Abstract
Objective
We assessed the impact of the transition from a primarily paper‐based electronic health record (EHR) to a comprehensive EHR on emergency physician work tasks and efficiency in an academic emergency department (ED).
Methods
We conducted a time motion study of emergency physicians on shift in our ED. Fifteen emergency physicians were directly observed for two 4‐hour sessions prior to EHR implementation, during go live, and then during post‐implementation. Observers performed continuous observation and measured times for the following tasks: chart review, direct patient care, documentation, physical movement, communication, teaching, handover, and other. We compared time spent on tasks during the 3 phases of transition and analyzed mean times for the tasks per patient and per shift using 2‐tailed t test for comparison.
Results
Physicians saw fewer patients per shift during go‐live (0.51 patient/hour, P < 0.01), patient efficiency increased in post‐implementation but did not recover to baseline (−0.31 patient/hour, P = 0.03). From pre‐implementation to post‐implementation, we observed a trend towards increased physician time spent charting (+54 seconds/patient, P = 0.05) and documenting (+36 seconds/patient, P = 0.36); time spent doing direct patient care trended towards decreasing (−0.43 seconds/patient, P = 0.23). A small percentage of shifts were spent receiving technical support and time spent on teaching activities remained relatively stable during EHR transition.
Conclusion
A new EHR impacts emergency physician task allocation and several changes are sustained post‐implementation. Physician efficiency decreased and did not recover to baseline. Understanding workflow changes during transition to EHR in the ED is necessary to develop strategies to maintain quality of care.
Keywords: electronic health record, physician workflow, time‐motion study
1. INTRODUCTION
1.1. Background
Adoption of a new electronic health record (EHR) has the potential to improve the delivery of care to patients by increasing the efficiency of information sharing between clinical staff. 1 EHR is currently the standard of practice for some hospitals. 2 Commonly cited EHR benefits include centralized clinical information and streamlined communication, automated safety warnings of potential drug interactions, and improved patient experience through the ability to provide patients with electronic access to their own chart. 2 , 3 However, introduction of EHR can create radical changes in task allocation, work processes, and efficiency for clinicians.
1.2. Importance
The emergency department (ED) faces unique challenges during hospital EHR implementation. 4 , 5 Despite transitioning to an EHR system, emergency physicians cannot alter the volume of patients presenting to the ED and, therefore, must maintain efficiency and productivity while continuing to provide quality care. As staff initially adapt to a new EHR system, workflow may suffer but, once staff become familiar with the system, there is a potential to improve work and information flow. 6 , 7 , 8 Limited studies have sought to examine changes in physician task allocation and time spent teaching learners before and after EHR implementation as well as the long term impact of adapting to new EHR system in the ED environment. 6 Understanding how emergency physicians alter their clinical time longitudinally during adoption of an EHR system in an academic ED is necessary to optimize support for successful transition.
1.3. Goals of this investigation
In June 2019, The Ottawa Hospital transitioned from a primarily paper‐based EHR to a comprehensive EHR (Epic) using a “big bang” approach, whereby the entire hospital transitioned to the new system on the same day. 9 The objective of this study was to assess the impact of the transition to Epic on emergency physician work activities in a tertiary care academic ED longitudinally during initial implementation (go‐live) and post‐implementation.
The Bottom Line
A time motion study in a single, academic emergency department of the impact of the transition from a primarily paper‐based electronic health record (EHR) to a computerized EHR showed that physicians saw 0.51 fewer patients per hour during the go‐live period and 0.31 fewer patients per hour in the post implementation period. These results suggest that strategies are needed to address workflow and efficiency when implementing a computerized EHR.
2. METHODS
2.1. Study design
We conducted a time motion observation study over 3 time periods during the transition to a new Epic EHR system (Figure 1): pre‐implementation (phase 1), go‐live (phase 2), and post‐implementation (phase 3). Phase 1 was from March 1–May 31, 2019, phase 2 was from July 1–September 1, 2019, and phase 3 was from January 1–March 1, 2020. Because the EHR was implemented on June 1, 2019, the pre‐implementation period spanned the 3 months before, and the go‐live period started 1 month after for a 3‐month duration. No observations were done during the first month of Epic go‐live to allow for a wash‐out period during expected technical glitches and initial optimization. To allow stabilization of practice habits, the post‐implementation observations were conducted 6–8 months after implementation.
