Abstract
Background:
Self-care instruction in pharmacy curricula is essential given the impact pharmacists have in caring for patients in the community and their evolving role in this area. The primary objective of this study was to strengthen our current understanding of self-care education across undergraduate Canadian pharmacy programs.
Methods:
A national curriculum survey and follow-up phone interview was conducted in 2019 to assess the quantity and quality of self-care instruction across Canadian pharmacy schools. Representatives were selected based on theirparticipation in the Association of Faculties of Pharmacy of Canada Self-Care Therapeutics and Minor Ailments special interest group.
Results:
Responses were received from all 10 pharmacy schools in Canada. Self-care education varies across Canadian pharmacy curricula, reflecting differences in scopes of practice across provinces, topics of interest and availability of space within curricula by the various faculties. Specifically, there was considerable variability in the number of hours devoted to self-care education, course content and methods for integration and teaching.
Conclusions:
Results of this study may help inform and evolve self-care curricula across the country. We argue that strategies for enhancing current programs may include establishing a minimum number of core hours and topics, expanding natural health product content and curricular content oversight by a lead faculty member. Can Pharm J (Ott) 2021;154:xx-xx.
Introduction
Advising patients on self-care, which includes over-the-counter (OTC) and natural health product (NHP) use, in the community is a key responsibility of Canadian pharmacists. The profession has been the purveyor of OTC medicines within our health care system for decades, if not a century. Anecdotes from years ago tell of Canadians turning to community pharmacists for help as the only health care provider in town, especially in rural parts of the country. Such symptoms make up a significant portion of what affects the public from a health standpoint. For perspective, Canadians suffered from an estimated 82 million headaches/migraines, 85 million colds/flu and 46 million episodes of indigestion/heartburn (circa 2011).1 Pharmacist services at the community level are crucial during the current pandemic, made more so given the intersecting issues of influenza, common colds and coronavirus disease 2019.
Knowledge Into Practice.
A description of the status of self-care education in Canadian pharmacy schools is lacking.
Results of this study provide insight into current educational efforts in preparing student pharmacists to deliver care to patients with common ambulatory ailments in community settings.
Canadian pharmacy schools generally claim adequate preparation of pharmacy students to advise on self-care and prescribe for certain indications, but some room for improvement was identified.
Mise En Pratique Des Connaissances.
Il n’y a pas de description de l’état de la formation sur l’automédication dans les facultés de pharmacie canadiennes.
Les résultats de cette étude renseignent sur les efforts éducatifs actuels pour préparer les étudiants en pharmacie à fournir des soins aux patients ambulatoires présentant des troubles courants dans les pharmacies communautaires.
Les facultés de pharmacie canadiennes indiquent généralement fournir une préparation adéquate aux étudiants en pharmacie quant aux conseils à fournir pour l’automédication et aux prescriptions dans certaines indications, toutefois, des aspects qui pourraient être améliorés ont été mis en évidence.
Community pharmacists will need little convincing to substantiate this role, as patients daily ask for assistance with a cold, selecting a vitamin or when to see a doctor for a rash. Attempts have been made to quantify this activity. The Canadian Pharmacist Intervention Study found that approximately 15.3 million encounters involving OTC medicines take place yearly (circa 1995).2 The estimated benefit of these activities potentially resulted in cost-savings to the health care system of $168.8 million (assuming only conditional referrals to physician care) to $265.8 million Canadian dollars (assuming half of the encounters prevented a physician visit).2 Pharmacists recommended that a patient see a physician in 8.6% of the cases.2
Given the impact pharmacists have in providing care to individuals with ambulatory conditions in the community, how the next generation of pharmacists is trained is critical. Questions remain as to which topics should constitute core material (given limited space within curricula and competition with other subjects), how best to deliver curricular content and the best balance between practice labs, didactic lectures, discovery learning and so on. For a global perspective, Sinopoulou and Rutter3 received feedback from 84 schools from 24 countries. The main focus during a student’s time in the various programs was symptom presentation (97%), how to gather information (often using mnemonics) (97%) and when to refer to medical care (74%).3 Instructors of pharmacy self-care courses at American universities have reinforced the importance of this material within a curriculum, suggested 10 topics to define what constitutes core material and have recommended instructional delivery methods.4 Others have also discussed ways to improve interactions between pharmacists and the public, be it at the practice level or within educational confines.5-8 Textbooks are also available for guidance.9-12
Studies evaluating current self-care pharmacy curricula in a Canadian context are lacking. In addition, pharmacists are taking on expanded scope of practice beyond advising on self-care by prescribing for ambulatory conditions and preventative medicine that previously required referral to another health care provider. An assessment of how Canadian pharmacy schools have incorporated instruction in curricula to prepare students for these expanded roles is needed. To address these questions and others, we aimed to strengthen our understanding of how pharmacy students are taught about self-care and minor/common ailments prescribing across Canada and to compare these results to previously published findings internationally.
