Abstract
The worldwide pandemic caused by the COVID-19 outbreak has led to an unprecedented burden on hospital structures, posing new challenges in terms of reshaping healthcare services. At the same time, the so-called ‘lockdown’ restrictions have decreased overall mobility, thereby challenging the traditional concept of clinical examination. Moreover, the need for security for both patients and healthcare personnel has posed a further limitation to face-to-face meeting. Telemedicine has provided a valuable solution for such issues, allowing the evaluation of oral and maxillofacial surgery patients through technological interfaces, restricting physical consultations to cases with high clinical priority, intercepting suspects, and maintaining contact with discharged patients. Thanks to the experience gained during the previous wave of infections, the purpose of this study was to present a reorganization of clinical services for oral and maxillofacial surgery in order to help cope with the latest COVID-19 resurgence.
Using commonly available software for telecommunications and online meetings, the Oral and Maxillofacial Surgery Department of the University Hospital of Udine has reshaped the organization of healthcare services, with telemedicine central to the continuity of assistance, while at the same time minimizing the risk of exposure for both patients and operators. Additionally, the high number of patients evaluated through telemedicine improved our ability to define signs and symptoms of diseases using informatic tools, thus allowing the introduction of the concept of ‘telesemiology’.
During our previous lockdown experience, between March and April 2020, 78 patients were evaluated using teleconsultation. All outpatient examinations were rescheduled and translated into a virtual platform, allowing each patient to undergo evaluation in the most appropriate setting. Special attention was paid to the follow-up of oncological patients. The rehabilitation team represented a crucial element in maintaining contact with more complex patients in this crucial time.
This study was based on our previous lockdown experience – a situation that many will be facing again over the coming months. Our hope is that the organizational structure that our department applied during the previous wave of infections may offer other colleagues a solution to facing the current COVID-19 recrudescence.
Keywords: COVID-19, Telemedicine, Teleconsultation, Organization model, Facial care project
1. Introduction
The worldwide pandemic caused by the COVID-19 outbreak led to an unprecedented burden on hospital structures, with the need for radical modification of healthcare services in order to manage the emergency. Moreover, the need to arrest the spread of the virus and to protect the most vulnerable patients involved radical changes in assistance paths, including outpatient consultations, inpatient care, and surgery, making it essential to find solutions to ensuring continuity of care, even in this emergency situation (Di Bartolomeo et al., 2020; Zimmermann and Nkenke, 2020). At the same time, governments imposed so-called lockdown restrictions, affecting social life, public mobility, and work places, which in Italy officially began on March 10, 2020.
Since then, traditional healthcare paradigms of have been deeply reshaped, in particular for specialties of the head and neck region, including oral and maxillofacial surgery, dentistry, ENT. Imposed limitations provided the impulse for a conceptual rethinking of traditional models of assistance to patients, initiating remote video consultations, decreasing overcrowding of waiting rooms, postponing all deferrable surgeries, and introducing nasopharyngeal swabs to test patients prior to any procedure (Barca et al., 2020a, 2020b). Such measures were effective in decreasing the spread of infection between healthcare workers, while at the same time protecting the most vulnerable patients.
Since the epidemiological trend at the time raised optimistic predictions, on May 4, 2020 the Italian government initiated the so-called ‘Phase 2’, which abolished many of the restrictions imposed by Phase 1 and allowed a greater circulation of people. Phase 2 constraints were further loosened after the declaration of Phase 3, based on restoring social life to a quasi-ordinary condition. In the months that followed, especially during summer, with the desire for economic recovery and the approval of scientific committees, the government was prompted to progressively revoke all previously imposed limitations. This decision implicitly opened the gates to a potential new wave of infections, a risk concealed by the misguided optimistic predictions raised by a steep decline in daily diagnosed new cases. Since October, Italy reported a worrying rise in daily diagnosed new cases, which had increased from a few hundred during the summer to several thousands during the winter, exceeding the maximum peak reached during the first wave, with reports that intensive care units were close to becoming saturated again.
At the same time, our institution started a close collaboration with rehabilitative medicine, advocating a model of comprehensive care for patients undergoing major maxillofacial surgery procedures, especially for oncological diseases (Al-Maweri et al., 2020; Pareek et al., 2020). In order to maintain our vision of global assistance, which had been jeopardized by the reduction in healthcare personnel and the impossibility for patients to meet their families, we extended the role of telemedicine in our hospital, creating a network organization based on interaction between the hospital and the community, which allowed suspended activities to be conducted using a telemedicine interface (Tel et al., 2020).
