Abstract
With global number of cases 106 million and death toll surpassing 2.3 million as of mid-February 2021, the COVID-19 pandemic is certainly one of the major threats that humankind have faced in modern history. As the scientific community navigates through the overwhelming avalanche of information on the multiple health impacts caused by the pandemic, new reports start to emerge on significant ancillary effects associated with the treatment of the virus. Besides the evident health impacts, other emerging impacts related to the COVID-19 pandemic, such as water-related impacts, merits in-depth investigation. This includes strategies for the identification of these impacts and technologies to mitigate them, and to prevent further impacts not only in water ecosystems, but also in relation to human health. This paper has critically reviewed currently available knowledge on the most significant potential impacts of the COVID-19 pandemic on the wastewater pathway into surface water, as well as technologies that may serve to counteract the major threats posed, key perspectives and challenges. Additionally, current knowledge gaps and potential directions for further research and development are identified. While the COVID-19 pandemic is an ongoing and rapidly evolving situation, compiling current knowledge of potential links between wastewater and surface water pathways as related to environmental impacts and relevant associated technologies, as presented in this review, is a critical step to guide future research in this area.
Keywords: COVID-19, SARS-CoV-2 pandemic, Assessing environmental impact, Wastewater presence, Potential for surface water dispersion
Graphical abstract
1. Introduction
Worldwide, the impacts on public health and the economic impact of the COVID-19 pandemic is more evident as scientific information starts to flow, providing a better understanding of its complexity (Pulido et al., 2020). In recent studies, evidence of emerging side effects of the pandemic besides the regrettable global number of infection cases and deaths is of increasing concern (Abbas et al., 2020; Wu et al., 2020b; Xu et al., 2020b; Zhao et al., 2015). The emerging impacts of the COVID-19 pandemic on the environment, however, remain unelucidated at present, which is a significant knowledge gap requiring further investigation (Zambrano-Monserrate et al., 2020). Despite the fact that some studies report positive changes such as the reduction in pollution indices in highly populated regions including cleaner beaches, environmental noise reduction, and the reduction in greenhouse gas emissions to the atmosphere (Muhammad et al., 2020; Wang and Su, 2020), there are also other studies reporting on negative environmental consequences such as the increase in domestic solid residues, reduction in recycling, and the generation of long lasting plastic materials used for personal protection equipment (Klemes et al., 2020; Saadat et al., 2020; Sharma et al., 2020).
Similar trends have been observed in relation to the aquatic environment, with some studies demonstrating improvements in some water quality parameters (e.g., total dissolved solids, nutrients, suspended particulate matter) in water bodies in urban areas when the concentrations were compared for pre- and during lockdown periods (Hallema et al., 2020; Mandal and Pal, 2020; Yunus et al., 2020). However, other studies point to adverse consequences such as the excessive use of chlorine in wastewater treatment plants to enhance disinfection processes and to prevent the release of active viruses into receiving water bodies. Chlorine is commonly known to react with organic matter to produce disinfection by-products which can be harmful to human and ecosystem health (Cahill and Morris, 2020; Chu et al., 2020; Garcia-Avila et al., 2020; Zambrano-Monserrate et al., 2020). However, it is important to note that a comprehensive investigation is needed into the potential implications of the COVID-19 pandemic on the aquatic environment, which needs to extend beyond the concentration of conventional contaminants or the efficacy of conventional wastewater treatment processes.
This review critically evaluates currently available worldwide knowledge regarding the potential presence of the SARS-CoV-2 virus (which causes COVID-19) and pharmaceuticals used to counteract the effects of COVID-19, in wastewater pathways, to assess the potential for interaction between wastewater pathways and surface water in ways that may impact human health. The review also compiles information and critically reviews current and emerging technologies that may serve to arrest the major threats posed to human and environmental health in these wastewater-to-surface water pathways. The result of this effort, and the ultimate goal of this paper is to identify current knowledge gaps and potential directions for further research and ongoing knowledge creation in these areas.
2. SARS-CoV-2 transmission: current knowledge and relationships to environmental parameters
Currently, human infection with the SARS-CoV-2 virus occurs mainly through contact with droplets or aerosols containing the virus (Meng et al., 2020; Ortiz-Prado et al., 2020). The generation and aerosolization of SARS-CoV-2 virus-laden droplets and aerosols, airborne dispersion, and subsequent deposition on surfaces are governed by flow physics. Relatively large droplets (>100 μm) would evaporate slowly and are likely to settle on surfaces, and smaller droplets (<100 μm) would undergo rapid evaporation and form droplet nuclei (<10 μm) that would remain airborne and disperse over a wide spatial extent. However, such dispersion behavior of droplets can change depending on temperature and humidity which are found to influence droplet properties such as size, expanding the critical size of small and large droplets to 50–150 μm (Feng et al., 2020; Mittal et al., 2020). In fact, a recent study reports that the increase in temperature and humidity can lead to increased number of COVID-19 infections as evident from caseloads from China and Indonesia, while noting the likelihood of rapid transmission due to high population density and mobility, particularly in urban areas (Barcelo, 2020).
Moreover, the association between air quality and the dispersion of SARS-Cov-2 have been shown. Some Italian cities, where the air pollution limits set for PM10 were exceeded for periods <100 days/year, reported >1000 infections. This figure increased to >3000 infections when the air quality remained poor for >100 days/year (Coccia, 2020).
In a study about the relationship between temperature and caseloads to determine the linear and nonlinear relationship between annual average temperature and confirmed cases, the results have shown that temperature had a negative linear relationship with the number of confirmed cases with the curve flattening at a threshold of 25.8 °C. However, no evidence was found supporting that the curve declined for temperatures above 25.8 °C (Prata et al., 2020). Meteorological parameters have also been shown to influence infectious disease propagation, and mathematical relationships have been investigated to assess the impact of this parameter on COVID-19 spread. For example, Yueling et al. (2020) developed an additive model considering the effect of temperature, humidity and diurnal temperature range and the daily death counts from COVID-19. The study reported a positive association of COVID-19 daily deaths with diurnal temperature range, but negative association with relative humidity, concluding that temperature and humidity variation were significant factors on mortality rates. Variation in environmental temperature has been suggested to influence the surface stability of SARS-CoV-2, and temperature-dependent differences in SARS-CoV-2 stability in solution were reported recently (Kratzel et al., 2020).
These early findings provide important base knowledge and insight into potential links between environmental parameters and SARS-CoV-2/COVID-19 impacts, but additional research is needed on the effect of seasonal changes, usually accompanied by temperature fluctuations, on virus stability. This lack of information is identified as a significant knowledge gap which merits timely consideration as seasonal changes progress and the number of cases is increasing or stable, but high in many regions. A better understanding of the effects of environmental temperature on the stability or infection potential of the SARS-CoV-2 virus will certainly serve to more accurately model, predict, and mitigate the immediate term occurrence of new cases.
3. The potential of SARS-Co-V-2 virus presence in wastewater pathways to surface water
In addition to virus transmission via respiratory droplets, there is increasing concern about the potential spread of SARS-CoV-2 to environmental surface water (Ahmed et al., 2020; Cuevas-Ferrando et al., 2020; Randazzo et al., 2020), a potential exposure pathway that is so far largely under-studied. Some viruses (e.g. fish and crustacean viruses such as infectious haematopoietic necrosis virus, (Oidtmann et al., 2017)) are well known to remain viable and infectious, at least temporarily, in natural freshwater environments including lakes and streams, in manufactured environments such as wastewater treatment plants, and in sewage-polluted waters. Therefore, similar to other harmful viruses and pathogens, it is possible that an environmental exposure risk from SARS-CoV-2 exists via contact with such surface waters, and this represents another knowledge gap requiring further study. Conventional risk methodology identifies three exposure pathways when considering the wastewater to surface water pathway, namely, inhalation, dermal contact, and ingestion of polluted water (Foladori et al., 2020).
It is well established that the release of under-treated or untreated sewage into surface waterways poses an epidemiological risk and can lead to the spread of disease through the ‘fecal-oral’ transmission route. Exposure to surface water where there is a sewage spill or release of inadequately treated wastewater increases the risk of ingesting fecal-borne pathogens such as E. coli, giardia, and hepatitis (Chung et al., 2015). Evidence suggest that SARS-CoV-2 may also be shed from human hosts via fecal matter expulsion for weeks after respiratory symptoms abate. For example, (Cheung et al., 2020) have reported that 48.1% of 4243 patients, (Wu et al., 2020a) reported that 55% of 74 patients, had fecal samples positive for the virus. It follows that SARS-CoV-2 may be a candidate for fecal-oral transmission (Arslan et al., 2020; Yeo et al., 2020). Furthermore, other coronaviruses have been shown to exhibit survival for many days in natural and wastewaters (Grundy et al., 2009). As such, despite the fact that dilution may keep the risk low, it is conceivable that high concentrations of water-borne SARS-CoV-2 may occur as the virus is shed from fecal matter as infection rates peak. Whether such environmental viral loads could represent a risk to humans coming into contact with contaminated water sources is unknown, and requires further study. The lack of information on the ability of the SARS-CoV-2 virus to remain viable in wastewaters and in environmental surface water, and the lack of information about infectivity of detected SARS-CoV-2 from environmental samples, are significant gaps in knowledge which merit further investigation. Currently, it is not clear whether the potential presence in wastewater effluent and the potential pathways into freshwater elevates the risk of infection and the spread of COVID-19 (Musmarra et al., 2016; Naddeo, 2020). Under the circumstances, it is essential that further research is undertaken to assess the potential transmission of COVID-19 from wastewater and/or surface water exposure. Here, we further explore some of the factors that may influence this pathway.
While the risk to human health associated with SARS-CoV-2 exposure from environmental samples is unknown, it is important to note that if fecal-oral transmission of COVID-19 is determined to be a concern, this issue would be particularly significant in areas with poor sanitation and/or where diagnostic capacity might be limited, such as, for example, in developing countries (Lodder and de Roda Husman, 2020; Street et al., 2020). A number of very recent studies have reported an increased number of cases where SARS-CoV-2 has been found in feces and/or urine of infected patients (Wang et al., 2020; Xiao et al., 2020; Xu et al., 2020a), although the mechanism of COVID-19-induced gastrointestinal symptoms remains unknown (Kitajima et al., 2020). As such, wastewater monitoring has been proposed as part of the SARS-CoV-2 surveillance strategy and has the potential to combat the disease through early detection. Along with Wastewater-Based Epidemiology (WBE), this can evolve into a potential highly cost-effective approach to the current wide scale screening resulting in reduced resource costs (Mao et al., 2020; Street et al., 2020). In fact, this approach would help to identify the presence asymptomatic individuals in the community who may be carriers of the virus with the ability to infect other people, but not show the symptoms themselves. However several factors may affect the detection of SARS-CoV-2 in wastewater samples and the subsequent implementation of wastewater based epidemiology approaches.
