Abstract
This study examined the between-person associations of seven health behaviors in adults with obesity participating in a weight loss intervention, as well as the covariations between these behaviors within-individuals across the intervention. The present study included data from a 12-month weight loss trial (N = 278). Seven health behaviors (physical activity, sedentary behavior, sleep duration, and consumption of fruits, vegetables, total fat and added sugar) were measured at baseline, 6- and 12-months. Between- and within-participants network analyses were conducted to examine how these behaviors were associated through the 12-month intervention and covaried across months. At the between-participants level, associations were found within the different diet behaviors and between total fat and sedentary behaviors. At the within-participants level, covariations were found between sedentary and diet behaviors, and within diet behaviors. Findings suggest that successful multiple health behaviors change interventions among adults with obesity will need to (1) simultaneously target sedentary and diet behaviors; and (2) prevent potential compensatory behaviors in the diet domain.
Keywords: Multiple health behavior change, Weight loss, Obesity, Network analyses
Introduction
Health behavior change is a key component of weight management strategies in overweight and obese adults (Dombrowski et al., 2010). Improving physical activity, diet, and sleep behaviors reduces weight and improves overall health among adults with obesity (Jensen et al., 2014). However, it is unclear whether interventions should target these behaviors individually or together in some combinations, and if the latter, which combinations actually promote successful behavior change (Prochaska et al., 2010; Geller et al., 2017).
Diet and physical activity are commonly targeted simultaneously in weight loss interventions and are typically assumed to be independent behaviors. However, they may interact with one another in synergistic or antagonistic ways (Prochaska et al., 2010; Geller et al., 2017). Multiple health behavior change interventions explicitly seek to leverage the potential positive interactive effects, while minimizing the deleterious ones (Spring et al., 2012; King et al., 2013). The multiple health behavior approach assumes that behaviors are inter-related and covary over time (Prochaska et al., 2010). More specifically, health behaviors are assumed to be inter-related in both health-enhancing (e.g., physical activity and vegetables consumption) and health-reducing (e.g., sedentary behavior and sugar consumption) ways (Boudreaux et al., 2003; de Vries et al., 2008; Lippke et al., 2012; Fleary & Nigg, 2019).
While associations between behaviors have been demonstrated in cross sectional studies, the covariance of health behaviors over time has received less attention, in particular whether changes in one behavior are associated with changes in other behaviors (Rosenberg et al., 2007; Spring et al., 2012). Moreover, recent research has shown that associations of health behaviors observed between-individuals differs significantly from those seen within-individuals (Conroy et al., 2015). For example, while some health behaviors have been consistently found to be positively correlated cross-sectionally (e.g. physical activity and fruit consumption; de Vries et al., 2008; Fleary & Nigg, 2019) both observational and interventional studies have shown different patterns of change in health behaviors over time. Improvements in diet have been more closely tied to reductions in sedentary behavior than increases in physical activity (Rosenberg et al., 2007; Spring et al., 2012).
Gaining a better understanding of how health behaviors covary between and within individuals could inform how health behaviors should be targeted in multiple health behaviors intervention among overweight and obese adults. However, to our knowledge, there has yet to be a study that explored and compared the associations between multiple health behaviors at the between- and within-individuals levels among overweight and obese adults participating to a weight loss intervention (Geller et al., 2017). Therefore, the primary objective of this study was to examine the between-person patterns of associations between seven self-reported health behaviors (physical activity, sleep duration, sedentary behavior, as well as added sugar, total fat, vegetables and fruits consumption) measured over 1 year among overweight and obese adults who participated in a weight loss intervention. The second objective was to assess how these behaviors covary within-individuals across the intervention. The distinction between these two-levels of analysis is crucial since results obtained at the between- and within-individual levels might not be equivalent (see Fisher et al., 2018), as confirmed in the multiple health behavior change literature (e.g., Conroy et al., 2015). Furthermore, if the objective is to build more effective multiple health behavior change interventions, the results obtained at the within-participant level should be more informative as they represent dynamical processes (i.e., co-variations), and thus, contrast with the between-participant analyses that represent average associations over time.
Unique to our study, we analyzed these behavioral associations using network analyses. Compared to cluster analyses and mixed-model analyses, this statistical approach offers a unique ability to efficiently visualize, understand, and compare the associations and covariations between behaviors (Costantini et al., 2019; Heino et al., 2019; Mkhitaryan et al., 2019). Our hypothesis was that, as in the study described above, we would see different patterns of associations in the between-participant and within-participant analyses.
