Abstract
Introduction
The Public Health Center (PHC)—known as hokenjo in Japan—assume a crucial role in disease control. Coronavirus disease 2019 (COVID-19) is one of many designated infectious diseases monitored by the agency. During the present pandemic, patients who suspected COVID-19 were instructed to call the Coronavirus Consultation Center in the PHC prior to visiting the hospital. The aim of this study was to elucidate the differences in polymerase chain reaction (PCR) positivity between PHC referrals and direct walk-in patients.
Methods
The present was a single-center, retrospective cohort study conducted at the Tokyo Metropolitan Hospital from March to September, 2020. Patients who received a PCR test for SARS-CoV-2 were included and categorized into the PHC referral or direct walk-in groups. The outcomes included the total number of patients undergoing PCR tests and the percentage of PCR positivity in each group.
Results
We identified 1680 patients (781 PHC referred and 899 direct walk-in groups). The percentage of PCR positivity did not significantly differ between the PHC referral and direct walk-in groups during the first wave (30.5% vs. 29.2%; p = 0.78). PCR positivity was significantly higher in the PHC referral group than the direct walk-in group during the second wave (30.1% vs. 23.1%; p = 0.051) and entire study period (30.2% vs. 24.7%; p = 0.011).
Conclusions
Despite health authority recommendations, the number of direct walk-in patients were higher than PHC referral patients. The percentage of PCR positivity was significantly higher in the PHC referral group than in the direct walk-in group.
Keywords: PCR, Public health center, Health center, COVID-19, SARS-CoV-2
1. Introduction
The Public Health Center (PHC), known as hokenjo, assumes a vital role in disease surveillance, prevention and control in Japan [1]. Coronavirus disease 2019 (COVID-19) is one of many designated infectious diseases (Class II) falling under the jurisdiction of PHCs. At the time this manuscript was authored on September 25, 2020, it was mandated by public health law that patients diagnosed with COVID-19 were to be reported to the regional PHC for purposes of disease surveillance in Japan [2,3]. Physicians confirming a positive real-time polymerase chain reaction (PCR) for SARS-CoV-2 were required to notify the regional PHC immediately after diagnosis. In the initial phase of the pandemic, PCR tests were only made available to patients after approval by the PHC. A lack of testing resources, compounded by strict testing thresholds adopted by the PHCs, resulted in a large volume of PCR requests from physicians being denied by the regional PHCs [4]. Patients who suspected COVID-19 were instructed to call the Coronavirus Consultation Center in the PHC prior to visiting the hospital.
Beginning on March 6, 2020, PCR tests for SARS-CoV-2 became covered by the national health insurance in Japan and were made available at designated COVID-19 healthcare facilities [5]. Following this decision, physicians were granted the relative freedom to determine which patients warranted testing.
Japanese public health authorities instructed patients who suspected COVID-19 to make hospital visits only after consulting regional PHCs. While never officially stated, the overarching intention of instructing patients to consult regional PHCs prior to making hospital visits was likely to increase the prior probability of patients being allocated the use of limited hospital resources; however, this strategy inadvertently backfired, creating a vacuum of inquiries which overwhelmed and ultimately incapacitated the understaffed PHCs [6]. The ensuing confusion led to a noticeable proportion of patients bypassing the PHC and directly visiting their local hospitals.
The question remains whether this public health strategy was grounded upon scientific merit and succeeded in efficiently funneling patients with a higher prior probability for COVID-19 into designated COVID-19 healthcare facilities in comparison with direct walk-in patients. The present study aimed to elucidate the difference in the percentage of PCR positivity for SARS-CoV-2 between PHC referred and direct walk-in patients. Additionally, in order to determine which pathway was more commonly adopted by the general public, the total number of PHC referrals and direct walk-ins were assessed.
2. Materials and methods
2.1. Study setting
We conducted a single-center, retrospective cohort study based on medical chart data obtained by the Tokyo Metropolitan Hiroo Hospital between March 1 and September 11, 2020. This hospital is located in central Tokyo and is a designated tertiary-care emergency medical center. Shortly after the pandemic started, this facility began accepting suspected cases of COVID-19. To avoid cross contamination between patients with suspected or confirmed COVID-19 and those not suspected of COVID-19, we segregated patients by zone and established an emergency room (ER) tailored specifically for COVID-19 patients called the “COVID-ER.” Patients with fever, cough, dyspnea, myalgias, diarrhea, headache, anosmia or ageusia were referred to the COVID-ER. Patients transported by emergency medical services and walk-ins presenting with COVID-19 like symptoms were also assessed and treated in the COVID-ER. In contrast, regional PHCs initially referred patients to our facility based on fever ≥37.5 °C continuing for 4 or more days.
