Abstract
Severe coronavirus disease (COVID-19) is currently managed with systemic glucocorticoids. Opportunistic fungal infections are of concern in such patients. While COVID-19 associated pulmonary aspergillosis is increasingly recognized, mucormycosis is rare. We describe a case of probable pulmonary mucormycosis in a 55-year-old man with diabetes, end-stage kidney disease, and COVID-19. The index case was diagnosed with pulmonary mucormycosis 21 days following admission for severe COVID-19. He received 5 g of liposomal amphotericin B and was discharged after 54 days from the hospital. We also performed a systematic review of the literature and identified seven additional cases of COVID-19 associated mucormycosis (CAM). Of the eight cases included in our review, diabetes mellitus was the most common risk factor. Three subjects had no risk factor other than glucocorticoids for COVID-19. Mucormycosis usually developed 10–14 days after hospitalization. All except the index case died. In two subjects, CAM was diagnosed postmortem. Mucormycosis is an uncommon but serious infection that complicates the course of severe COVID-19. Subjects with diabetes mellitus and multiple risk factors may be at a higher risk for developing mucormycosis. Concurrent glucocorticoid therapy probably heightens the risk of mucormycosis. A high index of suspicion and aggressive management is required to improve outcomes.
Keywords: Zygomycosis, Mucorales, Tocilizumab, Dexamethasone, Diabetes, CAPA
Introduction
The pandemic coronavirus disease 2019 (COVID-19) continues to be a significant problem worldwide. While several treatment options have been evaluated, none except systemic glucocorticoids have been shown to improve survival in COVID-19. Unfortunately, the widespread use of glucocorticoids can lead to secondary bacterial or fungal infections. Invasive pulmonary aspergillosis complicating the course of COVID-19 is widely recognized;[1] however, mucormycosis is uncommonly suspected or diagnosed. Herein, we report a case of pulmonary mucormycosis in a patient with severe COVID-19. We also perform a systematic review of literature to identify cases of COVID-19 associated mucormycosis (CAM) and describe their clinical features, risk factors, and outcome.
Case Presentation
A 55-year-old man with long-standing diabetes mellitus, hypertension, and ischemic cardiomyopathy presented with fever, dry cough, and progressive breathlessness of three days duration. He was diagnosed with type 2 diabetes mellitus ten years before the current illness and was on irregular treatment with different oral hypoglycemic drugs. Blood sugar monitoring was infrequent. He also had end-stage renal disease and was receiving maintenance hemodialysis for the last one year. The patient was a never- smoker and denied any substance abuse. At admission, the respiratory rate was 26 breaths/minute, blood pressure 110/80 mmHg, and heart rate of 90 beats/minute. The oxygen saturation was 84% while breathing ambient air and improved to 95% with a venturi mask (fraction of inspired oxygen, 0.5). The patient was not obese (body mass index of 24 kg/m2).
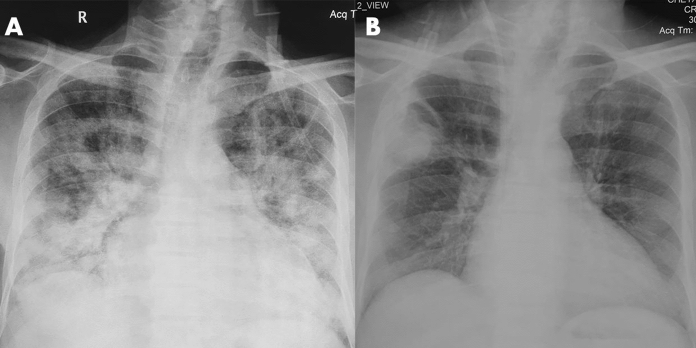
Chest radiograph showed bilateral diffuse interstitial opacities and cardiomegaly (Fig. 1a). A nasopharyngeal swab was positive for SARS-CoV-2 by RT–PCR. The hemoglobin at admission was 7.8 g/dL, and glycated hemoglobin was 5.3% (Table 1). He was started on intravenous dexamethasone (6 mg once a day for 14 days) and remdesivir (200 mg on day 1 and 100 mg on days 2–5). Supportive care, including oxygen supplementation, thromboprophylaxis for venous thrombosis, and maintenance hemodialysis, were continued. His random plasma glucose at admission was 140 mg/dL and increased to a maximum of 300 mg/dL during dexamethasone therapy. After 14 days of therapy, he had clinical improvement, hypoxemia improved, and radiological resolution.