Methods
Study design and participants
The present study analyzed data from a 12-month weight-loss intervention (CTRN: NCT01171586) among overweight and obese English- and Spanish-speaking adults (see Godino et al., 2019). Potential participants were screened via telephone for meeting the following inclusion criteria: 21–60 years old, overweight (BMI 27.0–39.9 kg/m2), owner of a cell phone capable of sending and receiving SMS, and residency in San Diego County. Exclusion criteria included experiencing pulmonary, cardiovascular, or musculoskeletal problems that would limit the ability to comply with study protocols; using medications that altered weight; having a history of eating disorders, weight loss surgery, substance abuse, or psychiatric disorders; being a smoker or recently quitting smoking; participating in another weight loss program; living with someone enrolled in the study; and being pregnant or intending to become pregnant (see for further details: Godino et al., 2019).
Participants were randomized to either a short message service (SMS)-only weight loss intervention, SMS plus brief monthly counseling calls from a health coach, or control, receiving only print-based weight loss materials. Those randomized to the SMS intervention received content to promote physical activity, reduce sedentary behavior, get the recommended hours of sleep per night, and increase consumption of fruits and vegetables, and reduce total fat and added sugar. The content consisted of approximately 2100 English or Spanish SMS that were delivered 2–4 times daily and were developed based on the Strategies for Weight Management (SWM) Inventory, which contains behavioral strategies focusing on reducing energy intake and increasing energy expenditure in overweight and obese adults (Kolodziejczyk et al., 2015). Programming logic for SMS was developed to maximize participant preferences for content and recognize progress toward mastering the adoption of behaviors in the SWM (for a detailed description of the algorithm, see Godino et al., 2019). In addition to the SMS intervention, one group of participants received two brief (5–10 min) counseling calls from a health coach in the first month, followed by one call in subsequent months. Participants randomized to the control group received standard print materials related to weight loss that were comparable to what one would receive from community centers or nonprofit governmental organizations.
Based on the goals of the present analyses, for purpose of parsimony and to maximize statistical power, participants were pooled together and analyzed independently from their intervention group.
Measures and procedures
A total of seven self-reported health behaviors were analyzed. Each behavior was measured at three time points: baseline, 6 months and 12 months. Questions were asked to estimate each behavior over the past month, for a typical day or week depending on the behavior (see examples below for each item).
Physical activity
The physical activity score was calculated by summing moderate and vigorous recreational activities and commuting activities measured with the Global Physical Activity Questionnaire (e.g., During the past month, in a typical week, on how many day do you do moderate-intensity sports, fitness or recreational (leisure) activities; Bull et al., 2009). This score was expressed in average minutes per day of moderate to vigorous physical activity.
Sedentary behavior
Sedentary behavior was measured with a 16-item survey (Rosenberg et al., 2010) assessing the mean time spent per day in activities such as watching tv, playing computer games, and doing paper work (e.g., during the past month, in a typical weekday, how much time do you spend sitting while watching television?). An average score of total daily sedentary behavior was calculated as follow: [(5 * sum of week-days scores) + (2 * sum weekend-days scores)]/7.
Sleep
Sleep quantity was computed by taking the average of self-reported sleep time expressed in hours per day for both week-days and weekend-days (e.g., During the past month, at what time do you usually go to bed in the evening?). Score was computed as follow: [(5 * week-days sleep duration) + (2 * weekend-days sleep duration)]/7.
Diet behaviors
Diet behaviors were estimated through a 124-item food frequency questionnaire (Subar et al., 2001) scored using the Diet*Calc analysis program (2005). Four behaviors were retained including (1) total vegetables and (2) fruits consumption reported in daily cup equivalents, (3) total fat, and (4) added sugar daily intake expressed in grams per day (e.g., Over the past month, how often did you drink tomato juice or other vegetable juice? Each time you drank tomato juice or other vegetable juice, how much did you usually drink?). To limit the occurrence of spurious positive correlations due to a “quantity effect” (i.e., people that eat more in general, are more likely to eat a greater variety of food), all these variables were centered (i.e., z-score) before running the main analyses.
Statistical analyses
Preliminary analyses were conducted to detect extreme values and outliers (i.e., based on the inter quartile range), and data distribution was inspected for each behavioral variable. Missing data were handled with imputation method (results for the network analyses were similar with and without imputation), and each variable was standardized.
Networks were then computed based on partial correlations methods (Costantini et al., 2019). In network analyses, an edge (i.e., association) between two nodes (i.e., variable included in the network, behaviors for the present analyses) is drawn if they correlate after controlling for all other variables in the network. Edges are characterized by two main properties: the weight and the sign of the association. Weight is graphically represented by the thickness of the lines connecting two variables; thick to thin lines indicate strong to weak associations. Signs were represented here by the color of the edges, with positive and negative associations represented with blue and red lines respectively (see Epskamp et al., 2018).
