Abstract
Objectives
To assess the clinical outcomes of using a bipedicle advancement flap to cover the skin defects after digital mucous cyst (DMC) excision.
Methods
Data for 15 patients (18 fingers) with DMC, admitted to the Department of Orthopaedics and Surgery of the Affiliated Zhongshan Hospital of Dalian University from January 2016 to January 2018, were analyzed retrospectively. This study included 4 men and 11 women, with a mean age of 64 ± 7.8 years (range, 47–77 years). A total of 5 cases involved the thumb, 4 involved the index finger, 5 involved ithe middle finger, and 4 involved the ring finger. Among a total of 18 digital mucous cysts, 7 cases were in the left hand and 11 were in the right hand. Approximately 77.8% of cases had osteophytes. The cysts ranged in size from 0.5–1.0 cm to 0.7–1.2 cm. All patients underwent cyst and osteophyte excision and a bipedicle advancement flap to cover the resultant defect. The same surgical procedure was applied to all patients. Postoperative flap survival, healing, and infection were evaluated. The preoperative and postoperative ranges of motion (ROM) of the distal interphalangeal (DIP) and thumb interphalangeal joints (TIPJ) were recorded. Postoperative patient satisfaction was assessed by the visual analog scale (VAS, 0–10) during follow‐up visits. The Shapiro–Wilk test was used to determine whether the data for the difference between the preoperative and postoperative ROM of the DIP/TIPJ were normally distributed or not. The homogeneity of variance was expressed as mean ± standard deviation. A paired t‐test was used to compare the preoperative and postoperative ROM of the DIP/TIPJ.
Results
The patients were followed up for 20 ± 6.0 months (range, 12–36 months). All the flaps survived after surgery, and the incisions healed well. The sutures were removed 2 weeks postoperatively. No infections occurred and there was no cyst recurrence at follow up. After systemic physical therapy and functional exercises, the ROM of all the fingers was restored to the preoperative ROM by 1 month after surgery. The scores for patient satisfaction with surgery by means of the VAS were 8.5 ± 1.0 points, 2.8 ± 1.4 points, 2.0 ± 1.6 points, 1.5 ± 1.2 points, and 1.1 ± 1.3 points preoperatively, and 1, 3, 6, and 12 months postoperatively, respectively. The data for the difference between preoperative and postoperative VAS scores were normally distributed. There were significant differences between the preoperative and postoperative VAS scores. The preoperative DIP/TIPJ ROM was 71.7° ± 14.0°, and the postoperative ROM at 1, 3, 6, and 12 months were 69.3° ± 15.3°, 70.4° ± 12.7°, 71.5° ± 15.6°, and 71.8° ± 15.6°, respectively. The data for the difference between preoperative and postoperative ROM of the DIP/TIPJ were normally distributed. No difference was found between the preoperative and postoperative ROM.
Conclusion
The bipedicle advancement flap provides a simple and effective technique for covering skin defects following DMC excision.
Keywords: Bipedicle advancement flap, Distal interphalangeal joint, Mucous cyst, Osteophyte

(A) A transverse spindle‐shaped incision was made around the site of the thin skin on the surface of the cyst. (B) A new incision with a similar length and arc to the proximal edge of the incisional defect was made at the proximal side of the defect (a:b ≥ 1:2). (C) The incision was sutured.
Introduction
Digital mucous cysts (DMC), also known as myxoid cysts, periungual ganglion cysts, synovial cysts, nail cysts, dorsal cysts, mucous cysts, and myxomatous cutaneous cysts, are benign cysts typically involving the lateral or dorsal surfaces of the distal interphalangeal joings (DIPJ) or thumb interphalangeal joints (TIPJ) or located beneath the proximal nail fold anterior to the nail matrix. They are the most common tumor or cyst of the hand and are often caused by degenerative changes in DIPJ or TIPJ 1 , 2 , 3 , 4 .
