Abstract
Background
Reconstruction intramedullary nail spanning the whole length of the femur has been the gold standard treatment for complete atypical diaphyseal fractures of the femur (ADF). However, in cases of incomplete ADF combined with severe bowing, this approach might have complications and lead to iatrogenic complete fracture. We report two cases of incomplete ADF with severe bowing using a precontoured plate (PCP) after rapid prototyping (RP) of the deformed femurs with three‐dimensional printing (3DP) technology.
Case presentation
Two patients presented with gradually worsening thigh pain, especially during walking. The patients had been using bisphosphonates for 4 and 10 years, respectively. Radiography showed an incomplete fracture in the lateral cortex of the right femur shaft. The lateral bowing angles measured in the affected femurs were 15° and 14°, and the anterior bowing angles were 20° and 16°, respectively. In bone scans, both patients showed hot uptake in the right mid‐shaft of the femur. Preoperatively, the affected femur of the patient was reconstructed by 3DP RP using CT, and the plate was bent to the shape of the bone model. The ADF was fixed with a PCP using the minimally invasive plate osteosynthesis technique. Both patients were encouraged to start full weight‐bearing and return to their preinjury activity level in daily life immediately after surgery. At 2 years postoperatively, radiography showed healing of the fracture site without recurrence of thigh pain and implant‐related problems.
Conclusion
Although intramedullary nailing is the standard surgical treatment for complete ADF, PCP using 3DP RP could be an effective treatment option for incomplete ADF with severely curved femur.
Keywords: Diaphyseal femoral fracture, Incomplete fracture, Precontoured plate, Minimally invasive surgery, Three‐dimensional printing
Although intramedullary nailing is the standard surgical treatment for complete atypical femoral fractures, using a precontoured plate after rapid prototyping of the deformed femur with three‐dimensional printing could be an effective treatment option for incomplete atypical femoral fractures with severely curved femur.
Introduction
For complete atypical diaphyseal fractures of the femur (ADF), reconstruction intramedullary nailing (IMN) panning the whole length of the femur has been considered the standard surgical treatment 1 , 2 . However, in cases of incomplete ADF combined with severe bowing, this procedure might result in complications and lead to iatrogenic complete fracture, resulting in delayed union or non‐union 3 , 4 . Plating has been proposed as an alternative 5 , 6 but may have disadvantages, such as the potential risk of developing neck fractures, the considerable time necessary to modify the plate into a form that fits perfectly to the bowed femur during the operation, and the insufficient length to cover the whole femur due to the complexity of the three‐dimensional (3D) deformity 7 . We report two cases of incomplete ADF with markedly curved femurs using a pre‐contoured plate (PCP) after rapid‐prototyping (RP) the deformed femurs with three‐dimensional printing (3DP) technology.
Case Reports
Patient 1
A 75‐year‐old woman presented to our clinic with a 3‐month history of right thigh pain. She was able to walk independently outdoors before symptom onset. The patient had no history of recent trauma, and thigh pain was aggravated during walking, especially in the stance phase. However, she had no pain in other sites. The patient had used ibandronate 4 years previously due to osteoporosis. The patient had undergone internal fixation with proximal femur nail for intertrochanteric fracture of the left femur 11 years previously in another institution and internal fixation for left distal radius fracture 6 years previously in our institution. The patient complained of limb‐length discrepancy due to a shorter left leg after the previous surgery on the left femur. Besides osteoporosis, the patient had never been diagnosed with any disease affecting the bone metabolism, such as osteogenesis imperfecta.
On physical examination, there was mild tenderness in the right mid‐thigh. There was no clinical sign of infection, such as erythema, and local heat was not observed. The results of routine laboratory tests, including serum C‐reactive protein level and erythrocyte sedimentation rate, were within normal limits. Plain radiography showed transverse radiolucent fracture line on the apex of the lateral cortex of the right mid‐shaft of the femur (Fig. 1), but the contralateral side of the femur was intact. According to Sasaki et al. 8 , the lateral bowing angle was 14° and the anterior bowing angle was 16°. Bone single photon emission computed tomography (SPECT) showed hot uptake in the right femoral shaft (Fig. 2). The bone mineral density (BMD) of the lumbar spine (L1–4, 0.639 g/cm2; T‐score: −3.9) and the proximal femur (0.607 g/cm2; T‐score, −2.7) was evaluated by dual‐energy X‐ray absorptiometry (DEXA).
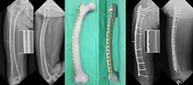
Fig. 1.