This paper provides a solution to avoiding discontinuity in global assistance for patients, illustrating how the Oral and Maxillofacial Surgery Department of the Academic Hospital of Udine maintained the relationship between the hospital and the community during the most critical months of the COVID-19 era. Considering current events, the unfavorable trend of the contagion curve, and the prospect of new restrictions, our purpose is to share the experience gained in the past to allow other colleagues in the field of head and neck specialties to maintain an elevated standard of care, while minimizing the risk of exposure for both patients and physicians.
2. Materials and methods
2.1. Protocol for telemedicine in the Department of Oral and Maxillofacial Surgery
The interface for telemedicine applications adopted at our institution relies entirely upon Zoom software (Zoom Video Communications Inc, San Jose, CA, USA). We designated a physical space in our department for teleconsultations, setting up a dedicated professional workstation (iMac Pro, Apple Inc, Cupertino, CA) with a high-speed internet connection. Schedules of web meetings were shared in the Cloud between all members of our unit using iCal® calendar (Apple Inc, Cupertino, CA). Two nurses normally responsible for the organization of appointments for patients were assigned the management of schedules for teleconsultations, establishing 3 days in each week for teleconsultations. Three clinicians, one senior maxillofacial surgeon, the rehabilitation physician, and one resident worked in rotation to cover the entire session, which was dedicated to telemedicine, organizing web calls, contacting patients, and maintaining communication with spoke hospitals and general practitioners.
Before starting a teleconsultation, the patient was given a copy of the privacy policy and a module containing the information required, including the download link, and a short explanatory description of telemedicine and related possibilities, including limits and pitfalls, with special attention given to privacy issues. Prior to any teleconsultation, patients were asked to sign a copy of the informed consent, which included a statement that teleconsultations do not replace physical examinations. Additionally, patients had to accept or decline the possibility that screenshots of the video consultations could be taken as follow-up. An additional questionnaire was administered enquiring whether the patient owned appropriate technology to undergo teleconsultation. This was particularly important for elderly patients, who in many cases had to seek the assistance of younger familiars – another aspect evaluated by the questionnaire. Teleconsultations were programmed exactly as normal consultations, employing the same management database used in ordinary clinical activity, and the schedule was communicated to each patient by phone call. The Maxillofacial Surgery examination office was assigned a Zoom account with a unique ID, represented by a univocal code composed of 10 characters, transforming the Zoom ID in a virtual room environment (VRE), representing the consultation office. This ID was shared with all patients by sending an institutional email 15 min before the officially scheduled time of the examination. According to the weekly organization, the VRE destined for teleconsultations was made more specific, alternating between options for jaw deformities, oral pathology, temporomandibular joint (TMJ) disease, and pediatrics. A dedicated space was organized for the rehabilitation physician, responsible for the care of recently discharged patients who had previously undergone major surgeries or had experienced complications relating to their surgical treatment. After receiving their ID, the patient was called by telephone and given the meeting password, a second check deemed necessary to avoid possible intrusion. In cases where the previous meeting was still active, the patient entered the waiting room, and was admitted to the teleconsultation only after the previous meeting had concluded. Once the teleconsultation had concluded, the resident recorded it in the clinical registry, validating this with a digital signature, thus replicating the traditional path for ordinary physical consultations.
2.2. The relationship between the hospital and the community in the COVID-19 era
Promoting the widespread adoption of telemedicine for Oral and Maxillofacial Surgery involved a redefinition of the interaction between the hospital and the community. Regional healthcare reorganization played a crucial role in defining the allocation of resources for the treatment of COVID-19 patients with severe respiratory symptoms. During the lockdown, the COVID-19 pandemic prompted the adoption of hub-and-spoke organizational design, which assigned the distribution of healthcare assistance in a network structure, with primary institutions (the ‘hubs’) providing the most complete array of services, and complementary structures (the ‘spokes’) – more widespread in the community – delivering more essential care. The result was that more complex procedures, such as those involving severe trauma or oncology, were referred to hub centers. In fact, as the urgent situation led to a strict redefinition of the times and spaces available for performing surgical procedures, it was important to make a selection of cases to be treated. The availability of a fully connected interface between the community and the hub center allowed a ranking of relevance or urgency, facilitating the triage of those patients needing surgery at a time when resources were limited.
