Abstract
Background
The aim of the study is to evaluate the impact of COVID-19 pandemic on vascular surgery practice in a regional hub center for complex vascular disease.
Methods
This is an observational single-center study in which we collected clinical and surgical data during (P1) and after (P2) the COVID-19 outbreak and the lockdown measures implemented in Northern Italy. We compared those data with the two-month period before the pandemic (P0).
Results
Compared to P0, ambulatory activities were severely reduced during P1 and limited to hospitalized patients and outpatients with urgent criteria. We performed 61 operations (18 urgent and 43 elective), with a decrease in both aortic (−17.8%), cerebrovascular (−53.3%), and peripheral artery (−42.6%) disease treatments. We also observed a greater drop in open procedures (−53.2%) than in endovascular ones (−22%). All the elective patients were treated for notdeferrable conditions and they were COVID-19 negative at the ward admission screening; despite this one of them developed COVID19 during the hospital stay. Four COVID-19 positive patients were treated in urgent setting for acute limb ischemia. Throughout P2 we gradually rescheduled elective ambulatory (+155.5%) and surgical (+18%) activities, while remaining substantially lower than during P0 (respectively −45.6% and −25.7%).
Conclusions
Despite COVID-19 pandemic, our experience shows that with careful patient's selection, dedicated prehospitalization protocol and proper use of personal protective equipment it is possible to guarantee continuity of care.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the causative pathogen of the respiratory infectious disease known as coronavirus disease 2019 (COVID-19).1 Its human transmission occurs through close contact and via respiratory droplets, even in asymptomatic patients; the airborne transmission is still under debate.2 , 3 The COVID-19 was declared a Public Health Emergency of International Concern on January 30 by the World Health Organization.4 On March 11, the World Health Organization declared COVID-19 a pandemic, pointing the alarming levels of spread and severity of the disease and the sustained risk of further global spread.5 Italy was at the center of the pandemic outbreak in Europe, until the governmental decision to implement lockdown measures to the whole country from March 9 to May 3.6 As of September 1, there was more than 25 million of confirmed cases and more than 840,000 deaths worldwide, with 270,189 cases and more than 35,000 deaths in Italy only.7 Within the Italian territory, Liguria is a small northwestern region and above the most densely populated (1,550,640 ab.–283.3 ab./km2), with the largest national over 65 years population in Italy (28.5%) and the second largest in Europe (average 20.3%).8 In this context, Liguria was among the highest affected regions in terms of the number of infected and deaths in Italy.9 The “Ospedale Policlinico San Martino” is located in Genoa, the capital of Liguria; it is the largest hospital in the region as well as the regional hub center for vascular diseases since before the pandemic outbreak. Which is why it was established as the referring regional hospital for the COVID-19 emergency. The Polyclinic is also a University Hospital with a partnership with the University of Genoa and it is home to the school of specializations of healthcare professions, Vascular Surgery included. In this context, all the activities were reorganized to avoid gatherings and to ensure dedicated environments for virus isolation and continuation of care. According to ministerial directives, all frontal lessons, training activities, and research projects were suspended during the lockdown. Therefore, the cancellation of ambulatory activities and the reduction of operative room schedule brought the approbation of teleworking and online webinar by the Organizing Committee of the single schools, allowing to maintain continuity in resident education and scientific working by individual study. This report aims to compare the impact of the healthcare measures implemented to manage this global ongoing pandemic on vascular surgery practice during three distinct phases.
Materials and Methods
To report the impact of the COVID-19 pandemic on our practice, we analyzed clinical and surgical activities trends comparing three distinct periods: from January 1 to February 29 (Phase 0 or P0), from March 1 to April 30 (Phase 1 or P1) and from May 1 to June 30 (Phase 2 or P2). In this time interval, our activities varied due to the implementation of local protocols adopted to prevent the virus from spreading.
Study Design and Data Collection
This retrospective study compared clinical and surgical data that were prospectively collected into a dedicated database, including pre-, intra-, and perioperative variables. Comparative analysis was focused on the volume of outpatient clinical activities (ambulatory visits, advanced medication, and ultrasound duplex examination), consultations and surgical schedule according to the type of disease (aortic, carotid, or peripheral artery diseases), intervention (endovascular or open surgery) and timing (elective or urgent). Aortic interventions included abdominal, thoracic and thoraco-abdominal aneurysms, acute aortic syndromes and aortic branches aneurysms. We especially focused on the impact of different peripheral artery diseases (PAD) during the 3 periods (intermittent claudication, chronic limb-threatening ischemia, and acute limb ischemia). We analyzed the number of accesses and length of intensive care unit (ICU) stay, postoperative length of hospital stays (LOS), and in-hospital mortality. This study was performed in accordance with the Institutional Ethics Committee rules. Individual consent fort this retrospective analysis was waived. All patients gave signed consent to the processing of personal and clinical data to be collected prospectively in the integrated institution database.