Radiographs of patient 1. Plain radiographs showed transverse radiolucent line on the apex of the lateral cortex of the right mid‐shaft of the femur.
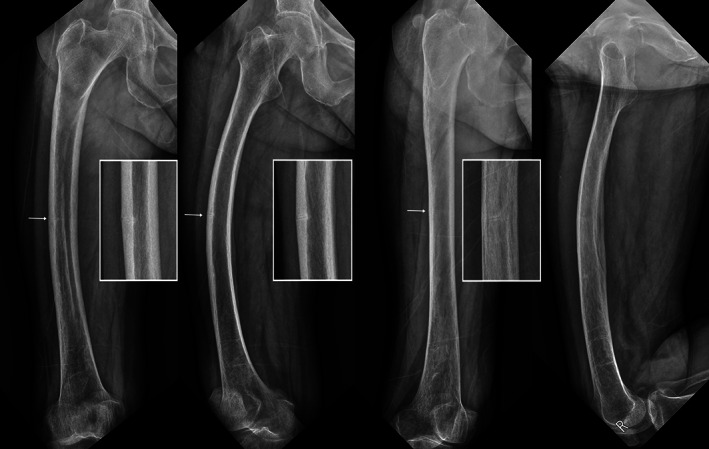
Fig. 2.
Bone single photon emission CT of patient 1. (A) Preoperative nuclear medical images showed hot uptake in the right femoral shaft (arrowhead). (B) Two years after surgery, no or minimal uptake of the right femoral mid‐shaft was observed (arrowhead).
The patient was advised to discontinue ibandronate use and start teriparatide injection 2 , 9 . According to the scoring system for identifying impending complete fractures in incomplete atypical femoral fractures (AFF) 10 , the patient scored a total of 9 points, an indication for prophylactic surgery: 2 for diaphyseal lesion, 3 for functional pain, 3 for intact on the contralateral side, and 1 point for a focal radiolucent line. Due to severe bowing of the affected femur, we planned to perform prophylactic PCP spanning the whole length of the bowed femur. CT was performed on the patient's right femur, and a bone model was reconstructed using KM3D version 1.0 (Kyungpook National University, Institute of Advanced Convergence Technology, Daegu, Korea). A locking compression plate (DePuySynthes, Oberdorf, Switzerland) was precontoured preoperatively according to the shape of the bone model (Fig. 3). The bone model was sterilized for intraoperative use and placed on the same position to that of the femur under C‐arm guidance to enhance the accurate position of the PCP (Fig. 4A). Taking into consideration the 3D bending of the plate, an anterolateral skin incision, instead of a lateral incision, for plate entry was made, and submuscular insertion of PCP was performed using the routine minimally invasive plate osteosynthesis (MIPO) technique (Fig. 4B). To reduce the potential risk of femoral neck fracture due to stress concentration, one 80‐mm locking screw was inserted through the screw hole in the plate and two additional cannulated screws were inserted using the same incision at the entry site (Fig. 4C). The patient was encouraged to start full weight bearing and return to the pre‐injured activity level of daily life immediately after surgery.
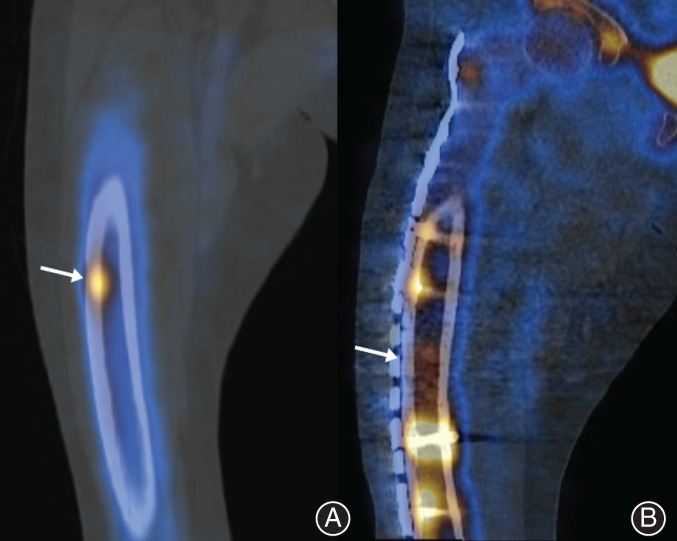
Fig. 3.

