Abstract
Objective:
Mental illness is an important public health concern, often starting early in life and particularly impacting children from low-and middle-income countries. Our aims were to 1) determine, in a representative sample of public preschool 4- to 5-year old children in Brazil, the prevalence of internalizing and externalizing disorders and socioemotional development delays; and 2) to identify modifiable risk factors associated with mental, behavioral, or developmental disorders (MBDD), such as microsystem (i.e., parent-child relationship), mesosystem (social support), and macrosystem contextual factors (neighborhood disadvantage).
Methods:
A random sample of public preschool children was recruited in the city of Embu das Artes (São Paulo metropolitan area) (n=1,292 from 30 public preschools). Six-month prevalence of MBDD was measured using the Child Behavior Checklist (CBCL) and the Ages and Stages Questionnaires: Social-Emotional (ASQ:SE).
Results:
Six-month prevalence estimates were 25.4% for internalizing disorders, 12.1% for externalizing disorders, and 30.3% for socioemotional development delays. MBDD prevalence estimates were higher in families with stressful relationships and parental depression or anxiety, and in families with lower social capital.
Conclusion:
At least 25% of preschool children living in an urban area in Brazil presented a mental health disorder. These mental disorder were associated with modifiable factors such as stressful family relationships and lower social capital. Prevention and intervention measures such as family therapy are needed to decrease such high prevalence.
Keywords: Children, epidemiology, internalizing and externalizing disorders, family
Introduction
The early onset of mental illness is an important public health concern,1,2 with consequences ranging from a reduced likelihood of completing basic education3 to poor social cohesiveness and reduced capacity to cope with future adversities. In the absence of adequate treatment, childhood mental illness also correlates with negative outcomes later in life4-6: when untreated, mental health symptoms in preschoolers remain stable throughout adolescence.7,8 The extent to which unfavorable environments, such as family conflicts and poverty, contribute to these outcomes deserves further research.9,10
While substantial research has been conducted on the determinants of child mental health in high-income regions such as the United States and Europe, only a few studies with longitudinal design are available, demonstrating associations between social-emotional skills in U.S. preschoolers (ages 5-6), and educational and mental health outcomes, such as poor educational achievement and mental disorders later in life.11 Externalizing problems in British preschool children were shown to be mediated by family poverty and parental socioeconomic position.12 Conversely, little is known about the drivers of childhood mental illness in lower- and middle-income (LMICs) and low-income communities.
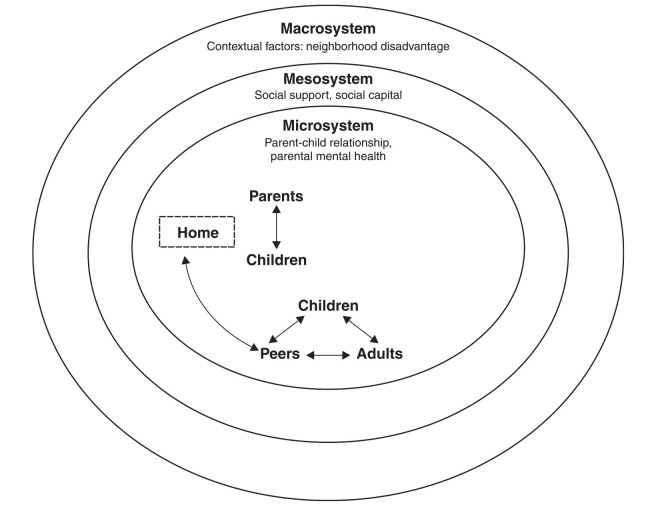
Considering ecodevelopmental theory (EDT; Figure 1), the following factors may impact childhood mental illness: neighborhood social stressors (macrosystem), social networks and support (mesosystem), and family and parent-child relationship (microsystem). According to EDT, these systems are inter-related (e.g., parental social networks influence parent-child relationships, while neighborhood characteristics affect parental stress). Human development occurs in a context where aspects of the social environment interact.13 Building on this perspective, we proposed to use a multifactorial approach that acknowledges the interplay among these factors to study the influence of multiple social ecological levels on mental health.14
Figure 1. Conceptual model of mental health determinants based on ecodevelopmental theory.
In Brazil, cross-sectional studies show that mental health problems in school-age children are associated with low socioeconomic status (SES) and with a combination of low income, illiteracy, unemployment, and poor housing conditions. Limited access to health and education increase the risk of mental health problems.15-19 In the latest Brazilian census (2010), the school-age population was estimated as greater than 60 million in the country. Specifically, the São Paulo metropolitan area had an estimated population of 3,178,893 children and adolescents, with 400,000 exhibiting mental health problems.20
Despite the recognition of psychiatric disorders as a major cause of impairment in children and adolescents, with lasting effects and burden for caregivers, mental health is still neglected21,22 Likewise, the notion that early identification of risk factors is critical to prevent the development and persistence of disorders over time23 has not been sufficient to bridge the huge gap between mental health needs and the resources available, especially in LMICs.24 Preventive interventions, including social skill training for children, child-rearing practices for parents, and support for teachers concerning at-risk children, have shown some efficacy in reducing the persistence or incidence of later mental disorders.25,26 However, as most of these studies have been conducted in high income countries (HICs), our knowledge is limited regarding which factors (e.g., cultural, contextual) should be targeted in preventive interventions in LMIC or low-income communities, where poverty is pervasive and the need is greatest.
Therefore, the present study – the Brazilian Preschool Mental Health Survey (Pre-K) – was performed with a representative sample of public preschool children aged 4 to 5 years in the metropolitan area of São Paulo to 1) determine prevalence estimates of internalizing and externalizing disorders and socioemotional development delays; and 2) identify modifiable risk factors associated with internalizing and externalizing disorders during early childhood, including micro- (i.e., parent-child relationship, parental psychopathology), meso- (parental social networks), and macrosystem contextual factors (i.e., neighborhood disadvantage).
