Abstract
Study Objective
Among a comprehensive range of frontline emergency department health care personnel, we assessed symptoms of anxiety and burnout, specific coronavirus disease 2019 (COVID-19) work-related stressors, and risk for post-traumatic stress disorder (PTSD). We also determined whether COVID-19 serologic testing of HCP decreased their self-reported anxiety.
Methods
In a prospective cohort study from May 13, 2020, to July 8, 2020, we used electronic surveys to capture participant self-reported symptoms before and after serologic testing for anti-SARS-CoV-2 immunoglobulin G antibodies. Participants were physicians, nurses, advanced practice providers, and nonclinical ED personnel at 20 geographically diverse United States EDs. We evaluated these domains: 1) the effects of the COVID-19 pandemic on overall stress and anxiety; 2) COVID-19-related work stressors; 3) burnout; and 4) PTSD risk (measured using the Primary Care-PTSD Screen for DSM-5, a 5-item screening instrument in which a score of ≥3 signifies high risk for PTSD). We also assessed perceptions of whether results of COVID-19 antibody testing decreased participants’ self-reported anxiety.
Results
Of 1,606 participants, 100% and 88% responded to the baseline and follow-up surveys, respectively. At baseline, approximately half (46%) reported symptoms of emotional exhaustion and burnout from their work, and 308 (19.2%, 95% confidence interval [CI] 17.3% to 21.1%) respondents screened positive for increased PTSD risk. Female respondents were more likely than males to screen positive (odds ratio [OR] 2.03, 95% CI 1.49 to 2.78). Common concerns included exposing their family and the health of coworkers diagnosed with COVID-19. After receiving antibody test results, 54% (95% CI 51.8 to 56.7) somewhat agreed, agreed, or strongly agreed that knowledge of their immune status had decreased their anxiety. A positive serology result indicating prior SARS-CoV-2 infection was associated with a higher likelihood of reporting decreased anxiety (2.83, 95% CI 1.37 to 5.83).
Conclusion
Symptoms of anxiety and burnout were prevalent across the spectrum of ED staff during the COVID-19 pandemic. One-fifth of ED personnel appeared to be at risk for PTSD. Increased provision of serologic testing may help to mitigate anxiety.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has challenged health care personnel throughout the health care system, leading to unprecedented levels of stress and anxiety.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Facing unique stressors during their frontline work, health care personnel in emergency departments may be particularly vulnerable to poor mental health during the pandemic.
Editor’s Capsule Summary.
What is already known on this topic
COVID-19 created a generational event that triggered concerns in many health care workers.
What question this study addressed
What were the psychologic reactions associated with being an emergency department (ED) health care worker during the pandemic?
What this study adds to our knowledge
Using electronic surveys across many types of workers at volunteer sites, 46% responding noted anxiety and burnout and 19.2% some elements of post-traumatic stress disorder. Women had higher frequency of reporting these features, and antibody testing mitigated some of the feelings.
How this is relevant to clinical practice
ED health care workers should have access to programs that address their concerns and reactions to current or future external stressors.
We previously reported moderate-to-severe stress levels induced by work during the pandemic and identified several potential stress mitigation measures, including broadly available SARS-CoV-2 testing of health care personnel, even for those not experiencing symptoms.7 That study, however, was limited to academic emergency physicians in California, New Jersey, and Louisiana. Little is known about the effects on other ED personnel in a geographically diverse sample of EDs across the United States.
Goals of This Investigation
The objectives of the current study, conducted during the acute phase of the COVID-19 pandemic, were: 1) to assess the symptoms of anxiety and burnout and the risk for post-traumatic stress disorder (PTSD) in a national sample (20 geographically diverse US hospitals) of ED personnel over a broad range of staff roles, including nurses and nonclinical personnel (eg, clerks and others without routine patient contact); 2) to describe specific concerns of ED personnel arising from their work during the pandemic; and 3) to determine whether the previously reported stress mitigation measure of SARS-CoV-2 serologic testing for ED personnel would decrease self-reported anxiety.
Materials and Methods
Study Design and Setting
We conducted this prospective cohort study as part of the COVID-19 Evaluation of Risks in Emergency Departments Project (COVERED), a SARS-CoV-2 infection surveillance analysis of physicians, nurses, advanced practice providers (nurse practitioners and physician assistants), and nonclinical ED personnel in 20 US academic EDs in 15 states; the protocol was previously described.14 Participants in the parent study were recruited from ED staff who had not previously been diagnosed with COVID-19. The sample size was determined by the parent study, which included 1,606 participants (approximately 40 doctors or advanced practice providers, 20 nurses, and 20 nonclinical ED personnel at each of the 20 sites). This project was reviewed by a Centers for Disease Control and Prevention (CDC) Human Subjects Advisor (STARS Tracking Number: 0900f3eb81b18773, NCEZID Tracking Number: 040920PK) and classified on April 9, 2020 as public health surveillance deemed not to be research under the provision as defined in 45 CFR 46.102(l)(2). It was reviewed by the institutional review boards at all sites, and informed consent was obtained from all participants. We followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.15
Measurements
We administered baseline electronic surveys (as part of enrollment in the parent study) from May 13, 2020, to July 8, 2020 (during a 1-week period at each site). Participants then underwent reverse transcriptase-polymerase chain reaction (RT-PCR; Architect i2000, Abbott Laboratories, Chicago, Illinois) testing of nasal swabs and anti-SARS-CoV-2 immunoglobulin G serologic testing (Cobas SARS-CoV-2; Roche, Basel, Switzerland). Approximately 2 to 3 weeks after receiving their test results, the participants were asked to complete a follow-up survey.
