Abstract
Functional activation of human epidermal growth factor receptor 2 (HER2) has been shown to strongly promote carcinogenesis, leading to the investigation of HER2-directed agents in cancers with HER2 genomic alterations. This has been best documented in the context of HER2 gene amplification in breast and gastric/gastroesophageal junction carcinomas for which several HER2-directed agents are available and have become a part of standard treatment regimens. Somatic HER2 gene mutations have been recently described at low frequency in a variety of human cancers and have emerged as a novel predictive biomarker for HER2-directed therapies. Preclinical data also indicate that activating HER2 mutations are potent oncogenic drivers in a manner that is analogous to HER2 amplification. HER2 mutations may clinically confer sensitivity to HER2-directed agents as recently shown in a phase II clinical trial with antibody-drug conjugate against HER2 trastuzumab deruxtecan in patients with non-squamous non-small cell lung carcinoma.
Keywords: HER2, targeted therapy, mutations, amplification
The oncogenic potential and activation of human epidermal growth factor receptor 2 (HER2) has been well established in several human malignancies, most notably in breast and gastric/gastroesophageal junction (GEJ) carcinomas. The primary mechanism of the HER2 activation in these cancers is HER2 gene amplification that leads to the complete HER2 protein overexpression on the cellular membrane [1,2]. In recent years, other genomic alterations of HER2 have also been recognized leading to protein activation among which HER2 gene mutations represent the most important form [3]. HER2 mutations are usually of activating type and the majority of them are seen without concurrent HER2 gene amplification [3-5]. The highest prevalence (>10%) of HER2 mutations has been observed in prostate neuroendocrine carcinomas, metastatic cutaneous squamous cell carcinomas and urothelial bladder carcinoma. Additionally, HER2 mutations have also been reported in common cancers such as pulmonary, colorectal and breast cancers, indicating a potential for HER2-directed therapies in these cancers [4,6-12]. HER2 mutations are enriched in certain specific histological subtypes, for instance in invasive lobular carcinoma of the breast (5-18%) [13-15] and in ~2-3% of pulmonary adenocarcinomas [16-21]. Recently, HER2 mutations were reported to occur more frequently in microsatellite instable (MSI-H) colorectal carcinomas than in microsatellite stable (MSS) cases [10, 11]. HER2 genomic alterations were also enriched in RAS wild-type and anti-EGFR therapy resistant colorectal carcinomas [22]. Studies in non-small cell lung carcinomas (NSCLC) revealed mutations affecting predominantly exon 20 and were seen without amplification of HER2 gene. In addition, HER2 mutations were mutually exclusive with other common oncogenic drivers in NSCLC. In contrast to epidermal growth factor receptor (EGFR) mutations, the frequency of HER2 mutations appear to be similar between Asian and Caucasian populations [16].
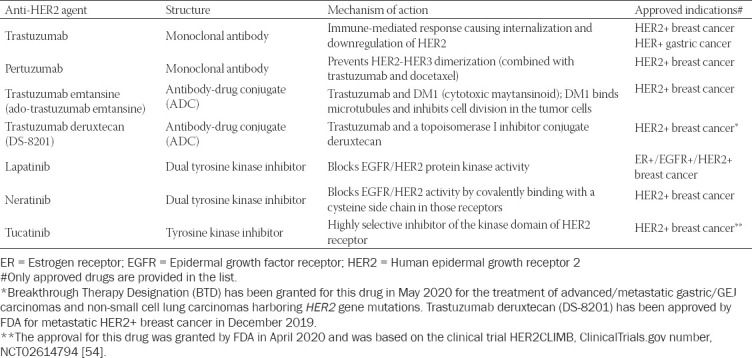
The anti-HER2 antibody trastuzumab has been a cornerstone and effective therapy in treatment of HER2-positive breast and gastric cancers. However, the number of approved anti-HER2 therapeutic agents has been markedly expanded in recent years, with the addition of tyrosine kinase inhibitors (lapatinib, neratinib, tucatinib), antibodies (pertuzumab), and antibody-drug conjugates [ado-trastuzumab emtansine (T-DM1)] and trastuzumab deruxtecan (DS-8201)] (summarized in Table 1) [3]. Used alone or in combination with other targeting agents or conventional chemotherapeutics, these anti-HER2 agents have remarkably improved the outcome of patients with HER2-positive breast cancer [23, 24].