In accordance with our hypotheses, and following the method proposed by Costantini et al. (2019), two different networks were built. First, a between-participant network was computed to estimate the average associations between behaviors during the intervention. This network tested the average pattern of associations across the entire trial between each behavior (i.e., first study objective). The between-participants network was created by averaging the scores of each participant for each behavior across the three assessments of the trial (i.e., baseline, 6 months, 12 months). Second, a within-participant network was computed to estimate the covariation hypothesis. The within-participants network was computed by subtracting the mean of each participant’s behavior across the three time points from each participant’s scores at each time. Thus, estimating a network of inter-relationships, centered on each person’s “average” behavioral pattern over 12-months. This method allowed us to test if variations from the mean level for one behavior were associated with variations from the mean for other behaviors, hence covariation (Costantini et al., 2019).
According to recommendations, ‘least absolute shrinkage and selection operator’ (LASSO) estimation, using Extended Bayesian information Criterion (EBIC), was applied to estimate the covariation structure in the two networks (Epskamp et al., 2018; Costantini et al., 2019). Further, a correction for false positive edges was applied (see, Jankova & van de Geer, 2018). This approach is recommended to build sparse, conservative networks with lower sensitivity and higher specificity to weak associations, instead of denser networks’ estimation methods. Analyses were performed with the statistical software R (version 3.6.2), following the guideline provided by Costantini et al. (2019). The data and code used in the present study are available as supplemental materials.
Results
Descriptive statistics
Participants (N = 278, 260, and 253 at baseline, 6-month, and 12-month visits, respectively) were 77% male, 41% Hispanic, 44% college graduate or higher, and 22% unemployed. Participants were on average 41.7 (SD = 11.1) years old and had a mean BMI of 32.7 (SD = 3.4) kg/m2. Means and standard deviations for each behavioral variable are presented in Table 1, with results indicating that participants, on average, met national recommendations for physical activity, sleep, vegetable consumption, fat consumption, and fruit consumption, but not added sugar consumption at baseline, 6, and 12 months.
Table 1.
Means and standard deviations for each behavioral variable
| Time 1 M (± SD) | Time 2 M (± SD) | Time 3 M (± SD) | Average recommendations | |
|---|---|---|---|---|
| Self-reported PA (minutes per day) | 74.5 (74.2) | 51.3 (56.7) | 56.2 (59.5) | 30 min per day |
| Sedentary Behavior (specific unit) | 21.7 (7.2) | 20.4 (7.2) | 20 (7.3) | NA |
| Sleep duration (hours per day) | 7.8 (1) | 7.9 (1) | 7.9 (1.1) | > 7 h per days |
| Vegetables (cup equivalent per day) | 2.2 (1.4) | 2.1 (1.4) | 1.9 (1.4) | 2–3 cups per day |
| Fruits (cup equivalent per day) | 1.6 (1.1) | 1.6 (1.1) | 1.5 (1.1) | 1.5–2 cups per day |
| Fat (grams per day) | 83.6 (42) | 61.6 (37.6) | 59.5 (33) | 44–78 g (for an average 2000 calories per day diet) |
| Added sugar (grams per day) | 113.8 (64.3) | 90.9 (58.1) | 85.8 (57.6) | 25–38 g per day (for women and men respectively) |
US recommendations are proposed for information in accordance with the Center for Disease Control and prevention guidelines
Between-participant network analysis
The graphical representation of the between-participants network analysis is presented in Fig. 1 (left part). Positive associations emerged between eating behaviors, except between total fat and fruit consumption, which were negatively related; and vegetables and added sugar consumption, which were not significantly related. Results showed one association between two different health behaviors. Specifically, sedentary behavior was positively related to total fat intake. No other inter-relationships between the seven health behaviors were found.
Fig. 1.