After consulting with survey content experts, we utilized an abbreviated version of our previously published mental health survey7 to assess the following domains: 1) the effects of the COVID-19 pandemic on stress and anxiety symptoms (hereafter collectively referred to as “COVID-19 stress and anxiety”); 2) work-related stressors; 3) work-related symptoms of emotional exhaustion, cynicism, and burnout (hereafter collectively referred to as “burnout”); and 4) PTSD risk (measured using the Primary Care-PTSD Screen for DSM-5 [PC-PTSD-5], a validated 5-item screening instrument in which a score of 3 or more signifies a high risk for PTSD).16 COVID-19 stress, work-related stressors, and job stress over the prior week were rated on a 7-point Likert scale where 1=not at all, 4=somewhat, and 7=extremely. Scores 4 or more were considered increased stress responses. To assess the perceived stress mitigation effect of serologic testing, we asked participants to rate their agreement with the following statements: “Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing would decrease my anxiety” (prior to testing), and “Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing has decreased my anxiety” (after receiving their test result). Both questions were rated on a 7-point Likert scale where 1=strongly disagree and 7=strongly agree. See the Supplemental material for the survey questions.
Analysis
We reported the health care personnel characteristics and key responses as raw counts, frequencies, percentages, medians, and interquartile ranges (IQRs). Logistic regression was used to measure the difference in the percentage of the participants who screened positive for PTSD symptoms; the model included site and participant random effects. We performed explanatory multivariable logistic regression to identify factors associated with the risk of PTSD and antibody positive-associated decrease in anxiety, in which a positive response was defined as any level of agreement that testing decreased anxiety. We performed multivariable logistic regression to identify factors associated with a score of 4 or more on questions about stress/anxiety because of COVID-19 and job-related emotional exhaustion/burnout. Variables included in the multivariable models were selected a priori based on existing literature and included the following participant characteristics: quartiles of age, sex, race/ethnicity, home living situation (living alone or with a spouse or significant other, children, roommates, or other family), type of health care personnel (physician, advanced practice provider, nurse, or nonclinical staff), and community COVID-19 prevalence at the time of the baseline survey (quartiles as determined by local public health reports).1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Baseline models also included a dichotomous variable for participant belief that they had previously been infected (but not diagnosed) with SARS-CoV-2, and follow-up models included SARS-CoV-2 RT-PCR test results and serology test results. Standard errors were clustered at the site level. All analyses were conducted using Stata v13.0 (StataCorp LLC, College Station, TX).
Results
Characteristics of Study Subjects
Of 1,606 participants in the parent study, 1,606 (100%) completed the baseline survey (638 physicians, 156 advanced practice provider, 410 nurses, and 402 nonclinical staff) and 1,413 (88%) completed the follow-up survey (Table 1 ).
Table 1.
Participant characteristics and community COVID-19 incidence at 20 emergency departments in the United States, May to July 2020.
| Frequency | Percent (%) | ||
|---|---|---|---|
| Sex | Male | 581 | (36.2) |
| Female | 1,018 | (63.4) | |
| Other | 8 | (0.4) | |
| Race/ethnicity∗ | Asian | 134 | (8.3) |
| Black | 131 | (8.2) | |
| Hispanic | 152 | (9.5) | |
| American Indian / Alaska Native | 12 | (0.7) | |
| Native Hawaiian / Pacific Islander | 6 | (0.4) | |
| White | 1,280 | (79.7) | |
| Other | 59 | (3.7) | |
| Health care personnel category | Nurse | 410 | (26) |
| Nonclinical staff | 402 | (25) | |
| Attending / fellow physician | 362 | (23) | |
| Resident physician | 276 | (17) | |
| Advanced practice provider (physician assistant, nurse practitioner) | 156 | (10) | |
| Home living situation† | Spouse or significant other | 1,112 | (69) |
| Children | 689 | (43) | |
| Alone | 249 | (16) | |
| Other family‡ | 141 | (9) | |
| Roommate(s) | 111 | (7) | |
| COVID-19 status | Belief prior undiagnosed infection | 191 | (12) |
| RT-PCR positive | 5 | (0.3) | |
| Serology positive | 31 | (1.9) | |
| Community cumulative incidence§ | 1st quartile (lowest) | — | (0.4) |
| 2nd quartile | — | (0.6) | |
| 3rd quartile | — | (1.0) | |
| 4th quartile (highest) | — | (1.6) |
Home living categories are not mutually exclusive, except for alone.
Other family=parents, grandparents, aunts, uncles, or other family not including a spouse/significant other and/or children.
Community cumulative incidence defined as cumulative cases as of June 29, 2020.