Table 1.
Overview of the anti-HER2 agents that have been approved in breast and gastric cancers
One of the most recent antibody-drug conjugates (ADC) against HER2 is trastuzumab deruxtecan (Enhertu; DS-8201; AstraZeneca and Daiichi Sankyo Company, Limited (Daiichi Sankyo). It is composed of an anti-HER2 antibody (trastuzumab), a cleavable tetrapeptide-based linker, and a cytotoxic topoisomerase I (TOP1) inhibitor (“payload”) (Table 1). Previously, it was published that TOP1 was overexpressed in 63% of all invasive breast carcinomas [25]. Enhertu appears to exhibit a higher drug-to-antibody ratio than another anti-HER2 ADC trastuzumab emtansine (Kadsyla) (approximately 8 vs. 3-4) while retaining a favorable pharmacokinetic characteristics [26]. In contrast to trastuzumab emtansine, trastuzumab deruxtecan has a released payload that may easily cross the cell membrane, which potentially allows for potent cytotoxic effects on cancer cells regardless of target expression [27-29]. In addition, the released payload has a substantially shorter half-life, which may minimize systemic exposure and potential side effects [30]. In breast cancer, trastuzumab deruxtecan has been shown to exhibit a durable therapeutic activity in a population of heavily pretreated patients (≥2 prior anti–HER2-based regimens) with advanced HER2-positive breast cancer [31]. This phase 2 study (II DESTINY-Breast01 trial) revealed that a response to trastuzumab deruxtecan was achieved in 60.9% of the patients of which 6% had a complete response (CR) while 54.9% of patients had a partial response [31]. The preliminary data from the II DESTINY-Breast01 trial were presented at the San Antonio 2019 meeting [32] and led to the accelerated approval by the Food and Drug Administration (FDA) in December 2019.
The results from another ongoing trial named Phase II DESTINY-Lung01 trial have just been presented at the 2020 American Society of Clinical Oncology (ASCO) Virtual Scientific Program [33]. This trial showed that trastuzumab deruxtecan also achieved a clinically significant tumor response in patients with HER2-mutant advanced non-squamous NSCLC whose disease had progressed following one or more previous systemic therapies (chemotherapy or immunotherapy with immune checkpoint inhibitors against PD-1/PD-L1) [33]. The confirmed objective response rate (ORR) was achieved in 61.9% of patients treated with trastuzumab deruxtecan monotherapy (6.4mg/kg). A disease control rate (DCR) of 90.5% with a median progression-free survival (PFS) of 14 months were remarkable achievements in this study. However, other relevant endpoints such as a median duration of response and overall survival (OS) have not been reached at the time of data cut-off [33]. Nevertheless, these encouraging results, after many failed trials and extensive research on HER2 in NSCLC [34-36], may pave a new way for the treatment of a small subset of NSCLC harboring HER2 gene mutations. Interestingly, for the predictive purposes HER2-overexpressing non-squamous NSCLC (defined as scores 2+ and 3+ by immunohistochemistry/IHC/) or non-squamous NSCLC harboring a HER2-activating mutation, were used in this trial. From the provided abstract [33], it is not clear whether the differences in a treatment response were observed between HER2-mutant NSCLC and HER2-overexpressing NSCLC (2+ and 3+ scores by IHC). In contrast, an ongoing, phase II trial with trastuzumab deruxtecan in advanced gastric/GEJ carcinomas (DESTINY-Gastric01) enrolled only those patients whose cancers were HER2-positive (Score 3+ by IHC or 2+ IHC with confirmatory HER2 amplification by in situ hybridization assay). A clinical trial on NSCLC with ADC trastuzumab emtansine (T-DM1) reported responses to the targeted drug only in IHC 3+ NSCLC while no responses were found in 2+ NSCLC cases [37]. It is well-known that HER2 status assessed by IHC (particularly score 2+) is not an optimal approach for selection of the patients having a mutant HER2 cancer as recently shown in case of colorectal carcinoma [38]. Apart from the well-documented examples of mutation-specific IHC antibodies (e.g. BRAF p.V600E, IDH1 p.R132H, or H3K27M), which tend to correlate well with the specific mutations [39], IHC antibodies that target specific proteins may lack correlation with the DNA-level mutational events. There are several possible reasons including the fact that the mutation may not result in (increased) protein expression (e.g. due to transcriptomic silencing of genetic variant or discordance between the DNA alterations and RNA expression)[40], hence IHC may be consequently negative/low positive; another possibility is that the antibody may target a specific epitope that may or may not be altered by the mutation. In case of trastuzumab deruxtecan, another important therapeutic target is TOP1, which is inhibited by the ADC payload deruxtecan. TOP1 is an enzyme with an active role in DNA function by the cleavage one of the two backbones in double-stranded DNA enabling the double helix to be untwisted [41]. TOP1 status has been extensively studied by immunohistochemistry, most notably in colorectal carcinoma where it has been shown to predict a response to irinotecan-based chemotherapy [42,43]. It is well-known that irinotecan may reversibly stabilize the TOP1 cleavable complex, resulting in single-strand DNA breaks and ultimate cell death [44]. In addition, a high TOP1 expression has also been demonstrated in several other cancers, including small cell lung, gastric/gastroesophageal, esophageal, thymic, anal, breast, prostate and poorly differentiated neuroendocrine carcinomas [25]. The same study as well as several other studies also revealed a common TOP1 overexpression in NSCLC [45,46]. Another ADC sacituzumab govitecan-hziy (TRODELVY, Immunomedics, Inc.) was recently approved for the patients with metastatic triple-negative breast cancer (TNBC). It represents an anti-Trop-2 (=trophoblast cell-surface antigen 2) ADC and contains irinotecan metabolite, SN-38 that is conjugated to a humanized anti-TROP-2 antibody (sacituzumab govitecan) [47]. Although both Trop-2 and TOP1 expression have been well-documented in various cancers including breast cancer [25,48-52], predictive testing was not conducted in this trial (IMMU-132-01 (NCT 01631552) clinical trial [53].
In short, recent data indicate that HER2 mutations may be successfully targeted with the available anti-HER2 treatment modalities. ADC such as trastuzumab deruxtecan represent novel promising therapeutic means for the patients with advanced non-squamous NSCLC. Despite the remarkable achievements, we believe that further efforts should be made to optimize the treatment with these ADC where molecular targets are well characterized and may be easily assessed prior to targeted treatments.
Footnotes
Conflict of interest statement: The authors declare no conflict of interests
Funding: None.