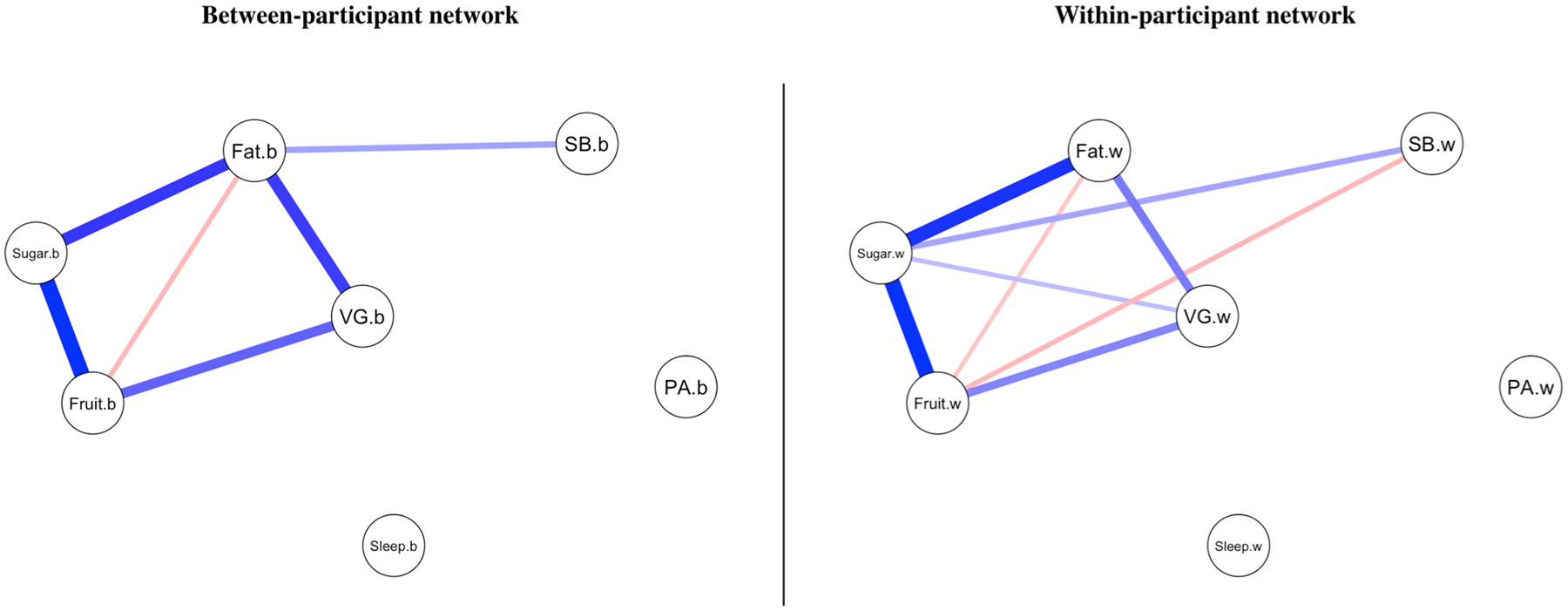
Network analyses. Note: PA = physical activity; SB = sedentary behavior; VG = vegetables; .b = between-participant; .w = within-participant; Blue edges/lines = positive correlation; Red edges/lines = negative correlation
Within-participant network analysis
The graphical representation of the within-participants network analysis is presented in Fig. 1 (right part). A pattern of positive associations between the different eating behaviors was observed. Significant and positive covariations were found between (1) fruits, vegetables, and added sugar consumption, and (2) total fat, vegetables, and added sugar consumption. This means, for example, that at each specific time point of the study, when participants reported consuming more fat than their average annual level of fat consumption throughout the study, they also reported higher consumption of vegetables and added sugar. Unlike the between-participant network, a positive and significant covariation was found between vegetables and added sugar consumption.
Covariations across behaviors were also observed between diet behaviors and sedentary behavior. A significant, and negative, covariation was found between sedentary behavior and fruit consumption. When participants reported more sedentary behavior than their average level across the study, they also reported less fruit intake. A positive covariation was found between sedentary behavior and added sugar, such that participants who reported more sedentary behavior than their average level throughout the study, also reported greater consumption of added sugar. No other significant covariations were found.
Discussion
This study yields new empirical insights into the associations between health behaviors among adults enrolled in a weight loss intervention. While these findings are generally aligned with the results of previous multiple health behavior research (i.e., Rosenberg et al., 2007; Spring et al., 2012), they expand on past work by using a novel statistical approach to examine both within- and between-participant associations for a variety of behaviors. As hypothesized, different patterns of association were observed at the between- and within-participant levels. This confirms that this analytical distinction is important when examining associations between health behaviors, since results obtained at the two levels differs and could lead to contradictory interventional perspectives.
Between-participant network
Between participants, we found a significant association between fat consumption and sedentary behavior throughout the course of the study. This is consistent with previous research (Rosenberg et al., 2007), though, contrary to expectations, we found no associations between physical activity and other health behaviors.
The positive associations between added sugar and total fat, as well as fruits and vegetables, support findings from previous studies highlighting associations between health-enhancing and health-reducing diet behaviors (de Vries et al., 2008). We also found that more time spent engaged in sedentary behavior was associated with consuming more fat throughout the study. This pattern of association is consistent with the result of a systematic review indicating that a higher level of sedentary behavior is related to a less healthy diet (Hobbs et al., 2015).