Methods
In 2018, a Self-Care Therapeutics and Minor Ailments (SCTMA) special interest group (SIG) of members from the Association of Faculties of Pharmacy of Canada (AFPC) was formed. The goal of the SIG is to address key issues related to self-care education, contribute expertise in nonprescription therapeutics and minor/common ailment education, serve as a resource for pharmacy faculties and educators in Canada and collaborate with and support one another. To understand current efforts and perspectives in teaching self-care across Canadian pharmacy curricula, a cross-sectional survey was completed from February 6 to 27, 2019. This study received approval by the University of Waterloo institutional review board (ORE#40257).
Participants were identified by their representation and voting status in the AFPC SCTMA SIG, with only 1 faculty member per institution serving as a voting member of the group. Thus, 1 faculty member from each of the 10 schools of pharmacy in Canada was invited to participate. SIG members who consented to completing the survey were encouraged to discuss responses with other faculty members at their institution who taught in this area.
The “Self Care Curriculum US Colleges/Schools” survey, which was first used in US colleges and schools of pharmacy, was adapted with permission to assess education on self-care and the expanded role of pharmacist prescribing in a Canadian context. Eight researchers and pharmacists edited the survey to ensure ease of completion, seamless flow, an acceptable length of time for survey completion, appropriate question wording and structure, readability and reliability. Face and content validity were assessed by 5 research investigators through survey pilot testing. The survey was composed of quantitative (e.g., multiple-choice questions and Likert scales) and qualitative (e.g., text entry) measures.
Surveys were distributed electronically via an email attachment to potential participants. Participants returned the completed questionnaire electronically in the same manner to the principal investigator. A reminder email to complete the survey was sent to each participant 1 week before the survey deadline. After surveys were returned, 2 members of the research team contacted participants individually to review responses via a 30- to 60-minute phone interview. The purpose of the interview was to clarify (where needed) and reaffirm the respondent’s position on certain questions. Calls were not recorded, but notes were taken to document the conversations. Responses helped inform the current state of instruction on self-care across Canadian pharmacy curricula.
Two researchers analyzed qualitative data from the survey using thematic coding; follow-up phone interviews were also conducted. Quantitative survey data were summarized using sample frequencies (counts and percentages) and descriptive sample means.
Results
One faculty member from each of the 10 Canadian schools of pharmacy completed the survey (100% response rate). Findings from the survey described self-care course status, content and instructional methodology.
General overview of curricula
All 10 Canadian pharmacy schools instruct on self-care therapies (e.g., nonprescription medicines, nonpharmacological measures). All schools purport that their curriculum adequately prepares graduates to effectively gather relevant information from patients seeking self-care, effectively assess/triage patients seeking self-care and counsel patients on the proper use of nonprescription medications. The majority of schools (90%) report that their curriculum prepares graduates to advise on the proper selection of nonprescription medications, and most schools (80%) prepare graduates to prescribe schedule I drug therapy when indicated and appropriate for patients requiring these services. When considering patients seeking self-care, 80% and 90% of pharmacy schools agree they prepare graduates to effectively assess/triage older adults (≥65 years of age) and younger patients (≤18 years of age), respectively. Moreover, 80% agree that they prepare graduates to tailor interactions and recommendations on nonprescription medications for these 2 patient populations.