4. Isolation, identification and quantification of SARS-CoV-2 in wastewater and surface water
Detection and monitoring of the SARS-CoV-2 virus in wastewater is challenging due to dilution (Lu et al., 2020), thus requiring concentration of viral particles in water samples for accurate quantification (Bofill-Mas and Rusinol, 2020; Kitajima et al., 2020; La Rosa et al., 2020). A recent review by Lu et al. (2020) identified the several approaches for effective primary concentration of SARS-CoV-2 virions from wastewater. Concentration would be even more difficult in surface water bodies such as lakes and rivers, where the potential discharge of virus carrying wastewater is further diluted. In a recent review paper, Kitajima et al. (2020) suggested that the limited information on the presence of SARS-CoV-2 in wastewater is mainly because of the lack of past research focused on the virus, and the initial information proposing person-to-person as the only spread mechanisms. Importantly, they also found that other studies have suggested that standard virus concentration methods are inefficient for recovering enveloped viruses from water samples. Nevertheless, a study from 2013 reported the detection of coronaviruses in wastewater (Wong et al., 2013), and studies of the SARS outbreak in 2004 (caused by the enveloped coronavirus SARS-CoV) showed virus RNA being detected in 100% of untreated and 30% of disinfected wastewater samples collected from a hospital in Beijing, China (Wang et al., 2005). The presence of SARS-CoV-2 has already been reported in wastewater in Australia, France, the Netherlands, and USA (Ahmed et al., 2020; Gonzalez et al., 2020; Hata and Honda, 2020; Kitajima et al., 2020; Lodder and de Roda Husman, 2020; Medema et al., 2020), confirming that it can be concentrated from and detected in varied wastewater environments.
Bogler et al. (2020) identified three main approaches for the detection and monitoring of SARS-CoV-2 in wastewater, namely, qualitative, quantitative molecular, and in-vitro counts by plaque-forming units (PFU). Each of these approaches have different capabilities for detection (e.g. estimates of virus RNA or estimates of infective virions), different speeds of detection, and different levels of sensitivity, which require certain virus concentrations to be present in wastewater. Many of the most recent studies focusing on detection of SARS-CoV-2 in wastewater have employed detection of viral RNA and targeted gene analysis via quantitative RT-qPCR (Lodder and de Roda Husman, 2020). The technique was deemed effective in detecting the virus in wastewater even within a week after the first reported cases of COVID-19. However, this method of gene fragment identification does not provide information about the viability or infectivity of the virus from such environments. One study (Rimolldi et al., 2020) found that SARS-CoV-2 viral particles isolated from wastewater did not appear to infect VERO E6 cells (a kidney cell line from African green monkeys) when cultured together. However, caution must be exercised when interpreting such outcomes, as in vitro experimental conditions are rarely representative of the precise biological host conditions that may foster infection and disease development. Therefore, we identify the lack of information about the viability and infectivity of SARS-CoV-2 particles from wastewater and other environmental reservoirs as a significant knowledge gap requiring further research.
As evidence builds on the occurrence of SARS-CoV-2 in wastewater (Collivignarelli et al., 2020; Nemudryi et al., 2020), there is a significant need to identify the feasibility of testing and detection methodology for broad scale implementation, to understand the main environmental pathways and fate of the virus, as well as to assess SARS-CoV-2 infection capacity as a function of time and the related inactivation mechanisms implemented during wastewater treatment. Some studies have suggested monitoring wastewater to identify the transmission of the virus within entire communities, suggesting well-established approaches such as Wastewater-Based Epidemiology could be implemented to identify fragment biomarkers of the virus that represent a particular community (Daughton, 2020). For example, a recent study investigated the efficiency of computational analysis for SARS-CoV-2/COVID-19 surveillance (Hart and Halden, 2020). It was found that one infected individual is detectable (at least in theory) among 100–2,000,000 persons through wastewater monitoring, meaning that 2.1 billion people could be monitored globally in 105,600 sewage treatment plants, potentially saving billions of dollars. However, in their study, Hart and Halden (2020) did not incorporate field-based data because relatively few studies have quantified the SARS-CoV-2 virus in wastewater effluent. This lack of field-based information represents another significant knowledge gap which requires further exploration, because validation of the computational analysis with field results presents the best opportunity for optimized model accuracy, thereby creating the highest likelihood of cost effective COVID-19 monitoring.
It is important to note that the use of WBE or other epidemiology approaches do not indicate risk of disease development associated with exposure to sewage contaminated waters. Complementary clinical testing campaigns would be required to accomplish this, because SARS-CoV-2 RNA detection in wastewater using RT-qPCR is not necessarily indicative of viable or transmissible virus load. Rather, the use of WBE may have benefits over clinical testing as an indicator of community spread because one wastewater treatment plant is potentially able to provide an estimate of SARS-CoV-2 incidence within a large population.
Because the risks to human health associated with exposure to wastewater which contains indicators of SARS-CoV-2 genes has not been quantified, it is important to assess the effectiveness of current wastewater treatment practices in removing or deactivating viruses in wastewater. It is expected that many conventional sewage treatment methods including disinfection are able to inactivate the SARS-CoV-2 virus. Regrettably, in some developing countries or in rural areas of developed countries such sewage treatment practices are not prevalent. As some developing countries are already susceptible to the COVID-19 pandemic because of the limitations in basic sanitation and environmental conditions that can favor the virus spread (Usman et al., 2020), it is important to understand the environmental factors that could affect the transmission and virus survival after release in wastewater. It has been suggested that SARS-CoV-2 virus is capable of surviving for several days in untreated sewage, and for a much longer period in low-temperature regions. While this scenario is not yet been well studied, it is imperative that more work is done to understand this potential exposure risk since around 1.8 billion people worldwide are estimated to be using sewage contaminated drinking water sources (Bhowmick and Dhar, 2019).
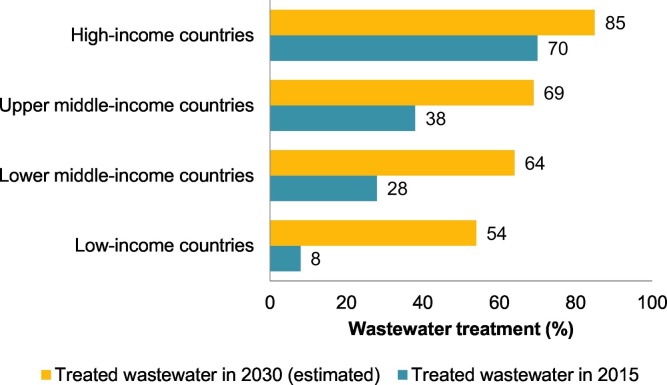
Is has also been suggested that in some cases conventional wastewater treatment processes may not be capable of completely removing SARS-CoV-2 (Lesimple et al., 2020; Zhang et al., 2020a), and is such situations pretreatment techniques are suggested to minimize the entry of the virus into wastewater due to the unknown infectivity of SARS-CoV-2 from such environments. These include, membrane filtration, virus inactivation using ultraviolet radiation and chlorination. Further, the incorporation of effective monitoring tools has been recommended for wastewater treatment plants, in order to identify any increase in the virus load which may accompany outbreaks or re-emergence after control measures to stop the spread of the disease are lifted (Venugopal et al., 2019). It is important to note that advanced monitoring and treatment of wastewater would be especially limited in resource-constrained regions such as low income countries which had capacity to treat only about 8% of wastewater in 2015 (Street et al., 2020). Overall wastewater treatment capacity is expected to reach 54% by 2030 even in low-income countries (see Fig. 1 ), but this is still low when considering potential impacts in the context of disease propagation. Hence, research is essential for developing economically feasible alternative approaches to effectively detect the virus in wastewater (Adelodun et al., 2020; Street et al., 2020).
Fig. 1.
Capacity of wastewater treatment in regions with different income levels (modified from (WWP, 2017)).
Some recent studies have also reported the presence of pathogenic microorganisms in wastewater plumbing systems, confirming that even in countries where conventional wastewater treatment is prevalent, the potential for disease transmission may exist (Gormley et al., 2020). For example, empty U-bends in bathrooms were noted as a potentially hazardous SARS-CoV-2 virus propagation mechanism in a study by Gormley et al. (2020). They found that U-bends in bathrooms draws contaminated air into the room, highlighting the need for more studies on the transmission role of wastewater plumbing systems. Based on all this evidence, if SARS-CoV-2 proves to remain viable and infective in wastewater environments, the risk of disease spread from wastewater exposure would be much higher in regions which lack access to effective wastewater treatment relative to regions where conventional wastewater treatment is widely available (Nwobodo and Chukwu, 2020).
Several preventive measures have been proposed to mitigate these potential exposure pathways, such as decentralization of wastewater treatment systems, extensive community-wide monitoring of the spread of the virus, improved sanitation infrastructure and policy intervention. However, the limited knowledge on the fate, viability, and infectivity of SARS-CoV-2 in wastewater remains as a significant knowledge gap, and the effectiveness of any proposed wastewater treatment measures remains difficult to validate (Adelodun et al., 2020). These complications are further compounded by the fact that the treatment of excreta in rural communities commonly occurs via decentralized self-processing approaches including, for example, the use septic-tank or biogas systems. These systems may require improved raw sewage management to prevent contamination compared with centralized systems where the use of state-of-the-art ventilation and plumbing systems may suffice to control viral aerosols (Huraimel et al., 2020; Meng et al., 2020).
In contrast to wastewater, research studies are yet to investigate virus prevalence in surface waters. In fact, a recent study noted the lack of research into the presence of not only the current SARS-CoV-2 virus, but also other types of coronaviruses in surface water (La Rosa et al., 2020). Some studies have found limited evidence via RT-qPCR techniques of various coronaviruses in river, lake, and reservoir water (Alexyuk et al., 2017; Blanco et al., 2019). Despite these studies reporting low detection rates (number of positive samples), their findings suggest the possibility of surface water contamination with coronaviruses via discharge of poorly treated wastewater. Therefore, extensive field-based investigations are necessary to understand SARS-CoV-2 virus prevalence not only in raw and treated wastewater, but also in receiving surface waters. These investigations should include assessment of virus viability and infectivity, if detected. This will generate knowledge required for quantitative risk assessment and to assist in monitoring outbreaks within communities.
