Abstract
A novel coronavirus was identified as the cause of a cluster of pneumonia cases in Wuhan, China in December 2019. This cluster quickly spread across the globe and led the World Health Organization (WHO) to declare severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) a pandemic on March 11, 2020. It’s sudden emergence, ceaseless human-to-human transmission, and rapid spread has led to continuous pandemicity. As of June 9, 2020, there were 7 039 918 confirmed cases and 404 396 deaths globally. The rate of spread of COVID-19 is affected through respiratory droplets, most commonly when infected individuals cough or talk. The virus is released through respiratory secretions that infect individuals once contact with mucous membranes is made directly or indirectly. Our research was conducted via an electronic literature review on PubMed, Google Scholar, and MedLine Plus. Data were then collected from peer-reviewed articles that included applicable keywords and published between January 1, 2020, and June 9, 2020. This article highlights the rapid spread of SARS-CoV-2 worldwide and indicates a higher number of mortalities in the elderly and those with comorbidities. As the number of cases increases, an immediate need to “flatten the curve” is essential to avoid catastrophic overwhelming of hospital systems across the affected countries. To do so, there is an emphasis on detection, testing, isolating the infected, and organizing the healthcare response to the virus. The rapid spread of infection has impacted over 200 countries and territories to date. This report takes a closer look at the cases, fatalities, and recoveries in different regions of the world with details regarding the geographic scale of SARS-CoV-2 spread, risks, and the subsequent impact on the countries affected. Also, this report discusses some effective measures that were carried out by some countries that helped them to mitigate the pandemic and flatten the curve of COVID-19 spread as early as possible.
Keywords: Coronavirus, COVID-19, SARS-CoV-2, global outbreak, pandemic
Introduction
What began as an emerging pneumonia-like illness in Wuhan, China in December 2019 has now been declared as a global pandemic by the World Health Organization (WHO) on March 11, 2020.1 The Chinese Center for Disease Control and Prevention (CDC) ruled out related coronaviruses such as influenza, avian influenza, adenovirus, severe acute respiratory syndrome coronavirus (SARS-CoV-1), and Middle East respiratory syndrome coronavirus (MERS-CoV) as possible causes for the respiratory syndrome, but eventually declared it as a novel coronavirus, giving it the name COVID-19.2 Wuhan, South China Seafood Market was noted to be the epicenter of COVID-19.2 Though the actual route of transmission is uncertain at this point, it is speculated to be a zoonotic disease transmitted to humans; however, the prevalence of human-to-human transmission has led to the pandemicity.3
Nationwide diagnostics of 4021 patients in China performed by January 26, 2020, revealed that patients between the ages of 30 to 65-years accounted for 71.45% of the confirmed cases, while pediatric patients less than 10-years old accounted for 0.35%.4 The elderly population, particularly those without immunization, as well as front-line workers and their respective families are believed to be among the high-risk group.4 Also, patients with underlying diseases such as asthma, diabetics, and heart disease are most susceptible to COVID-19.4
Since the first patient admission was reported on December 12, 2019, and the first death of a Chinese national in early January 2020, travel-related cases began emerging in Thailand, Japan, South Korea, France, and the United States of America (USA) by mid-January.3 By the end of January, the novel coronavirus had spread through the Western Pacific, South-East Asia, USA, Canada, Europe, and Eastern Mediterranean countries.5 This spread constituted a Public Health Emergency of International Concern (PHEIC). As of June 9, 2020, there were 7 039 918 confirmed cases with 404 396 deaths and 3 596 972 that recovered, globally.6,7
Respiratory droplets from coughing, sneezing, and talking; indirect contact by touching contaminated surfaces with hands leading to contact with oral and nasal cavities, eyes, and mucous membranes; fecal-oral transmission and aerosol transmission have been implicated as the causes of the spread of COVID-19, a virus with an incubation period between 2 and 14-days.4 As clustered cases emerged earlier on, efforts to bring awareness to the general public by ending public gatherings, tracking and managing close contacts, and self-isolation to curb the transmission had failed;4 at which time, countries began establishing stricter monitoring and control measures for transportation facilities, workplace environments, and civil aviation.4 When these attempts proved inadequate, emergency shutdowns, and curfews worldwide were implemented as it was declared a pandemic in early March of 2020 due to escalating cases. Also, WHO has raised its global risk assessment for the new coronavirus to “very high,” as some countries struggle to contain the pathogen.7 The purpose of this article is to explore the geographic scale of COVID-19 spread, risks, and the subsequent impact on the countries affected, in addition to efforts made by different countries toward mitigating the spread and impact of the pandemic.
