagnostic tool for various imaging studies in medicine.11 Nevertheless, the characterization of odontogenic cysts using HU has not been thoroughly investigated in dentistry, particularly in a study with a large number of cysts. If HU values can be used to identify OKCs, it will be useful information for the oral surgeons. Thus, the purpose of the present study was to evaluate the usefulness of HU assessment, acquired by means of multislice CT, in the differentiation of RCs, DCs and OKCs. However, this study does not actively recommend CT examination of odontogenic cysts.
Methods and materials
This study was approved by the Ethics Committee (Approval No. 1904–015) of our institution. This study was a retrospective study and provided ethical consideration to patients by providing a refusal opportunity.The investigation was performed in accordance with the tenets of the Declaration of Helsinki.
Inclusion and exclusion criteria
In total, 307 multislice CT imaging examinations of odontogenic cysts (RCs, DCs and OKCs), performed between January 2014 and December 2018, were included in this study. There were 174 males and 133 females, ages 6–94 years (average 47.3 years). All included cysts had undergone previous histopathological examinations and were confirmed odontogenic cysts.
The following exclusion criteria were used in this study:
Lesion diameter of <10 mm, which would impede assessment of the region of interest.
Artefacts that would influence measurement of HU values.
Cysts with a high concentration in the lesion (those with HU values > 90). Lesion concentrations were heterogeneous; however, those containing ≤90 HUs were included in the present study. An example of a cyst excluded for this reason is shown in Figure 1.
Cysts involving infection, such as those with areas of aeration in the lesion.
Recurrent cysts.
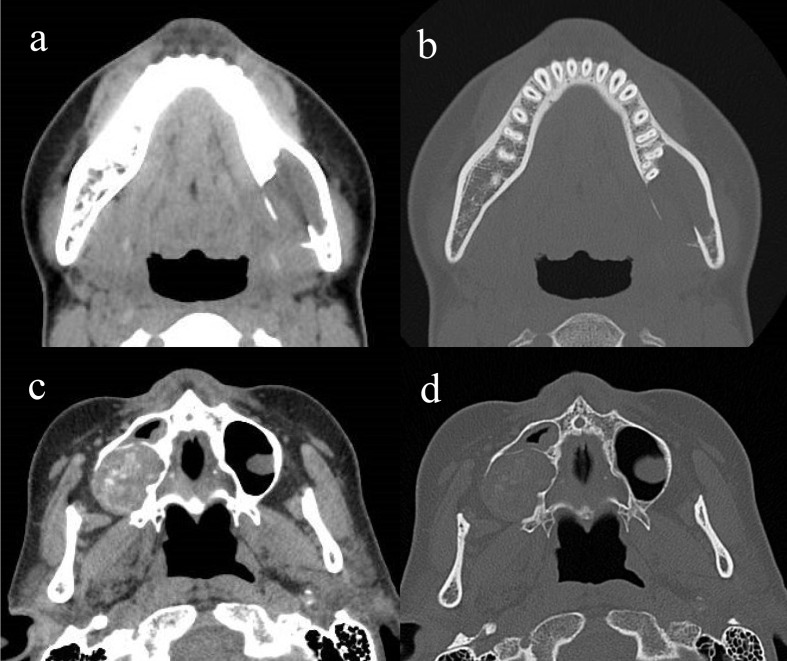
Figure 1.
Excluded cases. A case of dentigerous cyst was excluded because of bone artefact (a: soft condition, b: bone condition). When a substance with high X-ray absorption exists in a specific projection direction, an artefact occurs. This bone artefact occurs in the centre of the lesion due to lingual cortical bone behind the lesion. A case of odontogenic keratocyst was excluded because it contained high density area over 90 HU (c: soft condition, d: bone condition).
Imaging examination assessment
HU measurements from CT examinations were performed using axial slices. Imaging examinations were assessed on a high-resolution medical image monitor (EIZO Corporation, Ishikawa, Japan). The region of interest area for HU measurements was set in a freehand manner in the centre of the lesion, at a distance of approximately 1–2 mm from the lesion margin. The first round HU value measured from a plurality of slices was defined as the HU value of one observer. After the first measurement, the second round measurement was performed about 1-month later. The mean values between the first round HU value and the second round HU value were used as data for each observer. CT HU assessments were performed by two distinct observers with experience in CT examinations and HU measurement (12 years of experience, 22 years of experience). For multilocular OKCs, the septum was not included in the region of interest. When an axial slice exhibited extremely low or high HU values during multiple measurements, the two observers and other simultaneous co-authors (24 years of experience, 8 years of experience) confirmed using coronal slices if the cyst met exclusion criteria.