Digital mucous cysts tend to occur in middle‐aged and elderly people, with peak incidence rates in those between 40 and 70 years of age. A female‐to‐male predilection of 2:1 is observed in those with DMC 5 . The mechanism of DMC formation remains unknown. Studies have described occupation‐induced DMC resulting from repetitive stress, but such research is limited 6 , 7 . It is widely recognized among scholars that DMC can be due to degenerative changes in the fibroma capsule of the joint or synovial tissue, especially if there is communication between the cyst and adjacent joint space. It is possible that the development of osteophytes and an increase in synovial fluid associated with osteoarthritis (OA) are contributing factors to the formation of DMC. According to some reports, the prevalence of mucous cysts in OA of DIP/TIPJ ranges from 64% to 93% 8 , 9 , 10 .
The pathogenesis and development of DMC likely relate to degenerative, metaplastic, and neoplastic processes. Currently, there are two independent mechanisms. Considered as a focal cutaneous mucinosis, DMC of the myxomatous (superficial) type are independent of the adjacent joint, with growth owing to metaplasia of dermal fibroblasts leading to excess production of hyaluronic acid, the viscous fluid extruded with the opening of the cyst 11 . In the second type of DMC, referred to as the ganglion (deep) type, there is a pedicle which enables communication of the cyst with the joint cavity 2 , 10 . Clinically, the cysts are round to oval, rubbery nodules on the lateral or dorsal surfaces of fingers and occasionally on toes. They mainly occur on the index and middle fingers and are more often on the dominant hand. They are usually slow‐growing, well‐localized, solitary masses 5 . Occasionally, multiple mucous cysts have been observed concurrently 6 . DMC are often asymptomatic, but occasionally pain and tenderness are experienced, as well as nail deformities and decreased ROM. Although several conservative therapies have been performed, including expression of cystic contents, cryosurgery, CO2 laser therapy, steroid/sclerosant injection, and infrared coagulation 12 , 13 , 14 , 15 , 16 , 17 , surgical excision management is the first‐line treatment because of its high cure rate 5 .
However, many patients have skin defects that are too large to be sutured directly, and skin necrosis may occur after surgery due to high tension at the incision after removal of a DMC. Various reconstructive methods have been reported for these skin defects, such as skin grafting and skin flaps. Yet, skin grafting requires additional procedures and causes donor site morbidity 3 , and the function of the grafted skin is often poor. Many authors believe that the risk of skin necrosis is reduced by skin flaps (e.g. rotation flaps, rhomboid flaps, and digital artery perforator flaps), which allow excision of mucous deposits invading the thin skin overlying the cyst. Therefore, many authors advocate skin excision and the use of local flaps to cover the resulting defect. Imran et al. designed a rhomboid flap to cover the defect with no complications 18 . Jiménez and his team designed a Zitelli bilobed flap for skin coverage after cyst excision, with no flap necrosis and no nail deformities developing after the surgery 19 . Okochi and his colleagues reported a lateral finger flap for skin coverage of the defect after the excision, with no flap necrosis, infection, or hematoma 20 . Crawford et al. reported a Kleinert rotation‐advancement skin flap, with a better cosmetic result and no flap necrosis and infection4. Johnson SM reported a local advancement skin flap and did not observe skin necrosis during the follow up 21 .
The recurrence of DMC is another challenge. It is widely accepted that recurrence after mucous cyst excision may result from incomplete removal of either the pedicle or the osteophyte 18 , 20 . Therefore, complete removal of the pedicle and osteophyte are two important steps in treating DMC. Current accepted practices involve removal of the DMC and pedicle, partial capsulectomy, and osteophytectomy at the DIPJ/TIPJ, with lower recurrence rates compared to all other treatment modalities. Eaton and colleagues reported recurrence in 1 of 44 patients (2.3%) with osteophytectomy 22 . Kleinert et al. reported no recurrence with pedicle and osteophyte excision 23 . Yamashita reported no recurrence with excision of both the cyst and osteophytes 24 .
Although these flaps can sufficiently repair skin defects after DMC removal and lead to excellent results, the procedure is challenging in terms of significant donor site morbidity and requires intensive postoperative monitoring, microsurgical skill, appropriate equipment, and many operating room resources 21 . Therefore, identifying a simpler and easier method is necessary. The purpose of this retrospective study is to: (i) evaluate the outcomes of treating DMC using cyst and osteophyte excision and a bipedicle advancement flap to cover the defect; (ii) to evaluate patients' satisfaction with surgery outcomes according to VAS; and (iii) to assess the influence on the ROM of the DIP/TIPJ caused by the surgery.
