Abstract
Objective:
To investigate the differences in imaging characteristics and the diagnostic accuracy of 225 intraosseous jaw lesions on panoramic radiographs (PAN) versus cone beam computed tomography (CBCT).
Methods:
225 sets of PAN and CBCT images with biopsy-proven histopathological diagnoses were retrospectively compared in terms of radiographic features and diagnostic accuracy. The imaging characteristics of PAN and CBCT were independently evaluated by two oral and maxillofacial radiologists who were required to answer 12 questions and provided up to three differential diagnoses with their confidence scores.
Results:
Odds ratios (ORs) were statistically significant for border cortication (OR = 1.521; p = .003) and border continuity (OR = 0.421; p = .001), involvement on neurovascular canals (OR = 2.424; p < .001), expansion (OR = 7.948; p < .001), cortical thinning (OR = 20.480; p < .001) as well as its destruction (OR = 25.022; p < .001) and root resorption (OR = 2.477; p < .001). Furthermore, imaging features in the posterior and mandibular regions showed better agreement than those in the anterior and maxillary regions, respectively. The diagnostic accuracy of the first differential diagnosis was higher on CBCT than on PAN (Observer 1:78.7 vs 64.4%; Observer 2: 78.7 vs 70.2% (p < .001)). The observers’ confidence scores were also higher at CBCT interpretation compared with PAN.
Conclusions:
CBCT demonstrated a greater number of imaging characteristics of intraosseous jaw lesions compared with PAN, especially in the anterior regions of both jaws and in the maxilla. Diagnostic accuracy is improved with CBCT compared to PAN, especially for lesions in the maxilla. Radiologists have greater confidence when using CBCT.
Keywords: Radiographic characteristics, Diagnostic accuracy, Intra-osseous jaw lesion, Panoramic radiography, Cone beam computed tomography
Introduction
Panoramic radiography (PAN) and cone beam computed tomography (CBCT) are two radiographical modalities used in the diagnosis and treatment planning and management of oral and maxillofacial diseases. Not only do they show the imaging features of lesions, but they also guide the clinicians to make the most appropriate diagnoses as well as the subsequent treatment plans, and to monitor healing and/or the disease recurrence during follow up.
PAN, as the most common imaging technique, can provide an overview of the jaws and dentition, but anatomic structures and lesions in the anterior jaws are not well-defined due to the superimposition of cervical vertebrae. In addition, the image quality of PAN may be influenced by superimposition of surrounding anatomic structures, air shadows, ghost images, and sensitivity to patient positioning errors. Such errors will also result in imaging distortion and unequal magnification in the horizontal and vertical dimension.1 CBCT, which has been widely introduced in maxillofacial imaging since late 1990s, has advantages over the two-dimensional PAN, due to its three-dimensional nature.2,3 CBCT not only displays anatomic structures and lesions in the axial, coronal and sagittal planes, but also allows for a variety of post-processing effects to be performed. These include multiple planar reconstruction, minimum/maximum intensity projection, and volume rendering, which can accurately demonstrate the location, size, shape and relationship to the surrounding tissues of the lesions, and can facilitate the diagnostic process.
Nevertheless, CBCT also has its disadvantages. For example, CBCT is prone to various artefacts, especially metal and motion artefacts, which can have a deleterious effect on the image quality.1,4,5 Compared with spiral CT, its contrast resolution is lower and soft tissues are poorly demonstrated.5 The radiation dose and cost are also important factors that should be considered when making clinical decisions. The dose is mainly dependent on equipment type and exposure settings, including the field of view, exposure time(s), tube current (mA) and the energy/potential (kV).6 Compared with PAN, the effective radiation dose of CBCT is usually significantly higher and this should be taken into consideration when imaging is required.7
It is well known that CBCT has many advantages in the diagnosis of oral and maxillofacial diseases.8–11 Compared with PAN, CBCT can provide more information to aid clinicians in making diagnoses, designing treatment plans, and monitoring follow-ups postoperatively. Currently, there is a paucity of studies focusing on the differences of radiographical characteristics between PAN and CBCT for imaging the intraosseous jaw lesions in a quantitative method. The most recent study, with 31 cases included, showed that although there were differences in the radiographical appearances of intraosseous lesions on PAN and CBCT, CBCT did not aid in improving diagnostic accuracy.12 The authors concluded that the low number of cases in their study was a limitation.12 Therefore, the objectives of this study, using a greater number of lesions were: (1) to investigate the differences in imaging characteristics of intraosseous jaw lesions between PAN and CBCT; and (2) to further determine the diagnostic efficacy of the two radiographical modalities when evaluating intraosseous jaw lesions.