Methodology
An electronic literature review search was performed on PubMed, Google Scholar, and MedlinePlus.
The search was limited to peer-reviewed articles published from January 1, 2020, through June 9, 2020, for the compiled data. The articles were selected if they included keywords such as coronavirus, COVID-19, SARS-CoV-2, global outbreak, and pandemic. Articles were then reviewed and included based on the applicability to the topic.
Pattern of Spread
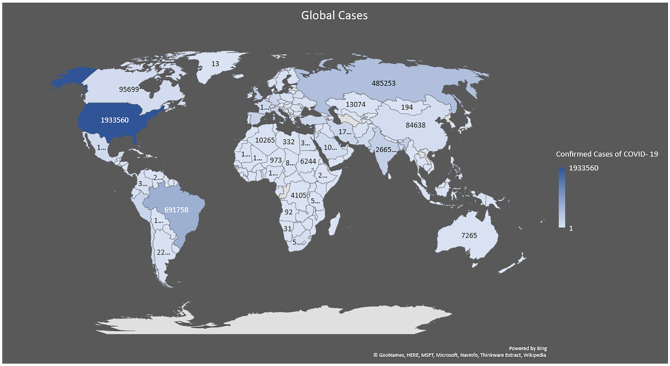
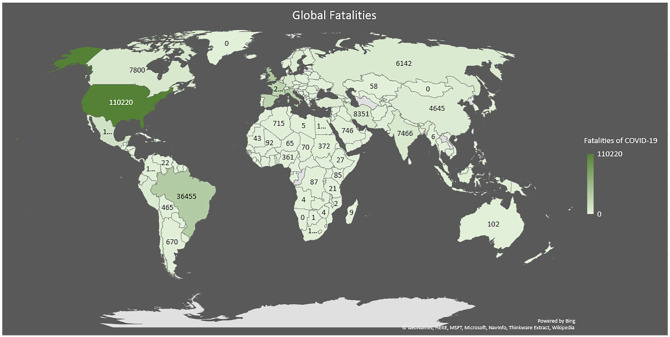
The world is currently experiencing an outbreak of the novel coronavirus, which started in Wuhan, China, and has rapidly spread globally to impact 213 countries and territories as of June 9, 2020.1,6 On March 11, 2020, WHO announced that COVID-19 could now be characterized as a pandemic that needs to be stopped, as it rapidly spreads to parts of Asia and Europe, with cases and fatalities illustrated appropriately in Figures 1 and 2.7-9 To date, China is no longer the leading country with the most confirmed COVID-19 cases and deaths.10 China’s-WHO Joint Mission Team reported that the COVID-19 epidemic rapidly spread between January 10 and 12, 2020, but following rigorous containment and quarantine efforts, the number of new cases in China began peaking and plateaued by late-January 2020.9,10
Figure 1.
Global confirmed cases of COVID-19, as of June 9, 2020.
The situation in numbers is obtained for cases by WHO.7
Figure 2.
Global confirmed fatalities due to COVID-19, as of June 9, 2020.
The situation in numbers is obtained for fatalities by WHO.7
Many different factors determine the spread of this virus which should be addressed immediately to flatten the curve. Measures such as early detection, testing, isolating the infected persons, and mobilizing the healthcare response to the virus is crucial in this regard.8 Despite rigorous mitigation efforts (i.e., travel bans, quarantine, social distancing, isolation of infected populations, etc.), the growing prevalence and disease severity have overwhelmed even the most advanced countries and healthcare infrastructures.11 Countries like Italy, the United Kingdom (UK), and the USA have experienced great strain on their healthcare system. This is partially due to limited health care professionals, critical care facilities with sparse mechanical ventilators, and the shortage of personal protective equipment (PPE), further jeopardizing public health outcomes.11,12 With little time to prepare, the pandemic is causing a major health crisis along with profound social and economic consequences across Asia, Europe, and North America.9 However, the current data may not represent the true disease burden of the ongoing COVID-19 pandemic in other parts of Asia, the Middle East, Africa, and Latin America, as many countries are limited by test availability, test processing rates, data collection, and reporting capabilities.9,13
As of June 9, 2020, the USA is the North American country with the highest number of confirmed cases of COVID-19 which was 1 993 560, Mexico had 117 103 cases, and Canada had 95 699, as shown in Figure 1.7 In South America, the WHO reported total confirmed cases in Brazil as 691 758, Peru had 196 515 cases, and Chile had 138 846 cases.7 The most affected countries in the African region were South Africa with 50 879 cases, Nigeria with 12 801 cases, and Algeria with 10 265 cases.7 In Europe, the Russian Federation had 485 253 confirmed cases, the UK 287 403 cases, and Spain had 241 717 cases. China is still the Western Pacific country with the most confirmed cases of COVID-19 which was 84 638. India had 266 598 total confirmed cases, whereas Bangladesh (68 504) and Indonesia (32 033) of South-East Asia had fewer reported cases.7 Australia reported 7265 confirmed cases, followed by New Zealand which had 1154, and Guam 171 cases7 (Figure 1).