Materials and Methods
Inclusion and Exclusion Criteria
The inclusion criteria were: (i) patients diagnosed with DMC; (ii) patients treated with cyst and osteophyte excision and a bipedicle advancement flap to cover the defect; (iii) postoperative flap survival, incision healing and infection were evaluated, the ROM of the DIP/TIPJ was measured 2 months postoperatively, postoperative patient satisfaction was assessed using the VAS score at the 12‐month follow up, and reoperative and postoperative comparisons were made with the ROM of DIP/TIPJ; (iv) there was no significant difference between the preoperative and postoperative ROM of the DIPJ/TIPJ; and (v) a retrospective study.
The exclusion criteria were: (i) septic DIP or thumb IP arthritis; (ii) subungual cysts resulting in severe nail deformity; (iii) cyst rupture with infection; or (iv) a comorbidity that may influence the clinical effect of the flap, such as diabetes, rheumatoid arthritis, and gout.
General Information
This retrospective analysis included data for 15 patients (18 fingers) with DMC who underwent cyst and osteophyte excision with the application of a bipedicle advancement flap to cover the resultant defect from January 2016 to January 2018 in the Department of Orthopaedics and Surgery of the Affiliated Zhongshan Hospital of Dalian University. There were 4 male and 11 female patients, with a mean age of 64 ± 7.8 years (range, 47–77 years). A total of 5 cases involved the thumb, 4 involved the index finger, 5 involved the middle finger, and 4 involved the ring finger. The cysts ranged in size from 0.5–1.0 cm to 0.7–1.2 cm. Among the total 18 mucous cysts, there were 7 cases on left hands and 11 cases on right hands. Approximately 77.8% of cases had osteophytes. The characteristics of the patients are shown in Table 1.
TABLE 1.
Summary of the results
| Indicator | (Mean ± SD) | P‐value | |
|---|---|---|---|
| Shapiro–Wilk test* | Paired t‐test* | ||
| Preoperative DIP/TIPJ ROM † | |||
| Preoperative | 71.7° ± 14.0° | ||
| Postoperative 1 month | 69.3° ± 15.3° | 0.694 | 0.83 |
| Postoperative 3‐month | 70.4° ± 12.7° | 0.713 | 0.78 |
| Postoperative 6‐month | 71.5° ± 15.6° | 0.745 | 0.82 |
| Postoperative 12‐month | 71.8° ± 15.6° | 0.796 | 0.93 |
| VAS score ‡ | |||
| Preoperative | 8.5 ± 1.0 | ||
| Postoperative 1‐month | 2.8 ± 1.4 | 0.143 | <0.001 |
| Postoperative 3‐month | 2.0 ± 1.6 | 0.236 | <0.001 |
| Postoperative 6‐month | 1.5 ± 1.2 | 0.276 | <0.001 |
| Postoperative 12‐month | 1.1 ± 1.3 | 0.216 | <0.001 |
Compared to the preoperative value.
DIP/TIPJ ROM, range of motion of the distal interphalangeal/thumb interphalangeal joint.
VAS score, visual analog scale score.
Preoperative Preparation
All patients underwent X‐rays to evaluated osteophyte formation at the cyst site. The preoperative ROM of the DIP/TIPJ was recorded.
Surgical Procedure
Anesthesia and Position
The surgery was performed under a digital nerve block using 2% lidocaine solution. The patient was placed in a supine position, and the affected hand was placed on the operating table. A digital tourniquet was applied.
Incision and cyst excision with osteophyte
A transverse spindle‐shaped incision was made around the thin skin on the surface of the cyst, and the length of the incision exceeded that of the cyst (Fig. 1A). Because the skin on the surface of the cyst was very thin and could not be dissected, this skin was excised with the cyst. If there was a pedicle that connected the cyst to the joint cavity, it was also be removed completely. After the cyst was completely resected, a longitudinal incision was made in the joint capsule using the preoperative X‐ray findings and palpation to locate the position of the osteophyte, and the osteophyte was completely removed with a rongeur. The extent of osteophytectomy did not exceed the edge of the normal articular cartilage. The joint capsule was sutured tightly. Then, the tourniquet was removed to observe blood circulation, and any skin without blood circulation was resected completely, leaving a spindle‐shaped skin defect.