FIGURE 1.
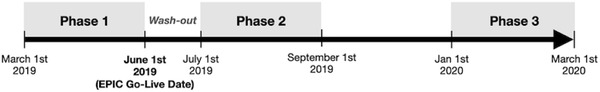
Timeline of EHR Implementation
2.2. Setting
The Ottawa Hospital is an academic tertiary care hospital comprising 2 ED campuses with ≈174,000 patient visits per year. During the study period there were ≈500 ED visits a day. The ED is staffed by ≈90 physicians. Most shifts are also staffed with residents (emergency medicine and off‐service) and medical students.
2.3. EHR implementation
Prior to the adoption of Epic EHR, The Ottawa Hospital ED used a primarily paper‐based EHR (OACIS), in which laboratory reports could be viewed electronically, but prescriptions and patient chart information were hand‐written. Post implementation, Epic adoption made the hospital a level 6 Healthcare Information and Management Systems Society (HIMMS) Electronic Medical Record Adoption Model. 10 The Epic EHR system provides patient problem lists, medications, allergies, test values, and imaging reports electronically. All nursing and physician's notes are documented either by dictation or a typed electronic entry. Patient orders, prescriptions, outpatient and inpatient referrals, as well as communications between the care team, are all electronic. All emergency physicians received the same Epic standard training which consisted of 2 4‐hour classroom sessions and “at‐the‐elbow” support by Epic trainers on shift during the first month following implementation.
2.4. Observers
Shift observers/data collectors (“observers”) were volunteer medical students. Study investigators trained the 6 observers during a 2‐hour training session. The training session reviewed task categories (Table 1), the data collection tool, and provided practice coding using mock scenarios. All observers also completed 4 hours of direct time‐motion practice observation during an ED shift with one of the investigators (SCS or EK). The investigator‐trainers (SCS, EK, and GC) provided feedback to ensure consistent data collection approaches among all observers.
TABLE 1.
Definitions of time motion categories and emergency physician activities
| Category | Activity |
|---|---|
| Chart review | Retrieving or reviewing data prior to seeing patient |
| Direct patient care | Having direct patient contact |
| Documentation | Inputting data into a document |
| Team communication | Communicating verbally in person or on the phone with a nurse, clerk, consultant, radiologist, allied health care professional, or nursing home |
| Discrete teaching | Orienting or directly teaching a student/resident about a medical topic |
| Technical/logistical teaching | Teaching a student/resident logistical EHR functions |
| Clinical case review with learner | Reviewing student/resident case presentation |
| Handover | Directly handing over care of a patient to a different emergency physician |
| Physical movement | Walking to and from any task |
| Tech/IT support | Receiving technical or IT support to complete work |
| Other | Any other activity done by the physician on shift: chit/chat, taking break, going to the bathroom, having dinner, etc |
2.5. Data collection
Fifteen physician participants were selected for time motion observations and represented a range in patient flow efficiencies based on previous ED performance metrics (Table 2). The physician participants were observed in all 3 study phases. Physicians on the Epic implementation team were not eligible to participate in this study.
TABLE 2.
