Abstract
The COVID-19 pandemic has greatly affected the mental health of individuals due to severe changes in their normal life routines. These changes might give rise to stress-induced factors and result in developing maladaptive behaviors. Therefore, the present study tested an explorative sequential mediation model regarding the COVID-19 pandemic as a global natural experiment and hypothesized that fear and depression would be serial mediators of the relationship between intolerance of uncertainty and emotional eating. An online cross-sectional survey with convenience sampling was adopted. A total of 362 participants were recruited from Turkey, and each completed a battery of demographic questions and psychometric scales. The standardized instruments used to test the model’s constructs were the Intolerance of Uncertainty Scale, Fear of COVID-19 Scale, Hospital Anxiety and Depression Scale, and Three-Factor Eating Questionnaire-R21. The model was tested using a bootstrapping method utilizing IBM AMOS 24 software. Results showed that emotional eating was positively associated with intolerance of uncertainty, fear of COVID-19, and depression. Moreover, fear of COVID-19 had positive correlation with intolerance of uncertainty and depression. Significant negative association was also found between age and intolerance of uncertainty. In addition, females significantly reported higher levels of emotional eating and fear of COVID-19 than males. The study’s hypothesized sequential mediation model was further supported. It is concluded that depression most likely developed by fear was triggered by intolerance of uncertainty during the COVID-19 pandemic and leading to emotional eating. The study is significant because it advances theories of emotional eating with an investigation examining some of its underlying mechanisms. Also, it is one of a few research studies highlighting to what extent the COVID-19 pandemic-related cognitions and emotions are associated with maladaptive behaviors in the case of emotional eating.
Keywords: COVID-19, Fear of COVID-19, Intolerance of uncertainty, Depression, Emotional eating
The novel coronavirus disease-2019 (COVID-19) has affected global public health since the first case appeared in China (Bao et al. 2020; Torales et al. 2020). The World Health Organization (2020a) subsequently declared COVID-19 as a pandemic in March 2020. At the time of writing (end of November 2020), the global number of confirmed cases had passed 50 million with over 1 million deaths (World Health Organization 2020b). As one of the world’s fastest-growing pandemics, Turkey (where the present study was carried out) reported its first case on March 11, 2020, and the number of confirmed cases has exceeded 400,000 with over 10,000 deaths (Turkish Ministry of Health 2020; World Health Organization 2020b).
To control the rising numbers of cases and deaths, the Turkish government, like in many countries, has imposed government interventions and restrictions such as the compulsory use of face masks in public, spatial distancing, and lockdowns. However, Turkish citizens have felt under a lot of stress and have experienced mental health issues because of the change to daily life routines caused by the pandemic and government reaction to it. For example, Morgul et al. (2020) conducted a survey in Turkey and reported that 64% of participants categorized themselves as psychologically fatigued because of the COVID-19 pandemic. Moreover, a public opinion survey reported that 90% of adults were worried about getting infected and 70% reported that there would be dramatic changes in their lives after the pandemic in Turkey (Coker 2020).
According to the Center for Disease Control and Prevention (2020), stress during infectious disease pandemics may lead individuals to fear and worry about their own and loved ones’ health, experience changing eating and sleeping patterns, have worsening chronic and mental health conditions, and increased drug use (although the report did not mention whether this use was licit and/or illicit). For nearly a year, individuals around the world have stressed over COVID-19. Previous research regarding the stress-induced outcomes of the COVID-19 pandemic has broadly addressed negative emotions, sleeping issues, drug use, and chronic and mental health conditions (e.g., Auer et al. 2020; Cao et al. 2020; Kavoor 2020; Li et al. 2020; Liang 2020; Pakpour and Griffiths 2020; Rajkumar 2020; Simione and Gnagnarella 2020; Wang et al. 2020; Xiang et al. 2020; Yao et al. 2020). However, the published literature has had a limited focus on how the COVID-19 pandemic has changed eating behaviors despite the media’s calling attention to a risk of emotional eating as a coping strategy for individuals during the pandemic (e.g., Muhlheim 2020; Ro 2020; Warren 2020). Therefore, the present study was designed to identify some potential underlying mechanisms of emotional eating during the COVID-19 pandemic among a Turkish sample. The present study is significant because it is one of a few to elucidate how stress-induced factors arising from the COVID-19 pandemic changes individuals’ eating patterns. Little is known about the underlying mechanisms of emotional eating (Macht and Simons 2011). Consequently, the present study also advances the current understanding concerning emotional eating by investigating several potential underlying mechanisms.
Literature Review
There are various psychological theories explaining the relationship between eating habits and emotions. The core commonality of such theories is that they have an emphasis on bidirectional effects between eating behaviors and emotions. For instance, emotional eating theory asserts that individuals tend to show more emotional eating because negative emotional states may lead to an increase in eating motivations or that eating can function to decrease the intensity of experienced negative emotions (Macht and Simons 2011). Moreover, escape theory posits that individuals might eat more to avoid awareness created in response to ego-threatening stimuli because self-threatening negative moods and awareness raise the desire for binge eating among emotional eaters (Heatherton and Baumeister 1991; Wallis and Hetherington 2004). Regarding the COVID-19 pandemic in relation to these two theories, it can be argued that the pandemic has caused stress among large numbers of individuals around the world because it is an ego-threatening stimulus signaling a risk of death for themselves and/or their loved ones, which may lead to negative emotions and maladaptive behaviors as dysfunctional coping strategies such as emotional eating to reduce the intensity of such cognitive and emotional states. However, the specific cognitions and emotions underlying mechanisms that trigger emotional eating during the pandemic are still unclear.