Race/ethnicity categories are not mutually exclusive
COVID-19 Stress and Anxiety
Before serologic testing, 1,030 (64%) respondents (64% of physicians/advanced practice providers, 68% of nurses, and 61% of nonclinical staff) reported feeling stress and anxiety because of COVID-19 “somewhat” or more strongly. The health care personnel characteristics associated with reporting higher stress and anxiety included female sex (odds ratio [OR] 1.99, 95% confidence interval [CI] 1.64 to 2.42), living with a partner or roommate (OR 1.26 and 1.62; 95% CI 1.00 to 1.60 and 1.15 to 2.29, respectively), suspected prior infection (OR 1.39, 95% CI 1.05 to 1.84), and work involving direct patient contact (nonclinical work OR 0.70, 95% CI 0.55 to 0.91; Table 2 ).
Table 2.
Factors associated with stress, anxiety, burnout, and PTSD symptoms among emergency department health care personnel in the United States, May to July 2020.
| In the past week, how much has the COVID-19 pandemic affected your stress or anxiety levels? |
In the past week, to what extent are you experiencing severe, ongoing job stress where you felt emotionally exhausted, burned out, cynical about your work and fatigued, even when you wake up? |
PTSD screen (score ≥3) |
To what extent do you agree or disagree with the following statement: Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing would decrease my anxiety. |
To what extent do you agree or disagree with the following statement: Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing has decreased my anxiety. |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Odds Ratio | (95% CI) | Odds ratio | (95% CI) | Odds ratio | (95% CI) | Baseline Survey |
Follow-up Survey |
|||
| Odds ratio | (95% CI) | Odds ratio | (95% CI) | |||||||
| Female | 1.99 | (1.64-2.42) | 1.54 | (1.26-1.88) | 2.03 | (1.49-2.78) | 1.17 | (0.96-1.42) | 1.30 | (1.07-1.57) |
| Age (reference category=youngest quartile) | ||||||||||
| 2nd quartile (30-35 years) | 1.19 | (0.99-1.44) | 1.29 | (0.99-1.68) | 1.46 | (0.94-2.26) | 1.20 | (0.85-1.69) | 0.71 | (0.51-0.99) |
| 3rd quartile (36-45 years) | 1.07 | (0.88-1.29) | 1.07 | (0.81-1.41) | 1.21 | (0.81-1.82) | 0.98 | (0.66-1.46) | 0.72 | (0.49-1.05) |
| 4th quartile (46 and older) | 0.81 | (0.63-1.04) | 0.72 | (0.53-0.97) | 0.91 | (0.51-1.61) | 0.79 | (0.5-1.23) | 0.75 | (0.54-1.04) |
| Race (base=White) | ||||||||||
| Black | 1.51 | (1.18-1.93) | 1.29 | (0.98-1.71) | 1.09 | (0.66-1.79) | 0.59 | (0.37-0.93) | 0.64 | (0.46-0.89) |
| American Indian / Alaskan Native | 0.95 | (0.34-2.64) | 1.04 | (0.3-3.59) | 0.41 | (0.04-4.03) | 0.60 | (0.15-2.39) | 1.83 | (0.73-4.57) |
| Asian | 1.10 | (0.84-1.43) | 0.97 | (0.73-1.29) | 0.96 | (0.65-1.41) | 0.76 | (0.47-1.23) | 1.24 | (0.87-1.77) |
| Native Hawaiian / Pacific Islander | 1.12 | (0.57-2.21) | 1.05 | (0.52-2.11) | 1.05 | (0.08-14.59) | 0.63 | (0.12-3.23) | 1.79 | (0.53-6.01) |
| Other race | 1.49 | (0.85-2.63) | 1.75 | (1.06-2.89) | 1.82 | (0.86-3.87) | 1.09 | (0.53-2.22) | 0.77 | (0.41-1.46) |
| Hispanic | 0.77 | (0.49-1.22) | 0.98 | (0.68-1.42) | 0.73 | (0.47-1.14) | 1.01 | (0.62-1.64) | 0.99 | (0.75-1.29) |
| Health care personnel category (base = physician/advanced practice provider) | ||||||||||
| Nurse | 0.90 | (0.71-1.15) | 1.63 | (1.16-2.29) | 1.08 | (0.82-1.41) | 1.11 | (0.77-1.59) | 1.44 | (1.11-1.86) |
| Nonclinical | 0.70 | (0.55-0.91) | 1.23 | (1.01-1.5) | 0.81 | (0.62-1.06) | 0.79 | (0.6-1.03) | 1.80 | (1.29-2.52) |
| Home cohabitants (base=alone) | ||||||||||