Characteristics of physicians and shifts observed
| Phase 1 Pre‐implementation | Phase 2 Go live | Phase 3 Post‐implementation | |
|---|---|---|---|
| Number of physicians observed | 15 | 15 | 15 |
| Male, no. (%) | 11 (73.3) | 11 (73.3) | 11 (73.3) |
| Years in practice:<10, no. (%) 10–20, no. (%) >20, no. (%) | 6 (40.0) 6 (40.0) 4 (26.7) | 6 (40.0) 6 (40.0) 4 (26.7) | 6 (40.) 6 (40.0) 4 (26.7) |
| Physician efficiency tier Low no. (%) Middle no. (%) High no. (%) | 3 (20.0) 6 (40.0) 6 (40.0) | 3 (20.0) 6 (40.0) 6 (40.0) | 3 (20.0) 6 (40.0) 6 (40.0) |
| Time of direct observation (h:m:s) | 116:50:22 | 110:39:25 | 108:03:35 |
| Shift time, no. (%) | 29 (100) | 28 (100) | 27 (100) |
| Beginning of shift | 12 (41.3) | 13 (46.4) | 15 (55.6) |
| End of shift | 17 (58.6) | 15 (53.6) | 12 (44.4) |
All physicians were directly observed for 8 hours during each phase. Observation sessions lasted 4 hours, during either the first or second half of a shift. Shift observations occurred during a range of times throughout the day (Appendix A). The number of observations performed by each observer is outlined in Appendix B. All shift observations occurred in the ambulatory area of our ED, which consists of Canadian Triage and Acuity Scale (CTAS), 2–5 patients who can sit in chairs for assessment and work up. This area of the department was chosen as it was felt there are consistent patient volumes and the patient flow is in the most direct control of the emergency physician.
Observers recorded second‐by‐second observations using a time‐stamped spreadsheet on an iPad to record physician time allocated across tasks (Table 1). Task categories were chosen based on an adaptation of observational categories that previously have been used in the ED as well as current state process mapping of our emergency physician workflow. 11 , 12 A study investigator (GC) performed quality assurance check on each observer's data collection sheets to ensure time estimates were reasonable and consistent among the observers.
2.6. Analysis
Results were analyzed using descriptive statistics. The percentage of time spent by physicians doing defined tasks during pre‐implementation (phase 1), go‐live (phase 2), and post‐implementation (phase 3) were analyzed using 2‐tailed t test for comparison. We compared phase I to phase II, phase II to phase III, and phase I to phase III. Results are presented with associated P values and 95% confidence intervals in Table 3; significance was considered at α < 0.05.
TABLE 3.
Distribution of observed activities across observation periods
| Observed activity | Pre‐implementation (n = 29) Phase I mean (95% CI) | Go‐live (n = 28) Phase II mean (95% CI) | Post‐implementation (n = 27) Phase III mean (95% CI) | Pre‐ to go‐live change Phase I to phase II comparison | P‐value | Go‐live to post‐ change Phase II to phase III comparison | P‐value | Pre‐ to post‐ change Phase I to phase III comparison | P‐value |
|---|---|---|---|---|---|---|---|---|---|
| Chart review min:sec/pt | 2:47 (2:24–3:10) | 2:50 (2:19–3:21) ↑ | 3:41 (2:48–4:35) ↑ | 0:03 | 0.88 NS | 0:51 | 0.09 NS | 0:54 | 0.05 ↑ |
| Direct patient care min:sec/pt | 9:06 (8:23–9:48) | 8:56 (7:57–9:54) ↑ | 8:23 7:25–9:22) ↓ | 0:10 | 0.77 NS | 0:33 | 0.43 NS | 0:43 | 0.23 NS |
| Documentation min:sec/pt | 5:28 (4:45–6:11) | 7:12 (6:06–8:18) ↑ | 6:04 (4:52–7:16) ↓ | 1:44 | 0.01 ↑ | 1:08 | 0.16 NS | 0:36 | 0.38 NS |
| Patient efficiency patients seen/hour | 2.72 (2.54–2.90) | 2.21 (2.00–2.42) ↓ | 2.41 (2.19–2.63) ↑ | 0.51 | <0.01 ↓ | 0.2 | 0.18 NS | 0.31 | 0.03 ↓ |
| Tech/IT support proportion of shift | N/A | 0.8 ( 0.4–1.2) | 0.2 (0.1–0.3) ↓ | N/A | 0.6 | <0.01 NS | N/A | ||
| Learner activities (n = 13) | Learner activities (n = 24) | Learner activities (n = 20) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| All learner activities % of shift | 12.8 (9.0–16.6) | 15.3 (12.5–18.1) ↑ | 14.2 (9.2–19.2) ↓ | 2.5 | 0.28 NS | 1.1 | 0.68 NS | 1.4 | 0.68 NS |
| Discrete teaching % of shift | 5.6 (1.8–9.3) | 5.8 (3.6–7.9) ↑ | 5.6 (2.6–8.6) ↓ | 0.2 | 0.91 NS | 0.2 | 0.96 NS | 0.0 | 0.98 NS |
| Tech/logical teaching % of shift | 0.3 (0.0–0.6) | 0.5 (0.2–0.9) ↑ | 0.6 (0.3–0.9) ↑ | 0.2 | 0.37 NS | 0.1 | 0.81 NS | 0.3 | 0.20 NS |
| Clinical case review with learner % of shift | 7.0 (4.7–9.3) | 9.0 (6.9–11.1) ↑ | 8.0 (5.0–11.0) ↓ | 2.0 | 0.21 NS | 1.0 | 0.56 NS | 1.0 | 0.60 NS |
↑↓, indicate statistical significance.