Precontoured plate for patient 1. The locking compression plate was precontoured according to the shape of the bone model. Because of the three‐dimensional complex deformity of the severely bowed femur, the proximal part of the precontoured plate was placed on the anterolateral aspect of the proximal femur. (A) Anteroposterior view. (B) Lateral view.
Fig. 4.

Surgical process of patient 1. (A) Before making the incision, the sterilized bone model was placed on the same position to that of the femur under C‐arm guidance to enhance the accurate position of the PCP and reduce the operative time. (B) After submuscular insertion of PCP, we confirmed the correct position of the plate matching the bowed femur using both fluoroscopic guidance and preoperative images (shown in Fig. 3 using a smartphone). (C) Immediate postoperative radiography demonstrated the accurate position of the PCP, similar to the preoperative planning shown in Fig. 3, with additional screws toward the right femoral neck.
Thigh pain subsided 6 weeks postoperatively, and the patient returned to complete daily life. Radiography performed 2 years postoperatively showed bone union and no progression of femoral bowing or implant‐related problems (Fig. 5).
Fig. 5.
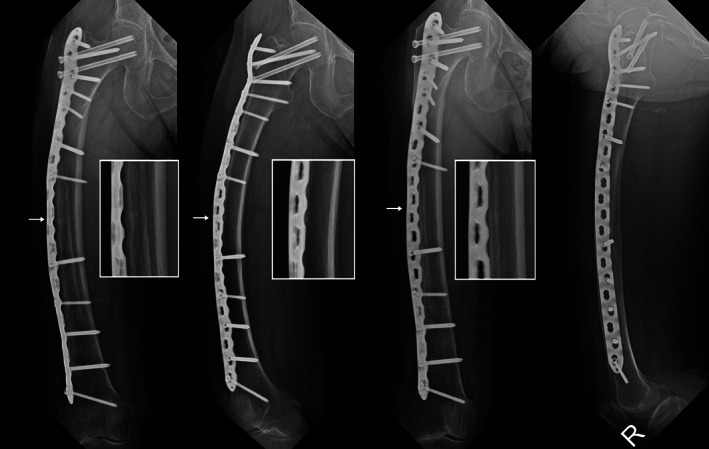
Radiographs of patient 1 at last follow up. Radiographs taken at 2 years postoperatively showed bone union and no progression of femoral bowing or implant‐related problems.
Patient 2
A 78‐year‐old woman visited our orthopaedic department due to right thigh pain for 6 months. Thigh pain developed insidiously and gradually worsened. She had been unable to walk independently for 1 week. The patient had no history of recent trauma. No pain was noted in other sites. The patient had been using alendronate for treatment of osteoporosis for 10 years. The patient underwent total knee arthroplasty on both knees 10 years previously. She was diagnosed with an intertrochanteric fracture of the left femur and fracture of the symphysis pubis 4 years previously after slipdown. For intertrochanteric fractures, internal fixation with proximal femoral nail has been performed in another institution. She complained that the left lower limb was shortened after the previous surgery. Besides osteoporosis, she had never been diagnosed with any disease that might affect the bones.
On physical examination, there was moderate tenderness in the right thigh. There was no clinical sign of infection. Results of routine laboratory tests revealed no specific abnormality. Radiographs showed transverse radiolucent line in the lateral cortex of the mid‐shaft of the femur (Fig. 6), but there was no abnormality on the contralateral side of the femur. The curvature of the femur was marked, the lateral bowing angle was 15°, and the anterior bowing angle was 20°. Bone SPECT showed hot uptake in the right femoral shaft and symphysis pubis (Fig. 7). On DEXA, BMD of the lumbar spine (L2‐4, 0.718 g/cm2, T‐score: ‐2.7) and proximal femur (0.413 g/cm2, T‐score: ‐3.8) was obtained.
Fig. 6.
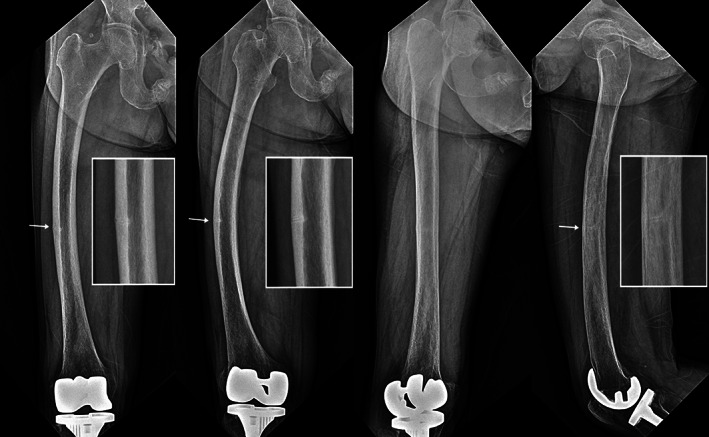
Radiographs of patient 2. Plain radiographs showed transverse radiolucent line in the lateral cortex of the mid‐shaft of the femur.