| Spouse or significant other | 1.26 | (1.00-1.60) | 0.98 | (0.79-1.21) | 1.02 | (0.75-1.4) | 1.08 | (0.8-1.46) | 0.97 | (0.8-1.18) |
| Children | 1.04 | (0.86-1.26) | 0.84 | (0.72-0.98) | 0.85 | (0.64-1.14) | 0.99 | (0.73-1.35) | 0.89 | (0.72-1.11) |
| Roommate | 1.62 | (1.15-2.29) | 1.25 | (0.86-1.81) | 1.25 | (0.75-2.11) | 0.87 | (0.58-1.3) | 0.88 | (0.58-1.36) |
| Other family | 1.05 | (0.75-1.45) | 0.81 | (0.58-1.14) | 0.93 | (0.52-1.66) | 0.91 | (0.65-1.29) | 0.78 | (0.58-1.05) |
| Community COVID-19 cumulative incidence (base=low incidence) | ||||||||||
| 2nd quartile | 1.22 | (0.76-1.96) | 1.08 | (0.64-1.81) | 1.19 | (0.58-2.43) | 1.25 | (0.79-1.99) | 0.91 | (0.61-1.36) |
| 3rd quartile | 1.08 | (0.64-1.84) | 0.95 | (0.59-1.53) | 0.86 | (0.45-1.65) | 0.80 | (0.56-1.14) | 0.74 | (0.52-1.07) |
| 4th quartile (highest incidence) | 1.22 | (0.76-1.94) | 1.16 | (0.69-1.93) | 1.01 | (0.5-2.04) | 0.98 | (0.73-1.32) | 0.60 | (0.37-0.96) |
| COVID-19 infection | ||||||||||
| Belief of prior infection | 1.39 | (1.05-1.84) | 1.83 | (1.43-2.35) | 1.36 | (0.84-2.2) | 1.51 | (1.1-2.07) | 0.74 | (0.59-0.93) |
| PCR positive | n/a | n/a | n/a | n/a | 0.23 | (0.03-1.8) | ||||
| Serology positive | n/a | n/a | n/a | n/a | 2.83 | (1.37-5.83) | ||||
Anxiety and burnout symptoms were analyzed using an ordered logistic regression on a scale from 1 to 7 where 1=“not at all,” 4=“somewhat,” and 7=“extremely.” PTSD and knowledge of prior exposure were modeled as logistic regression. Risk for PTSD is indicated by the presence of 3 or more of the following: nightmares, trigger avoidance, feeling on edge, feeling numb, and feeling guilty. Standard errors clustered at the site level. Base (comparison) groups were male, age quartile 1 (young), White race, physician/advanced practice provider, lives alone, community COVID-19 cumulative incidence quartile 1 (low), and no belief of prior infection. PCR and serology results were only available at the follow-up survey.
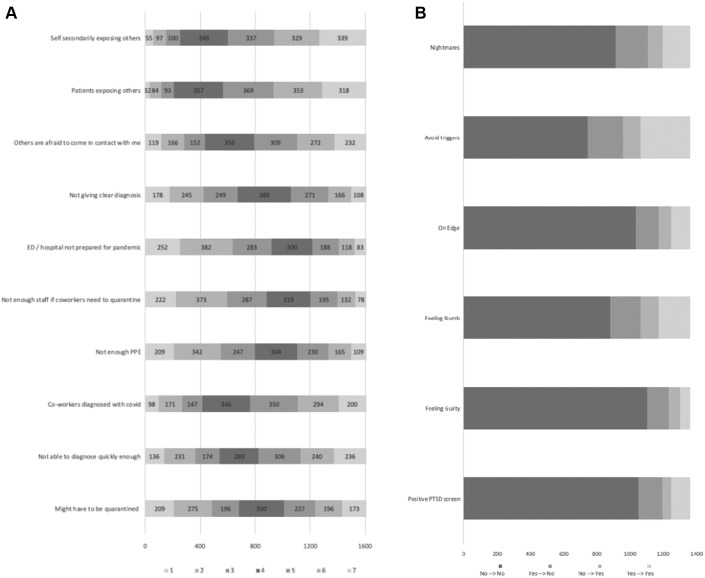
Specific Worries about Work During the COVID-19 Pandemic
Participants expressed concerns about the specific worries described in Figure 1 . The highest-rated (greatest) concerns were secondarily exposing the participants’ family members (median score 5 on the 7-point Likert scale, IQR 4 to 6), patients with an unclear diagnosis exposing others in their community (median 5, IQR 4 to 6), family members and others being afraid to come into contact with the participant because of their work in the health care setting (median 5, IQR 3 to 6), and the well-being of coworkers diagnosed with COVID-19 (median 5, IQR 3 to 6).
Figure 1.
Worries and concerns about COVID-19 among emergency department health care personnel in the United States, May to July 2020. Responses to: “To what extent are you experiencing the following worries and concerns about COVID-19?”. Scale: 1=not at all, 4=somewhat, 7=extremely. N=1,606 for each question.
Job-related Emotional Exhaustion, Burnout, and Cynicism
Prior to testing, 741 (46%) respondents (40% of physicians/advanced practice providers, 55% of nurses, and 50% of nonclinical staff) reported feeling burnout symptoms in the prior week “somewhat” or more strongly. Factors associated with higher ratings included female sex (OR 1.54, 95% CI 1.26 to 1.88) and suspected prior infection (OR 1.83, 95% CI 1.43 to 2.35; Table 2). Participants in the oldest age quartile (age >46 years) reported lower job-related stress and burnout scores (OR 0.72, 95% CI 0.53 to 0.97).
