Abstract
Objectives:
Coronary artery calcium measured by CT predicts future coronary events. Similarly, carotid artery calcium on dental panoramic radiographs has been associated with increased cardiovascular events. Pre-procedural assessment of candidates for valve replacement in our institution includes panoramic radiographs and chest tomography. We aimed to assess the association of carotid calcium on panoramic radiographs with coronary artery calcium on chest tomography.
Methods:
Paired pre-procedural panoramic radiographs and chest tomography scans were done in 177 consecutive patients between October 2016 and October 2017. Carotid calcium was quantified using NIH’s ImageJ. Coronary artery calcium was quantified by the Agatston score using Philips Intellispace portal, v. 8.0.1.20640.
Results:
Carotid calcium maximal intensity, area and perimeter were higher among patients with high coronary artery calcium. Non-zero carotid calcium was found in half of patients with high coronary artery calcium, doubling prevalence of low coronary artery calcium.
Conclusion:
Carotid calcium identified in panoramic radiographs was associated with high coronary artery calcium. Awareness of carotid calcium recognized by dental practitioners in low-cost, low radiation and commonly done panoramic radiographs may be useful to identify patients at risk of coronary disease with potential future cardiovascular events.
Keywords: Radiography, Panoramic, ComputerizedTomography, Carotid artery, Coronary artery
Introduction
Coronary heart disease (CHD) and stroke are the leading causes of death and disability associated with cardiovascular disease (CVD).1 Currently, coronary artery calcium (CAC) scoring, carotid intima-media thickness, carotid plaque presence, carotid plaque score, and total plaque area and endothelial function tests are used to assess risk for CVD and CVD events (coronary and cerebrovascular).2–5 Carotid calcium can be recognized in dental panoramic radiographs and has been associated with CVD risk.6–8 Panoramic radiography provides images of the middle and mainly lower thirds of the face are obtained using an extra oral technique in which the X-ray machine rotates around the patient, acquiring a virtual image. This technique enables examination of both upper and lower jaws as well as the neighboring structures in a single X-ray Image. Along with intraoral radiographs, it is considered the dental diagnostic imaging of choice.8
Our institutional pre-procedural preparation protocol for valve replacement, either transcutaneous aortic valve replacement (TAVR) or surgical valve (any valve) replacement (SVR) include dental panoramic radiographs as part of the assessment of oral health and pre/post-procedural treatment if necessary. All candidates had also a non-gated non-contrast enhanced chest CT scan. In TAVR candidates, CT was done for CAC scoring, aortic valve calcium scoring and angiography as part of the TAVR valve sizing,9,10 and in SVR candidates, it was done to assess ascending aortic calcium as a means to evaluate feasibility and location for placement of the aortic clamp, that could be scored for CAC11 as well. This provided us with a unique situation where we had paired dental panoramic radiographs with carotid calcium and cardiac CT scans with CAC measurements.
The reliability of panoramic radiographs12 as a screening tool for detecting carotid calcium was previously assessed by many studies, but no consensus was achieved. A meta-analysis published in 2019 aimed to determine the diagnostic accuracy of panoramic radiography in detecting calcified carotid artery atheroma, summarized the data from 12 studies (out of 773), and concluded that most studies reported excellent sensitivity and good specificity. The diagnostic accuracy of panoramic radiographs was good or excellent in 50% of the studies.13 Nonetheless, other studies found that these radiographs do not seem to be a good screening tool for detection of carotid stenosis and are not cost effective for this purpose.14–16
To assess the use of panoramic radiographs as a screening tool for coronary artery disease, our aim was to determine the association of carotid calcium on dental panoramic radiographs with clinically important level coronary artery calcification in chest CT.
Methods and materials
Study population
Between October 2016 and October 2017, all candidates for aortic valve replacement were prospectively referred to our Oral medicine unit for evaluation and treatment if needed. The oral medicine team was blinded to the type of planned interventional treatment (TAVR vs SVR).