5. Technology perspective and challenges
5.1. Next generation sensing devices for SARS-CoV-2 detection in environmental samples
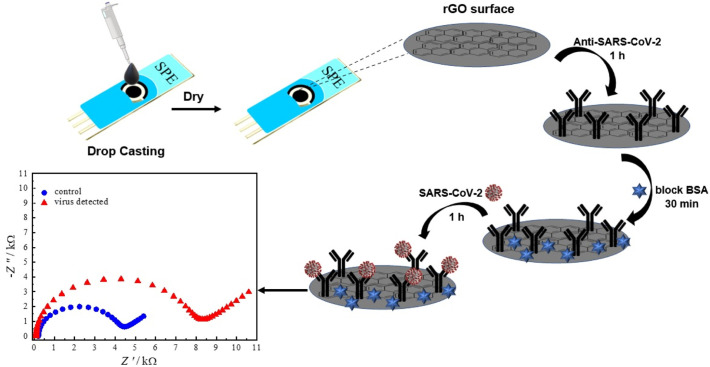
It is clear that an accurate, low-cost, and easy-to-use SARS-CoV-2 monitoring system can support the strategies adopted by the authorities to reduce the economic and social impacts of the COVID-19 pandemic. This is particularly important since different countries around the world are at widely varying stages of the pandemic. In this sense, electrochemical sensors have several advantages because they can be miniaturized and allow in situ analysis (Rocha et al., 2020). Several biosensors combined with nanotechnology, especially those that use reduced graphene oxide (rGO) in their preparation, have been successfully used in the determination of different molecules of environmental and biological interest (Cesarino et al., 2015; Da Silva et al., 2018). The technology is ready to be developed for use in the detection of SARS-CoV-2 in environmental samples. For example, impedimetric biosensors constructed by immobilizing biological recognition elements to an electrode surface (Fig. 2 ) have been suggested can be used for this purpose. In previous studies (Donini et al., 2020; Kohori et al., 2018; Rocha et al., 2020), the immobilization of antibodies and enzymes on the surface of rGO-modified carbon electrodes was found to not require immobilization agents such as pyrene-NHS, or EDC-NHS, reducing one step in the preparation of the immunosensor, which reduces the cost and detection time. Thus, a simple, inexpensive and less aggressive immobilization procedure for biomolecules using rGO can be employed to prepare an impedimetric immunosensor for the detection of SARS-CoV-2. The carbon screen-printed electrode (SPE)/rGO platform can detect the antigen-antibody binding procedures of SARS-CoV-2 via impedance changes in a low frequency range.
Fig. 2.
Schematic representation of the impedimetric immunosensors preparation for SARS-CoV-2 detection in environmental samples.
Some recent studies (Chandra, 2020a; Layqah and Eissa, 2019; Tymm et al., 2020) highlight the use of electrochemical sensors in the diagnosis of COVID-19. Although the focus of these studies was on clinical analysis, these sensors can also be evaluated for the detection of SARS-CoV-2 in water. Chandra, 2020a, Chandra, 2020b conceptualized a miniaturized electrochemical impedance spectroscopy-based detection of COVID-19 using metallic nanoparticles (NPs), electrochemically engineered nano-dendroids, and graphene oxide (GO) nanocomposites. Layqah and Eissa (2019) demonstrated an electrochemical immunosensor for the coronavirus (CoV) associated with the Middle East Respiratory Syndrome (MERS) using an array of NPs-modified carbon electrodes. The assay was performed in 20 min with detection limit (LOD) as low as 0.4 and 1.0 pg·mL−1 for HCoV and MERS-CoV, respectively. In the work by Tymm et al. (2020), the diagnostics for SARS-COV-2 using different methodology of detection was emphasized. In regards to electrochemical sensors, another study presented an in-house built biosensor device (eCovSens) and compared it with a commercial potentiostat consisting of a fluorine-doped tin oxide electrode and NPs. The LOD was found to be 90fM with eCovSens and 120 f. with potentiostat for spiked saliva samples (Mahari et al., 2020). Although some SARS-CoV-2 detection methods have been developed, the need for technologies with faster turnaround of testing results remains because of the pressure on increasing healthcare and the need for early diagnosis. The lack of sensitive, rapid and specific biosensors for SARS-CoV-2 detection is a paramount knowledge gap broadly identified and attracting significant attention not only because of the urgent need to provide biosensors capable of helping during the ongoing pandemic, but also to alleviate other virus-related illness such as human immunodeficiency virus (HIV), or hepatitis A virus (HAV).
Table 1 lists the different types of sensors developed for detecting specific viruses with the potential to cause water-borne diseases. As shown, all the studies report laboratory scale technology maturity status, meaning that the technology is being tested and several further steps are needed before it may be available for public use. A variety of sensing device technologies have been reported for potential application for SARS-CoV-2 as well as other coronaviruses (e.g., MERS-CoV) and other non-related viruses such as the hepatitis virus. In a very recent paper, a complete review of state-of-the-art ultrasensitive electrochemical sensors for the detection of pathogenic viruses was presented (Khan et al., 2020). In their work, Khan et al. (2020) reviewed the range of applications of chemical biosensors for different virus detection and discussed several different fabrication techniques, detection principles, and applications for virus detection as well as the potential of these devices for rapid identification of the COVID-19 virus.
Table 1.
Available technologies for detection of SARS-CoV-2 virus and other virus with the potential for causing water-borne diseases.
| Sensing device technology | Virus type | Main findings | Technology maturity status | References |
|---|---|---|---|---|
| Optic fiber biosensors | SARS-CoV-2 | The study provides an overview of evanescent wave absorbance and localized surface plasmon resonance-based optic fiber platform for potential screening of COVID-19 | Laboratory scale | (Nag et al., 2020) |
| Electrochemical sensors | SARS-CoV-2 | Point-of-care sensing techniques integrated with smartphones are proposed to not only track the disease spreading, but it is anticipated that powerful integrative electrochemical label-free technologies can be escalated to develop a personalized analytical system to combat COVID-19 | Laboratory scale | (Chandra, 2020b) |
| Graphene-based sensors | SARS-CoV-2 | Antibody-conjugated graphene sheets are suggested capable of rapidly detecting targeted virus proteins, useful for large population screening, but also for the development of environmental sensors | Laboratory scale | (Palmieri and Papi, 2020) |
| Electrochemical biosensor | SARS-CoV-2 | A sensitive electrochemical detection technology using calixarene functionalized graphene oxide for SARS-CoV-2 has been developed. The technology was confirmed to practicably detect the RNA of SARS-CoV-2 without nucleic acid amplification | Laboratory scale | (Zhao et al., 2021) |
| Electrochemical biosensor | Hepatitis virus | A pulse-triggered electrochemical sensor has been fabricated using graphene quantum dots and gold-embedded polyaniline nanowires, prepared via an interfacial polymerization and self-assembly | Laboratory scale | (Chowdhury et al., 2019) |
| Electrochemical immunosensor | MERS-CoV | The device uses specific envelop protein antibody as recognition element, possesses a dynamic range of 0.001 to 100 ng/mL, and detection limit of 1 pg/mL | Laboratory scale | (Layqah and Eissa, 2019) |
Technology maturity status = Laboratory scale: Technology concept and/or application formulated; Bench scale: Component and/or breadboard validation in laboratory environment; Field application: System prototype demonstration in a space environment.
5.2. Virus inactivation in water
Viruses in general are considered to have relatively higher resistance to conventional water disinfection process compared to bacteria (Garcia-Gil et al., 2020), which highlights the significance of the search for novel, cost-effective methodologies for viral inactivation in water (Adelodun et al., 2020; Zhang et al., 2020c). Usually, it is assumed that predatory microorganisms (e.g., protozoa) in wastewater can inactivate a significant proportion of the viruses present (Yang et al., 2005). Conventional secondary wastewater treatment processes are capable of removing 2–3 log10-cycles of virus content through adsorption to the solid particles of activated sludge (Zhang et al., 2018). Membrane technologies (e.g., ultra, nano-filtration, reverse osmosis) have also proven to be another efficient approach towards the removal of viruses and/or solid-associated viruses, achieving removal efficiencies in the range from 0.2 log10- to 6.5 log10-cycles using ultra-filtration and reverse osmosis, respectively (Bhowmick and Dhar, 2019). The use of any of these technologies for the removal of viruses involves only mechanical separation, but not the inactivation of the viruses. In this regard, tertiary treatment processes have been reported to be effective for virus inactivation with variable efficiency (Carducci et al., 2020), and several different technologies have been tested for the inactivation of different viruses in water. Table 2 shows a selected overview of recent studies which have reported on the use of conventional and non-conventional methodologies for the inactivation of viruses in water.
Table 2.
Available technologies for virus inactivation in water.
| Virus type | Inactivation method | Main findings | Technology maturity statusa | References |
|---|---|---|---|---|
| African swine fever virus | Ozone (O3) | 2-log10 (99%) viral reduction using O3, 5 mg/L after 1 min at room temperature | Field application | (Zhang et al., 2020b) |
| MS2, ΦX174 bacteriophages | Solar disinfection | Inactivation outcome highly dependent on detention time, radiation availability, presence and concentration of organic carbon and radiation pathway | Field application | (Zhang et al., 2020c) |
| MS2 | Wet peroxide oxidation | Al/Fe-pillared clay catalyst (Al/Fe-PILC) to assist wet peroxide oxidation, optimal initial ratio 1.2 mg H2O2/mg Fe | Laboratory scale | (Ibarguen-Mondragon et al., 2020) |
| Coxsackie B, adenovirus | Chlorine disinfection | Coxsackie B virus required higher concentration and longer detention times for 4-log10 inactivation | Field application | (Rachmadi et al., 2020; Wati et al., 2019) |
| Different types | Cold plasma | Generation of ROS involved in the inactivation process | Laboratory scale | (Filipic et al., 2020; Filipić et al., 2019) |
| MS2, ΦX174 bacteriophages | Electrocoagulation-electro oxidation | The coupled process was found to be inconsistent in the removal/inactivation of viruses in surface and groundwater | Bench scale | (Heffron et al., 2019) |
| MS2 | CO2 bubbles | Up to 3-log10 viral reduction was observed using CO2 at 205 °C | Laboratory scale | (Sanchis et al., 2019) |
| rAdV-GEP | Alternative water disinfectants | N-chlorotaurine, bromamine-T, and grape seed extract were tested. Inactivation of 2.5 to 4-log10 was achieved after 120 min, depending on the chemical tested | Laboratory scale | (Garcia et al., 2019) |
| PEDV, FeCoV | Photocatalysis with graphene oxide (GO), carbon dots | Viruses from the Coronaviridiae family (porcine epidemic diarrhea virus and Alpha coronavirus 1) were inactivated | Laboratory scale | (Chen et al., 2016; Innocenzi and Stagi, 2020) |
| MS2 | Photocatalysis with TiO2 | Nano P25 TiO2 showed higher efficiency for virus inactivation that carbon nanotubes, ZnO, and Fe3O4 | Laboratory scale | (Chen et al., 2017) |
Technology maturity status = Laboratory scale: Technology concept and/or application formulated; Bench scale: Component and/or breadboard validation in laboratory environment; Field application: System prototype demonstration in a space environment.
From the information provided in Table 2, it is important to note that different advanced oxidation processes (AOPs) have been tested and identified as having great potential and provides a variety of alternatives for virus inactivation. For example, the use of either solar disinfection, ozonation, wet oxidation, or even cold plasma to generate reactive oxygen species (ROS) have shown significant potential for inactivation not only of bacteria and other pathogenic microorganisms (Huesca-Espitia et al., 2017), but also virus inactivation. Other methodologies have been reported, including conventional chlorination procedures, the use of alternative disinfectants (Garcia et al., 2019; Rachmadi et al., 2020), and the application of high temperature CO2 injection in water for viruses inactivation (Sanchis et al., 2019). No studies on the inactivation or removal of SARS-CoV-2 in water are available, probably because of the reported very low survival of the virus in surface water, wastewater, sludge and biosolids at temperatures higher than 20 °C, and the higher inactivation rate of Coronavirus when compared with others such as enteric viruses (e.g., Adenoviridae, Astroviridae, Caliciviridae) considered by WHO as a concern in relation to water (Carraturo et al., 2020; La Rosa et al., 2020). However, the virus poses high risks due to its highly infectious nature and resistance to conventional water and wastewater treatment technologies (Garcia-Gil et al., 2020; Haleem et al., 2020). Assessing the time elapsed since the start of the outbreak and the release of active or inactive virus into receiving water bodies is a further interesting research area which merits exploration, because it is only in the last few months that the virus has gained attention and there has not been adequate time to undertake studies on its mobility through various pathways such as sewers, water treatment plants and surface water bodies.