Fig. 7.
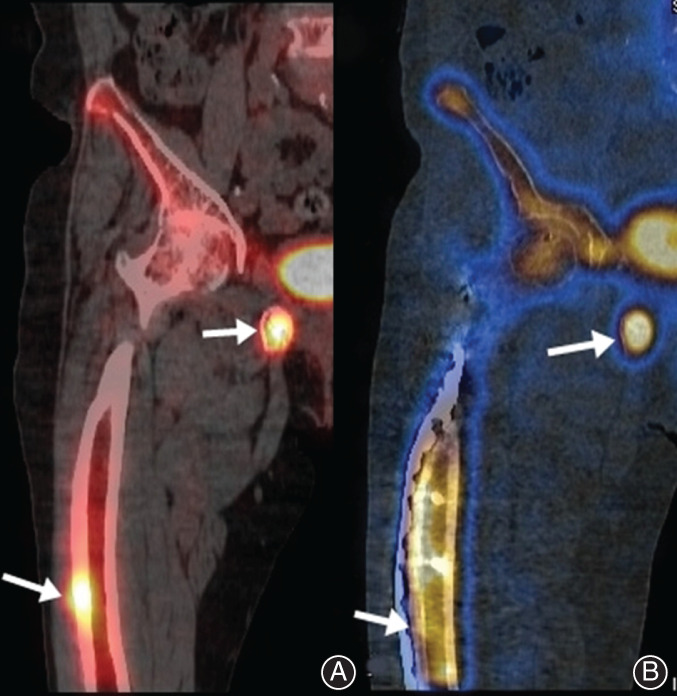
Bone single photon emission CT of patient 2. (A) Preoperative nuclear medical images showed hot uptake in the mid‐shaft of the right femur shaft and around the symphysis pubis (arrowhead). (B) Sixteen months after surgery, uptake in the mid‐shaft of the right femur was decreased, but hot uptake was still observed around the symphysis pubis (arrowhead).
The patient was advised to discontinue alendronate use and start teriparatide injection. Based on the scoring system to evaluate impending complete fractures, the patient scored 9 points, which was an indication for prophylactic surgery. Because the curvature of the affected femur was marked, we planned prophylactic surgery using PC‐WBP. We performed CT to obtain the morphologic features of the affected femur, and the bone model was reconstructed using 3DP RP. A locking compression plate (DePuySynthes, Oberdorf, Switzerland) was molded preoperatively according to the shape of the bone model (Fig. 8). The bone model was sterilized and used intraoperatively to assist the MIPO technique (Fig. 9A). Three additional cannulated screws were fixed using the same incision at the entry site to decrease the potential risk of femoral neck fracture (Fig. 9B). The patient was encouraged to start full weight‐bearing and return to their preinjury activity level in daily life immediately after surgery.
Fig. 8.

Precontoured plate for patient 2. The locking compression plate was prebent to match the shape of the reconstructed bone model preoperatively. Because the curvature of the femur was more severe than that in patient 1, the proximal part of the precontoured plate was placed on the more anterior aspect of the proximal femur. (A) Anterioposterior view. (B) Lateral view.
Fig. 9.
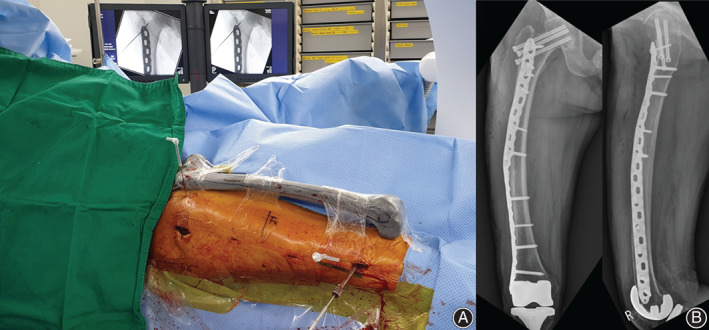
Surgical process of patient 2. (A) Bone model was sterilized and used intraoperatively to assist minimally invasive plate osteosynthesis (MIPO) technique. (B) Immediate postoperative plain X‐rays of the right femur.
