Abstract
To address financial and scheduling conflicts associated with residency interviews for otolaryngology candidates, our residency program implemented virtual interviews as an alternative to the traditional in-person format for our visiting subinterns during the 2018-2019 and 2019-2020 interview cycles. Applicants then completed an anonymous survey about their interview experience. We found that, overall, positive attitudes toward virtual interviews increased among 2019-2020 candidates as compared with the year prior. Our results demonstrated an average cost savings per interview of $500 to $1000 when virtual technology was utilized. Based on feedback, improvements may be considered regarding eye contact, minimizing distractions, and providing the option to extend the interview length. Our experience provides a preliminary framework for transitioning to virtual interviews in the upcoming 2020-2021 otolaryngology residency selection process during the COVID-19 era, as well as for future studies assessing the utility of this method and its impact on overall match statistics.
Keywords: otolaryngology, residency selection, recruitment, interviews, virtual interviews, COVID-19
Otolaryngology residency positions are among the most highly sought by US medical students.1 Commensurate with this interest, applicants apply to numerous programs to increase their chances of a successful match.2-5 For aspiring otolaryngology residents, this translates to an increased financial burden and overlap of interview dates, reducing potential interactive opportunities between candidates and programs. In the 2018-2019 cycle, our program piloted virtual interviews (VIs) for select candidates to address the limitations of face-to-face interviews (FFIs). Our goal was to improve flexibility, optimize program resources, and minimize expenses for applicants.
Our experience has become increasingly relevant as the COVID-19 pandemic presents novel challenges to trainee education and recruitment throughout the country. Formal recommendations have been made to cancel visiting subinternships6 and commit to VIs for all applicants in the 2020-2021 cycle.7 In this study, we highlight our 2-year experience utilizing VIs, share applicant feedback, and propose strategies to enhance use of VIs during these unprecedented times.
Methods
This study was determined exempt from Institutional Review Board of the University of California San Diego. Otolaryngology applicants interviewing at the University of California San Diego during the 2018-2019 and 2019-2020 cycles were included. The majority participated in traditional FFIs consisting of 6 to 8 unstructured meetings 15 minutes long. Applicants who participated in a 4-week subinternship at our program were offered a single 15-minute VI via Zoom (Zoom Video Communications, Inc) with multiple faculty and a chief resident.
Following the applicant and program rank list submission date, an anonymous survey (SurveyMonkey Inc) about applicant experiences and attitudes toward VIs was distributed. No identifying information was collected, and applicants were informed that their participation would not affect the match process.
Results
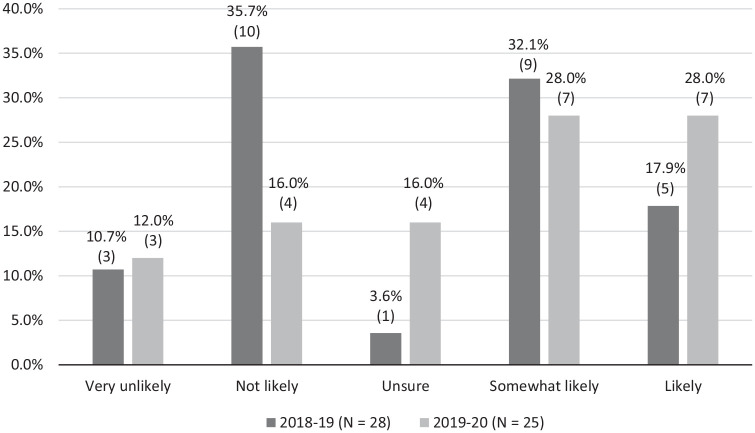
Of 94 total senior medical students, 53 FFI and 12 VI applicants completed the survey (n = 65; response rate, 69.1%). Respondents estimated an average interview expense between $500 and $1000 and did not have prior experience with VIs (67.9% FFI, 91.7% VI). For VI respondents, audio and visual quality met expectations (75% and 67%, respectively), and 58% reported that the overall experience met expectations ( Table 1 ). However, 58% reported suboptimal eye contact. VI respondents also noted the financial benefit and feasibility as positive aspects but reported difficulty with eye contact, flow of conversation, and time limitations ( Table 2 ). After stratification by interview cycle, 28.0% of 2019-2020 FFI applicants reported that they would have chosen VIs if offered, as compared with only 17.9% of 2018-2019 FFI applicants ( Figure 1 ).