COVID-19 Emergency Protocol
A careful triage allowed hospitalization for elective nondeferrable cases. Triage consisted of temperature evaluation and compilation of dedicated forms (medical status, previous or active contact with suspected or confirmed infected patients). We performed the nasopharyngeal swab (NPS) before each hospitalization and patients were kept in isolation until the test result. The reverse transcription polymerase chain reaction (RT-PCR) was used to test the SARS-CoV-2 specific nucleic acid on this sample. Those who tested positive were reported to the Health Department and the Emergency Service in order to be safely discharged home with dedicated COVID-19 personnel (care assistant and ambulance) and put in quarantine. All patients treated in emergency setting were considered positive while waiting for test results and addressed to a dedicated COVID-19 pathway.
Surgical masks and hand sanitizer were available for daily activities. In the presence of suspected or confirmed COVID-19 patient, it was mandatory for healthcare workers to use the following personal protective equipment (PPE): surgical cap, face-shield, filtering face piece (FFP) mask, total body gown, apron, double-gloves, and overshoes. In our Unit, healthcare workers asymptomatic for respiratory illness were screened once per month with IgG and IgM antibodies to SARS-CoV-2 in a serum sample. In contrast, NPS was performed in any suspected clinical case.
Outpatient Clinical Activities
The reorganization of activities involved the cancellation of all nonurgent outpatients’ clinical practices, which included medical examinations, surgical medications, and Doppler ultrasound exams—keeping in consideration possible urgent cases limited to clinical conditions that cannot be delayed. Our Unit was reorganized as part of the grouping program to create dedicated pathways and units for COVID-19 and non-COVID-19 patients. We shared ward beds with other departments to relocate patients properly and create specialized “COVID-19 free” units.
Surgical Activities
In order to avoid ward overcrowding, prolonged LOS and ICU overload, the operating schedule was canceled for all elective deferrable cases and Day Surgery activities (e.g., chronic venous insufficiency). Despite each patient was individually evaluated for interventional eligibility, we filled a list of criteria for elective interventions (Table I ). Medical conditions that we treated with urgency or emergency criteria included symptomatic aneurysms, acute aortic syndromes, acute limb ischemia (ALI) and arterial traumatic injuries.
Table I.
Eligibility criteria for elective hospital admission and interventions
| Pathology | Criteria |
|---|---|
| Aortic aneurysms | AAA ≥ 60 mm or TAA ≥ 70 mm Rapidly growing aneurysm (0.5 cm in 6 months or 1 cm in 1 year) |
| Carotid artery stenosis | Symptomatic patients Asymptomatic patients with high-grade stenosis (≥ 70% ECST) and unstable carotid plaque (lipid or hemorrhage core, predominantly echolucent) |
| Peripheral artery diseases | CLTI |
AAA, abdominal aortic aneurysm; CLTI, chronic limb-threatening ischemia; ECST, European Carotid Surgery Trial; TAA, thoracic aortic aneurysm.
Statistical Analysis
In descriptive analyses, mean and standard deviation, and medians with interquartile ranges were presented for continuous variables; proportions and 95% confidence intervals were presented for categorical variables. Statistical analysis was conducted using the R Statistical Software (version 3.6.0, R Foundation for Statistical Software, Vienna, Austria).
Results
Outpatient Activities
Between P0 and P1, we had a significant reduction in outpatient activities that were progressively restored only as the lockdown period ended (P2); this trend was highlighted for visits (385 vs 58 vs 109) and Doppler ultrasound (2062 vs 569 vs 1264), but not for advanced medications (106 vs 17 vs 15). In comparison to P0, the number of vascular consultations increased for both P1 (+50.6%) and P2 (+77.9%) despite a reduction of those performed in emergency room (respectively −40.5% in P1 and −32.4% in P2; Table II ).
Table II.