2.7. Ethical considerations
We obtained research ethics exemption for this project by the Ottawa Hospital Research Institute Research Ethics Board (REB).
3. RESULTS
Table 2 describes the physician characteristics that are enrolled in the study. The same 15 physicians were observed throughout the study. Physicians represented varying years of experience in practice and efficiency (patients seen per hour) before study implementation. Performance metrics at our center calculate physician efficiency in comparison to the physician group. Using performance metrics from the previous year, physicians from the slowest third, middle third, and fastest third of our physician group were observed. Approximately half of the observations occurred for the first half of the shift and half of the observations occurred during the second half of the shifts.
Table 3 presents the breakdown of the average time spent by physicians on pre‐specified task categories with associated P values and 95% confidence intervals during pre‐implementation (phase 1), go‐live (phase 2), and post‐implementation (phase 3). In most categories, there was a trend towards increased time spent per patient by physicians doing tasks after EHR implementation. Physician time spent reviewing charts demonstrated a statistically significant trend towards increasing from phase 1 to phase 3 (+54 seconds/patient, P = 0.05), with the biggest increase occurring between phase 2 and phase 3. Physician time spent documenting per patient also trended towards increasing after EHR introduction, but was not statistically significant. Documentation time per patient increased from phase 1 to phase 2 and then decreased in phase 3 but did not return to pre‐implementation levels (+36 seconds/patient between phase 1 and phase 3, P = 0.37).
Physician time spent on direct patient care per patient encounter did not change significantly but trended down following EHR implementation (−43 seconds/patient between phase 1 and phase 3, P = 0.23). Although time spent with each patient remained relatively stable (9:06 minute:second/patient in phase 1 and 8:56 minute:second/patient in phase 2), physician efficiency decreased significantly between phase 1 and phase 2 by 0.51 patient/hour (2.72 patients/hour in phase 1 to 2.21 patients/hour in phase 2, P < 0.01) and only increased by 0.2 patients/hour in phase 3 (2.41 patients/hour in phase 3). Physician efficiency did not recover to pre‐implementation levels and remained statistically decreased from phase 1 to phase 3 (2.72 patients/hour in phase 1 to 2.41 patients/hour in phase 3, −0.31, P = 0.03). As such, although time spent doing direct patient care per patient remained similar, the overall percentage of the physician's shift during which they performed direct patient care decreased significantly from phase 1 to phase 2 (41.1% of shift in phase 1 vs 31.9% of shift in phase 2, P < 0.1). The percentage of the physician shift performing direct patient care did not recover to phase 1 levels during phase 3 (31.9% of shift in phase 2 vs 32.5% of shift in phase 3, P = 0.77).
Table 3 outlines the number of observation shifts during which staff physicians supervised a learner (learner activity). Learners were considered medical students or resident doctors. The number of observation shifts with learners present was 13 during phase 1, 24 during phase 2, and 20 during phase 3. Figure 2 represents the proportion of shifts distributed across all activities. Across all teaching categories, the proportion of the shift with learners present that physicians spent doing activities involving a learner remained relatively stable—between 12.8% to 14.2% of shift time with learners was spent teaching (P = 0.68). Time spent on shift doing discrete teaching was unchanged between phases 1 and 3 (+0.0%, P = 0.98). Technical/logistical teaching and clinical case review with learners trended towards increasing from phase 1 to phase 3 but was not statistically significant (+0.3%, P = 0.2; +1.0%, P = 0.6). The proportion of the shift spent by emergency physicians receiving technical/IT support increased in phase 2 but decreased significantly from phase 2 to phase 3 (−0.6%, P < 0.01).