Fig. 1.
Chest radiograph at admission a showing bilateral diffuse infiltrates and cardiomegaly. In the third week of hospitalization, a cavity with intracavitary content b can be seen in the right upper zone
Table 1.
Partial list of investigations in the index patient with pulmonary mucormycosis (PM) following treatment for COVID-19
| Investigations | At presentation | Day 21 (Diagnosis of PM) |
|---|---|---|
| Hemoglobin, g/dL | 7.8 | 6.6 |
| TLC, /µL | 6100 | 12,500 |
| DLC (N/L/E), % | 90/6/4 | 82/9/7.4 |
| Absolute lymphocyte count, /µL | 366 | 1125 |
| Absolute neutrophil count, /µL | 5490 | 10,250 |
| Platelet count, /µL | 60,000 | 222,700 |
| Blood urea, mg/dL | 20 | 63 |
| Serum creatinine, mg/dL | 8.4 | 3 |
| Total bilirubin, mg/dL | 0.3 | 0.5 |
| Alanine aminotransferase, U/L | 48 | 15 |
| Aspartate aminotransferase, U/L | 8 | 3 |
| Alkaline phosphatase, IU/L | 144 | 100 |
| Arterial pH | 7.33 | 7.44 |
| pCO2 | 22 | 29 |
| HCO3 | 13 | 20 |
| PO2 | 36.5 | 65 |
| Glycated hemoglobin, % | 5.3 | - |
DLC: differential leukocyte count; E: eosinophil; L: lymphocyte; N: neutrophil; TLC: total leukocyte count
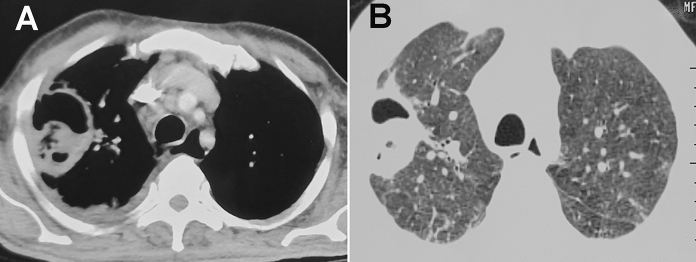
Three days later, the patient complained of cough, expectoration, and burning micturition. There was no fever, and he was not catheterized during hospitalization. Urine culture showed the growth of Escherichia coli. He was treated with intravenous meropenem 1 g every day (dose modified for renal impairment) for 10 days. Chest radiograph performed 21 days after admission showed a cavity with intracavitary contents in the right upper zone (Fig. 1B). Computed tomography (CT) of the thorax confirmed a thick-walled cavity in the right upper lobe (Fig. 2A, B). Minimal pleural effusion was also seen on the right side. Sputum examination with Gram stain, stain for acid-fast bacilli, and fungal smear was negative. The sputum culture on Sabouraud dextrose agar (SDA) at 25 °C and 37 °C grew a pure culture of cottony grayish white colony 6 days after incubation. Lactophenol cotton blue (LCB) mount from the growth revealed aseptate hyphae with nodal rhizoids and short sporangiophores with terminal spherical sporangia filled with brownish sporangiospores (Fig. 3), suggestive of Rhizopus microsporus. The identification was confirmed by matrix-assisted laser desorption/ionization time of flight (MALDI-TOF; Bruker Daltonics, Billerica, MA, USA), which gave a good discriminatory score of 2.1. The isolate was deposited in the National Culture Collection of Pathogenic Fungi (NCCPF), PGIMER, Chandigarh, India, with the accession number NCCPF 710,496. The in vitro antifungal susceptibility testing (AFST) of the isolate was performed by the microbroth dilution method as per the Clinical Laboratory Standards Institute (CLSI)-M38A2 guidelines.[2] The minimum inhibitory concentrations (MICs) of the isolate were as follows: amphotericin B, 0.5 µg/mL; itraconazole, 0.03 µg/mL; posaconazole, 2.0 µg/mL. Serum beta-d-glucan (Fungitell, Associates of Cape Cod, Inc, MA, USA) and serum galactomannan index were 189 pg/mL and 0.18 (Platelia Aspergillus galactomannan antigen, Bio-Rad, France), respectively. The patient was treated with liposomal amphotericin B (3 mg/kg) for probable pulmonary mucormycosis. His symptoms improved, and he was discharged 54 days after hospitalization (cumulative dose of amphotericin B, 5 gm). The patient received liposomal amphotericin (3 mg/kg/day) on an outpatient basis for 25 days after discharge and is scheduled for right upper lobectomy. At the time of discharge and after completion of amphotericin therapy, chest radiograph showed significant resolution of the right upper zone cavity (Fig. 4a, b).