Of interest to those developing multiple health behavior change interventions, fruit consumption was positively correlated with added sugar intake, and vegetable consumption was positively correlated with total fat intake. This could be due to participants choosing to consume fruits and vegetables in foods that also contain high amounts of sugar or fat, such as sugar sweetened fruit yogurt or salads with high fat dressing. This may highlight a need for more education in multiple health behavior change intervention on healthy ways to consume fruits and vegetables that do not simultaneously increase sugar and fat consumption. Measuring diet behaviors is complex, and the results from this study could also be re-explored using other diet indicators, such as food diversity (Drescher et al., 2007).
Physical activity across the trial was not associated with other behaviors, a finding that conflicts with previous studies showing positive associations between physical activity and fruit and vegetable consumption (de Vries et al., 2008; Fleary & Nigg, 2019). This might be explained by methodological reasons. Notably, physical activity scores were surprisingly high in the present study, especially at the first measurement point. It is possible that the physical activity measure was compromised due to social desirability (as well as the other behavioral outcomes). More research is needed to better understand the complex, and inherent, relationships between energy expenditure and food intake among individuals with obesity (see, Manore et al., 2017).
The lack of association between physical activity and sedentary behavior was expected since most previous research has found these behaviors to be relatively independent (Pearson et al., 2014; see also, Keadle et al., 2017). The absence of association between sleep and physical activity is discussed below in the ‘within-participant network’ section.
Within-participant network
The observed within-participant patterns of health behaviors support previous findings from the literature showing significant covariations between sedentary behavior and diet behaviors, and non-significant covariations between diet behaviors and physical activity (Rosenberg et al., 2007; Spring et al., 2012). Specifically, four differences with the between-participant network were found that might be fruitfully explored in future studies of interventions targeting multiple health behavior change in the weight loss context.
Change in sedentary behavior were associated with changes in added sugar and fruits intake, while at the between-participant level sedentary behavior was only associated with fat consumption. This is consistent with previous research showing that sedentary behaviors covary with poor dietary behaviors (Rosenberg et al., 2007; Spring et al., 2012). Thus, results from the within-participant network, in accordance with those from previous studies (i.e., Rosenberg et al., 2007; Spring et al., 2012), point to addressing sedentary behaviors simultaneously with diet behaviors. Future studies could explore the utility of interventions designed to (1) take advantage of the health-enhancing covariations and (2) prevent health-reducing covariations between these behaviors, respectively. Further research could examine how specific sedentary behaviors, such as screen time might trigger specific unhealthy snacks consumption (Hobbs et al., 2015); or, how sedentary breaks during specific stressful moments could prevent the consumption of unhealthy food (Healy et al., 2008).
The positive covariation between vegetables and added sugar consumption could be due to a “compensatory behavior”, such as eating dessert to reward oneself for eating more vegetables (Geller et al., 2017). Recently, an ecological-momentary assessment (EMA) study found strong co-occurrence between both healthy and unhealthy diet behaviors at the daily level (i.e., eating more vegetables to compensate a previous unhealthy meal; Dohle & Hofmann, 2018). Assuming that these compensatory behaviors persist over a longer time scale (i.e., 6-months), it is possible that participants partially compensated for a greater consumption of sugar by increasing vegetable’s intake over the study, and vice versa. These results suggest the need to further understand compensatory behaviors, especially in the diet domain, and how they can be addressed in multiple health behavior change interventions (Amrein et al., 2017; Radtke & Scholz, 2016).
Like in the between-participant network, change in physical activity was not significantly related to changes in sleep behavior. While the results from the literature are mixed concerning this association (Dolezal et al., 2017), this could be explained by both our measure of sleep behavior, representing quantity of sleep instead a quality indicators (Pilcher et al., 1997), and the inability of the 6-month and yearly time-scale used in the present study to capture associations that are better measured using daily-, weekly-, or monthly-level assessments (Irish et al., 2014). In fact, past research suggests that associations between physical activity and sleep are likely to be stronger at micro-temporal scales (i.e., daily or weekly; Irish et al., 2014) comparing to longer time scales, as the ones used in this study.
Overall, differences were found between the two networks. This confirms that different patterns of results could be expected when considering change over time (Conroy et al., 2015; Scholz, 2019), and demonstrate how associations observed in cross-sectional studies are not sufficient to inform the design of multiple health behavior change interventions.
Study strengths, limitations and perspectives
The strengths of this study include the simultaneous observation and analysis of seven health behaviors measured at three time points over 1 year among a diverse group of overweight and obese adults enrolled in a weight loss intervention; thus, providing unique information about this specific population and context. Further, this study utilized network analyses, which is a relatively innovative method in behavioral science to test and visualize complex patterns of associations (i.e., 49 edges/associations tested here) in an intelligible and parsimonious way (see Heino et al., 2019).