In our region (Friuli Venezia Giulia) the only hub center for oral and maxillofacial surgery is located in Udine, while Trieste and Pordenone, the other hub hospitals, are integrated within a major organization of the Dentistry Faculty. Additionally, minor hospitals serve the coast and the mountain area, but they do not offer specialist consultation in the field of oral and maxillofacial surgery. In addition to this structure, a close relationship has been established with general practitioners, thus establishing a capillary organization to intercept possible diseases deserving immediate clinical attention. During the COVID-19 period, thanks to the support provided by the hub-and-spoke organizational model, all traumas and oncological patients have been referred to our center, as before, maintaining efficient care while ensuring the safety of operators. Additionally, the use of telemedicine to filter access has enabled improved triage, while allowing for decreases in activity and healthcare staff. A summary of the telemedicine-based reorganization of the regional healthcare network is presented in Fig. 1 .
Fig. 1.
Organization of telemedicine services for oral and maxillofacial surgery during COVID-19 lockdown in our region, Friuli Venezia Giulia.
2.3. Virtual outpatient consultations and the ‘telesemiology’ concept
In the COVID-19 era, traditional outpatient consultations pose further challenges and expose operators to significantly higher risk, due to a high flow of patients who cannot systematically undergo nasopharyngeal swab. Therefore, a crucial decision was to modulate the flow of outpatient consultations, decreasing the daily number of patients needing a physical examination by the oral and maxillofacial surgeon. During the pandemic, all non-urgent public and private practice first consultations, identified with the letters D (deferrable) and P (planned), were suspended, maintaining the service only for short-term and urgent consultations, which were identified by the letters U (urgent) and B (short). Priorities were identified by general practitioners, who were specifically instructed by published guidelines and asked to action the emergency requests. Only urgent or non-deferrable outpatient procedures were continued, such as biopsies of suspect oral lesions. Although teleconsultations were used for all fields of oral and maxillofacial surgery, they played the most prominent role for complex categories of patients, especially oncological and recently operated individuals, preferring to maintain them safely at home rather than increasing the unquestionable risk of exposure to contagion.
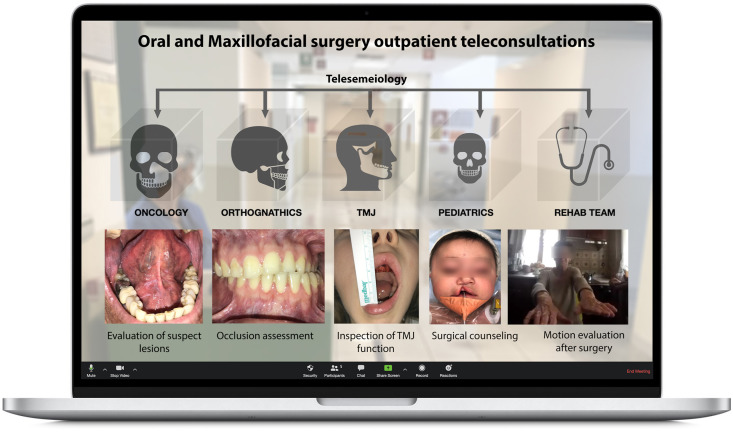
Teleconsultations were performed within the VRE organization, following a well-defined schedule, and were made specific for each type of clinical situation encountered, including oral pathology, jaw deformities, TMJ disorders, pediatrics, and rehabilitation medicine. Thus, the previous organization of outpatient rooms as well as weekly schedules were maintained, but translated into a virtual platform using Zoom (Fig. 2 ).
Fig. 2.
Organization of oral and maxillofacial surgery virtual outpatient consultations using virtual room environments (VREs).
As part of their teleconsultations, clinicians were trained to collect a complete anamnesis and to evaluate visual signs of diseases and surgical complications. Our group introduced the concept of ‘telesemiology’, a novel term coined to define the complex of signs and symptoms detectable through a visual clinical inspection mediated by technological devices. Telesemiology relies upon patients' collaboration, as they are requested to perform specific tasks in front of the camera, with careful guidance by the physician throughout the examination. Cooperation was not always easy, especially for inspection of the oral cavity.