Outpatients and inpatients activities comparison between January-February (P0), March-April (P1), and May-June (P2)
| Activities | P0 | P1 % variance (P0 vs P1) | P2 % variance (P1 vs P2) |
|---|---|---|---|
| Ambulatory visits | 385 | 58 (−84.9) | 109 (+87.9) |
| Advanced medications | 106 | 17 (−83.6) | 15 (+11.7) |
| DUS | 2062 | 569 (−72.4) | 1264 (+122.1) |
| Consultations, | 77 | 116 (+50.6) | 137 (+18.1) |
| ER | 37 | 22 (−40.5) | 25 (+13.6) |
| Interventions, (E/U) | 97 (86/11) | 61 (43/18) | 72 (51/21) |
| −37.1 (−50/+63.6) | +18.0 (18.6/16.6) | ||
| Endo/open | 50/47 | 39/22 (−22.0/−53.2) | 30/42 (-23.1/+90.9) |
DUS, Doppler ultrasound; E, elective; ER, emergency room; U, urgency.
Categorical variables are presented as number (%).
Inpatient Activities
From January 1 to June 30, we performed 230 interventions divided between P0, P1, and P2 (97 vs 61 vs 72). Demographics and clinical data were collected into a dedicated database (Table III ). We observed a decrease in interventions during P1 (P0 vs P1, −37.1%) and a gradual reestablishment of a regular operative planning during P2 (P1 vs P2, +18%), for both endovascular (50 vs 39 vs 30) and open (47 vs 22 vs 42) procedures. Also, we observed an increase in overall urgent procedures in P1 (+63.6% vs P0) and in P2 (+18.0% vs P1).
Table III.
Demographic and clinical data
| Age, years | 72.2 ± 10.7 | 72.2 ± 8.9 | 71.7 ± 11.9 |
|---|---|---|---|
| Sex (Male) | 73 (75.2) | 46 (75.4) | 51 (70.8) |
| Hypertension | 62 (63.9) | 28 (45.9) | 30 (41.6) |
| Dyslipidemia | 35 (36.1) | 22 (36.1) | 13 (18.1) |
| COPD | 7 (7.2) | 12 (19.7) | 9 (12.5) |
| CAD | 26 (26.8) | 7 (11.5) | 13 (18.1) |
| CKDa | 5 (5.1) | 4 (6.5) | 7 (9.7) |
| DM | 22 (22.7) | 13 (21.3) | 15 (20.8) |
| Previous CVD | 14 (14.4) | 9 (14.7) | 12 (16.6) |
| Previous PAD | 11 (11.3) | 4 (6.5) | 5 (6.9) |
CAD, coronary artery disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CVD, cerebrovascular disease; DM, diabetes mellitus; F, female; GFR, glomerular filtration rate; M, male; PAD, peripheral artery disease.
Categorical variables are presented as number (%). Continuous variables are presented as mean ± standard deviation.
GFR ≤30 ml/min.
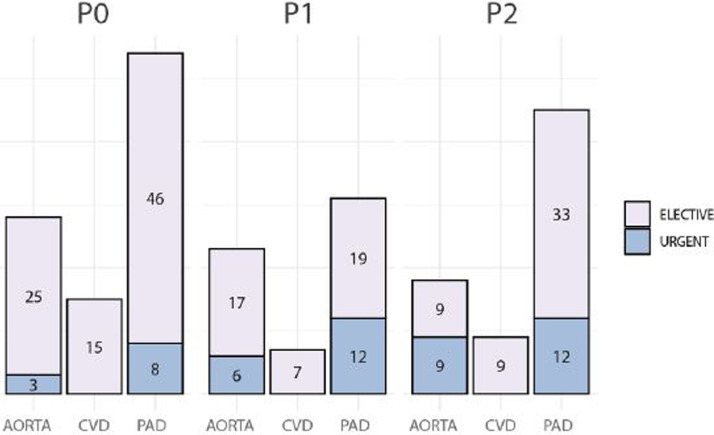
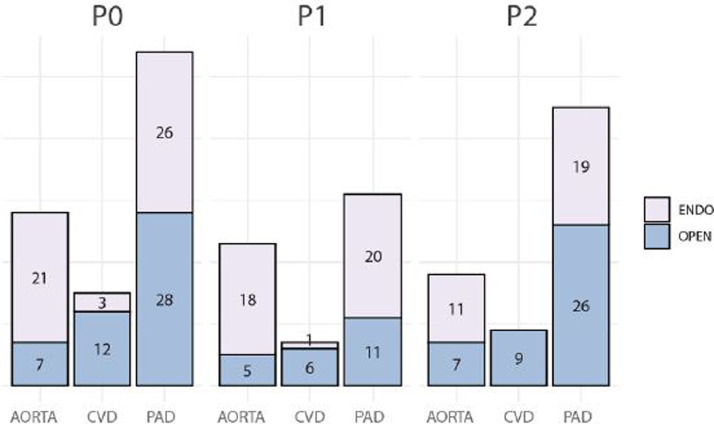
During P1, the number of aortic interventions slightly decreased (−17.8%) and 6 of them were performed in urgent settings (26%); similarly, the number of cerebrovascular disease (CVD) and PAD interventions were lower, and all the procedures for CVD were performed in elective setting (Fig. 1 ). Compared to P0, we had a slight increase in urgent aortic (3 vs 6, +100%) and PAD (8 vs 12, +50%) interventions during P1; we also registered decreasing trend in open surgical treatments of the aortic (7 vs 5, −28.5%), carotid (12 vs 6, −50%), and peripheral (28 vs 11, −60.7%) districts. Even the overall endovascular procedures decreased but the reduction was less evident (Fig. 2 ). In comparison with P1, we observed a rise for PAD interventions in P2 (31 vs 45, +45.1%), with an increase in both elective (19 vs 33, +73.3%) and open (11 vs 26, +136.3%) procedures. Regarding the underlying pathology which led to the interventions, ALI was the only that had a rise during P1 (+60%) (Table IV ). Looking in detail these results, the amputation rate was 12.9% (7 of 54 in P0), 3.2% (1 of 31 in P1), and 13.3% (6 of 45 in P2) of total PAD procedures in the 3 different periods; this reached a +500% (1 vs 6) from P1 to P2.
Fig. 1.
Distribution between elective and urgent surgery. CVD, cerebrovascular disease; PAD, peripheral artery disease.
Fig. 2.
Distribution between endovascular and open surgery. CVD, cerebrovascular disease; PAD, peripheral artery disease.
Table IV.
Focus on peripheral artery diseases leading to interventions
| Clinical condition | P0 (n) | P1 (n) % variance (P0 vs P1) | P2 (n) % variance (P1 vs P2) |
|---|---|---|---|
| Intermittent claudication | 16 | 8 (−50) | 10 (+25) |
| CLTI | 25 | 13 (−48) | 22 (+69.2) |
| ALI | 5 | 8 (+60) | 6 (-25) |
| Other | 8 | 2 (−75) | 7 (+250) |
ALI, acute limb ischemia; CLTI, chronic limb-threatening ischemia; E, elective; U, urgency.
Item “Other” includes: arterial traumatic injury of the extremities, arterial access complications, arteriovenous fistula complications, graft failure and peripheral graft infections.
Categorical variables are presented as number (%).
During P1, we recorded a slight increase in postoperative ICU accesses (7 vs 11, +57.1%) and a shorter LOS. Regarding elective mortality, one patient died in each phase; the one during P1 was due to a COVID-19 infection after revascularization for CLTI (Table V ).
Table V.
Postoperative data
| Variables | P0 | P1 | P2 |
|---|---|---|---|
| LOS, days | 6.0 (8.8) | 5.1 (5.1) | 5.9 (6.8) |
| ICU, n | 7 | 11 | 5 |
| Days, | 1.9 (7.8) | 2.7 (2.2) | 5.9 (7.6) |
| In-hospital mortality (E/U), n (n/n) | 4 (1/3) | 2 (1/1) | 8 (1/7) |
E, elective; ICU, intensive care unit; LOS, length of stay; U, urgency.
Continuous variables are presented as median (interquartile range).
COVID-19
During P1 and P2, all the patients treated electively were COVID-19 negative at the preoperative triage examinations. One patient became COVID-19-positive after an elective revascularization procedure for CLTI; afterward, the patient was transferred to the COVID-unit, where passed away 19 days later. Four patients with confirmed diagnosis of COVID-19 infection were treated in urgent settings for acute limb ischemia (ALI), 3 during P1, and 1 during P2. They were then admitted to the dedicated COVID-19 Unit where only the one from P2 group died due to multiple organ failure after 24 hour from intervention. None of our specialists or residents were infected. A ward nurse was infected, though was fully recovered after proper treatment and isolation in a dedicated COVID-19 unit. The nurse did not require ICU stay.