FIGURE 2.
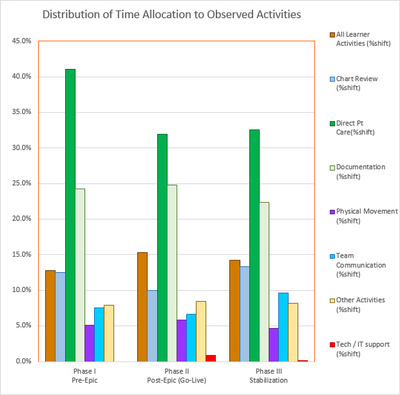
Distribution of time allocated across observation periods
4. LIMITATIONS
This study has several limitations. We limited our direct observations to emergency physicians in an ambulatory care area of our ED and we did not study resident doctors, medical students, or nurses. Our findings document the implementation of a single EHR in one ED implemented using a “big bang” approach and may not be generalizable across other institutions, clinical settings or EHR systems. We did not observe physicians after their scheduled shift time that may have been used to further complete patient chart documentation. Unfortunately, we did not evaluate physician and patient satisfaction that can be a strong concern during EHR implementation. Finally, although we compare time spent per task longitudinally for physician, there are no established standards to identify which distribution of tasks are best for efficiency, quality of care of patients, and optimization of teaching learners.
5. DISCUSSION
This study demonstrates a comprehensive picture of workflow changes in the ED during the EHR go‐live and post‐implementation periods by tracking physician tasks. We found that overall physician workflow changed during the transition to EHR. Although our study validates some anticipated workflow changes during initial EHR implementation, our findings also demonstrate that some changes in workflow are continually sustained throughout the post‐implementation period, even 6–8 months after EHR introduction.
As expected, during the go‐live period, time spent on chart review, documentation, and receiving technical/IT support on shift increased. However, there was a sustained trend toward increased time spent on both chart review and documentation in the post‐implementation period. In fact, time spent on chart review increased most between the go‐live period and the post‐implementation period. The increased time spent on chart review may reflect the improvement in the legibility and usefulness of past medical documentation available in the EHR. Time spent on documentation also showed a sustained increase in the post‐implementation period, which may be attributed to increased space for documentation in the chart resulting in longer patient notes. These findings are consistent with the initial increase in documentation times from a systematic review of pre/post EHR time motion studies in various clinical settings across nurses, physicians, and interns. 6 However, in contrast to the sustained increase in documentation time, Baumann et al 6 demonstrated that, although documentation may initially suffer, it may recover as staff become more familiar with the system. Differences in our study findings may be because of differences in setting: only 1 study included in the systematic review took place in the ED setting. 6 Although reviewing charts and thorough documenting may take more time post‐EHR implementation in the ED setting, detailed charting may positively impact provider information exchange. 1 Improving provider communication is a benefit of a comprehensive EHR that ultimately has the potential to improve patient safety by decreasing medical errors that can result from inadequate clinical data. 1 , 13 Moreover, a well‐functioning EHR that facilitates detailed patient charting adds to data acquisition over time, improves completeness of medical records and allows for easy coding of patient visits for reimbursement and creation of databases for research purposes.