2.4. Checklist for teleconsultations
To further standardize teleconsultations, a prominent role was played by the creation of a checklist, which formed a systematic framework for conducting teleconsultations and a comprehensive tool for standardizing registration of clinical parameters. A section for general evaluation, containing various items, was designed to explore common clinical problems, such as pain, function, temperature, and swelling. More specific sections were designed for each subspecialty, including trauma, jaw deformities (mostly postoperative patients), TMJ disorders, oral pathology and oncology, and rehabilitation. Specific sections incorporated a more detailed telesemiology evaluation, such as mouth opening and referred joint noises in TMJ disorders, and occlusion in jaw deformities. The section for oral pathology and oncology included the evaluation of critical items, such as neck adenopathies, directly appreciable on virtual inspection if grossly visible or eventually referred by the patient as swollen masses, as well as wound examination, and eventually visual assessment of the flap, for recently discharged patients who had undergone complex surgical procedures. As for the rehabilitation items, a dedicated list was designed containing specific exercises the patient was asked to replicate while sitting in front of the camera, aiming to assess potential physical impairments caused by surgery, such as accessory nerve injuries in neck dissections. An overview of the checklist used for telesemiology is presented in Table 1 .
Table 1.
Telesemiology checklist for teleconsultations.
| CHECKLIST FOR TELECONSULTATIONS AND TELESEMIOLOGY |
|---|
| General status |
| 1. Do you have pain? How much on a scale from 0 to 10? Location and description? 2. Do you have fever? What is your temperature? 3. Swelling? Postoperative edema? 4. Are you aware of a bad taste in the mouth or bad smell in the nose? 5. Do you have impaired function? |
| Facial trauma |
| 6. Do you have altered vision, such as diplopia? (specific for orbital surgery) 7. Do you perceive subcutaneous crepitation? 8. Do you feel any change in occlusion? 9. Do you feel any sensory disturbances? 10. Are there any disturbances in motion of the facial muscles? 11. Do you perceive alterations in TMJ function? |
| Jaw deformity/after orthognathic surgery: |
| 1. Do you have reduced sensitivity in the lower lip and chin and inferior dental arch? (specific for mandibular orthognathic surgery) 2. Do you perceive altered occlusion? The same as after discharge, or different? Do you perceive precontacts? 3. What is the extent of mouth opening? 4. Check of elastodontic maneuvers for discharged patients |
| TMJ disorders |
| 1. What is the degree of mouth opening? 2. Do you perceive articular blocks when opening the mouth? Do you perceive clicks? 3. Do you feel pain around the ear, corresponding with the temporomandibular joint? 4. Do you feel pain during chewing movements? 5. Do you perceive any swelling around the joint? |
| Oral pathology and oncology |
| •Visual inspection of the lesion (eventually ask for a physical consultation) •Check of the area of removal for skin cancers, and healing of the scar •Psychological and performance status (weight loss, fatigue) •Mouth opening, tongue movement, speech function •Swallowing, edema, guided self-palpation of the neck, scar of the neck and healing, neck mobility •Check of donor site when a free flap is harvested |
| Rehabilitation |
| •Instructions to perform autonomous physical therapy with demonstration exercises •Evaluation and reassessment of medical therapy •Psychological evaluation and familiar context •Follow-up of postoperative complications •Monitoring of complications after radiation therapy |
3. Results
During the lockdown period of March and April 2020, 78 patients were evaluated using teleconsultations. In all cases, doctors performing the virtual examination followed the items presented in the checklist. Patients were evaluated in the most appropriate VRE, based on their clinical problem, resulting in the following distribution of categories of teleconsultation: 45% oral pathology and oncology, 10% jaw deformities with a previously booked appointment or patients recently discharged form orthognathic surgery, 25% symptomatic TMJ disorders, 5% pediatrics, including intraoperative consultations and referrals from the pediatrics department, 15% rehabilitation cases, mostly including recently operated oncological patients, patients with severe postoperative complications, and fragile patients, often with inadequate social support. In very rare cases — invariably elderly and isolated people — it was not possible to establish a digital contact with the patient, and a telephone triage was performed to establish clinical priorities and eventually call the patient for physical consultation.
