Abstract
Background
Interscalene brachial plexus block (ISBPB) is commonly used with general anesthesia for postoperative pain management in shoulder surgery. This study investigated the incidence of hypothermia and changes in the body temperature in patients undergoing arthroscopic shoulder surgery under ISBPB with propofol sedation.
Methods
This retrospective study enrolled 220 patients who underwent arthroscopic shoulder surgery. Patients were divided into general anesthesia (n = 34) and ISBPB with propofol sedation (n = 186) groups, and medical records were retrospectively compared. In addition, patients from the ISBPB group were further divided according to age (elderly [≥ 65 years], n = 98 vs. young [< 65 years], n = 88), and the incidence of hypothermia and changes in the body temperature were compared.
Results
Twenty-seven patients (12.3%) experienced perioperative hypothermia (range: 35.3–35.9℃). The incidence of perioperative hypothermia was 29.4% and 9.1% in the general anesthesia and ISBPB groups, respectively, and there was a significant difference between the two groups (P = 0.002). The incidence of perioperative hypothermia according to age in the ISBPB group was 9.2% and 9.1% in the elderly and young groups, respectively, and there was no significant difference between the two groups (P = 0.983).
Conclusions
The incidence of perioperative hypothermia during arthroscopic shoulder surgery under ISBPB with propofol sedation is lower than that under general anesthesia. Furthermore, when using ISBPB with propofol sedation, the incidence of perioperative hypothermia in elderly patients is similar to that in younger patients.
Keywords: Arthroscopy, Body temperature, Brachial plexus block, Interscalene, Sedation, Shoulder
Introduction
Inadvertent perioperative hypothermia (core body temperature < 36℃), caused by impairment of thermoregulation due to anesthesia and a low operating room temperature, occurs frequently during surgery. It also occurs in patients undergoing arthroscopic shoulder surgery because this is commonly performed under general anesthesia, and a large amount of cold irrigation fluid is used at relatively high pressures to ensure visibility of the operative field [1,2]. Despite mild body temperature decreases of approximately 1–2˚C, perioperative hypothermia can lead to various complications, including serious cardiovascular problems and increased risk of bleeding [3–7].
Various methods have been reported to prevent hypothermia during an arthroscopic shoulder surgery [1,2,8–13], and only few studies assessing interscalene brachial plexus block (ISBPB), which is widely used for postoperative pain control in shoulder surgery, have been reported [8–10]. A previous study reported that preoperative ISBPB can be useful in preventing hypothermia by reducing the amount of volatile anesthetics in patients undergoing arthroscopic shoulder surgery under general anesthesia [8]. However, other studies have reported that hypothermia occurs more frequently in elderly patients or when active warming is not performed despite using preoperative ISBPB with general anesthesia [9,10]. As such, the effect of ISBPB on preventing perioperative hypothermia is not clear. In addition, ISBPB was used as a supplement to general anesthesia in these studies, and the role of ISBPB is to reduce the thermoregulatory impairment caused by general anesthesia. There is no previous study comparing the effects of ISBPB and general anesthesia on hypothermia. ISBPB is used as the main anesthetic method for arthroscopic shoulder surgery with propofol sedation in our hospital. Therefore, the present retrospective study aimed to evaluate the incidence of perioperative hypothermia and changes in body temperature when ISBPB with propofol sedation was used as the primary anesthetic modality during arthroscopic shoulder surgery.
Materials and Methods
Study sample
The present study was approved by the Institutional Review Board of Presbyterian Medical Center, Jeonju, Korea (PMCIRB 2020-03-007) and registered at the Clinical Research Information Service (Ref: KCT0004918). The clinical research was done following the ethical principles for medical research involving human subjects in accordance with the Helsinki Declaration 2013. The present study was included 245 patients who underwent arthroscopic shoulder surgery between September 1, 2018, and February 29, 2020. Patients who were converted to general anesthesia due to incomplete ISBPB (n = 4), converted from arthroscopic to open surgery (n = 7), and those who underwent sedation using other sedatives without propofol (n = 14) were excluded (Fig. 1). The 220 patients were enrolled and divided into the general anesthesia group (Group GA, n = 34) and the ISBPB with propofol sedation group (Group ISBPB, n = 186). In addition, differences according to age (elderly patients ≥ 65 years, younger patients < 65 years) were compared in patients from the ISBPB group.
Fig. 1.
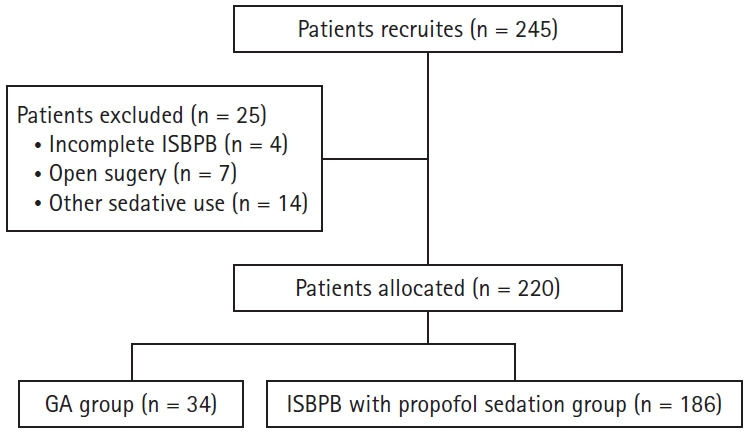
Flowchart of patient allocation. ISBPB: interscalene brachial plexus block, GA: general anesthesia.
Methods
Data were retrospectively collected and analyzed using anesthetic and post-anesthetic care unit (PACU) records. All patients were monitored by noninvasive blood pressure measurements, electrocardiogram (ECG), and pulse oximetry. However, no premedication and pre-warming were performed before anesthesia.
As for the anesthetic method, ISBPB was performed except 1) when the patient wanted general anesthesia, 2) in patients who had a tendency of bleeding or who were taking anticoagulants, 3) when ISBPB was difficult to perform due to abnormal findings such as infection of the area where the nerve block was performed.
General anesthesia was induced with propofol, remifentanil, and rocuronium, and maintained with inhalation anesthetics using desflurane (or sevoflurane) and 50% oxygen-air mixture. Body temperature was measured with an esophageal stethoscope with temperature sensor (DeRoyal®, DeRoyal Industries Inc., USA).
ISBPB was performed by the anesthesiologist under ultrasound and nerve stimulator guidance with an in-plane technique using a mixture of 0.75% ropivacaine and 2% lidocaine. The pin-prick test was used to assess the adequacy of the nerve block, and propofol was administered with a target-controlled infusion pump to achieve appropriate sedation (Modified observer’s alertness/sedation [MOAA/S] score 1–3). The body temperature was measured on the side contralateral to the surgical area using a tympanic thermometer (ThermoScan IRT 4520, Braun, Germany). While supplying oxygen via a facial mask, respiration was continuously monitored during surgery by end tidal CO2 and ECG. The oral airway was used when the upper airway was obstructed.
All patients underwent surgery in the beach-chair position by the same orthopedic surgeon. During the surgery, passive warming using a cotton blanket was performed, and active warming was performed using a forced-air warming device (WarmTouchTM 6000, Covidien, USA) placed on the knee area of the patient in both groups. In addition, humidified and heated respiratory circuit was used in the general anesthesia group. A three-liter normal saline bag, which was stored at room temperature, was used as the irrigation fluid.
Body temperature investigated was measured over time as follows: in the ward before leaving to the operating room (baseline); on arrival to the operating room; in 15 min intervals until the end of anesthesia; and on admission to the PACU. Changes in body temperature and the incidence of perioperative hypothermia (the lowest temperature) were examined and compared between the two groups. The severity of hypothermia was classified into Mild (35.5–35.9℃), Moderate (35.0–35.4℃), and Profound (< 35.0℃).
Statistical analysis
Statistical analysis was performed using SPSS ver. 23 (IBM Corp., USA), and patient characteristics are expressed as mean ± standard deviation (SD). Categorical data were analyzed using the chi-squared test or Fisher’s exact test. In addition, a logistic regression analysis adjusted with propensity score was performed to assess the correlation between the type of anesthesia and incidence of hypothermia. A P value < 0.05 was considered to be statistically significant.
Results
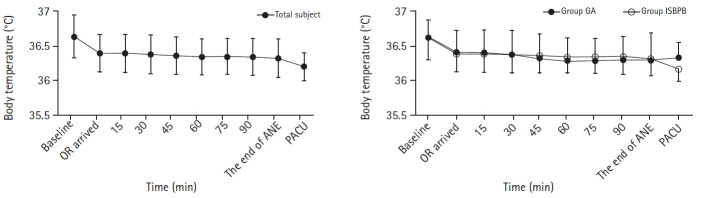
The present study included 220 patients (108 female, 112 male) with a mean ± SD age of 63.5 ± 11.1 years. There were no significant differences in demographic and perioperative data except sex (P = 0.013) between Group GA and Group ISBPB (Table 1). Body temperature on arrival to the operating room were 36.4 ± 0.3˚C in both groups and gradually decreased over time in Group GA and Group ISBPB, but there was no significant difference between the two groups (Fig. 2). Overall, perioperative hypothermia occurred in 27 (12.3%) patients, with the body temperature ranging between 35.3˚C and 35.9˚C and all cases occurred during the intraoperative period. The incidence of hypothermia was 29.4% and 9.1% in Group GA and Group ISBPB, respectively, and a significant relevance was found between perioperative hypothermia and the anesthetic method used (P = 0.002, odds ratio: 0.172, 95% CI: 0.057, 0.517). Two patients with perioperative hypothermia in Group GA experienced moderate hypothermia (Table 2).
Table 1.
Patient Demographic and Perioperative Data
| Variable | Group GA | Group ISBPB |
P value |
P value |
||
|---|---|---|---|---|---|---|
| Overall | < 65 yr | ≥ 65 yr | (GA vs. ISBPB) | (< 65 yr vs. ≥ 65 yr) | ||
| Number | 34 (15.5) | 186 (84.5) | 88 (47.3) | 98 (52.7) | ||
| Age (yr) | 60.1 ± 13.6 | 64.1 ± 10.5 | 55.3 ± 8.2 | 72.0 ± 4.3 | 0.118 | < 0.001 |
| Sex (F/M) | 10/24 | 98/88 | 41/47 | 57/41 | 0.013 | 0.115 |
| Height (cm) | 162.1 ± 9.3 | 159.8 ± 9.7 | 163.6 ± 9.4 | 156.5 ± 8.6 | 0.201 | < 0.001 |
| Weight (kg) | 67.2 ± 11.2 | 63.3 ± 11.5 | 66.9 ± 12.5 | 60.1 ± 2.9 | 0.069 | < 0.001 |
| Body mass index (kg/m2) | 25.5 ± 2.8 | 24.7 ± 3.3 | 24.9 ± 3.7 | 24.5 ± 2.9 | 0.215 | 0.351 |
| Duration of anesthesia (min) | 134.1 ± 27.9 | 129.4 ± 24.6 | 126.9 ± 25.7 | 131.6 ± 23.4 | 0.316 | 0.194 |
| Duration of operation (min) | 88.2 ± 25.8 | 81.5 ± 22.2 | 79.3 ± 24.2 | 83.4 ± 20.2 | 0.112 | 0.215 |
| Irrigation fluid (L) | 12.8 ± 2.0 | 13.2 ± 3.20 | 13.3 ± 3.8 | 13.1 ± 2.7 | 0.470 | 0.632 |
| Propofol dose (mg/kg/h) | 5.4 ± 1.5 | 5.9 ± 1.4 | 5.0 ± 1.4 | < 0.001 | ||
Values are presented as number (%), mean ± SD or number of patients. GA: general anesthesia, ISBPB: interscalene brachial plexus block.