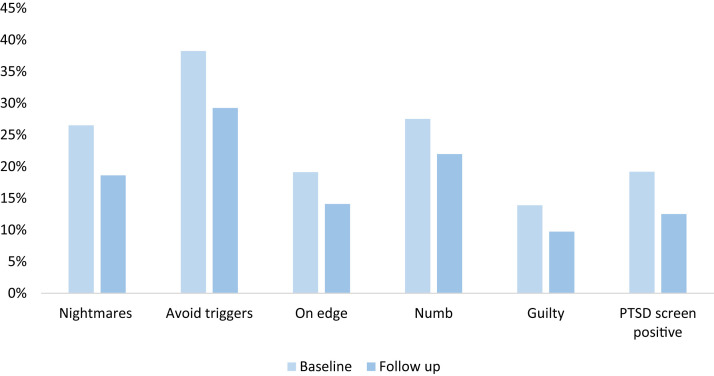
PTSD Risk
Prior to testing, 308 (19.2%, 95% CI 17.3 to 21.1%) respondents (18% of physicians/advanced practice providers, 23% of nurses, and 18% of nonclinical staff) screened positive for PTSD risk (score ≥3). Female respondents were more likely to screen positive than were males (OR 2.03, 95% CI 1.49 to 2.78). Among the participants who responded to both surveys, fewer respondents (12.5%) screened positive for PTSD risk after testing (difference 6.5%, 95% CI 4.6 to 8.5%; Figure 2 ).
Figure 2.
Emergency department personnel responses to the Primary Care post-traumatic stress disorder (PTSD) screening instrument for DSM-5, United States, May to July 2020: the proportion reporting “yes” to experiencing each symptom in the week prior to the baseline and in the follow-up surveys. A positive PTSD screen was defined as positive response to 3 or more of the 5 items.
Community COVID-19 Prevalence
The community COVID-19 prevalence was not associated with positive responses to the anxiety, burnout, or PTSD symptom questions in any of the multivariable logistic regression models (Table 2).
Effect of Serologic Testing on Self-Reported Anxiety
Prior to COVID-19 testing, 75.6% (95% CI 73.5 to 77.7%) of participants somewhat agreed, agreed, or strongly agreed that knowing their prior exposure and immunity to SARS-CoV-2 would decrease their anxiety. After receiving their test results, 54% (95% CI 51.8 to 56.7) somewhat agreed, agreed, or strongly agreed that knowledge of their immune status had decreased their anxiety. A positive serology result, ie, evidence of past infection, was associated with a higher likelihood of reporting a decrease in anxiety (OR 2.83, 95% CI 1.28 to 6.25; Table 2).
Limitations
Our study selected health care personnel from large academic centers and may not reflect the experience of health care personnel in smaller community EDs. Because of the potentially taxing extent of survey items for the parent project, we used abbreviated scales instead of comprehensive instruments to measure anxiety, burnout, and the risk of PTSD. Although our questions were reviewed by survey and content methodology experts and we used questions from some validated instruments, our final survey instrument and questions were not externally validated.
We only surveyed at 2 points in time (approximately 3 weeks apart) during 1 stage of a lengthy pandemic and were unable to observe or control for day-to-day variables that could impact the participants’ reports of anxiety levels, burnout, and PTSD symptoms, such as a very stressful workday prior to completing the survey. Similarly, in terms of timing, we conducted this work from May to July 2020—prior to COVID-19 vaccination of ED providers. Receipt of COVID-19 vaccines has likely had a substantial impact on health care personnel emotional well-being and anxiety levels. Finally, lack of a control group who did not receive serologic testing precludes causal inferences regarding relief of anxiety and PTSD symptom reduction after serologic testing.
Discussion
In this study conducted at 20 US EDs, 4 central findings advance our understanding of the impact of the COVID-19 pandemic on the mental well-being of US frontline ED personnel. First, we found that self-reported feelings of work-related anxiety, emotional exhaustion, and burnout were prevalent across the full spectrum of ED staff, including nurses and nonclinical personnel. Second, primary stressors included concerns about health care personnel and patients infecting others with COVID-19 and the health of coworkers diagnosed with COVID-19. Third, over half of the ED personnel reported 1 or more mental health symptoms of PTSD (eg, nightmares) and nearly 1 in 5 screened positive for increased PTSD risk. Finally, most respondents (54%) reported that their anxiety was diminished by learning their test results, although this was a lower proportion of participants than those who predicted that serologic testing would decrease their anxiety (75%). This mitigating effect was especially pronounced among those who had positive serology for antibodies to COVID-19.
Our findings were consistent with those of international investigators, who have documented increased symptoms of anxiety, depression, insomnia, and PTSD risk in health care personnel and have found slightly greater risk in women.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 In our previous research, conducted from February 23 to April 10, 2020, the limited availability of personal protective equipment (PPE) was academic emergency physicians’ primary concern.7 At the later time of this study, PPE was no longer among the top 5 listed worries, suggesting that PPE became more widely available.
In terms of practical, actionable items from this research, the stress mitigation effect of serologic testing has substantial face validity. The ED personnel serve as the initial hospital caregivers for the majority of critically ill patients with known or suspected COVID-19 infection. They also deal with many patients with undifferentiated symptoms consistent with COVID-19, whose SARS-CoV-2 test results are often unknown while in the ED. This can lead to the ED personnel being uncertain of exposure to COVID-19 and the secondary risk to their families. By clarifying exposure and risks, testing of health care personnel may logically relieve anxiety, especially in those who test positive indicating some level of perceived immunity.