Course status of nonprescription medications
All schools agree that the curriculum of an entry-to-practice program (e.g., Doctor of Pharmacy program) should require coursework in nonprescription drug therapy, and 90% of schools believe it should be integrated across all years of the curriculum. Select text responses explaining why schools should mandate nonprescription drug instruction are found as follows:
Essential knowledge for a pharmacist, regardless of practice setting. Pharmacists are the only health care professionals with extensive training in this area.
As a core duty of a pharmacist, OTC drug therapy is a must within a curriculum.
Students have an increasing difficulty recognizing the contextual differences of OTC vs Rx therapy. Due to the Rx-to-OTC movement, more medications are becoming available for minor ailments.
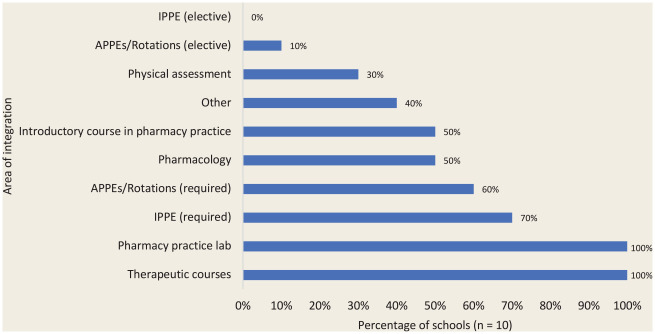
All Canadian pharmacy schools report incorporating nonprescription drug therapy content in their curriculum, of which 70% also incorporate pharmacist prescribing for minor/common ailments. Half of schools do not offer stand-alone nonprescription drug therapy courses in their curriculum, while 20% of schools require 1 course and 30% of schools require 2 or more courses. The number of contact hours spent with students on required self-care coursework focused on nonprescription drug therapy ranges from 13 to 91 hours. The number of contact hours offered as elective coursework in nonprescription drug therapy is less, with 20% of schools offering elective coursework in nonprescription drug therapy, ranging from 26 to 32 hours. In the past 5 years, 40% of schools indicated that their curriculum in nonprescription drug therapy has gained required status, 50% retained required status and 10% lost required status. This content was most commonly placed within therapeutic courses and pharmacy practice labs, followed by introductory pharmacy practice experiences (IPPEs), required advanced pharmacy practice experiences (APPEs)/rotations, introductory courses in pharmacy practice and pharmacology courses (Figure 1).
Figure 1.
Areas of integration of nonprescription drug therapy into Canadian pharmacy school curricula
Course content
Nonprescription drug curricula are overseen by a designated instructor/lead faculty in 60% of Canadian pharmacy schools, all of whom are pharmacists. All pharmacy school curricula educate on the pathophysiology of self-treatable medical conditions, as well as the therapeutics of nonprescription medication, and most (90%) educate on the pharmacology of nonprescription medications. To educate students on properly assessing a patient, formulating a differential diagnosis and triaging, schools use the following information-gathering mnemonics: QuEST/SCHOLAR (60%), PQRSTA (10%) and other methods (60%).
All topic areas and categories of nonprescription therapy that are currently being covered in pharmacy school curricula are presented in Tables 1 and 2, respectively. The top categories of nonprescription therapy and topic areas believed to be core components for a Doctor of Pharmacy program are presented in Table 3.
Table 1.
