Sir—A hypercoagulable state associated with a high prevalence of thromboembolic disease was reported during the first wave of the COVID-19 UK pandemic, with a 22–37% reported incidence of pulmonary embolism (PE) on computed tomography (CT) pulmonary angiography (CTPA) examinations1, 2, 3 and a 28% incidence of thromboembolism (venous or arterial) in the intensive care unit (ICU) COVID-19 patients in a systematic review.4 The current British Society of Thoracic Imaging (BSTI) guidelines suggest that CTPA be performed in patients with disproportionate hypoxia or a sudden clinical deterioration, but only if the outcome will influence anticoagulation treatment decisions.5, 6, 7
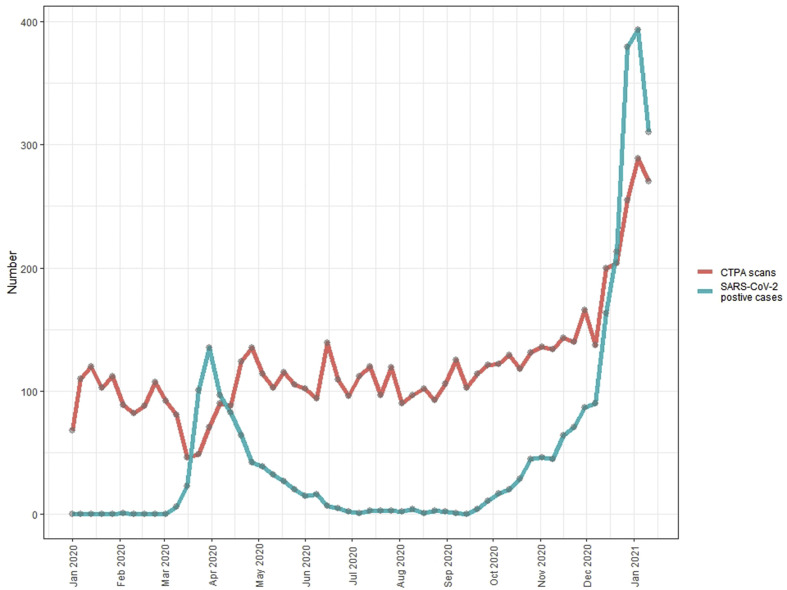
In our ∼1,100-bed tertiary referral centre in the UK, we have noticed a substantial increase in CTPA examinations performed for all indications (Fig 1 ) throughout December 2020 and early January 2021. The overall trend in the number of CTPA examinations does not mirror that of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) polymerase chain reaction (PCR)-positive cases at our institution (Fig 1) with a decrease in CTPA examinations initially observed in the first wave. The rapid rise of PCR-positive cases is thought to be caused, in part, by the variant of concern (VOC). There has been no interim change in the institutional guidance for performing CTPA, which recommend following the current BSTI guidelines,7 nor in the criteria determining hospital admission.
Figure 1.
CTPA investigations for all indications and SARS-CoV-2-positive cases in our tertiary centre over time (weeks).
We performed a service evaluation of CTPA examinations in adults in our institution performed with “COVID” or “coronavirus” specified in the clinical history, comparing a 35-day period corresponding to the local peak PCR confirmed COVID-19 cases 20/3/20 to 24/4/20 (referred to as the first wave) to a 35-day period early in the second wave 1/12/20 to 5/01/21 (referred to as the second wave). The study took place as part of an institutionally improved Trust retrospective service evaluation. Repeat studies in the same patient were excluded, whilst the result closest to the date of the CTPA was used in patients with multiple PCR results. The number of examinations with “COVID” mentioned in the clinical history, over total positive cases in the same time period at our institution, we term the CTPA burden.