As of June 9, 2020, the USA had the highest number of fatalities from COVID-19 in North America, which was 110 220 deaths, followed by Mexico with 13 699 and Canada with 7800, as seen in Figure 2.7 In South America, Brazil had the highest number of fatalities which were 36 455 deaths, Peru had 5465 deaths, and Chile with 2264.7 South Africa had the highest number of fatalities which were 1080 deaths, followed by Algeria with 715, and Nigeria with 361 in the continent of Africa.7 In Europe, the countries with very high recorded fatalities were the UK with 40 597 deaths, Italy with 33 964 deaths, and France with 29 149 deaths.7 In Asia, Iran had the highest number of fatalities which was 5957, followed by China with 4643, and India with 1074 deaths. Australia had the highest number of fatalities in their Oceania region which was 102, followed by New Zealand with 22 deaths, and Guam with 5 fatalities7 (Figure 2).
Table 1 highlights the confirmed cases and fatalities surrounding COVID-19 by depicting the top 5 affected countries, as well as the 5 least affected countries in each region categorized by WHO, as of June 9, 2020.
Table 1.
Confirmed cases and fatalities of COVID-19 in most and least affected countries per region.
| Total number of confirmed cases | Total deaths | |
|---|---|---|
| Region: Africa | ||
| Most affected countries | ||
| South Africa | 50 879 | 1080 |
| Nigeria | 12 801 | 361 |
| Algeria | 10 265 | 715 |
| Ghana | 9910 | 48 |
| Cameroon | 8060 | 215 |
| Least affected countries | ||
| Lesotho | 4 | 0 |
| Seychelles | 11 | 0 |
| Gambia | 28 | 1 |
| Namibia | 31 | 0 |
| Eritrea | 41 | 0 |
| Region: Americas | ||
| Most affected countries | ||
| USA | 1 933 560 | 110 220 |
| Brazil | 691 758 | 36 455 |
| Peru | 196 515 | 5465 |
| Chile | 138 846 | 2264 |
| Mexico | 117 103 | 13 699 |
| Least affected countries | ||
| Saint Kitts and Nevis | 15 | 0 |
| Dominica | 16 | 0 |
| Saint Lucia | 19 | 0 |
| Belize | 19 | 2 |
| Grenada | 23 | 0 |
| Region: Eastern Mediterranean | ||
| Most affected countries | ||
| Iran | 173 832 | 8351 |
| Saudi Arabia | 105 283 | 746 |
| Pakistan | 108 317 | 2172 |
| Qatar | 70 158 | 57 |
| United Arab Emirates | 39 376 | 281 |
| Least affected countries | ||
| Syrian Arab Republic | 144 | 6 |
| Libya | 332 | 5 |
| Yemen | 500 | 113 |
| Jordan | 831 | 9 |
| Tunisia | 1087 | 49 |
| Region: Europe | ||
| Most affected countries | ||
| Russia | 485 253 | 6142 |
| UK | 287 403 | 40 597 |
| Spain | 241 717 | 27 136 |
| Italy | 235 278 | 33 964 |
| Germany | 184 543 | 8711 |
| Least affected countries | ||
| Holy See | 12 | 0 |
| Liechtenstein | 83 | 1 |
| Monaco | 99 | 1 |
| Montenegro | 324 | 9 |
| Malta | 630 | 9 |
| Region: South East Asia | ||
| Most affected countries | ||
| India | 266 598 | 7466 |
| Bangladesh | 68 504 | 930 |
| Indonesia | 32 033 | 1883 |
| Thailand | 3121 | 58 |
| Nepal | 3762 | 14 |
| Least affected countries | ||
| Timor-Leste | 24 | 0 |
| Bhutan | 59 | 0 |
| Myanmar | 244 | 6 |
| Sri Lanka | 1857 | 11 |
| Maldives | 1916 | 8 |
| Region: Western Pacific | ||
| Most affected countries | ||
| China | 84 638 | 4645 |
| Singapore | 38 296 | 25 |
| Philippines | 22 474 | 1011 |
| Japan | 17 210 | 916 |
| Republic of Korea | 11 852 | 274 |
| Least affected countries | ||
| Papua New Guinea | 8 | 0 |
| Fiji | 18 | 0 |
| Lao People’s Democratic Republic | 19 | 0 |
| Cambodia | 126 | 0 |
| Brunei Darussalam | 141 | 2 |
Source: Data sourced from WHO situation report 141 through June 9, 2020.7
North and Central America
USA
Different parts of the USA are seeing varying levels of COVID-19 activity, which are dependent on many factors, such as the duration and severity of the pandemic phase, recent travels, and public health responses.1 As of June 9, 2020, there have been 1 933 560 reported cases with 110 220 deaths and 788 062 recoveries from COVID-19 within the USA.6,7 In the USA, 802 cases were reported on March 13, 2020, one of the highest numbers of new cases reported in a single day.1 New York State, as of June 8, 2020, has the highest number of cases reported in the USA, which was over 379 000.14 Over half of these cases in New York State are from one of the busiest cities in the world, New York City.14 Washington State reported 24 354 cases with a total of 1176 deaths, as of June 9, 2020.15 Of those cases in Washington, individuals between the age ranges of 40 to 59-years constituted the group with the highest number of confirmed cases. Furthermore, 34% of cases were seen in individuals over the age of 80 with a 53% case fatality rate.15 California was in a state of emergency, with 133 489 positive cases and 4697 deaths, as of June 9, 2020.16
Canada