It is also important to note the use, in some cases, of bacteriophage viruses such as MS2 or ΦX174 to run experiments in water as a surrogate of other human pathogenic viruses. Bacteriophages have been reported as a surrogate also for SARS-CoV-2 for testing inactivation using UV-C lamps because of their similar envelope and size to coronavirus (Cadnum et al., 2020; Carducci et al., 2020). However, very little is known about other characteristics that may be different between bacteriophage viruses and SARS-CoV-2. For example, bacteriophage is known to possess a double stranded RNA genome which means greater stability compared to single-stranded RNA genome in coronaviruses (Carducci et al., 2020). Usually the difference may be considered appropriate from an inactivation perspective, as bacteriophages may serve as a conservative surrogate for SARS-CoV-2, but further studies are required to robustly assess these differences and their potential influence in relation to the use of surrogates. This presents a significant knowledge gap which merits further investigation.
Another interesting pending research avenue is the role potentially played by nanomaterials in the inactivation of SARS-CoV-2 in water (Sportelli et al., 2020). Nanotechnology has been used in the past for the production of contamination-safe personnel protection equipment based on the significant antimicrobial and antiviral properties of some specific nanomaterials (Chen et al., 2016). In a recent review, Kokkinos et al. (2020) provided information on the outstanding capacity of nanomaterials for the removal and inactivation of different viruses in water (Kokkinos et al., 2020). These researchers collated knowledge demonstrating the disinfection potential of doped-TiO2 nanofibers, Fe3O4-SiO2-NH2 nanoparticles, Ag-doped TiO2, Bi2WO6, and NeTiO2 for the inactivation of a wide variety of viruses including bacteriophage MS2, f2, and poliovirus-1 in water with highly encouraging results.
Nevertheless, the reported nanomaterials are just a few compared to the wide variety of nanoparticles, nanotubes, nanosheets, nanorods, nanocages, nanobranches, and several other engineered nanomaterials (ENMs) reported in literature with different and versatile characteristics and potential for application in virus inactivation (Bandala and Berli, 2019). However, the use of nanomaterials for water treatment needs to be considered with caution due to the potential toxic nature of some of these materials which can be concerning (Gardea-Torresdey et al., 2014; Backshi et al., 2015). The interactions between ENMs and biological systems is known to be complex and with considerable inherent difficulties in monitoring of their effects either in vivo or in vitro, and with oversimplified measurement of their effects on living organisms.
This dearth of information about the efficacy of engineered nanomaterials on the inactivation of viruses in water is considered as another significant knowledge gap since several ENMs have proven to be efficient in the inactivation of a significant diversity of pathogenic microorganisms, and only a few of them have been investigated for virus inactivation. Additionally, as the nanotechnology industry grows, new ENMs are created with specific features and great expectation for their use in different applications. This in turn results in increasing the knowledge gap as the number of untested materials increase (Bandala and Berli, 2019).
6. COVID-19 related pharmaceuticals in wastewater pathways into surface water
6.1. The risk of COVID-19 related drugs in wastewater pathways into surface water
Additional to the risk of the potential release of SARS-CoV-2 virus to surface water, wastewater also possess the potential for carrying chemical contaminants harmful to the aquatic ecosystem and potentially dangerous to human health. Among many different chemical compounds, pharmaceuticals are the most significant because of the threat posed by their biological activity, persistence, and mobility in the environment (Bandala and Rodriguez-Narvaez, 2019). Consequently, the effort of controlling the adverse health effects caused by COVID-19 may also have significant adverse repercussions on the water ecosystem. As an example, one of the common symptoms of COVID-19, and any other viral upper respiratory tract infection, is fever. As the number of COVID-19 infections and hospitalization cases peak, it would be expected that the amount of drugs being used to control fever, dyspnea, or other related symptoms will correspondingly increase.
Usually, only a small part of these drugs are metabolized within the human body with a significant fraction being released from the patient organism through their feces and urine which will eventually end up in sewage (Zeidman et al., 2020). It is well-known that conventional wastewater treatment is not capable of degrading most of these pharmaceuticals, and many are instead released back into receiving water bodies (Rodriguez-Narvaez et al., 2017). Many of these pharmaceuticals are considered to be endocrine disrupting compounds able to generate health impacts even at trace concentrations in water. Therefore, their quantification in water and associated risk is fundamental research as well as assessing the correlation between the amounts of pharmaceuticals being released into surface water and the development of cost effective technologies for their degradation and removal (Rodríguez-Narvaez et al., 2020).
The medical community have devoted a significant amount of effort identifying allopathic drugs, natural products, and homeopathic products with treatment potential against COVID-19 symptoms (Dong et al., 2020). Either in agreement with WHO or otherwise, at least 12 potential COVID-19 treatments are currently being widely tested/used, including drugs used for HIV and malaria such as chloroquine, and experimental antiviral drugs (Colson et al., 2020; Kupferschmidt and Cohen, 2020). As result, a significant amount of active ingredients and their metabolized relatives are being released into the sewer on a daily basis (Bensalah et al., 2020). The significant presence of these compounds in water bodies and drinking water sources highlights the need for cost-effective treatment as their non- or low-biodegradable characteristics leads to their persistence in water and potential health and environmental risks (Zaied et al., 2020).
The lack of information about the type and amount of COVID-19-related active principal and metabolites being released into sewage, arriving in the wastewater influent, or being released with the wastewater treatment plant effluent into receiving water bodies is a highly significant knowledge gap which merits further investigation because of the known and unknown biological activity of these chemicals and the potential effects these may have on aquatic species and/or human health. Very little is known about the mass balance for COVID-19-related drugs or their metabolites in wastewater treatment plants. Therefore, the efficacy of the water treatment processes on their elimination cannot be assessed solely using the currently available knowledge. Consequently, this can also be highlighted as an important research avenue. Further, knowledge creation about the persistence, bioaccumulation, bioconcentration, biomagnification and/or environmental fate of the active principal and/or metabolites after their release into aquatic ecosystems is another challenging research avenue which requires attention.
6.2. Detection and quantification of COVID-19 relevant pharmaceuticals in wastewater effluent and surface water
In the last decades, the wastewater treatment sector has been facing several different technology challenges related with the increased water stress, wastewater reuse in agriculture and other industrial applications (Gómez-López et al., 2009). Additionally, the improvement in analytical technologies used for water analysis have shown that many of the conventional wastewater treatments currently used do not suffice to eliminate some pollutants generated from anthropogenic activities (Krzeminski et al., 2019). Further, the reuse of wastewater effluent without appropriate treatment can lead to the dispersion of these pollutants in soil and water matrices (Medrano-Rodríguez et al., 2020). One of the major outcomes of the dispersion of pollutants from poorly or improperly treated wastewater is the detection of organic molecules of anthropogenic origin (pharmaceuticals and personal care products) at trace levels (ng/L-μg/L) in water bodies (Blanchet et al., 2017; Reis et al., 2019; Wang et al., 2018). These pollutants, also called contaminants of emerging concern (CECs), are considered as a proxy for anthropogenic activity and in many cases have served as tracers to assess their level of consumption in the surrounding communities. The presence of CECs in water resources pose a range of different consequences depending on their chemical composition, toxicity, and potential for bioaccumulation in the trophic chain (Guedes-Alonso et al., 2020; Hernández et al., 2019; Martínez-Piernas et al., 2019; Yuan et al., 2018; Zhang et al., 2019).
Due to the stress caused by the pandemic, people have resorted to using non-prescribed drugs as a form of COVID-19 prevention. Although chloroquine (CQ) and hydroxychloroquine (HCQ) present an unproven hypothesis to treat COVID-19, the consumption of these and other drugs has increased considerably in recent months. Consequently, significant quantities of wastewater contaminated with CQ and HCQ being released into the environment is a distinct possibility. Considering this scenario, the generation of methodologies for the degradation of these drugs, as well as protocols for their determination in wastewater effluent and surface water resources is a significant research need.
A recent state-of-the-art review (Saka, 2020) into the detection techniques and quantitative determination methods for CQ and its related metabolites found that the main methods used for CQ analysis are liquid chromatography, capillary electrophoresis, electroanalytical, spectrophotometric, and ELISA-based methods. In most of the studies, detection and quantification of CQ were performed in pharmaceutical dosage formulations and biological matrices and the most frequently used technique is high performance liquid chromatography (HPLC). In this case, the potential use of electroanalytical methods emerges as highly significant for the determination of CQ, HCQ, and other pharmaceuticals in wastewater effluent and surface water because of their ability to make in situ analysis possible. Some carbon-based electrochemical sensors, particularly carbon nanotubes and graphene have been successfully used in the analysis of CECs. For example, sensors based on rGO-metal nanoparticles have been used for estriol hormone and glyphosate detection in water samples (Cesarino et al., 2015; Donini et al., 2018; Setznagl and Cesarino, 2020), where the devices yielded low limits of detection for the target analytes.
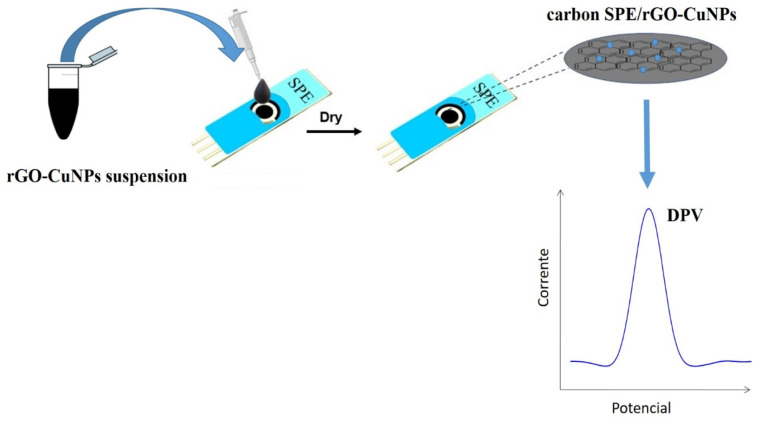
Among the metallic nanoparticles studied, copper nanoparticles were found showing the best results when compared to the other nanoparticles. Fig. 3 illustrates a schematic overview of the preparation procedure of a sensor based on rGO-CuNPs composite that could be used in the analysis of COVID-19-relevant pharmaceuticals in wastewater effluent and surface water using differential pulse voltammetry (DPV) technique. As shown, the preparation procedure is simple and uses relatively inexpensive materials, but the resulting sensors possess wide applicability for environmental sample analysis. For example, a recent study reported the development of a sensor based on reduced graphene oxide for tetracycline determination that uses just 10 μL of the sample and generates highly selective results within 6 min (Lorenzetti et al., 2020). Another study used a graphene-oxide-based electrochemical sensor for selective, highly sensitive (0.6 μAμM−1 cm−2), and strong anti-interference capacity for detection of naproxen (Qian et al., 2020).