Methods
Sampling
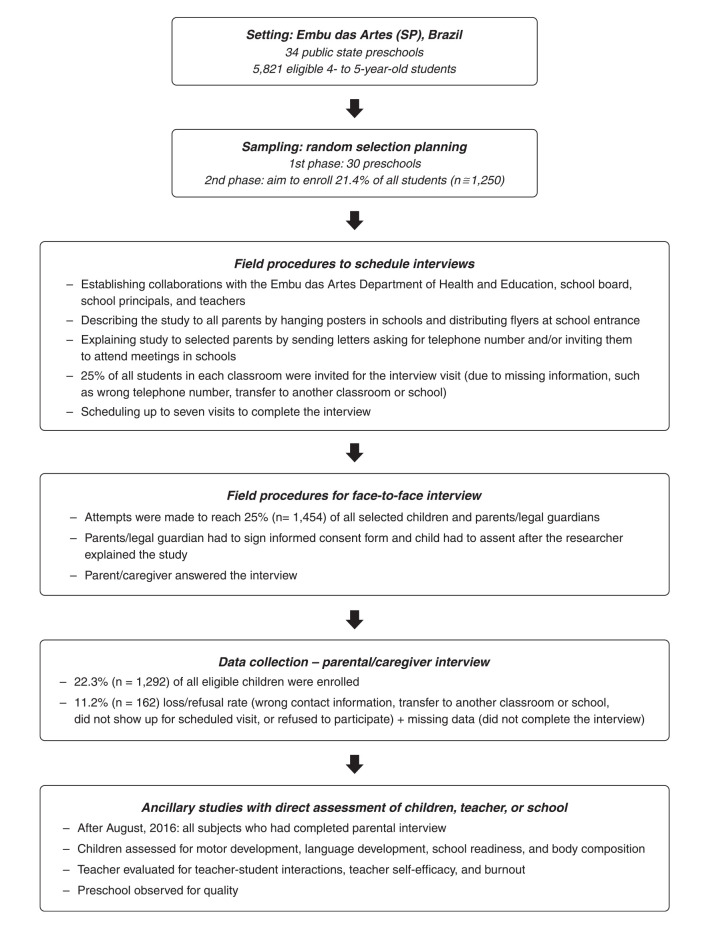
In the first stage of sampling, schools were selected using probability proportional to size (PPS) sampling, with the size variable determined by the number of eligible 4- to 5-year-olds in each school (Figure 2). We randomly selected 30 out of 34 existing preschools using PPS (of note, in Brazil children attend public preschools in the neighborhood where they live). In the second stage, a list of all eligible 4- to 5-year-olds in each classroom of selected schools was produced; eligible participants were then randomly selected. Our goal was to estimate the prevalence rate of internalizing problems, externalizing problems, and social-emotional developmental delays. We planned to sample 1,250 children (21.4% of the 5,821 children enrolled in all preschools in 2016), with approximately 40 children from each school and 5 children per classroom.
Figure 2. The Brazilian Preschool Mental Health Survey flowchart.
Since children in the same school are more alike than children from different schools, we assumed a range of intra-cluster correlation (ICC) of 0.01 to 0.1, which corresponds to a range of design effect of 1.49 to 5.90. We expected that the prevalence of internalizing disorders (p) would be around 10-18%, similar to the prevalence of externalizing disorders. The prevalence estimated for our sample would achieve reasonable precision with the margin of error (MOE) displayed in Table 1. The 95% confidence interval (95%CI) estimate of the prevalence is equal to p ± MOE.
Table 1. Margin of error for the 95%CI of baseline prevalence estimates.
| Prevalence estimate (p) | ICC = 0.01 | ICC = 0.05 | ICC = 0.10 |
|---|---|---|---|
| 10 | 0.020 | 0.031 | 0.040 |
| 15 | 0.024 | 0.037 | 0.048 |
| 18 | 0.026 | 0.040 | 0.052 |
95%CI = 95% confidence interval; ICC = intra-cluster correlation.
We invited 1,454 selected children and parents (25% of the 5,821 eligible students) in each classroom because of missing data, such as lack of telephone number/wrong number or student transfer to another classroom or school. For each subject, up to seven attempts were made to schedule the interview. We enrolled 1,292 children and parents (22.3% of all eligible children). All parents or guardians providing informed consent for participation were interviewed, even if the target sample had already been met in that specific classroom.
Study design and target population
The present cohort study was performed in 2016, in Embu das Artes, a city with a population of 261,781 (2015) located in the São Paulo city metropolitan area. A representative sample of 1,292 children aged 4 to 5 years attending public preschools and their parents were interviewed.
The average age of the household head in Embu das Artes was 43 years; residents under the age of 30 years accounted for 54.1%. The proportion of children under age 6 was 9.4% of the total population in 2010.20 Almost 36% of the city’s population met criteria for high or very high social vulnerability according to the São Paulo Index of Social Vulnerability (ĺndice Paulista de Vulnerabilidade Social [IPVS]): the IPVS was created by researchers at the Sistema Estadual de Análise de Dados (SEADE), a government bureau, using census data. Less than 10% of the population was categorized as very low vulnerability. The average monthly household income was 1,672 BRL (approximately 420 USD), and 22.8% of households had an income of less than half the per capita minimum wage.27 In Embu das Artes, urban violence is pervasive and in 2012 the city homicide rate of 27.33 deaths per 100,000 people was 1.81 times that of São Paulo state.28
By law, all children ages 4-5 years old are offered universal preschooling in Brazil. In the São Paulo metropolitan area, 80% of children in this age group attend preschools on a regular basis. Given this high attendance, we were able to capture most children in that age group, enhancing the generalizability of our findings.
Data collection
Collaborations were established with the Embu das Artes Department of Health and Education, school board, school principals, and teachers before recruiting participants. After that, the parents of selected students received letters explaining the study and asking for consent to participate. To increase privacy, the interview was conducted in a room without the presence of other family members (parent and child were interviewed in separate rooms). Strict security procedures were followed to ensure confidentiality of the study data.
Data collection from parent interviews for the Brazilian Preschool Mental Health Survey was completed through face-to-face interviews in private rooms in the schools, mostly during weekends. Interviews were conducted in Portuguese by local trained health professionals from UNIFESP, between May 2016 and December 2016. Data were collected via a computerized-assisted survey with personal smartphones, together with flashcards with response choices listed in color. The entire interview process with the parent or legal guardian (i.e., obtaining informed consent and actual interview with parent/child) ranged from 1.75 hours, in the case of few distractions, up to a maximum of 3 hours. Data were collected using 18 LUMIA 640 smartphones for data insertion in real time. Using a Windows app developed in Visual Studio/C#, we stored all the instruments of the study. Data were exported to a STATA 14 file. All variables assessed and instruments used are described in Tables S1 and S2 (170.7KB, pdf) (online-only supplementary material).
Ancillary studies with direct assessment of children, teacher, or school
After August, 2016, we also assessed children regarding specific measures on motor development, language development, school readiness, body composition, teacher-student interactions, teacher self-efficacy and burnout, and school quality. Children were assessed directly in sessions lasting up to 40 minutes during school days or weekends. Children answered questions related to language ability and school readiness, were evaluated on motor development, and body composition. Teachers answered questions regarding teacher-student interactions, teacher self-efficacy, and burnout. We also observed each child in their classrooms and the whole preschool to evaluate school quality. Each of these evaluations were conducted by trained health professionals in the specific assessment. All assessments are displayed in Tables S3 (170.7KB, pdf) (online-only supplementary material).
Interviewer training and field work quality control
Interviews were carried out by trained health professionals that were social workers, speech pathologists, psychologists, child psychiatrists, and occupational therapists. All health professionals were trained in 2-day theoretical seminars and role-play activities, and five direct supervised field interviews. In each preschool, there was always at least one researcher experienced in child psychopathology and urban violence to clarify any doubts during the interviews. Moreover, two experienced chief field supervisors were always available on-site or at UNIFESP.
Recruitment and refusal rates (11.2%), as well as the completed interview data, were monitored by local researchers on a daily basis to ensure adherence to the study protocol as well as adequacy of interview follow-up procedures. Interviews that were either incomplete or incorrectly administered were returned to the interviewer to re-contact the interviewee and complete it.