All self care/ambulatory conditions currently being covered in Canadian pharmacy school curricula
| Topic area | Percentage of schools | Topic area | Percentage of schools |
|---|---|---|---|
| Acne | 100 | Insect bites/stings | 80 |
| Allergic rhinitis | 100 | Lactose intolerance | 50 |
| Atopic dermatitis | 100 | Leg cramps | 20 |
| Allergic contract dermatitis | 90 | Lice | 100 |
| Burns (uncomplicated) | 90 | Low back pain | 80 |
| Calluses and corns | 90 | Musculoskeletal strains and sprains | 90 |
| Common cold | 100 | N&V of pregnancy, unspecified | 80 |
| Complementary and alternative therapies | 60 | Nutritional supplements/herbal remedies | 50 |
| Conjunctivitis: bacterial, viral, allergic | 90 | Obesity | 50 |
| Constipation | 90 | Onychomycosis | 70 |
| Contraception | 90 | Oral aphthous ulcers | 70 |
| Cough | 100 | Oral thrush | 80 |
| Diabetes care | 70 | Oral/dental care | 70 |
| Diaper dermatitis (irritant contact dermatitis, Candida) | 90 | Otic disorders | 90 |
| Diarrhea, noninfectious | 90 | Pinworms and threadworms | 70 |
| Diarrhea, infectious | 90 | Seborrheic dermatitis | 90 |
| Dysmenorrhea | 90 | Shingles | 80 |
| Emergency contraception (oral) | 90 | Sleep disorders, minor | 80 |
| Erectile dysfunction | 80 | Smoking cessation | 100 |
| Eyelid conditions | 70 | Sore throat/pharyngitis | 70 |
| Fever management | 90 | Sunburn/sunscreens | 90 |
| Foot care | 100 | Superficial bacterial skin infections: impetigo and folliculitis | 100 |
| Fungal skin infections (superficial; self-treatable) | 90 | Superficial wound care | 80 |
| Gas/bloating | 70 | Teething | 40 |
| Hair loss | 30 | Tinea corporis infection (ringworm) | 80 |
| Headache | 100 | Tinea cruris skin infection (jock itch) | 80 |
| Heartburn/GERD | 100 | Tinea pedis infection (athlete’s foot) | 90 |
| Hemorrhoids | 100 | UTI (cystitis)—acute, uncomplicated | 90 |
| Herpes labialis (cold sores) | 80 | Urticaria | 70 |
| Home diagnostics | 60 | Vitamins/minerals | 70 |
| Hormonal contraception | 90 | Vulvovaginal candidiasis (vaginal yeast infection) | 90 |
| Impacted ear wax | 60 | Warts (excluding facial and genital) | 100 |
| Infant colic | 80 | Xerophthalmia (dry eyes) | 80 |
| Infant nutrition | 70 | Other | 0 |
| Influenza | 90 |
GERD, gastroesophageal reflux disease; N&V, nausea & vomiting; UTI, urinary tract infection.
Table 2.
All categories of nonprescription therapy currently being covered in Canadian pharmacy school curricula
| Category of nonprescription therapy | Percentage of schools | Category of nonprescription therapy | Percentage of schools |
|---|---|---|---|
| Acne products | 100 | Home testing products | 70 |
| Analgesics/antipyretics | 100 | Homeopathic products | 40 |
| Anthelmintic products | 70 | Incontinence products | 40 |
| Antidiarrheal products | 90 | Insect repellants | 70 |
| Antiemetics | 90 | Male sexual health products | 30 |
| Antiperspirant and deodorant products | 10 | Mouth products | 70 |
| Baby care products | 50 | Musculoskeletal products | 90 |
| Breastfeeding products | 30 | Nutrition products | 70 |
| Constipation products | 90 | Ophthalmic products | 90 |
| Contact lens products | 60 | Oral rehydration products | 70 |
| Contraceptive products | 90 | Ostomy products | 40 |
| Cough/cold/allergy products | 100 | Otic products | 90 |
| Dental products | 50 | Pediculicides | 90 |
| Diabetes products | 70 | Psoriasis products | 90 |
| Feminine care products | 40 | Respiratory products | 60 |
| First aid products | 90 | Scabicides | 90 |
| Foot care products | 90 | Skin products for dermatitis and dry skin | 100 |
| Fungal skin infection products | 80 | Sleep aid products | 70 |
| Heartburn/reflux products | 100 | Smoking cessation products | 100 |
| Hemorrhoid products | 100 | Vitamins and minerals | 60 |
| Herbal/natural health products | 70 | Other | 0 |
Table 3.
