Abstract
Coronavirus disease 2019 (COVID-19) first emerged in China in December 2019 and was declared a pandemic by the World Health Organization on March 11, 2020. Clinicians around the world looked to cities that first experienced major surges to inform their preparations to prevent and manage the impact the pandemic would bring to their patients and health care systems. Although this information provided insight into how COVID-19 could affect the Canadian palliative care system, it remained unclear what to expect. Toronto, the largest city in Canada, experienced its first known case of COVID-19 in January 2020, with the first peak in cases occurring in April and its second wave beginning this September. Despite warnings of increased clinical loads, as well as widespread shortages of staff, personal protection equipment, medications, and inpatient beds, the calls to action by international colleagues to support the palliative care needs of patients with COVID-19 were not realized in Toronto. This article explores the effects of the pandemic on Toronto's palliative care planning and reports of clinical load and capacity, beds, staffing and redeployment, and medication and PPE shortages. The Toronto palliative care experience illustrates the international need for strategies to ensure the integration of palliative care into COVID-19 management, and to optimize the use of palliative care systems during the pandemic.
Key Words: Palliative care, COVID-19, Coronavirus, Health care systems, Pandemic
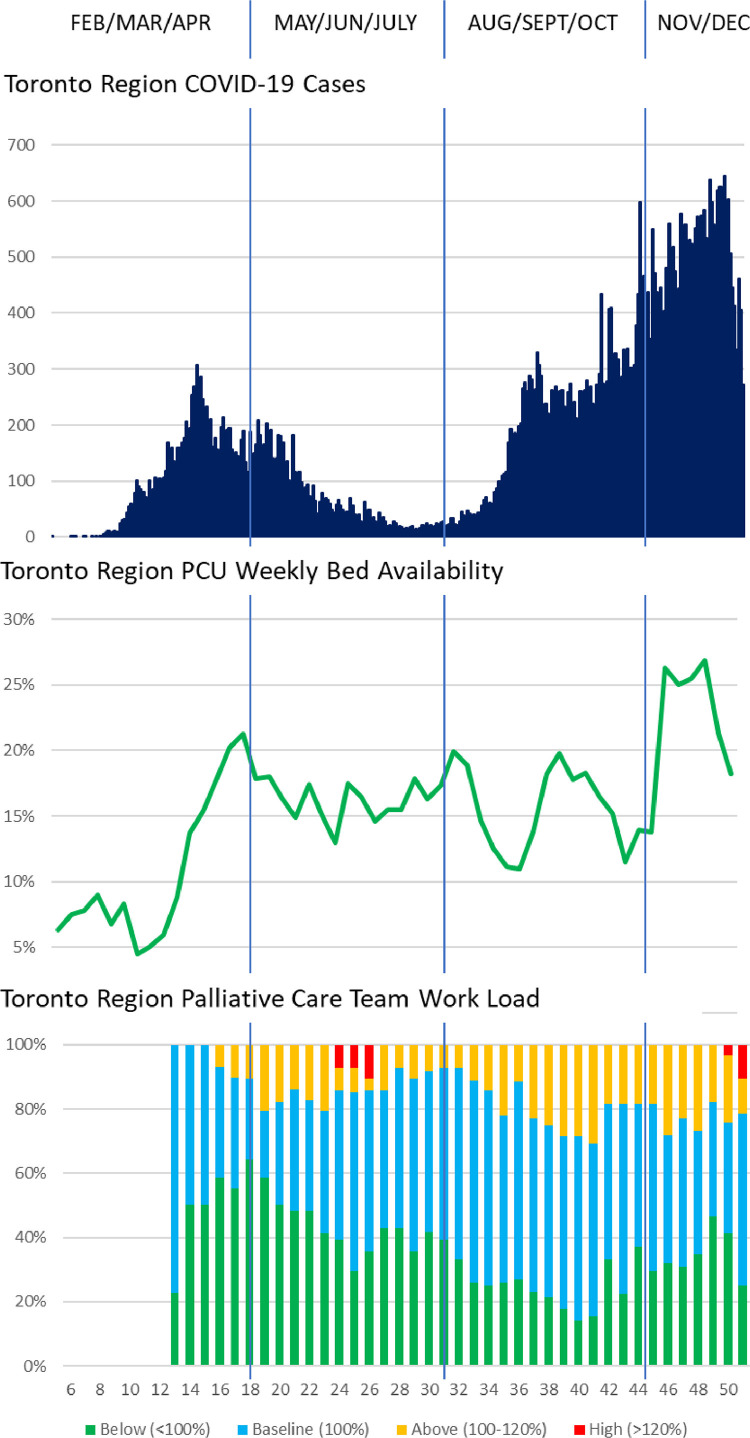
Toronto is the largest city in Canada with a population of over 6 million. Toronto experienced its first known case of COVID-19 in January 2020; on March 23, a state of emergency was declared in response to the city's first COVID-related death. Toronto's first wave of new cases peaked in April and May (Fig. 1 ). By August 31, 2020, almost 16,000 new cases were reported; of these, 12.1% were hospitalized and 1174 died. Cases decreased over the summer but are again rising rapidly. As of December 23, we have reported almost 61,000 cases, and 1932 deaths.
Fig. 1.
Toronto reporting: COVID-19 cases, PCU bed availability and palliative care team workload.
Palliative care has been identified as a basic need for patients with COVID-19,1, 2, 3 but has been underused in previous epidemics.4 In March, the palliative care sector in Toronto began to mobilize recommendations and reporting structures to prepare for the pandemic. Weekly reporting by palliative care programs to Ontario Health (Toronto) began on clinical load and capacity, staffing and redeployment, medication and personal protection equipment (PPE) shortages, and new clinical innovations, to help prepare for and manage the expected surge in COVID-19 cases. In addition, Toronto's inpatient palliative care bed availability is captured daily and is managed by an online program that oversees 8 palliative care units (PCUs) and 2 hospices. We analyzed the Toronto region's palliative care bed availability, as well as the routine regional reports by palliative care programs, to determine trends in palliative care utilization for the region during the COVID-19 pandemic.