2.2. Patient selection and outcomes
We extracted consecutive patients who visited the COVID-ER during the study period. Patients who received a real-time reverse transcriptase-PCR for SARS-CoV-2 via a nasopharyngeal swab, sputum or saliva sample were included in the present study. Patients with multiple visits to the COVID-ER were excluded. Also excluded were patients transported via emergency medical service because patients referred from regional PHCs did not utilize such services. Patients were divided into the PHC referral and direct walk-in groups.
We described patient characteristics including age, sex, race, and specimen of PCR (nasopharyngeal swab, sputum or saliva). We also documented the severity of COVID-19 upon admission or reception at the COVID-ER. Severity of disease was categorized using the Interim Guidance issued by the World Health Organization. In the guidance document, the severity of COVID-19 has been divided into five categories: asymptomatic, mild, moderate, severe and critical [7]. The outcomes were defined as the difference in the percentage of PCR positivity for SARS-CoV-2, along with the total number of patients who visited the COVID-ER, documented between PHC referred and direct walk-in patients. The percentage of PCR positivity among the two groups was analyzed for three defined periods: i) during the entire study period, ii) during the first wave of COVID-19 in Japan (March 1 to May 25, 2020), and iii) during the second wave (May 26 to September 11, 2020). In the present study, we defined the first wave of COVID-19 in Japan from March 1 to May 25, 2020 because the state of emergency was lifted on May 25, 2020 [8]. The daily trends on the total number of patients receiving a PCR test and that of patients with PCR positivity was assessed. Next the trends in the percentage of PCR positivity, along with the total number of patients who visited the COVID-ER, were categorically analyzed for PHC referred and direct walk-in patients.
2.3. Statistical analysis
Continuous variables were reported as median and interquartile range (IQR), and categorical variables were reported as number and percentage. Continuous variables were compared between the groups using the Wilcoxon rank-sum test, and categorical variables were compared using the chi-square test. For plotting the trends, we used the moving average of 7 days (including the 3 days before and after the index date). All two-sided p-values less than 0.05 were considered significant. All analyses were performed using Stata MP15 (StataCorp, College Station, TX, USA).
3. Results
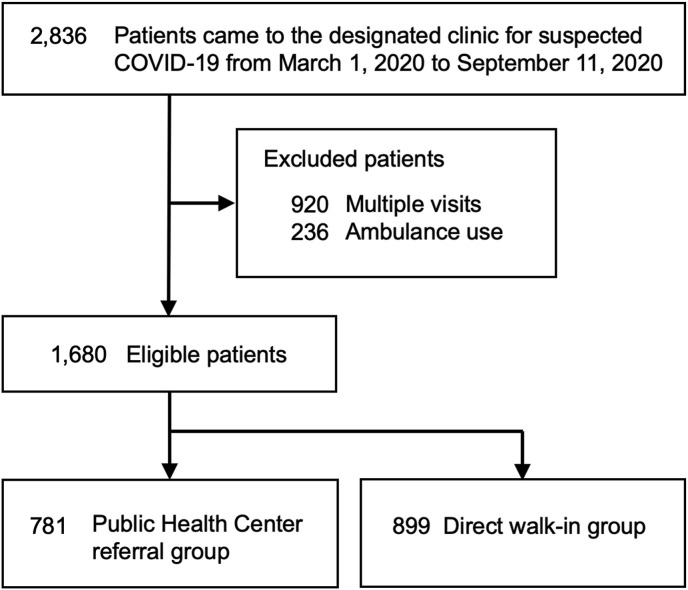
We identified 2836 patients who visited the COVID-ER and underwent PCR testing during the study period. After application of the exclusion criteria, we analyzed 1680 patients: 781 PHC referrals and 899 direct walk-ins (Fig. 1 ). The characteristics of patients who received a PCR test for SARS-CoV-2 are shown in Table 1 . The PHC referred patients were significantly younger than direct walk-ins. Direct walk-in patients were more likely to be admitted than PHC referrals. Severity of COVID-19 upon admission or reception at the COVID-ER is listed in Supplementary Table S1.