Following the resurgence of the pandemic — since October 10, 2020 — we reintroduced systematic teleconsultations to decrease crowding of spaces, and 33 patients were evaluated in this period. Remarkably, three patients sent by the general practitioner for oral disease examination, and initially evaluated through teleconsultations, had a confirmed diagnosis of squamocellular carcinoma of the oral cavity, which we would not have intercepted if the patient had not been evaluated. Given the large number of asymptomatic COVID-19-positive patients who are confined in quarantine, the number of patients requiring teleconsultations is expected to increase.
Patients followed up in the rehabilitation VRE with the rehabilitation physician showed progressive improvement of physical symptoms and were invited to continue their physical therapy alone. Progress was assessed through multiple evaluations by asking the patient to repeat the same physical maneuvers.
Finally, telemedicine allowed continued follow-up for patients for whom seriated assessments played a crucial role, mainly oncological patients, thus maintaining the usual timing of consultations without exposing the patients to unnecessary risk by requiring them to attend a physical evaluation.
4. Discussion
The lessons learnt from Phase 1 of lockdown are not destined to remain historical concepts. Autumn 2020 confirmed the predictions of a new wave of infections; however, we could not have imagined that this new wave would lead to an even higher rate of new cases and place healthcare systems under the same pressure.
It is thus essential to reinstate the changes made to the traditional clinical examination of our patients. Oral and maxillofacial surgeons, and many other specialists involved in the head and neck region, despite not being front-line specialists in facing these diseases, are unquestionably exposed to a high risk of contagion. Moreover, due to the massive reallocation of resources into COVID-19 units, and the need to perform meticulous protection of professionals, there are fewer resources available, both in terms of time to dedicate to each patient for a conventional examination and in terms of healthcare personnel. This will become even more the case when, in the eventuality of a new lockdown, the necessary reorganzarion of shifts will mean a halving of the number of professionals available (Chigurupati et al., 2020). In our opinion, such considerations are sufficient to legitimize, both conceptually and practically, the integration of telemedicine into routine clinical activity. Firstly, in the current period, telemedicine could reduce the number and size of patient gatherings, making hospitals safer, while at the same time causing a decrease in mobility and thus reducing crowding on public transport crowding for those unable to travel with a private car. Moreover, if the situation becomes worse, hospitals will be forced to cancel or defer all non-essential consultations to further reduce the mobility of people (Moon et al., 2020).
Nevertheless, modern healthcare institutions have an ethical commitment to maintaining a high quality of care, while simultaneously reducing the number of consultations. Such a change cannot rely upon cancelling outpatient consultation services, which would lead to dramatic consequences, including losing many patients to follow-up, as well as missing a high number of diagnoses. The solution, in our experience, is to integrate a filtering system, which can allow a more efficient triage structure between patients with different levels of priority, establishing a sort of ‘urgency scale’ to redistribute waiting lists for physical examinations (Al-Izzi et al., 2020). In this regard, previous reports in the literature have described how the implementation of telemedicine, and particularly of teleradiology, has provided considerable support in the triage of maxillofacial trauma (Brucoli et al., 2019).
A low-priority examination might potentially conceal a severe disease, which has not been recognized by the general practitioner, or which has been underestimated by the patient. In such cases, teleconsultations offer a fundamental tool in allowing the specialist in maxillofacial surgery to raise the suspicion of disease, and subsequently intercept it (Cronin et al., 2020; Shanti et al., 2020). Moreover, in our experience, telemedicine has improved the exchange of information between colleagues across the region, leading to closer contact between specialists and general practitioners. This seems obvious in times of normal clinical activities, but under the threat of further lockdown and the potential curtailment of opportunities for physical examination, telemedicine becomes an essential concept to consider. In this regard, we have retained our assistance protocols, changing only the modalities for applying them. Consequently, all oncological patients have had their follow-up performed in the correct time sequence, while all referrals from spoke hospitals and general practitioners have been evaluated via first-line screening to define their level of priority (Yan et al., 2020).