Toronto's palliative care system includes a large group of connected clinical teams and health care institutions. This includes a total of 29 palliative care teams from 23 institutions; 11 of which are hospital-based teams with consultation services in inpatient (and some also in outpatient) settings; six oversee palliative care inpatient beds; four are community home visiting teams; and seven include a combination of the above. The region also has 221 PCU and hospice beds located in acute care, complex care and community centers. Almost all of these teams and institutions have academic affiliations with the University of Toronto.
Palliative care inpatient bed availability was approximately 7% during January 2020, dipped to 4.5% as hospitals worked to transfer patients from acute to palliative care beds in preparation for the anticipated surge, and climbed to more than 20% in May. The second wave also brought high levels of bed availability at the beginning of September but reached their highest levels for 2020 in the months of November and December (Fig. 1). On one day, 29.6% or 64 of 216 palliative care beds were empty. As of December 2020, bed availability has still not returned to baseline pre-COVID-19 percentages. Reasons for this marked reduction of admissions to PCUs and hospices may include restrictive visitation policies that were adopted to prevent COVID-19 transmission as well as patients’ fears of infection risk.
As Toronto's new COVID-19 cases began to peak, most palliative care teams reported that their clinical loads decreased and were below baseline (Fig. 1). Over the March to August period, approximately half of the teams indicated they had seen patients with COVID-19, but most patients seen by consultation teams in acute care settings no longer had an active infection; rather they were seen postinfection for symptom management and discharge planning. Teams that indicated above average clinical loads during Toronto's first surge provided either community home visits or ambulatory care. In June, several community-based teams reported their highest (>120%) clinical loads, as these teams stretched to support the patients avoiding the acute care system. Despite a subsequent decrease and stabilization in COVID-19 cases within the region over the summer, 20%–30% of teams still did not see a return to normal clinical loads; despite entering into the second wave, they remain below their baseline in terms of patient care. In December 2020, two community-based teams and one acute care team supporting the long-term care (LTC) sector have returned to reporting clinical loads over 120%. One-third of the palliative care teams have had below baseline clinical loads for more than seven months of this year.