Data analysis
Data management for this study involved several steps. We constructed a database combining data from the parental interview, direct child evaluation (motor and language development, school readiness and body composition measures), teacher assessments from the survey (teacher-student interactions, teacher self-efficacy, and burnout) and preschool observations (Figure 2). We weighted each respondent by: 1) a factor that accounted for their probability of being selected within their stratum (to obtain citywide estimates accounting for different sampling probabilities within strata); and 2) as necessary, to account for potential bias introduced by non-response. Then, we developed descriptive statistics (e.g., frequency counts, percentages, means) to characterize the sample, while applying the complex sample weights. Weighted point estimates and confidence intervals were used to estimate population values for all descriptive variables. Finally, specific aims were evaluated including prevalence of internalizing and externalizing disorders, as well as their associations with each level of our conceptual model (Figure 1). To evaluate these associations, we performed hierarchical mixed-effects logistic regressions29 and the outcome variables of interest were internalizing and externalizing disorders and socioemotional development delays. Results were presented as odds ratios (ORs), and p-values. First, the microsystem variables were introduced (Step 1); next, the mesosystem variables (Step 2) and then we added the macrosystem variables (Step 3). In the end, we presented a final model that included only the significant variables (p < 0.05). Stata 14 was used to handle svy commands for data analysis.
Ethics statement
Institutional review board (IRB) approval was obtained from both the Universidade Federal de São Paulo (UNIFESP) (protocol 981.943) and Columbia University (protocol AAAP9754). Our research group at UNIFESP provided outpatient treatment for the children who were diagnosed with MBDD in Embu das Artes.
Results
Sociodemographic characteristics of the sample
The sample included 1,292 children and their parents/caregivers. Most children were male (51.8%); also, based on parental report, most children were non-white (58.5%), and protestant (49.9%). Most caregivers were the biological mother (81%), and most self-reported as non-white (70.9%), married (71.9%), had high school-level education or higher (60.5%), and were currently employed (53.4%). Regarding SES, 62.5% had middle SES (Table 2).
Table 2. Sociodemographic characteristics of a representative sample of 4- and 5-year-old preschool children in Embu das Artes, state of São Paulo, Brazil, and their caregivers (n=1,292).
| n | wt (%) | 95%CI | |
|---|---|---|---|
| Child characteristics | |||
| Preschool stage | |||
| First year | 702 | 50.5 | 50.0-51.1 |
| Second year | 590 | 49.5 | 48.9-50.0 |
| Age (years) | |||
| 4 | 409 | 29.5 | 28.6-30.3 |
| 5 | 883 | 70.5 | 69.7-71.4 |
| Sex | |||
| Male | 666 | 51.8 | 50.7-52.9 |
| Female | 626 | 48.2 | 47.0-49.3 |
| Race | |||
| White | 541 | 41.5 | 40.6-42.4 |
| Non-white* | 751 | 58.5 | 57.6-59.4 |
| Participant has a religion | 1,119 | 86.8 | 86.1-87.4 |
| Religion | |||
| Protestant | 568 | 49.9 | 48.3-51.5 |
| Catholic and others† | 551 | 50.1 | 48.5-51.7 |
| Missing | 173 | 13.2 | 12.6-13.9 |
| Participant attends religious activities | 962 | 74.2 | 73.4-74.9 |
| Participant is adopted | 31 | 2.3 | 2.1-2.6 |
| Caregiver characteristics | |||
| Interviewed | |||
| Biological mother | 1,040 | 81.0 | 80.4-81.5 |
| Others‡ | 252 | 19.0 | 18.5-19.6 |
| Race | |||
| White | 385 | 29.1 | 28.1-30.1 |
| Non-white§ | 907 | 70.9 | 69.9-71.9 |
| Marital status | |||
| Married | 930 | 71.9 | 70.7-73.0 |
| Other|| | 362 | 28.1 | 27.0-29.3 |
| Educational attainment | |||
| Incomplete primary education | 36 | 17.5 | 16.6-18.5 |
| Incomplete secondary education | 284 | 22.0 | 20.9-23.1 |
| Complete secondary education or more | 784 | 60.5 | 59.5-61.4 |
| Employment status | |||
| Employed | 692 | 53.4 | 52.3-54.5 |
| Unemployed | 262 | 20.7 | 19.9-21.6 |
| Housewife | 297 | 22.8 | 22.2-23.5 |
| Medical leave | 17 | 1.4 | 1.2-1.6 |
| Maternal figure is present | 1,289 | 99.8 | 99.7-99.9 |
| Paternal figure is present | 1,205 | 93.4 | 93.1-93.7 |
| Socioeconomic status¶ | |||
| High | 339 | 26.3 | 24.9-27.7 |
| Medium | 781 | 62.5 | 61.4-63.6 |
| Low | 143 | 11.2 | 10.6-11.9 |
| Missing | 29 | 2.2 | 1.9-2.5 |
95%CI = 95% confidence interval; wt (%) = weighted proportions.
Mixed = 588; black = 116; Asian = 36; others = 11.
Catholic, spiritualism, traditional African religions, had no religion (n=3).
Biological father, grandparents, legal guardian, stepmother, adoptive parent.
Mixed = 588; black = 259; Asian = 48; others = 12.
Single, divorced, widowed.
Criteria proposed by the Brazilian Market Research Association (Associação Brasileira de Empresas de Pesquisa [ABEP]), described in Tables S2 (170.7KB, pdf) (online-only supplementary material).
Prevalence of internalizing and externalizing disorders and socioemotional development delays
The 6-month prevalence estimates were 25.4% for internalizing disorders, 12.1% for externalizing disorders, and 30.3% for socioemotional development delays. Girls had more internalizing disorders than boys, while boys had more externalizing disorders (Table 3).
Table 3. Prevalence of externalizing and internalizing disorders and socioemotional developmental delays in a representative sample of 4- and 5-year-old preschool children in Embu das Artes, state of São Paulo, Brazil, stratified by sex.