This study has several limitations. Network analyses require a relatively high number of participants. For the purpose of parsimony and to save statistical power, we did not split our sample in different groups according to potentially important covariates such as sex, age, or socio-economic status which could influence the associations between behaviors. Future research should examine if networks’ shapes differ base on these characteristics. Networks could also be specified for intervention and control groups separately, to explore potential differences in networks’ shape depending on a treatment allocation (Costantini et al., 2019). We computed distinct networks for each group of the present study as ancillary analyses (i.e., SMS and phone calls, SMS only and control group). If the shape of these group-based networks were mainly similar to the ones reported above in the main analyses, some differences were observed. For example, a positive covariation was found between physical activity and vegetable consumption for the SMS-only group at the within-participant level. Future interventional studies might use network analyses to compare the effects of an intervention on several outcomes (see, Heino et al., 2019; Mkhitaryan et al., 2019). Another limitation, specific to the within-participant network, concerns the relatively low number of observations per subject in this study (3 times), as well as the time between measures (every 6 months). Additionally, all variables were assessed by self-report, and may have been subject to bias. Relatedly, levels of physical activity were markedly high at baseline, and thus there was little room for improvement across the study. Regarding the measures of diet behaviors, is it possible that some of the positive associations observed were due to a ‘quantity effect’ (i.e., people that eat more in general, are more likely to eat a greater variety of food). To prevent this issue, we centered all the diet variables before running the analyses. Nonetheless, future work might choose to compute a ratio score considering each participant’s total amount of food consumed, or use other qualitative (i.e., instead of quantitative) diet measures. Lastly, this was a single-site study in which the entire sample resided in San Diego County and were primarily (77%) female, which may limit the generalizability of the findings.
Future research could apply methods like EMA, as it might allow for a more in depth test of the covariations and sequentially between health behaviors at different time scales (Conroy et al., 2017; Dunton, 2018). Notably, this would allow for assessment of how different measurement intervals (i.e., days, weeks, months, years) shape multiple health behaviors associations over time (Scholz, 2019). Similarly, to better understand potential heterogeneity in these relationships, network analyses could be applied to model covariations between behaviors for each individual separately, thus adopting an idiographic approach (i.e., building a network model for each participant separately; see, Epskamp et al., 2018). This would allow for testing the idiosyncratic nature of multiple health behavior change and potentially lead to the development of highly individualized interventions using, for example, methods from control system engineering (Hekler et al., 2018). Finally, it is important to note that the present study differs slightly from other studies testing the role of an intervention targeting one behavior on other behaviors (i.e., targeting physical activity and assessing the effect of the intervention on fruit consumption). If some of this kind of interventional study explicitly test covariations between behaviors (see Spring et al., 2012), others only report the effect of the intervention targeting one specific behavior on other behaviors, without testing covariations between behaviors (e.g., Spring et al., 2018). To better understand health behaviors covariations in different contexts, we recommend the need to further systematically test this phenomenon in future multiple health behavior change interventions (via networks analyses or other methods).
Conclusion
A recent synthesis from the literature about multiple health behavior change has argued for more research about the associations between health behaviors to informed the design of future interventions (Geller et al., 2017). The findings from our study, and especially those related to the covariations between behaviors, if confirmed in other studies that address multiple health behaviors in similar weight loss context, suggest that successful multiple behavior change interventions will need to (1) simultaneously target sedentary and diet behaviors; and (2) address potential compensatory behaviors in the diet domain.
Acknowledgements
The first author wish to thanks the Dr Giulio Costantini (Univeristy of Milano-Bicocca) for his advices concerning the network analyses and the Dr Paquito Bernard (Université du Québec à Montréal) for his feedbacks on an earlier draft. This work was supported by NIH Grant R01 CA138730.
Footnotes
Conflict of interest All authors declare that they have no competing interests with the present research.
Ethical approval This study was approved by the ethical committee of the University of California, San Diego; Participants provided written informed consent at the time of enrollment at the baseline study visit.