CT scanners
Images were acquired using three different types of CT scanner: Aquilion ONE (hereafter referred to as “scanner A”; Canon Medical Systems Corporation, Tochigi, Japan); Discovery CT750 HD (hereafter referred to as “scanner D”; GE Healthcare, Milwaukee, WI, USA); and SOMATOM Definition Flash (hereafter referred to as “scanner S”; Siemens, Nurnberg, Germany). CT scans were obtained with the following parameters: field of view: 12.9×12.9 to 32×32 cm; tube voltage: 120–140 kV; tube current: 150–500 mA.
Statistical analysis
Normality was confirmed using the Shapiro–Wilk test. Intra- and inter-observer reliabilities were determined using intraclass correlation coefficients. Differences in HU values among scanners and among types of odontogenic cysts were assessed using one-way analysis of variance; multiple comparisons were performed post hoc, using the Tukey–Kramer honestly significant difference test. All statistical analyses were performed using JMP®, v.14 (SAS Institute Inc., Cary, NC, USA).
Results
Of the 307 cysts initially screened, only 164 (64 RCs, 57 DCs, and 43 OKCs) were included in the final analysis after application of inclusion and exclusion criteria (Table 1). There were 94 males and 70 females, aged 6–94 years (average 46.3 years). 59 DCs, 31 OKCs and 53 RCs were excluded using the exclusion criteria. The breakdown is (a) lesion diameter of <10 mm, (b) artefacts, (c) cysts with a high concentration, (d) cysts involving infection and (e) recurrent cysts; in this order in DC, (a) 20 cases, (b) 44 cases, (c) 0 case, (d) 11 cases and (e) 0 case; in OKC, (a) 4 cases, (b) 10 cases, (c) 6 cases, (d) 9 cases and (e) 3 cases; in RC, (a) 27 cases, (b) 14 cases, (c) 0 case, (d) 15 cases and (e) 0 case. There are overlaps in each disease. Notably, among the 43 OKCs included, 30 were unilocular and 13 were multilocular. The mean HU values (±standard deviations) of each type of cyst, assessed by the three different scanners, are shown in Table 2. Tests of intra- and inter-observer reliability confirmed that there were no differences between the two observers in terms of HU measurements (intraobserver reliability: r = 0.98 for observer one and r = 0.9694 for observer 2; interobserver reliability: r = 0.9744).
Table 1.
Number of cases
| scanner A | scanner D | scanner S | Total | |
|---|---|---|---|---|
| dentigerous cyst (DC) | 23 | 15 | 19 | 57 |
| odontogenic keratocyst (OKC) | 24 | 7 | 12 | 43 |
| radicular cyst (RC) | 23 | 22 | 19 | 64 |
| 70 | 44 | 50 | 164 |
Table 2.
Mean ± SD
| scanner A | scanner D | scanner S | Total | |
|---|---|---|---|---|
| dentigerous cyst (DC) | 48.0 ± 11.9 | 60.8 ± 11.2 | 52.2 ± 13.4 | 52.8 ± 12.2 |
| odontogenic keratocyst (OKC) | 39.2 ± 12.6 | 25.5 ± 11.7 | 42.5 ± 13.9 | 37.9 ± 12.8 |
| radicular cyst (RC) | 43.4 ± 11.2 | 57.4 ± 10.3 | 53.2 ± 14.2 | 51.1 ± 11.8 |
| 43.4 ± 11.9 | 53.5 ± 10.8 | 50.2 ± 13.8 | 48.2 ± 12.2 |
Comparison of HU values among CT scanners
During assessment of DCs, significant differences in HU values between scanners A and D were observed (one-way analysis of variance, F (2, 56)=5.5496;Tukey–Kramer honestly significant difference test, p = 0.0044). No statistically significant differences in HU values were observed between scanners A and S (p = 0.4016) or between scanners D and S (p = 0.1141) (Figure 2a).