It is obvious that the COVID-19 pandemic is uncertain in nature. The ambiguity of when the pandemic will end is the most uncertain question (Zandifar and Badrfam 2020). There are also uncertain questions about the severity of infection and the efficiency of prevention methods (Mertens et al. 2020). What is striking is that Turkish individuals’ most prominent cultural pattern is uncertainty avoidance (Hofstede and Hofstede 2005). Therefore, depending upon the insights from the uncertain nature of the pandemic and the distinctive cultural characteristic of Turkey, it was hypothesized that the uncertainty of the pandemic as a cognition would prompt individuals to experience more negative emotions, particularly fear (H1), because fear is the dominant negative emotion under threatening conditions and such conditions might lead to psychological stress and behavior change (Nabi and Myrick 2018; Witte and Allen 2000). From a social psychological perspective, the individuals’ fear can be a fear of something (e.g., deadly virus) or a fear for something (e.g., for health, family) (Rietzer 1944). Current studies support these claims and have established a significant correlation between uncertainty and fear in the case of COVID-19 (i.e., fear of COVID-19) and fear for one’s own and loved ones’ health (e.g., Mertens et al. 2020; Satici et al. 2020). For example, a cross-country level survey carried out in Turkey reported the mediating role of fear of COVID-19 in the relationship between intolerance of uncertainty and mental health (Satici et al. 2020). That is, intolerance of uncertainty can cause fear of COVID-19, which then might result in mental health issues. Therefore, it was hypothesized that intolerance of uncertainty would predict fear of COVID-19 (H2) and this fear would explain mental disorders (H3).
A review study reported that the most salient mental health problems as a consequence of the pandemic were depressive symptoms (Rajkumar 2020). In addition, it was found that fear of COVID-19 might trigger depressive symptoms and lead to depression (Egunjobi 2020). Previous research conducted in different contexts has also confirmed that depression is related to fear (Butzer and Kuiper 2006; de Jong-Meyer et al. 2009). Consequently, it was hypothesized that fear of COVID-19 would predict depression (H3). As discussed, fear may also induce stress (Nabi and Myrick 2018). Relatedly, theories of affect regulation dispute the notion that depressive symptoms change eating behavior as a way of regulating and reducing negative emotions (Macht 2008; Ouwens et al. 2009; Torrado et al. 2015). Furthermore, it is found that emotional eating is associated with depression and intolerance of uncertainty (Konttinen et al. 2010; Lazarevich et al. 2016; van de Poppe 2018; van Strien et al. 2016). Therefore, regarding the first three hypotheses of the present study and taking into account the extant research on emotional eating, a sequential mediation model was hypothesized in which the fear of COVID-19 and depression serially mediated the relationship between intolerance of uncertainty and emotional eating (H4) (see Fig. 1).
Fig. 1.
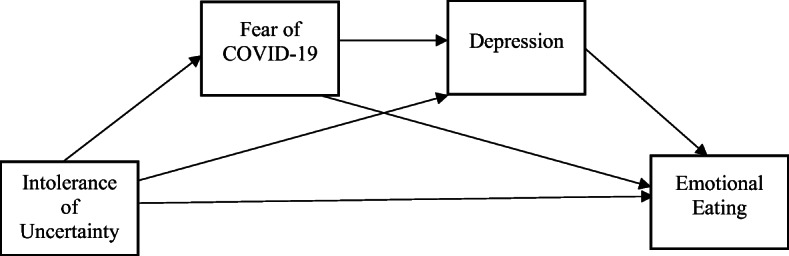
Proposed model: mediating roles of fear of COVID-19 and depression on the relationship between intolerance of uncertainty and emotional eating
Methods
Participants and Procedure
The cross-sectional data were collected from 362 participants (242 females, 116 males, and four other) living in the different cities of Turkey. Since the COVID-19 pandemic and lockdowns prevented in-person data collection, the participants of the study were recruited utilizing online survey software (i.e., Qualtrics) between April 15 and May 15, 2020. The present study obtained ethical approval from the research team’s university ethics committee (No. 84892257-604.01.02-E.15141) in accordance with the Helsinki declaration. After formulating the survey in the Turkish language, it was shared on different social media platforms including Facebook, Instagram, and WhatsApp. It was also shared with the Turkish students of a public university and two foundation universities via e-mail. Informed consent was obtained from all volunteering participants. The convenience sample comprised individuals whose ages ranged between 18 and 67 years (M = 26.89 years, SD = 8.22). Table 1 provides detailed information concerning the socio-demographics and COVID-19-related characteristics of the study participants.
Table 1.
Descriptive characteristics of the study sample
| Variables | n | % | Mean | SD | Range |
|---|---|---|---|---|---|
| Age | 362 | 26.89 | 8.22 | 18–67 | |
| Gender | |||||
| Female | 242 | 66.9 | |||
| Male | 116 | 32 | |||
| Other | 4 | 1.1 | |||
| Last completed degree | |||||
| Non-university graduates | 177 | 48.9 | |||
| Having bachelor’s degree | 124 | 34.3 | |||
| Having master/doctoral degree | 61 | 16.9 | |||
| Work status | |||||
| Full-time from work | 43 | 11.9 | |||
| Part-time from work | 44 | 12.2 | |||
| Full-time from home | 20 | 5.5 | |||
| Part-time from work | 29 | 8 | |||
| Not working | 226 | 62.4 | |||
| Diagnosis of mental illness | |||||
| Yes | 44 | 12.2 | |||
| No | 318 | 87.8 | |||
| Diagnosis of physical illness | 2 | 2.5 | |||
| Yes | 86 | 23.8 | |||
| No | 276 | 76.2 | |||
| Being in high-risk group for COVID-19 | |||||
| Yes | 33 | 9.1 | |||
| No | 314 | 86.7 | |||
| Not sure | 15 | 4.1 | |||
| Having high-risk family members for COVID-19 | |||||
| Yes | 259 | 71.5 | |||
| No | 85 | 23.5 | |||
| Not sure | 18 | 5 | |||
| The loss of a loved one due to COVID-19 | |||||
| Yes | 19 | 5.2 | |||
| No | 341 | 94.2 | |||
| Not knowing | 2 | 0.6 | |||
Measures
The online survey included a demographic information form, the Intolerance of Uncertainty Scale (IUS-12), Fear of COVID-19 Scale (FCV-19S), Hospital Anxiety and Depression Scale (HADS), and Three-Factor Eating Questionnaire-R21 (TFEQ-R21).