| Total (n=1,292) | Female (n=622) | Male (n=670) | |||||
|---|---|---|---|---|---|---|---|
| n (%) | 95%CI | n (%) | 95%CI | n (%) | 95%CI | p-value | |
| Child Behavior Checklist (CBCL) | < 0.001 | ||||||
| Externalizing disorders (total) | |||||||
| Normal | 1,057 (81.8) | 81.1-82.5 | 526 (84.5) | 83.6-85.4 | 530 (79.2) | 78.2-80.1 | |
| Subclinical | 80 (6.2) | 5.8-6.6 | 35 (5.6) | 4.9-6.3 | 45 (6.7) | 6.4-7.1 | |
| Clinical | 156 (12.1) | 11.5-12.6 | 62 (9.9) | 9.4-10.4 | 94 (14.1) | 13.1-15.1 | |
| Attention problems | < 0.001 | ||||||
| Normal | 1,139 (88.1) | 87.5-88.7 | 567 (91.1) | 90.3-91.9 | 571 (85.3) | 84.3-86.3 | |
| Subclinical | 88 (6.8) | 6.4-7.2 | 31 (5.0) | 4.4-5.7 | 57 (8.5) | 7.7-9.3 | |
| Clinical | 66 (5.1) | 4.8-5.4 | 24 (3.9) | 3.5-4.3 | 42 (6.2) | 5.7-6.8 | |
| Aggressive behavior | < 0.001 | ||||||
| Normal | 1,158 (89.6) | 89.2-90.0 | 569 (91.5) | 90.8-92 | 589 (87.9) | 87-88.7 | |
| Subclinical | 79 (6.1) | 5.8-6.6 | 35 (5.6) | 5.1-6.3 | 44 (6.6) | 6.0-7.3 | |
| Clinical | 55 (4.2) | 3.9-4.6 | 18 (2.9) | 2.5-3.4 | 37 (5.5) | 4.8-6.3 | |
| Internalizing disorders (total) | 0.010 | ||||||
| Normal | 757 (58.6) | 57.5-59.6 | 355 (57.0) | 55.6-58.4 | 402 (60.0) | 58.7-61.3 | |
| Subclinical | 207 (16.0) | 15.3-16.8 | 106 (17.1) | 15.8-18.5 | 101 (15.1) | 14.1-16.1 | |
| Clinical | 328 (25.4) | 24.7-26.1 | 161 (25.9) | 25.0-26.8 | 167 (24.9) | 24.0-25.9 | |
| Emotionally reactive | 0.025 | ||||||
| Normal | 972 (75.3) | 74.5-76.0 | 472 (75.8) | 75.0-76.7 | 500 (74.7) | 73.6-75.8 | |
| Subclinical | 198 (15.3) | 14.7-16.0 | 97 (15.6) | 14.6-16.6 | 101 (15.1) | 14.2-16.0 | |
| Clinical | 122 (9.4) | 8.9-9.9 | 53 (8.6) | 7.8-9.4 | 68 (10.2) | 9.4-11.1 | |
| Anxiety/depression | 0.087 | ||||||
| Normal | 1,010 (78.1) | 77.5-78.8 | 483 (77.6) | 76.8-78.4 | 526 (78.6) | 77.6-79.6 | |
| Subclinical | 176 (13.6) | 13.1-14.1 | 89 (14.2) | 13.4-15.1 | 87 (13.0) | 12.5-13.6 | |
| Clinical | 107 (8.2) | 7.7-8.8 | 51 (8.1) | 7.7-8.6 | 56 (8.4) | 7.5-9.3 | |
| Somatic complaints | < 0.001 | ||||||
| Normal | 992 (76.8) | 76.2-77.4 | 460 (73.9) | 72.9-74.9 | 532 (79.5) | 78.3-80.5 | |
| Subclinical | 199 (15.4) | 14.9-16.0 | 97 (15.6) | 14.8-16.5 | 102 (15.2) | 14.3-16.3 | |
| Clinical | 101 (7.8) | 7.4-8.2 | 65 (10.4) | 9.8-11.2 | 36 (5.3) | 4.9-5.8 | |
| Withdrawn | < 0.001 | ||||||
| Normal | 1,140 (88.2) | 87.7-88.8 | 566 (90.9) | 90.2-91.7 | 574 (85.7) | 84.8-86.6 | |
| Subclinical | 46 (3.6) | 3.2-4.0 | 21 (3.4) | 2.9-4.0 | 25 (3.7) | 3.3-4.2 | |
| Clinical | 105 (8.2) | 7.7-8.7 | 35 (5.6) | 5.1-6.2 | 71 (10.5) | 9.7-11.5 | |
| Sleep problems | 0.030 | ||||||
| Normal | 1,238 (95.8) | 95.5-96.1 | 594 (95.4) | 95-95.8 | 644 (96.1) | 95.6-96.6 | |
| Subclinical | 13 (1.0) | 0.9-1.2 | 8 (1.3) | 1.0-1.6 | 5 (0.7) | 0.5-1.0 | |
| Clinical | 41 (3.2) | 2.9-3.5 | 21 (3.3) | 2.9-3.8 | 21 (3.1) | 2.7-3.6 | |
| Ages and Stages Questionnaires: Social-Emotional (ASQ:SE) | |||||||
| Socioemotional development delays | < 0.001 | ||||||
| Low risk | 628 (49.8) | 48.9-50.8 | 324 (25.7) | 24.8-26.6 | 304 (24.2) | 23.2-25.2 | |
| Monitor zone | 254 (19.9) | 19.0-20.7 | 130 (9.9) | 9.1-10.7 | 124 (10.0) | 9.6-10.4 | |
| High risk | 387 (30.3) | 29.4-31.2 | 162 (12.5) | 11.9-12.3 | 225 (17.7) | 17.1-18.4 | |
95%CI = 95% confidence interval; CBCL = Child Behavior Checklist; ASQ:SE = Ages and Stages Questionnaires: Social-Emotional30.
Absolute and relative frequencies are weighted. The sum of subgroups may not coincide with the total due the weighting. p-level description of the chi-square test considering the sampling plan.
Bold type denotes significance at p < 0.05.
Associations of internalizing and externalizing disorders and socioemotional development delays with micro-, meso- and macrosystem variables
The results for each of the steps in the hierarchical mixed-effects logistic regression models as well as the final model are presented in Table 4. For the final model, internalizing disorders were significantly associated with parental stress and psychopathology, social capital and support, and social disorders in the neighborhood. Regarding externalizing disorders, associations were with male sex, non-white race, low SES, parental stress and psychopathology, and social capital. Socioemotional development delays were associated with male sex, non-white race, high SES, parental psychopathology, social capital and support, and social disorders. Notably, the most significant association was between internalizing and externalizing disorders and clinical parental stress.
Table 4. Hierarchical logistic regression for factors associated with externalizing and internalizing disorders and socioemotional developmental delays in a representative sample of 4- and 5-year-old preschool children in Embu das Artes, state of São Paulo, Brazil (n=1,292).