Fig. 1.
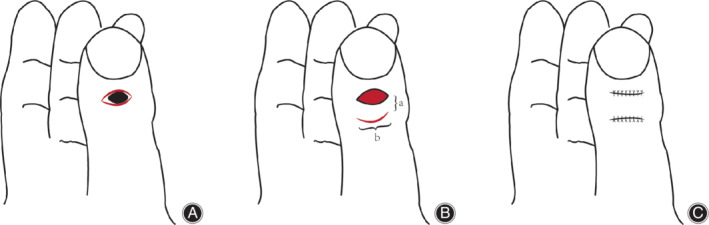
(A) A transverse spindle‐shaped incision was made around the site of the thin skin on the surface of the cyst. (B) A new incision with a similar length and arc to the proximal edge of the incisional defect was made at the proximal side of the defect (a:b ≥ 1:2). (C) The incision was sutured.
Design of the Bipedicle Advancement Flap
At the proximal side of the defect, a new incision with a similar length and arc to the proximal edge of the incisional defect was made (Fig. 1B). The distance between the two incisions was at least half the length of the proximal edge of the incisional defect (a:b ≥ 1:2). The new incision extended along the surface of the extensor tendon. The tissue was separated from the surface of the tendon, and then an advancement flap with two pedicles was created. The flap was pulled to the distal end to allow the defect to be sutured with little to no tension. The proximal edge of the new incision was also separated along the proximal side of the surface of the tendon and pulled to the distal side, and then the new incision was sutured. Finally, the defect was covered with the bipedicle advancement flap (Fig. 1C). Figure 2A–E shows a representative case.
Fig. 2.

(A) Preoperative anteroposterior (AP) and oblique radiographs. The osteophyte is shown (red arrow). (B) A transverse spindle‐shaped incision was made around the site of thin skin on the surface of the cyst. The length of the incision exceeded that of the cyst. (C) The thin skin was excised with the cyst. Then, a new incision with a similar length and arc to the proximal edge of the incisional defect was made at the proximal side of the defect. (D) The defect was covered with the bipedicle advancement flap. (E) Postoperative AP and oblique radiography. The osteophyte was completely removed (red arrow).
Postoperative Treatment
Dressing change was performed for every 3 days after the operation to observe the flap survival, wound healing, and infection. The sutures were removed 2 weeks postsurgery. Active movement of the DIP/TIPJ began on the 3rd day after surgery and there was no obvious joint pain. Patients were to avoid excessive flexion and extension of the joint for 3 weeks and to start normal functional exercise after 4 weeks.
Clinical Evaluation
Postoperative flap survival, incision healing, and infection were evaluated. The ROM of the DIP/TIPJ was measured 1, 3, 6 and 12 months postoperatively. Postoperative patient satisfaction was assessed using the VAS score at 1, 3, 6, and 12‐month follow‐up.
Range of Motion of the Distal Interphalangeal/Thumb Interphalangeal Joints
The ROM refers to the distance and direction a joint can move between the flexed position and the extended position. Devices to measure range of motion in the joints of the body include the goniometer and inclinometer, which use a stationary arm, protractor, fulcrum, and a movement arm to measure the angle from the axis of the joint. Each specific joint has a normal range of motion that is expressed in degrees. The normal ROM of the DIPJ is 60°–90°. The normal ROM of the TIPJ is 90°. Pain, swelling, and stiffness associated with arthritis can limit the range of motion of a particular joint and impair function and the ability to perform usual daily activities.
Visual Analog Scale
Affected finger pain is an important sign and a frequent patient complaint. A self‐reported score on the 10‐point VAS was used for the assessment of patients' pain. A minimum of 0 indicates no pain. A score of 1–3 indicates mild pain, with the sleep quality of patients not affected; 4–6 indicates moderate pain, with sleep quality affected; 7–10 indicates severe pain, with patients not able to sleep due to pain; the maximum value is 10.
Intraoperative Recommendations
When designing the incision, the length of the incision exceeded that of the cyst because of the skin on the surface of the cyst being very thin, not being dissected, and being excised with the cyst.