Fig. 1.
Patient flow. COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction.
Table 1.
The characteristics of patients who received a PCR test for SARS-CoV-2.
| Public Health Center referral group (n = 781) | Direct walk-in group (n = 899) | p-value | |
|---|---|---|---|
| Age, years, median (IQR) | 37 (28–49) | 42 (28–65) | <0.001 |
| Male sex, n(%) | 441 (56.5) | 530 (59.0) | 0.30 |
| Non-Japanese, n(%) | 41 (5.2) | 71 (7.9) | 0.030 |
| Period, n(%) | 0.38 | ||
| First wave | 220 (28.2) | 236 (26.3) | |
| Second wave | 561 (71.8) | 663 (73.7) | |
| Specimens used for PCR, n(%)a | |||
| Nasopharyngeal swab | 777 (99.5%) | 888 (98.8%) | 0.12 |
| Sputum | 4 (0.5%) | 10 (1.1%) | 0.28 |
| Saliva | 0 (0.0%) | 3 (0.3%) | 0.25 |
IQR, interquartile range; PCR, polymerase chain reaction.
Some patients received more than one PCR test.
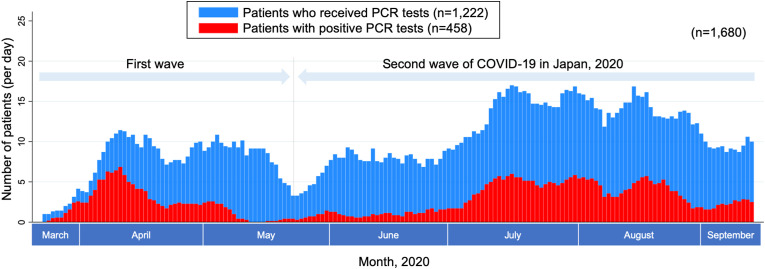
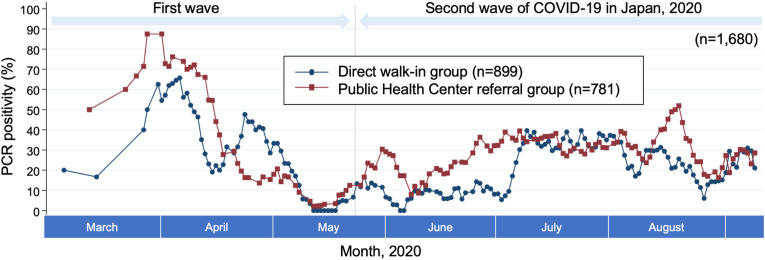
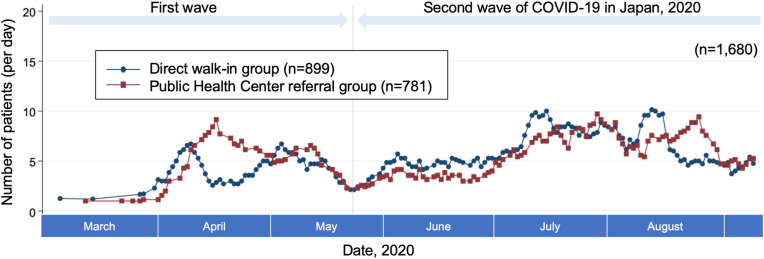
Fig. 2 demonstrates the daily trends on the total number of patients who received a PCR test during the study period along with PCR positivity. The percentage of PCR positivity spanning the entire data period was 27.3% (458/1680). Fig. 3 demonstrates the percentage of PCR positivity for the PHC referred and direct walk-in groups. During the first wave of the pandemic in Japan, PCR positivity did not significantly differ between the PHC referred and direct walk-in groups. In contrast, during the second wave and across the entire study period, the percentage of PCR positivity was significantly higher in the PHC referred group than the direct walk-in group (Table 2 ). The total number of patients in the direct walk-in group was higher than the PHC referral group for the entire study period and the first and second waves. Fig. 4 demonstrates the daily trends of the total number of patients who visited the COVID-ER for both groups.