A frequent concern with transition to EHR is that more time will be spent using the computer and less time will be spent doing direct patient care. Our study findings demonstrated a non‐significant trend toward decreased time for physicians performing direct patient care. We also observed a statistically significant overall decrease in physician flow efficiency in both phases 2 and 3. In phase 3, changes in time spent on various physician tasks post‐implementation ultimately resulted in our physicians’ total patient flow rate still an average of 0.3 patients per hour less than in phase 1. These findings are consistent with physician workflow behaviors observed by Meadors et al 11 during the 7‐day period immediately after the EHR go‐live; however, they did not evaluate if this change was sustained. The sustained decrease in patient flow per physician is an important consideration for resource planning and staffing emergency physicians. Although time spent on various tasks on shift has the potential to return to pre‐implementation, sustained changes may occur that require extra resources to maintain efficiency and productivity, because the volume of patients presenting to the ED cannot be altered the same way as in an outpatient clinic. 12
Another concern for our emergency physicians with transition to EHR was that less time would be available for on‐shift teaching. Interestingly, our study demonstrated that the proportion of the shift spent doing discrete teaching around medical topics, teaching around the EHR itself, and reviewing clinical cases remained similar across all periods. These findings may be of interest for academic teaching centers transitioning to EHR; however, more studies are needed to investigate the impact EHR transition has on learner activities.
Overall, changes in time allocated to various task categories are expected to change while integrating new technology and then reverse with long‐term use of the EHR. In particular, physician time completing computer‐based tasks usually increases from the pre‐implementation to the go‐live phase and then reverses. 12 , 14 However, in our study, changes in time spent on direct patient care, chart review, and documentation did not revert back to pre‐implementation levels duration during the post‐implementation period (6–8 months post EHR implementation). Furthermore, overall physician efficiency also remained statistically decreased in the post‐implementation period. Changes in physician workflow processes resulting in decreased overall direct patient care and physician efficiency may impact patient experience and wait times in the ED. Few studies have examined both the immediate and sustained emergency physician workflow changes during the adoption of a new EHR system.
As physicians initially adapt to a new EHR system, changes in time allocated to various tasks changes, with some being sustained post‐implementation. The most pronounced sustained changes are those required for reviewing the patient's chart and doing documentation. Overall physician efficiency also decreases during initial EHR introduction and does not fully recover even 6–8 months post‐implementation. Understanding the emergency physician workflow changes from our study may help other EDs to develop mitigation strategies and solutions to maintain efficiencies and quality of patient care during adoption of a new EHR. Further longer‐term studies are warranted to assess the impact of EHR implementation.
CONFLICT OF INTEREST
The authors have no conflicts of interest to disclose.
Biography
Samantha Calder‐Sprackman, MD, MSc, works in the Department of Emergency Medicine at the University of Ottawa, Ottawa, Ontario, Canada.

APPENDIX A. Distribution of time of day for shifts observed
A.1.
| Pre‐implementation (phase 1) | Go‐live (phase 2) | Post‐implementation (phase 3) | |
|---|---|---|---|
| Start of shift observation | 17 | 15 | 12 |
| End of shift observation | 12 | 13 | 15 |
| Shift start 6:00:00 | 1 | 2 | 0 |
| Shift start 8:00:00 | 0 | 0 | 1 |
| Shift start 9:00:00 | 0 | 1 | 0 |
| Shift start 10:00:00 | 2 | 5 | 0 |
| Shift start 12:00:00 | 0 | 0 | 1 |
| Shift start 13:00:00 | 0 | 1 | 1 |
| Shift start 14:00:00 | 11 | 2 | 5 |
| Shift start 15:00:00 | 1 | 0 | 0 |
| Shift start 16:00:00 | 2 | 4 | 4 |
| Shift start 18:00:00 | 3 | 2 | 8 |
| Shift start 19:00:00 | 0 | 0 | 1 |
| Shift start 20:00:00 | 7 | 10 | 5 |
| Shift start 22:00:00 | 2 | 1 | 1 |
APPENDIX B. Number of observations performed by each observer
B.1.
| Observer ID | Phase 1 | Phase 2 | Phase 3 |
|---|---|---|---|
| A (Trisha) | 6 | 6 | 6 |
| B (Jade) | 6 | 6 | 6 |
| C (Simran) | 6 | 5 | 6 |
| D (Julia) | 6 | 4 | 6 |
| E (Courtney) | 6 | 0 | 6 |
| F (Khadeer) | 0 | 8 | 0 |
APPENDIX C. Distribution of the proportion of observed activities across observation periods
C.1.