The long diameter of the transverse spindle‐shaped incision should be parallel to the skin of the dorsal side of the thumb IP or DIP joint, allowing the surgical scar to be easily hidden.
The osteophyte was completely removed. The extent of the osteophytectomy cannot exceed the edge of the normal articular cartilage.
The ratio of the length to the width of the bipedicle advancement flap is less than 2:1, to enable a sufficient blood supply.
The flap pedicle and the digital extensor tendon should be protected carefully.
Statistical Analysis
SPSS Statistics 22.0 software (IBM SPSS, Chicago, IL, USA) was used for all statistical analyses. The Shapiro–Wilk test was used to determine whether the measurement data were normally distributed. The homogeneity of variance was expressed as mean ± standard deviation. A paired t‐test was used to compare the preoperative and postoperative ROM of the DIP/TIPJ. A 5% significance level was applied for all tests (P < 0.05).
Results
General Results
All patients were examined at 1, 3, 6, and 12 months after the surgery and every year thereafter through the outpatient service. The patients were followed up for 20 ± 6.0 months (range, 12–36 months).
There were 15 patients with 18 DMC cases in this study. All the flaps survived after surgery, and the incisions healed well. No infections occurred. The sutures were removed 2 weeks postoperatively. Basic information on patients is listed in Table 1. No cyst recurrence was noted. After systemic physical therapy and functional exercises, the ROM of all the fingers was restored to the preoperative ROM by 1 month after surgery.
Functional Evaluation
Visual Analog Scale
The preoperative pain was more obvious and the average VAS score reached 8.5 ± 1.0 points. The scores were significantly decreased at 1 month after surgery and the average score was 2.8 ± 1.4 points. At the 3, 6, and 12‐month follow up, the average VAS scores were 2.0 ± 1.6 points, 1.5 ± 1.2 points, and 1.1 ± 1.3 points, respectively. According to the P‐value of the Shapiro–Wilk test, the data for the difference between preoperative and postoperative VAS were normally distributed. There was significant difference between the preoperative and postoperative VAS score (Table 1).
Range of Motion of the Distal Interphalangeal/Thumb Interphalangeal Joints
The preoperative DIP/TIPJ ROM was 71.7° ± 14.0° (range 42°–92°), and the postoperative ROM at 1, 3, 6, and 12‐month follow up were 69.3° ± 15.3°, 70.4° ± 12.7°, 71.5° ± 15.6°, and 71.8° ± 15.6°, respectively. According to the P‐value of the Shapiro–Wilk test, the data for the difference between preoperative and postoperative ROM of the DIP/TIPJ were normally distributed. No difference was found between the preoperative and postoperative ROM of the DIP/TIPJ (Table 1).
Discussion
Summary of the Major Results of the Study
The aim of this study was to evaluate the outcomes of treating DMC using cyst and osteophyte excision and a bipedicle advancement flap to cover the defect. In our research, DMC were treated with cyst resection, osteophytectomy, and a bipedicle advancement flap to cover the defect. All the flaps survived after surgery, and the incisions healed well. No infections occurred, and no cyst recurred during the follow up. No difference was found between the preoperative and postoperative ROM of the DIP/TIPJ.
Osteophytes
Whether removing osteophytes is necessary remains controversial. Although some authors have reported successful treatment of DMC without osteophytectomy 25 , it is widely accepted that recurrence after mucous cyst excision may result from incomplete removal of either the pedicle or the osteophyte, and removing these components is an important step for treating DMC and results in a low cyst recurrence rate 8 . However, some authors have reported that aggressive osteophytectomy causes a decreased ROM of the DIP joint. In our study, osteophyte formation was found in 14 fingers, and all the osteophytes were removed. We ensured that the excision did not involve the edge of the normal articular cartilage when the osteophytes were removed. We also removed any pedicle that connected the cyst to the joint cavity.