In order to maintain the same organizational principles, the structure of the outpatient consultation rooms has also been preserved, including, in addition to general maxillofacial surgery examination, dedicated sessions for oncology and oral pathology, jaw deformities, TMJ disorders, pediatrics, and rehabilitation. The ability to recreate virtual physical spaces for clinical examinations led to a completely digital reorganization of consultation rooms, with traditional phases of clinical examinations replaced by telesemiology. However, by definition, the concept of telesemiology depends on the quality of technological devices and, inevitably, not all patients own the highest-quality cameras on their portable devices or laptops; additionally, the bandwidth or speed of their internet connection can be another limiting factor, especially in remote and mountainous regions. Another variable compromising the quality of signs detectable through a clinical examination is inadequate compliance from the patient, especially in relation to oral cavity examination. Therefore, the clinician has to be versatile and aware of the possibilities during each teleconsultation: for instance, in a case of oral pathology, a lesion localized in the mouth vestibule, in the apex of the tongue, or in the lips will allow a better evaluation than a lesion located deep in the mouth, where even in a physical examination the use of dental mirrors, appropriate lighting, or endoscope would be necessary. On the other hand, the inspection of superficial wounds in recently operated patients, and the evaluation of occlusion and mouth opening, are much easier parameters to define. Therefore, the role of the clinician is not only to perform an interpretation of the visual signs of diseases, but also to apply clinical judgment in order to decide for which patients a physical examination is unavoidable, and for which patients the elements provided by telesemiology have been sufficient.
However, there is an additional role of consultations, both physical and virtual, which must not be neglected in the shadow of clinical data, represented by the empathy and communication between the clinician and the patient. Especially for elderly people, in times of isolation, even a teleconsultation creates a more familiar environment, which is helpful when facing the challenging time of postoperative recovery, as well as in reinforcing trust with the healthcare team, and increasing compliance and self-confidence, all of which have clear clinical benefits. The psychological status of the patient during the recovery period has a particular importance for the rehabilitation physician, a novel implementation in our team, whose role has become even more essential in times of lockdown. Telemedicine brings the rehabilitation team to the patient's home, albeit digitally, conveying the sensation of a closer follow-up. Even though there are no validated questionnaires reporting patients' perception of telemedicine services and related satisfaction, our patients were satisfied with the continuous clinical assistance provided during lockdown at a time when reduced contact with doctors could make patients feel uncertain of their care.
The current literature lacks reports on the use of a clinically validated telemedicine platform. The choice of Zoom was based on its increased popularity during the lockdown, ease of use, availability free of charge, and multi-platform compatibility. In our opinion, the COVID-19 pandemic will provide an even stronger incentive for companies to begin the process of clinical approval for telemedicine platforms, while considering the number of problems that may arise, relating mainly to security issues, privacy of data, and stability of connection. During the current emergency, however, our institution has fully accepted our proposal, integrating telemedicine into assistance protocols. As the ongoing situation has demonstrated the full potential of such systems, it is foreseeable that the field of telesemiology will continue to develop in the near future, leading not only to clinically validated platforms, but also to the creation of specific hardware, such as cameras for the oral cavity, improved lighting systems, technology for the remote monitoring of parameters, and so forth.
Moreover, telemedicine has provided undeniable benefits for educational purposes, allowing smart working to be introduced to the field of healthcare (Brar et al., 2020; Chao et al., 2020). During this time, teams of senior physicians, researchers, and residents have shared and upgraded clinical protocols, reviewed literature, improved knowledge, performed virtual surgical planning, and written papers online (Wagner et al., 2019).
All we can gather from our experience of the previous lockdown era has to be critically re-examined in light of current events and knowledge, allowing us to design and apply protocols for the prompt adoption of innovative solutions. The second COVID-19 wave has raised many questions on the evolution of the pandemic, but this time, a lack of organization and inexperience are not excuses we can have.
5. Conclusions
This paper assimilates our previous experience, which developed during the months of early lockdown, and represents a scenario that we face over the coming months. We hope that many clinicians will become proficient in the use of telesemiology, not just in the field of maxillofacial surgery, but also in other areas. In this situation, telemedicine allows us to preserve the quality of care, while providing comprehensive support for both patients and physicians.