There was no significant difference in patient demographics between the first and second wave. During the first wave, 99 CTPA examinations were performed, 3 were reported as non-diagnostic or equivocal for PE (Table 1 ). 273 CTPA examinations were performed in the second wave, of which 9 were non-diagnostic or equivocal for PE. PCR-positive rates were 39.3% for the first wave cohort and 75.0% for the second wave cohort, whilst CT features of COVID-19 were reported on 61.6% in the first wave cohort and 87.5% on the second wave cohort. A similar proportion of CTPA requests originated from the emergency department (29% versus 27%) and whilst 10% of request originated from the ICU during first wave, these account for only 3% during the second wave. Requests from the respiratory high-dependency unit (HDU) accounted for a greater proportion of requests in the second wave.
Table 1.
Characteristics of patients undergoing computed tomography pulmonary angiography (CTPA) investigations performed in first wave versus second wave of SARS-CoV-2 infection.
| First wave 20/3/20 to 24/4/20 | Second wave 1/12/20 to 5/01/21 | p-Value | |
|---|---|---|---|
| SARS-CoV-2 PCR positive cases at our institution (n) | 487 | 1073 | |
| CTPA examinations performed with “COVID” on the clinical request form (n) | 99 | 273 | |
| Median age (years) | 58.4 | 61.4 | p=0.11 |
| Male: female ratio | 0.56 | 0.62 | p=0.30 |
| Requesting location (%) | |||
| ED | 29 (29.2) | 73 (26.7) | p=0.70 |
| ICU | 10 (10.1) | 7 (2.6) | p<0.01 |
| Respiratory HDU | 7 (7.0) | 43 (15.8) | p<0.01 |
| Other | 54 (54.5) | 150 (54.9) | p=0.95 |
| SARS-CoV-2 PCR results (%) in individuals with CTPA requests | |||
| Positive | 39 (39.3) | 205 (75.0) | p<0.01 |
| Negative | 58 (58.6) | 22 (8.1) | p<0.01 |
| Not performed | 2 (2.0) | 46 (16.8) | p<0.01 |
| CT features of COVID-19 (%) | |||
| Positive | 61 (61.6) | 239 (87.5) | p<0.01 |
| Negative | 33 (33.0) | 14 (5.1) | p<0.01 |
| Indeterminate | 5 (5.1) | 20 (7.3) | p=0.45 |
| Proportion of CTPA examinations positive for PE excluding non-diagnostic or equivocal studies (%) | 21/96 (21.9) | 31/264 (11.7) | p=0.02 |
| Proportion of CTPA positive for PE in patients with CT features of COVID-19 (%) | 19/59 (32.2) | 29/232 (12.5) | p<0.01 |
| Proportion of CTPA positive for PE incidence in PCR positive cases (%) | 11/35 (31.4) | 24/193(12.4) | p<0.01 |
| CTPA burden | 0.20 | 0.25 | p=0.02 |
Mann-Whitney U-test was used for non-parametric values and the chi-squared test was used for comparison of proportions.
PCR, polymerase chain reaction, SARS-CoV-2, severe acute respiratory syndrome coronavirus 2, ED, emergency department, ICU, intensive care unit, HDU, high dependency unit, PE, pulmonary embolism.
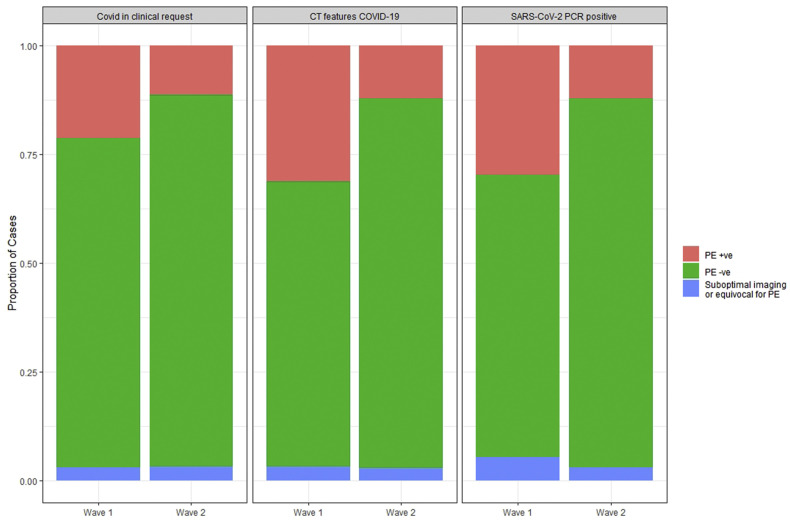
The incidence of PE in the overall cohort of CTPA examinations containing search term “COVID” was lower in the more recent time interval compared with the first wave (11.7% in second wave versus 21.9% in first wave, p=0.02). The difference was greater when comparing only patients with CT features of COVID-19 (12.5% in second wave versus 32.2% in first wave) and when comparing only PCR-positive cases (12.4% in second wave versus 31.4% in first wave, p<0.01; Fig 2 ). Although there has been a near threefold increase in the number of CTPA examinations performed in the same time interval containing “COVID” on the clinical request form, when compared to the background caseload, the CTPA burden has only slightly increased (0.25 in second wave versus 0.20 in first wave, p=0.02).