Bipedicle Advancement Flaps
The usefulness of bipedicle advancement flaps to cover skin defects has been established, and the use of such flaps has been widely reported in the literature in various anatomic areas, including the scalp, eyelids, ears, upper forehead, nose, chin, mucosa, lip, neck, trunk, and extremities 26 . However, only a few studies have reported using this flap to cover defects after removal of a DMC. Mucous cysts are subcutaneous but may be covered with thin skin with or without ulceration. In this study, the bipedicle advancement flap was used to cover the postoperative skin defect when the incision could not be sutured directly due to high tension at the incision. When we made the second incision, we used a similar length and arc to the proximal edge of the incisional defect and maintained a distance between the two incisions of at least half the length of the proximal incisional edge. The new incision extended along the extensor tendon surface, and the flap was separated from the tendon surface. These steps were performed to maintain as much blood circulation as possible to the flap.
The use of a bipedicle flap for skin coverage after DMC excision has the following advantages: 1.The flap is safe due to its dual pedicle blood supply, thus decreasing the risk of flap necrosis or flap failure.
2.Bipedicle flaps allow increased tissue movement by direct advancement. The artery providing the blood supply does not need to be dissected, and the flap pedicle does not need to be twisted when covering the defect.
3. Use of this flap often allows scars to be hidden in the skin lines of the dorsal side of the DIP/TIPJ; 4. donor site morbidity and postoperative monitoring requirements are minimal. As the flaps use local tissue, the surgeon has a greater ability to successfully match the skin color and texture.
5. Importantly, once a bipedicle flap fails, other strategies can still be applied to cover the defect 27 .
Limitations of the study
The study included a small number of patients, was designed as a retrospective analysis, and did not include a comparison with other treatments. In addition, the follow‐up time was short. Due to these factors, the conclusion reached may be biased. A prospective clinical study is planned to compare the efficacy of cyst and osteophyte excision and a bipedicle advancement flap to cover the resultant defect with other techniques.
Conclusion
In conclusion, mucous cyst excision together with removal of osteophytes on the affected side, and coverage with a bipedicle advancement flap provide reliable treatment results with high patient satisfaction and a low recurrence rate.
Acknowledgments
Thanks to all patients involved in this study from the Affiliated Zhongshan Hospital of Dalian University.
Disclosure: This research received no specific grant from any founding agency in the public, commercial, or not‐for‐profit sectors.
References
- 1. MacCollum MS. Mucous cysts of the fingers. Br J Plast Surg, 1975, 28: 118–120. [DOI] [PubMed] [Google Scholar]
- 2. Kim EJ, Huh JW, Park HJ. Digital mucous cyst: a clinical‐surgical study. Ann Dermatol, 2017, 29: 69–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lee HJ, Kim PT, Jeon IH, Kyung HS, Ra IH, Kim TK. Osteophyte excision without cyst excision for a mucous cyst of the finger. J Hand Surg Eur Vol, 2014, 39: 258–261. [DOI] [PubMed] [Google Scholar]
- 4. Crawford RJ, Gupta A, Risitano G, Burke FD. Mucous cyst of the distal interphalangeal joint: treatment by simple excision or excision and rotation flap. J Hand Surg Br, 1990, 15: 113–114. [DOI] [PubMed] [Google Scholar]
- 5. Jabbour S, Kechichian E, Haber R, Tomb R, Nasr M. Management of digital mucous cysts: a systematic review and treatment algorithm. Int J Dermatol, 2017, 56: 701–708. [DOI] [PubMed] [Google Scholar]