REFERENCES
- 1.Yan M, Schwaederle M, Arguello D, Millis SZ, Gatalica Z, Kurzrock R. HER2 expression status in diverse cancers:review of results from 37,992 patients. Cancer Metastasis Rev. 2015;34(1):157–64. doi: 10.1007/s10555-015-9552-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389(10087):2415–29. doi: 10.1016/S0140-6736(16)32417-5. [DOI] [PubMed] [Google Scholar]
- 3.Meric-Bernstam F, Johnson AM, Dumbrava EEI, Raghav K, Balaji K, Bhatt M, et al. Advances in HER2-Targeted Therapy: Novel Agents and Opportunities Beyond Breast and Gastric Cancer. Clin Cancer Res. 2019;25(7):2033–41. doi: 10.1158/1078-0432.CCR-18-2275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Connell CM, Doherty GJ. Activating HER2 mutations as emerging targets in multiple solid cancers. ESMO Open. 2017;2(5):e000279. doi: 10.1136/esmoopen-2017-000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wen W, Chen WS, Xiao N, Bender R, Ghazalpour A, Tan Z, et al. Mutations in the Kinase Domain of the HER2/ERBB2 Gene Identified in a Wide Variety of Human Cancers. J Mol Diagn. 2015;17(5):487–95. doi: 10.1016/j.jmoldx.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrelli F, Tomasello G, Barni S, Lonati V, Passalacqua R, Ghidini M. Clinical and pathological characterization of HER2 mutations in human breast cancer: a systematic review of the literature. Breast Cancer Res Treat. 2017;166(2):339–49. doi: 10.1007/s10549-017-4419-x. [DOI] [PubMed] [Google Scholar]
- 7.Priedigkeit N, Hartmaier RJ, Chen Y, Vareslija D, Basudan A, Watters RJ, et al. Intrinsic Subtype Switching and Acquired ERBB2/HER2 Amplifications and Mutations in Breast Cancer Brain Metastases. JAMA Oncol. 2017;3(5):666–71. doi: 10.1001/jamaoncol.2016.5630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bose R, Kavuri SM, Searleman AC, Shen W, Shen D, Koboldt DC, et al. Activating HER2 mutations in HER2 gene amplification negative breast cancer. Cancer Discov. 2013;3(2):224–37. doi: 10.1158/2159-8290.CD-12-0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Greulich H, Kaplan B, Mertins P, Chen TH, Tanaka KE, Yun CH, et al. Functional analysis of receptor tyrosine kinase mutations in lung cancer identifies oncogenic extracellular domain mutations of ERBB2. Proc Natl Acad Sci U S A. 2012;109(36):14476–81. doi: 10.1073/pnas.1203201109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kloth M, Ruesseler V, Engel C, Koenig K, Peifer M, Mariotti E, et al. Activating ERBB2/HER2 mutations indicate susceptibility to pan-HER inhibitors in Lynch and Lynch-like colorectal cancer. Gut. 2016;65(8):1296–305. doi: 10.1136/gutjnl-2014-309026. [DOI] [PubMed] [Google Scholar]
- 11.Loree JM, Bailey AM, Johnson AM, Yu Y, Wu W, Bristow CA, et al. Molecular Landscape of ERBB2/ERBB3 Mutated Colorectal Cancer. J Natl Cancer Inst. 2018;110(12):1409–17. doi: 10.1093/jnci/djy067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chmielecki J, Ross JS, Wang K, Frampton GM, Palmer GA, Ali SM, et al. Oncogenic alterations in ERBB2/HER2 represent potential therapeutic targets across tumors from diverse anatomic sites of origin. Oncologist. 2015;20(1):7–12. doi: 10.1634/theoncologist.2014-0234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christgen M, Bartels S, Radner M, Raap M, Rieger L, Christgen H, et al. ERBB2 mutation frequency in lobular breast cancer with pleomorphic histology or high-risk characteristics by molecular expression profiling. Genes Chromosomes Cancer. 2019;58(3):175–85. doi: 10.1002/gcc.22716. [DOI] [PubMed] [Google Scholar]