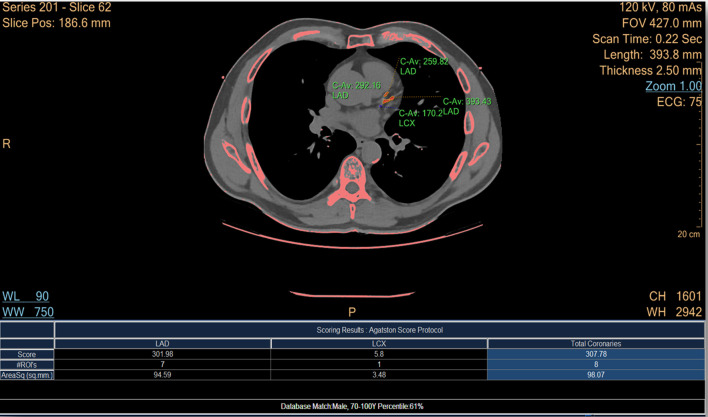
Coronary calcium scoring (Figure 1). All scans were performed using a 256-row scanner (Brilliance iCT, Philips Healthcare, Cleveland, OH). Non-gated chest LDCT scan ranged from the apical to the top of the diaphragm. Scanning parameters were as follows: tube voltage, 120 kV; tube current, 50 mA; collimation, 128 * 0.625 mm; pitch, 0.758 [Rongrong Fan, MS]. IMR, an optimized protocol to reduce image noise and improve image resolution for CACS on non-gated chest LDCT, was adopted in our study. Parameter setting of soft tissue Level 1 was chosen. The reconstruction slice thickness and interval were both 2.5 mm. Agatston calcium score was measured using a commercial CAD workstation (Philips Intellispace portal, v. V8.0.1.20640 (2016); Philips Healthcare Nederland B.V.) with Heart-Beat CS Agatston analysis software. Traditional coronary artery calcium scoring (CAC) on a non-enhanced scan involves1 reconstruction of images with 3 mm slice thickness,2 calcium segmentation, performed semi-automatically by selecting all pixels >130 HU in the coronary arteries, and3 Scoring (by the software), measured slice by slice by summing the two-dimensional area of each lesion in the slice multiplied by a factor determined by the maximal intensity of the calcium lesion in that slice. Patients with previous PCI were automatically scored at 400 Agatston.
Figure 1.
Coronary artery calcium scoring. Screenshot of the calcium-scoring application. Thresholds for calcium are automatically highlighted. Separate coronary region of interest are manually selected (with automatic 3D extension) to calculate separate and cumulative CAC score. 3D, three-dimensional; CAC, coronary artery calcium; FOV, filed of view.
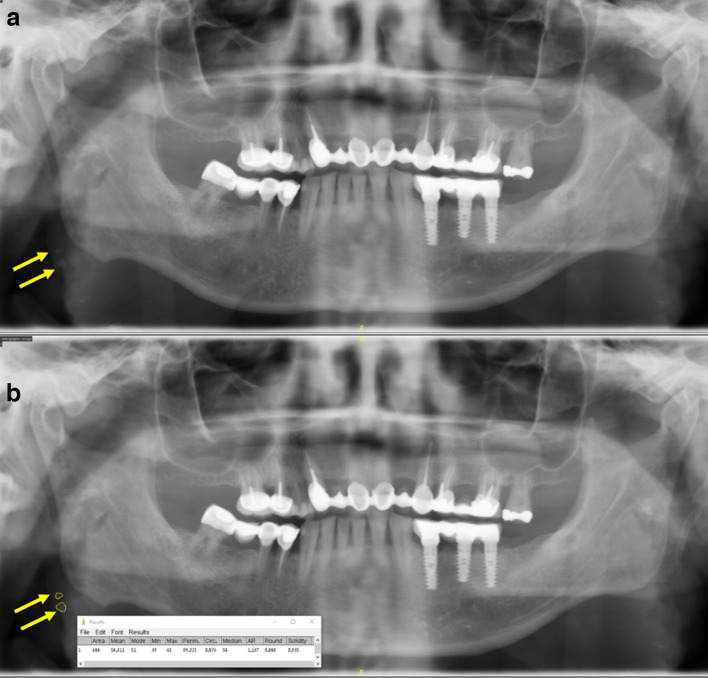
Quantitative assessment of carotid calcium (Figure 2). Panoramic radiographs analyses were performed using NIH’s ImageJ.17 The region of interest (ROI) was set at the carotid bifurcation (area posterior to the angle of the mandible adjacent to of C3–C4 vertebrae). Using the free-hand selection tool, a ROI was drawn around the calcification. The intensity of the ROI was assessed using the measurement tools on the Analyze menu (Analyze/Measure)of ImageJ to characterize the ROI by calculating the minimum, maximum, mean, and median of the ROI’s pixel intensity as well as its perimeter. Panoramic radiographs were analyzed by a single reviewer (DPBA) blinded to the CAC measurements.
Figure 2.
Carotid calcium in dental panoramic radiograph. A - Dental panoramic radiograph. Arrows mark carotid calcium. B- NIH ImageJ calculations of carotid calcium region of interest.
Statistical analysis
Patients were divided into two group based on their coronary calcium score according to the outcomes of the CONFIRM study5 for values suggested as cut-off values requiring positive interventions5 : Group 1 – CAC <100, included patients with CAC = 0 (no coronary artery disease) and patients with CAC = 1–99 (statin treatment was not associated with improved outcomes) Group 2 – CAC ≥100, included patients with CAC = 100–299 (statin treatment was shown to be associated with improved outcomes) and patients CAC ≥300 (coronary angiography suggested).