Discussion
The establishment of a strict emergency protocol allowed the continuation of vascular surgery activity during the COVID-19 pandemic outbreak, as underlined by the experience of some high-volume center for vascular pathology in northern Italy.10., 11., 12. Despite this, 1 patient developed fever and respiratory symptoms during the postoperative hospital stay and tested positive for COVID-19 at the NPS. After the patient's transfer to the dedicated Unit, we continued to apply the same emergency protocol since no one among the other inpatients or our staff members were found positive at the NPS or developed symptoms suggestive for COVID-19 infection. We treated only four COVID-19 patients and as mentioned above, all these patients were treated for ALI in urgent setting. This observation was consistent with the experience of Bellosta et al, in which it was reported a high prevalence of ALI in COVID-19 patients.12 This it may be related to the higher hypercoagulability state associated to a D-dimer increase that was pointed out in COVID-19 patients.13 , 14 In contrast to these studies that made a comparison with the same period 1 year before, our analysis was focused on a 6-month time interval to better highlight the activities variation related to the lockdown period. In this way, we were able to evaluate a trend line of how our hospital policies of postponing the deferrable interventions, influenced the volume of clinical and surgical activities. During P1, these policies resulted in a strong reduction in elective procedures, especially for CVD (−53.3%) and PAD (−42.6%) compared to aortic pathologies (−17.8%); this difference could be influenced by the centralization of care from spoke and nonspoke units of more complex cases. As a regional hub for complex vascular diseases, collaboration and communication with spoke and nonspoke regional vascular units were fundamental and possible thanks to a well-established telemedicine system.
On the other hand, we observed a slight increase in both aortic and PAD urgent interventions during P1 and P2 (Fig. 1); this could be explained by the increase of centralization of cases from spoke and nonspoke units and the late referral due to the fear of infection. In fact, we had an increase in amputation rate during P2 compared to P1 (+500%), although it returned almost to the P0 value (7 vs 1 vs 6). In fact, it represents the 13.3% of total P2-PAD procedures (6/45), just like the 12.9% stands for the P0-PAD (7/54). Also, people's fear of infection and lockdown restrictions policies, could justify the decrease of consultations in ER compared to P0 (−40.5% in P1 and −32.4% in P2). The COVID-19 had a severe impact on people's mental health, especially for medical workers that had to deal with the threat of contagion, inadequate PPEs, excessive work, stigma, isolation and lack of contact with their families; in response to this, setting up dedicated psychological intervention teams could be a right response to protect the mental health of medical workers.15
During P1, we performed fewer open procedures (−53.2%) compared to endovascular ones (−22%) and this was more evident for PAD interventions (open vs endo, −60.7% vs −23.1%). The policy of reducing LOS and avoiding ward and ICU overload, it might have led to choose the less-invasive treatment; however, we kept choosing the best personalized treatment as the reduction of access was possible following the above-mentioned criteria for ward admission collected in Table I. With the lockdown suspension, we rescheduled the postponed ambulatory and surgical activities and we gradually returned to the volume of activities of the pre-lockdown era. Despite the number of infections and fatalities are drastically reduced compared with previous months, we are keeping security measures for outpatient activities (triage) and at ward admission (triage, serology, and NPS test); in fact, there are still sparse outbreaks and new cases were daily reported.16
PPEs supply and adequate training in their use are crucial for preventing healthcare workers’ contagion and spreading of the disease.17 , 18 These precautions are even more significant if we consider that the international scientific community is still looking for a cure; nowadays there are no drugs with a specific indication for COVID-19 and the hyperimmune plasma therapy efficacy still need to be proved.19., 20., 21. In addition, despite national and international efforts, vaccines are still under clinical evaluation.22
Limitations
The descriptive nature of the study was aimed to highlight the experience of a single center in response to COVID-19 pandemic. The numbers showed activity volume variations in broad terms, as regular practice may vary from month to month. For the purposes of description, we considered a 2-month interval for each phase, starting from the first day of the following month.
Open Issues
At the time of the article's submission, there are no specific and unique treatments for COVID-19 and vaccines are still under testing. Despite the flattening of the curve of infections in some countries, the pandemic is still ongoing, and we could not exclude another outbreak or the application of new restrictions. Considering the need to avoid gatherings, the rescheduling of postponed ambulatory and surgery activities is extremely time consuming and it is still ongoing. Despite the implementation of tele-working, resident training was severely affected by the necessary measures undertaken to tackle this global pandemic, and only with an accurate and renewed planning of the activities it could be possible to fill this gap.
Conclusions
COVID-19 pandemic is still significantly affecting healthcare systems and surgical daily practice worldwide. Our experience shows that the implementation of essential care services and tailored approaches, according to safety standards and clinical-anatomical data, is helpful to reduce ward overcrowding and to guarantee a safe hospital stay. Availability and proper use of PPE it is necessary. Nowadays we are gradually restoring regular activities, maintaining high attention on a healthcare crisis that it is still globally active.