Fig. 2.
Computed tomography showing thick-walled cavity in the right upper lobe in the corresponding mediastinal A and lung window B sections
Fig. 3.

Lactophenol cotton blue (LCB) mount from the growth revealed aseptate hyphae with nodal rhizoids and short sporangiophores with terminal spherical sporangia filled with brownish sporangiospores, suggestive of Rhizopus microsporus
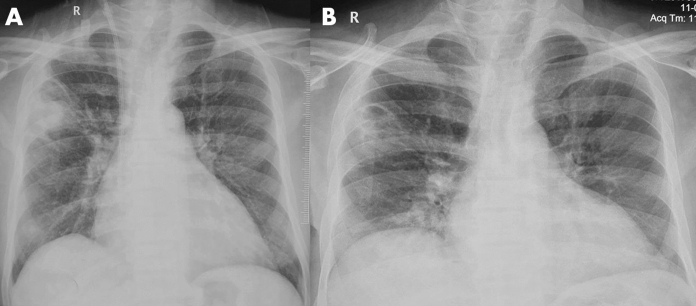
Fig. 4.
Chest radiograph performed at discharge A and after completing amphotericin therapy B showed significant resolution of the right upper zone cavity
Discussion
COVID-19 has already claimed more than one million lives worldwide. In the absence of an effective vaccine or antiviral therapy, supportive care plays a vital role in the management of COVID-19. Glucocorticoids and probably remdesivir are the only drugs proven to be beneficial in COVID-19. Glucocorticoids are inexpensive, widely available, and have been shown to reduce mortality in hypoxemic patients with COVID-19.[3] Nevertheless, glucocorticoids can increase the risk of secondary infections. Moreover, the immune dysregulation caused by the virus and the use of concurrent immunomodulatory drugs such as tocilizumab could further increase the risk of infections in COVID-19 patients.[4, 5].
We performed a systematic review of the PubMed and Embase databases till January 9, 2021, using the following free text terms: (“COVID” OR “SARS-CoV” OR “coronavirus”) AND (mucor* OR “zygomycosis”). We identified 21 citations, of which seven described mucormycosis in association with COVID-19 (Table 2)[6–11]. We excluded one study that described the detection of various respiratory pathogens in the throat swab of patients with SARS-CoV-2 infection (no invasive mucormycosis cases were reported).[12].
Table 2.