Methods and materials
The methodology described below was adapted from the above-mentioned study by Lim et al.12
Case selection
This retrospective study was approved by the Biomedical Institutional Review Board of Peking University School and Hospital of Stomatology (PKUSSIRB-201946079). Imaging data were obtained from Picture Archiving and Communication System (PACS) in the Department of the Oral and Maxillofacial Radiology, Peking University School and Hospital of Stomatology from March 2014 to December 2018. 225 cases containing both PAN and CBCT data were included. Inclusion criteria: 1) Patients with intraosseous lesions of the maxilla and/or mandible, including recurrent and multiple lesions; 2) PAN and CBCT examinations with a time interval of no more than 3 months; and 3) with definitive histopathological diagnoses. Exclusion criteria: 1) Soft tissue lesions in the oral and maxillofacial region; 2) incomplete imaging data (i.e., either PAN or CBCT images were not available); 3) histopathological diagnoses were not definitive; 4) image quality of PAN or CBCT were not satisfactory, for example, poor imaging quality due to artefacts, or the region of interest not fully included; and 5) surgical treatment was performed during the interval between the examination of PAN and CBCT.
Preparation and interpretation of PAN and CBCT images
No clinical information was included when the images were retrieved. All the images were viewed in PACS. Two oral and maxillofacial radiologists, both with 5 years of experience, interpreted the PAN images and CBCT images separately. The PAN images were sorted chronologically by acquisition date, while the CBCT images were sorted alphabetically by name. The observers were allowed to adjust the contrast and magnification of the PAN images. For CBCTs, 3D images could be manipulated or reconstructed freely. There was no time limit imposed. After reviewing every image, the observers were asked to complete 13 questions (Supplementary Material 1), including imaging features (Questions 1 to 12) and differential diagnoses (Question 13).12 In the 13th question, the observers provided up to three ranked differential diagnoses and gave a score of 1–5 based on their confidence for each diagnosis (one represented very uncertain, and five represented very certain). When the first differential diagnosis was consistent with the histopathological diagnosis, three points were assigned. Accordingly, 2 and 1 points were assigned when the second or third differential diagnosis was consistent, respectively. If none of the differential diagnoses was correct, then 0 points were assigned.
After a “wash-out” period of at least 1 month, 20 sets of PAN and CBCT images were randomly selected to examine intraobserver reliability.
Statistical analysis
Simple κ statistics were used to compare the concordance between PAN and CBCT images and the intra- and interobserver reliability.13 Conditional logistic regression was computed to assess whether there were differences in the odds of a “Yes” response between PAN and CBCT except for Question 1 (lesion shape) and Question 5 (internal contents). The paired chi-square test was used to assess the associations about lesion shape and internal contents between the two examinations and to compare the diagnostic accuracy of PAN and CBCT.
Simple κ statistics were also used to compare the agreement in different regions of jaws.13 Comparisons were made between the maxilla and mandible, and between the anterior and posterior regions of both jaws. The anterior region was defined as extending from the midline to the distal surface of the canine both in maxilla and mandible. The posterior region was defined as extending from the mesial surface of the first premolar to the distal aspect of maxillary tuberosity in maxilla, and mesial aspect of the first premolar to the mandibular angle, ramus and condyle in mandible.
Results
Summary of the jaw lesions by category
225 cases with paired PANs and CBCTs were included. These intraosseous jaw lesions included cysts, benign tumours, malignant tumours, inflammatory lesions, fibro-osseous lesions, bone and cartilage lesions (Table 1). The most common intraosseous lesions were cysts, accounting for 54.22%. 66.67% of the lesions were located in the mandible (Table 2).
Table 1.
Summary of lesions by category
| Category | Diagnosis | N= (%) |
|---|---|---|
| Cysts(n = 122) | Dentigerous cyst Radicular cyst or residual cyst Odontogenic keratocyst(OKC) Nasopalatine duct cyst Lateral periodontal cyst Odontogenic calcifying cyst |
43 (19.11%) 34 (15.11%) 31 (13.78%) 12 (5.33%) 1 (0.44%) 1 (0.44%) |
| Benign tumours (n = 42) | Odontoma Ameloblastoma Cementoblastoma Adenomatoid odontogenic tumour Odontogenic myxoma Osteoblastoma |
21 (9.33%) 16 (7.11%) 2 (0.89%) 1 (0.44%) 1 (0.44%) 1 (0.44%) |
| Malignant tumours(n = 4) | Primary intraosseous squamous cell carcinoma of the jaws Osteosarcoma |
3 (1.33%) 1 (0.44%) |
| Inflammatory lesions(n = 31) | Osteomyelitis Periapical granuloma |
27 (12.00%) 4 (1.78%) |
| Fibro-osseous lesions(n = 11) | Osseous dysplasias Ossifying fibroma Fibrous dysplasia |
6 (2.67%) 4 (1.78%) 1 (0.44%) |
| Bone and osteochondromatous lesions(n = 13) | Osteoma Osteochondroma |
8 (3.56%) 5 (2.22%) |
| Others(n = 2) | Simple bone cyst | 2 (0.89%) |
| Total | 225 (100%) |
Table 2.