- 14.Ross JS, Wang K, Sheehan CE, Boguniewicz AB, Otto G, Downing SR, et al. Relapsed classic E-cadherin (CDH1)-mutated invasive lobular breast cancer shows a high frequency of HER2 (ERBB2) gene mutations. Clin Cancer Res. 2013;19(10):2668–76. doi: 10.1158/1078-0432.CCR-13-0295. [DOI] [PubMed] [Google Scholar]
- 15.Ross JS, Gay LM, Wang K, Ali SM, Chumsri S, Elvin JA, et al. Nonamplification ERBB2 genomic alterations in 5605 cases of recurrent and metastatic breast cancer: An emerging opportunity for anti-HER2 targeted therapies. Cancer. 2016;122(17):2654–62. doi: 10.1002/cncr.30102. [DOI] [PubMed] [Google Scholar]
- 16.Pillai RN, Behera M, Berry LD, Rossi MR, Kris MG, Johnson BE, et al. HER2 mutations in lung adenocarcinomas: A report from the Lung Cancer Mutation Consortium. Cancer. 2017;123(21):4099–105. doi: 10.1002/cncr.30869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arcila ME, Chaft JE, Nafa K, Roy-Chowdhuri S, Lau C, Zaidinski M, et al. Prevalence, clinicopathologic associations, and molecular spectrum of ERBB2 (HER2) tyrosine kinase mutations in lung adenocarcinomas. Clin Cancer Res. 2012;18(18):4910–8. doi: 10.1158/1078-0432.CCR-12-0912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kris MG, Johnson BE, Berry LD, Kwiatkowski DJ, Iafrate AJ, Wistuba II, et al. Using multiplexed assays of oncogenic drivers in lung cancers to select targeted drugs. JAMA. 2014;311(19):1998–2006. doi: 10.1001/jama.2014.3741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Li BT, Ross DS, Aisner DL, Chaft JE, Hsu M, Kako SL, et al. HER2 Amplification and HER2 Mutation Are Distinct Molecular Targets in Lung Cancers. J Thorac Oncol. 2016;11(3):414–9. doi: 10.1016/j.jtho.2015.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tomizawa K, Suda K, Onozato R, Kosaka T, Endoh H, Sekido Y, et al. Prognostic and predictive implications of HER2/ERBB2/neu gene mutations in lung cancers. Lung Cancer. 2011;74(1):139–44. doi: 10.1016/j.lungcan.2011.01.014. [DOI] [PubMed] [Google Scholar]
- 21.Xu F, Yang G, Xu H, Yang L, Qiu W, Wang Y. Treatment outcome and clinical characteristics of HER2 mutated advanced non-small cell lung cancer patients in China. Thorac Cancer. 2020;11(3):679–85. doi: 10.1111/1759-7714.13317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.La Salvia A, Lopez-Gomez V, Garcia-Carbonero R. HER2-targeted therapy: an emerging strategy in advanced colorectal cancer. Expert Opin Investig Drugs. 2019;28(1):29–38. doi: 10.1080/13543784.2019.1555583. [DOI] [PubMed] [Google Scholar]
- 23.Baselga J, Cortes J, Kim SB, Im SA, Hegg R, Im YH, et al. Pertuzumab plus trastuzumab plus docetaxel for metastatic breast cancer. N Engl J Med. 2012;366(2):109–19. doi: 10.1056/NEJMoa1113216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verma S, Miles D, Gianni L, Krop IE, Welslau M, Baselga J, et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–91. doi: 10.1056/NEJMoa1209124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heestand GM, Schwaederle M, Gatalica Z, Arguello D, Kurzrock R. Topoisomerase expression and amplification in solid tumours:Analysis of 24,262 patients. Eur J Cancer. 2017;83:80–7. doi: 10.1016/j.ejca.2017.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jerez Y, Herrero B, Arregui M, Moron B, Martin M, Echavarria I. Neratinib for the treatment of early-stage, hormone receptor-positive, HER2-overexpressed breast cancer. Future Oncol. 2020;16(17):1165–77. doi: 10.2217/fon-2020-0046. [DOI] [PubMed] [Google Scholar]