Top categories of nonprescription therapy and topic areas believed to be core components for instruction
| Category of nonprescription therapy | Percentage of schools | Topic area | Percentage of schools |
|---|---|---|---|
| Analgesics/antipyretics | 100 | Allergic rhinitis | 100 |
| Cough/cold/allergy products | 100 | Common cold | 90 |
| Heartburn/reflux products | 100 | Heartburn/GERD | 90 |
| Skin products for dermatitis and dry skin | 100 | Smoking cessation | 80 |
| Constipation products | 90 | Constipation | 60 |
| Smoking cessation products | 80 | Headache | 60 |
| Acne products | 50 | Acne | 50 |
| Ophthalmic products | 50 | Atopic dermatitis | 50 |
| Vitamins and minerals | 50 | Vulvovaginal candidiasis (vaginal yeast infection) | 40 |
| Antidiarrheal products | 40 | Conjunctivitis (bacterial, viral, allergic) | 30 |
| Antiemetic products | 40 | Fever management | 30 |
| Herbal/natural health products | 40 | Hemorrhoids | 30 |
| Contraceptive products | 30 | Herpes labialis (cold sores) | 30 |
| First aid products | 30 | Hormonal contraception | 30 |
| Urinary tract infection (cystitis)—acute, uncomplicated | 30 | ||
| Vitamins/minerals | 30 |
GERD, gastroesophageal reflux disease.
All Canadian pharmacy school curricula instruct on NHPs, with the number of contact hours as required coursework varying. Only 20% of schools offer a dedicated course (required or elective) on NHPs, and only 30% of schools feel that this topic is covered in adequate depth.
Course instructional methodology
Various methods of teaching are used to deliver instruction on self-care, with the most common being lectures and use of active learning strategies. Across all schools, the laboratory/experiential components used for nonprescription drug therapy instruction are mock patient interviews/symptom assessments (90%), mock patient counselling on self-care (90%), product demonstrations (60%), nonprescription drug aisle with products (40%), virtual patients (40%), vignettes (20%) and others (40%).
All schools require students to use a textbook in nonprescription drug therapy.
Discussion
Pharmacists’ scope of practice across Canada continues to evolve, including prescriptive authority for select conditions and preventative medicine expanding in most jurisdictions. As such, it is imperative that pharmacy curricula across the country equip students with the knowledge and skills to practise to their optimal scope when caring for patients in this area. More important, lifelong learning skills should be emphasized as a foundational aspect for the profession, as scope of practice evolves and the drug market changes.13 Studies report that pharmacy students are motivated to expand their roles as future pharmacists, to include pharmacist-led services that are patient focused.14 Given this motivation, it is encouraging that all Canadian pharmacy schools claim to adequately prepare students to assess and manage patients seeking self-care and/or expanded pharmacy services. Basic patient assessment and triage skills are a critical component of any self-care curriculum.15 These skills, in addition to active listening, health literacy and culturally safe care, can be nurtured through practice in skills-based labs and final year rotations.16 It is essential that pharmacy graduates are equipped with a framework or thought process that guides their questions during a patient assessment and structures their counselling on these ailments and nonprescription medications. Recognizing that it is impossible to teach everything in a curriculum, students should be able to readily identify and access appropriate resources in practice.
Self-care pharmacy education in Canada is integrated in various ways, such as through required or elective coursework and as stand-alone courses, similar to the variability found across American pharmacy schools.4,15 It has been argued that integration of self-care topics in various therapeutic courses or in pharmacy practice labs, without a stand-alone course on self-care, is inadequate to prepare students for management of these topics in practice.4 The variability in integration of self-care education reflects multiple factors, including school resources, and pharmacist scope of practice as per jurisdiction and faculty members.4,17 When integrated into the curriculum, self-care education is commonly embedded within therapeutic courses, pharmacy practice labs, required IPPEs, required APPEs/rotations, introductory courses in pharmacy practice and pharmacology material. This is strikingly similar to American findings, where it is mainly integrated in therapeutic courses, labs, IPPEs and APPEs.4,15 If pharmacy schools choose to integrate self-care instruction within a curriculum, careful oversight by a lead faculty member or curriculum committee to ensure adequate content coverage is essential.18 In our opinion, early introduction of self-care content is ideal as it exposes students to simpler topics and therapeutic care principles early and provides them with time to apply what they have learned during rotations and build upon this knowledge and skill over the rest of their career.