Distribution of the lesions in different regions of the jaws
| Locations | Anterior | Posterior | Both anterior and posterior | Total |
|---|---|---|---|---|
| Maxilla | 46 (20.44%) | 21 (9.33%) | 8 (3.56%) | 75 (33.33%) |
| Mandible | 18 (8.00%) | 122 (54.22%) | 10 (4.44%) | 150 (66.67%) |
| Total | 64 (28.44%) | 143 (63.56%) | 18 (8.00%) | 225 (100%) |
Intra- and interobserver reliability
Intraobserver reliability for Questions 1–12 was almost perfect with most of the κ values over 0.8 (ranging from 0.725 to 1.000). The agreements between Observer one and Observer two for each question in Questions 1–12 on PAN and CBCT were acceptable with the κ values over 0.7 (range from 0.700 to 0.876).
The agreement between PAN and CBCT
The overall agreement between PAN and CBCT in regards to lesion characteristics was shown in Table 3. Strong agreements between PAN and CBCT were seen in Q1 (Lesion shape, κ = 0.611), Q2 (Border definition, κ = 0.714), Q3 (Border cortication, κ = 0.627), Q5 (Internal contents, κ = 0.644) and Q11 (Tooth displacement, κ = 0.710).
Table 3.
Overall agreement between PAN and CBCT with respect to lesion features
| Qn # |
Questions | Overall κ value | Strength of agreementa |
|---|---|---|---|
| 1 | What is the lesion’s shape? | 0.611 | Substantial |
| 2 | Are its borders well-defined? | 0.714 | Substantial |
| 3 | Are its borders well-corticated in terms of thickness? | 0.627 | Substantial |
| 4 | Are its borders continuously corticated? | 0.165 | Slight |
| 5 | The lesion’s internal contents are mostly radiolucent/≤Soft tissue density, Mixed or Radiopaque/≥Bone density | 0.644 | Substantial |
| 6 | Is the lesion multilocular? | 0.429 | Moderate |
| 7 | Does it appear to be affecting the incisive canal or the inferior alveolar canal? | 0.523 | Moderate |
| 8 | Does it appear to expand the normal surrounding anatomic boundaries? | 0.200 | Slight |
| 9 | Does it appear to be causing cortical thinning? | 0.074 | Slight |
| 10 | Does it appear to be causing cortical destruction? | 0.061 | Slight |
| 11 | Does it appear to be causing tooth displacement? | 0.710 | Substantial |
| 12 | Dose it appear to be causing root resorption? | 0.400 | Fair |
Strength of agreement is interpreted as follows: 0.01–0.20: Slight, 0.21–0.40: Fair, 0.41–0.60: Moderate, 0.61–0.80: Substantial, 0.81–1.00: Almost perfect.13
When the overall agreement was analysed by lesion location, the κ values of the imaging features in the mandible were higher than those in the maxilla. Similarly, the κ values of the imaging features in the posterior regions were higher than those in the anterior regions of both jaws, except for Q4 (continuity of border cortication) and Q5 (internal contents) (Table 4).
Table 4.
Overall agreement between PAN and CBCT with respect to lesion features in different regions of jaws
| Qn# | Questions | Anteriora | Posteriora | Maxillaa | Mandiblea |
|---|---|---|---|---|---|
| 1 | What is the lesion’s shape? | 0.581 | 0.621 | 0.480 | 0.659 |
| 2 | Are its borders well-defined? | 0.495 | 0.740 | 0.491 | 0.791 |
| 3 | Are its borders well-corticated in terms of thickness? | 0.262 | 0.760 | 0.441 | 0.703 |
| 4 | Are its borders continuously corticated? | 0.300 | 0.113 | 0.177 | 0.157 |
| 5 | The lesion’s internal contents are mostly radiolucent/≤Soft tissue density, Mixed or Radiopaque/≥Bone density | 0.710 | 0.637 | 0.654 | 0.631 |
| 6 | Is the lesion multilocular? | 0.062 | 0.453 | 0.268 | 0.481 |
| 7 | Does it appear to be affecting the incisive canal or the inferior alveolar canal? | 0.359 | 0.596 | 0.377 | 0.571 |
| 8 | Does it appear to expand the normal surrounding anatomic boundaries? | 0.022 | 0.317 | 0.108 | 0.237 |
| 9 | Does it appear to be causing cortical thinning? | 0.012 | 0.119 | 0.043 | 0.086 |
| 10 | Does it appear to be causing cortical destruction? | 0.031 | 0.084 | 0.008 | 0.083 |
| 11 | Does it appear to be causing tooth displacement? | 0.649 | 0.740 | 0.648 | 0.740 |
| 12 | Dose it appear to be causing root resorption? | 0.379 | 0.398 | 0.325 | 0.449 |
Strength of agreement is interpreted as follows: 0.01–0.20: Slight, 0.21–0.40: Fair, 0.41–0.60: Moderate, 0.61–0.80: Substantial, 0.81–1.00: Almost perfect.13
Table 5 displayed the OR of a “Yes” response on CBCT compared to a “Yes” response on PAN for all lesion features except for Q1 (lesion shape) and Q5 (internal contents). The ORs were statistically significant for Q3 (border cortication, OR = 1.521, p = 0.003), Q4 (continuity of border cortication, OR = 0.421, p = 0.001), Q7 (effect on the incisive canal or the inferior alveolar canal (IAC), OR = 2.424, p < 0.001), Q8 (expansion of surrounding anatomic boundaries, OR = 7.948, p < 0.001), Q9 (cortical thinning, OR = 20.480, p < 0.001), Q10 (cortical destruction, OR = 25.022, p < 0.001) and Q12 (root resorption, OR = 2.477, p < 0.001). There were also statistically significant differences in lesion shape and internal contents between the two examinations (p < 0.001).