Our findings were remarkably consistent across all demographic groups and “hotspot” sites. The CDC advocates for the early recognition of the signs of stress (irritation, anxiety, lack of motivation, feeling burned out, and difficulty sleeping) in ED personnel.17 Along with following CDC recommendations, which provide guidance to employers to develop and implement a COVID-19 response plan (including healthy work conditions, improved leave policies, and resilience building among workers),18 it is important that ED leadership consider provision of serologic testing for ED personnel. Considering that over half of the participants reported experiencing at least 1 symptom of PTSD and as many as 20% were at increased risk, employers should also similarly consider assuring that health care personnel are aware of available well-being programs and encourage workers to take time off, get adequate rest, and utilize the resources available to them.
In conclusion, symptoms of anxiety, emotional exhaustion, and burnout were prevalent across the full spectrum of ED staff during the COVID-19 pandemic, and as many as one-fifth were at risk for PTSD. Future work should focus on organizational efforts to prevent pandemic-associated stress to the extent possible through healthy work design and supportive workplace policies. As health care personnel continue to serve on the frontlines in this pandemic, it is critical to explore ways to mitigate the long-term effects of chronic stress. Increasing the provision of SARS-CoV-2 testing shows promise for achieving this aim.
Acknowledgments
The authors acknowledge the following participating Project COVERED emergency departments: Allegheny General Hospital, Pittsburgh, PA; Baystate Medical Center, Springfield, MA; Denver Health, Denver, CO; Detroit Receiving Hospital/Sinai-Grace Hospital, Detroit, MI; Hennepin County Medical Center, Minneapolis, MN; Jackson Memorial Hospital, Miami, FL; Johns Hopkins Medical Institute, Baltimore, MD; University Medical Center, New Orleans, LA; Mount Sinai Hospital East/Elmhurst Hospital Center, New York, NY; Orlando Regional Medical Center, Orlando, FL; University of Alabama at Birmingham Hospital, Birmingham, AL; Ronald Reagan-UCLA Medical Center/Olive View-UCLA Medical Center, Los Angeles, CA; University of Iowa, Iowa City, IA; University of Massachusetts Memorial Medical Center, Worcester, MA; University of Mississippi Medical Center, Jackson, MS; UCSF Zuckerberg San Francisco General, San Francisco, CA; UT Southwestern Medical Center, Dallas, TX; Truman Medical Center, Kansas City, MO; Thomas Jefferson University, Philadelphia, PA; and Washington University Barnes-Jewish Hospital, St. Louis, MO. The authors would like to acknowledge Ashley Mason, PhD, and Elissa Epel, PhD, for their assistance in the development of the survey instrument. The authors would also like to acknowledge the following individuals: Aishat Adeyemi, BA, Lisa Allen, MPH, Gregory Almonte, Otuwe Anya, MS, Paula Arellano-Cruz, BS, Ruzana Aronov, Danielle Beckham, RN, MSN, CRC, Lauren Buck, BS, Samuel Ceckowski, BS, Maxime Centeno, Virginia, Chan, BS, Anna Marie Chang, MD, MSCE, Melissa Connor, RN, Gabriella Dashler, BS, Jenna Davis, MSN, Cynthia Delgado, BS, Veronica Delgado PA, MS, Brianna DiFronzo, BS, Radhika L Edpuganti, BS, Alyssa Espinera, MD, Fresa Estevez, Shelly Ann Evans, MBA, RN, Cathy Fairfield, BSN, Phillip Fairweather, MD, Theodore Falcon, BS, Brian Fuller, MD, MSCI, David Gallegos, Samuel Ganier, MD, Stephanie Gravitz, MPH, Jeffrey Harrison, Kyle Herbert MD, Judy Hermans, MPH, Elisabeth Hesse, MD, MTM&H, Emily Hopkins, MSPH, Alan Jones, MD, Kia M. Jones, DrPH, Momina Khan, BS, Laura Iavicoli, MD, Robin Kemball, MPH, Laurie Kemble, BHSRT, CCRC, Stuart Kessler, MD, Preeta K. Kutty, MD, MPH, Catherine Lind RN, NP, Karina Loayza, LCSW, Carol Lynn Lyle, PA, MPH, Virginia B. Mangolds, MS, RN, Hannah Makarevich-Manilla, MPH, CCRC, Thomas Mazzocco, RN, L. Clifford McDonald, MD, Sarah Meram, MS, Valerie H. Mika, MS, Reynaldo Padilla, BA, Giacomo Passaglia, BS, Rebekah Peacock, BSN, Danielle Perez, BS, Kye E. Poronsky, MA, Eric Raines, EMT-P, Monica N. Ramage, MSN, RN, Kavita Rampertaap MSN, RN, Sarah Reineck, BS, Nicole Renzi, RN, Erin P. Ricketts, MSPH, Stephanie Rodriguez, Justin Sabol, BS, Valeria Samame, MPHTM, Katie Schneider, MSN, Robert Sellman PA, Kristine Sernulka BSN, CCRP, Jennifer Siller, DNP, RN, Colleen Smith, MD, Timothy Smith, BS, Kelly Szabo, MPH, CCRC, Meghan Tinetti BSN, CCRP, Julia Vargas, BS, Samuel Vargas, Kavey Vidal, Lori Wilkerson, RN, CRC, Darleen Williams, DNP, APRN-CNS, Sallie Anne Wright, MPH, BSMT, and Isaias Yin, LVN.