The patient did not report pain in the right thigh and returned to complete daily life at the last follow‐up. Radiography performed at 16 months postoperatively showed ongoing union and no progression of femoral bowing or implant‐related problems (Fig. 10).
Fig. 10.
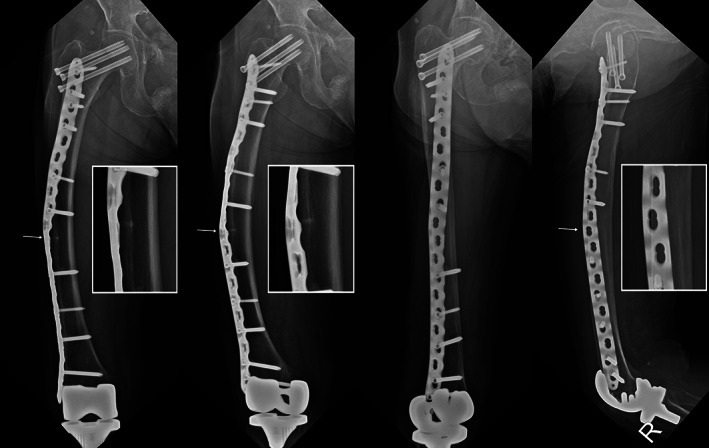
Radiographs of patient 2 at last follow‐up. Radiography performed 16 months postoperatively showed and no progression of femoral bowing or implant‐related problems.
Discussion
We diagnosed incomplete ADF through physical examination and radiologic evaluation in two patients complaining of mid‐thigh pain and confirmed the indication for prophylactic surgery with a scoring system. Both patients had severely bowed femurs, and the bone model was reconstructed with 3DP RP. A locking compression plate spanning the whole femur was contoured preoperatively according to the shape of the bone model and then fixed to the bone using the MIPO technique. At 18 months postoperatively, we observed bone union, no progression of bowing, and no implant‐related problems on radiography. Furthermore, the patients did not complain of pain and were able to return to their preinjury daily lives.
The treatment choice for incomplete ADF depends on the patient's symptoms and radiological findings. If there is no pain, conservative treatment can be attempted initially for an incomplete ADF without a radiolucent fracture line 1 . Recently, Min et al. (2017) developed a scoring system to determine the necessity of prophylactic surgery for incomplete ADF 10 . Both cases in the present study corresponded to the indication for surgery. Prophylactic surgery foe incomplete ADF, if indicated, has been reported to reduce pain and prevent progression to complete fracture 1 . Moreover, compared to the surgery for complete ADF, prophylactic fixation for incomplete ADF has advantages, such as shorter time for union, shorter hospital stay and fewer complications 2 .
Reconstruction IMN has been considered as a standard method of prophylactic fixation for incomplete subtrochanteric AFF due to its better load‐sharing capacity and less bending moment 1 , 2 . However, prophylactic nailing for incomplete ADF, which is usually combined with a bowed femur, remains a challenge. Various methods for ADF have been proposed to overcome the significant anterolateral bowing of the femur, including far lateral entry point, use of the contralateral side of the nail, and external rotation of the nail 3 . However, in cases combined with severe anterolateral bowing, IMN may cause iatrogenic progression to complete fracture, which may lead to delayed union or non‐union 1 , 2 . Moreover, if femoral bowing occurs bilaterally, which is common in patients with ADF, IMN with iatrogenic or intentional complete fractures may straighten the curved femur and make the affected side longer than the contralateral side, leading to limb length discrepancy (LLD). Because both patients in our report complained of LLD due to a shortened contralateral lower limb after previous fixation for an intertrochanteric fracture, there was a potential risk of worsening LLD when complete fracture occurred during IMN.
Biomechanically, tensile loading is concentrated in the lateral cortex of the curved femur in daily life, such as walking, and ADF occur in the region where maximal tensile loading is applied 2 . By placing the plate on the lateral side, the tensile force is reduced to prevent crack propagation, and the strain that prohibits bone formation is reduced to promote the healing process 6 . It can also prevent the progression to complete fracture that may occur during nail insertion and maintain lower limb length. Biologically, a previous study reported that lateral plate fixation had advantages over nailing in terms of less intramedullary damage and faster bone union in incomplete ADF 5 . Nevertheless, long‐term follow up might be necessary to identify further progression of deformity and subsequent hardware failure.