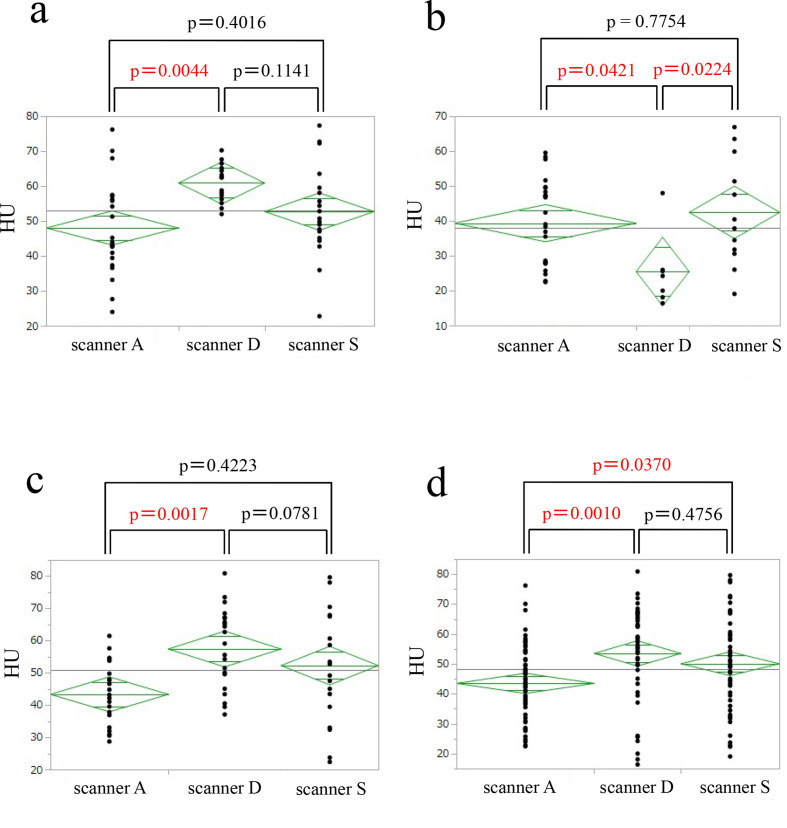
Figure 2.
HU of lesions according to CT scanner using one-way ANOVA text with Tukey-Kramer's HSD post-hoc test. (a) dentigerous cyst, (b) odontogenic keratocyst, (c) radicular cyst, (d) all odontogenic cysts.
During assessment of OKCs, significant differences in HU values were observed between scanners A and D (p = 0.0421), as well as between scanners D and S (p = 0.0224). No statistically significant differences in HU values were observed between scanners A and S (p = 0.7754) (Figure 2b).
During assessment of RCs, significant differences in HU values were observed between scanners A and D (p = 0.0017), as well as between scanners D and S (p = 0.0781). No statistically significant differences in HU values were observed between scanners A and S (p = 0.4223) (Figure 2c).
When all types of lesions were assessed concurrently, scanner A exhibited HU values that significantly differed from those of scanner D (p = 0.0010) and S (p = 0.0370). No statistically significant differences in HU values were observed between scanners D and S (p = 0.4756) (Figure 2d).
Comparison of HU values among odontogenic cysts
When scanner A was used, significant differences in HU values were observed between DCs and RCs (p = 0.0340). No statistically significant differences in HU values were observed between DCs and RCs (p = 0.3660) or between OKCs and RCs (p = 0.4704) (Figure 3a).