Footnotes
Please see page 36 for the Editor’s Capsule Summary of this article.
Supervising editor: Donald M. Yealy, MD. Specific detailed information about possible conflict of interest for individual editors is available at https://www.annemergmed.com/editors.
Author contributions: All authors conceived and designed the study and critically reviewed the manuscript for important intellectual content. MF, ZT, RR, RW, JCM, NA, and SS acquired, analyzed, and interpreted the data. RR, JCM, KH, NM, and SS drafted the manuscript. JCM, RR, and NM performed the statistical analysis. RR takes responsibility for the paper as a whole.
All authors attest to meeting the four ICMJE.org authorship criteria: (1) Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; AND (2) Drafting the work or revising it critically for important intellectual content; AND (3) Final approval of the version to be published; AND (4) Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Fundingand support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). This project was funded by a cooperative agreement from the Centers for Disease Control and Prevention (CDC) (U01CK000480) and the Institute for Clinical and Translational Science at the University of Iowa through a grant from the National Center for Advancing Translational Sciences at the National Institutes of Health (UL1TR002537).
The findings and conclusions in this article are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
The Project COVERED Emergency Department Network includes the following: Monica Bahamon, MPH, Jestin N. Carlson MD, MSc, Makini Chisolm-Straker, MD, MPH, Brian Driver, MD, Brett Faine, Pharm D, MS, James Galbraith, MD, Philip A. Giordano, MD, John P. Haran, MD, PhD, Amanda Higgins, MS, Jeremiah Hinson, MD, Stacey House, MD, PhD, Ahamed H. Idris, MD, Efrat Kean, MD, Elizabeth Krebs, MD, MSc, Michael C. Kurz, MD, MS, Lilly Lee SM, MD, Stephen Y. Liang, MD, MPHS, Stephen C. Lim, MD, Gregory Moran, MD, Utsav Nandi, MD, MSCI, Kavitha Pathmarajah, MPH, James H. Paxton, MD, MBA, Yesenia Perez, BS, Richard Rothman, MD, PhD, Walter A. Schrading, MD, Jessica Shuck, BA, Patricia Slev, MD, Howard A. Smithline, MD, Kimberly Souffront, PhD, FNP-BC, RN, Mark Steele, MD, Michelle St. Romain, MD, Amy Stubbs, MD, Morgan Swanson, BS, Josh Tiao, MD, Jesus R. Torres, MD, MPH, Stacy Trent, MD, MPH, Lisandra Uribe, BS, Arvind Venkat, MD, Gregory Volturo, MD, Kelli Wallace, MS, Kurt D. Weber, MD.
A podcast for this article is available at www.annemergmed.com.
Contributor Information
Project COVERED Emergency Department Network:
Monica Bahamon, Jestin N. Carlson, Makini Chisolm-Straker, Brian Driver, Brett Faine, Pharm D, James Galbraith, Philip A. Giordano, John P. Haran, Amanda Higgins, Jeremiah Hinson, Stacey House, Ahamed H. Idris, Efrat Kean, Elizabeth Krebs, Michael C. Kurz, Lilly Lee, Stephen Y. Liang, Stephen C. Lim, Gregory Moran, Utsav Nandi, Kavitha Pathmarajah, James H. Paxton, Yesenia Perez, Richard Rothman, Walter A. Schrading, Jessica Shuck, Patricia Slev, Howard A. Smithline, Kimberly Souffront, Mark Steele, Michelle St. Romain, Amy Stubbs, Morgan Swanson, Josh Tiao, Jesus R. Torres, Stacy Trent, Lisandra Uribe, Arvind Venkat, Gregory Volturo, Kelli Wallace, and Kurt D. Weber
Supplemental Online Content
1. Baseline Survey Questions
2. Follow-up Survey Questions
1. Baseline Survey Questions
1. In the past week, how much has the COVID-19 pandemic affected your stress or anxiety levels?
| 1 Not at all | 2 | 3 | 4 Somewhat | 5 | 6 | 7 Extremely |
2. In the past week, to what extent are you experiencing severe, ongoing job stress where you felt emotionally exhausted, burned out, cynical about your work and fatigued, even when you wake up?
| 1 Not at all | 2 | 3 | 4 Somewhat | 5 | 6 | 7 Extremely |
3. To what extent do you agree or disagree with the following statement:
Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing would decrease my anxiety?
| 1 Strongly disagree | 2 Disagree | 3 Somewhat disagree | 4 Neither disagree nor agree | 5 Somewhat agree | 6 Agree | 7 Strongly agree |
4. In the past week, have you
-
a)
had nightmares related to the pandemic or thought about the pandemic when you did not want to? □ Yes □ No
-
b)
tried hard not to think about the pandemic or gone out of your way to avoid situations that reminded you of it? □ Yes □ No
-
c)
been constantly on guard, watchful, or easily startled? □ Yes □ No
-
d)
felt numb or detached from people, activities, or your surroundings? □ Yes □ No
-
e)
felt guilty or unable to stop blaming yourself or others for the effects of the pandemic or any problems the pandemic may have caused? □ Yes □ No