References
- Al-Izzi T., Breeze J., Elledge R. Following COVID-19 clinicians now overwhelmingly accept virtual clinics in Oral and Maxillofacial Surgery. Br J Oral Maxillofac Surg. 2020 doi: 10.1016/j.bjoms.2020.07.039. S026643562030382X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barca I., Cordaro R., Kallaverja E., Ferragina F., Cristofaro M.G. Management in oral and maxillofacial surgery during the COVID-19 pandemic: our experience. Br J Oral Maxillofac Surg. 2020 doi: 10.1016/j.bjoms.2020.04.025. S0266435620301777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barca I., Novembre D., Giofrè E., Caruso D., Cordaro R., Kallaverja E. Telemedicine in oral and maxillo-facial surgery: an effective alternative in post COVID-19 pandemic. Int J Environ Res Public Health. 2020;7:7365. doi: 10.3390/ijerph17207365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brar B., Bayoumy M., Salama A., Henry A., Chigurupati R. A survey assessing the early effects of COVID-19 pandemic on oral and maxillofacial surgery training programs. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 doi: 10.1016/j.oooo.2020.08.012. S2212440320311603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brucoli M., Boffano P., Franchi S., Pezzana A., Baragiotta N., Benech A. The use of teleradiology for triaging of maxillofacial trauma. J Craniomaxillofac Surg. 2019;47:1535–1541. doi: 10.1016/j.jcms.2019.07.007. [DOI] [PubMed] [Google Scholar]
- Chao T.N., Frost A.S., Brody R.M., Byrnes Y.M., Cannady S.B., Luu N.N. Creation of an interactive virtual surgical rotation for undergraduate medical education during the COVID-19 pandemic. J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.06.039. S1931720420302324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chigurupati R., Panchal N., Henry A.M., Batal H., Sethi A., D’innocenzo R. Considerations for oral and maxillofacial surgeons in COVID-19 era: can we sustain the solutions to keep our patients and healthcare personnel safe? J Oral Maxillofac Surg. 2020;78 doi: 10.1016/j.joms.2020.05.027. 1241–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cronin A.J., Lopez Jtj, Pabla R. Evaluation of remote OMFS assessments in the era of pandemic COVID-19 control measures. Br J Oral Maxillofac Surg. 2020;58(1023–8) doi: 10.1016/j.bjoms.2020.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Bartolomeo M., Pellacani A., Negrello S., Chiarini L., Anesi A. Emerging challenges and possible strategies in maxillo-facial and oral surgery during the COVID-19 pandemic. J Oral Sci. 2020;62(452–4) doi: 10.2334/josnusd.20-0235. [DOI] [PubMed] [Google Scholar]
- Maweri Sa A.L., Halboub E., Warnakulasuriya S. Impact of COVID-19 on the early detection of oral cancer: a special emphasis on high risk populations. Oral Oncol. 2020;106 doi: 10.1016/j.oraloncology.2020.104760. 104760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon H.S., Wang T.T., Rajasekaran K., Brewster R., Shanti R.M., Panchal N. Optimizing telemedicine encounters for oral and maxillofacial surgeons during the COVID-19 pandemic. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020 doi: 10.1016/j.oooo.2020.08.015. S2212440320311640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pareek P., Vishnoi J.R., Kombathula S.H., Vyas R.K., Misra S. Teleoncology: the youngest pillar of oncology. JCO Glob Oncol. 2020;1455–60 doi: 10.1200/GO.20.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shanti R.M., Stoopler E.T., Weinstein G.S., Newman J.G., Cannady S.B., Rajasekaran K. Considerations in the evaluation and management of oral potentially malignant disorders during the COVID-19 pandemic. Head and Neck. 2020;42 doi: 10.1002/hed.26258. 1497–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tel A., Robiony M., Bocin E., Sembronio S., Costa F., Bresadola V. Redesigning the paradigms of clinical practice for oral and maxillofacial surgery in the era of lockdown for COVID-19: from tradition to telesemeiology. Int J Environ Res Public Health. 2020 doi: 10.3390/ijerph17186622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner F., Knipfer C., Holzinger D., Ploder O., Nkenke E. Webinars for continuing education in oral and maxillofacial surgery: the Austrian experience. J Craniomaxillofac Surg. 2019;47:537–541. doi: 10.1016/j.jcms.2019.01.009. [DOI] [PubMed] [Google Scholar]
- Yan F., Rauscher E., Hollinger A., Caputo M.A., Ready J., Fakhry C. The role of head and neck cancer advocacy organizations during the COVID-19 pandemic. Head and Neck. 2020;(42):1526–1532. doi: 10.1002/hed.26287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann M., Nkenke E. Approaches to the management of patients in oral and maxillofacial surgery during COVID-19 pandemic. J Craniomaxillofac Surg. 2020 doi: 10.1016/j.jcms.2020.03.011. S1010518220300834. [DOI] [PMC free article] [PubMed] [Google Scholar]