Demographic Information Form
This form included questions concerning participants’ age, gender, education level, work status, relationship status, and diagnosis history of mental and physical illness. It also contained questions in relation to the COVID-19 pandemic such as whether they were healthcare workers or not, whether they or their relatives were in a high-risk group (or not) for COVID-19 infection, and whether they knew someone who had died of COVID-19 or not during the pandemic.
The Intolerance of Uncertainty Scale
The short 12-item version of the IUS (Carleton et al. 2007; Turkish version: Saricam et al. 2014) was developed to assess intolerance of uncertainty. The Turkish version of the IUS (α = .88) is a two-factor scale that assesses prospective anxiety (α = .84) and inhibitory anxiety (α = .77). Each item (e.g., “I must get away from all uncertain situations”) is scored on a 5-point scale ranging from 1 (not at all characteristic of me) to 5 (entirely characteristic of me). Higher scores obtained from the scale indicate higher intolerance of uncertainty. In the present study, the scale’s internal reliability was excellent (α = .90).
The Fear of COVID-19 Scale
The FCV-19S is a seven-item unidimensional scale developed by Ahorsu et al. (2020) to assess the fear of COVID-19. Each item (e.g., “I am most afraid of coronavirus-19”) is scored on a 5-point scale ranging from 1 (strongly disagree) to 5 (strongly agree). Higher scores indicate higher levels of fear of COVID-19. The scale has been widely used to assess fear of COVID-19 and has been validated in different cultural contexts (e.g., Mahmood et al. 2020; Martinez-Lorca et al. 2020; Masuyama et al. 2020; Perz et al. 2020). Although the scale has since been validated in Turkish, there was no Turkish version of this scale when the data were collected. Therefore, a Turkish version of FCV-19S was developed for the present study. The scale was translated into Turkish by three researchers using the translation-back-translation method (Brislin et al. 1973). Given that the original seven-item factor structure of the FCV-19S was identified as unidimensional using exploratory factor analysis (Ahorsu et al. 2020), in the present study, confirmatory factor analysis (CFA) was carried out. The results showed that the one-factor solution had good fit to the data (𝜒2[10] = 25.52, 𝜒2/df = 2.55, p < .01, RMSEA = .07, GFI = .98, CFI = .98, TLI = .97). Moreover, its correlations with other constructs were examined to assess the concurrent validity of the FCV-19S. In the present study, the FCV-19S also showed very good internal consistency (α = .87) and test-retest reliability (α = .79).
The Hospital Anxiety and Depression Scale
The HADS was developed by Zigmond and Snaith (1983); Turkish version: Aydemir et al. 1997) to assess the levels of depression and anxiety. The Turkish form of HADS comprises 14 items with two sub-dimensions: depression (seven items, α = .78) and anxiety (seven items, α = .85). For the present study, only the depression subscale of the HADS was used. Each item (e.g., “I feel as if I am slowed down”) is scored on a 4-point scale which have different range categories. For example, the item above is scored on a 4-point scale ranging from 1 (definitely as much) to 4 (hardly at all). Higher scores indicate a higher level of depression. In the present study, the scale’s internal reliability was low (α = .61) but acceptable (see Robinson et al. 1991).
The Three-Factor Eating Questionnaire-R21
The TFEQ-R21 was developed by Stunkard and Messick (1985) and revised by Cappelleri et al. (2009); Turkish version: Karakus et al. 2016). The Turkish version of TFEQ-R21 comprises 21 items assessing three domains of eating behavior: cognitive restraint (CR, α = .80), uncontrolled eating (UE, α = .79), and emotional eating (EE, α = .87). For the present study, only the EE subscale with six items was used. Each item (e.g., “When I feel depressed, I want to eat”) is scored on a 4-point scale ranging from 1 (definitely false) to 4 (definitely true). Higher scores indicate eating greater emotional eating. In the present study, the scale’s internal reliability was excellent (α = .95).
Statistical Analyses
Statistical analyses were performed in two phases: (i) descriptive statistics and (ii) hypothesis testing. Descriptive statistical analyses included means, standard deviations, ranges, percentages, t and F tests for means and variances, and correlational analyses. For hypothesis testing, path analysis with maximum likelihood method was conducted using IBM AMOS 24.0 (Arbuckle 2009). Power analysis was run using a priori sample size calculator for structural equation models (Soper 2020). To estimate the indirect effects of mediational variables for the proposed model, a bias-corrected bootstrapping method with 5000 resamples and 95% confidence interval was used. In the light of the suggested cut-off points for the fit indices before, particular fit indexes were used: root mean square of error of approximation (RMSEA), Bentler Comparative Fit Index (CFI), Tucker-Lewis index (TLI), and standardized root mean square residual (SRMR), with model Chi-square (𝜒2) and Chi-square/degrees of freedom ratio (𝜒2/df-ratio) values to interpret the results of model testing. Chi-square/df-ratio was suggested by Wheaton et al. (1977) to be less than 5, when the sample size is small. Browne and Cudeck (1993) suggested a cut-off for RMSEA < .05 referring to a good fit, and RMSEA < .08 referring to a reasonable fit. GFI, AGFI, CFI, and TLI values range from 0 to 1, and .95 represents a perfect fit, while .90 is an acceptable fit for these indices (Kline 2005).
Results
Descriptive Statistics
Means, standard deviations of the scores, and the correlation matrix for the variables of the study’s mediation model are provided in Table 2. Intolerance of uncertainty had positive association with fear of COVID-19 (r = .27, p < .01), depression (r = .18, p < .01), and emotional eating (r = .17, p < .01). Fear of COVID-19 had positive correlation with depression (r = .28, p < .01) and emotional eating (r = .15, p < .01). In addition, depression and emotional eating were positively associated (r = .20, p < .01).
Table 2.
Descriptive statistics and intercorrelations of the study variables (N = 362)
| Mean | SD | 1 | 2 | 3 | 4 | |
|---|---|---|---|---|---|---|
| 1. Intolerance of Uncertainty | 39.14 | 9.31 | – | |||
| 2. Fear of COVID-19 | 17.01 | 5.68 | .27** | – | ||
| 3. Depression | 10.05 | 2.94 | .18** | .28** | – | |
| 4. Emotional Eating | 12.99 | 5.21 | .17** | .15** | .20** | – |
p < .01**
To investigate the relationship between demographic variables (i.e., age, gender, education, relationship status, and work status) and model variables (i.e., emotional eating, depression, fear of COVID-19, and intolerance of uncertainty), independent samples t-tests, analyses of variance (ANOVAs), and Pearson correlations were performed. The results showed that age had a significant negative relationship with intolerance of uncertainty (r = −.15, p < .01). Moreover, compared to males (MEE = 11.51, SDEE = 5.17; MFCV = 14.61, SDFCV = 5.07), females (MEE = 13.71, SDEE = 5.11; MFCV = 18.17, SDFCV = 5.58) reported significantly higher levels of emotional eating (t[356] = 3.811, p < .01) and fear of COVID-19 (t[356] = 5.819, p < .01). However, no significant differences for emotional eating, depression, fear of COVID-19, and intolerance of uncertainty were found across the groups with regard to education, relationship status, or work status.
Hypotheses Testing
After the correction for the non-significant relationship between fear of COVID-19 and emotional eating based on modification indices, the findings showed that the modified proposed model perfectly fitted the data (𝜒2(1) = 1.731, 𝜒2/df = 1.731, p = .188, RMSEA = .045, GFI = .998, CFI = .991, TLI = .945) (see Table 2). Moreover, given the emotional eating theories stressing the bidirectional effects between eating behaviors and emotions and the explorative nature of the present study, the model was also run inversely. However, although the model indexes were acceptable, they were not perfect (𝜒2(2) = 6.43, 𝜒2/df = 3.22, p < .05, RMSEA = .078, GFI = .991, CFI = .994, TLI = .832) (see Table 3).
Table 3.
Summary of the model fit indices for the proposed model
| χ2 | df | p | RMSEA | GFI | CFI | TLI | |
|---|---|---|---|---|---|---|---|
| Model | 1.731 | 1 | .188 | .045 | .998 | .991 | .945 |
Standardized regression estimates of the tested model are shown in Fig. 2 with lines indicating the significant paths and dashed lines indicating the non-significant paths. Firstly, H1 was that intolerance of uncertainty would be associated with fear of COVID-19. This hypothesis was supported because intolerance of uncertainty had a positive significant direct effect on fear of COVID-19 (β = .27, p < .001). H2 was that fear of COVID-19 would be associated with depression. This hypothesis was supported. Fear of COVID-19 positively predicted depression (β = .25, p < .001). Moreover, it was found that intolerance of uncertainty positively and directly predicted depression (β = .11, p < .05). H3 was that depression would be associated with emotional eating. This hypothesis was supported. The findings showed that depression positively predicted emotional eating (β = .18, p < .001). However, there was no significant association between fear of COVID-19 and emotional eating (β = .07, p = .18). Additionally, intolerance of uncertainty positively and directly predicted emotional eating (β = .13, p < .05). The total and direct effects of the proposed model are summarized in Table 4.
Fig. 2.
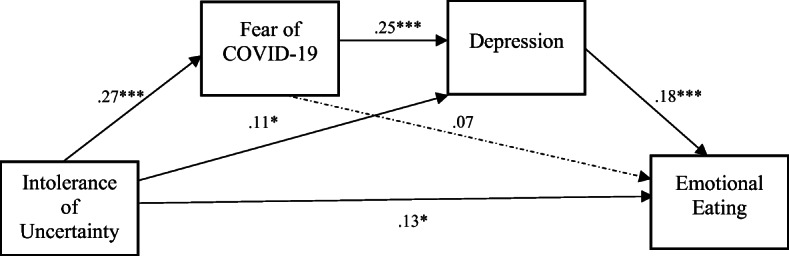
Standardized parameter estimates for proposed model: mediating roles of fear of COVID-19 and depression on the relationship between intolerance of uncertainty and emotional eating
Table 4.
Summary of the total and direct effects for the proposed model
| Pathways | Total | Direct | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β | SE | Lower | Upper | p | β | SE | Lower | Upper | p | |
| IU ➔ FCV-19 | .27 | .06 | .183 | .362 | .001 | .27 | .03 | .183 | .362 | .000 |
| FCV-19➔ depression | .25 | .06 | .160 | .344 | .001 | .25 | .03 | .160 | .344 | .000 |
| IU ➔ depression | .18 | .05 | .086 | .267 | .001 | .11 | .02 | .008 | .201 | .035 |
| Depression ➔ EE | .18 | .05 | .090 | .269 | .002 | .18 | .09 | .090 | .269 | .000 |
| IU ➔ EE | .17 | .05 | .076 | .252 | .001 | .13 | .03 | .038 | .223 | .010 |
| FCV-19➔ EE | .04 | .02 | .021 | .081 | .002 | – | – | – | – | – |
IU intolerance of uncertainty, FCV-19 fear of COVID-19, EE emotional eating
As expected, intolerance of uncertainty had significant positive total indirect effect on emotional eating (β = .03, p < .001). Also, each specific indirect effect was calculated using AMOS 24.0 serial mediation plugin (Gaskin et al. 2020). Firstly, intolerance of uncertainty was positively and indirectly associated with depression via fear of COVID-19 (β = .07, p < .001). Secondly, the results showed that intolerance of uncertainty had a significant positive indirect effect on emotional eating via depression (β = .02, p < .05). Thirdly, the results showed that depression mediated the relationship between fear of COVID-19 and emotional eating (β = .04, p < .001). Finally, the serial mediating roles of fear of COVID-19 and depression in the relationship between intolerance of uncertainty and emotional eating was also confirmed (therefore supporting H4). Fear of COVID-19 and depression sequentially mediated the relationship between intolerance of uncertainty and emotional eating (β = .07, p < .001). The indirect effects of the proposed model are summarized in Table 5.