Table 5.
Odds ratio of a “Yes” response on CBCT compared to a “Yes” response on PAN
| Qn # |
Questions | Odds ratio | 95% CI | p -value* |
|---|---|---|---|---|
| 2 | Are its borders well-defined? | 1.274 | 0.914,1.774 | 0.152 |
| 3 | Are its borders well-corticated in terms of thickness? | 1.521 | 1.151,2.009 | 0.003 |
| 4 | Are its borders continuously corticated? | 0.421 | 0.250,0.708 | 0.001 |
| 6 | Is the lesion multilocular? | 1.268 | 0.729,2.205 | 0.400 |
| 7 | Does it appear to be affecting the incisive canal or the inferior alveolar canal? | 2.424 | 1.855,3.169 | <0.001 |
| 8 | Does it appear to expand the normal surrounding anatomic boundaries? | 7.948 | 5.902,10.703 | <0.001 |
| 9 | Does it appear to be causing cortical thinning? | 20.480 | 14.583,28.760 | <0.001 |
| 10 | Does it appear to be causing cortical destruction? | 25.022 | 16.691,37.510 | <0.001 |
| 11 | Does it appear to be causing tooth displacement? | 1.287 | 0.979,1.693 | 0.070 |
| 12 | Dose it appear to be causing root resorption? | 2.477 | 1.774,3.458 | <0.001 |
*p < 0.05 indicated statistical significance.
The overall accuracy of differential diagnosis on PAN and CBCT
The overall accuracy of observers’ differential diagnosis on CBCT was significantly higher than on PAN (p < 0.001). The accuracy of the first diagnosis on CBCT (Observer 1: 78.7%, Observer 2: 78.7%) was significantly higher than on PAN (Observer 1: 64.4%, Observer 2: 70.2%) (p < 0.001) (Table 6). The results showed that both observers had higher confidence scores on CBCT compared to PAN (Observer 1: 4.15 vs 3.81; Observer 2: 4.64 vs 4.33, respectively) when the correct diagnosis was made regardless of the rank at which it was listed.
Table 6.
The percentage of correct diagnosis on PAN and CBCT
| Observer 1 | Observer 2 | |||
| Correct Diagnosis | CBCT/PAN(n) | CBCT/PAN(%) | CBCT/PAN(n) | CBCT/PAN(%) |
| First | 177/145 | 78.7%/64.4% | 177/158 | 78.7%/70.2% |
| Second | 31/41 | 13.8%/18.2% | 21/24 | 9.3%/10.7% |
| Third | 6/10 | 2.7%/4.4% | 0/3 | 0.0%/1.3% |
| Total | 214/196 | 95.1%/87.1% | 198/182 | 88.0%/80.9% |
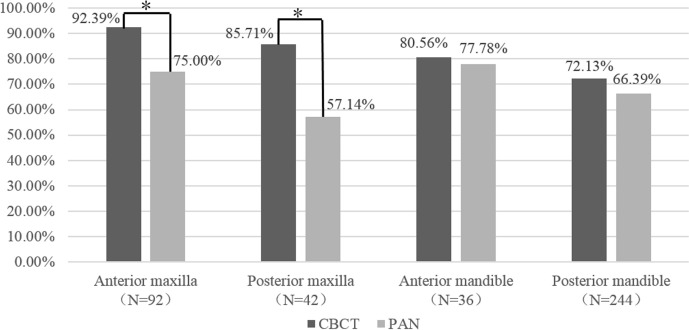
These results were further analysed based on lesion location. The frequency of correct diagnoses made on the first attempt on CBCT were higher than on PAN across all locations (Figure 1). The accuracy of the first diagnosis on CBCT was much higher than that on PAN in the maxilla, both in the anterior and posterior regions (p < 0.05). In the mandible, CBCT had a slightly higher diagnostic accuracy than PAN both in the anterior and posterior regions, but this was not statistically significant (p > 0.05).
Figure 1.
Frequency of correct diagnosis at the first attempt on CBCT versus PAN at different locations in the jaws (*p < 0.05, indicated statistical significance).
Discussion
In the evaluation of intraosseous jaw lesions, clinicians are mainly concerned about the location, size, shape and boundary of the lesions and the relationship with its associated surrounding structures. It is important to choose appropriate radiological examinations to obtain comprehensive diagnostic information, which can aid in planning an appropriate treatment strategy. Our results have shown that significant differences are noted in the radiographical features of intraosseous lesions on CBCT compared to PAN, namely in lesion expansion, cortical involvement, effect on the neurovascular canals and root resorption, especially in the anterior regions of both jaws and in the maxilla. Diagnostic accuracy and clinicians’ confidence while evaluating CBCT have also been shown to be superior compared to PAN. These results could facilitate clinicians’ decisions in choosing the appropriate imaging modalities during surgical planning or follow up.