| Step 1 | Step 2 | Step 3 | Final model | |||||
|---|---|---|---|---|---|---|---|---|
| OR (95%CI) | p-value | OR (95%CI) | p-value | OR (95%CI) | p-value | OR (95%CI) | p-value | |
| Internalizing disorders | ||||||||
| Constant* | 0.20 (0.14-0.30) | < 0.001 | 0.65 (0.33-1.28) | 0.22 | 0.38 (0.18-0.83) | 0.01 | 0.42 (0.20-0.90) | 0.03 |
| Microsystem variables | ||||||||
| Female (vs. male) | 1.16 (0.88-1.55) | 0.30 | ||||||
| Race (white vs. non-white) | 0.86 (0.64-1.14) | 0.29 | ||||||
| Socioeconomic status (middle class) | ||||||||
| High | 1.00 (0.61-1.63) | 0.98 | ||||||
| Low | 0.83 (0.60-1.15) | 0.27 | ||||||
| Parental stress (typical stress) | ||||||||
| High | 3.30 (1.82-5.99) | < 0.001 | 3.13 (1.73-5.66) | < 0.001 | 3.04 (1.68-5.51) | < 0.001 | 3.13 (1.73-5.67) | < 0.001 |
| Clinical | 21.56 (6.14-75.77) | < 0.001 | 27.55 (6.24-121.67) | < 0.001 | 27.17 (6.19-119.15) | < 0.001 | 27.60 (6.31-120.75) | < 0.001 |
| Parental psychopathology† (no vs. yes) | 3.60 (2.67-4.85) | < 0.001 | 3.11 (2.30-4.20) | < 0.001 | 2.83 (2.08-3.84) | < 0.001 | 2.93 (2.17-3.97) | < 0.001 |
| Mesosystem variables‡ | ||||||||
| Social support | 0.99 (0.98-1.00) | 0.02 | 0.99 (0.98-1.00) | 0.03 | 0.99 (0.98-1.00) | 0.02 | ||
| Social capital | 0.98 (0.97-1.00) | 0.01 | 0.98 (0.97-1.00) | 0.01 | 0.98 (0.97-1.00) | 0.01 | ||
| Macrosystem variables‡ | ||||||||
| Social disorder | 1.02 (1.00-1.04) | 0.056 | 1.03 (1.01-1.04) | 0.01 | ||||
| Cultural disorder | 1.03 (1.00-1.07) | 0.06 | ||||||
| Mixed-effect logistic regression parameters | ||||||||
| Number of observations | 1,209 | 1,177 | 1,176 | 1,176 | ||||
| Log likelihood | -607.72 | -586.54 | -581.44 | -583.17 | ||||
| Wald chi-square | 121.84 | 120.86 | 130.1 | 128.70 | ||||
| Prob > chi-square | 0.0000 | 0.0000 | 0.000 | 0.000 | ||||
| Externalizing disorders | ||||||||
| Constant* | 0.14 (0.08-0.22) | < 0.001 | 0.17 (0.05-0.53) | 0.002 | 0.16 (0.07-0.38) | < 0.001 | 0.24 (0.12-0.50) | < 0.001 |
| Microsystem variables | ||||||||
| Female (vs. male) | 0.64 (0.43-0.95) | 0.03 | 0.51 (0.33-0.78) | 0.01 | 0.50 (0.32-0.77) | 0.01 | 0.50 (0.33-0.78) | 0.01 |
| Race (white vs. non-white) | 0.59 (0.39-0.89) | 0.01 | 0.60 (0.39-0.94) | 0.03 | 0.60 (0.39-0.93) | 0.02 | 0.61 (0.39-0.94) | 0.03 |
| Socioeconomic status (middle class) | ||||||||
| High | 1.19 (0.64-2.19) | 0.58 | 1.14 (0.59-2.20) | 0.70 | 1.15 (0.60-2.20) | 0.69 | 1.09 (0.57-2.09) | 0.79 |
| Low | 0.60 (0.38-0.94) | 0.03 | 0.56 (0.35-0.90) | 0.02 | 0.55 (0.34-0.89) | 0.01 | 0.55 0.34-0.88) | 0.01 |
| Parental stress (typical stress) | ||||||||
| High | 4.21 (2.21-8.03) | < 0.001 | 4.30 (2.16-8.57) | < 0.001 | 4.11 (2.06-8.18) | < 0.001 | 4.19 (2.12-8.31) | < 0.001 |
| Clinical | 41.2 (14.60-116.10) | < 0.001 | 44.44 (15.23-129.68) | < 0.001 | 41.77 (14.46-120.69) | < 0.001 | 42.24 (14.63-121.97) | < 0.001 |
| Parental psychopathology† (no vs. yes) | 2.17 (1.44-3.27) | < 0.001 | 2.4 3(1.57-3.77) | < 0.001 | 2.20 (1.42-3.42) | < 0.001 | 2.35 (1.53-3.62) | < 0.001 |
| Mesosystem variables‡ | ||||||||
| Social support | 1.01 (0.99-1.02) | 0.42 | ||||||
| Social capital | 0.98 (0.96-1.00) | 0.02 | 0.98 (0.96-1.00) | 0.03 | 0.98 (0.96-1.00) | 0.02 | ||
| Macrosystem variables‡ | ||||||||
| Social disorder | 1.03 (1.00-1.06) | 0.08 | ||||||
| Cultural disorder | 1.00 (0.95-1.05) | 0.90 | ||||||
| Mixed-effect logistic regression parameters | ||||||||
| Number of observations | 1,209 | 1,167 | 1,166 | 1,167 | ||||
| Log likelihood | -363.70 | -330.74 | -329.36 | -331.08 | ||||
| Wald chi-square | 106.12 | 106.03 | 107.69 | 106.11 | ||||
| Prob > chi-square | 0.0000 | 0.0000 | 0.0000 | 0.0000 | ||||
| Socioemotional development delays | ||||||||
| Constant* | 0.33 (0.23-0.47) | < 0.001 | 1.17 (0.57-2.43) | 0.67 | 0.75 (0.34-1.68) | 0.49 | 0.80 (0.36-1.77) | 0.58 |
| Microsystem variables | ||||||||
| Female (vs. male) | 0.64 (0.48-0.84) | 0.01 | 0.59 (0.44-0.77) | < 0.001 | 0.58 (0.44-0.76) | < 0.001 | 0.58 (0.44-0.76) | < 0.001 |
| Race (white vs. non-white) | 0.72 (0.55-0.96) | 0.02 | 0.75 (0.57-0.98) | 0.04 | 0.75 (0.57-0.99) | 0.04 | 0.75 (0.57-0.99) | 0.04 |
| Socioeconomic status (middle class) | ||||||||
| High | 1.87 (1.17-2.98) | 0.01 | 2.18 (1.36-3.48) | 0.01 | 2.22 (1.39-3.57) | 0.01 | 2.27 (1.42-3.64) | 0.01 |
| Low | 1.07 (0.78-1.48) | 0.67 | 1.16 (0.84-1.60) | 0.37 | 1.17 (0.85-1.62) | 0.35 | 1.17 (0.84-1.62) | 0.35 |
| Parental stress (typical stress) | ||||||||
| High | 3.97 (2.13-7.41) | < 0.001 | ||||||
| Clinical | § | § | § | |||||
| Parental psychopathology† (no vs. yes) | 2.84 (2.12-3.80) | < 0.001 | 3.13 (2.35-4.17) | < 0.001 | 2.89 (2.16-3.87) | < 0.001 | 2.96 (2.21-3.96) | < 0.001 |
| Mesosystem variables‡ | ||||||||
| Social support | 0.99 (0.98-1.00) | 0.01 | 0.99 (0.98-1.00) | 0.01 | 0.99 (0.98-1.00) | 0.01 | ||
| Social capital | 0.99 (0.97-1.00) | 0.03 | 0.99 (0.98-1.00) | 0.04 | 0.99 (0.98-1.00) | 0.04 | ||
| Macrosystem variables‡ | ||||||||
| Social disorder | 1.02 (1.00-1.04) | 0.07 | 1.02 (1.00-1.04) | 0.02 | ||||
| Cultural disorder | 1.02 (0.99-1.06) | 0.18 | ||||||
| Mixed-effect logistic regression parameters | ||||||||
| Number of observations | 1,186 | 1,146 | 1,145 | 1,145 | ||||
| Log likelihood | -640.16 | -639.93 | -636.17 | -637.07 | ||||
| Wald chi-square | 103.52 | 118.71 | 122.38 | 122.37 | ||||
| Prob > chi-square | 0.0000 | 0.0000 | 0.0000 | 0.0000 | ||||
We present three multilevel mixed-effect regression models, as discussed. For each variable of the regression, we provide the odds ratio (OR), 95% confidence interval (95%CI), and p-value. In the mixed-effect logistic regression parameters section, we included total number of observations, log likelihood, Wald chi-square and Prob > chi-square (the probability of getting a logistic regression test statistic under the null hypothesis, i.e., that all of the regression coefficients in the model are equal to zero).