Continuous variables are presented as medians and confidence intervals (CI). Comparison between groups was performed using the Mann–Whitney test (independent samples) for continuous variables as normal distributions could not be assured, and the Fisher's exact test for categorical variables. Statistical significance was set at p < 0.05. Statistical analyses were done using MedCalc Statistical Software version 18.11.6 (MedCalc Software bvba, Ostend, Belgium; https://www.medcalc.org; 2019).
The following predetermined variables were tested as univariable associates of CAC > 100: age, sex and body mass index; cardiovascular risk factors: smoking, hypertension, hypercholesterolemia, history of diabetes mellitus and renal failure; cardiovascular disease history: previous percutaneous coronary interventions (PCI), and presence of carotid calcium on panoramic radiographs. A process of a stepwise multiple logistic regression analysis was used to identified the independent prognostic variables for the risk score for CAC ≥ 100 in randomly selected 75% of cases (training cohort). Previous PCI was excluded from the model as it already indicated presence of coronary calcium. A simple score system was developed from all (except previous PCI) significant indicators of risk (p < 0.01, β coefficients > 0.5) developed:each risk factor was weighted proportionally to the value of the β-coefficients of the logistic regression rounded to the nearest integer. The risk assessment score of each patient was obtained by summing all individual points. A receiver operating characteristic curve was used to evaluate the discriminative power of the model. This curve represented corresponding values of sensitivity and specificity with all values of the score as a criterion to predict CAC ≥ 100 on cardiac CT scans. The criterion value was set at the optimal combination of sensitivity/specificity combination. The predictive performance of the model was assessed through internal cross-validation on the rest 25% of cases (validation cohort).
Results
Patients
During the study period, 177 consecutive patients (age 69 ± 12 years, 53% male gender, CI 45–61) had paired pre-procedural dental panoramic radiographs and chest CT/Cardiac CTs. The median time between pre-procedural examination and TAVR or SVR was 5 days (95% CI for the median: 4–7 days). Coronary disease risk factors were common – 131 (74%, CI 67–80) had hypertension, 72 (41%, CI 34–49) had diabetes mellitus, 114 (64%, CI 56–71) had dyslipidemia, 46 (26%, CI 20–33) were current or past smokers, and 38 (21%, CI 15–28) – had renal failure (serum creatinine ≥1.3 mg dl−1). Patients undergoing TAVR were a decade older compared patients undergoing SVR (n = 60, age 79 ± 6, 42% CI 29–55 male gender vs n = 117, age = 64±11, 59% CI 50–68 male gender, p < 0.01 respectively).
Carotid calcium
Carotid calcification defined as non-zero maximal intensity of carotid ROIs was demonstrated in 33% (n = 58) of patients. In these patients, the average maximal intensity was 883 ± 439 Hounsfield units (HU), the ROI perimeter was 24 ± 18 mm, its area was 30 ± 40 mm2 with an average raw integrated density of 2.79 × 106 ± 0.49 x 106. There were no clinical differences between patients without compared to patients with carotid calcium on panoramic radiographs (Table 1).
Table 1.
Clinical characteristics of patient with carotid calcium identified by NIH ImageJ
| No carotid calcium n = 119 | Carotid calcium n = 58 | p-value | |
|---|---|---|---|
| Age (years) (median,CI for median) | 69 (63–72) | 72 (67–77) | 0.435 |
| Sex male n, (%, CI) | 66 (55, 46–64) | 28 (48, 35–62) | 0.262 |
| Body mass index (median, 25, 75 percentiles) | 29 (28–31) | 29 (27, 31) | 0.571 |
| Dyspnea n, (%, CI) | 82 (69, 60–77) | 35 (60, 46–73) | 0.644 |
| Chest pain n, (%, CI) | 56 (47, 38–56) | 25 (43, 30–57) | 0.300 |
| Previous PCI n, (%, CI) | 41 (34, 26–43) | 24 (41, 28–55) | 0.501 |
| Diabetes mellitus n, (%, CI) | 48 (40, 31–49) | 24 (41, 29–55) | 0.869 |
| Dyslipidemia n, (%, CI) | 75 (63, 54–72) | 39 (67, 53–79) | 0.614 |
| Hypertension n, (%, CI) | 86 (72, 63–80) | 45 (78, 65–88) | 0.583 |
| Smoking n, (%, CI) | 66 (55, 46–74) | 25 (43, 30–57) | 0.058 |
| Renal failure n, (%, CI) | 26 (22, 15–31) | 12 (21, 11–34) | 0.697 |
CI, confidence interval;PCI, Percutaneous coronary intervention.