Fig. 3.
Schematic representation of a carbon SPE/rGO-CuNPs to be used for the analysis of pharmaceuticals in wastewater effluents and surface water.
One of the common characteristic of this type of sensors, however, is they are usually disposable after use which make them convenient for field applications, but may also imply some drawbacks considering the accumulation in the environment of the base materials used for their manufacture. As noted earlier, there is an increasing concern about unknown and undesirable interaction of nanomaterials with the environment after their release into water or soil. In this regard, the development of re-usable sensors emerges as a very interesting research avenue worthy of consideration to increase the life cycle of the technology and to avoid the release of nanoparticles into the environment. Until now, very few studies on the development of reusable electrochemical sensors are available, and even fewer devoted to the detection of pharmaceuticals in water (Costa-Rama et al., 2020) which makes this a significant knowledge gap worthy of further exploration.
7. Conclusions
In this paper, a review of the most significant potential impacts of the COVID-19 pandemic on the wastewater pathway into surface water, as well as different technologies that may serve to counteract the major threats posed, key perspectives and challenges was undertaken. The following are the main findings:
-
•
Besides the best understood spreading of the SARS-CoV-2 virus through droplets and aerosols in airborne dispersion, very little is known about the effect of environmental conditions, such as temperature or humidity, on the transmissibility of the virus. This is identified as a significant knowledge gap as the climate moves towards fall/winter season.
-
•
Fecal-oral transmission of the SARS-CoV-2 virus has been reported. However, there is a significant lack of information on the role wastewater effluent may play in such infection pathways, in the spread of COVID-19 resulting from the release of poorly or untreated wastewater effluents into freshwater bodies, or in the factors that may influence the transmission and survival of the virus in aquatic ecosystems.
-
•
Additional to the identification and quantification of the SARS-CoV-2 in water and wastewater using conventional methodologies such as RT-PCR, other emerging approaches such as wastewater-based epidemiology (WBE) have been suggested to complement information and identify fragment biomarkers of the virus. The use of WBE as a preventative and monitoring measure has been found to be particularly appealing for application in developing countries and/or rural communities where scattered population and lack of resources limits widespread application of RT-PCR technology.
-
•
The need for accurate, low-cost, and easy-to-use sensors for either SARS-CoV-2 monitoring or related pharmaceuticals in wastewater pathways into surface water was identified as a significant knowledge gap which merits further exploration in order to reduce not only economic and social impacts of the COVID-19 pandemic, but also other undesirable impacts on the aquatic environment.
-
•
Virus inactivation and/or degradation of COVID-19 related pharmaceuticals in water was found to be not only important, but also a challenging scientific task because of the relatively high resistance of the virus to conventional water disinfection processes compared to bacteria and the known and unknown biological activity of some pharmaceuticals. Different technologies have been proposed and successfully tested, but most of these have significant drawbacks such as high cost, the involvement of phase change separation without inactivation/degradation of the viruses/pharmaceuticals, or the risk to the environment from the release of potentially toxic compounds during treatment. The search for novel, cost-effective methodologies for virus inactivation and pharmaceuticals degradation in water is also identified as an important future research avenue worthy of consideration.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
This work was partially supported by Nevada Water Resources Research Institute (Grant No. G16AP00069).
Editor: Damia Barcelo
References
- Abbas A.M., Fathy S.K., Khamees A.A., Salem A.S., Ahmed L. A focused review on the genital and sexual affection of COVID-19 patients. J. Gynecol. Obstet. Hum. Reprod. 2020;30:101848. doi: 10.1016/j.jogoh.2020.101848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adelodun B., Odedishemi F., Gbemisola R., Olalekan H., Choi K. Snowballing transmission of COVID-19 ( SARS-CoV-2 ) through wastewater : any sustainable preventive measures to curtail the scourge in low-income countries ? Sci. Total Environ. 2020;742:140680. doi: 10.1016/j.scitotenv.2020.140680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed W., Angel N., Edson J., Bibby K., Bivins A., Brien J.W.O., Choi P.M., Kitajima M., Simpson S.L., Li J., Tsharke B., Verhagen R., Smith W.J.M., Zaugg J., Dierens L., Hugheholtz P., Thomas K.V., Mueller J.F. First confirmed detection of SARS-CoV-2 in untreated wastewater in Australia: a proof of concept for the wastewatersurveillance of COVID-19 in the community. Sci. Total Environ. 2020;728:138764. doi: 10.1016/j.scitotenv.2020.138764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexyuk M.S., Turmagambetova A.S., Alexyuk P.G., Bogoyavlenskiy A.P., Berezin V.E. Comparative study of viromes from freshwater samples of the Ile-Balkhash region of Kazakhstan captured through metagenomic analysis. VirusDisease. 2017;28:18–25. doi: 10.1007/s13337-016-0353-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arslan M., Xu B., El-din M.G. Transmission of SARS-CoV-2 via fecal-oral and aerosols – borne routes : environmental dynamics and implications for wastewater management in underprivileged societies. Sci. Total Environ. 2020;743:140709. doi: 10.1016/j.scitotenv.2020.140709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Backshi S., He Z., L., Harris W., G. Natural nanoparticles: implications for environment and human health. Crit. Rev. Environ. Sci. Technol. 2015;44:861–904. doi: 10.1080/10643389.2014.921975. [DOI] [Google Scholar]
- Bandala E.R., Berli M. Engineered nanomaterials (ENMs) and their role at the nexus of food, energy, and water. Mater. Sci. Energy Technol. 2019;2:29–40. doi: 10.1016/j.mset.2018.09.004. [DOI] [Google Scholar]
- Bandala E.R., Rodriguez-Narvaez O.M. On the nature of hydrodynamic cavitation process and its application for the removal of water pollutants. Air, Soil Water Res. 2019;12:1–6. doi: 10.1177/1178622119880488. [DOI] [Google Scholar]
- Barcelo D. An environmental and health perspective for COVID-19 outbreak: meteorology and air quality influence, sewage epidemiology indicator, hospitals disinfection, drug therapies and recommendations. J. Environ. Chem. Eng. 2020;8:104006. doi: 10.1016/j/jece.2020.104006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bensalah N., Midassi S., Ahmad M.I., Bedoui A. Degradation of hydroxychloroquine by electrochemical advanced oxidation processes. Chem. Eng. J. 2020;402:126279. doi: 10.1016/j.cej.2020.126279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhowmick G.D., Dhar D. Coronavirus disease 2019 (COVID-19) outbreak : some serious consequences with urban and rural water cycle. Clean Water. 2019;3:1–8. doi: 10.1038/s41545-020-0079-1. [DOI] [Google Scholar]
- Blanchet G., Libohova Z., Joost S., Rossier N., Schneider A., Jeangros B., Sinaj S. Spatial variability of potassium in agricultural soils of the canton of Fribourg, Switzerland. Geoderma. 2017;290:107–121. doi: 10.1016/j.geoderma.2016.12.002. [DOI] [Google Scholar]
- Blanco A., Abid I., Al-Otaibi N., Perez-Rodriguez F.J., Fuentes C., Guix S., Pinto R.M., Bosch A. Glass wool concentration optimization for the detection of enveloped and non-enveloped waterborne viruses. Food Environ. Virol. 2019;11:184–192. doi: 10.1007/s12560-019-09378-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bofill-Mas S., Rusinol M. Recent trends on methods for the concentration of viruses from water samples. Curr. Opin. Environ. Sci. Heal. 2020;16:7–13. doi: 10.1016/j.coesh.2020.01.006. [DOI] [Google Scholar]
- Bogler A., Packman A., Furman A., Gross A., Kushmaro A., Ronen A., Hill C., Vaizel-Ohayon D., Morghenroth E. Rethinking wastewater risks and monitoring in light of the COVID-19 pandemic. Nat. Sustain. 2020;1–10 doi: 10.1038/s41893-020-00605-2. [DOI] [Google Scholar]
- Cadnum J.L., Li D.F., Jones L.D., Redmond S.N., Pearlmutter B., Wilson B.M., Donskey C.J. Evaluation of ultraviolet-C light for rapid decontamination of airport security bins in the era of SARS-CoV-2. Pathog. Immun. 2020;5:133. doi: 10.20411/pai.v5i1.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cahill N., Morris D. Recreational waters – a potential transmission route for SARS-CoV-2 to humans ? Sci. Total Environ. 2020;740:140122. doi: 10.1016/j.scitotenv.2020.140122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carducci A., Federigi I., Liu D., Thompson J.R., Verani M. Making Waves: coronavirus detection , presence and persistence in the water environment: state of the art and knowledge needs for public health. Water Res. 2020;179:115907. doi: 10.1016/j.watres.2020.115907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carraturo F., Del Giudice C., Morelli M., Cerullo V., Libralato G., Galdiero E., Guida M. Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. Environ. Pollut. 2020;265:115010. doi: 10.1016/j.envpol.2020.115010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cesarino I., Cincorro F.H., Machado S.A.S. A synergistic combination of reduced graphene oxide and antimony nanoparticles for estriol hormone detection. Sensors Actuators B Chem. 2015;210:453–459. doi: 10.1016/j.snb.2015.01.013. [DOI] [Google Scholar]
- Chandra P. Miniaturized label-free smartphone assisted electrochemical sensing approach for personalized COVID-19 diagnosis. Sensors Int. 2020;1:100019. doi: 10.1016/j.sintl.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra P. Miniaturized label-free smartphone assisted electrochemical sensingapproach for personalized COVID-19 diagnosis. Sensors Int. 2020;1:100019. doi: 10.1016/j.sintl.2020.100019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y., Hsueh Y., Hsieh C., Tzou D., Chang P. Antiviral activity of graphene – silver nanocomposites against non-enveloped and enveloped viruses. Int. J. Environ. Res. Public Health. 2016;13:430. doi: 10.3390/ijerph13040430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen R., Xue X., Liu L., Wang J.Y.L., Shen Z., Zhang T., Zheng X. Removal of waterborne pathogen by nanomaterial-membrane coupling system. J. Nanosci. Nanotechnol. 2017;18:1027–1033. doi: 10.1166/jnn.2018.13963. [DOI] [PubMed] [Google Scholar]