Bold type denotes significance at p < 0.05.
Constant or intercept.
Parental psychopathology comprised depression and/or anxiety disorders.
Continuing scores.
For socioemotional delays, we were not able to calculate the association with the clinical parental stress because only one child with normal socioemotional development was in the clinical level of parental stress.
Discussion
In the Brazilian Preschool Mental Health Study, 6-month prevalence estimates of 25.4, 12.1, and 30.3% were recorded for internalizing disorders, externalizing disorders, and socioemotional development delays, respectively. Children with mental, behavioral, or developmental disorders (MBDD) faced higher parental stress, parental psychopathology (depression and/or anxiety), and lower social capital than children without MBDD. Moreover, children with internalizing disorders and socioemotional development delays had lower social support and social disorders in the neighborhood than children without these mental problems.
Overall MBDD prevalence estimates in preschool children have been reported to range from 5 to 26.7% worldwide.8,31-33 These rates vary depending on data collection methods (such as telephone survey or face-to-face interview), type of informant (child or parent), instruments used, and type of sample assessed (e.g., age range).8,31 In the Brazilian birth cohort established in the city of Pelotas (south of Brazil), approximately 13% of 3,585 children aged 6 years presented a psychiatric DSM-IV diagnosis when assessed using the Development and Well-Being Assessment (DAWBA) scale, an instrument with structured and open-ended questions answered by the parents.34 Other LMIC samples in the 4-6 year age range were observed to have similar MBDD prevalence estimates (19.2% in Sri Lanka,35 22.4% in India,36 and 26.7% in Peru37) based on structured interviews such as CBCL. Conversely, MBDD prevalence was lower in HICs: 15.2 to 15.4% in urban areas in the United States38 and 16.2% in Lithuania.39 Nonetheless, MBDD prevalence estimates that were similar to the estimates observed in the present study have been reported in school age children worldwide, ranging from 13.1 to 26.4%,40,41 as well as in other samples in Brazil.41-44 Interestingly, a Brazilian sample including 479 children aged 6-17 years living in Embu das Artes in 2003 presented a prevalence of 24.6% (20.7-28.5) for internalizing and externalizing disorders without considering global impairment; however, the estimate was only 7.3% (5.0-9.6) when global impairment needing treatment was also considered.45 In fact, MBDD starts early in life, with more than half of adult mental illness beginning prior to age 14.46 It should be noted that adequate treatment is not provided to 81% of 6-12 year old Brazilian children with mental disorders.22
It is noteworthy that the prevalence of delayed socioemotional development in our sample (30.3%) was two to three times higher than that detected in U.S. samples using the ASQ-SE (ranging from 7.5 to 12.5%).47,48
In our sample, children with MBDD faced higher parental stress, parental psychopathology, and lower social capital. Accordingly, in a study of 12,347 children aged 11 years from the UK Millennium Cohort Study, 47% of the variance in mental disorder symptoms were explained by parental health, cognitive ability, SES, home environment, social relations, and general health variables.49 Good quality parent-child relationships may promote resilience against different types of environmental risk in children.50 Adaptive parent child-relationships (e.g., affectionate and supportive parenting) and parental social support can mitigate the development of child mental health problems by buffering the effects of exposure to adversities such as violence.51 Positive parenting, parental responsiveness, and warmth have consistently been linked to lower internalizing and externalizing symptoms among youth,52 while harsh and authoritarian parenting can exacerbate child behavior problems over time.51
Children with internalizing disorders and socioemotional development delays had lower social support and social disorders in the neighborhood. In the UK Millennium Cohort Study, neighborhood deprivation was associated with peer problems at preschool age.12 That study also reported that experience of persistent economic hardship and very early poverty undermined cognitive functioning at 5 years of age.53 Children exposed to poverty seem to be more vulnerable to decreased self-regulation and verbal cognitive ability, possible protective factors for young children growing up in poor families.12
The present study has limitations that need to be addressed. First, we used the CBCL, which relies on parental reports to understand child behavior and emotions rather than directly observing children in home environments. The Preschool Age Psychiatric Assessment (PAPA) is considered the gold standard structured parent interview for diagnosis of psychiatric disorders in preschool children.54 The CBCL lacks specific information about “severity, duration, onset, or context of behaviors.” However, in contrast to the PAPA, which requires 3 hours to be completed, the CBCL is shorter, easy to implement, and more economical. MBDD prevalence estimates were not significantly different using a screening questionnaire (CBCL 6-18) compared to a diagnostic instrument (Diagnostic Interview Schedule for Children [DISC], similar to PAPA).55 Additionally, the Brazilian version of the CBCL has high sensitivity (80.4%) for correctly identifying psychiatric cases.56 Since this study was conducted solely in the city of Embu das Artes, the results cannot be directly generalized to other regions with distinct sociodemographic characteristics.
In conclusion, the 6-month estimates of MBDD prevalence in 4- to 5-year-old children (25.4% for internalizing disorders, 12.1% for externalizing disorders, and 30.3% for socioemotional development delays) were high in the present study. Moreover, children with MBDD faced higher parental stress, parental depression and/or anxiety, and lower social capital than children without MBDD. Considering that at least one-fourth of preschool children living in an urban area in Brazil present a mental health problem, interventions such as parental training are needed to decrease the expected negative outcomes in later life. This study provides the baseline for a follow-up study to be performed after 5 years to examine the course of mental illness. There is a dearth of longitudinal research from developing countries using an ecological approach, and this research will fill some of those gaps.
Disclosure
SCC has received consulting fees from Pfizer and in 2019 received honoraria for lectures from Lundbeck. The other authors report no conflicts of interest.
Acknowledgements
This work was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (grant 466688/2014-8) to conduct the baseline epidemiological study, and by Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) (grant 2016/10120-1) to conduct the school evaluation (PI SCC). The project was also partially funded by the Columbia President’s Global Innovation Fund (grant UR008509; PI SSM) and by FAPESP (grant 2016/11202-1; Co-I JP). EF received a scholarship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES); MM received a scholarship from FAPESP.
We would like to thank the Embu das Artes Municipality, the Embu das Artes Secretaries of Health and Education. This research would not have been possible without the cooperation and support from the Embu das Artes school board and caregivers who participated in our study. We would like to thank Rebeca Pessoa, Clara Brandão, and Magdalena Cerda, for their help. Also we would like to thank our statistical experts: Mitti Koyama, Solange Andreoni, and Qixuan Chen.