| Phase I | Phase II | Phase III | |
|---|---|---|---|
| Observed activity | Pre‐implementation mean (n = 29) | Post‐implementation (go‐live) mean (n = 28) | Post‐implementation (stabilization) mean (n = 27) |
| Chart review (proportion of shift) | 12.5% | 10.0% | 13.4% |
| Direct patient care (proportion of shift) | 41.1% | 31.9% | 32.5% |
| Documentation (proportion of shift) | 24.3% | 24.8% | 22.4% |
| Physical movement (proportion of shift) | 5.1% | 5.8% | 4.6% |
| Team communication (proportion of shift) | 7.5% | 6.6% | 9.6% |
| Other activities (proportion of shift) | 7.9% | 8.5% | 8.2% |
| Non‐patient‐ / Non‐learner‐specific Activities (proportion of shift) | 21.1% | 22.2% | 23.1% |
| Tech/IT support (proportion of shift) | N/A | 0.8% | 0.2% |
| All learner activities (proportion of shift) | 12.8% (n = 13) | 15.3% (n = 24) | 14.2% (n = 20) |
Calder‐Sprackman S, Clapham G, Kandiah T, et al. The impact of adoption of an electronic health record on emergency physician work: A time motion study. JACEP Open. 2021;2:e12362 10.1002/emp2.12362
This work was funded by a grant from the Ottawa Department of Emergency Medicine.
Supervising Editor: Chadd K. Kraus, DO, DrPH.
REFERENCES
- 1. Bates DW, Gawande AA. Improving safety with information technology. N Engl J Med. 2003;348(25):2526–34. [DOI] [PubMed] [Google Scholar]
- 2. Fletcher GS, Payne TH. Selection and implementation of an electronic health record. PM&R. 2017;9(5):S4–12. [DOI] [PubMed] [Google Scholar]
- 3. Menachemi N, Collum TH. Benefits and drawbacks of electronic health record systems. Risk Manag Healthc Policy. 2011;4:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Handel DA, Hackman JL. Implementing electronic health records in the emergency department. J Emerg Med. 2010;38(2):257–63. [DOI] [PubMed] [Google Scholar]
- 5. Kennebeck SS, Timm N, Farrell MK, Spooner SA. Impact of electronic health record implementation on patient flow metrics in a pediatric emergency department. J Am Med Inf Assoc. 2012;19(3):443–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Baumann AL, Baker J, Elshaug AG. The impact of electronic health record systems on clinical documentation times : a systematic review. Health Policy (New York). 2018;122(8):827–36. [DOI] [PubMed] [Google Scholar]
- 7. Asaro P V, Boxerman SB. Effects of computerized provider order entry and nursing documentation on workflow. Acad Emerg Med. 2008;15(10):908–15. [DOI] [PubMed] [Google Scholar]
- 8. Banner L, Olney CM. Automated clinical documentation: does it allow nurses more time for patient care? Comput Inf Nurs. 2009;27(2):75–81. [DOI] [PubMed] [Google Scholar]
- 9. Owens K. EMR implementation: big bang or a phase approach? J Med Pract Manag. 2008;23(5):279–81. [PubMed] [Google Scholar]
- 10. HIMSS Analytics. Electronic Medical Record Adoption Model HIMSS. 2017.
- 11. Meadors M, Benda N, Hettinger AZ, Ratwani RM. Going live: implementing an electronic health record system in the emergency department. Int Symp Hum Factors Ergon Heal Care Adv Cause. 2014;44–9. [Google Scholar]
- 12. Benda NC, Meadors ML, Hettinger AZ, Ratwani RM. Emergency physician task switching increases with the introduction of a commercial electronic health record. Ann Emerg Med. 2016;67(6):741–6. [DOI] [PubMed] [Google Scholar]
- 13. Sidlow R, Katz‐Sidlow RJ. Using a computerized sign‐out system to improve physician‐nurse communication. Jt Comm J Qual Patient Saf. 2006;32(1):32–6. [DOI] [PubMed] [Google Scholar]
- 14. Pizziferri L, Kittler AF, Volk LA, et al. Primary care physician time utilization before and after implementation of an electronic health record : a time‐motion study. J Biomed Inform. 2005;38:176–88. [DOI] [PubMed] [Google Scholar]