Various teaching methods are used, with some schools relying more on traditional didactic instruction (lectures), while others emphasize more active learning methods, such as team-based or problem-based learning. It is recommended that traditional teaching methods be combined or replaced with opportunities for active learning and practical application, such as through experiential rotations, to consolidate learning.13,18,19
The core self-care content covered across pharmacy school curricula varies. It is worth noting that several conditions have been approved for pharmacist prescribing in 7 Canadian provinces: dermatitis (atopic mild/moderate eczema, allergic contact and irritant contact), acne (mild to moderate), allergic rhinitis, candidal stomatitis, oral aphthae, hemorrhoids and dysmenorrhea (among others).20 Yet, when asked to rank the top 10 essential core components for instruction, only atopic dermatitis, acne and allergic rhinitis were reported by at least half of pharmacy schools. However, this does not infer that these topics are not covered at all in curricula.
As it stands, some Canadian pharmacy schools feel that pharmacy curricula inadequately cover NHPs, while others are uncertain of the breadth of education provided to students. This parallels findings from a Canadian study that showed most pharmacists feel unequipped to counsel on NHPs, as they relate to drug interactions and adverse effects, even though knowledge of NHPs is an expectation for providing pharmaceutical care.21 This may be due to the inadequacy of formal pharmacy education on NHPs, highlighting a need for more consistent emphasis on its teaching across pharmacy schools. It has been recommended that core competencies for Canadian pharmacy students relating to NHPs include incorporating NHP knowledge in pharmaceutical care, accessing and evaluating NHP-related information from reliable sources and educating patients and other health care professionals on the efficacy and safety of NHPs.21 Additional competencies include familiarity with NHP regulations in Canada and reporting of NHP-related adverse effects to Health Canada.21
Limitations and strengths
Our study provides a valuable description of pharmacy instruction in Canada; however, some limitations should be considered. The survey was only disseminated to 1 SIG member from each faculty; therefore, responses may be limited to that individual’s perspective, especially if responses were not discussed with other faculty members. Further, variability in survey responses is affected by how each faculty structures their program. It was challenging to clearly define the number of contact hours spent on self-care education, especially when it is integrated into courses throughout curricula. Some programs are also in the process of transitioning from a Bachelor of Science in Pharmacy to a Doctor of Pharmacy degree, adding to the challenge in determining the current status of instruction. Follow-up interviews with respondents aided in clarifying some of these details. While our study evaluated pharmacy schools’ self-care teaching tailored to some patient populations, little is known about other vulnerable populations, such as pregnancy and lactation.
Our study also had several strengths. It is the first in Canada to examine the landscape of self-care education across pharmacy schools. The results of the study were a culmination of efforts from faculty members representing each Canadian pharmacy school; thus, all pharmacy schools in Canada were represented. This study supports the SCTMA SIG’s mission in providing a network for pharmacy educators to exchange approaches to self-care education and paves the way for future discussion when designing a self-care curriculum. This study also further supports the SCTMA SIG’s goals in establishing guidelines for best practice in self-care (including nonprescription therapeutics) education. We hope that these findings will help to inform and advance the evolution of self-care curricula across the country, as self-care and minor/common ailments continue to gain attention in the provision of patient-focused health care.
Conclusions and future directions
Although Canadian pharmacy school curricula prepare students to care for patients with minor/common ailments in the community, the variability in the extent of its teaching reflects differences in pharmacy practice in different provinces, as well as factors such as importance attributed to the topic and available space, by the various institutions. As interest in self-care products continues to grow among consumers and as prescriptive authority for pharmacist-led services evolves, pharmacy education must adapt its self-care curricula to meet these demands.