- 27.Tolcher AW. The Evolution of Antibody-Drug Conjugates:A Positive Inflexion Point. Am Soc Clin Oncol Educ Book. 2020;40:1–8. doi: 10.1200/EDBK_281103. [DOI] [PubMed] [Google Scholar]
- 28.Staudacher AH, Brown MP. Antibody drug conjugates and bystander killing:is antigen-dependent internalisation required? Br J Cancer. 2017;117(12):1736–42. doi: 10.1038/bjc.2017.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.2019. https: //www.oncozine.com/trastuzumab-deruxtecan-approved-for-the-treatment-of-metastatic-her2-positive-breast-cancer/
- 30.File D, Curigliano G, Carey LA. Escalating and De-escalating Therapy for Early-Stage HER2-Positive Breast Cancer. Am Soc Clin Oncol Educ Book. 2020;40:1–11. doi: 10.1200/EDBK_100023. [DOI] [PubMed] [Google Scholar]
- 31.Modi S, Saura C, Yamashita T, Park YH, Kim SB, Tamura K, et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Breast Cancer. N Engl J Med. 2020;382(7):610–21. doi: 10.1056/NEJMoa1914510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krop IE, Saura C, Yamashita T, Park YH, Kim S-B, Tamura K, et al. Abstract GS1-03:[Fam-] trastuzumab deruxtecan (T-DXd;DS-8201a) in subjects with HER2-positive metastatic breast cancer previously treated with T-DM1:A phase 2, multicenter, open-label study (DESTINY-Breast01) Cancer Research. 2020;80(4 Supplement) GS1-03-GS1- [Google Scholar]
- 33.Smit EF, Nakagawa K, Nagasaka M, Felip E, Goto Y, Li BT, et al. Trastuzumab deruxtecan (T-DXd;DS-8201) in patients with HER2-mutated metastatic non-small cell lung cancer (NSCLC):Interim results of DESTINY-Lung01. Journal of Clinical Oncology. 2020;38(15_suppl):9504. [Google Scholar]
- 34.Jebbink M, de Langen AJ, Boelens MC, Monkhorst K, Smit EF. The force of HER2 - A druggable target in NSCLC? Cancer Treat Rev. 2020;86:101996. doi: 10.1016/j.ctrv.2020.101996. [DOI] [PubMed] [Google Scholar]
- 35.Dziadziuszko R, Smit EF, Dafni U, Wolf J, Wasag B, Biernat W, et al. Afatinib in NSCLC With HER2 Mutations:Results of the Prospective, Open-Label Phase II NICHE Trial of European Thoracic Oncology Platform (ETOP) J Thorac Oncol. 2019;14(6):1086–94. doi: 10.1016/j.jtho.2019.02.017. [DOI] [PubMed] [Google Scholar]
- 36.Hotta K, Aoe K, Kozuki T, Ohashi K, Ninomiya K, Ichihara E, et al. A Phase II Study of Trastuzumab Emtansine in HER2-Positive Non-Small Cell Lung Cancer. J Thorac Oncol. 2018;13(2):273–9. doi: 10.1016/j.jtho.2017.10.032. [DOI] [PubMed] [Google Scholar]
- 37.Peters S, Stahel R, Bubendorf L, Bonomi P, Villegas A, Kowalski DM, et al. Trastuzumab Emtansine (T-DM1) in Patients with Previously Treated HER2-Overexpressing Metastatic Non-Small Cell Lung Cancer:Efficacy, Safety, and Biomarkers. Clin Cancer Res. 2019;25(1):64–72. doi: 10.1158/1078-0432.CCR-18-1590. [DOI] [PubMed] [Google Scholar]
- 38.Ross JS, Fakih M, Ali SM, Elvin JA, Schrock AB, Suh J, et al. Targeting HER2 in colorectal cancer: The landscape of amplification and short variant mutations in ERBB2 and ERBB3. Cancer. 2018;124(7):1358–73. doi: 10.1002/cncr.31125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gatalica Z, Feldman R, Vranic S, Spetzler D. Immunohistochemistry-Enabled Precision Medicine. Cancer Treat Res. 2019;178:111–35. doi: 10.1007/978-3-030-16391-4_4. [DOI] [PubMed] [Google Scholar]
- 40.Adashek JJ, Kato S, Parulkar R, Szeto CW, Sanborn JZ, Vaske CJ, et al. Transcriptomic silencing as a potential mechanism of treatment resistance. JCI Insight. 2020;5(11) doi: 10.1172/jci.insight.134824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cummings J, Smyth JF. DNA topoisomerase I and II as targets for rational design of new anticancer drugs. Ann Oncol. 1993;4(7):533–43. doi: 10.1093/oxfordjournals.annonc.a058584. [DOI] [PubMed] [Google Scholar]