Table 5.
Summary of the specific indirect effects for the proposed model
| Pathways | β | SE | Lower | Upper | p |
|---|---|---|---|---|---|
| IU ➔ FCV-19 ➔ depression | .07 | .02 | .012 | .035 | .001 |
| IU ➔ depression ➔ EE | .02 | .01 | .002 | .026 | .043 |
| FCV-19 ➔ depression ➔ EE | .04 | .02 | .020 | .074 | .001 |
| IU ➔ FCV-19 ➔ depression ➔ EE | .07 | .01 | .003 | .014 | .001 |
IU intolerance of uncertainty, FCV-19 fear of COVID-19, EE emotional eating
Discussion
The objective of present research was to test a sequential mediation model to explain to what extent stress-induced factors during the COVID-19 pandemic might lead to developing maladaptive behaviors. More specifically, regarding the pandemic as a natural experiment, the present study focused on fear and depression that individuals frequently have experienced in this specific time in order to identify some of the underlying mechanisms between their levels of intolerance of uncertainty and emotional eating. Relatedly, the present study tested the hypotheses with respect to the associations between intolerance of uncertainty, the fear of COVID-19, depression, and emotional eating and analyzed a sequential mediation model by fully testing these associations together.
The results of the present study showed that when intolerance of uncertainty of the participants increased, their fear of COVID-19 also increased. This result confirmed a previous finding in the literature (Satici et al. 2020). Moreover, increased intolerance of uncertainty was associated with increased levels of depression in the present study. Also, mediation analysis found that intolerance of uncertainty exerted a significant indirect effect on depression via fear of COVID-19. Similarly, Taha et al. (2014) found that individuals with a high intolerance of uncertainty were more likely to perceive a pandemic as threatening and that individuals had increased levels of anxiety. This result may be explained by the insufficient governmental support and policies in Turkey. After the head of the Turkish Ministry of Health announced the first confirmed cases in the country, the information about the locations of such cases was not provided. Also, some immediate problems including the government’s lack of financial support and obtaining masks for public went unresolved during the initial period of the pandemic in Turkey. More accurate information provided by the Turkish government might have decreased perceived threat and anxiety (Taha et al. 2014).
Furthermore, the results demonstrated that while depression positively predicted emotional eating, fear of COVID-19 did not have any direct effect on emotional eating. Some studies (e.g., Goossens et al. 2009; Ouwens et al. 2009) have shown that increased levels of depression have been associated with an increase in emotional eating. Although fear is also one of negative emotions, the scale’s questions in the present study specifically concerned the COVID-19 pandemic (e.g., “I am most afraid of coronavirus-19”, “I cannot sleep because I’m worrying about getting coronavirus-19”). Therefore, the finding of depression as a mediator between fear of COVID-19 and emotional eating appears to be reasonable. Moreover, mediation analysis showed that individuals who had higher intolerance of uncertainty showed more depressive symptoms, which in turn was associated with greater emotional eating.
The study’s main hypothesis was supported as results suggested that intolerance of uncertainty led to higher fear of COVID-19, which in turn increased the level of depressive symptoms, and elevated depressive symptoms increased emotional eating. As discussed, previous literature has shown associations between intolerance of uncertainty and emotional eating and between intolerance of uncertainty and disordered eating (e.g., Renjan et al. 2016; Sternheim et al. 2011). Emotional eating theory (Macht and Simons 2011) proposed that emotional eaters try to manage their moods by overeating in response to negative affect because of its negative reinforcement effect. It has also been found that overeating lifts individuals out of their negative mood states (Spoor et al. 2007). In addition, self-threatening negative affect and high aversive self-awareness can lead to overeating among emotional eaters (Wallis and Hetherington 2004). As with the nature of all pandemics, the COVID-19 pandemic has brought about uncertainty over many things including health and finances and has led to negative emotions in many individuals’ lives. Individuals in many countries have also been requested to stay at home in self-quarantine. Consequently, to cope with the negative effects of these new living conditions, participants may have fed their emotions by eating more than was needed.
Regarding demographic factors, it was found that gender had a significant association with emotional eating and fear of COVID-19 whereas age was negatively associated with intolerance of uncertainty. More specifically, females were found to have significantly higher levels of emotional eating, which is in line with the findings of previous empirical studies (e.g., Larsen et al. 2006). It was also found that females reported higher levels of fear of COVID-19, which has also been found in other recent studies (e.g., Broche-Perez et al. 2020; Hossain et al. 2020; Sakib et al. 2020). Therefore, it appears that the COVID-19 pandemic has emotionally affected females more negatively than males. Additionally, the present study also found a significant (albeit small) negative correlation between age and intolerance of uncertainty. More specifically, younger participants reported higher levels of intolerance of uncertainty which has also been reported in previous studies (e.g., Bottesi et al. 2019). They discussed this finding from a developmental perspective and argued that older people better cope with intolerance than young people because of their longer life experience.