Footnotes
How to cite this article: Caetano SC, Ribeiro MVV, Askari MS, Sanchez ZM, do Rosário MC, Perissinoto J, et al. An epidemiological study of childhood development in an urban setting in Brazil. Braz J Psychiatry. 2021;43:43-54. http://dx.doi.org/10.1590/1516-4446-2020-0934
References
- 1.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu C, Black MM, Richter LM. Risk of poor development in young children in low-income and middle-income countries: an estimation and analysis at the global, regional, and country level. Lancet Glob Health. 2016;4:e916–22. doi: 10.1016/S2214-109X(16)30266-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kessler RC, Foster CL, Saunders WB, Stang PE. Social consequences of psychiatric disorders, I: educational attainment. Am J Psychiatry. 1995;152:1026–32. doi: 10.1176/ajp.152.7.1026. [DOI] [PubMed] [Google Scholar]
- 4.Copeland WE, Shanahan L, Costello EJ, Angold A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch Gen Psychiatry. 2009;66:764–72. doi: 10.1001/archgenpsychiatry.2009.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paula CS, Mari JJ, Bordin IAS, Miguel EC, Fortes I, Barroso N, et al. Early vulnerabilities for psychiatric disorders in elementary schoolchildren from four Brazilian regions. Soc Psychiatry Psychiatr Epidemiol. 2018;53:477–86. doi: 10.1007/s00127-018-1503-4. [DOI] [PubMed] [Google Scholar]
- 6.Flouri E, Midouhas E, Joshi H, Sullivan A. Neighbourhood social fragmentation and the mental health of children in poverty. Health Place. 2015;31:138–45. doi: 10.1016/j.healthplace.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 7.Anselmi L, Barros FC, Teodoro ML, Piccinini CA, Menezes AM, Araujo CL, et al. Continuity of behavioral and emotional problems from pre-school years to pre-adolescence in a developing country. J Child Psychol Psychiatry. 2008;49:499–507. doi: 10.1111/j.1469-7610.2007.01865.x. [DOI] [PubMed] [Google Scholar]
- 8.Lavigne JV, Arend R, Rosenbaum D, Binns HJ, Christoffel KK, Gibbons RD. Psychiatric disorders with onset in the preschool years: I. Stability of diagnoses. J Am Acad Child Adolesc Psychiatry. 1998;37:1246–54. doi: 10.1097/00004583-199812000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301:386–9. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- 10.Weissman MM, Warner V, Wickramaratne P, Moreau D, Olfson M. Offspring of depressed parents. 10 years later. Arch Gen Psychiatry. 1997;54:932–40. doi: 10.1001/archpsyc.1997.01830220054009. [DOI] [PubMed] [Google Scholar]
- 11.Jones DE, Greenberg M, Crowley M. Early social-emotional functioning and public health: the relationship between kindergarten social competence and future wellness. Am J Public Health. 2015;105:2283–90. doi: 10.2105/AJPH.2015.302630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flouri E, Mavroveli S, Tzavidis N. Cognitive ability, neighborhood deprivation, and young children’s emotional and behavioral problems. Soc Psychiatry Psychiatr Epidemiol. 2012;47:985–92. doi: 10.1007/s00127-011-0406-4. [DOI] [PubMed] [Google Scholar]
- 13.Bronfenbrenner U. Ecology of the family as a context for human development: research perspectives. Dev Psychol. 1986;22:723–42. [Google Scholar]
- 14.Coatsworth JD, Pantin H, Szapocznik J. Familias Unidas: a family-centered ecodevelopmental intervention to reduce risk for problem behavior among Hispanic adolescents. Clin Child Fam Psychol Rev. 2002;5:113–32. doi: 10.1023/a:1015420503275. [DOI] [PubMed] [Google Scholar]
- 15.Bordin IA, Paula CS, do Nascimento R, Duarte CS. Severe physical punishment and mental health problems in an economically disadvantaged population of children and adolescents. Braz J Psychiatry. 2006;28:290–6. doi: 10.1590/s1516-44462006000400008. [DOI] [PubMed] [Google Scholar]
- 16.Goodman A, Fleitlich-Bilyk B, Patel V, Goodman R. Child, family, school and community risk factors for poor mental health in Brazilian schoolchildren. J Am Acad Child Adolesc Psychiatry. 2007;46:448–56. doi: 10.1097/chi.0b013e31803065b5. [DOI] [PubMed] [Google Scholar]
- 17.Bordin IA, Duarte CS, Peres CA, Nascimento R, Curto BM, Paula CS. Severe physical punishment: risk of mental health problems for poor urban children in Brazil. Bull World Health Organ. 2009;87:336–44. doi: 10.2471/BLT.07.043125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fleitlich-Bilyk B, Goodman R. Prevalence of child and adolescent psychiatric disorders in southeast Brazil. J Am Acad Child Adolesc Psychiatry. 2004;43:727–34. doi: 10.1097/01.chi.0000120021.14101.ca. [DOI] [PubMed] [Google Scholar]
- 19.Vitolo YL, Fleitlich-Bilyk B, Goodman R, Bordin IA. [Parental beliefs and child-rearing attitudes and mental health problems among schoolchildren] Rev Saude Publica. 2005;39:716–24. doi: 10.1590/s0034-89102005000500004. [DOI] [PubMed] [Google Scholar]
- 20.Richter LM, Daelmans B, Lombardi J, Heymann J, Boo FL, Behrman JR, et al. Investing in the foundation of sustainable development: pathways to scale up for early childhood development. Lancet. 2017;389:103–18. doi: 10.1016/S0140-6736(16)31698-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378:1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 22.Fatori D, Salum GA, Rohde LA, Pan PM, Bressan R, Evans-Lacko S, et al. Use of mental health services by children with mental disorders in two major cities in Brazil. Psychiatr Serv. 2019;70:337–41. doi: 10.1176/appi.ps.201800389. [DOI] [PubMed] [Google Scholar]
- 23.Costello EJ, Egger H, Angold A. 10-year research update review: the epidemiology of child and adolescent psychiatric disorders: I. Methods and public health burden. J Am Acad Child Adolesc Psychiatry. 2005;44:972–86. doi: 10.1097/01.chi.0000172552.41596.6f. [DOI] [PubMed] [Google Scholar]
- 24.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–89. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 25.Blewitt C, Fuller-Tyszkiewicz M, Nolan A, Bergmeier H, Vicary D, Huang T, et al. Social and emotional learning associated with universal curriculum-based interventions in early childhood education and care centers: a systematic review and meta-analysis. JAMA Netw Open. 2018;1:e185727. doi: 10.1001/jamanetworkopen.2018.5727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buchanan-Pascall S, Gray KM, Gordon M, Melvin GA. Systematic review and meta-analysis of parent group interventions for primary school children aged 4-12 years with externalizing and/or internalizing problems. Child Psychiatry Hum Dev. 2018;49:244–67. doi: 10.1007/s10578-017-0745-9. [DOI] [PubMed] [Google Scholar]
- 27.Estado de São Paulo, Assembleia Legislativa do Estado de São Paulo ĺndice Paulista de Vulnerabilidade Social – IPVS versão 2010 [Internet] 2010 [cited 2015 Oct 4]. https://ipvs.seade.gov.br/view/index.php. [Google Scholar]
- 28.Deepask Violence in the cities of Brazil: number of murders and homicide rate per 100 thousand inhabitants – EMBU DAS ARTES, SP [Internet] 2015 [cited 2015 Oct 4]. https://www.deepask.com/goes?page=embu-das-artes/SP-Violence-in-the-cities-of-Brazil:-Number-of-murders-and-homicide-rate-per-100-thousand-inhabitants. [Google Scholar]