Summary of the COVID-19 associated mucormycosis (CAM) reported in the literature
| Author/country | Age in years/sex | Comorbid illness | Clinical presentation | Treatment for COVID-19 | Other treatments | Investigations | Antemortem diagnosis of CAM | Organs involved by CAM | Outcome | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|
| Hanley et al./UK[6] | 22/male | Obesity (BMI 48.8) | COVID ARDS (mechanically ventilated) | None mentioned | Linezolid | Lymphocyte count and serum creatinine, not provided | No (Autopsy diagnosis) | Lungs | Died (D27) | No traditional risk factors |
| Hypothyroidism | Pulmonary emboli | Meropenem | Hilar lymph nodes | |||||||
| Caspofungin | Heart and pericardium | |||||||||
| Brain | ||||||||||
| Kidney | ||||||||||
| Werthman-Ehrenreich/USA[10] | 33/female | Hypertension | Altered mentation, proptosis | Remdesivir | Vancomycin | Lymphopenia (5.9%) | Yes (suspected at presentation) | Rhino-orbito-cerebral | Died (D26) | – |
| Asthma | DKA and rhino-orbital mucormycosis | Convalescent plasma | Piperacillin tazobactam | Elevated serum creatinine (2.28 mg/dL) | ||||||
| Previously undiagnosed diabetes mellitus | No mention of glucocorticoids | Amphotericin B (formulation not mentioned) | ||||||||
| Mehta et al./India[7] | 60/male | Diabetes mellitus | COVID ARDS requiring mechanical ventilation | Inj methylprednisolone 40 mg BD | Meropenem | Lymphopenia (9.60%) | Yes (Symptoms developed at D10) | Rhino-orbital | Died | – |
| Peripheral vascular disease due to diabetes | Dexamethasone 4 mg BD | Oseltamivir | Elevated serum creatinine (1.57 mg/dL) | |||||||
| Tocilizumab 400 mg | Amphotericin (0.5 mg/kg/day, conventional) | |||||||||
| Monte junior ESD et al./Brazil[8] | 86/male | Hypertension | COVID ARDS and diarrhea | Hydrocortisone | Ceftriaxone | Lymphopenia (5.3%) | No | Gastric (presentation with malena, drop in hemoglobin, and large ulcers identified on endoscopy) | Died (D5) | No traditional risk factors |
| Azithromycin | Elevated serum creatinine (2.34 mg/dL) | |||||||||
| Oseltamivir | ||||||||||
| Placik et al./ USA[9] | 49/male | COVID ARDS | Remdesivir | Ceftriaxone | Lymphocyte count and serum creatinine, not provided | Yes (D14 developed spontaneous pneumothorax) | Pulmonary mucormycosis with bronchopleural fistula and pneumothorax | Died (D21) | Surgery and amphotericin for mucormycosis (6 days) | |
| Tocilizumab | Azithromycin | |||||||||
| Dexamethasone | Amphotericin B (formulation not mentioned) | |||||||||
| Mekkonen et al./USA[11] | 60/male | Diabetes mellitus (HbA1C 14%) | COVID ARDS (mechanically ventilated) | Remdesivir | Cefepime | NA | Yes (D10 of hospitalization) | Rhino-orbital | Died (D31) | The patient had symptoms suggestive of mucormycosis on D2 of hospitalization (D8 of illness) |
| Asthma | Dexamethasone (6 mg) | Vancomycin | ||||||||
| Hypertension | Convalescent plasma therapy (single session) | Amphotericin B (liposomal) | ||||||||
| Endoscopic surgical debridement | ||||||||||
| Pasero et al./Italy [13] | 66/male | Hypertension | COVID ARDS (mechanically ventilated) | Hydroxychloroquine | Meropenem | Lymphopenia (400/µL) | Yes (D14 after ICU admission) |
Lung Maxillary sinus thickening on computed tomography (not proven to be mucormycosis) |
Died (D62) | No traditional risk factors |
| Lopinavir–ritonavir | Linezolid | Renal failure requiring dialysis (creatinine not provided) | ||||||||
| Amphotericin B (20 days of liposomal preparation 5 mg/kg/d) | ||||||||||
| Isavuconazole after stopping amphotericin | ||||||||||
| Index case | 55/male | Diabetes mellitus | COVID ARDS (not mechanically ventilated) | Dexamethasone | Meropenem | Lymphopenia (6%) | Yes (Suspected when worsened on D14, Rhizopus microsporus isolated in sputum) | Lung | Alive (D54) |
Partial resolution of lung lesion Awaiting right upper lobectomy |
| Ischemic cardiomyopathy | Amphotericin B (liposomal preparation 3 mg/kg/day; cumulative 5 g) | Elevated serum creatinine (range 3–8 mg/dL) | ||||||||
| End-stage renal disease |
ARDS: acute respiratory distress syndrome; BMI–body mass index; COVID: coronavirus disease; E.coli: Escherichia coli; HbA1c: glycated hemoglobin
Of the eight cases reported thus far (including the index case), 3 and 2 cases were from the United States of America and India, respectively. One case each was reported from Brazil, Italy, and the United Kingdom.[6, 8, 13] The median (range) age was 57.5 (22–86) years, and seven were men. Diabetes mellitus (n = 4, 50%) was the most common predisposing condition; in one case, diabetes was previously undiagnosed. No traditional risk factors for mucormycosis were identified in three (37.5%) of the subjects.[6, 8, 13] Acute respiratory distress syndrome due to COVID-19 was present in seven cases. Elevated serum creatinine was seen in 5 cases, while the details were not available in the remaining three. Two subjects presented with symptoms suggesting mucormycosis (rhino-orbital mucormycosis), while the others developed mucormycosis following treatment for COVID-19 (usually between 10 and 14 days of hospitalization).[10, 11] The diagnosis was established postmortem in two subjects.[6, 8] The site of involvement by mucormycosis was rhino-orbito-cerebral (n = 3), pulmonary (n = 3), gastric (n = 1), and disseminated (n = 1). All except the index case died.