- Cheung K.S., Hung I.F.N., Chan P.P.Y., Lung K.C., Tso E., Liu R., Ng Y.Y., Chu M.Y., Chung T.W.H., Tam A.R., Yip C.C.Y., Leung K., Yim-Fong A., Zhang R.R., Lin Y., Cheng H.M., Zhang A.J.X., To, K.K.W, Leung W.K. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology. 2020;159:81–95. doi: 10.1053/j.gastro.2020.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury A.D., Takemura K., Li T., Suzuki T., Park E.Y. Electrical pulse-induced electrochemical biosensorfor hepatitis E virus detection. Nat. Commun. 2019;10:3737. doi: 10.1038/s41467-019-11644-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu W., Fang C., Deng Y., Xu Z. Intensified disinfection amid COVID-19 pandemic poses potential risks to water quality and safety. Environ. Sci. Technol. 2020 doi: 10.1021/acs.est.0c04394. In press. [DOI] [PubMed] [Google Scholar]
- Chung J.W., Foppen J.W., Gerner G., Krebs R., Lens P.N.L. Removal of rotavirus and adenovirus from artificial ground water using hydrochar derived from sewage sludge. J. Appl. Microbiol. 2015;119:876–884. doi: 10.1111/jam.12863. [DOI] [PubMed] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729:138474. doi: 10.1016/j.scitotenv.2020.139631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collivignarelli M.C., Collivignarelli C., Miino M.C., Abba A., Pedrazzani R., Bertanza G. SARS-CoV-2 in sewer systems and connected facilities. Process. Saf. Environ. Prot. 2020;143:196–203. doi: 10.1016/j.psep.2020.06.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colson P., Rolain J.M., Lagier J.C., Brouqui P., Raoult D. Chloroquine and hydroxychloquine as viable weapons to fight COVID-19. Int. J. Antimicrob. Agents. 2020;4:105932. doi: 10.1016/j.ijantimicag.2020.105932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costa-Rama E., Nouws H.P.A., Delerue-Matos C., Blanco-Lopez M.C., Fernandez-Abedul M.T. In: Frontiers in Water-Energy-Nexus-Nature-Based Solutions. Naddeo V., Balakrishna M., Choo K.H., editors. Springer; Cham: 2020. Electrochemical sensors for emerging contaminants: Diclofenac preconcentration and detection on paper-based electrodes; p. 56. [DOI] [Google Scholar]
- Cuevas-Ferrando E., Perez-Cataluna A., Allende A., Guix S., Randazzo W., Sanchez G. Recovering coronavirus from large volumes of water. Sci. Total Environ. 2020 doi: 10.1016/jscitontenv.2020.143101. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Da Silva M.K.L., Simoes R.P., Cesarino I. Evaluation of reduced graphene oxide modified with antimony and copper nanparticles for levofloxacin oxidation. Electroanalysis. 2018;30:2066–2076. doi: 10.1002/elan.201800265. [DOI] [Google Scholar]
- Daughton C.G. Wastewater surveillance for population-wide Covid-19: the present and future. Sci. Total Environ. 2020;736:139631. doi: 10.1016/j.scitotenv.2020.139631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong L., Hu S., Gao J. Discovering drugs to treat coronavirus disease 2019 ( COVID-19) Drug Discov. Ther. 2020;14:58–60. doi: 10.5582/ddt.2020.01012. [DOI] [PubMed] [Google Scholar]
- Donini C.A., Silva M.K.L., Simoes R.F., Cesarino I. Reduced graphene oxide modified with silver nanoparticles for the electrochemical detection of estriol. J. Electroanal. Chem. 2018;809:67–73. doi: 10.1016/j.jelechem.2017.12.054. [DOI] [Google Scholar]
- Donini C.A., Silva M.K.L., Bronzato G.R., Leao A.L., Cesarino I. Evaluation of a biosensor based on reduced graphene oxide and glucose oxidase enzyme on the monitoring of second-generation ethanol production. J. Solid State Electrochem. 2020;24:2011–2018. doi: 10.1007/s10008-019-04471-7. [DOI] [Google Scholar]
- Feng Y., Marchal T., Sperry T., Yi H. Influence of wind and relative humidity on the social distancing effectiveness to prevent COVID-19 airborne transmission: a numerical study. J. Aerosol Sci. 2020;147:105585. doi: 10.1016/j.jaerosci.2020.105585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipić A., Primc G., Zaplotnik R., Mehle N., Gutierrez I. Cold atmospheric plasma as a novel method for inactivation of potato virus Y in water samples. Food Environ. Virol. 2019;11:220–228. doi: 10.1007/s12560-019-09388-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filipic A., Gutierrez-Aguirre I., Primc G., Mozeti M., Dobnik D. Cold plasma, a new hope in the field of virus inactivation. Trends Biotechnol. 2020 doi: 10.1016/j.tibtech.2020.04.003. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foladori P., Cutrupi F., Segata N., Manara S., Pinto F., Malpei F., Bruni L., La G. SARS-CoV-2 from faeces to wastewater treatment: what do we know? A review. Sci. Total Environ. 2020;743:140444. doi: 10.1016/j.scitotenv.2020.140444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia T., Boff L., Regina C., Barardi M., Nagl M. Inactivation of adenovirus in water by natural and synthetic compounds. Food Environ. Virol. 2019;11:157–166. doi: 10.1007/s12560-019-09370-8. [DOI] [PubMed] [Google Scholar]
- Garcia-Avila F., Valdiviezo-Gonzales L., Cadme-Galabay M., Gutierrez-Ortega H., Altamirano-Cardenas L., Zhidon-Arevalo C., Pinto L.F. Considerations on water quality and the use of chlorine in times of SARS-CoV-2 (COVID-19) pandemic in the community. Case Stud. Chem. Environ. Eng. 2020;2:100049. doi: 10.1016/j.cscee.2020.100049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Gil A., Martinez A., Polo-Lopez M.I., Marugan J. Kinetic modeling of the synergistic thermal and spectral actions on the inactivation of viruses in water by sunlight. Water Res. 2020;183:116074. doi: 10.1016/j.watres.2020.116074. [DOI] [PubMed] [Google Scholar]
- Gardea-Torresdey J.L., Rico C.M., White J.C. Trophic transfer, transformation, and impact of engineered Nanomaterials in terrestrial environments. Environ. Sci. Technol. 2014;48:2526–2540. doi: 10.1021/es4050665. [DOI] [PubMed] [Google Scholar]
- Gómez-López M.D.D., Bayo J., García-Cascales M.S.S., Angosto J.M.M. Decision support in disinfection technologies for treated wastewater reuse. J. Clean. Prod. 2009;17:1504–1511. doi: 10.1016/j.jclepro.2009.06.008. [DOI] [Google Scholar]
- Gonzalez R., Curtis K., Bivins A., Bibby K., Weir M.H., Yetka K., Thompson H., Keeling D., Mitchell J., Gonzalez D. COVID-19 surveillance in Southeastern Virginia using wastewater-based epidemiology. Water Res. 2020;186:116296. doi: 10.1016/j.watres.2020.116296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormley M., Aspray T.J., Kellya D.A. COVID-19: mitigating transmission via wastewater plumbing systems. Correspondence. 2020;8 doi: 10.1016/S2214-109X(20)30112-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grundy P.M., Gerba C.P., Pepper I.L. Survival of coronaviruses in water and wastewater. Food Environ. Virol. 2009;1:10. doi: 10.1007/s12560-008-9001-6. [DOI] [Google Scholar]
- Guedes-Alonso R., Montesdeoca-Esponda S., Herrera-Melián J.A., Rodríguez-Rodríguez R., Ojeda-González Z., Landívar-Andrade V., Sosa-Ferrera Z., Santana-Rodríguez J.J. Pharmaceutical and personal care product residues in a macrophyte pond-constructed wetland treating wastewater from a university campus: presence, removal and ecological risk assessment. Sci. Total Environ. 2020;703:135596. doi: 10.1016/J.SCITOTENV.2019.135596. [DOI] [PubMed] [Google Scholar]
- Haleem A., Javaid M., Vaishya R., Deshmukh S.G. Areas of academic research with the impact of COVID-19. Am. J. Emerg. Med. 2020;38:1524–1526. doi: 10.1016/j.ajem.2020.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallema D.W., Robinne F., Mcnulty S.G. Pandemic spotlight on urban water quality. Ecol. Process. 2020;9:20–22. doi: 10.1186/s13717-020-00231-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart O.E., Halden R.U. Computational analysis of SARS-CoV-2/COVID-19 surveillance by wastewater-based epidemiology locally and globally: feasibility, economy, opportunities and challenges. Sci. Total Environ. 2020;730:138875. doi: 10.1016/j.scitotenv.2020.138875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hata A., Honda R. Potential sensitivity of wastewater monitoring for SARS-CoV-2: comparison with norovirus cases. Environ. Sci. Technol. 2020;54:6451–6452. doi: 10.1021/acs.est.0c02271. [DOI] [PubMed] [Google Scholar]
- Heffron J., Ryan D.R., Mayer B.K. Sequential electrocoagulation-electrooxidation for virus mitigation in drinking water. Water Res. 2019;160:435–444. doi: 10.1016/j.watres.2019.05.078. [DOI] [PubMed] [Google Scholar]
- Hernández F., Calısto-Ulloa N., Gómez-Fuentes C., Gómez M., Ferrer J., González-Rocha G., Bello-Toledo H., Botero-Coy A.M., Boıx C., Ibáñez M., Montory M. Occurrence of antibiotics and bacterial resistance in wastewater and sea water from the Antarctic. J. Hazard. Mater. 2019;363:447–456. doi: 10.1016/J.JHAZMAT.2018.07.027. [DOI] [PubMed] [Google Scholar]
- Huesca-Espitia L.C., Aurioles-López V., Ramírez I., Sánchez-Salas J.L., Bandala E.R. Photocatalytic inactivation of highly resistant microorganisms in water: a kinetic approach. J. Photochem. Photobiol. A Chem. 2017;337:132–139. doi: 10.1016/j.jphotochem.2017.01.025. [DOI] [Google Scholar]
- Huraimel H.A., Slhosani M., Kunhbdulla S., Stietiya M.H. SARS-CoV-2 in the environment: modes of transmission, early detection and potential role of pollutants. Sci. Total Environ. Total. 2020;744:140946. doi: 10.1016/j.scitotenv.2020.140946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibarguen-Mondragon E., Revelo-Romo D., Hidalgo A., García H., Galeano L. Mathematical modelling of MS2 virus inactivation by Al / Fe-PILC-activated catalytic wet peroxide oxidation (CWPO) Environ. Sci. Pollut. Res. 2020;27:19836–19844. doi: 10.1007/s11356-020-08365-4. [DOI] [PubMed] [Google Scholar]