- 29.Agresti A. Categorical data analysis. 3rd ed. Hoboken: Wiley; 2013. [Google Scholar]
- 30.Squires J, Bricker D, Twombly E. Ages and stages questionnaires: social emotional. Baltimore: Brookes; 2002. [Google Scholar]
- 31.Brauner CB, Stephens CB. Estimating the prevalence of early childhood serious emotional/behavioral disorders: challenges and recommendations. Public Health Rep. 2006;121:303–10. doi: 10.1177/003335490612100314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Earls F. Application of DSM-III in an epidemiological study of preschool children. Am J Psychiatry. 1982;139:242–3. doi: 10.1176/ajp.139.2.242. [DOI] [PubMed] [Google Scholar]
- 33.Keenan K, Shaw DS, Walsh B, Delliquadri E, Giovannelli J. DSM-III-R disorders in preschool children from low-income families. J Am Acad Child Adolesc Psychiatry. 1997;36:620–7. doi: 10.1097/00004583-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 34.Petresco S, Anselmi L, Santos IS, Barros AJ, Fleitlich-Bilyk B, Barros FC, et al. Prevalence and comorbidity of psychiatric disorders among 6-year-old children: 2004 Pelotas Birth Cohort. Soc Psychiatry Psychiatr Epidemiol. 2014;49:975–83. doi: 10.1007/s00127-014-0826-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Samarakkody D, Fernando D, McClure R, Perera H, De Silva H. Prevalence of externalizing behavior problems in Sri Lankan preschool children: birth, childhood, and sociodemographic risk factors. Soc Psychiatry Psychiatr Epidemiol. 2012;47:757–62. doi: 10.1007/s00127-011-0377-5. [DOI] [PubMed] [Google Scholar]
- 36.Bele SD, Bodhare TN, Valsangkar S, Saraf A. An epidemiological study of emotional and behavioral disorders among children in an urban slum. Psychol Health Med. 2013;18:223–32. doi: 10.1080/13548506.2012.701751. [DOI] [PubMed] [Google Scholar]
- 37.Westgard C, Alnasser Y. Developmental delay in the Amazon: the social determinants and prevalence among rural communities in Peru. PLoS One. 2017;12:e0186263. doi: 10.1371/journal.pone.0186263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robinson LR, Holbrook JR, Bitsko RH, Hartwig SA, Kaminski JW, Ghandour RM, et al. Differences in health care, family, and community factors associated with mental, behavioral, and developmental disorders among children aged 2-8 years in rural and urban areas – United States, 2011-2012. MMWR Surveill Summ. 2017;66:1–11. doi: 10.15585/mmwr.ss6608a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Grazuleviciene R, Andrusaityte S, Petraviciene I, Balseviciene B. Impact of psychosocial environment on young children’s emotional and behavioral difficulties. Int J Environ Res Public Health. 2017;14:e1278. doi: 10.3390/ijerph14101278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–44. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 41.Husky MM, Boyd A, Bitfoi A, Carta MG, Chan-Chee C, Goelitz D, et al. Self-reported mental health in children ages 6-12 years across eight European countries. Eur Child Adolesc Psychiatry. 2018;27:785–95. doi: 10.1007/s00787-017-1073-0. [DOI] [PubMed] [Google Scholar]
- 42.La Maison C, Munhoz TN, Santos IS, Anselmi L, Barros FC, Matijasevich A. Prevalence and risk factors of psychiatric disorders in early adolescence: 2004 Pelotas (Brazil) birth cohort. Soc Psychiatry Psychiatr Epidemiol. 2018;53:685–97. doi: 10.1007/s00127-018-1516-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paula CS, Coutinho ES, Mari JJ, Rohde LA, Miguel EC, Bordin IA. Prevalence of psychiatric disorders among children and adolescents from four Brazilian regions. Braz J Psychiatry. 2015;37:178–9. doi: 10.1590/1516-4446-2014-1606. [DOI] [PubMed] [Google Scholar]
- 44.Bordin IA, Curto BM, Murray J. Maternal recognition of child mental health problems in two Brazilian cities. Braz J Psychiatry. 2018;40:63–71. doi: 10.1590/1516-4446-2016-1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paula CS, Duarte CS, Bordin IA. Prevalence of mental health problems in children and adolescents from the outskirts of Sao Paulo city: treatment needs and service capacity evaluation. Braz J Psychiatry. 2007;29:11–7. doi: 10.1590/s1516-44462007000100006. [DOI] [PubMed] [Google Scholar]
- 46.Kessler RC, Amminger GP, Aguilar-Gaxiola S, Alonso J, Lee S, Ustün TB. Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry. 2007;20:359–64. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hunter LR, Lynch BA. Impact of implementing mental health screening by mail with a primary care management model. J Prim Care Community Health. 2014;5:9–13. doi: 10.1177/2150131913484340. [DOI] [PubMed] [Google Scholar]
- 48.Nguyen DR, Ee J, Berry-Caban CS, Hoedebecke K. The effects of military deployment on early child development. US Army Med Dep J. 2014:81–6. [PubMed] [Google Scholar]
- 49.Patalay P, Fitzsimons E. Correlates of mental illness and wellbeing in children: are they the same? Results from the UK Millennium Cohort Study. J Am Acad Child Adolesc Psychiatry. 2016;55:771–83. doi: 10.1016/j.jaac.2016.05.019. [DOI] [PubMed] [Google Scholar]
- 50.Flouri E, Midouhas E, Joshi H, Tzavidis N. Emotional and behavioural resilience to multiple risk exposure in early life: the role of parenting. Eur Child Adolesc Psychiatry. 2015;24:745–55. doi: 10.1007/s00787-014-0619-7. [DOI] [PubMed] [Google Scholar]
- 51.Pettit GS, Bates JE, Dodge KA. Supportive parenting, ecological context, and children’s adjustment: a seven-year longitudianl study. Child Dev. 1997;68:908–23. doi: 10.1111/j.1467-8624.1997.tb01970.x. [DOI] [PubMed] [Google Scholar]
- 52.Bakoula C, Kolaitis G, Veltsista A, Gika A, Chrousos GP. Parental stress affects the emotions and behaviour of children up to adolescence: a Greek prospective, longitudinal study. Stress. 2009;12:486–98. doi: 10.3109/10253890802645041. [DOI] [PubMed] [Google Scholar]
- 53.Schoon I, Jones E, Cheng H, Maughan B. Family hardship, family instability, and cognitive development. J Epidemiol Community Health. 2012;66:716–22. doi: 10.1136/jech.2010.121228. [DOI] [PubMed] [Google Scholar]
- 54.Egger HL, Angold A. The Preschool Age Psychiatric Assessment (PAPA): a structured parent interview for diagnosing psychiatric disorders in preschool children. In: DelCarmen-Wiggins R, Carter AS, editors. Handbook of infant, toddler, and preschool mental health assessment. New York: Oxford University Press; 2004. pp. p. 223–43. [Google Scholar]
- 55.Douma JCH, Dekker MC, De Ruiter KP, Maughan B, Koot HM. Help-seeking process of parents for psychopathology in youth with moderate to borderline intellectual disabilities. J Am Acad Child Adolesc Psychiatry. 2006;45:1232–42. doi: 10.1097/01.chi.0000230167.31246.db. [DOI] [PubMed] [Google Scholar]
- 56.Bordin IAS, Mari JJ, Caeiro MF. Validação da versão brasileira do Child Behavior Checklist (CBCL) (Inventário de Comportamentos da Infância e Adolescência): dados preliminares. Rev ABP-APAL. 1997;17:55–66. [Google Scholar]