Fig. 2.
Perioperative body temperature measured in the ward (baseline); on arrival to the operating room; in 15 min intervals until the end of anesthesia; and on admission to the PACU in all subjects of both groups. Error bars indicate standard deviations. OR: operating room, ANE: anesthesia, PACU: post-anesthetic care unit, GA: general anesthesia, ISBPB: interscalene brachial plexus block. No significant difference was observed in perioperative body temperatures between the two groups at each time point.
Table 2.
Incidence and Severity of Hypothermia
| Variable | Overall (n = 220) | Group GA (n = 34) | Group ISBPB (n = 186) | P value* |
|---|---|---|---|---|
| Hypothermia | 27 (12.3) | 10 (29.4) | 17 (9.1) | 0.002† |
| Mild (35.5–35.9℃) | 25 | 8 | 17 | |
| Moderate (35.0–35.4℃) | 2 | 2 | 0 | |
| Profound (< 35.0℃) | 0 | 0 | 0 |
Values are presented as number of patients (%). GA: general anesthesia, ISBPB: interscalene brachial plexus block.
Logistic regression analysis adjusted with propensity score,
Statistical significance was found between perioperative hypothermia and anesthetic methods (GA vs. ISBPB; odd ratio: 0.172, 95% CI: 0.057, 0.517).
In group ISBPB, there was no significant difference in demographic and perioperative data between elderly (≥ 65 years) and younger (< 65 years) patients, except age, height, weight, and propofol dosage. The dosage of propofol used for sedation was significantly higher in younger patients than elderly patients (5.9 ± 1.4 vs. 5.0 ± 1.4 mg/kg/h, respectively; P < 0.001). The incidence of hypothermia was similar in elderly and younger patients (9.2% vs. 9.1%, P = 0.983).
Discussion
In the present study, the incidence of perioperative hypothermia was significantly lower in patients using ISBPB with propofol sedation than general anesthesia (9.1% vs. 29.4%, P = 0.002) during arthroscopic shoulder surgery. In addition, the incidence of perioperative hypothermia between elderly and younger patients in the ISBPB group was similar (9.2% vs. 9.1%, P = 0.983). In demographic data, there was no significant difference between the two groups, except for sex. The female sex is a risk factor for hypothermia, but the difference in sex (female/male = 10/24 in Group GA) was considered not to significantly affect the results [13,14].
Perioperative hypothermia should be prevented through active and appropriate methods as it can cause various, and sometimes serious complications. According to the National Institute for Health and Care Excellence Clinical Guideline, perioperative body temperature should be monitored at < 30 min intervals before the induction of anesthesia until the end of surgery. Moreover, the operating room temperature should be maintained at ≥ 21°C for management of the body temperature, while fluids or blood should be warmed before use. When the body temperature falls below 36.5°C during surgery, it is recommended that a forced air warming device be used [15]. Other reported methods for maintaining perioperative body temperature include pre-warming and warmed inspired gas [11,16]. Arthroscopic shoulder surgery is a common surgical procedure in orthopedic surgery. It requires the use of a large amount of irrigation fluid during surgery to ensure a clear operating field of view, and this, in addition to anesthesia, is one of several important factors that can decrease body temperature during surgery [1]. Room-temperature or cold irrigation fluid is absorbed by the systemic circulation through injured blood vessels and soft tissues in the shoulder region, which is relatively close to the center of the body, resulting in a decrease in body temperature. Kim et al. [2] reported that the incidence of hypothermia was 91.3% when room-temperature fluid was used and 17.4% when warmed fluid (37–39°C) was used. However, whether the use of warmed irrigation fluid can reduce perioperative hypothermia remains unclear [1,12]. Among the various methods for maintaining body temperature during the perioperative period, it is also important to choose an anesthetic method that is more advantageous for maintaining the body temperature according to the type of surgery. However, research investigating anesthetic modalities for perioperative temperature management is lacking, and our study therefore investigated this.
Lim et al. [8] reported that performing ISBPB in the preoperative period with general anesthesia reduced the amount of inhalation anesthetic required and consequently decreased the degree of perioperative hypothermia. A combination of general anesthesia and ISBPB may be beneficial for perioperative temperature management by reducing the impairment of thermoregulation by anesthetic agents. Regional (ISBPB) or general anesthesia can be used in shoulder surgery. However, regional anesthesia has a few limitations, such as requiring additional local anesthesia after ISBPB in the posterior area of the shoulder, and patients experiencing severe discomfort due to positioning during surgery because the operation is commonly performed in the sitting or ‘deck’ position. Regional anesthesia is mainly used in combination with general anesthesia for postoperative pain management in shoulder surgery. To overcome these limitations of regional anesthesia, we performed sedation using propofol with ISBPB. By inhibiting thermoregulatory vasoconstriction, propofol can reduce the core body temperature similar to sevoflurane in general anesthesia [17]. Despite using propofol, which can cause hypothermia, the incidence of perioperative hypothermia was lower under ISBPB with propofol sedation than under general anesthesia with inhalation agents in the present study.
In elderly patients, the ability to control the body temperature is diminished; thus, the risk of hypothermia is increased under general anesthesia. Chun et al. [9] reported that although ISBPB was performed before general anesthesia and active warming was performed during an arthroscopic shoulder surgery, a significant temperature reduction occurred in elderly patients compared to young adult patients. The incidence of hypothermia in elderly patients was 93.1%, of whom 39.9% experienced a severe decrease in body temperature (≤ 34.9℃). However, in the present study, the incidence of hypothermia in the elderly patients of Group ISBPB was 9.2%, and there was no difference compared to younger patients. In addition, it was significantly lower than that reported by Chun et al. [9]. We speculate that ISBPB with sedation using propofol better preserved the ability to control the body temperature than general anesthesia in elderly patients.
The present investigation had limitations inherent to studies with retrospective designs. Firstly, the difference in the number of cases between the two groups was large. Thus, we performed the statistics adjusted with propensity score. Secondly, the ambient room temperature is an important cause of decreases in body temperature during surgery; however, we were not able to assess the operating room temperature in the present study. Thirdly, tympanic and esophageal thermometers were used in the two groups, and there was no protocol when using the thermometer. Finally, because active warming using a forced-air warming device was performed, it is difficult to clearly determine the effect of ISBPB alone. As such, future prospective studies investigating the effects of anesthesia combining ISBPB and sedation on perioperative body temperature management are required.
In conclusion, the incidence of perioperative hypothermia during arthroscopic shoulder surgery under ISBPB with propofol sedation is lower than that during general anesthesia. Furthermore, when using ISBPB with propofol sedation, the incidence of perioperative hypothermia in elderly patients is similar to that of younger patients.
Footnotes
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Ji Hye Lee (Writing – original draft)
Hyun Joo Heo (Data curation; Formal analysis)
Yu Yil Kim (Conceptualization; Supervision; Writing – review & editing)
Seung Min Baek (Data curation; Investigation)
Ki Man Kim (Data curation; Investigation)
Da Wa Jung (Data curation; Investigation)
References
- 1.Board TN, Srinivasan MS. The effect of irrigation fluid temperature on core body temperature in arthroscopic shoulder surgery. Arch Orthop Trauma Surg. 2008;128:531–3. doi: 10.1007/s00402-007-0368-x. [DOI] [PubMed] [Google Scholar]
- 2.Kim YS, Lee JY, Yang SC, Song JH, Koh HS, Park WK. Comparative study of the influence of room-temperature and warmed fluid irrigation on body temperature in arthroscopic shoulder surgery. Arthroscopy. 2009;25:24–9. doi: 10.1016/j.arthro.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Frank SM, Fleisher LA, Breslow MJ, Higgins MS, Olson KF, Kelly S, et al. Perioperative maintenance of normothermia reduces the incidence of morbid cardiac events. A randomized clinical trial. JAMA. 1997;277:1127–34. [PubMed] [Google Scholar]
- 4.Leslie K, Sessler DI, Bjorksten AR, Moayeri A. Mild hypothermia alters propofol pharmacokinetics and increases the duration of action of atracurium. Anesth Analg. 1995;80:1007–14. doi: 10.1097/00000539-199505000-00027. [DOI] [PubMed] [Google Scholar]
- 5.Rajagopalan S, Mascha E, Na J, Sessler DI. The effects of mild perioperative hypothermia on blood loss and transfusion requirement. Anesthesiology. 2008;108:71–7. doi: 10.1097/01.anes.0000296719.73450.52. [DOI] [PubMed] [Google Scholar]
- 6.Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334:1209–15. doi: 10.1056/NEJM199605093341901. [DOI] [PubMed] [Google Scholar]
- 7.Gentilello LM, Jurkovich GJ, Stark MS, Hassantash SA, O’Keefe GE. Is hypothermia in the victim of major trauma protective or harmful? A randomized, prospective study. Ann Surg. 1997;226:439–47. doi: 10.1097/00000658-199710000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim SH, Lee W, Park J, Kim MH, Cho K, Lee JH, et al. Preoperative interscalene brachial plexus block aids in perioperative temperature management during arthroscopic shoulder surgery. Korean J Anesthesiol. 2016;69:362–7. doi: 10.4097/kjae.2016.69.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chun EH, Lee GY, Kim CH. Postoperative hypothermia in geriatric patients undergoing arthroscopic shoulder surgery. Anesth Pain Med. 2019;14:112–6. [Google Scholar]
- 10.Shin KS, Lee GY, Chun EH, Kim YJ, Kim WJ. Effect of short-term prewarming on body temperature in arthroscopic shoulder surgery. Anesth Pain Med. 2017;12:388–93. [Google Scholar]
- 11.Jo YY, Kim HS, Chang YJ, Yun SY, Kwak HJ. The effect of warmed inspired gases on body temperature during arthroscopic shoulder surgery under general anesthesia. Korean J Anesthesiol. 2013;65:14–8. doi: 10.4097/kjae.2013.65.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oh JH, Kim JY, Chung SW, Park JS, Kim DH, Kim SH, et al. Warmed irrigation fluid does not decrease perioperative hypothermia during arthroscopic shoulder surgery. Arthroscopy. 2014;30:159–64. doi: 10.1016/j.arthro.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 13.Deakin CD. Changes in core temperature compartment size on induction of general anaesthesia. Br J Anaesth. 1998;81:861–4. doi: 10.1093/bja/81.6.861. [DOI] [PubMed] [Google Scholar]
- 14.Yi J, Xiang Z, Deng X, Fan T, Fu R, Geng W, et al. Incidence of inadvertent intraoperative hypothermia and its risk factors in patients undergoing general anesthesia in Beijing: a prospective regional survey. PLoS One. 2015;10:e0136136. doi: 10.1371/journal.pone.0136136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence . London: NICE; 2008. Apr, Inadvertent perioperative hypothermia overview [Internet] [updated 2018 Jan 12; cited 2020 Apr 7]. Available from https://pathways.nice.org.uk/pathways/inadvertent-perioperative-hypothermia. [PubMed] [Google Scholar]
- 16.Forbes SS, Eskicioglu C, Nathens AB, Fenech DS, Laflamme C, McLean RF, et al. Evidence-based guidelines for prevention of perioperative hypothermia. J Am Coll Surg. 2009;209:492–503. doi: 10.1016/j.jamcollsurg.2009.07.002. [DOI] [PubMed] [Google Scholar]
- 17.Im UJ, Lee DJ, Kim MC, Lee JS, Lee SJ. Difference in Core temperature in response to propofol-remifentanil anesthesia and sevoflurane-remifentanil anesthesia. Korean J Anesthesiol. 2009;57:704–8. doi: 10.4097/kjae.2009.57.6.704. [DOI] [PubMed] [Google Scholar]