Strengths, Limitations, and Future Research
The present study is significant because it is one of the few studies advancing emotional eating theories by investigating intolerance of uncertainty, fear, and depression as the underlying mechanisms, and the associations between them. Also, it established the extent to which stress-related factors due to a pandemic change the eating patterns among individuals. Therefore, the study highlighted the complex relationship between the pandemic and human psychology comprising cognitive (i.e., intolerance of uncertainty), affective (i.e., fear and depression), and behavioral (i.e., eating) components. However, this study has some limitations, and the findings should be interpreted with some caution. First, the study sample comprised more females (many of who were non-working) with a mean age of 27 years. Therefore, the findings cannot be generalized to the entire Turkish population. Consequently, replicating the study in other cities of Turkey and cultures will strengthen the cross-country and cultural validity of the model. Second, the data (i.e., feelings, thoughts, behaviors, affective states [fear, depression], and behaviors [emotional eating]) were assessed in the present study at the peak of the pandemic using a cross-sectional survey, which makes it difficult to draw causal inferences, and directions between the variables and findings may have been different if the data were collected at other stages during the pandemic. Future studies using a longitudinal design are thus highly recommended to monitor and identify the long-term effects of intolerance to the uncertainty of the COVID-19 pandemic among individuals. Also, government interventions and restrictions such as social isolation and lockdowns might be a risk for healthy groups to develop eating disorders and affect individuals suffering from such disorders (Weissman et al. 2020). The study’s model was tested among a non-clinical sample and so studies focusing on the relationship between affective states and eating patterns among clinical samples of eating disorder patients during the pandemic are also needed.
Conclusions and Clinical Implications
This study provided evidence that individuals tend to eat more than usual depending on how much they find uncertain situations as uncomfortable and may feel fearful and/or depressed due to COVID-19. Moreover, the present study found that females were more prone to emotional eating than males. Consequently, it is recommended that practitioners should focus on and encourage their clients to explore causal and contributing factors underlying their cognitions and emotions as well as their eating behaviors. It is also important that government and health agencies should develop appropriate psychoeducational materials informing the general public about the pandemic-related cognitions and emotions. This may help individuals, particularly women, to normalize what they thought and felt during this time and cope with such states effectively. Finally, the Turkish government should impose some restrictions and/or develop guidelines for the content of the pandemic-related news because mass media news concerning uncertainty and negative consequences of the pandemic (e.g., suicides and scenes from intensive care units) may increase fear and trigger depressive symptoms among some individuals.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Halil Pak, Email: halil.pak@outlook.com.
Yankı Süsen, Email: ysusen@ybu.edu.tr.
Merve Denizci Nazlıgül, Email: merve.denizci@yeditepe.edu.tr.
Mark Griffiths, Email: mark.griffiths@ntu.ac.uk.
References
- Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed]
- Arbuckle JL. Amos 18.0 [computer software] Chicago, IL: Small Waters; 2009. [Google Scholar]
- Auer, M., Malischnig, D., & Griffiths, M. D. (2020). Gambling before and during the COVID-19 pandemic among European regular sports bettors: An empirical study using behavioral tracking data. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00327-. [DOI] [PMC free article] [PubMed]
- Aydemir Ö, Güvenir T, Küey L, Kültür S. Reliability and validity of the Turkish version of hospital anxiety and depression scale. Turkish Journal of Psychiatry. 1997;8(4):280–287. [Google Scholar]
- Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. The Lancet. 2020;395(10224):37–38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottesi G, Noventa S, Freeston MH, Ghisi M. Seeking certainty about intolerance of uncertainty: addressing old and new issues through the intolerance of uncertainty scale-revised. PLoS One. 2019;14(2):e0211929. doi: 10.1371/journal.pone.0211929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brislin RW, Lonner WJ, Thorndike RM. Cross-cultural research methods. Chichester, UK: Wiley; 1973. [Google Scholar]
- Broche-Perez, Y., Fernandez-Fleite, Z., Jimenez-Puig, E., Fernandez-Castillo, E., & Rodriguez-Martin, B. C. (2020). Gender and fear of COVID-19 in a Cuban population sample. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00343-8. [DOI] [PMC free article] [PubMed]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Butzer B, Kuiper NA. Relationships between the frequency of social comparisons and self-concept clarity, intolerance of uncertainty, anxiety, and depression. Personality and Individual Differences. 2006;41(1):167–176. doi: 10.1016/j.paid.2005.12.017. [DOI] [Google Scholar]
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cappelleri JC, Bushmakin AG, Gerber RA, Leidy NK, Sexton CC, Lowe, M. R. … Karlsson, J. Psychometric analysis of the three-factor eating questionnaire-R21: results from a large diverse sample of obese and non-obese participants. International Journal of Obesity. 2009;33(6):611–620. doi: 10.1038/ijo.2009.74. [DOI] [PubMed] [Google Scholar]
- Carleton RN, Norton MPJ, Asmundson GJ. Fearing the unknown: a short version of the intolerance of uncertainty scale. Journal of Anxiety Disorders. 2007;21(1):105–117. doi: 10.1016/j.janxdis.2006.03.014. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Mental health and coping during COVID-19. Retrieved June 11, 2020, from: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html
- Coker, E. D. (2020). The coronavirus pandemic and public opinion research – highlights from the fourth week. Retrieved June 11, 2020, from: https://www.ipsos.com/tr-tr/koronavirus-salgini-ve-toplum-arastirmasi-4-donemden-one-cikanlar
- de Jong-Meyer R, Beck B, Riede K. Relationships between rumination, worry, intolerance of uncertainty and metacognitive beliefs. Personality and Individual Differences. 2009;46(4):547–551. doi: 10.1016/j.paid.2008.12.010. [DOI] [Google Scholar]
- Egunjobi, J. P. (2020). The perception of Covid-19 as a fear factor in the preparation for the pandemic aftermath. ResearchGate. 10.13140/RG.2.2.14933.17125.