As of June 9, 2020, there have been roughly 95 699 reported cases, 7800 deaths, and 55 572 discharged cases related to COVID-19 in Canada.6,7 The highest number of cases were seen in highly populated provinces, such as Quebec with 53 185 confirmed (5029 deaths) and Ontario with 31 090 confirmed (2464 deaths), as of June 9, 2020.17 There was an increased risk of more severe outcomes for Canadians who are aged 65 and over with compromised immune systems or with underlying medical conditions.17
Mexico
In Mexico, there have been a total of 117 103 cases, 13 699 deaths, and 90 748 recovered, as of June 9, 2020.6,7 The cases of COVID-19 in Mexico were predominately through community-based transmission, according to the United States embassy in Mexico.7,18 As stated by WHO, the new confirmed cases in a single day as of June 9, 2020, were 3484 and the new deaths were 188.7
Central America
In Central America, Panama has the highest number of confirmed cases with 16 425 cases (393 deaths), Honduras had 6327 cases (258 deaths), and Costa Rica had 1318 cases (10 deaths), as of June 9, 2020.6,7 On March 10, 2020, Panama became the second country in Latin America and the first Central American country to have a confirmed coronavirus-related death.19 A 40-year-old Panamanian woman who had traveled to Spain became Panama’s first confirmed case of COVID-19, in early March of 2020.19 On March 11, 2020, Honduras reported its first 2 cases of COVID-19 involving 2 women who had traveled to Europe: a 42-year-old who arrived from Spain and a 37-year-old who returned from Switzerland.19
Caribbean Islands
The Caribbean Public Health Authority (CARPHA) stated that as of June 8, 2020, there were 33 157 cases and 937 deaths related to COVID-19 in 33 countries and territories in the Caribbean region.20 On March 21, 2020, 48 new cases were reported in the Caribbean region amongst people over the age of 50, making it one of the highest numbers of reported cases in a single day in the Caribbean.20 It is estimated that 40% of the cases were imported into the Caribbean by travelers and 36% were caused by close contacts, according to CARPHA.20 As of June 9, 2020, the Dominican Republic had roughly 20 000 confirmed cases followed by Cuba with roughly 2200 cases.6,7 The Dominican Republic had its first confirmed case of COVID-19, reported on March 1, 2020, involving a 62-year-old Italian tourist.19 Furthermore, the Dominican Republic reported its first death from the virus on March 16, 2020, which involved a 47-year-old human immunodeficiency virus (HIV) positive woman, who also had tuberculosis (TB) and had traveled to Spain, recently.19
South America
In total, there were more than 1 219 723 cases of COVID-19 in South America that have been reported, as of June 9, 2020.6,21 As of June 9, 2020, the WHO reported the total confirmed cases in Brazil as 691 758 cases, Peru had 196 515 cases, and Chile had 138 846 cases, as shown in Figure 1.7 Dr. Carissa F. Etienne, the Director of Pan American Health Organization (PAHO), states that there were 3 main scenarios by which COVID-19 was introduced into the Americas: importation, community transmission, and outbreaks in enclosed areas such as nursing homes.22 It is important to note that the transmission of COVID-19 in the majority of the countries in South America was via local transmission, except for Curacao and Suriname where transmission was believed to have occurred via sporadic cases.7 Brazil is seen to have the highest number of fatalities which were 18 912 deaths, followed by Peru 4757 and Chile which had 4696 deaths, as seen in Figure 2.7
Africa
The outbreak of COVID-19 in the WHO African region has rapidly progressed over the past several weeks with large areas affected, as shown in Figure 1. The WHO situation report of June 9, 2020, showed a cumulative total of 140 498 reported cases and 3352 deaths related to COVID-19 across 47 countries and territories in the African region.7 The most affected countries in the WHO African region were South Africa (50 879 cases), Nigeria (12 801 cases), Algeria (10 265 cases), Ghana (9 910 cases), and Cameroon (8 060 cases).7 It is estimated that the majority of cases have arisen from community transmission or clusters of cases, although a few African countries show sporadic cases (ie, Uganda, Rwanda, Zimbabwe, Eritrea, Namibia, Gambia, and Lesotho).7 South Africa is seen to have the highest number of fatalities which was 1080, followed by Algeria which had 715 deaths, and Nigeria with 361, as shown in Figure 2.7 This recent upsurge in cases and deaths, over the past weeks, is concerning as many low-income African countries have extremely vulnerable populations that have a very high prevalence of HIV, malnutrition, and various chronic illnesses. According to WHO, African governments will need to strictly adhere to mitigation methods to reduce the spread of the virus and in doing so, prevent further straining/stretching of an already fragile health system.23