Teams all reported consistently adequate staffing and several teams indicated that they had staff redeployed to other services; these were mainly nurses or other allied health professionals. Several teams assisted in providing palliative care for LTC homes, which were severely affected by the COVID-19 pandemic. The Toronto region maintains almost 1900 beds across 36 LTC homes which had just over 300 deaths due to COVID-19 by the end of December. In response to the needs of these patients, Toronto's palliative care sector mobilized to develop partnerships to support LTCs’ ability to provide palliative care in these homes. In addition, palliative care teams joined with internists to support the establishment of a new structure called LTC+,5 which allowed for LTC homes to connect with internists or acute care specialists (including palliative care) at any time. Although many palliative partners reported that they had helped support LTC homes with education resources for both goals of care discussions and symptomatic management in the spring, many still had not built strong relationships by the end of the summer. Most teams and LTC+ report only a few points of engagement between LTC and palliative care partners, apart from four palliative care teams which have developed stronger ties. Their support has included virtual rounding, in-person shared care models and regular or scheduled interactions to support ongoing palliative care integration.
Medication shortages were not infrequent for some palliative care medications, particularly at the peak of the first surge of the COVID pandemic. Medications for which shortages were reported included: midazolam, methotrimeprazine, haloperidol, scopolamine, fentanyl, dexamethasone, lorazepam, hydromorphone, ondansetron and propofol; methotrimeprazine was most frequently reported. This differed from the second surge which saw few medication shortages reported, and none in the months of November or December. A total of seven palliative care teams indicated that their supplies of PPE were “at risk”: i.e., they had current supplies but no reasonable access to future supply, and this occurred only in the first wave. No teams indicated a limited or nonexistent supply of PPE.
In terms of clinical innovations, all teams reported integrating virtual strategies into patient care, and many reported they had developed innovative tools to support goals of care conversations or symptomatic optimization, including changing their models of care to build capacity for palliative care integration. An online repository was built to house and share these innovations including other guidance, policy, educational, and reporting documents. Over 100 documents have been collected including 24 different communication tools, 32 focused on symptom management, and 20 supporting system planning. It also supports communication of our regional reporting, including the frequently changing status of institutional visitor policies.
In summary, although Toronto's community-based palliative care teams reported higher workloads in managing patients outside the acute care system, hospital-based palliative care teams reported under-use to support the care of patients with COVID-19. This occurred despite an influx of patients to acute care centers and the development of structures for palliative care consultants to support the LTC sector. In addition, Toronto palliative care teams faced medication shortages, especially those medications also used in the intensive care system (i.e. sedatives and opioids) during the first wave. These results differ from many early international reports published on COVID-19’s impact on palliative care. An Italian study indicated that COVID-19 brought significant stress to the acute care system,6 and although a Spanish report indicated a similar decrease in inpatient workload, many palliative care staff were redeployed to other services such as the emergency room. A New York team reported the development of virtual innovations to support acute care, and indicated increased workloads in acute care.7 A study focused on the support provided by hospices in Italy's response to COVID-19 reported that only one hospice (out of 16) had decreased admissions, whereas in Toronto inpatient palliative care bed utilization decreased significantly.8 Lastly, international reports warned of PPE and medication shortages, and outbreaks of COVID-19 in hospices; although Toronto reported various medication shortages, there have been neither outbreaks, nor a lack of PPE.8 , 9
It is unclear why palliative care providers in hospital-based teams our region were less involved in managing the pandemic response or in the clinical management of patients with COVID, while there was higher utilization of palliative care teams in the community. However, palliative care teams are often the only providers of community end-of-life care in Toronto,10 and are therefore the most responsible physicians in this setting. In contrast, the provision of palliative care for patients on acute care units requires palliative care referral by acute care providers, and it is possible that these acute care services feel that they are capable of managing patients’ palliative care needs. The lack of admission to PCUs could be due to the precipitous decline of patients with COVID-19 at the end of life, and the desire of patients without COVID-19 to remain out of hospital to avoid infection. Stakeholder engagement is in process to better understand the reasons behind the variable relationships between LTC and palliative partners. In addition, the current data highlight the need for further research in this area, which could include qualitative interviews with patients, administrators, and acute and palliative care providers to determine reasons and mechanisms for these findings; a formal pre-post analysis of access to palliative care before and after COViD-19 pandemic; or an analysis of how redeployment to other areas affected quality of palliative care.