Imaging features on PAN and CBCT
Comparison of imaging features between PAN and CBCT in the present study was not fully in agreement with the most recent report from Lim et al, in terms of Q2 (border definition), Q4 (continuity of border cortication) and Q7 (effect on the incisive canal or IAC).12
In our results, substantial agreements between PAN and CBCT were shown in Q1 (lesion shape), Q2 (border definition), Q3 (border cortication), Q5 (internal contents) and Q11 (tooth displacement).
In describing lesion shape, although there was strong agreement in the lesion shape between PAN and CBCT, the present study also showed statistical difference between the two modalities. 330 of the total 450 cases were evaluated as the same shape types both on PAN and CBCT, of which 169 cases were evaluated as round or ovoid (usually seen in cysts) and 55 cases were evaluated as “cannot tell” (usually seen in osteomyelitis or malignant tumours), and this may contribute to the substantial agreement in the current study. 26.67% of the cases were evaluated as having different shapes on the two imaging modalities, for instance, round or ovoid on PAN, but scalloped or irregular on CBCT. One explanation for this could be that CBCT is able to display the morphology of lesions from different slices and various views.14 This is diagnostically important as different morphological characteristics often guide differential diagnoses. For example, round or oval shapes are more common in cysts, while lobular or irregular shape suggests the growth characteristics of the other lesions such as ameloblastoma.14–16
The result of Q2 (the border definition) in our study showed substantial agreement, while Lim et al reported only fair agreement.12 90.89% of the cases in this study were described to have the same border definition on PAN and CBCT. This might be attributed to the relatively large sample size and the type of pathology within the sample. The sample size of this study was 225 cases, of which cysts, benign tumours and tumour-like lesions accounted for nearly 80%, while this proportion in Lim’s study was only 50% out of 31 cases.12 Most cysts and benign tumours manifest well-defined borders, and this is also a differentiating feature between benign and malignant diseases.17
In terms of the lesion’s internal contents, substantial agreement was shown between PAN and CBCT, but there was still a statistical difference between the two methods. 81.78% of the cases were evaluated with the same internal densities, of which 61.11% cases were evaluated as radiolucent both on PAN and CBCT. The large proportion of cysts with radiolucency may contribute to the strong agreement. 18.22% of the cases were described as different internal densities between PAN and CBCT (i.e., low density was indicated on PAN, while mixed or high density on CBCT and vice versa). Projection position, exposure condition and overlapping might contribute to inaccurate judgement on PAN, while CBCT could avoid this effectively by virtue of its three-dimensional nature and high spatial resolution.18
Poor agreement was shown in Q4 (continuity of border cortication), Q8 (expansion of surrounding anatomic boundaries), Q9 (cortical thinning) and Q10 (cortical destruction) with significant ORs, respectively, which were consistent with Lim’s results, except for the moderate agreement for Q4 in their study.12
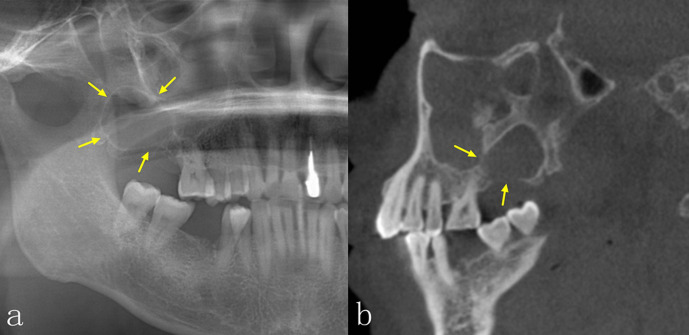
In our study, continuity of the corticated borders was defined as a continuous dense line at the edges of the lesion. Some of the lesions showed clear and continuous corticated borders on PAN because of superimposition, but may appear to be discontinuous on consecutive CBCT images (Figure 2).11
Figure 2.
Odontogenic keratocyst. Continuity of corticated borders were noted on PAN (Figure 2a) but discontinuity was noted on CBCT (Figure 2b, sagittal view).
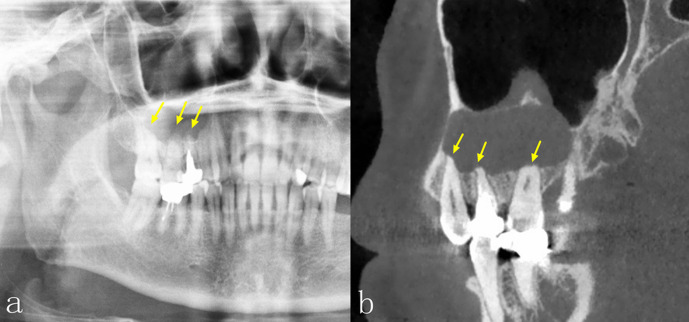
The expansion, thinning and destruction of the bony cortical plates were often related and might be seen when the lesion effaces the cortical bone. Technically, it was impossible to observe the buccal and/or lingual involvements of the lesions on PAN because of its two-dimensional limitations. However, CBCT could successfully overcome this deficiency given its three-dimensional nature and capability for multiplanar reconstruction, and its sensitivity to subtle changes due to the high-spatial resolution used (Figure 3).11,19–22 Defining the boundaries and extent of the lesions could guide surgical plans and also help to avoid damage to surrounding vital anatomic structures.