Europe
The spread of COVID-19 has been significantly higher in the WHO European region than in any other region of the world, as shown in Figure 1. As of June 9, 2020, there have been a cumulative total of 2 303 361 confirmed cases and 184 671 total deaths related to COVID-19 across 60 countries and territories in the European region.7,24 Overnight, the European region has had a significant increase of 16 801 new confirmed cases and 551 new deaths, mostly acquired via community transmission or cluster of cases.7 The most affected countries in the WHO European region were the Russian Federation (485 253 cases), the UK (287 403 cases), Spain (241 717 cases), Italy (235 278 cases), and Germany (184 543 cases).7 Of all the reported cases in the European region, 11% resulted in death, which implies that 89% of infected persons recovered.25 The WHO European region situation update for COVID-19 showed that 75% of the cumulative deaths were reported from the UK (40 597 fatalities), Italy (33 964 fatalities), France (29 149 fatalities), and Spain (27 136 fatalities), as shown in Figure 2.7,25 The fatality rate showed that 94% of all deaths were in persons aged 60-years and older.25 The COVID-19 situation in Europe has strongly affected the health care system throughout the region with 17% of the reported infections involving healthcare workers.25 Due to the dire situation, many member states have implemented strategies to focus most of their efforts on severe cases and conducting sentinel surveillance.25
Asia
As of June 9, 2020, India (South-East Asia) was the country with the most confirmed cases of COVID-19 which was 266 598, followed by the Islamic Republic of Iran (Eastern Mediterranean) with 173 832, and China (Western Pacific) with 84 638 in the Asian region. A majority of these cases were classified as community transmission and clusters of cases, as shown in Figure 1.7 Iran had the highest deaths related to COVID-19 which was 8351, followed by India with 7466, and China with 4642 deaths. These countries experienced larger outbreaks of local transmission and/or are clustered in time, geographic location, and common exposures which lead to the fatalities, as shown in Figure 2.7
Oceania
Out of the 14 countries that fall under the region of Oceania, Australia has reported 7265 confirmed cases of COVID-19, as of June 9, 2020, followed by New Zealand which had 1154 cases, and Guam with 171 cases, as shown in Figure 1. Cases in Australia, New Zealand, and Guam were due to a cluster of cases, whereas the 8 cases in Papua New Guinea were due to sporadic cases.7 Australia was seen to have the most fatalities which stood at 102, followed by New Zealand with 22, and Guam with 5 deaths, as seen in Figure 2.7
Discussion
The ideology of “slowing the spread” comes to mind when thinking about control of the spread of COVID-19 around the globe. The confirmed cases and deaths peak in countries with COVID-19 depending on population education and awareness, preventative measures, surveillance of the infected, and interventions taking place.26 Although slowing the spread may result in an increased time to confirm case and death peak, the goal of this practice is to prevent hospital systems from being strained beyond their capacity, thus resulting in less mortality.27
In Canada, it was found that with isolation practices, the peak would be delayed by 2 to 4-wk, and intensive care unit (ICU) admissions could be reduced up to 53.6%.28 Also, Canada has been prompt at relocating its PPE between various facilities, depending on the need.29 Other countries yet to see the peak would benefit substantially by implementing aggressive social distancing, self-isolation, closure of schools and other institutions, encouraging working from home, and/or placing hard limits on the size of crowds at events so that the burden on hospitals will be lessened resulting in increased capacity to treat and ultimately, decreased mortality.30
Also, regions such as Sub-Saharan Africa have reported a significantly lower number of positive COVID-19 cases when compared to their northern hemisphere counterparts who have a much higher testing capacity.31 Furthermore, travel from China to the USA, as well as to various parts of Europe have caused the number of confirmed cases in each visiting country to be skewed.31 However, no country is more immune to the virus when compared to another.31 The common goal globally is to eradicate the virus. This can be achieved by observing those countries whose approaches have flattened the curve, learning from those whose infection rate has risen and avoiding their strategies, and by adopting ideas that are proven to be successful at slowing the rate of infection.30 However, geographical location and the timing of spread may serve as a fundamental reason why some countries have been more or less devastated by the virus.29