Fig. 2.
Daily trends on the total number of patients who received a PCR test. Moving average of 7 days (including the 3 days before and after the index date) applied. COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction.
Fig. 3.
Percentage of PCR positivity for Public Health Center referrals and direct walk-ins. Moving average of 7 days (including the 3 days before and after the index date) applied. COVID-19, coronavirus disease 2019; PCR, polymerase chain reaction.
Table 2.
Percentage of PCR positivity for Public Health Center referrals and direct walk-ins.
| Outcomes | Public Health Center referral group n (%) |
Direct walk-in group n (%) | p-value |
|---|---|---|---|
| Total (n = 1680) | 236/781 (30.2%) | 222/899 (24.7%) | 0.011 |
| First wave (n = 456) | 67/220 (30.5%) | 69/236 (29.2%) | 0.78 |
| Second wave (n = 1224) | 169/561 (30.1%) | 153/663 (23.1%) | 0.005 |
PCR, polymerase chain reaction.
Fig. 4.
Daily trends of the total number of Public Health Center referrals and direct walk-ins visiting the COVID-ER Moving average of 7 days (including the 3-days before and after the index date) applied.COVID-19, coronavirus disease 2019.
4. Discussion
The present study demonstrated that the percentage of PCR positivity for SARS-CoV-2 did not significantly differ between PHC referrals and direct walk-in patients during the first wave of the pandemic in Japan. In contrast, PCR positivity was significantly higher in PHC referred patients during the second wave.
Through public service announcements, patients who suspected COVID-19 were instructed to call Coronavirus Consultation Centers in the regional PHC before visiting hospitals. Following this announcement, only patients referred via PHCs were technically allowed to make hospital visits for COVID-19 related issues; however, in actuality the number of direct walk-ins outnumbered PHC referred patients during each period assessed in the present study. There are several possible reasons for these findings: i) the patient attempted contact with the PHC, but was not connected due to an overwhelming number of inquiries, ii) the patient consulted the call center but failed to meet the strict criteria for referral, iii) the patient was unware of the public health recommendation and visited the hospital directly without consulting the PHC.
For PHC referred patients, physicians were required to send a fax to the PHC requesting permission to conduct a PCR test. Once approved, a representative from the PHC was dispatched to the hospital to collect a specimen for PCR analysis. The results of the PCR test were subsequently reported to the hospital by the PHC via telephone. This protocol is wrought with complexity and imposed an unnecessary burden upon both hospital and PHC staff.
During the first wave, when PCR testing was limited, PCR positivity did not significantly differ between the PHC referred and direct walk-in groups. During this initial phase of the pandemic, only relatively severe patients with a high likelihood of infection were allowed to make hospital visits, regardless of whether they came directly to the hospital or were referred by the PHC. In contrast, during the second wave, PCR positivity was significantly higher in PHC referred patients. During the second wave, PCR testing saw expanded use as testing was made available at the physician's discretion [9]. As a result, for direct walk-in patients, PCR testing could be performed as a precautionary measure even in patients presenting with minor or atypical symptoms. On the opposite end of the spectrum, patients referred by the PHC were selected on the basis of close contact with a known COVID-19 patient, patient clusters, and patients with typical symptoms for COVID-19. These factors may have contributed to the difference observed in the percentage of PCR positivity between the two groups.
The patient referral system operated by the PHC, combined with the strict criteria adopted during the initial phase of the pandemic, may have theoretically prevented patients from overwhelming hospital capacities. During the entire study period, the percentage of PCR positivity was higher in the PHC referral group in comparison with the direct walk-in group. These results collectively indicate that the PHC selectively and correctly screened patients with a higher likelihood for COVID-19. On September 4, 2020, the Minister of Health, Labour and Welfare, Japan announced that patients will be allowed to make direct hospital visits without prior consultation with the Coronavirus Consultation Center in the PHC ahead of the winter influenza season [10]. This policy was expected to alleviate the burden imposed upon the PHC but came with the risk of overwhelming hospitals with patients during the winter months where an increased strain would likely be imposed as a result of seasonal demands.