Human and animal rights and informed consent All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Amrein MA, Rackow P, Inauen J, Radtke T, & Scholz U (2017). The role of compensatory health beliefs in eating behavior change: A mixed method study. Appetite, 116, 1–10. 10.1016/j.appet.2017.04.016 [DOI] [PubMed] [Google Scholar]
- Boudreaux ED, Francis JL, Carmack Taylor CL, Scarinci IC, & Brantley PJ (2003). Changing multiple health behaviors: Smoking and exercise. Preventive Medicine, 36(4), 471–478. [DOI] [PubMed] [Google Scholar]
- Bull FC, Maslin TS, & Armstrong T (2009). Global physical activity questionnaire (GPAQ): Nine country reliability and validity study. Journal of Physical Activity & Health, 6(6), 790–804. [DOI] [PubMed] [Google Scholar]
- Conroy DE, Hedeker D, Mcfadden HG, Pellegrini CA, Pfammatter AF, Phillips SM, et al. (2017). Lifestyle intervention effects on the frequency and duration of daily moderate-vigorous physical activity and leisure screen time. Health Psychology, 36(4), 299–308. 10.1037/hea0000418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy DE, Ram N, Pincus AL, Coffman DL, Lorek AE, Rebar AL, et al. (2015). Daily physical activity and alcohol use across the adult lifespan. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 34(6), 653–660. 10.1037/hea0000157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costantini G, Richetin J, Preti E, Casini E, Epskamp S, & Perugini M (2019). Stability and variability of personality networks. A tutorial on recent developments in network psychometrics. Personality and Individual Differences, 136, 68–78. 10.1016/j.paid.2017.06.011 [DOI] [Google Scholar]
- de Vries H, van’t Riet J, Spigt M, Metsemakers J, van den Akker M, Vermunt JK, et al. (2008). Clusters of lifestyle behaviors: Results from the Dutch SMILE study. Preventive Medicine, 46(3), 203–208. 10.1016/j.ypmed.2007.08.005 [DOI] [PubMed] [Google Scholar]
- Dohle S, & Hofmann W (2018). Consistency and balancing in everyday health behaviour: An ecological momentary assessment approach. Applied Psychology Health and Well-Being. 10.1111/aphw.12148 [DOI] [PubMed]
- Dolezal BA, Neufeld EV, Boland DM, Martin JL, & Cooper CB (2017). Interrelationship between sleep and exercise: A systematic review. Advances in Preventive Medicine. 10.1155/2017/1364387 [DOI] [PMC free article] [PubMed]
- Dombrowski SU, Avenell A, & Sniehott FF (2010). Behavioural interventions for obese adults with additional risk factors for morbidity: Systematic review of effects on behaviour, weight and disease risk factors. Obesity Facts, 3(6), 377–396. 10.1159/000323076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drescher LS, Thiele S, & Mensink GBM (2007). A new index to measure healthy food diversity better reflects a healthy diet than traditional measures. The Journal of Nutrition, 137(3), 647–651. 10.1093/jn/137.3.647 [DOI] [PubMed] [Google Scholar]
- Dunton GF (2018). Sustaining health-protective behaviors such as physical activity and healthy eating. JAMA, 320(7), 639–640. 10.1001/jama.2018.6621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher AJ, Medaglia JD, & Jeronimus BF (2018). Lack of group-to-individual generalizability is a threat to human subjects research. Proceedings of the National Academy of Sciences. 10.1073/pnas.1711978115 [DOI] [PMC free article] [PubMed]
- Fleary SA, & Nigg CR (2019). Trends in health behavior patterns among U.S. adults, 2003–2015. Annals of Behavioral Medicine, 53(1), 1–15. 10.1093/abm/kay010 [DOI] [PubMed] [Google Scholar]
- Geller K, Lippke S, & Nigg CR (2017). Future directions of multiple behavior change research. Journal of Behavioral Medicine, 40(1), 194–202. 10.1007/s10865-016-9809-8 [DOI] [PubMed] [Google Scholar]
- Godino JG, Golaszewski NM, Norman GJ, Rock CL, Griswold WG, Arredondo E, et al. (2019). Text messaging and brief phone calls for weight loss in overweight and obese English- and Spanish-speaking adults: A 1-year, parallel-group, randomized controlled trial. PLOS Medicine. 10.1371/journal.pmed.1002917 [DOI] [PMC free article] [PubMed]
- Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, et al. (2008). Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care, 31(4), 661–666. 10.2337/dc07-2046 [DOI] [PubMed] [Google Scholar]
- Heino MTJ, Knittle K, Fried E, Sund R, Haukkala A, Borodulin K, et al. (2019). Visualisation and network analysis of physical activity and its determinants: Demonstrating opportunities in analysing baseline associations in the Let’s Move It trial. Health Psychology and Behavioral Medicine, 7(1), 269–289. 10.1080/21642850.2019.1646136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hekler EB, Rivera DE, Martin CA, Phatak SS, Freigoun MT, Korinek E, et al. (2018). Tutorial for using control systems engineering to optimize adaptive mobile health interventions. Journal of Medical Internet Research. 10.2196/jmir.8622 [DOI] [PMC free article] [PubMed]
- Hobbs M, Pearson N, Foster PJ, & Biddle SJH (2015). Sedentary behaviour and diet across the lifespan: An updated systematic review. British Journal of Sports Medicine, 49(18), 1179–1188. 10.1136/bjsports-2014-093754 [DOI] [PubMed] [Google Scholar]
- Irish LA, Kline CE, Rothenberger SD, Krafty RT, Buysse DJ, Kravitz HM, et al. (2014). A 24-hour approach to the study of health behaviors: Temporal relationships between waking health behaviors and sleep. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 47(2), 189–197. 10.1007/s12160-013-9533-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jankova J, & van de Geer S (2018). Inference for high-dimensional graphical models In Drton M, Maathuis M, Lauritzen S, & Wainwright M (Eds.), Handbook of graphical models. Boca Raton: CRC Press. [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. (2014). 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Obesity Society. Circulation, 129(25 Suppl 2), S102–S138. 10.1161/01.cir.0000437739.71477.ee [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keadle SK, Conroy DE, Buman MP, Dunstan DW, & Matthews CE (2017). Targeting reductions in sitting time to increase physical activity and improve health. Medicine and Science in Sports and Exercise, 49(8), 1572–1582. 10.1249/mss.0000000000001257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Castro CM, Buman MP, Hekler EB, Urizar GG, & Ahn DK (2013). Behavioral impacts of sequentially versus simultaneously delivered dietary plus physical activity interventions: the CALM Trial. Annals of Behavioral Medicine, 46(2), 157–168. 10.1007/s12160-013-9501-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolodziejczyk JK, Norman GJ, Roesch SC, Rock CL, Arredondo EM, Madanat H, et al. (2015). Exploratory and confirmatory factor analyses and demographic correlate models of the strategies for weight management measure for overweight or obese adults. American Journal of Health Promotion. 10.4278/ajhp.130731-quan-391 [DOI] [PubMed]
- Lippke S, Nigg CR, & Maddock JE (2012). Health-promoting and health-risk behaviors: Theory-driven analyses of multiple health behavior change in three international samples. International Journal of Behavioral Medicine, 19(1), 1–13. 10.1007/s12529-010-9135-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manore MM, Larson-Meyer DE, Lindsay AR, Hongu N, & Houtkooper L (2017). Dynamic energy balance: An integrated framework for discussing diet and physical activity in obesity prevention—Is it more than eating less and exercising more? Nutrients, 9(8), 905 10.3390/nu9080905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mkhitaryan S, Crutzen R, de Vries N, & Steenaart E (2019). Network approach in health behavior research: How can we explore new questions? Health Psychology and Behavioral Medicine. 10.31234/osf.io/btv36 [DOI] [PMC free article] [PubMed]
- Pearson N, Braithwaite RE, Biddle SJH, van Sluijs EMF, & Atkin AJ (2014). Associations between sedentary behaviour and physical activity in children and adolescents: A meta-analysis: Active and sedentary behaviours in youth. Obesity Reviews, 15(8), 666–675. 10.1111/obr.12188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilcher JJ, Ginter DR, & Sadowsky B (1997). Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. Journal of Psychosomatic Research, 42(6), 583–596. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Nigg CR, Spring B, Velicer WF, & Prochaska JO (2010). The benefits and challenges of multiple health behavior change in research and in practice. Preventive Medicine, 50(1–2), 26–29. 10.1016/j.ypmed.2009.11.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radtke T, & Scholz U (2016). Beliefs are not behavior. Zeitschrift Für Gesundheitspsychologie, 24(3), 119–129. 10.1026/0943-8149/a000161 [DOI] [Google Scholar]
- Rosenberg D, Norman GJ, Sallis JF, Calfas KJ, & Patrick K (2007). Covariation of adolescent physical activity and dietary behaviors over 12-months. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 41(5), 472–478. 10.1016/j.jadohealth.2007.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg DE, Norman GJ, Wagner N, Patrick K, Calfas KJ, & Sallis JF (2010). Reliability and validity of the Sedentary Behavior Questionnaire (SBQ) for adults. Journal of Physical Activity & Health, 7(6), 697–705. [DOI] [PubMed] [Google Scholar]
- Scholz U (2019). It’s time to think about time in health psychology. Applied Psychology: Health and Well-Being. 10.1111/aphw.12156 [DOI] [PubMed]
- Spring B, Pellegrini C, Mcfadden HG, Pfammatter AF, Stump TK, Siddique J, et al. (2018). Multicomponent mHealth intervention for large, sustained change in multiple diet and activity risk behaviors: The make better choices 2 randomized controlled trial. Journal of Medical Internet Research. 10.2196/10528 [DOI] [PMC free article] [PubMed]
- Spring B, Schneider K, McFadden HG, Vaughn J, Kozak AT, Smith M, et al. (2012). Multiple behavior changes in diet and activity: A randomized controlled trial using mobile technology. Archives of Internal Medicine, 172(10), 789–796. 10.1001/archinternmed.2012.1044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subar AF, Thompson FE, Kipnis V, Midthune D, Hurwitz P, McNutt S, et al. (2001). Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. American Journal of Epidemiology, 154(12), 1089–1099. [DOI] [PubMed] [Google Scholar]