By rapidly scaling up mass testing of their population at a very early stage, countries like South Korea (11 719 cases and 273 deaths), Vietnam (329 cases and 0 deaths), and Taiwan (443 cases and 7 deaths), as of June 6, 2020, were able to see a fall in the infection rate.29,32,33 These 3 countries were taught to compensate for weakness in their health care systems based on their experience with the 2003 SARS-CoV-1 outbreak thus, enabling them to respond more effectively in flattening the curve.33,34
Germany is another country that constructively flattened the curve. It is seen as the country with the region’s fifth-highest number of confirmed cases (184 543) with only 8711 deaths.7,33 This is largely due to the outstanding German health care system; in particular, the country’s nursing professionals consist of 13 nurses per 1000 people, allowing them to focus on patient management and survival.33,35 Taiwan, Iceland, and Sweden being perhaps the most notable exceptions, did not shut down the whole country, but instead employed early case detection, established at-risk contacts, and quarantined the infected.36 As of April 11, 2020, South Korea had flattened the curve without shutting down the country by implementing stricter protocols, including public awareness campaigns, personal hygiene practices such as hand-washing, and early detection of the virus by testing the general public.37 Hong Kong, Singapore, and Japan also took similar measures by taking action immediately to manage the outbreak, readjusted surveillance systems to identify potential cases, and provided diagnostic tests and increased testing capacity which led to earlier recovery.38 As of June 8, 2020, Finland is the most successful in flattening the curve and/or containing the rate of spread with an average 7-day decline of cases by −10.8%.39
Conclusion
Since December 2019, the outbreak that started in the city of Wuhan, China has managed to spread to over 200 countries and territories and turned from an epidemic into a pandemic. The rate of transmission, methods of containment, number of individuals infected, and the death rates vary widely amongst different countries. The conclusion drawn from this research is that the virus spreads quickly, often through those who do not know that they are carriers, and seems to present more severely in those with advanced age and underlying health conditions. From this research and by the statistics from different areas of the world, it can be concluded that infection from the virus results in death in individuals who are 80-years old or older, with a case fatality rate reaching up to 50% of deaths among infected individuals in this age group.
The transmissibility of the virus also seems to be higher in densely populated areas. Given that the incubation period can be 2 to 14-days, and many younger and healthy infected individuals have mild or no symptoms, the metropolitan New York City, has seen substantially increased transmission of the virus despite mitigation measures that were in place. Countries and areas that have had aggressive containment measures, such as complete lockdowns and stay at home orders, have seen considerable decreases in rates of transmissibility. What is evident is that the mitigation efforts are slowing down the spread when acted upon aggressively, but there is still widespread transmission and death amongst individuals in countries where the SARS-CoV-2 infection has been reported, which is depicted graphically in the figures above. To slow the spread, and ultimately eradicate the SARS-CoV-2 virus, countries must work together to develop a vaccine or create an effective therapeutic intervention to prevent further increase in death and transmission. Citizens of the affected countries should adhere to instructions from CDC, WHO, and their local administrators concerning social distancing, avoiding large gatherings, seeking testing when symptomatic, and wearing face masks, to forestall further spread of this virus.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: A.S.: Conceptualization, and design, approval of the final version, responsibility for the accuracy, and integrity of all aspects of research. C.O.: Supervision and revising the article for intellectual content; editing. Z.H.: Writing—review, and editing. R.P.:Writing—review, and editing. P.D.: Writing—review, and editing. S.P.: Writing—review, and editing. U.J.: Writing—review, and editing. J.M.: Writing—review, and editing. A.M.: Writing—review, and editing; project administration.