Figure 3.
Dentigerous cyst. Expansion of boundaries in the anterior maxilla was not noted on PAN (Figure 3a) but clearly shown on CBCT with expansion and cortical thinning on the labial side (Figure 3b, axial view).
Moderate and fair agreements of imaging features were shown in Q6 (lesion locularity), Q7 (effect on the incisive canal or IAC) and Q12 (root resorption).
With regard to the locularity, 30 cases were evaluated as multilocular on CBCT, of which, 15 were evaluated as unilocular on PAN. CBCT has been proven to show the thickness, length and shape of the internal septum more accurately than PAN, which could provide more detailed information for disease diagnosis and differential diagnosis.21,23
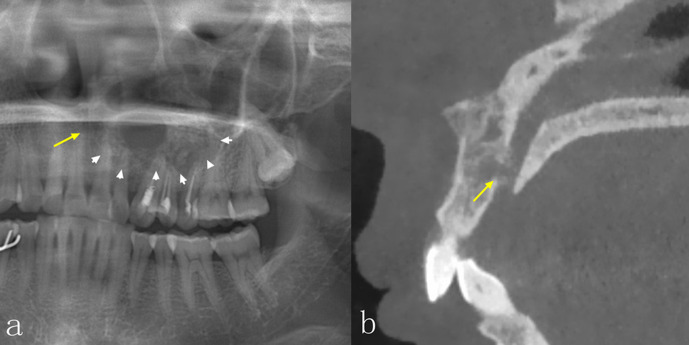
Root resorption can be due to various etiologic factors including inflammation, adjacent impacted teeth, trauma and a variety of lesions, such as benign and malignant tumours and cysts. There was a statistically significant OR of 2.477 on root resorption between the two methods, and this finding was inconsistent with the most recent study by Lim et al, which had insufficient cases to demonstrate differences between PAN and CBCT for this radiographic feature.12 However, it has been proven that CBCT is a more reliable tool for detection of subtle root resorption compared with PAN.11,20,24,25 Our sample size was large enough to show the higher rate of detection of root resorption on CBCT (Figure 4).
Figure 4.
Odontogenic keratocyst. Root resorption was not noted on PAN (Figure 4a) but the irregular and blunted root apices were noted on CBCT (Figure 4b, sagittal view).
Although there was moderate agreement of the effect on neurovascular canals (including displacement, expansion and destruction) between PAN and CBCT, the two modalities still showed significant difference (OR = 2.424, p < 0.001) (Figure 5). 72.89% of the cases were evaluated as the same effect on neurovascular canals both on CBCT and PAN, of which 34.22% paired cases were responded “no” for both CBCT and PAN and this may have led to the moderate agreement. However, neurovascular canals of 62 (23.11%) cases were involved on CBCT as follows: 32 cases showed destruction, 26 cases showed displacement and four cases showed expansion, all of which were not seen on PAN. This further supported that CBCT could better distinguish the involvement type.26,27 Precise evaluations of such involvement are quite valuable since it may effectively prevent iatrogenic injury and avoid unnecessary harm to patients.
Figure 5.
Ameloblastoma. The incisive canal was not involved on PAN (Figure 5a), but was destructed on CBCT (Figure 5b, sagittal view).
Imaging features based on lesion location
The overall agreements of the imaging features between PAN and CBCT in the mandible or posterior regions were higher than those in the maxilla or anterior regions, respectively, except for Q4 (continuity of the border cortication) and Q5 (internal contents). These results were not surprising. The superimposition of the maxillary sinus and the overlap of cervical vertebrae in the anterior regions on PAN may fail to provide sufficient information for image interpretation,1 while mandibular structures are relatively visible and less overlap in the posterior regions would contribute to better imaging interpretation. CBCT, as a three-dimensional imaging modality, would overcome issues of superimposition and overlap, regardless of lesion location.28 These results could potentially be useful if guidelines were developed for the use of CBCT in imaging intraosseous pathology as they indicate that diagnostic yield would be the greatest in the anterior regions of both jaws and in the maxilla.
Diagnostic accuracy and clinicians’ confidence
Contrary to the results from Lim et al.’s study,12 our results showed that the accuracy of the first differential diagnosis on CBCT was higher than that on PAN. CBCT could provide more comprehensive and detailed imaging information, which was helpful for making the diagnosis.8 Although diagnostic accuracy was closely related to the experience of doctors, the discrepancy between the two studies is most likely attributed to the larger sample size in our study. CBCT was accurate in showing the characteristics of lesions, such as location, locularity, internal density, expansion and its effect on the surrounding structures, which could help doctors to make a more accurate diagnosis. It was not surprising that the percentage of correct diagnoses on the first attempt was higher on CBCT than PAN in all regions of jaws, especially in the maxilla.
The limitations of this study
Although our study has yielded some noteworthy findings to support that CBCT was able to demonstrate more radiographic features than PAN and had better diagnostic accuracy in a semi-quantitative way, there are still some limitations need to be addressed. First, there was no unified and quantitative index for describing the imaging features of the lesions. Most of the questions were set to “yes”, “no” and “cannot tell” and lacked of calibration when it came to select “cannot tell”. When there was only a slight variation in the radiographic traits of the lesion, the judgement of the results was greatly influenced by the experience and subjectivity of the observer. Second, as a retrospective study, the scanning parameters of different cases were not completely uniform, although the observers could adjust the contrast, magnification, brightness, size and so on, it was still possible that image interpretation was affected. Finally, the number of cases in the maxilla and the anterior regions was relatively small that might lead to a bias in outcomes, which warrant a further study with a much larger sample size.
Conclusions
The significant differences in the radiographic appearances of intraosseous lesions between PAN and CBCT were shown in the integrity of the corticated borders, expansion of surrounding anatomic boundaries, cortical thinning, cortical destruction and root resorption, especially in the anterior regions of both jaws and in the maxilla. CBCT also improved diagnostic accuracy, especially for lesions in the maxilla. Radiologists were more confident when using CBCT compared to PAN. These findings could potentially be used in the development of guidelines for imaging intraosseous pathology in the jaws.
Footnotes
The authors Donald A Tyndall and Kaiyuan Fu contributed equally to the work.
Contributor Information
Donald A Tyndall, Email: don_tyndall@unc.edu.
Kaiyuan Fu, Email: kqkyfu@bjmu.edu.cn.
REFERENCES
- 1.Suomalainen A, Pakbaznejad Esmaeili E, Robinson S. Dentomaxillofacial imaging with panoramic views and cone beam CT. Insights Imaging 2015; 6: 1–16. doi: 10.1007/s13244-014-0379-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol 1998; 8: 1558–64. doi: 10.1007/s003300050586 [DOI] [PubMed] [Google Scholar]
- 3.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol 1999; 28: 245–8. doi: 10.1038/sj.dmfr.4600448 [DOI] [PubMed] [Google Scholar]
- 4.Spin-Neto R, Wenzel A. Patient movement and motion artefacts in cone beam computed tomography of the dentomaxillofacial region: a systematic literature review. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 121: 425–33. doi: 10.1016/j.oooo.2015.11.019 [DOI] [PubMed] [Google Scholar]
- 5.Tang X, Krupinski EA, Xie H, Stillman AE. On the data acquisition, image reconstruction, cone beam artifacts, and their suppression in axial MDCT and CBCT - A review. Med Phys 2018; 45: e761–82. doi: 10.1002/mp.13095 [DOI] [PubMed] [Google Scholar]
- 6.Suomalainen A, Kiljunen T, Käser Y, Peltola J, Kortesniemi M. Dosimetry and image quality of four dental cone beam computed tomography scanners compared with multislice computed tomography scanners. Dentomaxillofac Radiol 2009; 38: 367–78. doi: 10.1259/dmfr/15779208 [DOI] [PubMed] [Google Scholar]
- 7.Chinem LAS, Vilella BdeS, Maurício CLdeP, Canevaro LV, Deluiz LF, Vilella OdeV. Digital orthodontic radiographic set versus cone-beam computed tomography: an evaluation of the effective dose. Dental Press J Orthod 2016; 21: 66–72. doi: 10.1590/2177-6709.21.4.066-072.oar [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod 2008; 34: 273–9. doi: 10.1016/j.joen.2007.11.023 [DOI] [PubMed] [Google Scholar]
- 9.Kaeppler G, Cornelius C-P, Ehrenfeld M, Mast G. Diagnostic efficacy of cone-beam computed tomography for mandibular fractures. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116: 98–104. doi: 10.1016/j.oooo.2013.04.004 [DOI] [PubMed] [Google Scholar]
- 10.Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, et al. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J Endod 2016; 42: 356–64. doi: 10.1016/j.joen.2015.12.015 [DOI] [PubMed] [Google Scholar]
- 11.Guo J, Simon JH, Sedghizadeh P, Soliman ON, Chapman T, Enciso R. Evaluation of the reliability and accuracy of using cone-beam computed tomography for diagnosing periapical cysts from granulomas. J Endod 2013; 39: 1485–90. doi: 10.1016/j.joen.2013.08.019 [DOI] [PubMed] [Google Scholar]