Our initial recommendations for change are outlined in Table 4. In addition, we encourage faculty members representing each Canadian pharmacy school who also serve on the AFPC SCTMA SIG to meet again to discuss strategies for improving and expanding current education in this area. It is our hope that these national curriculum survey findings help to inform curricular reforms and strategic planning for enhancing current pharmacy education. This study will encourage discussion about the importance of self-care education in pharmacy curricula and help to facilitate a national effort to redefine what constitutes an ideal self-care curriculum that positions graduates for success in practice. ■
Table 4.
Deficiencies identified and changes recommended
| Deficiency identified | Recommended change(s) |
|---|---|
| The core self-care content covered across Canadian pharmacy school curricula varies, with a range of 13 to 91 hours total (for required courses). | Establish a minimum number of contact hours and core topics to be covered for nonprescription therapy, prescribing for ambulatory conditions and preventative medicine for an entry-to-practice pharmacy curriculum. However, based on the feedback attained here, we cannot at this time recommend what the minimum content hour standard should be, other than it may lie between 13 and 91 hours. |
| Self-care education in Canada is integrated in various ways, such as through required or elective coursework and as stand-alone courses, similar to the variability found across American pharmacy schools. 4,15 | We believe that both integrated and stand-alone approaches are acceptable ways to deliver self-care content. However, we hope that integration does not weaken its importance within a course. Thus, self-care therapy should preferably be overseen by a designated faculty lead to ensure adequate coverage of self-care topics within the curriculum. |
| Some Canadian pharmacy schools feel that pharmacy curricula inadequately cover natural health products (NHPs), while others are uncertain of the breadth of education provided to students. | Expand the NHP content in pharmacy curricula. |
| Various teaching methods are used, with some schools relying more on traditional didactic instruction (lectures), while others emphasize more active learning methods, such as team-based or problem-based learning. | Encourage faculty to adopt learning methods beyond delivery by didactic lectures. Consider reinforcing self-care material in the final year of pharmacy education during required advanced pharmacy practice experiences (APPEs)/rotations and through formal assessments and evaluations.16 |
| Self-care education varies across Canadian pharmacy curricula, reflecting differences in scopes of practice across provinces, topics of interest and availability of space within curricula by the various faculties. | Develop national teaching and assessment tools to prepare students for prescriptive authority to ensure that curricula remain up-to-date with the ever-evolving self-care landscape and with changing regulations on prescribing in each jurisdiction. |
Acknowledgments
We thank Emily Ambizas, chair of AACP self-care SIG, for sharing the US survey instrument. Colleen Maxwell, Mina Tadrous, Areen Duqoum and Pauline Bal contributed to survey development.
Footnotes
Author’s Note:In this manuscript, we have used the terms self-care and nonprescription medications interchangeably, but we acknowledge that nonprescription medications are just one of the many elements of self-care.
Editor’s Note:While the term minor ailment was used in the survey instrument, we feel that this term may undermine the severity of the illness and the professional importance of pharmacist services and training. Minor ailments are also referred to as common ailments, ambulatory conditions, minor illnesses, self-limiting conditions and self-treatable conditions. In this article, the term ambulatory conditions will be used.
Author Contributions:NN conceived, initiated and supervised the project; NN, EB and JT contributed to the questionnaire development and collected the data; all authors contributed to result synthesis and writing of the manuscript; NN finalized the manuscript with all author approvals.
Funding:This work was partially supported by the Canadian Frailty Network (Technology Evaluation in the Elderly Network), which is supported by the Government of Canada through the Networks of Centres of Excellence (NCE) Program (Grant ID: CAT2017-21).
Declaration of Conflicting Interests:The authors have no conflict of interest to report.
ORCID iD:Nardine Nakhla  https://orcid.org/0000-0001-6066-2522
https://orcid.org/0000-0001-6066-2522
Contributor Information
Nardine Nakhla, School of Pharmacy, University of Waterloo, Waterloo, Ontario.
Emily Black, College of Pharmacy, Dalhousie University, Halifax, Nova Scotia.
Hiba Abdul-Fattah, School of Pharmacy, University of Waterloo, Waterloo, Ontario.
Jeff Taylor, College of Pharmacy and Nutrition, University of Saskatchewan, Saskatoon, Saskatchewan.