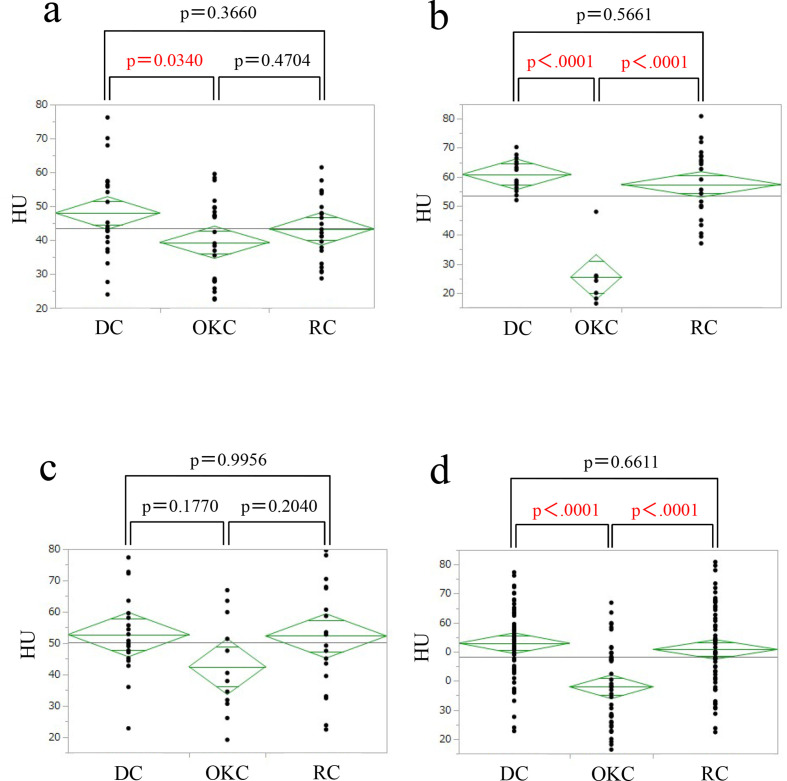
Figure 3.
HU of lesions according to odontogenic cysts using one-way ANOVA text with Tukey-Kramer's HSD post-hoc test. (a) scanner A, (b) scanner D, (c) scanner S, (d) all scanners.
When scanner D was used, significant differences in HU values were observed between DCs and OKCs (p < 0.0001), as well as between OKCs and DCs (p < 0.0001). No statistically significant differences in HU values were observed between DCs and RCs (p = 0.5661) (Figure 3b).
When scanner S was used, no statistically significant differences in HU values were observed among the lesions (Figure 3c).
When all types of CT scanners were concurrently included in the analysis, significant differences in HU values were observed between DCs and OKCs (p < 0.0001), as well as between OKCs and RCs (p < 0.0001). No statistically significant differences in HU values were observed between DCs and RCs (p = 0.6611) (Figure 3d).
Discussion
In the present study, three types of odontogenic cysts (RCs, DCs and OKCs) were assessed using three distinct CT scanners (Figure 4). In summary, HU values of DCs and OKCs were more often useful for differentiating between these two lesions. Additionally, HU values often differed among CT scanners, which indicates that HU values in general may vary among models of CT scanners.
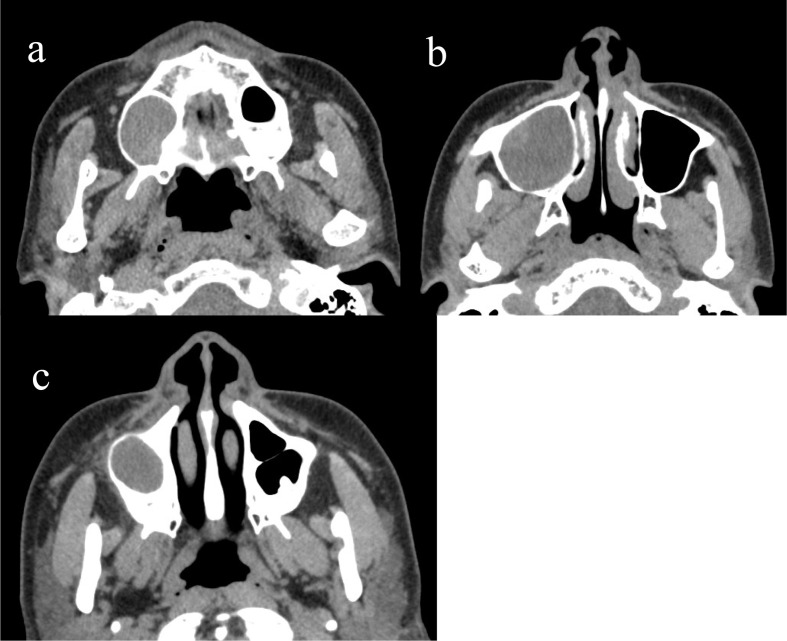
Figure 4.
CT images of representative cases used for HU measurements. DC showed 46.8 HU (a), OKC showed 25.2 HU (b) and RC showed 32.04 HU (c).
Each CT scanner was from a separate manufacturer: scanner A was from Canon Medical Systems Corporation, scanner D was from GE Healthcare, and scanner S was from Siemens. When HU values were compared among scanners, scanners A and D were found to exhibit significant differences in HU values, regardless of lesion type. Scanner S tended to consistently exhibit higher HU values, compared with scanner A. Compared with the other scanners, scanner D exhibited higher HU values for DCs and RCs, whereas it exhibited lower HU values for OKCs. Therefore, the usefulness of scanner D appeared to differ according to lesion type, and no consistent trend was observed.
All CT scanners had been calibrated and verified before imaging examinations (to prevent failures during imaging acquisitions); this included analysis of a phantom to check whether HU values were appropriate. Furthermore, cysts with heterogeneous density were excluded. Nonetheless, differences were observed in HU values among the scanners. These differences in HU values among scanners were expected due to the high variability in HU measurements when image acquisition was previously compared among distinct equipment models.12,13
Moreover, HU accuracy may be influenced by a number of factors inherent to imaging acquisition and processing itself (e.g., convolution kernel, spectral energy, beam hardening, scatter and reconstruction artefacts)11 and by factors associated with each patient (e.g., patient size or position in the scanner).14,15 To the best of our knowledge, no comparisons of HU values among CT scanners have been previously performed with respect to odontogenic lesions. Further studies are needed for comparison with the present findings. Although HU characterization of lesions is a valuable and effective mechanism in the diagnostic hypothesis elaboration, professionals must be aware of the variations between scanners in clinical practice, with carefulness while interpreting absolute HU values and always considering other imaging and clinical features.
The major reasons for exclusion were 68 cases (41.7%) due to artefacts and 51 cases (31.3%) with a size of 10 mm or less. Therefore, in order to obtain the HU value as additional information, it is necessary to judge whether the case is worth CT scanning. In particular, it is necessary to confirm whether the case will not occur artefacts and the case is the small size of the lesion. In cases where there is a high risk of artefacts from the occlusal plane, such as DCs occurring in the third molar of the mandible, it may be necessary to take measures such as imaging with the lower edge of the mandible as the reference plane. CBCT is recommended because it is difficult to determine the internal properties from CT images when the lesion size is small.
Regarding the mean HU value obtained for DCs (52.8 ± 12.2 HUs), previous reports have shown wide variation (i.e., 3.9–22.9 HUs), suggesting internal serous fluid.16,17 Regarding the mean HU value obtained for OKCs (37.9 ± 12.8 HUs), published reports include similar values (i.e., 28.4–40 HUs).18,19 The significant difference in HU values between DCs and OKCs is presumably associated with dissimilarities in internal content between these two cysts. DCs often originate as a result of fluid accumulation between reduced enamel epithelium and the tooth crown, between reduced enamel epithelium layers,20 or (gradually) from inflammatory processes.21 Cholesterol clefts and degenerated cellular components are frequently observed in the lumen of DCs. Konouchi et al reported that most DCs exhibited high signal intensity on T1W images22; this phenomenon was attributed to the presence of high-density protein solution within the lumen. Cystic cavities of OKCs typically contain desquamated keratin, which increases the viscosity of cystic fluid within OKCs.20 In this study, HU values of OKCs were significantly lower than those of DCs and RCs. This may be partly attributed to the exclusion of cysts with HU values >90. Although OKCs were presumed to have high HU values because of their keratin content, there were few OKCs with low HU values in this study.
Notably, RCs originate in response to tissue necrosis from dental pulp origin.21 Cystic cavities of RCs are filled with cell debris containing proteins and intracellular particles, which increases the viscosity of cystic fluid within RCs.20 DCs with inflammatory changes can appear similar to RCs.23 These similarities between DCs and RCs may explain the lack of a significant difference in HU values between these two cysts, as well as the significant difference in HU values observed between RCs and OKCs. Fortunately, imaging differentiation between RCs and DCs, or between RCs and OKCs, may be possible because RCs are associated with necrotic teeth roots; hence, this lesion might be distinguishable from other pathological odontogenic cysts based on its location and other related clinical signs. However, if an RC exhibits a large diameter because of an extended absence of treatment, or if an RC is involved with more than one or two teeth, diagnosis may be difficult and HU value may suggest, at least, that the lesion assessed is not an OKC, which is a much more aggressive lesion.