- 12.Lim LZ, Padilla RJ, Reside GJ, Tyndall DA. Comparing panoramic radiographs and cone beam computed tomography: impact on radiographic features and differential diagnoses. Oral Surg Oral Med Oral Pathol Oral Radiol 2018; 126: 63–71. doi: 10.1016/j.oooo.2018.03.019 [DOI] [PubMed] [Google Scholar]
- 13.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–74. doi: 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 14.Kitisubkanchana J, Reduwan NH, Poomsawat S, Pornprasertsuk-Damrongsri S, Wongchuensoontorn C. Odontogenic keratocyst and ameloblastoma: radiographic evaluation. Oral Radiol 2020;06 Feb 2020. doi: 10.1007/s11282-020-00425-2 [DOI] [PubMed] [Google Scholar]
- 15.MacDonald-Jankowski DS. Keratocystic odontogenic tumour: systematic review. Dentomaxillofac Radiol 2011; 40: 1–23. doi: 10.1259/dmfr/29949053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kreppel M, Zöller J. Ameloblastoma-Clinical, radiological, and therapeutic findings. Oral Dis 2018; 24(1-2): 63–6. doi: 10.1111/odi.12702 [DOI] [PubMed] [Google Scholar]
- 17.Avril L, Lombardi T, Ailianou A, Burkhardt K, Varoquaux A, Scolozzi P, et al. Radiolucent lesions of the mandible: a pattern-based approach to diagnosis. Insights Imaging 2014; 5: 85–101. doi: 10.1007/s13244-013-0298-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chindasombatjaroen J, Poomsawat S, Boonsiriseth K. Two unique cases of calcifying cystic odontogenic tumor in the maxillary posterior region. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118: 497–504. doi: 10.1016/j.oooo.2014.06.006 [DOI] [PubMed] [Google Scholar]
- 19.Linz C, Müller-Richter UDA, Buck AK, Mottok A, Ritter C, Schneider P, et al. Performance of cone beam computed tomography in comparison to conventional imaging techniques for the detection of bone invasion in oral cancer. Int J Oral Maxillofac Surg 2015; 44: 8–15. doi: 10.1016/j.ijom.2014.07.023 [DOI] [PubMed] [Google Scholar]
- 20.Alves DBM, Tuji FM, Alves FA, Rocha AC, Santos-Silva ARD, Vargas PA, et al. Evaluation of mandibular odontogenic keratocyst and ameloblastoma by panoramic radiograph and computed tomography. Dentomaxillofac Radiol 2018; 47: 20170288. doi: 10.1259/dmfr.20170288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luo J, You M, Zheng G, Xu L. Cone beam computed tomography signs of desmoplastic ameloblastoma: review of 7 cases. Oral Surg Oral Med Oral Pathol Oral Radiol 2014; 118: e126–33. doi: 10.1016/j.oooo.2014.07.008 [DOI] [PubMed] [Google Scholar]
- 22.Kämmerer PW, Thiem D, Eisenbeiß C, Dau M, Schulze RKW, Al-Nawas B, et al. Surgical evaluation of panoramic radiography and cone beam computed tomography for therapy planning of bisphosphonate-related osteonecrosis of the jaws. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 121: 419–24. doi: 10.1016/j.oooo.2015.11.012 [DOI] [PubMed] [Google Scholar]
- 23.Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Di Bartolomeo F, et al. Odontogenic keratocyst: imaging features of a benign lesion with an aggressive behaviour. Insights Imaging 2018; 9: 883–97. doi: 10.1007/s13244-018-0644-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alamadi E, Alhazmi H, Hansen K, Lundgren T, Naoumova J. A comparative study of cone beam computed tomography and conventional radiography in diagnosing the extent of root resorptions. Prog Orthod 2017; 18: 37. doi: 10.1186/s40510-017-0191-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alqerban A, Jacobs R, Souza PC, Willems G. In-Vitro comparison of 2 cone-beam computed tomography systems and panoramic imaging for detecting simulated canine impaction-induced external root resorption in maxillary lateral incisors. Am J Orthod Dentofacial Orthop 2009; 136: 764.e1–764.e11. doi: 10.1016/j.ajodo.2009.03.036 [DOI] [PubMed] [Google Scholar]
- 26.Abdi I, Taheri Talesh K, Yazdani J, Keshavarz Meshkin Fam S, Ghavimi MA, Arta SA. The effect of ameloblastoma and keratocystic odontogenic tumor on the displacement pattern of inferior alveolar canal in CBCT examinations. J Dent Res Dent Clin Dent Prospects 2016; 10: 155–61. doi: 10.15171/joddd.2016.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sahman H, Sekerci AE, Sisman Y, Payveren M. Assessment of the visibility and characteristics of the mandibular incisive canal: cone beam computed tomography versus panoramic radiography. Int J Oral Maxillofac Implants 2014; 29: 71–8. doi: 10.11607/jomi.3304 [DOI] [PubMed] [Google Scholar]
- 28.Meng Y, Zhao Y-N, Zhang Y-Q, Liu D-G, Gao Y. Three-Dimensional radiographic features of ameloblastoma and cystic lesions in the maxilla. Dentomaxillofac Radiol 2019; 48: 2019006648:20190066.. doi: 10.1259/dmfr.20190066 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.