Table 1.
Applicant Impressions Regarding the Quality of Virtual Interviews. a
| Audio | Video | Eye contact | Overall | |
|---|---|---|---|---|
| Poor | 0 (0) | 0 (0) | 3 (25.0) | 1 (8.3) |
| Suboptimal | 3 (25.0) | 4 (33.3) | 7 (58.3) | 4 (33.3) |
| Met expectations | 9 (75.0) | 8 (66.7) | 2 (16.7) | 7 (58.3) |
| Exceeded expectations | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
Data are listed as No. (%). Bold indicates majority
Table 2.
Sample Open-ended Comments From Virtual Interviewees.
| Positive | “Web-based interview seemed feasible since I already knew the faculty.” “Audio and visual quality was fine.” “I absolutely appreciate the intent to save money.” |
| Negative | “Hard to tell who was speaking, especially the people in the back.” “Obvious negative flow on conversation due to lag.” “Conference room setting was unexpected.” |
Figure 1.
Face-to-face interviewees’ responses regarding likelihood of electing for virtual interviews if given the opportunity. Data are listed as % (No.).
Discussion
Our study demonstrates that VIs may be a flexible cost-saving alternative to FFI in the otolaryngology resident selection process. In addition to historical concerns regarding cost and interview scheduling, safety measures related to COVID-19 have emphasized the need for alternative interview strategies.8 As the otolaryngology literature lacks a robust analysis of VI practices, we share our experiences and suggestions to prepare for the upcoming interview cycle.9-14
Despite advancements in video conference technology, we identified several opportunities for improvement. Thirty-three percent of candidates noted suboptimal visual quality. Applicants also noted difficulty maintaining eye contact and unexpected interruptions in conversation due to video lag and poor internet connection. The majority of our candidates did not have prior experience with VIs at the time of this study. As virtual communication has increased in prevalence during the COVID-19 pandemic, we anticipate increased familiarity during the upcoming interview cycle. Nevertheless, applicants should be reminded to test audiovisual quality in advance, ensure a reliable internet connection, and limit simultaneous use of other programs to improve bandwidth and minimize technical failures.15
One applicant emphasized difficulty distinguishing which interviewer was speaking and reported an increased number of distractions as faculty and residents gathered in one conference room. Providing multiple mini-interview sessions with fewer faculty per session may mitigate this concern while allowing candidates to engage in more focused conversations.
Regarding interview duration, our VI applicants commented that despite their preexisting familiarity with faculty and residents, the 15 minutes allotted was insufficient. Institutions may consider increasing the amount of time designated per interview in the upcoming cycle to permit greater faculty and interviewee dialogue.
VIs can improve the otolaryngology residency selection process by increasing exposure among applicants and programs, improving efficiency, and reducing financial burden. By extending this technology to resident recruitment, programs can provide a valuable opportunity for applicants to familiarize themselves with training programs with which they may not have otherwise interfaced. As in-person visiting subinternships are discouraged during the pandemic,6 hosting virtual lectures, facility tours, and social hours can increase a program’s applicant exposure and enhance the subsequent VI experience.
Limitations include this being a single-institution study with a limited number of participants, which may affect generalizability. Additionally, we offered VIs only to applicants who had attended a 4-week subinternship and were familiar with our faculty, residents, and facility. As VIs take on a prominent role in the 2020-2021 residency cycle, further studies are needed to understand the feasibility of this technology on a broader applicant pool, assess the impact of the interview format on faculty impressions, and determine its effect on ranking decisions and match outcomes.
Conclusion
Our experience provides a framework for the upcoming transition to VIs as well as future investigations evaluating the effectiveness of this method on a larger scale. Although there remains room for minor technological improvements, we found that candidates’ attitudes toward VIs at our institution have become more favorable over subsequent years. Widespread use of this modality during otolaryngology interviews has become a mandate; however, it will afford the opportunity to increase applicant and program exposure, significantly decrease interview expenses, and maintain safety during this critical time.
Author Contributions
Morgan E. Davis, concept, design, data collection, analysis, writing, review; Aria Jafari, concept, design, data collection, analysis, writing, review; Kayva Crawford, concept, design, data collection, analysis, writing, review; Bridget V. MacDonald, concept, design, data collection and visual interpretation; Deborah Watson, concept, design, data collection, analysis, review.