Recently, some case reports using plates in an incomplete ADF demonstrated good clinical and radiological results 5 , 6 . Nevertheless, we are concerned about peri‐implant fractures due to stress concentration around the proximal or distal end of the plate by introducing a plate with insufficient length to span the whole length of the femur, as in previous case series. Our speculation for the use of a short plate in previous studies was that, although it was difficult to perform IMN in a severely bowed femur, it was also difficult and required time to contour the longer plate spanning the whole length of the femur during surgery due to the three‐dimensional complex structure of the deformed femur. Moreover, conventional open or mini‐open plating might require extensive incision for placement of the long plate. Thus, we precontoured the plate preoperatively using 3DP RP, and the reconstructed bone model was able to facilitate MIPO during surgery to reduce the operative time. In addition, prophylactic screw fixation toward the femoral neck was performed through the same incision as for plate entry to prevent potential femoral neck fractures due to stress concentration around the tip of the plate. As well as plate fixation in situ according the shape of 3DP RP, we can use this for planning and simulating corrective osteotomy and then fix the osteotomy site with IMN, which might be more sound from a biomechanical point of view. However, this corrective osteotomy may lead to delayed union, non‐union, and limb lengthening. Moreover, both patients had undergone internal fixation for intertrochanteric fractures and had subsequent limb shortening on the contralateral side. Thus, simple valgus osteotomy may aggravate the limb length discrepancy. Even combined shortening osteotomy still has risks for nonunion, delayed union, longer operation time, and more bleeding in patients who are 75 and 78 years of age. Because reduced bone turnover rate and decreased potential for direct bone healing have been reported as characteristics of bisphosphonate‐related ADF 1 , we believe that PCP fixation using MIPO technique could preserve periosteal bone blood supply and subsequent indirect bone healing, similar to that in IMN.
Conclusion
Although IMN is the standard surgical treatment for ADF, we obtained satisfactory results after use of PCP with 3DP RP in incomplete ADF with severe bowing. Based on our experience, PCP fixation using 3DP RP could be an effective treatment option for incomplete ADF with severe bowing.
Disclosure: All authors declare that they have no conflict of interest.
Grant Sources: This work was supported by the Information & Communication Technology (ICT) Research & Development program of the Institute for Information and Communications Technology Promotion (IITP) and the Ministry of Science and ICT (MSIT) (2019–0‐01682, Development of custom artificial ankle joint fusion SW technology based on ceramic 3D printing).
References
- 1. Koh A, Guerado E, Giannoudis PV. Atypical femoral fractures related to bisphosphonate treatment: issues and controversies related to their surgical management. Bone Joint J, 2017, 99: 295–302. [DOI] [PubMed] [Google Scholar]
- 2. Starr J, Tay YKD, Shane E. Current understanding of epidemiology, pathophysiology, and Management of Atypical Femur Fractures. Curr Osteoporos Rep, 2018, 16: 519–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee KJ, Min BW. Surgical treatment of the atypical femoral fracture: overcoming femoral bowing. Hip Pelvis, 2018, 30: 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Yun HH, Oh CH, Yi JW. Subtrochanteric femoral fracture during trochanteric nailing for the treatment of femoral shaft fracture. Clin Orthop Surg, 2013, 5: 230–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tsuchie H, Miyakoshi N, Nishi T, Abe H, Segawa T, Shimada Y. Combined effect of a locking plate and Teriparatide for incomplete atypical femoral fracture: two case reports of curved femurs. Case Rep Orthop, 2015, 2015: 213614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kharazmi M, Michaelsson K, Hallberg P, Schilcher J. Lateral fixation: an alternative surgical approach in the prevention of complete atypical femoral fractures. Eur J Orthop Surg Traumatol, 2018, 28: 299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lee JY, Soh T, Howe TS, Koh JS, Kwek EB, Chua DT. Bisphosphonate‐associated peri‐implant fractures: a new clinical entity? A series of 10 patients with 11 fractures. Acta Orthop, 2015, 86: 622–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sasaki S, Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. Low‐energy diaphyseal femoral fractures associated with bisphosphonate use and severe curved femur: a case series. J Bone Miner Metab, 2012, 30: 561–567. [DOI] [PubMed] [Google Scholar]
- 9. Shane E, Burr D, Abrahamsen B, et al Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res, 2014, 29: 1–23. [DOI] [PubMed] [Google Scholar]
- 10. Min BW, Koo KH, Park YS, et al Scoring system for identifying impending complete fractures in incomplete atypical femoral fractures. J Clin Endocrinol Metab, 2017, 102: 545–550. [DOI] [PubMed] [Google Scholar]