- Innocenzi P., Stagi L. Carbon-based antiviral nanomaterials: Graphene, C-dots, and fullerenes. A perspective. Chem. Sci. 2020;11:6606–6622. doi: 10.1039/D0SC02658A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M.Z.H., Hasan M.R., Hossain S.I., Ahommed M.S., Daizy M. Ultrasensitive detection of pathogenic viruses with electrochemical biosensor: state of the art. Biosens. Bioelectron. 2020;166:112431. doi: 10.1016/j.bios.2020.112431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitajima M., Ahmed W., Bibby K., Carducci A., Gerba C.P., Hamilton K.A., Haramoto E., Rose J.B. SARS-CoV-2 in wastewater : state of the knowledge and research needs. Sci. Total Environ. 2020;739:139076. doi: 10.1016/j.scitotenv.2020.139076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klemes K.J., Fan Y.V., Tan R.R., Jiang P. Minimising the present and future plastic waste, energy and environmental footprints related to COVID-19. Renew. Sust. Energ. Rev. 2020;127:109883. doi: 10.1016/j.rser.2020.109883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohori N.A., Da Silva M.K.L., Cesarino I. Evaluation of graphene oxide and reduced graphene oxide in the immobilization of laccase enzyme and its application in the determination of dopamine. J. Solid State Electrochem. 2018;22:141–148. doi: 10.1007/s10008-017-3738-5. [DOI] [Google Scholar]
- Kokkinos P., Mantzavinos D., Venieri D. Current trends in the application of nanomaterials for the removal of emerging micropollutants and. Molecules. 2020;25:2016. doi: 10.3390/molecules25092016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratzel A., Steiner S., Todt D., V’kovski P., Bruggemann Y., Steinmann E., Thiel V., Pfaender S. Temperature-dependent surface stability of SARS-CoV-2. J. Inf. Secur. 2020;81:453–482. doi: 10.1016/j.jinf.2020.05.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krzeminski P., Tomei M.C., Karaolia P., Langenhoff A., Almeida C.M.R., Felis E., Gritten F., Andersen H.R., Fernandes T., Manaia C.M., Rizzo L., Fatta-Kassinos D. Performance of secondary wastewater treatment methods for the removal of contaminants of emerging concern implicated in crop uptake and antibiotic resistance spread: a review. Sci. Total Environ. 2019;648:1052–1081. doi: 10.1016/j.scitotenv.2018.08.130. [DOI] [PubMed] [Google Scholar]
- Kupferschmidt K., Cohen J. Race to find COVID-19 treatments accelerates. Science (80-. ) 2020;367:6485. doi: 10.1126/science.367.6485.1412. [DOI] [PubMed] [Google Scholar]
- La Rosa G., Bonadonna L., Lucentini L., Kenmoe S., Suffredini E. Coronavirus in water environments : occurrence, persistence and concentration methods - a scoping review. Water Res. 2020;179:115899. doi: 10.1016/j.watres.2020.115899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Layqah L.A., Eissa S. An electrochemical immunosensor for the corona virus associated with the Middle East respiratory syndrome using an array of gold nanoparticle-modified carbon electrodes. Microchim. Acta. 2019;186:224. doi: 10.1007/s0064-019-3345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lesimple A., Jasim S.Y., Johnson D.J., Hilal N. The role of wastewater treatment plants as tools for SARS-CoV-2 early detection and removal. J. Water Process Eng. 2020;38:101544. doi: 10.1016/j.jwpe.2020.101544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lodder W., de Roda Husman A.M. SARS-CoV-2 in wastewater: potential health risk, but also data source. Lancet Gastroenterol. Hepatol. 2020;5:533–534. doi: 10.1016/S2468-1253(20)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzetti A.S., Sierra T., Domini C.E., Lista A.G., Crevillen A.G., Escarpa A. Electrochemically reduced graphene oxide-based screen-printed electrodes for total tetracycline determination by adsorptive transfer stripping differential pulse voltammetry. Sensors. 2020;20:76. doi: 10.3390/s20010076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu D., Huang Z., Luo J., Zhang X., Sha S. Primary concentration – the critical step in implementing the wastewater based epidemiology for the COVID-19 pandemic: a mini-review. Sci. Total Environ. 2020;747:141245. doi: 10.1016/j.scitotenv.2020.141245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahari S., Roberts A., Shahdeo D., Gandhi S. eCovSens-ultrasensitive novel in house built printed circuit board based electrochemical device for rapid detection of nCovid-19. bioRxiv. 2020 doi: 10.1101/2020.04.24.059204. [DOI] [Google Scholar]
- Mandal I., Pal S. COVID-19 pandemic persuaded lockdown effects on environment over stone quarrying and crushing areas. Sci. Total Environ. 2020;732:139281. doi: 10.1016/j.scitotenv.2020.139281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao K., Zhang K., Du W., Ali W., Feng X., Zhang H. The potential of wastewater-based epidemiology as surveillance and early warning of infectious disease outbreaks. Curr. Opin. Environ. Sci. Heal. 2020;17:1–7. doi: 10.1016/jcoesh.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez-Piernas A., Plaza-Bolaños P., Fernández-Ibáñez P., Agüera A. Organic microcontaminants in tomato crops irrigated with reclaimed water grown under field conditions: occurrence, uptake, and health risk assessment. J. Agric. Food Chem. 2019;67:6930–6939. doi: 10.1021/acs.jafc.9b01656. [DOI] [PubMed] [Google Scholar]
- Medema G., Heijnen L., Elsinga G., Italiaander R., Brouwer A. Presence of SARS-coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. 2020;7(7):511–516. doi: 10.1021/acs.estlett.0c00357. [DOI] [PubMed] [Google Scholar]
- Medrano-Rodríguez F., Picos-benítez A., Brillas E., Bandala E.R. Electrochemical advanced oxidation discoloration and removal of three brown diazo dyes used in the tannery industry. J. Electroanal. Chem. 2020;873:114360. doi: 10.1016/j.jelechem.2020.114360. [DOI] [Google Scholar]
- Meng X., Huang X., Zhou P., Li C., Wu A. Alert for SARS-CoV-2 infection caused by fecal aerosols in rural areas in China. Infect. Control Hosp. Epidemiol. 2020;41:987. doi: 10.1017/ice.2020.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittal R., Ni R., Seo J.H. The flow physics of COVID-19. J. Fluid Mech. 2020;894:F2. doi: 10.1017/jfm.2020.330. [DOI] [Google Scholar]
- Muhammad S., Long X., Salman M. COVID-19 pandemic and environmental pollution: a blessing in disguise ? Sci. Total Environ. 2020;728:138820. doi: 10.1016/j.scitotenv.2020.138820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musmarra D., Prisciandaro M., Capocelli M., Karatza D., Iovino P., Canzano S., Lancia A. Degradation of ibuprofen by hydrodynamic cavitation: reaction pathways and effect of operational parameters. Ultrason. Sonochem. 2016;29:76–83. doi: 10.1016/j.ultsonch.2015.09.002. [DOI] [PubMed] [Google Scholar]
- Naddeo V. Editorial perspectives : 2019 novel coronavirus. Environ. Sci. Water Res. Technol. 2020;6:1213–1216. doi: 10.1039/d0ew90015j. [DOI] [Google Scholar]
- Nag P., Sadani K., Mukherji S. Optical fiber sensors for rapid screening of COVID-19. Transactions Indian Natl. Acad. Eng. 2020;5:233–236. doi: 10.1007/s41403-020-00128-4. (doi:1.1007/s41403-00128-4) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemudryi A., Nemudraia A., Wiegand T., Surya K., Buyukyoruk M., Cicha C., Vandewood K.K., Wilkinson R., Wiedenheft B. Temporal detection and phylogenetic assessment of SARS-CoV-2 in municipal wastewater. Cell Reports Med. 2020 doi: 10.1016/jxcrm.2020.100098. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nwobodo T., Chukwu K. COVID-19 era and watter supply: challenges for rural communities in eastern Nigeria. J. Geosci. Environ. Prot. 2020;8:219–233. doi: 10.4236/gep.2020.87013. [DOI] [Google Scholar]
- Oidtmann B., Dixon P., Way K., Joiner C., Bayley A.E. Risk of waterborne virus spread–review of survival of relevant fish and crustacean viruses in the aquatic environment and implications for control measures. Rev. Aquac. 2017;10:641–669. doi: 10.1111/raq.12192. [DOI] [Google Scholar]
- Ortiz-Prado E., Simbana-Rivera K., Gomez-Barreno L., Rubio-Neira M., Guaman L.P., Kyriakidis N.C., Muslin C., Jaramillo A.M.G., Barba-Ostria C., Cevallos-Robalino D., Sanchez-SanMiguel H., Unigarro L., Zalakeviciute R., Gadian N., Lopez-Cortes A. Clinical, molecular and epidemiological characterization of the SARS-CoV2 virus and the coronavirus disease 2019 (COVID-19), a comprehensive literature review. Diagn. Microbiol. Infect. Dis. 2020;98:115094. doi: 10.1016/j.diagmicrobio.2020.115094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmieri V., Papi M. Can graphene take part in the fight against COVID-19? Nano Today. 2020;33:100883. doi: 10.1016/j.nntod.2020.100883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prata D.N., Rodrigues W., Bermejo P.H. Temperature significantly changes COVID-19 transmission in (sub)tropical cities of Brazil. Sci. Total Environ. 2020;729:138862. doi: 10.1016/j.scitotenv.2020.138862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulido C.M., Villarejo-carballido B., Redondo-sama G. COVID-19 infodemic : more retweets for science-based information on coronavirus than for false information. Int. Sociol. 2020;35:377–392. doi: 10.1177/0268580920914755. [DOI] [Google Scholar]
- Qian L., Thiruppathi A.R., Elmahdy R., van der Zalm J., Chen A. Graphene-oxide-based electrochemical sensors for the sensitive detection of pharmaceutical drug naproxen. Sensors (Switzerland) 2020;20:1252. doi: 10.3390/s20051252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rachmadi A.T., Kitajima M., Kato T., Kato H., Okabe S., Sano D. Required chlorination doses to fulfill the credit value for disinfection of enteric viruses in water : a critical review. Environ. Sci. Technol. 2020;54:2068–2077. doi: 10.1021/acs.est.9b01685. [DOI] [PubMed] [Google Scholar]
- Randazzo W., Truchado P., Cuevas-Ferrando E., Simon P., Allende A., Sanchez G. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. Water Res. 2020;181:115942. doi: 10.1016/j.watres.2020.115942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis E.O., Foureaux A.F.S., Rodrigues J.S., Moreira V.R., Lebron Y.A.R., Santos L.V.S., Amaral M.C.S., Lange L.C. Occurrence, removal and seasonal variation of pharmaceuticals in Brasilian drinking water treatment plants. Environ. Pollut. 2019;250:773–781. doi: 10.1016/J.ENVPOL.2019.04.102. [DOI] [PubMed] [Google Scholar]
- Rimolldi S.G., Stefani F., Gigantiello A., Polesello S., Comandatore F., Mileto D., Maresca M., Longobardi C., Mancon A., Romeri F., Pagani C., Cappelli F., Rosconi C., Moja L., Gismondo M.R., Salerno F. Presence and infectivity of SARS-CoV-2 virus in wastewaters and rivers. Sci. Total Environ. 2020;744:140911. doi: 10.1016/j.scitotenv.2020.140911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rocha G.S., Silva M.K.L., Cesarino I. Reduced graphene oxide-based impedimetric immunosensor for detection of enterotoxin A in milk samples. Materials (Basel) 2020;13:1751. doi: 10.3390/ma13071751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez-Narvaez O.M., Peralta-Hernandez J.M., Goonetilleke A., Bandala E.R. Treatment technologies for emerging contaminants in water: a review. Chem. Eng. J. 2017;323:361–380. doi: 10.1016/j.cej.2017.04.106. [DOI] [Google Scholar]