References
- 1. CDC. Coronavirus disease 2019 (COVID-19) situation reports. Centers for Disease Control; 2020. Accessed April 30, 2020 https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html#covid19-pandemic [Google Scholar]
- 2. The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin J Epidemiol. 2020;41(2):145-151. [PMC free article] [PubMed] [Google Scholar]
- 3. Ralph R, Lew J, Zeng T, et al. 2019-nCoV (Wuhan virus), a novel coronavirus: human-to-human transmission, travel-related cases, and vaccine readiness. J Infect Dev Ctries. 2020;14:3-17. [DOI] [PubMed] [Google Scholar]
- 4. Special Expert Group for Control of the Epidemic of Novel Coronavirus Pneumonia of the Chinese Preventative Medicine Association. An update on the epidemiological characteristics of novel coronavirus pneumonia (COVID-19). Chin J Epidemiol. 2020;41:139-144. [Google Scholar]
- 5. WHO. Novel coronavirus (2019-nCoV) situation reports—30. World Health Organization; 2020. Accessed March 24, 2020 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200130-sitrep-10-ncov.pdf?sfvrsn=d0b2e480_2 [Google Scholar]
- 6. Meter, an Addax Company. COVID-19 coronavirus pandemic. World Meter; March 23, 2020. Accessed June 9, 2020 https://www.worldometers.info/coronavirus/ [Google Scholar]
- 7. WHO. Novel coronavirus (2019-nCoV) situation reports—141. World Health Organization; 2020. Accessed June 9, 2020 https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200609-covid-19-sitrep-141.pdf?sfvrsn=72fa1b16_2 [Google Scholar]
- 8. WHO. WHO Director-General’s opening remarks at the media briefing on COVID-19—11 March 2020. World Health Organization; 2020. Accessed April 30, 2020 https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 [Google Scholar]
- 9. Cross J. Summary of emergent infectious disease: coronavirus COVID-19 focus, compiled 19 March 2020. Presentation by Cross John W. 2020. Accessed April 30, 2020 https://www.researchgate.net/publication/340060965
- 10. Rabi FA, Al Zoubi MS, Kasasbeh GA, Salameh DM, Al-Nasser AD. SARS-CoV-2 and coronavirus disease 2019: what we know so far. Pathogens. 2020;9:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cavallo JJ, Donoho DA, Forman HP. Hospital capacity and operations in the coronavirus disease 2019 (COVID-19) pandemic—planning for the Nth patient. JAMA Health Forum. March 17, 2020. Accessed April 30, 2020 https://jamanetwork.com/channels/health-forum/fullarticle/2763353 [DOI] [PubMed]
- 12. Le NK, Le AV, Parikh J, et al. Ecological and health infrastructure factors affecting the transmission and mortality of COVID-19. BMC Infectious Diseases; March 30, 2020. Accessed April 30, 2020 10.21203/rs.3.rs-19504/v1 [DOI] [Google Scholar]
- 13. Rodriguez AMJ, Balbin GJR, Rabaan A, et al. Genomic epidemiology and its importance in the study of the COVID-19 pandemic. Infez Med. 2020;28:139-142. [PubMed] [Google Scholar]
- 14. Department of Health New York State. County by county breakdown of positive cases. New York Government; 2020. Accessed June 9, 2020 https://coronavirus.health.ny.gov/county-county-breakdown-positive-cases [Google Scholar]
- 15. Washington State Department of Health. 2019 Novel coronavirus outbreak (COVID-19). Washington Government. 2020. Accessed June 9, 2020 https://www.doh.wa.gov/Emergencies/Coronavirus
- 16. California Department of Public Health. Coronavirus (COVID-19) in California. California Government; 2020. Accessed June 9, 2020 https://covid19.ca.gov/ [Google Scholar]
- 17. Canada. Coronavirus disease (COVID-19): outbreak update. Government of Canada; 2020. Accessed June 9, 2020 https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html?topic=tilelink#a1 [Google Scholar]
- 18. U.S. Embassy. COVID-19 information. U.S. Embassy and Consulates in Mexico. 2020. Accessed April 30, 2020 https://mx.usembassy.gov/covid-19-information/
- 19. AS/COA. Where is the coronavirus in Latin America? Americas Society Council of the Americas. 2020. Accessed April 30, 2020 https://www.as-coa.org/articles/where-coronavirus-latin-america
- 20. CARPHA. Coronavirus disease (COVID-19). Caribbean Public Health Agency Situation Report No. 55. 2020. Accessed June 9, 2020 https://carpha.org/Portals/0/Documents/SitRepInfographics/Infographic%2010-SITREP56-COVID19.pdf
- 21. Statista. Number of confirmed cases of novel coronavirus (COVID-19) in Latin America and the Caribbean as of March 24, 2020, by country. Health & Pharmaceuticals State of Health Statista. 2020. Accessed April 30, 2020 https://www.statista.com/statistics/1101643/latin-america-caribbean-coronavirus-cases/
- 22. PAHO. PAHO director to health ministers—“reorganize health services to care for COVID-19 patients and save lives.” Pan American Health Organization; 2020. Accessed April 30, 2020 https://www.paho.org/hq/index.php?option=com_content&view=article&id=15758:paho-director-to-health-ministers-reorganize-health-services-to-care-for-covid-19-patients-and-save-lives&catid=740&lang=en&Itemid=1926 [Google Scholar]
- 23. WHO. COVID-19 situation report for the WHO African region. World Health Organization; 2020. Accessed March 25, 2020 https://apps.who.int/iris/bitstream/handle/10665/331587/SITREP_COVID-19_WHOAFRO_20200325-eng.pdf [Google Scholar]
- 24. WHO. COVID-19 situation in the WHO European region. World Health Organization; 2020. Accessed June 9, 2020 https://who.maps.arcgis.com/apps/opsdashboard/index.html#/ead3c6475654481ca51c248d52ab9c61 [Google Scholar]
- 25. WHO. COVID-19 situation update for the WHO European region—data for the week of 16-22 March 2020. World Health Organization; 2020. Accessed April 30, 2020 http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/weekly-surveillance-report [Google Scholar]
- 26. Villela DAM. The value of mitigating epidemic peaks of COVID-19 for more effective public health responses. Rev Soc Bras Med Trop. 2020;53:e20200135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kenyon C. Flattening-the-curve associated with reduced COVID-19 case fatality rates—an ecological analysis of 65 countries. J Infect. 2020;81:e98-e99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shoukat A, Wells CR, Langley JM, et al. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. CMAJ. 2020;192:E489-E496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cain P, Hartshorn M. Flattening the coronavirus curve: how Canada compares with other countries. Global News. May 5, 2020. Accessed June 8, 2020 https://globalnews.ca/news/6901193/flattening-the-curve-coronavirus-comparison-canada-other-countries/
- 30. Routley N. Infection trajectory: see which countries are flattening their COVID-19 curve. Healthcare. March 16, 2020. Accessed June 8, 2020 https://www.visualcapitalist.com/infection-trajectory-flattening-the-covid19-curve/
- 31. John Hopkins. COVID-19: coronavirus questions and answers. John Hopkins Bloomberg School of Public Health. 2020. Accessed June 6, 2020 https://www.jhsph.edu/covid-19/questions-and-answers/index.html
- 32. WHO. Coronavirus disease (COVID-19) dashboard. World Health Organization. June 6, 2020. Accessed June 6, 2020 https://covid19.who.int/?gclid=CjwKCAjwt-L2BRA_EiwAacX32Y5vIT6cz-kzRxHUdwm9P6RHwlKXZvh0GP-02DmNXi7f4xkHr-P6VRoCZbEQAvD_BwE
- 33. Thompson D. Three countries have kept coronavirus in check: here’s how they did it. WebMD HealthDay News. March 27, 2020. Accessed June 6, 2020 https://www.webmd.com/lung/news/20200327/how-three-countries-have-kept-covid-19-in-check#1
- 34. Adalja AA, Toner E, Inglesby TV. Priorities for the US health community responding to COVID-19. JAMA. 2020;323:1342-1344. [DOI] [PubMed] [Google Scholar]
- 35. Zander-Jentsch B, Wagner F, Rzayeva N, et al. Strengthening health systems through nursing: evidence from 14 European countries. European Observatory on Health Systems and Policies. 2019. Accessed June 6, 2020 https://pubmed.ncbi.nlm.nih.gov/31465161/ [PubMed]
- 36. Preskorn SH. The 5% of the population at high risk for severe COVID-19 infection is identifiable and needs to be taken into account when reopening the economy. J Psychiatr Pract. 2020;26:219-227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Petersen E, Wasserman S, Lee S-S, et al. COVID-19—we urgently need to start developing an exit strategy. Int J Infect Dis. 2020;96:233-239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Legido-Quigley H, Asgari N, Teo YY, et al. Are high-performing health systems resilient against the COVID-19 epidemic? Lancet. 2020;395:848-850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Evans T. Where is coronavirus rising and falling? John Hopkins University. June 8, 2020. Accessed June 8, 2020 https://informationisbeautiful.net/visualizations/covid-19-coronavirus-infographic-datapack/