Coronary artery calcium
Only 20 patients (5%) had a CAC of 0. Their age was 53 ± 14 years, and 40% of them were males. Concomitant CABG was done in one patient of this group. Table 2 compares the clinical characteristics of patients with CAC < 100 to patients with CAC ≥ 100. Higher age was the parameter that demonstrated the strongest association with CAC in the suggested intervention range (statin + aspirin/coronary angiography),patients with CAC ≥ 100 were a decade older; more of them were males, they were more likely to have had a previous coronary intervention, hypertension and renal failure compared to patients in the no-intervention CAC range (CAC < 100). While the left ventricular systolic function was similar in both groups, the CAC ≥ 100 had significantly more left ventricular hypertrophy.
Table 2.
Clinical characteristics of patients groups divided by clinically important coronary artery calcium
| CAC <100 n = 57 |
CAC ≥100 n = 120 |
p-value | |
|---|---|---|---|
| Age (years) (median, CI for median) | 64 (56–67) | 73 (70–76) | <0.0001 |
| Sex male n, (%, CI) | 22 (39, 26–53) | 72 (60, 51–69) | 0.008 |
| Body mass index (median, CI for median) | 31 (28–32) | 28 (27–39) | 0.200 |
| Dyspnea n, (%, CI) | 38 (81, 68-90( | 79 (84, 76–90) | 0.644 |
| Chest pain n, (%, CI) | 23 (68, 57–80) | 58 (71, 62–79) | 0.669 |
| Previous PCI n, (%, CI) | 7 (13, 6–25) | 58 (51, 42–60) | <0.0001 |
| Diabetes mellitus n, (%, CI) | 20 (35, 23–49) | 52 (46, 37–55) | 0.250 |
| Dyslipidemia n, (%, CI) | 28 (50, 36–64) | 86 (72, 63–80) | 0.004 |
| Hypertension n, (%, CI) | 29 (51, 37–65) | 102 (85, 77–91) | <0.0001 |
| Smoking n, (%, CI) | 16 (36, 24–50) | 32 (26, 18–35) | 1.000 |
| Renal failure n, (%, CI) | 6 (10, 4–21) | 32 (26, 18–35) | 0.019 |
CAC, coronary artery calcium; CI, confidence interval;PCI, Percutaneous coronary intervention.
Carotid and coronary calcium associations
Table 3 compares the carotid calcium seen in panoramic radiographs according to the CAC classification. There was large variability in all measured parameters, yet the average maximal intensity, ROI area and perimeter were significantly higher among patients in the high compared to the low CAC score group. Any level of carotid calcium (Non-zero maximal intensity in panoramic radiographs, Max >0) was found in nearly half of the patients with the high CAC score, and twice the prevalence of Max >0 in the low CAC score group. In a stepwise multivariable logistic regression model including coronary risk factors (Age ≥ 65, male sex, hypertension, hyperlipidemia, diabetes mellitus and smoking) and Max >0, Age >= 65, Male sex, hypertension, hyperlipidemia and Max >0 remained as significant associates of intervention level CAC score (Table 4).
Table 3.
Region of interest pixel parameters measured by NIH's ImageJ of carotid calcium lesions on panoramic radiographs
| CAC <100 n = 57 |
CAC ≥100 n = 120 |
p-value | |
|---|---|---|---|
| Intensity | |||
| Minimal (median, CI) | 0 (0–0) | 0 (0–191) | 0.209 |
| Maximal (median, CI) | 0 (0–65) | 0 (0–977) | 0.105 |
| Mean (median, CI) | 0 (0, 23) | 0 (0–578) | 0.140 |
| Median (median, CI) | 0 (0–20) | 0 (0–572) | 0.135 |
| Area (median, CI) | 0 (0–1) | 0 (0–8) | 0.077 |
| Perimeter | 0 (0–2) | 0 (0–11) | 0.091 |
| Maximal >0 (n, %, CI) | 13 (3, 6–25) | 59 (46, 37–55) | 0.009 |
CAC, coronary artery calcium; CI, confidence interval.
Table 4.
Predictors of CAC ≥ 100 in a stepwise logistic regression analysis
| β –Coefficient | HR 95% confidence intervals |
p-value | |
|---|---|---|---|
| Age ≥ 65 | 1.35 | 3.9 (1.7–8.5) | 0.0008 |
| Male sex | 1.01 | 2.8 (1.3–1.9 | 0.0091 |
| Hypertension | 1.27 | 3.6 (1.6–8.1) | 0.0023 |
| Dyslipidemia | 0.36 | 1.43 (0.6–3.2) | 0.386 |
| Non-zero carotid calcium | 0.79 | 2.2 (1.01–4.8) | 0.043 |
CAC, coronary artery calcium; HR, hazard ratio.
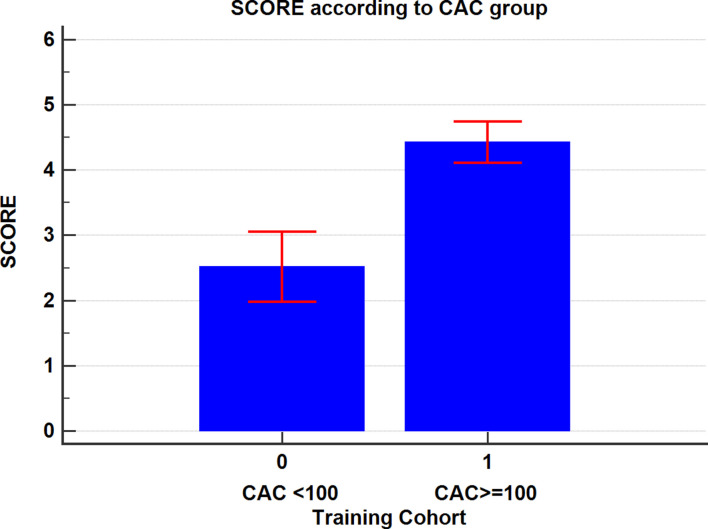
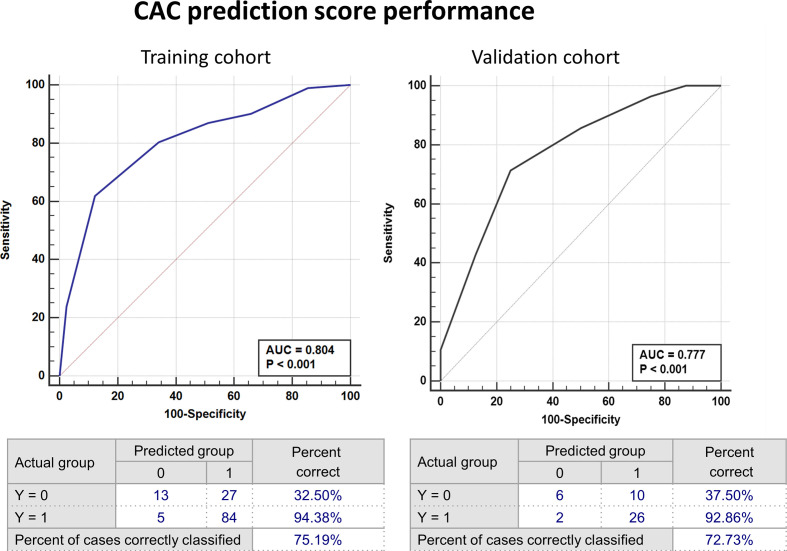
Using multiple regression analysis, a prediction score for CAC ≥ 100 was devised using the relative ratios of the β coefficients on randomly selected 75% of cases (training cohort). Age > 65 years and hypertension received 2 points each, male sex and Max >0 received 1 point each (maximum score = 6) for association with an intervention level CAC. Figure 3 demonstrates the score average for the two CAC groups in the training cohort. A score >3 was found to be 80% sensitive (95% CI 71–88) and 66% specific (95% CI 49–80) for CAC ≥ 100 (AUC = 0.804, p < 0.001, 95% CI 0.73–0.87).In the validation cohort score performance was similar (AUC = 0.78, p < 0.001, 95% CI 0.63–0.89) with sensitivity of 71% (95% CI 51–86) and specificity of 75% (95% CI 47–93)(Figure 4). A score of >2 demonstrated better performance as a screening tool in both cohorts being 86% sensitive (95% CI 67–96) and 50% specific (95% CI 24–75) for CAC ≥ 100. The positive and negative predictive values were 75 and 67%, respectively.
Figure 3.
Prediction model score in patients divided according to presence of intervention-level coronary calcium. Comparison of Score according to intervention-level coronary artery calcium (CAC ≥100 Agatson units) in traing group. CAC, coronary artery calcium.
Figure 4.
Performance of model for association with intervention-level CAC Comparison of ROC for model in the training and validation groups for association with CAC ≥100. AUC, area under curve; CAC, coronary artery calcium; ROC, receiver operating curves.
Discussion
We have shown here that in patients evaluated for either percutaneous or surgical valve intervention, presence of carotid calcium in dental panoramic radiographs was associated with clinically significant coronary artery calcium score measured on chest CTs done a few days apart.
The association between coronary and carotid artery atherosclerosis
Atherosclerosis is a systemic disease that may result in most cerebrovascular and cardiac events18 has a long asymptomatic period before clinical signs and/or symptoms actually occur. Early diagnosis may provide an opportunity to prevent subsequent events by specific interventions as life-style modifications, drug therapy (aspirin + statin) or therapeutic coronary catheterization.5 A simple, commonly used sensitive non-invasive screening tool would be ideal for that purpose.
The coronary-carotid diseases relationship has been described in several studies.19–22 Clinical findings indicate that arteries may be affected by atherosclerosis simultaneously in several sites. Finding disease at any site may suggest presence of arterial disease elsewhere.18,19 In fact, coronary and carotid arteries atherosclerosis were found to significantly correlate in three autopsy studies.19,23,24
Increased carotid artery intima–media thickness as well as non-invasive endothelial function tests are considered to be a marker of early stage atherosclerosis that may be a precursor of future carotid calcifications. Increased carotid wall thickness has been suggested as a general measure of atherosclerosis load.25,26 Morphologically coronary and carotid atherosclerosis formation has been shown to be similar in both cases.27
Therefore, detection of subclinical atherosclerotic lesions, such as in the carotid arteries, is of great importance in reducing future risk of cardiovascular events.28
Dental panoramic radiography
The anatomic intricacy of the dental-maxillofacial field makes diagnostic imaging difficult. Panoramic radiography provides a view of jaws and dentition, as well as adjacent structures. It has been used since the early 1950's in attempt to image the jaws, but it was also applied to other juxtaposed anatomic regions.12 Panoramic radiographs are routinely and widely performed in dental practice and carotid artery calcifications can be detected at early stage by routine dental panoramic radiograph.29 We have shown here that identification of carotid calcification in panoramic radiographs triples the risk of presence of high-enough CAC to warrant clinical intervention that may prevent future cardiovascular events.5 Regarding the CAC ≥ 100 prediction model, it needs to be acknowledged that there is a trade-off between sensitivities specificities according to the selected score criterion. As a screening tool in a rather high prevalence of disease (68% of cases had CAC ≥ 100 in our cohort) a score with higher sensitivity is probably preferred. A score >2 was found to be sensitive with high positive- and negative predictive values. However, the prevalence of CAC ≥ 100 in the general population was previously found to be actually lower, in the range of 20%.30 Recalculating these values for the infinite-data case scenario yielded a positive predictive value of 36.4% (CI 27.003 to 46.873%) and a negative predictive value of 92.3% (CI 89.0 to 94.7%). This would suggest further testing in patients with a high score, while reassuring patients with a low score are at low risk of coronary artery disease.
The role of the dental practitioners in prevention of coronary artery disease manifestations
Dentists and other dental care providers do not routinely check for the presence carotid calcifications, and if noted they usually overlooked and not reported. As shown, they can easily be detected on panoramic radiographs below the angle of the mandible, next to the third and fourth cervical vertebrae as irregular radio-opacities in variable sizes.31 Panoramic radiographs are abundantly done as the initial diagnostic tool for planning dental treatment in patients of all age groups, and may be repeated over time. Thus, dental practitioners are situated at strategic point where they could screen for early carotid and coronary atherosclerosis and prompt diagnostic and therapeutic measures that may result in reduction of subsequent cardiovascular adverse events.
Finally, dental practitioners should be aware of these not so rare findings, note their lack or presence, report them to the family physician for further evaluation and follow them over time.13,29,32
Limitations
This is a report of a small retrospective study, and as such may be biased. Larger prospective longitudinal studies are needed to confirm the effect of noting carotid calcium triggering interventions on subsequent events. The study group encompassed a large age and comorbidities group. Yet, it was a select group of patients undergoing valve replacement that may not represent the general population presenting to dental practitioners.
Conclusions
Carotid calcium identified in dental panoramic radiographs was associated with clinically significant CAC evaluated with cardiac CT. Awareness of carotid calcium recognized by dental practitioners in low-cost, low radiation and commonly done panoramic radiographs may be useful to identify patients at risk of coronary disease with potential future cardiovascular events.
Footnotes
Ethics: This study was approved by the institutional ethics board as part of the cardiovascular division clinical and interventional registry.
The authors Shemy Carasso and Dalit Porat Ben Amy contributed equally to the work.
Contributor Information
Shemy Carasso, Email: shemy.carasso@gmail.com.
Dalit Porat Ben Amy, Email: dalit.porat@gmail.com, dporat@pmc.gov.il.
Mariana Issawy, Email: mariana.issawy@gmail.com.
Fabio Kusniec, Email: Fkusniec@poria.health.gov.il.
Diab Ghanim, Email: DGanem@poria.health.gov.il.
Doron Sudarsky, Email: DSudarsky@poria.health.gov.il.
Gabby Elbaz-Greener, Email: gabbyelbaz@yahoo.com.
Wadi Kinany, Email: WKinany@poria.health.gov.il.
Chen Shmuel, Email: goldameir2000@gmail.com.
Imad Abu El-Naaj, Email: iabu@poria.health.gov.il.
Erez Kachel, Email: EKachel@poria.health.gov.il.
Offer Amir, Email: oamir@hadassa.org.il.
REFERENCES
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke Statistics-2017 update: a report from the American heart association. Circulation 2017; 135: e146–603. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gepner AD, Young R, Delaney JA, Budoff MJ, Polak JF, Blaha MJ, et al. Comparison of carotid plaque score and coronary artery calcium score for predicting cardiovascular disease events: the multi-ethnic study of atherosclerosis. J Am Heart Assoc 2017; 6: e00517914 02 2017. doi: 10.1161/JAHA.116.005179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gepner AD, Young R, Delaney JA, Tattersall MC, Blaha MJ, Post WS, et al. Comparison of coronary artery calcium presence, carotid plaque presence, and carotid intima-media thickness for cardiovascular disease prediction in the multi-ethnic study of atherosclerosis. Circ Cardiovasc Imaging 2015; 8. doi: 10.1161/CIRCIMAGING.114.002262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nambi V, Chambless L, Folsom AR, He M, Hu Y, Mosley T, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (atherosclerosis risk in communities) study. J Am Coll Cardiol 2010; 55 :: 1600–7Apr 13;55(15). doi: 10.1016/j.jacc.2009.11.075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho Y-K, Nam C-W, Koo B-K, Schulman-Marcus J, Hartaigh Bríain Ó, Gransar H, et al. Usefulness of baseline statin therapy in non-obstructive coronary artery disease by coronary computed tomographic angiography: from the confirm (coronary CT angiography evaluation for clinical outcomes: an international multicenter) study. PLoS One 2018; 13: e0207194. doi: 10.1371/journal.pone.0207194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen SN, Friedlander AH, Jolly DA, Date L. Carotid calcification on panoramic radiographs: an important marker for vascular risk. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002; 94: 510–4. doi: 10.1067/moe.2002.125580 [DOI] [PubMed] [Google Scholar]
- 7.Guimaraes Henriques JC, Kreich EM, Helena Baldani M, Luciano M. Cezar de melo Castilho J, CESAR de Moraes L. panoramic radiography in the diagnosis of carotid artery atheromas and the associated risk factors. Open Dent J 2011; 5: 79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borba DL, Hipólito UV, Pereira YCL. Early diagnosis of atherosclerosis with panoramic radiographs: a review. J Vasc Bras 2016; ; 15: 302–7Oct-Dec. doi: 10.1590/1677-5449.002316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Litmanovich DE, Ghersin E, Burke DA, Popma J, Shahrzad M, Bankier AA. Imaging in transcatheter aortic valve replacement (TAVR): role of the radiologist. Insights Imaging 2014; 5: 123–45. doi: 10.1007/s13244-013-0301-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blanke P, Weir-McCall JR, Achenbach S, Delgado V, Hausleiter J, Jilaihawi H, et al. Computed Tomography Imaging in the Context of Transcatheter Aortic Valve Implantation (TAVI)/Transcatheter Aortic Valve Replacement (TAVR): An Expert Consensus Document of the Society of Cardiovascular Computed Tomography. JACC Cardiovasc Imaging 2019; 12: 1–24. doi: 10.1016/j.jcmg.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 11.Hughes-Austin JM, Dominguez A, Allison MA, Wassel CL, Rifkin DE, Morgan CG, et al. Relationship of coronary calcium on standard chest CT scans with mortality. JACC Cardiovasc Imaging 2016; 9: 152–9. doi: 10.1016/j.jcmg.2015.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hallikainen D. History of panoramic radiography. Acta Radiol 1996; 37(3 Pt 2): 441–5. doi: 10.1177/02841851960373P207 [DOI] [PubMed] [Google Scholar]
- 13.Schroder AGD, de Araujo CM, Guariza-Filho O, Flores-Mir C, de Luca Canto G, Porporatti AL. Diagnostic accuracy of panoramic radiography in the detection of calcified carotid artery atheroma: a meta-analysis. Clin Oral Investig 2019; 23: 2021–40. doi: 10.1007/s00784-019-02880-6 [DOI] [PubMed] [Google Scholar]
- 14.Khosropanah SH, Shahidi SH, Bronoosh P, Rasekhi A. Evaluation of carotid calcification detected using panoramic radiography and carotid Doppler sonography in patients with and without coronary artery disease. Br Dent J 2009; 207: E8discussion 162-3. doi: 10.1038/sj.bdj.2009.762 [DOI] [PubMed] [Google Scholar]
- 15.Madden RP, Hodges JS, Salmen CW, Rindal DB, Tunio J, Michalowicz BS, et al. Utility of panoramic radiographs in detecting cervical calcified carotid atheroma. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 103: 543–8. doi: 10.1016/j.tripleo.2006.06.048 [DOI] [PubMed] [Google Scholar]
- 16.Deahl ST. Panoramic radiography does not reliably detect carotid artery calcification nor stenosis. J Evid Based Dent Pract 2007; 7: 172–3. doi: 10.1016/j.jebdp.2007.09.009 [DOI] [PubMed] [Google Scholar]
- 17.Schneider CA, Rasband WS, Eliceiri KW. Nih image to ImageJ: 25 years of image analysis. Nat Methods 2012; 9: 671–5. doi: 10.1038/nmeth.2089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lanzer P. Vascular multimorbidity in patients with a documented coronary artery disease. Z Kardiol 2003; 92: 650–9. doi: 10.1007/s00392-003-0954-z [DOI] [PubMed] [Google Scholar]
- 19.Mitchell JR, Schwartz CJ. Relationship between arterial disease in different sites. A study of the aorta and coronary, carotid, and iliac arteries. Br Med J 1962; 1: 1293–301. doi: 10.1136/bmj.1.5288.1293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kablak-Ziembicka A, Tracz W, Przewlocki T, Pieniazek P, Sokolowski A, Konieczynska M. Association of increased carotid intima-media thickness with the extent of coronary artery disease. Heart 2004; 90: 1286–90. doi: 10.1136/hrt.2003.025080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Granér M, Varpula M, Kahri J, Salonen RM, Nyyssönen K, Nieminen MS, et al. Association of carotid intima-media thickness with angiographic severity and extent of coronary artery disease. Am J Cardiol 2006; 97: 624–9. doi: 10.1016/j.amjcard.2005.09.098 [DOI] [PubMed] [Google Scholar]
- 22.Lekakis JP, Papamichael CM, Cimponeriu AT, Stamatelopoulos KS, Papaioannou TG, Kanakakis J, et al. Atherosclerotic changes of extracoronary arteries are associated with the extent of coronary atherosclerosis. Am J Cardiol 2000; 85: 949–52. doi: 10.1016/S0002-9149(99)00907-8 [DOI] [PubMed] [Google Scholar]
- 23.Holme I, Enger SC, Helgeland A, Hjermann I, Leren P, Lund-Larsen PG, et al. Risk factors and raised atherosclerotic lesions in coronary and cerebral arteries. statistical analysis from the Oslo study. Arteriosclerosis 1981; 1):: 250–6Jul-Aug;. doi: 10.1161/01.ATV.1.4.250 [DOI] [PubMed] [Google Scholar]
- 24.Young W, Gofman JW, Tandy R, Malamud N, Waters ES. The quantitation of atherosclerosis. II. Quantitative aspects of the relationship of blood pressure and atherosclerosis. Am J Cardiol 1960; 6: 294–9. [DOI] [PubMed] [Google Scholar]
- 25.Zureik M, Ducimetière P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr C, et al. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: longitudinal results from the aging vascular study (EVA) study. Arterioscler Thromb Vasc Biol 2000; 20: 1622–9. doi: 10.1161/01.atv.20.6.1622 [DOI] [PubMed] [Google Scholar]
- 26.Ikeda N, Gupta A, Dey N, Bose S, Shafique S, Arak T, et al. Improved correlation between carotid and coronary atherosclerosis SYNTAX score using automated ultrasound carotid bulb plaque IMT measurement. Ultrasound Med Biol 2015; 41: 1247–62. doi: 10.1016/j.ultrasmedbio.2014.12.024 [DOI] [PubMed] [Google Scholar]
- 27.Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol 2010; 30: 177–81. doi: 10.1161/ATVBAHA.108.173609 [DOI] [PubMed] [Google Scholar]
- 28.Zhang W, Jin H, Cheng W, Rao S, Lu X, Zeng M. Correlation of coronary atherosclerosis and subclinical plaque phenotype of carotid artery: a 320-row multidetector computed tomographic angiography study. J Comput Assist Tomogr 2013; ; 37: 701–6Sep-Oct. doi: 10.1097/RCT.0b013e318299f006 [DOI] [PubMed] [Google Scholar]
- 29.Friedlander AH, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol 1981; 52: 102–4. doi: 10.1016/0030-4220(81)90181-X [DOI] [PubMed] [Google Scholar]
- 30.Ilangkovan N, Mogensen CB, Mickley H, Lassen AT, Lambrechtsen J, Sand NPR, et al. Prevalence of coronary artery calcification in a non-specific chest pain population in emergency and cardiology departments compared with the background population: a prospective cohort study in southern Denmark with 12-month follow-up of cardiac endpoints. BMJ Open 2018; 8: e018391. doi: 10.1136/bmjopen-2017-018391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedlander AH, Manesh F, Wasterlain CG. Prevalence of detectable carotid artery calcifications on panoramic radiographs of recent stroke victims. Oral Surg Oral Med Oral Pathol 1994; 77: 669–73. doi: 10.1016/0030-4220(94)90332-8 [DOI] [PubMed] [Google Scholar]
- 32.Pornprasertsuk-Damrongsri S, Virayavanich W, Thanakun S, Siriwongpairat P, Amaekchok P, Khovidhunkit W. The prevalence of carotid artery calcifications detected on panoramic radiographs in patients with metabolic syndrome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 108: e57–62. doi: 10.1016/j.tripleo.2009.05.021 [DOI] [PubMed] [Google Scholar]