The Toronto palliative care experience illustrates the international need for strategies to ensure the integration of palliative care into COVID-19 management, and to optimize the use of palliative care systems during the pandemic. This may include developing partnerships between COVID-19 providers and palliative care teams, expanding the use of PCU beds for patients that do not meet the traditional criteria for admission, adopting strategies to allow hospital-based teams to support patients outside their institutions, and finally, the need for evidence based research to understand how every palliative system can support the needs of patients during a pandemic.
Disclosures and Acknowledgments
No funding was received for this study. The authors have no conflicts of interest to declare.
References
- 1.Radbruch L, Knaul FM, de Lima L, de Joncheere C, Bhadelia A. The key role of palliative care in response to the COVID-19 tsunami of suffering. Lancet. 2020;395:1467–1469. doi: 10.1016/S0140-6736(20)30964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Powell VD, Silveira MJ. What should palliative care's response be to the COVID-19 pandemic? J Pain Symptom Manag. 2020;60:e1–e3. doi: 10.1016/j.jpainsymman.2020.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fadul N, Elsayem AF, Bruera E. Integration of palliative care into COVID-19 pandemic planning. BMJ Support Palliat Care. 2021;11:40–44. doi: 10.1136/bmjspcare-2020-002364. [DOI] [PubMed] [Google Scholar]
- 4.Chen TJ, Lin MH, Chou LF, Hwang SJ. Hospice utilization during the SARS outbreak in Taiwan. BMC Health Services Res. 2006;6:94. doi: 10.1186/1472-6963-6-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Women's College Hospital. LTC+ Toronto, Ontario 2020. Available at: https://ltcplus.ca/. Accessed February 19, 2021.
- 6.Paterlini M. On the front lines of coronavirus: the Italian response to Covid-19. BMJ. 2020;368:m1065. doi: 10.1136/bmj.m1065. [DOI] [PubMed] [Google Scholar]
- 7.Ankuda C, Woodrell C, Meier D, Morrison R, Chai E. A Beacon for dark times: palliative care support during the coronavirus pandemic. NEJM Catal Innov Care Deliv. 2020 https://catalyst.nejm.org/doi/pdf/10.1056/CAT.20.0204 Available at: [Google Scholar]
- 8.Costantini M, Sleeman KE, Peruselli C, Higginson IJ. Response and role of palliative care during the COVID-19 pandemic: a national telephone survey of hospices in Italy. Palliat Med. 2020;34:889–895. doi: 10.1177/0269216320920780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Providing palliative care during the COVID-19 pandemic experiences from Spain 2020. Available at:https://www.euro.who.int/__data/assets/pdf_file/0008/445553/palliative-care-COVID-19.pdf. Accessed February 19, 2021.
- 10.Malik S, Goldman R, Kevork N. Engagement of primary care physicians in home palliative care. J Palliat Care. 2017;32:3–10. doi: 10.1177/0825859717706791. [DOI] [PubMed] [Google Scholar]