- Rodríguez-Narvaez O.M., Rajapaksha R.D., Ranasinghe M.I., Bai X., Peralta-hernández J.M., Bandala E.R. Peroxymonosulfate decomposition by homogeneous and heterogeneous co : kinetics and application for the degradation of acetaminophen. J. Environ. Sci. 2020;93:30–40. doi: 10.1016/j.jes.2020.03.002. [DOI] [PubMed] [Google Scholar]
- Saadat S., Rawtani D., Mustansar C. Environmental perspective of COVID-19. Sci. Total Environ. 2020;728:138870. doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saka C. Analytical methods on determination in pharmaceuticals and biological materials of Chloroquine as available for the treatment of COVID-19. Crit. Rev. Anal. Chem. 2020 doi: 10.1080/10408347.2020.1781592. [DOI] [PubMed] [Google Scholar]
- Sanchis A.G., Pashley R., Ninham B. Virus and bacteria inactivation by CO 2 bubbles in solution. Clean Water. 2019;2:1–9. doi: 10.1038/s41545-018-0027-5. [DOI] [Google Scholar]
- Setznagl S., Cesarino I. Copper nanoparticles and reduced graphene oxide modified a glassy carbon electrode for the determination of glyphosate in water samples. Int. J. Environ. Anal. Chem. 2020 doi: 10.1080/03067319.2020.1720667. [DOI] [Google Scholar]
- Sharma S., Zhang M., Gao J., Zhang H., Harsha S. Effect of restricted emissions during COVID-19 on air quality in India. Sci. Total Environ. 2020;728:138878. doi: 10.1016/j.scitotenv.2020.138878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sportelli M.C., Izzi M., Kukushkina E.A., Hossain S.I., Picca R.A., Ditaranto N., Cio N. Can nanotechnology and materials science help the fight against SARS-CoV-2 ? Nanomaterials. 2020;19:1–12. doi: 10.3390/nano10040802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Street R., Malema S., Mahlangeni N., Mathee A. Wastewater surveillance for Covid-19: an African perspective. Sci. Total Environ. 2020;743:140719. doi: 10.1016/j.scitotenv.2020.140719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tymm C., Zhou J., Tadimety A., Burklund A., Zhang J.X.J. Scalable COVID-19 detection enabled by lab-on-chip biosensors. Cell. Mol. Bioeng. 2020 doi: 10.1007/s12195-020-00642-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usman M., Farooq M., Hanna K. Existence of SARS-CoV-2 in wastewater: Implications for its environmental transmission in developing countries. Environ. Sci. Technol. 2020;54:7758–7759. doi: 10.1021/acs.est.0c02777. [DOI] [PubMed] [Google Scholar]
- Venugopal A., Ganesan H., Raja S.S., Govindasamy V., Arunachalam M., Narayanasamy A., Sivaprakash P., Rahman P.K.S.M., Gopalakrishnan A.V., Siama Z., Velligiri B. Novel wastewater surveillance strategy for early detection of coronavirus disease 2019 hotspots. Curr. Opin. Environ. Sci. Heal. 2019;17:8–13. doi: 10.1016/j.coesh.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Su M. A preliminary assessment of the impact of COVID-19 on environment – a case study of China. Sci. Total Environ. 2020;728:138915. doi: 10.1016/j.scitotenv.2020.138915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X., Li J.S., Guo T.K., Zhen B., Kong Q.X., Yi B., Li Z., Song N., Jin M., Xiao W.J., Zhu X.M., Gu C.Q., Yin J., Wei W., Yao W., Liu C., Li J.F., Ou G.R., Wang M.N., Fang T.Y., Wang G.J., Qiu Y.H., Wu H.H., Chao F.H., Li J.W. Concentration and detection of SARS coronavirus in sewage from Xiao Tang Shan Hospital and the 309th hos-pital. J. Virol. Methods. 2005;128:156–161. doi: 10.1016/j.jviromet.2005.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang J., Tian Z., Huo Y., Yang M., Zheng X., Zhang Y. Monitoring of 943 organic micropollutants in wastewater from municipal wastewater treatment plants with secondary and advanced treatment processes. J. Environ. Sci. (China) 2018;67:309–317. doi: 10.1016/j.jes.2017.09.014. [DOI] [PubMed] [Google Scholar]
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020;323:1834–1844. doi: 10.1001/jama.2020.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wati S., Robinson B.S., Mieog J., Blackbeard J., Keegan A.R. Chlorine inactivation of coxsackievirus B5 in recycled water destined for non-potable reuse. Water Heal. 2019;17:124–136. doi: 10.2166/wh.2018.393. [DOI] [PubMed] [Google Scholar]
- Wong M.V.M., Hashsham S.A., Gulari E., Rouillard J.M., Aw T.G., Rose J.B. Detection and characterization of human pathogenic viruses circulating in communitywastewater using multi target microarrays and polymerase chain reaction. J. Water Health. 2013;11:659–670. doi: 10.2166/wh.2013.322. [DOI] [PubMed] [Google Scholar]
- Wu Y., Guo C., Tang L. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Gastroenteology Hepatol. 2020;5:434–435. doi: 10.1016/S2468-1253(20)30083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L., Liu C., Yang C. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WWP . 2017. The United Nations World Water Development Report 2017-Wastewater: The Untapped Resource. (Paris) [Google Scholar]
- Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Li, Zhu B., Liang H., Fang C., Gong Y., Guo Q., Sun X., Zhao D., Shen J., Zhang H., Liu H., Xia H., Tang J., Zhang K., Gong S. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat. Med. 2020;26:502–505. doi: 10.1038/s41591-020-0817-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Shi, Wang Y., Zhang J., Huang L., Zhang C., Liu S., Zhao P., Liu H., Zhu L., Tai Y., Bai C., Gao T., Song J., Xia P., Dong J., Zhao J., Wang F. Pathological findings of COVID-19 associate with accurate respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. (doi:10.16/S2213-2600(20)30076-X) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H., Xie W., Xue X., Yang K., Ma J., Liang W., Zhao Q., Zhou Z., Pei D., Ziebuhr J., Hilgenfeld R., Yuen K.Y., Wong L., Gao G., Chen S., Chen Z., Ma D., Bartlam M., Rao Z. Design of wide-spectrum inhibitors targeting coronavirus main proteases. PLoS Biol. 2005;3 doi: 10.1371/journal.pbio.0030324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo C., Kaushal S., Yeo D. Enteric involvement of coronaviruses: is faecal–oral transmission of SARS-CoV-2 possible? Lancet Gastroenterol. Hepatol. 2020;5:335–337. doi: 10.1016/S2468-1253(20)30048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan Q.-B., Zhai Y.-F., Mao B.-Y., Hu N. Antibiotic resistance genes and intI1 prevalence in a swine wastewater treatment plant and correlation with metal resistance, bacterial community and wastewater parameters. Ecotoxicol. Environ. Saf. 2018;161:251–259. doi: 10.1016/J.ECOENV.2018.05.049. [DOI] [PubMed] [Google Scholar]
- Yueling M., Yadong Z., Jiangtao L., Xiaotao H., Bo W., Shihua F., Jun Y., Jingping N., Ji Z., Bin L. Effects of temperature variation and humidity on the death of COVID-19 in Wuhan, China. Sci. Total Environ. 2020;724:138226. doi: 10.1016/j.scitotenv.2020.138226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yunus A.P., Masago Y., Hijioka Y. COVID-19 and surface water quality : improved lake water quality during the lockdown. Sci. Total Environ. 2020;731:139012. doi: 10.1016/j.scitotenv.2020.139012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaied B.K., Rashid M., Nasrullah M., Zularisam A.W., Pant D., Singh L. A comprehensive review on contaminants removal from pharmaceutical wastewater by electrocoagulation process. Sci. Total Environ. 2020;726:138095. doi: 10.1016/j.scitotenv.2020.138095. [DOI] [PubMed] [Google Scholar]
- Zambrano-Monserrate M.A., Alejandra M., Sanchez-alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020;728:138813. doi: 10.1016/j.scitotenv.2020.138813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeidman A., Rodriguez-Narvaez O.M., Moon J., Bandala E.R. Removal of antibiotics in aqueous phase using silica-based immobilized nanomaterials: a review. Environ. Technol. Innov. 2020;20:101030. doi: 10.1016/j.eti.2020.101030. [DOI] [Google Scholar]
- Zhang C., Xu L., Xu P., Wang X.C. Elimination of viruses from domestic wastewater : requirements and technologies. World J. Microbiol. Biotechnol. 2018;32:69. doi: 10.1007/s11274-016-2018-3. [DOI] [PubMed] [Google Scholar]
- Zhang H., He H., Chen S., Huang T., Lu K., Zhang Z., Wang R., Zhang X., Li H. Abundance of antibiotic resistance genes and their association with bacterial communities in activated sludge of wastewater treatment plants: geographical distribution and network analysis. J. Environ. Sci. 2019;82:24–38. doi: 10.1016/J.JES.2019.02.023. [DOI] [PubMed] [Google Scholar]
- Zhang L., Luo Y., Wang W., Sun Y., Zhang J., Fatima M., Jia X., Qiu H. Efficient inactivation of African swine fever virus by ozonized water. Vet. Microbiol. 2020 doi: 10.1016/j.vetmic.2020.108796. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Ling, Huang X., Li J., Li W., Yi C., Zhang T., Jiang Y., He Y., Deng S., Zhang X., Wang X., Liu Y., Li G., Qu J. Potential spreading risks and disinfection challenges of medical wastewater by the presence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) viral RNA in septic tanks of Fangcang Hospital. Sci. Total Environ. 2020;741:140445. doi: 10.1016/j.scitotenv.2020.140445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Lardizabal A., Silverman A.I., Vione D., Kohn T., Nguyen T.H., Guest J.S. Global sensitivity analysis of environmental, water quality, photoreactivity, and engineering design parameters in sunlight inactivation of viruses. Environ. Sci. Technol. 2020;54:8401–8410. doi: 10.1021/acs.est.0c01214. [DOI] [PubMed] [Google Scholar]
- Zhao R., Coles N., Kong Z., Wu J. Effect of aged and fresh biochars in soil acidity under different incubation conditions. Soil Tillage Res. 2015;146:133–138. doi: 10.1016/j.still.2014.10.014. [DOI] [Google Scholar]
- Zhao H., Liu F., Xie W., Zhou T., Yang J.O., Jin L., Li H., Zhao C., Zhang L., Wei J., Zhang Y., Li C. Ultrasensitive supersandwich-type electrochemical sensor for SARS-CoV-2 from the infected COVID-19 patients using a smartphone. Sensors Actuators B Chem. 2021;15:128899. doi: 10.1016/j.snb.2020.128899. [DOI] [PMC free article] [PubMed] [Google Scholar]