While COVID-19 associated pulmonary aspergillosis (CAPA) has received much attention, mucormycosis, another devastating disease, remains unrecognized.[1, 14] The diagnosis of CAPA relies on the presence of risk factors, consistent radiology, and demonstration of Aspergillus in tissue culture or microscopy.[14] While galactomannan in bronchoalveolar lavage is a useful marker of invasive pulmonary aspergillosis, its role in CAPA has not been confirmed. Invasive mold infections (invasive pulmonary aspergillosis and pulmonary mucormycosis) share similar risk factors, clinical presentation, and radiology. The diagnosis of CAM is thus even more challenging. A lack of clinical suspicion and difficulty isolating the causative fungi might contribute to the underdiagnosis of mucormycosis. Two of the eight cases included in our review were diagnosed postmortem. Further, biomarkers such as beta-d-glucan and galactomannan, which aid in diagnosing invasive aspergillosis, are not available for mucormycosis. To our knowledge, we report the first successfully managed case of probable pulmonary mucormycosis developing after treatment for COVID-19. Diabetes mellitus has been associated with severe COVID-19. Those with diabetes are at an increased risk of death than those without.[15] Further, poorly controlled diabetic patients may have overt or covert renal dysfunction. In our review, four and five subjects had diabetes mellitus and renal dysfunction (serum creatinine not provided in the remaining three cases), respectively (Table 2). The presence of multiple risk factors or comorbid illnesses in severe COVID-19 patients, along with the additional immunosuppression caused by glucocorticoids, increases the net state of immune suppression, thereby predisposing them to invasive mold infections.
The index patient had unmonitored blood sugar in the past and was recently diagnosed with end-stage kidney disease. Glycated hemoglobin becomes unreliable in the presence of severe anemia, especially in patients undergoing hemodialysis.[16] The favorable outcome in the current case was probably because of the better glycemic control in-hospital, and the timely initiation of liposomal amphotericin B. Previous studies have shown that amphotericin B is generally well-tolerated and can be safely administered in subjects undergoing dialysis (even with the older deoxycholate and colloidal dispersion formulations of amphotericin).[17, 18] The current guideline for the management of mucormycosis recommends liposomal amphotericin B at a dose of 5–10 mg/kg per day. In the absence of central nervous system involvement, a dose of 5 mg/kg is suggested.[19] In a randomized controlled trial of 201 patients with invasive mold disease, liposomal amphotericin used at 3 mg/kg/day was equally effective but safer and better tolerated than 10 mg/kg/day dose amphotericin.[20] Our patient had end-stage kidney disease and was on concurrent nephrotoxic medications, yet he tolerated liposomal amphotericin well. The optimal duration of therapy in mucormycosis is not clear and is guided by the treatment regimen’s clinical response and tolerability.
Pulmonary mucormycosis is increasingly diagnosed, and the case fatality has improved over time.[21] Control of hyperglycemia, early treatment with liposomal amphotericin B, and surgery are essential for the successful management of mucormycosis.[19, 22, 23] However, COVID-19 has created a unique scenario where all three aspects of the management are compromised. Firstly, hyperglycemia is aggravated by the most effective therapy for severe COVID-19, namely glucocorticoids. Coexisting ARDS and multiorgan dysfunction preclude timely diagnostic imaging and testing.[13] Finally, the hospitals are overwhelmed by COVID-19 patients, and essential services, including diagnostics and surgeries, could be significantly curtailed.[24] Hence, the mortality in CAM (87.5% in the current series) maybe even higher than that observed in non-COVID patients.[21, 23, 25].