Overall, differentiation of OKCs and DCs remains challenging because of similar imaging features between these lesions, despite their distinct progression and treatment. Thus, HU assessment will provide useful information. However, the problem with obtaining HU values is that nearly half of them could not be evaluated because of artefacts and/or small size of lesions. Although there is the limitation, the HU values may be able to provide a supplementary useful additional information in some cases with difficult diagnoses.
Conclusion
HU values were found to vary among CT scanners and should always be associated with other lesion imaging features while interpreting and elaboration diagnostic hypothesis. Notably, the results suggest that OKCs may be able to be differentiated from DCs and RCs by using HU values. However, this study does not actively recommend CT examination of odontogenic cysts.
Footnotes
Acknowledgment: We thank Ryan Chastain-Gross, Ph.D., from Edanz Group (https://en-author-services.edanzgroup.com) for editing a draft of this manuscript.
Contributor Information
Kyonori Uehara, Email: uehara@amh.ako.hyogo.jp.
Miki Hisatomi, Email: tomi@md.okayama-u.ac.jp.
Luciana Munhoz, Email: dra.lucimunhoz@usp.br.
Toshiyuki Kawazu, Email: kawazu@okayama-u.ac.jp.
Shunsuke Okada, Email: okd@okayama-u.ac.jp.
Yohei Takeshita, Email: takeshita@okayama-u.ac.jp.
Emiko Arita Saito, Email: emiko.sp@terra.com.br.
Junichi Asaumi, Email: asaumi@md.okayama-u.ac.jp.
REFERENCES
- 1.Soluk-Tekkeşin M, Wright JM. The world Health organization classification of odontogenic lesions: a summary of the changes of the 2017 (4th) edition. Turk Patoloji Derg 2018; 34: 34. doi: 10.5146/tjpath.2017.01410 [DOI] [PubMed] [Google Scholar]
- 2.Bhat A, Mitra S, Chandrashekar C, Solomon M, Kulkarni S. Odontogenic cysts and odontogenic tumors in a large rural area from India. A 10-year reflection. Med Pharm Rep 2019; 92: 408–12. doi: 10.15386/mpr-1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prockt AP, Schebela CR, Maito FDM, Sant'Ana-Filho M, Rados PV. Odontogenic cysts: analysis of 680 cases in Brazil. Head Neck Pathol 2008; 2: 150–6. doi: 10.1007/s12105-008-0060-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramos GdeO, Porto JC, Vieira DSC, Siqueira FM, Rivero ERC. Odontogenic tumors: a 14-year retrospective study in SANTA Catarina, Brazil. Braz Oral Res 2014; 28: 33–8. doi: 10.1590/s1806-83242013005000030 [DOI] [PubMed] [Google Scholar]
- 5.Nair PN. New perspectives on radicular cysts: do they heal? Int Endod J 1998; 31: 155–60. doi: 10.1046/j.1365-2591.1998.00146.x [DOI] [PubMed] [Google Scholar]
- 6.Yahara Y, Kubota Y, Yamashiro T, Shirasuna K. Eruption prediction of mandibular premolars associated with dentigerous cysts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 28–31. doi: 10.1016/j.tripleo.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 7. De Andrade Freitas Oliveira LS, Souza do, Neves FS, DOS Santos JN, Campos PS, Crusoé-Rebello I. uncommon dentigerous cyst related to a maxillary lateral incisor in a 03-year-old boy. Oral Maxillofac Surg 2012; 16: 383–8. [DOI] [PubMed] [Google Scholar]
- 8.Wright JM, Vered M. Update from the 4th edition of the world Health organization classification of head and neck tumours: odontogenic and maxillofacial bone tumors. Head Neck Pathol 2017; 11: 68–77. doi: 10.1007/s12105-017-0794-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chrcanovic BR, Gomez RS. Recurrence probability for keratocystic odontogenic tumors: an analysis of 6427 cases. J Craniomaxillofac Surg 2017; 45: 244–51. doi: 10.1016/j.jcms.2016.11.010 [DOI] [PubMed] [Google Scholar]