- 6. Pietrzak A, Wojnowska D, Chodorowska G, Dybiec E, Gorzelak M, Urban J. Multiple myxoid cysts of both hands in a cashier‐a case report. Ann Univ Mariae Curie Sklodowska Med, 2003, 58: 478–481. [PubMed] [Google Scholar]
- 7. Connolly M, de Berker DA. Multiple myxoid cysts secondary to occupation. Clin Exp Dermatol, 2006, 31: 404–406. [DOI] [PubMed] [Google Scholar]
- 8. Kanaya K, Wada T, Iba K, Yamashita T. Total dorsal capsulectomy for the treatment of mucous cysts. J Hand Surg Am, 2014, 39: 1063–1067. [DOI] [PubMed] [Google Scholar]
- 9. Fritz GR, Stern PJ, Dickey M. Complications following mucous cyst excision. J Hand Surg Br, 1997, 22: 222–225. [DOI] [PubMed] [Google Scholar]
- 10. Li K, Barankin B. Digital mucous cysts. J Cutan Med Surg, 2010, 14: 199–206. [DOI] [PubMed] [Google Scholar]
- 11. Johnson WC, Helwig EB. Cutaneous focal mucinosis. A clinicopathological and histochemical study. Arch Dermatol, 1966, 93: 13–20. [PubMed] [Google Scholar]
- 12. Karrer S, Hohenleutner U, Szeimies RM, Landthaler M. Treatment of digital mucous cysts with a carbon dioxide laser. Acta Derm Venereol, 1999, 79: 224–225. [DOI] [PubMed] [Google Scholar]
- 13. Minami S, Nakagawa N, Ito T, et al A simple and effective technique for the cryotherapy of digital mucous cysts. Dermatol Surg, 2007, 33: 1280–1282. [DOI] [PubMed] [Google Scholar]
- 14. Weinheimer K, Patrick N, Darowish M. Treatment of distal Interphalangeal ganglion cysts by volar corticosteroid injection. Hand, 2019, 14: 381–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Esson GA, Holme SA. Treatment of 63 subjects with digital mucous cysts with percutaneous Sclerotherapy using Polidocanol. Dermatol Surg, 2016, 42: 59–62. [DOI] [PubMed] [Google Scholar]
- 16. Park SE, Park EJ, Kim SS, Kim CW. Treatment of digital mucous cysts with intralesional sodium tetradecyl sulfate injection. Dermatol Surg, 2014, 40: 1249–1254. [DOI] [PubMed] [Google Scholar]
- 17. Kemmett D, Colver GB. Myxoid cysts treated by infra‐red coagulation. Clin Exp Dermatol, 1994, 19: 118–120. [DOI] [PubMed] [Google Scholar]
- 18. Imran D, Koukkou C, Bainbridge LC. The rhomboid flap: a simple technique to cover the skin defect produced by excision of a mucous cyst of a digit. J Bone Joint Surg Br, 2003, 85: 60–862. [PubMed] [Google Scholar]
- 19. Jiménez I, Delgado PJ, Kaempf de Oliveira R. The Zitelli Bilobed flap on skin coverage after mucous cyst excision: a retrospective cohort of 33 cases. J Hand Surg Am, 2017, 42: 506–550. [DOI] [PubMed] [Google Scholar]
- 20. Okochi M, Saito M, Ueda K. Simple and easy reconstruction of nail matrix lesion using lateral finger flap after excision of digital mucous cyst. Case Reports Plast Surg Hand Surg, 2016, 3: 16–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnson SM, Treon K, Thomas S, Cox QG. A reliable surgical treatment for digital mucous cysts. J Hand Surg Eur Vol, 2014, 39: 856–860. [DOI] [PubMed] [Google Scholar]
- 22. Eaton RG, Dobranski AI, Littler JW. Marginal osteophyte excision in treatment of mucous cysts. J Bone Joint Surg Am, 1973, 55: 570–574. [PubMed] [Google Scholar]
- 23. Kleinert HE, Kutz JE, Fishman JH, McCraw LH. Etiology and treatment of the so‐called mucous cyst of the finger. J Bone Joint Surg Am, 1972, 54: 1455–1458. [PubMed] [Google Scholar]
- 24. Yamashita Y, Nagae H, Yamato R, Sedo H, Abe Y, Hashimoto I. Proximal nail fold flap for digital mucous cyst excision. J Med Invest, 2016, 63: 278–280. [DOI] [PubMed] [Google Scholar]
- 25. Flint ID, Siegle RJ. The bipedicle flap revisited. J Dermatol Surg Oncol, 1994, 20: 394–400. [DOI] [PubMed] [Google Scholar]
- 26. Lawrence C. Skin excision and osteophyte removal is not required in the surgical treatment of digital myxoid cysts. Arch Dermatol, 2005, 141: 1560–1564. [DOI] [PubMed] [Google Scholar]
- 27. Granzow JW, Li A, Suliman A, Caton A, Goldberg M, Boyd JB. Bipedicled flaps in posttraumatic lower‐extremity reconstruction. J Plast Reconstr Aesthet Surg, 2013, 66: 1415–1420. [DOI] [PubMed] [Google Scholar]