One alarming observation was the absence of traditional risk factors, such as diabetes mellitus, transplantation, or hematological malignancies, in three subjects with CAM. The development of mucormycosis can probably be attributed to the use of glucocorticoids and suggests a need for their judicious use. Thus, the use of glucocorticoids in mild COVID-19 cases (without hypoxemia) or the utilization of higher doses of glucocorticoids should be avoided. Further, in the absence of a clear benefit, drugs targeting immune pathways such as tocilizumab should be discouraged.[5].
In summary, physicians caring for critically ill COVID-19 patients must be aware of serious infections that can complicate the course of COVID-19. A high degree of clinical suspicion is required to diagnose pulmonary mucormycosis.[26] Early diagnosis and timely management are necessary to improve outcomes in pulmonary mucormycosis.
Compliance with ethical standards
Conflict of interest
The authors declare that there is no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Deepak Garg and Valliappan Muthu contributed equally to the manuscript and are the joint first authors.
References
- 1.Arastehfar A, Carvalho A, van de Veerdonk FL, Jenks JD, Koehler P, Krause R, et al. COVID-19 associated pulmonary aspergillosis (CAPA)-from immunology to treatment. J Fungi (Basel). 2020;6(2):91. doi: 10.3390/jof6020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reference method for broth dilution antifungal susceptibility testing of filamentous fungi: approved standard-second edition. CLSI document M38-A2. Clinical and Laboratory Standards Institute, Wayne, PA: CLSI, 2008.
- 3.Group WHOREAfC-TW. Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, et al. Association between administration of systemic corticosteroids and mortality among critically Ill patients with COVID-19 a meta-analysis. JAMA. 2020;324(13):1330–13341. doi: 10.1001/jama.2020.17023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar G, Adams A, Hererra M, Rojas ER, Singh V, Sakhuja A, et al. Predictors and outcomes of hais in COVID-19 patients. Int J Infect Dis. 2020;104(3):287–92. [DOI] [PMC free article] [PubMed]
- 5.Kimmig LM, Wu D, Gold M, Pettit NN, Pitrak D, Mueller J, et al. IL-6 inhibition in critically Ill COVID-19 patients is associated with increased secondary infections. Front Med (Lausanne) 2020;7:583897. doi: 10.3389/fmed.2020.583897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hanley B, Naresh KN, Roufosse C, Nicholson AG, Weir J, Cooke GS, et al. Histopathological findings and viral tropism in UK patients with severe fatal COVID-19: a post-mortem study. Lancet Microbe. 2020;1(6):e245–e253. doi: 10.1016/S2666-5247(20)30115-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mehta S, Pandey A. Rhino-orbital mucormycosis associated with COVID-19. Cureus. 2020;12(9):e10726. doi: 10.7759/cureus.10726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monte Junior ESD, Santos M, Ribeiro IB, Luz GO, Baba ER, Hirsch BS, et al. Rare and fatal gastrointestinal mucormycosis (Zygomycosis) in a COVID-19 patient: a case report. Clin Endosc. 2020;53(6):746–749. doi: 10.5946/ce.2020.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Placik DA, Taylor WL, Wnuk NM. Bronchopleural fistula development in the setting of novel therapies for acute respiratory distress syndrome in SARS-CoV-2 pneumonia. Radiol Case Rep. 2020;15(11):2378–2381. doi: 10.1016/j.radcr.2020.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Werthman-Ehrenreich A. Mucormycosis with orbital compartment syndrome in a patient with COVID-19. Am J Emerg Med. 2020. 10.1016/j.ajem.2020.09.032. [DOI] [PMC free article] [PubMed]
- 11.Mekonnen ZK, Ashraf DC, Jankowski T, Grob SR, Vagefi MR, Kersten RC, et al. Acute Invasive Rhino-Orbital Mucormycosis in a Patient With COVID-19-Associated Acute Respiratory Distress Syndrome. Ophthalmic Plast Reconstr Surg. 2020. 10.1097/IOP.0000000000001889. [DOI] [PMC free article] [PubMed]
- 12.Zhu X, Ge Y, Wu T, Zhao K, Chen Y, Wu B, et al. Co-infection with respiratory pathogens among COVID-2019 cases. Virus Res. 2020;285:198005. doi: 10.1016/j.virusres.2020.198005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pasero D, Sanna S, Liperi C, Piredda D, Branca GP, Casadio L, et al. A challenging complication following SARS-CoV-2 infection: a case of pulmonary mucormycosis. Infection. 2020. 10.1007/s15010-020-01561-x. [DOI] [PMC free article] [PubMed]
- 14.Koehler P, Bassetti M, Chakrabarti A, Chen SCA, Colombo AL, Hoenigl M, et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2020. 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed]
- 15.Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8(9):782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Radin MS. Pitfalls in hemoglobin A1c measurement: when results may be misleading. J Gen Intern Med. 2014;29(2):388–394. doi: 10.1007/s11606-013-2595-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wood JE, Mahnensmith MP, Mahnensmith RL, Perazella MA. Intradialytic administration of amphotericin B: clinical observations on efficacy and safety. Am J Med Sci. 2004;327(1):5–8. doi: 10.1097/00000441-200401000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Anaissie EJ, Mattiuzzi GN, Miller CB, Noskin GA, Gurwith MJ, Mamelok RD, et al. Treatment of invasive fungal infections in renally impaired patients with amphotericin B colloidal dispersion. Antimicrob Agents Chemother. 1998;42(3):606–611. doi: 10.1128/AAC.42.3.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Global guideline for the diagnosis and management of mucormycosis: an initiative of the european confederation of medical mycology in cooperation with the mycoses study group education and research consortium. Lancet Infect Dis. 2019;19(12):e405–e421. doi: 10.1016/S1473-3099(19)30312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cornely OA, Maertens J, Bresnik M, Ebrahimi R, Ullmann AJ, Bouza E, Heussel CP, Lortholary O, Rieger C, Boehme A, Aoun M, Horst H-A, Thiebaut A, Ruhnke M, Reichert D, Vianelli N, Krause SW, Olavarria E, Herbrecht R. Liposomal amphotericin B as initial therapy for invasive mold infection: A randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad Trial). Clin Infect Dis. 2007;44(10):1289–1297 [DOI] [PubMed]
- 21.Muthu V, Agarwal R, Dhooria S, Sehgal IS, Prasad KT, Aggarwal AN, et al. Has the mortality from pulmonary mucormycosis changed over time? a systematic review and meta-analysis. Clin Microbiol and Infect. 2021 doi: 10.1016/j.cmi.2020.12.035. [DOI] [PubMed] [Google Scholar]
- 22.Chougule A, Muthu V, Bal A, Rudramurthy SM, Dhooria S, Das A, et al. Pulmonary gangrene due to rhizopus spp staphylococcus aureus klebsiella pneumoniae and probable sarcina organisms. Mycopathologia. 2015;180(12):131–136. doi: 10.1007/s11046-015-9904-3. [DOI] [PubMed] [Google Scholar]
- 23.Patel A, Kaur H, Xess I, Michael JS, Savio J, Rudramurthy S, et al. A multicentre observational study on the epidemiology, risk factors, management and outcomes of mucormycosis in India. Clin Microbiol Infect. 2020;26(7):9–15. doi: 10.1016/j.cmi.2019.11.021. [DOI] [PubMed] [Google Scholar]
- 24.Pandey N, Kaushal V, Puri GD, Taneja S, Biswal M, Mahajan P, et al. Transforming a general hospital to an infectious disease hospital for COVID-19 over 2 weeks. Front Public Health. 2020;8:382. doi: 10.3389/fpubh.2020.00382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, Chen SC, et al. Contemporary management and clinical outcomes of mucormycosis: a systematic review and meta-analysis of case reports. Int J Antimicrob Agents. 2019;53(5):589–597. doi: 10.1016/j.ijantimicag.2019.01.002. [DOI] [PubMed] [Google Scholar]
- 26.Muthu V, Dhooria S, Singh Sehgal I, Thurai Prasad K, Agarwal R. The reversed halo sign and the bronchus sign: the eyes see only what the mind knows. Ann Am Thorac Soc. 2019;16(9):1203. doi: 10.1513/AnnalsATS.201905-360LE. [DOI] [PMC free article] [PubMed] [Google Scholar]