5. To what extent are you experiencing the following worries and concerns about COVID-19?
Provide a number for each statement using the 1 to 7 scale below:
| 1 Not at all | 2 | 3 | 4 Somewhat | 5 | 6 | 7 Extremely | ||
|---|---|---|---|---|---|---|---|---|
| I worry that I may be secondarily exposing family members or others because of my work | ____ | |||||||
| I worry that patients with unclear diagnoses are exposing others in the community I worry that others at home or elsewhere are afraid to come in contact with me because I’m a health care provider |
____ | |||||||
| I worry that we are having to send patients home without a clear diagnosis | ____ | |||||||
| I worry that our ED, clinic, or hospital is not prepared enough for the pandemic | ____ | |||||||
| I worry that we will not have enough staffing as coworkers are quarantined | ____ | |||||||
| I worry that the personal protective equipment (PPE) is unavailable or inadequate | ____ | |||||||
| I worry about the well-being of coworkers who have been diagnosed with COVID-19 | ____ | |||||||
| I worry that we are not able to accurately diagnose COVID-19 cases quickly enough | ____ | |||||||
| I worry that I might have to undergo quarantine and will not be able to work | ____ | |||||||
2. Follow-up (Post Serologic Testing) Questions
4. In the past week, how much has the COVID-19 pandemic affected your stress or anxiety levels?
| 1 Not at all | 2 | 3 | 4 Somewhat | 5 | 6 | 7 Extremely |
5. In the past week, to what extent are you experiencing severe, ongoing job stress where you felt emotionally exhausted, burned out, cynical about your work and fatigued, even when you wake up?
| 1 Not at all | 2 | 3 | 4 Somewhat | 5 | 6 | 7 Extremely |
-
6.To what extent do you agree or disagree with the following statement:
- Knowing my prior exposure and immunity to COVID-19 by serologic (blood) testing has decreased my anxiety?
| 1 Strongly disagree | 2 Disagree | 3 Somewhat disagree | 4 Neither disagree nor agree | 5 Somewhat agree | 6 Agree | 7 Strongly agree |
4. In the past week, have you
-
a)
had nightmares related to the pandemic or thought about the pandemic when you did not want to? □ Yes □ No
-
b)
tried hard not to think about the pandemic or gone out of your way to avoid situations that reminded you of it? □ Yes □ No
-
c)
been constantly on guard, watchful, or easily startled? □ Yes □ No
-
d)
felt numb or detached from people, activities or your surroundings? □ Yes □ No
-
e)
felt guilty or unable to stop blaming yourself or others for the effects of the pandemic or any problems the pandemic may have caused? □ Yes □ No
References
- 1.Azoulay E., De Waele J., Ferrer R. Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care. 2020;10:110. doi: 10.1186/s13613-020-00722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Du J., Dong L., Wang T. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. 2020;67:144–145. doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhang W.R., Wang K., Yin L. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. 2020;89:242–250. doi: 10.1159/000507639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai J., Ma S., Wang Y. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetwopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rossi R., Socci V., Pacitti F. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elbay R.Y., Kurtulmuş A., Arpacıoğlu S. Depression, anxiety, stress levels of physicians and associated factors in COVID-19 pandemics. Psychiatry Res. 2020;290:113130. doi: 10.1016/j.psychres.2020.113130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodriguez R.M., Medak A.J., Baumann B.M. Academic emergency medicine physicians' anxiety levels, stressors, and potential stress mitigation measures during the acceleration phase of the COVID-19 pandemic. Acad Emerg Med. 2020;27:700–707. doi: 10.1111/acem.14065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barello S., Palamenghi L., Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yin Q., Sun Z., Liu T. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin Psychol Psychother. 2020;27:384–395. doi: 10.1002/cpp.2477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sun D., Yang D., Li Y. Psychological impact of 2019 novel coronavirus (2019-nCoV) outbreak in health workers in China. Epidemiol Infect. 2020;148:e96. doi: 10.1017/S0950268820001090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao X., Zhu X., Fu S. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: a multi-center cross-sectional survey investigation. J Affect Disord. 2020;274:405–410. doi: 10.1016/j.jad.2020.05.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chew N.W.S., Lee G.K.H., Tan B.Y.Q. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu W., Wang H., Lin Y. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288:112936. doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohr N.M., Talan D., Krishnadasan A. COVID-19 Evaluation of Risk in Emergency Departments (Project COVERED) 2020. https://dr2.nlm.nih.gov/search/?q=22586 Available at:
- 15.Von Elm E., Altman D.G., Egger M. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 16.Prins A., Bovin M.J., Smolenski D.J. The primary care PTSD screen for DSM-5 (PC-PTSD-5): development and evaluation within a Veteran primary care sample. J Gen Intern Med. 2016;31:1206–1211. doi: 10.1007/s11606-016-3703-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nigam J.A.S., Streit J.M.K., Ray T.K. COVID-19 stress among your workers? Healthy work design and well-being solutions are critical. 2020. https://blogs.cdc.gov/niosh-science-blog/2020/06/12/covid-19-stress Available at:
- 18.CDC. Healthcare personnel and first responders: how to cope with stress and build resilience during the COVID-19 pandemic. Available at: https://www.cdc.gov/coronavirus/2019-ncov/hcp/mental-health-healthcare.html. Accessed November 16, 2020.