Figure 2.
Comparison between the first and second wave proportion of CTPA examinations positive for PE in overall cohort with “COVID” on the clinical request form, CT features of COVID-19 infection, and SARS-CoV-2 PCR positive.
Our service evaluation observes a reduced proportion of PE-positive CTPA both in the overall cohort of CTPA examinations with “COVID” on the clinical request form, and within the subgroups of only PCR-positive patients or those with CT features of COVID-19. This may reflect heightened awareness of the increase in thromboembolic disease identified in the first wave, resulting in a lower threshold for requesting CTPA examinations during the second wave. Importantly, however, although the numbers of CTPA examinations have increased, this reflects the similar trend in caseload at our institution: in the first wave, one CTPA was performed per five positive cases, whereas in the second wave, one CTPA was performed per four positive cases, although this is an approximation given patients with “COVID” on the clinical request form are not necessarily SARS-CoV-2 PCR positive. Meanwhile, a reduction in proportion of imaging requests from ICU is attributed to most COVID-19 patients being managed on respiratory HDU units, which is a change in practice from the first wave. The present data are limited and may not reflect nationwide trends given differences in locoregional prevalence and clinician behaviour. Future studies are needed to investigate the impact of the variant of concern as a risk factor for thromboembolism.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Poyiadji N., Cormier P., Patel P.Y. Acute pulmonary embolism and COVID-19. Radiology. 2020;297(3):E335–E338. doi: 10.1148/radiol.2020201955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Léonard-Lorant I., Delabranche X., Séverac F. Acute pulmonary embolism in patients with COVID-19 at CT angiography and relationship to d-dimer levels. Radiology. 2020;296(3):E189–E191. doi: 10.1148/radiol.2020201561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaminetzky M., Moore W., Fansiwala K. Pulmonary embolism at CT pulmonary angiography in patients with COVID-19. Radiol Cardiothorac Imaging. 2020;2(4) doi: 10.1148/ryct.2020200308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boonyawat K., Chantrathammachart P., Numthavej P. Incidence of thromboembolism in patients with COVID-19: a systematic review and meta-analysis. Thromb J. 2020;18(1):34. doi: 10.1186/s12959-020-00248-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.British Society of Thoracic Imaging . January 2021. Rationale for CTPA in covid-19 patients.https://www.bsti.org.uk/media/resources/files/Rationale_for_CTPA_in_Covid_considerations_F.pdf Available at: [Accessed 26 January 2021] [Google Scholar]
- 6.Nair A., Rodrigues J.C.L., Hare S. A British Society of Thoracic Imaging statement: considerations in designing local imaging diagnostic algorithms for the COVID-19 pandemic. Clin Radiol. 2020;75(5):329–334. doi: 10.1016/j.crad.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.BSTI. BSTI NHSE COVID-19 radiology decision support tool. https://www.bsti.org.uk/standards-clinical-guidelines/clinical-guidelines/bsti-nhse-covid-19-radiology-decision-support-tool/ Available at: [Accessed January 2021]