- 42.Braun MS, Richman SD, Quirke P, Daly C, Adlard JW, Elliott F, et al. Predictive biomarkers of chemotherapy efficacy in colorectal cancer:results from the UK MRC FOCUS trial. J Clin Oncol. 2008;26(16):2690–8. doi: 10.1200/JCO.2007.15.5580. [DOI] [PubMed] [Google Scholar]
- 43.Kostopoulos I, Karavasilis V, Karina M, Bobos M, Xiros N, Pentheroudakis G, et al. Topoisomerase I but not thymidylate synthase is associated with improved outcome in patients with resected colorectal cancer treated with irinotecan containing adjuvant chemotherapy. BMC Cancer. 2009;9:339. doi: 10.1186/1471-2407-9-339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fujita K, Kubota Y, Ishida H, Sasaki Y. Irinotecan, a key chemotherapeutic drug for metastatic colorectal cancer. World J Gastroenterol. 2015;21(43):12234–48. doi: 10.3748/wjg.v21.i43.12234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lu B, Zhang H, Zhang T, Cai Y, Hu Y, Zheng H, et al. Topoisomerase I expression is associated with prognosis in postoperative non-small cell lung cancer patients. Thorac Cancer. 2016;7(4):486–94. doi: 10.1111/1759-7714.12359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hou GX, Liu P, Yang J, Wen S. Mining expression and prognosis of topoisomerase isoforms in non-small-cell lung cancer by using Oncomine and Kaplan-Meier plotter. PLoS One. 2017;12(3):e0174515. doi: 10.1371/journal.pone.0174515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goldenberg DM, Stein R, Sharkey RM. The emergence of trophoblast cell-surface antigen 2 (TROP-2) as a novel cancer target. Oncotarget. 2018;9(48):28989–9006. doi: 10.18632/oncotarget.25615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vranic S, Palazzo J, Sanati S, Florento E, Contreras E, Xiu J, et al. Potential Novel Therapy Targets in Neuroendocrine Carcinomas of the Breast. Clin Breast Cancer. 2019;19(2):131–6. doi: 10.1016/j.clbc.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 49.Mojica WD, Brandwein-Weber M, Korangy EA. A case of metastatic lobular carcinoma with overexpression of Trop-2:Implications for the consideration of novel therapeutics. Breast J. 2017;23(6):757–9. doi: 10.1111/tbj.12924. [DOI] [PubMed] [Google Scholar]
- 50.Ambrogi F, Fornili M, Boracchi P, Trerotola M, Relli V, Simeone P, et al. Trop-2 is a determinant of breast cancer survival. PLoS One. 2014;9(5):e96993. doi: 10.1371/journal.pone.0096993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Liu D, Cardillo TM, Wang Y, Rossi EA, Goldenberg DM, Chang CH. Trop-2-targeting tetrakis-ranpirnase has potent antitumor activity against triple-negative breast cancer. Mol Cancer. 2014;13:53. doi: 10.1186/1476-4598-13-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumler I, Balslev E, Poulsen TS, Nielsen SL, Nygard SB, Romer MU, et al. Topoisomerase-1 gene copy aberrations are frequent in patients with breast cancer. Int J Cancer. 2015;137(8):2000–6. doi: 10.1002/ijc.29556. [DOI] [PubMed] [Google Scholar]
- 53.Bardia A, Mayer IA, Vahdat LT, Tolaney SM, Isakoff SJ, Diamond JR, et al. Sacituzumab Govitecan-hziy in Refractory Metastatic Triple-Negative Breast Cancer. N Engl J Med. 2019;380(8):741–51. doi: 10.1056/NEJMoa1814213. [DOI] [PubMed] [Google Scholar]
- 54.Murthy RK, Loi S, Okines A, Paplomata E, Hamilton E, Hurvitz SA, et al. Tucatinib, Trastuzumab, and Capecitabine for HER2-Positive Metastatic Breast Cancer. N Engl J Med. 2020;382(7):597–609. doi: 10.1056/NEJMoa1914609. [DOI] [PubMed] [Google Scholar]