References
- 1. Willemsen KR, Harrington GE. From patient to resource: the role of self-care in patient-centered care of minor ailments. SelfCare 2012;3(3):43-55. [Google Scholar]
- 2. Loh EA, Waruszynski MA, Poston J. Cost savings associated with community pharmacist interventions in Canada. Can Pharm J (Ott) 1996;129: 43-7. [Google Scholar]
- 3. Sinopoulou V, Rutter P. Approaches to over-the-counter medications teaching in pharmacy education: a global perspective. Pharm Educ 2019;19: 34-9. [Google Scholar]
- 4. Zierler-Brown SL, VanAmburgh JA, Casper KA, et al. Status and recommendations for self-care instruction in US colleges and schools of pharmacy, 2006. Am J Pharm Educ 2006;70(6):139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nakhla N. QuEST: a quick and effective approach to OTC counselling. Pharm Pract (Canada) 2017;4(1):35-6. [Google Scholar]
- 6. Seubert LJ, Whitelaw K, Hattingh L, Watson MC, Clifford RM. Interventions to enhance effective communication during over-the-counter consultations in the community pharmacy setting: a systematic review. Res Soc Admin Pharm 2018;14(11):979-88. [DOI] [PubMed] [Google Scholar]
- 7. Cavaco AM, Pereira PF. Pharmacists’ counseling protocols for minor ailments: a structure-based analysis. Res Soc Admin Pharm 2012;8:87-100. [DOI] [PubMed] [Google Scholar]
- 8. Taylor J, Rocchi M. The art and science of counselling patients on minor ailments/OTC medicines. Self-Care 2018;9(3):3-22. [Google Scholar]
- 9. Divine H, McIntosh T. Pharmacists’ patient care process in self-care. In: Krinsky DL, ed. Handbook of Nonprescription Drugs. 19th ed. Washington (DC): American Pharmaceutical Association; 2018. [Google Scholar]
- 10. Nakhla N. Pharmacist process for care of the self-treating patient. In: Compendium of therapeutics for minor ailments. Available: https://myrxtx.ca (accessed Aug. 2, 2019).
- 11. Rantucci MJ. Pharmacists talking with patients—a guide to patient counseling. 2nd ed. Philadelphia (PA): Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 12. Rutter P. Community pharmacy: symptoms, diagnosis and treatment. 4th ed. Edinburgh (UK): Elsevier; 2017. [Google Scholar]
- 13. Popovich NG. Nonprescription medication therapy and self-care instruction. Am J Pharm Educ 2006;70(6):136. [Google Scholar]
- 14. Zieck MR, Um IS, Chaar BB. The future of weight management in pharmacy education: perspectives of new generation pharmacists. Curr Pharm Teach Learn 2018;10(5):596-601. [DOI] [PubMed] [Google Scholar]
- 15. Nonprescriptions Medicine Academy Steering Committee; Ambizas EM, Bastianelli KM, Ferreri SP, et al. Evolution of self-care education. Am J Pharm Educ 2014;78(2):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Krypel LL. Constructing a self-care curriculum. Am J Pharm Educ 2006;70(6):140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Taylor JG, Joubert R. Pharmacist-led minor ailment programs: a Canadian perspective. Int J Gen Med 2016;9:291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rose TN, Van Amburgh JA, Miller DM. In the midst of curricular revision, remember the importance of over-the-counter and self-care education. Curr Pharm Teach Learn 2020;12(5):493-5. [DOI] [PubMed] [Google Scholar]
- 19. McFalls M. Integration of problem-based learning and innovative technology into a self-care course. Am J Pharm Educ 2013;77(6):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ontario College of Pharmacists. Expanded scope of practice. Available: https://www.ocpinfo.com/about/key-initiatives/expanded-scope-of-practice (accessed Dec. 12, 2019).
- 21. Byrne A, Boon H, Austin Z, Jurgens T, Raman-Wilms L. Core competencies in natural health products for Canadian pharmacy students. Am J Pharm Educ 2010;74(3):45. [DOI] [PMC free article] [PubMed] [Google Scholar]