- Gaskin J, James M, Lim J. AMOS plugin. Gaskination's StatWiki. 2020. Indirect effects. [Google Scholar]
- Goossens L, Braet C, Van Vlierberghe L, Mels S. Loss of control over eating in overweight youngsters: the role of anxiety, depression and emotional eating. European Eating Disorders Review. 2009;17(1):68–78. doi: 10.1002/erv.892. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hofstede G, Hofstede GJ. Cultures and organizations: software of the mind. New York: McGraw-Hill; 2005. [Google Scholar]
- Hossain MA, Jahid MIK, Hossain KMA, Walton LM, Uddin Z, Haque MO, Kabir MF, Arafat SMY, Sakel M, Faruqui R, Hossain Z. Knowledge, attitudes, and fear of COVID-19 during the rapid rise period in Bangladesh. PLoS One. 2020;15(9):e0239646. doi: 10.1371/journal.pone.0239646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karakus S, Yildırim H, Buyukozturk S. Adaptation of three factor eating questionnaire (TFEQ-R21) into Turkish culture: a validity and reliability study. TAF Preventive Medicine Bulletin. 2016;15(3):229. doi: 10.5455/pmb.1-1446540396. [DOI] [Google Scholar]
- Kavoor AR. COVID-19 in people with mental health illness: challenges and vulnerabilities. Asian Journal of Psychiatry. 2020;51:102051. doi: 10.1016/j.ajp.2020.102051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: The Guilford Press; 2005. [Google Scholar]
- Konttinen H, Mannistö S, Sarlio-Lahteenkorva S, Silventoinen K, Haukkala A. Emotional eating, depressive symptoms and self-reported food consumption. A population-based study. Appetite. 2010;54(3):473–479. doi: 10.1016/j.appet.2010.01.014. [DOI] [PubMed] [Google Scholar]
- Larsen JK, van Strien T, Eisinga R, Engels RCME. Gender differences in the association between alexithymia and emotional eating in obese individuals. Journal of Psychosomatic Research. 2006;60(3):237–243. doi: 10.1016/j.jpsychores.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Lazarevich I, Camacho MEI, Velázquez-Alva MC, Zepeda MZ. Relationship among obesity, depression, and emotional eating in young adults. Appetite. 2016;107:639–644. doi: 10.1016/j.appet.2016.09.011. [DOI] [PubMed] [Google Scholar]
- Li S, Wang Y, Xue J, Zhao N, Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. International Journal of Environmental Research and Public Health. 2020;17(6):2032. doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang, T. (2020). Handbook of COVID-19 prevention and treatment. Retrieved November 29, 2020, from: https://esge.org/documents/Handbook_of_COVID-19_Prevention_and_Treatment.pdf
- Macht M. How emotions affect eating: a five-way model. Appetite. 2008;50(1):1–11. doi: 10.1016/j.appet.2007.07.002. [DOI] [PubMed] [Google Scholar]
- Macht, M., & Simons, G. (2011). Emotional eating. In I. Nyklíček, A. Vingerhoets, & M. Zeelenberg (Eds.), Emotion regulation and well-being. Springer. 10.1007/978-1-4419-6953-8_17.
- Mahmood, Q. K., Jafree, S. R., & Qureshi, W. A. (2020). The psychometric validation of FCV19S in Urdu and socio-demographic association with fear in the people of the Khyber Pakhtunkhwa (KPK) province in Pakistan. International Journal of Mental Health and Addiction. Advanced online publication.10.1007/s11469-020-00371-4. [DOI] [PMC free article] [PubMed]
- Martinez-Lorca M, Martinez-Lorca A, Criado-Alvarez JJ, Armesilla MDC, Lattore JM. The fear of COVID-19 scale: validation in Spanish university students. Psychiatry Research. 2020;293:11350. doi: 10.1016/j.psychres.2020.113350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuyama, A., Schinkawa, H., & Kubo, T. (2020). Validation and psychometric properties of the Japanese version of the fear of COVID-19 scale among adolescents. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00368-z. [DOI] [PMC free article] [PubMed]
- Mertens, G., Gerritsen, L., Salemink, E., & Engelhard, I. (2020). Fear of the coronavirus (COVID-19): predictors in an online study conducted in March 2020. PsyArXiv. 10.31234/osf.io/2p57j. [DOI] [PMC free article] [PubMed]
- Morgul, E., Bener, A., Atak, M., Akyer, S., Aktas, S., Bhugra, D., Ventriglio, A., & Jordan, T. M. (2020). COVID-19 pandemic and psychological fatigue in Turkey. International Journal of Social Psychiatry. Advanced online publication. 10.1177%2F0020764020941889. [DOI] [PMC free article] [PubMed]
- Muhlheim L. Verywell Mind. 2020. Eating disorders during the coronavirus (COVID-19) pandemic. [Google Scholar]
- Nabi RL, Myrick JG. Uplifting fear appeals: considering the role of hope in fear-based persuasive messages. Health Communication. 2018;34(4):463–474. doi: 10.1080/10410236.2017.1422847. [DOI] [PubMed] [Google Scholar]
- Ouwens MA, van Strien T, van Leeuwe JFJ. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite. 2009;53(2):245–248. doi: 10.1016/j.appet.2009.06.001. [DOI] [PubMed] [Google Scholar]
- Pakpour AH, Griffiths MD. The fear of COVID-19 and its role in preventive behaviors. Journal of Concurrent Disorders. 2020;2(1):58–63. doi: 10.54127/WCIC8036. [DOI] [Google Scholar]
- Perz, C. A., Lang, B. A., & Harrington, R. (2020). Validation of the fear of COVID-19 scale in a US college sample. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00356-3. [DOI] [PMC free article] [PubMed]
- Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian Journal of Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renjan V, McEvoy PM, Handley AK, Fursland A. Stomaching uncertainty: relationships among intolerance of uncertainty, eating disorder pathology, and comorbid emotional symptoms. Journal of Anxiety Disorders. 2016;41:88–95. doi: 10.1016/j.janxdis.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Rietzer K. The social psychology of fear. American Journal of Sociology. 1944;49(6):489–498. doi: 10.1086/219471. [DOI] [Google Scholar]