There are several limitations in the present study. First, this is a retrospective observational study conducted in a single facility in Tokyo. The patients included in the present study may be skewed in favor of emergency cases and relatively severe patients given the facilities traditional role as an emergency care center. Given the single center nature of this study, the generalizability to areas outside of Tokyo or other facilities are questionable. Second, our study does not contain detailed patient characteristics, such as days after onset of disease, or details concerning specific symptoms. A small number of asymptomatic patients such as close contacts could be included in both groups which could have inadvertently influenced PCR positivity. We only focused on the percentage of PCR positivity between PHC referrals and direct walk-ins. Third, the implementation rate of PCR and severity of COVID-19 differed between the two groups. Although the degree of which is unknown, these discrepancies could have influenced PCR positivity. Finally, this study was not designed to evaluate and assess the PHC referral system under the COVID-19 pandemic.
In conclusion, the number of direct walk-ins was higher in comparison with PHC referred patients during the entire study period and the first and second waves. Although PCR positivity did not significantly differ between the PHC referred and direct walk-in groups during the first wave, PCR positivity was significantly higher in PHC referred patients during the second wave and the entire study period. The results of the present study highlights the difficulty in establishing an efficient system for visiting hospitals during a pandemic.
Authorship statement
All authors meet the ICMJE authorship criteria. MN designed this study and performed the statistical analysis. Yasuhiro Y contributed to data collection and management. MN and RHK edited the manuscript. Yuko Y, KY, YN, HG, Yoshihiro Y, TI, YM and YT provided professional suggestions in the conduct of the study and interpretation of the study results. All authors participated in the revision and approval of the final manuscript.
Funding
None.
Ethics approval (include appropriate approvals or waivers)
The study was approved by the Institutional Review Board at Tokyo Metropolitan Hiroo Hospital (approval number, J-41).
Consent to participate
Due to the anonymous nature of the data, the requirement for patient informed consent was waived.
Availability of data and material
Data will not be shared due to the policy of the institutional review board.
Declaration of competing interest
None.
Acknowledgements
The authors wish to express their deepest appreciation to the entire hospital staff involved in providing medical care to COVID-19 patients during an unprecedented and challenging period. We also would like to thank the Shibuya Public Health Center and other regional PHCs for their cooperation in providing invaluable medical services.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jiac.2021.02.001.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Takemura S., Ohmi K., Sone T. Public health center (Hokenjo) as the frontline authority of public health in Japan: contribution of the National Institute of Public Health to its development. J Natl Inst Public Heal. 2020;69:2–13. [Google Scholar]
- 2.Japan classifies Wuhan coronavirus as “designated infectious disease.” NIKKEI ASIAN Rev https://asia.nikkei.com/Spotlight/Coronavirus/Japan-classifies-Wuhan-coronavirus-as-designated-infectious-disease (accessed September 20, 2020).
- 3.Kampo. January 28 Ministry of health, Labour and Welfare. 2020. https://www.mhlw.go.jp/content/10900000/000589748.pdf
- 4.Hayasaki E. Covid-19: how Japan squandered its early jump on the pandemic. BMJ. 2020;369:2–4. doi: 10.1136/bmj.m1625. [DOI] [PubMed] [Google Scholar]
- 5.Chuikyo. Ministry of Health, Labour and Welfare https://www.mhlw.go.jp/content/12404000/000612063.pdf (accessed September 20, 2020).
- 6.Shimizu K., Wharton G., Sakamoto H., Mossialos E. 2020. Resurgence of covid-19 in Japan the government looks set to repeat its mistakes; pp. 1–2. [DOI] [PubMed] [Google Scholar]
- 7.World Health Organization. Clinical management of COVID-19 https://www.who.int/publications/i/item/clinical-management-of-covid-19 (accessed November 15, 2020).
- 8.Kuniya T. Evaluation of the effect of the state of emergency for the first wave of COVID-19 in Japan. Infect Dis Model. 2020;5:580–587. doi: 10.1016/j.idm.2020.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Looi M.K. Covid-19: Japan ends state of emergency but warns of “new normal. BMJ. 2020;369:m2100. doi: 10.1136/bmj.m2100. [DOI] [PubMed] [Google Scholar]
- 10.Ministry of Health Labour and Welfare https://www.mhlw.go.jp/content/000667888.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will not be shared due to the policy of the institutional review board.