- 10.Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Di Bartolomeo F, et al. Odontogenic keratocyst: imaging features of a benign lesion with an aggressive behaviour. Insights Imaging 2018; 9: 883–97. doi: 10.1007/s13244-018-0644-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lamba R, McGahan JP, Corwin MT, Li C-S, Tran T, Seibert JA, et al. Ct Hounsfield numbers of soft tissues on unenhanced abdominal CT scans: variability between two different manufacturers' MDCT scanners. AJR Am J Roentgenol 2014; 203: 1013–20. doi: 10.2214/AJR.12.10037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oh JH, Choi SP, Wee JH, Park JH. Inter-scanner variability in Hounsfield unit measured by CT of the brain and effect on gray-to-white matter ratio. Am J Emerg Med 2019; 37: 680–4. doi: 10.1016/j.ajem.2018.07.016 [DOI] [PubMed] [Google Scholar]
- 13.Birnbaum BA, Hindman N, Lee J, Babb JS. Multi-detector row CT attenuation measurements: assessment of intra- and interscanner variability with an anthropomorphic body CT phantom. Radiology 2007; 242: 109–19. doi: 10.1148/radiol.2421052066 [DOI] [PubMed] [Google Scholar]
- 14.Levi C, Gray JE, McCullough EC, Hattery RR. The unreliability of CT numbers as absolute values. AJR Am J Roentgenol 1982; 139: 443–7. doi: 10.2214/ajr.139.3.443 [DOI] [PubMed] [Google Scholar]
- 15.Hunter TB, Pond GD, Medina O. Dependence of substance CT number on scanning technique and position within scanner. Comput Radiol 1983; 7: 199–203. doi: 10.1016/0730-4862(83)90099-9 [DOI] [PubMed] [Google Scholar]
- 16.Martinelli-Kläy CP, Martinelli CR, Martinelli C, Macedo HR, Lombardi T. Unusual imaging features of dentigerous cyst: a case report. Dent J 2019; 776. doi: 10.3390/dj7030076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cankurtaran cz1, Branstetter bf 4th, Chiosea Si, Barnes El Jr. best cases from the AFIP: ameloblastoma and dentigerous cyst associated with impacted mandibular third molar tooth. Radiographics 2010; 30: 1415–20. [DOI] [PubMed] [Google Scholar]
- 18.Crusoé-Rebello I, Oliveira C, Campos PSF, Azevedo RA, dos Santos JN. Assessment of computerized tomography density patterns of ameloblastomas and keratocystic odontogenic tumors. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: 604–8. doi: 10.1016/j.tripleo.2009.03.008 [DOI] [PubMed] [Google Scholar]
- 19.Sánchez-Burgos R, González-Martín-Moro J, Pérez-Fernández E, Burgueño-García M, Clinical B-GM. Clinical, radiological and therapeutic features of keratocystic odontogenic tumours: a study over a decade. J Clin Exp Dent 2014; 6: e259–64. doi: 10.4317/jced.51408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eida S, Hotokezaka Y, Katayama I, Ichikawa Y, Tashiro S, Sumi T, et al. Apparent diffusion coefficient-based differentiation of cystic lesions of the mandible. Oral Radiol 2012; 28: 109–14. doi: 10.1007/s11282-012-0095-z [DOI] [Google Scholar]
- 21.Narang RS, Manchanda AS, Arora P, Randhawa K. Dentigerous cyst of inflammatory origin-a diagnostic dilemma. Ann Diagn Pathol 2012; 16: 119–23. doi: 10.1016/j.anndiagpath.2011.07.004 [DOI] [PubMed] [Google Scholar]
- 22.Konouchi H, Yanagi Y, Hisatomi M, Matsuzaki H, Takenobu T, Unetsubo T, et al. Mr imaging diagnostic protocol for unilocular lesions of the jaw. Japanese Dental Science Review 2012; 48: 81–91. doi: 10.1016/j.jdsr.2012.01.001 [DOI] [Google Scholar]
- 23.Robinson RA. Diagnosing the most common odontogenic cystic and osseous lesions of the jaws for the practicing pathologist. Mod Pathol 2017; 30(s1): S96–103. doi: 10.1038/modpathol.2016.191 [DOI] [PubMed] [Google Scholar]