- Ro, C. (2020). Coronavirus: how to avoid overeating when working from home. BBC, April 1. Retrieved November 29, 2020, from: https://www.bbc.com/worklife/article/20200331-how-to-eat-a-healthy-diet-when-work-from-home-coronavirus
- Robinson JP, Shaver PR, Wrightsman LS. Criteria for scale selection and evaluation. In: Robinson JP, Shaver PR, Wrightsman LS, editors. Measures of personality and social psychological attitudes. San Diego, CA: Academic Press; 1991. pp. 1–16. [Google Scholar]
- Sakib, N., Bhuiyan, A. I., Hossain, S., Al Mamun, F., Hosen, I., Abdullah, A. H., et al. (2020). Psychometric validation of the Bangla fear of COVID-19 scale: confirmatory factor analysis and Rasch analysis. International Journal of Mental Health and Addiction. Advance online publication.10.1007/s11469-020-00289-x. [DOI] [PMC free article] [PubMed]
- Saricam H, Erguvan FM, Akin A, Akca MŞ. The Turkish short version of the intolerance of uncertainty (IUS-12) scale: the study of validity and reliability. Route Educational and Social Science Journal. 2014;1(3):148–157. doi: 10.17121/ressjournal.109. [DOI] [Google Scholar]
- Satici, B., Saricali, M., Satici, S. A., & Griffiths, M. D. (2020). Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Advance online publication. International Journal of Mental Health and Addiction.10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed]
- Simione, L., & Gnagnarella, C. (2020). Differences between health workers and general population in risk perception, behaviors, and psychological distress related to COVID-19 spread in Italy. PsyArXiv. 10.31234/osf.io/84d2c. [DOI] [PMC free article] [PubMed]
- Soper, D. (2020). A-priori sample size calculator for structural equation models. Retrieved from https://www.danielsoper.com/statcalc/calculator.aspx?id=89
- Spoor ST, Bekker MH, Van Strien T, van Heck GL. Relations between negative affect, coping, and emotional eating. Appetite. 2007;48(3):368–376. doi: 10.1016/j.appet.2006.10.005. [DOI] [PubMed] [Google Scholar]
- Sternheim L, Startup H, Schmidt U. An experimental exploration of behavioral and cognitive–emotional aspects of intolerance of uncertainty in eating disorder patients. Journal of Anxiety Disorders. 2011;25(6):806–812. doi: 10.1016/j.janxdis.2011.03.020. [DOI] [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29(1):71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: The case of the 2009 H1N1 pandemic. British Journal of Health Psychology. 2014;19(3):592–605. doi: 10.1111/bjhp.12058. [DOI] [PubMed] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia J, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. Advance online publication. 2020;66:317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- Torrado YP, Velasco AGV, Galiot AH, Cambrodon IG. A strategy for weight loss based on healthy dietary habits and control of emotional response to food. Nutricion Hospitalaria. 2015;31(6):2392–2399. doi: 10.3305/nh.2015.31.6.8736. [DOI] [PubMed] [Google Scholar]
- Turkish Ministry of Health. (2020). The guideline of COVID-19. Retrieved November 29, 2020, from: https://covid19bilgi.saglik.gov.tr/depo/rehberler/COVID-19_Rehberi.pdf
- van de Poppe, R. V. (2018). The inhibitory effect of intolerance of uncertainty on the emotional eating response. Master’s thesis, Universiteit Utrecht, Utrecht, The Netherlands. Retrieved from https://dspace.library.uu.nl/handle/1874/367030
- van Strien T, Konttinen H, Homberg JR, Engels RCME, Winkens LHH. Emotional eating as a mediator between depression and weight gain. Appetite. 2016;100(1):216–224. doi: 10.1016/j.appet.2016.02.034. [DOI] [PubMed] [Google Scholar]
- Wallis DJ, Hetherington MM. Stress and eating: the effects of ego-threat and cognitive demand on food intake in restrained and emotional eaters. Appetite. 2004;43:39–46. doi: 10.1016/j.appet.2004.02.001. [DOI] [PubMed] [Google Scholar]
- Wang, Y., Di, Y., Ye, J., & Wei, W. (2020). Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychology, Health & Medicine. Advance online publication. 10.1080/13548506.2020.1746817. [DOI] [PubMed]
- Warren, C. S. (2020). How to curb emotional eating during the COVID-19 pandemic. Psychology today. Retrieved November 29, 2020, from: https://www.psychologytoday.com/us/blog/naked-truth/202003/how-curb-emotional-eating-during-the-covid-19-pandemic
- Weissman RS, Bauer S, Thomas JJ. Access to evidence-based care for eating disorders during the COVID-19 crisis. International Journal of Eating Disorders. 2020;53(5):369–376. doi: 10.1002/eat.23279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton B, Muthen B, Alwin DF, Summers G. Assessing reliability and stability in panel models. Sociological Methodology. 1977;8(1):84–136. doi: 10.2307/270754. [DOI] [Google Scholar]
- Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Education & Behavior. 2000;27(5):591–615. doi: 10.1177/2F109019810002700506. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020a). WHO Director-General's opening remarks at the media briefing on COVID-19, 11 March 2020. Retrieved November 29, 2020, from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19%2D%2D-11-march-2020
- World Health Organization. (2020b). Weekly operational update on COVID-19. Retrieved November 29, 2020, from: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19%2D%2D-20-november-2020
- Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, Ng CH. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020;7(3):228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H, Chen JH, Xu YF. Patients with mental health disorders in the COVID-19 epidemic. The Lancet Psychiatry. 2020;7(4):e21. doi: 10.1016/S2215-0366(20)30090-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A, Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian Journal of Psychiatry. 2020;51:101990. doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]