Disclosures
Competing interests: None.
Sponsorships: None.
Funding source: None.
Acknowledgments
We thank and acknowledge Norissa Gastelum, program administrator, for her help in identifying the study population, distributing the surveys, and collecting data for analysis.
Footnotes
Data from 2018-2019 were included in a poster presentation at the 2020 ACGME Annual Education Conference; February 27, 2020; San Diego, California.
References
- 1. Platt M. How do I match in otolaryngology? American Academy of Otolaryngology–Head and Neck Surgery. Published March 8, 2019. Accessed April 8, 2020 https://www.entnet.org/content/how-do-i-match-otolaryngology
- 2. National Resident Matching Program. Results and Data: 2018 Main Residency Match. National Resident Matching Program; 2018. [Google Scholar]
- 3. National Resident Matching Program. Results and Data: 2014 Main Residency Match. National Resident Matching Program; 2014. [Google Scholar]
- 4. Bhalla V, Sykes KJ, Kraft SM, Chiu AG. Commentary on Bowe et al, “The state of the otolaryngology match: a review of applicant trends, ‘impossible’ qualifications, and implications.” Otolaryngol Head Neck Surg. 2018;158(2):217-218. [DOI] [PubMed] [Google Scholar]
- 5. Eisenman DJ, Guardiani E. The otolaryngology match 2019: why was this year different from every other year? Otolaryngol Head Neck Surg. 2020;162(2):157-159. doi: 10.1177/0194599819888648 [DOI] [PubMed] [Google Scholar]
- 6. Society of University Otolaryngologists, Association of Academic Departments of Otolaryngology, Otolaryngology Program Directors Organization. SUO/AADO/OPDO statement regarding away rotations. Published April 27, 2020. https://cdn.ymaws.com/suo-aado.org/resource/resmgr/covid-19/suo-aado-opdo_away_rotation_.pdf
- 7. Coalition for Physician Accountability’s Work Group on Medial Students in the Class of 2021 Moving Across Institutions for Post Graduate Training. Final report and recommendations for medical education institutions of LCME-accredited, US osteopathic, and non-US medical school applicants. Accessed May 11, 2020 https://www.aamc.org/system/files/2020-05/covid19_Final_Recommendations_05112020.pdf
- 8. Centers for Disease Control and Prevention. Social distancing, quarantine, and isolation. Accessed May 11, 2020 https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
- 9. Daram SR, Wu R, Tang S-J. Interview from anywhere: feasibility and utility of web-based videoconference interviews in the gastroenterology fellowship selection process. Am J Gastroenterol. 2014;109(2):155-159. [DOI] [PubMed] [Google Scholar]
- 10. Melendez MM, Dobryansky M, Alizadeh K. Live online video interviews dramatically improve the plastic surgery residency application process. Plast Reconstr Surg. 2012;130(1):240e-241e. [DOI] [PubMed] [Google Scholar]
- 11. Pasadhika S, Altenbernd T, Ober RR, Harvey EM, Miller JM. Residency interview video conferencing. Ophthalmology. 2012;119(2):426-426.e5. [DOI] [PubMed] [Google Scholar]
- 12. Pourmand A, Lee H, Fair M, Maloney K, Caggiula A. Feasibility and usability of tele-interview for medical residency interview. West J Emerg Med. 2018;19(1):80-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shah SK, Arora S, Skipper B, Kalishman S, Timm TC, Smith AY. Outcomes/epidemiology/socioeconomics randomized evaluation of a web based interview process for urology resident selection. J Urol. 2012;187(4):1380-1384. [DOI] [PubMed] [Google Scholar]
- 14. Vadi MG, Malkin MR, Lenart J, Stier GR, Gatling JW, Applegate RL., II Comparison of web-based and face-to-face interviews for application to an anesthesiology training program: a pilot study. Int J Med Educ. 2016;7:102-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones RE, Abdelfattah KR. Virtual interviews in the era of COVID-19: a primer for applicants. J Surg Educ. 2020;77(4):733-734. doi: 10.1016/j.jsurg.2020.03.020 [DOI] [PMC free article] [PubMed] [Google Scholar]