Author Contributions
GAB made substantial contributions to the study design, acquisition, analysis and interpretation of data, first drafting of the manuscript and its final critical revision. SDG and JMMV processed the experimental data, performed the analysis, designed tables and figures, and revised the first drafting. PB and GS supervised the data collection and interpretation, revising the final version of the manuscript. DP and GP supervised the project from its concept, reviewed the final manuscript, and gave the final approval to the submitted version. All authors read and approved the final manuscript.
Footnotes
Declaration of Competing Interest: None.
Funding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gandhi M, Yokoe DS, Havlir DV. Asymptomatic transmission, the Achilles' heel of current strategies to control COVID-19. N Engl J Med. 2020;382:2158–2160. doi: 10.1056/NEJMe2009758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Morawska L, Milton DK. It is time to address airborne transmission of COVID-19. Clin Infect Dis. 2020:ciaa939. doi: 10.1093/cid/ciaa939. [published online ahead of print, 2020 Jul 6] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Statement on the second meeting of the International Health Regulations. Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). (2005) Available at: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov).
- 5.World Health Organization. News and media: virtual press conference on COVID-19—11 March 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/transcripts/who-audio-emergencies-coronavirus-press-conference-full-and-final-11mar2020.pdf?sfvrsn=cb432bb3_2.
- 6.Ministry of Health (Italy). News and media: Covid-19 cases in Italy. Available at: http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4105.
- 7.Ministry of Health (Italy). COVID-19: daily situation report. Available at: http://www.salute.gov.it/portale/nuovocoronavirus/homeNuovoCoronavirus.jsp?lingua=english [Accessed September 2, 2020]
- 8.Italian National Institute of Statistics. Demographic indicators. Available at: http://dati.istat.it/Index.aspx?DataSetCode=DCIS_INDDEMOG1 [Accessed June 30, 2020]
- 9.WHO Coronavirus Disease (COVID-19) dashboard. Available at: https://covid19.who.int/[Accessed September 2, 2020]
- 10.Pini R, Faggioli G, Vacirca A, et al. Is it possible to safely maintain a regular vascular practice during the COVID-19 pandemic? Eur J Vasc Endovasc Surg. 2020;60:127–134. doi: 10.1016/j.ejvs.2020.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mascia D, Kahlberg A, Melloni A, et al. Single-center vascular hub experience after 7 weeks of COVID-19 pandemic in Lombardy (Italy) Ann Vasc Surg. 2020 doi: 10.1016/j.avsg.2020.07.022. [published online ahead of print, 2020 Aug 5] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bellosta R, Luzzani L, Natalini G, et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. [published online ahead of print, 2020 Apr 29] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Violi F, Pastori D, Cangemi R, et al. Hypercoagulation and antithrombotic treatment in coronavirus 2019: a new challenge. Thromb Haemost. 2020;120:949–956. doi: 10.1055/s-0040-1710317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lippi G, Favaloro EJ. D-dimer is associated with severity of coronavirus disease 2019: a pooled analysis. Thromb Haemost. 2020;120:876–878. doi: 10.1055/s-0040-1709650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang L, Li Y, Hu S, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. 2020;7:e14. doi: 10.1016/S2215-0366(20)30047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ministry of Health. News and media, weekly report. Covid-19, 10-16 August. Available at: http://www.salute.gov.it/portale/nuovocoronavirus/dettaglioNotizieNuovoCoronavirus.jsp?lingua=italiano&id=5025.
- 17.World Health Organization. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19) and considerations during severe shortages. 2020. Available at: https://www.who.int/publications/i/item/rational-use-of-personal-protective-equipment-for-coronavirus-disease-(covid-19)-and-considerations-during-severe-shortages.
- 18.Liu M, Cheng SZ, Xu KW, et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross sectional study. BMJ. 2020;369:m2195. doi: 10.1136/bmj.m2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. “Solidarity” clinical trial for COVID-19 treatments. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-clinical-trial-for-covid-19-treatments [Accessed June 30, 2020]
- 20.University of Oxford. The RECOVERY trial – randomized evaluation of COVID-19 therapy. Available at: https://www.recoverytrial.net/results [Accessed June 30, 2020]
- 21.Li L, Zhang W, Hu Y, et al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA. 2020;324:460–470. doi: 10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. Draft landscape of COVID-19 candidate vaccines. Available at: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines.