Abstract
Background
Helping Babies Breathe (HBB) is a life-saving program that has helped reduce neonatal morbidity and mortality, but knowledge and skills retention after training remains a significant challenge for sustainability of impact. User-centred design (UCD) can be used to develop solutions to target knowledge and skills maintenance.
Methods
We applied a process of UCD beginning with understanding the facilitators of, and barriers to, learning and retaining HBB knowledge and skills. HBB Master Trainers and frontline HBB providers participated in a series of focus group discussions (FGDs) to uncover the processes of skills acquisition and maintenance to develop a mobile application called “HBB Prompt”. Themes derived from each FGD were identified and implications for development of the HBB Prompt app were explored, including feasibility of incorporating strategies into the format of an app. Data analysis took place after each iteration in Phase 1 to incorporate feedback and improve subsequent versions of HBB Prompt.
Results
Six HBB trainers and seven frontline HBB providers participated in a series of FGDs in Phase 1 of this study. Common themes included lack of motivation to practise, improving confidence in ventilation skills, ability to achieve the Golden Minute, fear of forgetting knowledge or skills, importance of feedback, and peer-to-peer learning. Themes identified that were not feasible to address pertained to health system challenges. Feedback about HBB Prompt was generally positive. Based on initial and iterative feedback, HBB Prompt was created with four primary functions: Training Mode, Simulation Mode, Quizzes, and Dashboard/Scoreboard.
Conclusions
Developing HBB Prompt with UCD to help improve knowledge and skills retention was feasible and revealed key concepts, including drivers for successes and challenges faced for learning and maintaining HBB skills. HBB Prompt will be piloted in Phase 2 of this study, where knowledge and skills retention after HBB training will be compared between an intervention group with HBB Prompt and a control group without the app.
Trial registration Clinicaltrials.gov (NCT03577054). Retrospectively registered July 5, 2018, https://clinicaltrials.gov/ct2/show/study/NCT03577054.
Keywords: Newborn resuscitation, Helping babies breathe, Mobile application, Uganda, Simulation, Human factors, User-centred design, mHealth
Background
Despite a significant reduction in global neonatal mortality from 1990 through 2018, approximately 2.5 million newborns die annually. These newborn deaths represent nearly half of the 5.3 million children under five who die each year [1]. The proportion of newborns who contribute to under-five mortality has been growing and the gap between reduction of childhood and infant mortality is rising. This is because strategies for newborn mortality reduction are challenging to implement [2]. The top three causes of newborn deaths continue to be prematurity, intrapartum-related events, and infection [2]. Approximately 10% of babies require help after birth in high-resource settings, compared with 15% in low-resource settings [3, 4]. Skilled personnel who can resuscitate babies immediately after delivery save lives [5, 6]. Standardized training through the Helping Babies Breathe (HBB) program has been shown to improve newborn resuscitation skills [7, 8].
The HBB curriculum, currently in its second edition (HBB 2.0), was designed to train frontline health providers in low-resource settings to provide life-saving interventions for newborns [9]. HBB has been taught in over 80 countries and has been shown to reduce neonatal mortality and morbidity [10]. HBB training materials are standardized with a flowchart that illustrates the steps in the HBB algorithm, accompanied by a facilitator flip chart that provides all the teaching prompts for HBB workshop delivery. The training program emphasizes the practice of individual steps, key skills, and integration of skills into the delivery setting through simulation. Illustrations and a green-yellow–red colour scheme are used to visually guide providers through the HBB algorithm. In Uganda, the HBB program has been deployed with the help of international health implementing partners in collaboration with the Ministry of Health due to the relatively high costs of HBB training [11]. One of the most essential skills HBB teaches is how to ventilate a newborn struggling to breathe, and to start doing so within one minute after birth, referred to as the Golden Minute. Skills deterioration after initial training is a significant barrier to sustained impact of programs like HBB [12]. Low dose high frequency (LDHF) practice, use of simulation, refresher training, and supportive supervision are strategies that help reduce the decay of skills over time [13–17]. However, implementing initial training, refresher training, and supportive supervision are all costly and resource intensive, particularly in settings where births occur at smaller facilities in rural communities spread out over a large geographic region [11]. Since 2010, the Ugandan Ministry of Health alongside implementing partners have been scaling up training for healthcare workers who look after newborns across the country using the HBB program. As of 2014, HBB was offered in more than 40% of health facilities [18].
Mobile health solutions have been increasingly popular as smart devices are ubiquitous. Their rate of ownership in low- and middle-income countries has grown exponentially, with over 5 billion unique users worldwide in 2019 [19], making it especially attractive when designing solutions aiming to reach large audiences [20]. In 2018, there were 19.8 million unique mobile phone users in Uganda, with half of these subscribers using the internet on their mobile phones [21]. This represents mobile internet penetration in 23% of the population. Of these users, only 16% had a smart phone compared with the average of 30% of users having smart phones in Sub-Saharan Africa [21]. Mobile applications have been tested in numerous settings within healthcare and medical education with varying success. Thoughtful development to optimize usability and utility for the target population is important [22–24]. Design processes with iterative prototyping have been successfully used to develop mobile apps for various purposes, such as supporting lifestyle interventions for cardiovascular health [25], clinical decision-making for osteoporosis treatment [26], and self-management for dementia patients [27]. Apps targeted towards newborn health [28–34] have been created and evaluated previously, some employing UCD, but none have informed their design by exploring the cognitive processes of learning newborn resuscitation skills. Understanding the underlying preferences, perceptions, facilitators and barriers that drive behaviours can help tailor the development of features and functions of apps [25, 35, 36]. Applying UCD and assessing human factors during the development of a mobile app can enhance user experience and increase the effectiveness of the tool.
In this paper we describe the UCD process of the development a mobile app (HBB Prompt) to improve knowledge and skills retention after initial HBB training.
Methods
Study overview
The study was conducted at Mbarara University of Science and Technology (MUST) in southwestern Uganda. This article describes Phase 1, the development of HBB Prompt. More details regarding the entire study can be found in the protocol paper [37]. Further details including the focus group discussion (FGD) guides for Phase 1 can be found in Additional file 1 and Additional file 2.
Objectives
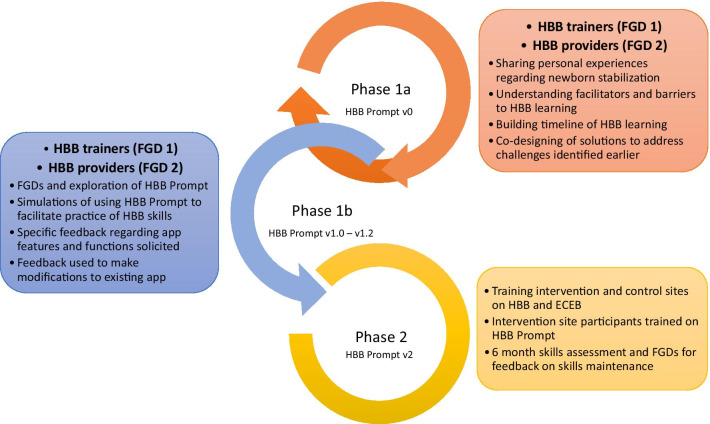
The overall objectives of the study were to apply a UCD framework to develop a mobile app to enhance HBB knowledge and skills maintenance (Phase 1) and to test its effectiveness in a pilot setting (Phase 2). The objective of Phase 1a of the study was to understand the facilitators and barriers to learning and maintaining HBB skills for providers with varying levels of experience with newborn resuscitation. Information from Phase 1a was incorporated into modifications of HBB Prompt version 0 (v0) to create version 1 (v1), which was used in Phase 1b UCD testing. Subsequently, the objective for Phase 1b was to evaluate how HBB Prompt v1 does or does not meet the needs of HBB users and how it could be feasibly improved prior to pilot testing in Phase 2 of this study. See Fig. 1.
Fig. 1.
Overview of HBB Prompt study. The HBB Prompt study is divided into Phase 1, where there were iterative UCD cycles to develop HBB Prompt and Phase 2, where the HBB Prompt app will be piloted. During Phase 1, HBB trainers formed one focus group (FGD 1) and HBB providers formed the second focus group (FGD 2). Each group went through Phase 1a and 1b separately to facilitate UCD of HBB Prompt
Participant recruitment
Participants for Phase 1 were recruited by letter from a register of previously HBB-trained healthcare workers who reside and care for newborns in southwestern Uganda. Participants who responded and who were able to attend the scheduled FGD sessions were included in the study. Inclusion criteria for the first focus group was any healthcare provider with HBB trainer experience (i.e. received previous training in HBB and also completed the HBB Master Trainer Course) allowing them to teach the HBB curriculum. Inclusion criteria for the second focus group was frontline providers who had previously received HBB training.
Phase 1: mobile app development
HBB Prompt v0 development
Study co-investigators collectively used their knowledge and experience with the HBB program, resuscitation education, and mobile app development to create foundational features of HBB Prompt v0. In particular, we sought to leverage strategies that have previously been shown to improve skills retention, including LDHF practice, use of simulation, refresher training, and supportive supervision [10, 38, 39]. This provided a framework for our two software developers to build features of the app that we anticipated HBB trainers and providers would request. The basic functions that were identified as most important were: training videos and information portal, self-practice mode and group simulation mode, knowledge assessments, and a practice dashboard.
The HBB Prompt app is an Android-based application that can run on smart devices with an Android Operating System, Version 4.0.3 and above. The Android platform was chosen due to lower cost and higher penetration of Android devices in Uganda and other low- and middle-income countries. The app was designed using Android Studio 3.0, an Integrated Development Environment provided by Google for design and development of Android apps. HBB Prompt, once installed, does not require internet connectivity; however, when internet connectivity is detected, it automatically logs usage data to a remote Linode server, which it maps according to device International Mobile Equipment Identity (IMEIs). Usage data tracked does not require runtime or dangerous permissions and therefore users do not need to be concerned about access to potentially sensitive data on their accounts. The app does not have access to audio or video recording, the camera function, or location data. Usage data recorded include user identification, date and time of login, time spent on each page of the app, and scores on quizzes or simulations. The app is designed to solely track in-app use, which is intended for education and practice only and not for direct patient care. The logged data can later be exported in comma-separated values (csv) format for further analysis.
Phase 1a
Two separate focus groups underwent the same sequence of exploratory activities: discussion of personal experiences with newborn resuscitation, facilitators and barriers to learning HBB knowledge and skills, perceptions of the timeline in acquisition of knowledge and skills, and generation of ideas on how to maintain and sustain HBB knowledge and skills. The composition of each focus group was primarily divided by HBB training experience so that input could be elicited separately from trainers (FGD 1) and frontline users (FGD 2) of the HBB curriculum. See Additional file 1 for details.
Phase 1b
The same focus groups were invited back to help co-design and provide feedback to improve the HBB Prompt v1. Participants explored the app, simulated use of the app and provided feedback regarding app content, interface, navigation, functionality, customizability, and usability. Two iterations of UCD feedback sessions took place prior to finalizing the app for Phase 2 pilot testing. See Additional file 2 for details.
Analysis
FGDs were recorded and thematic analysis was conducted, where investigators independently coded components of the transcript to highlight needs and mental models of the participants. These independent codes were aggregated and synthesized in order to uncover main themes consistent across investigators. After each iteration, categories and themes were reviewed together with the software developers to incorporate feasible improvements to HBB Prompt.
Results
Participants
The first focus group comprised six HBB trainers who were all physicians and the second focus group comprised seven midwives. Table 1 describes the demographic characteristics of the participants in each FGD, including level of practical and simulated experience with newborn care, emergency training, and comfort with mobile devices.
Table 1.
Focus group participant demographics and characteristics
| HBB trainers (n = 6) | HBB providers (n = 7) | |
|---|---|---|
| Provider type |
Medical Officers = 2 Medical Specialists = 4 |
Enrolled Midwife = 4 Registered Midwife = 3 |
| Years of experience as healthcare provider |
< 5 years = 1 5–10 years = 3 > 10 years = 2 |
< 5 years = 0 5–10 years = 4 > 10 years = 3 |
| Age |
21–30 years old = 1 31–40 years old = 5 |
21–30 years old = 1 31–40 years old = 5 41–50 years old = 1 |
| Sex |
Female = 4 Male = 2 |
Female = 7 Male = 0 |
| Health district | ||
| Ntungamo | 1 | 0 |
| Mbarara | 5 | 7 |
| Level of Health facilitya | ||
| Health Centre III | 0 | 4 |
| Health Centre IV | 0 | 2 |
| Hospital | 6 | 1 |
| Training courses attended | ||
| Helping Babies Breathe (HBB) | 6 | 7 |
| Essential Care for Every Baby (ECEB) | 6 | 5 |
| Essential Care for Small Babies (ECSB) | 4 | 4 |
| Helping Mothers Survive—Bleeding after birth | 2 | 1 |
| Comprehensive Emergency Maternal and Newborn Care (CEMONC) | 1 | 1 |
| Basic Emergency Maternal and Newborn Care (BEMONC) | 0 | 1 |
| Emergency Triage and Treatment (ETAT) | 4 | 1 |
| Master Trainer for HBB | 6 | 2 |
| Experience in last year | ||
| Number of births attended where babies not breathing at birth |
None = 2 1–10 = 2 11–20 = 1 > 20 = 1 |
None = 0 1–10 = 4 11–20 = 1 > 20 = 2 |
| Simulated deliveries with baby not breathing |
None = 0 1–10 = 2 11–20 = 2 > 20 = 2 |
None = 0 1–10 = 4 11–20 = 2 > 20 = 1 |
| Preterm deliveries attended |
None = 1 1–10 = 2 11–20 = 2 > 20 = 1 |
None = 1 1–10 = 5 11–20 = 1 > 20 = 0 |
| Simulated preterm deliveries |
None = 2 1–10 = 3 11–20 = 0 > 20 = 1 |
None = 2 1–10 = 4 11–20 = 0 > 20 = 1 |
| Deliveries attended in the last montha (at the time of first FGD session) | None = 6 |
None = 1 1–10 = 2 11–20 = 3 > 20 = 1 |
| Ownership of smart device |
Yes = 6 No = 0 |
Yes = 6 No = 1 |
| Comfort with using smart device (Likert scale 1–5) |
Not comfortable = 0 Somewhat comfortable = 4 Very comfortable = 2 |
Not comfortable = 1 Somewhat comfortable = 5 Very comfortable = 1 |
aHealth Centre III is a local clinic with access to delivery services and inpatient care, Health Centre IV is a small local hospital
Phase 1a
Exploring personal experience, facilitators and barriers
Themes that emerged from FGDs are summarized in Table 2. Important factors that motivated HBB learning and skills maintenance were supportive supervision and self-esteem. Additionally, continuing medical education opportunities, peer-to-peer learning, refresher courses, and timely feedback were all identified as positive drivers. Barriers identified were lack of equipment and health system issues such as inadequate transport for escalation of care.
Table 2.
Themes to address in HBB learning and skills maintenance during Phase 1a
| Themes | Implications on app development | Selected quotes |
|---|---|---|
| Facilitators | ||
| Peer-to-peer learning |
Design of rater mode to support group practice through simulation Scoreboard/Dashboard feature to keep each other accountable for practice |
“I see [peer learning] as helpful in the HBB training because most of us don’t go on the same pace. They sit in class together but then find that some pick faster and others nothing at all but when you are together in a health facility…we share what I did not get while someone did, so we learn from our friends” |
| Supportive supervision | “helpful when mentors use checklist while giving feedback—so every person knows where they made mistakes and where to keep learning” | |
| Continuing Medical Education and Refresher courses | Repository of HBB information including demonstration videos | |
| Self-confidence | Scoreboard/Dashboard feature to track practice statistics and longitudinal trends of scores on quizzes | “I know I can do some good work and since then I have never lost any other baby and I am glad that HBB did some good work” |
| Timely feedback |
Use of checklists to help review required steps in HBB after simulation completed Rater mode to help facilitate peer-to-peer feedback after simulation |
“If [you] practice the same thing in and out on your own—may not be as effective as having someone to give you feedback, someone with more experience to give you more input on how to improve” |
| Safe learning environment | Use of audio and visual prompts to facilitate different ways of learning | |
| Barriers | ||
| Inadequate or inappropriate resuscitation equipment for practice or for clinical use | Videos to review choice of and maintenance of resuscitation equipment | “We come here to do the training and practice but when we leave this place and go back to our health centres we don’t have what to use. You feel you have the skills, but you don’t have any equipment to use so some of the skills end up dying there.” |
|
Lack of motivation to practice Too much self-pride Lack of support from colleagues to practise together, or to acknowledge and support the importance of practice |
Scoreboard/Dashboard feature to track practice statistics and results of quizzes to encourage friendly competition and keep each other accountable Scoreboard/Dashboard to act as a reminder system to encourage ongoing practice |
|
| Lack of confidence | ||
| Infrequent trainings |
Videos to review individual HBB skills Simulation mode to put knowledge and skills together and applying them to simulated delivery scenario |
|
| Fear of not knowing how to translate skills from a training setting to real life scenarios | Design of simulation mode is to facilitate ongoing practice of skills to best mimic real-life resuscitations | |
Timeline of learning HBB and perceptions of what was difficult to learn and remember
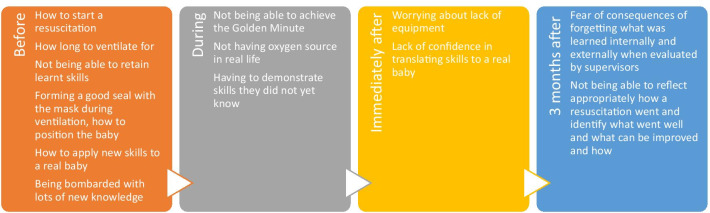
Participants explored the timeline of learning HBB skills and knowledge, including what was perceived as, and what was in reality, the most difficult to learn and remember (Fig. 2). A concern throughout was how to translate skills from a training environment to real-life scenarios. Before HBB training, many concerns surrounded learning about the steps to help a baby breathe and the fear of not retaining skills. During HBB training, there was fear of not achieving the Golden Minute. Three months after training, participants were worried about forgetting their skills and not effectively debriefing to improve after a resuscitation.
Fig. 2.
Insights about the timeline in HBB learning and skills maintenance during Phase 1a. Themes from FGDs with HBB trainers and providers regarding their thought process in relationship to the timing of HBB training
Co-designing solutions
Prior to being exposed to HBB Prompt v0, participants were asked to co-design solutions to help learn and maintain HBB skills. They identified promoting a safe learning environment as an important goal. To achieve this, suggestions emphasized the use of audio and visual prompts and written and video guides to facilitate different ways of learning. To counteract the inertia to practise, methods of motivating users were discussed, including setting reminders, promoting champions, having dedicated group practice sessions, and creating a friendly competitive environment to increase accountability. Participants also expressed the importance of a community of support, for example, through a message board or group chat to review cases and to encourage each other. Suggested mobile app features included information for each HBB skill (introduction, video demonstration, practice prompts, scenarios, and if possible, ability to provide feedback) and the ability to function offline as internet connectivity can often be unreliable.
Implications on app development
Themes that were not feasible to address using a mobile app included health system challenges such as lack of available equipment and transport for escalation of care for unstable babies. Additionally, due to limited funds to facilitate real-time internet connectivity of the app, the reminders, group chat and message board functions were not implemented. Otherwise, many themes identified in the FGDs were anticipated by the authors and already addressed by features in HBB Prompt v0.
Functions and features of the HBB Prompt v0 and modifications based on Phase 1a
Figure 3 shows screen shots of HBB Prompt v1 and Table 3 describes the features of HBB Prompt. Training mode was designed to demonstrate each step of the HBB algorithm through videos, aimed as a resource for refreshing knowledge and skills. In response to concerns about lack of equipment, a video demonstrating how to reprocess and maintain equipment was added. Other feedback from Phase 1a helped inform the video content, such as breaking down skills into digestible steps and troubleshooting when effective ventilation is not being achieved.
Fig. 3.
HBB Prompt v1.0 screenshots. a different scenarios users can choose from in Simulation Mode. b Performance checklist that appears once a simulation is complete. c Beginning of a simulation. Note the two countdown timers from the time the simulation begins and the time when the simulated infant is born. d Sample of dashboard statistics
Table 3.
HBB Prompt app features during Phase 1b
| App function | Description | Rationale for inclusion |
|---|---|---|
| Training videos | Series of training videos outlining the steps in HBB (Preparation for birth, Routine care, Golden Minute without ventilation, Golden Minute with ventilation, Golden Minute with normal or slow heart rate) | Videos to serve as review materials, with ability to visualize skills that are being demonstrated |
| Simulation mode—alone mode |
Option of targeting practice to a specific scenario that an individual user chooses versus a random scenario that is chosen from the pool of standard scenarios (Preparation for birth, Routine care, Golden Minute without ventilation, Golden Minute with ventilation, Golden Minute with normal or slow heart rate) Audio and visual cues that accompany the scenario that are timed to simulate an actual delivery |
To help prompt users through simulated delivery scenarios to facilitate in context practice of skills |
| Simulation mode—rater mode | Same as alone mode except that the designated rater has a checklist available to review |
To help prompt an observer to assess how well the user completes steps in the HBB algorithm in response to the prompts provided about the baby’s condition To help facilitate team practice and peer-to-peer learning of HBB skills and to assist the rater to systematically give targeted feedback |
| Quizzes/Knowledge Check | Sets of quizzes with questions generated from the HBB curriculum |
To help reinforce knowledge pertaining to the steps and reasoning for actions within the HBB algorithm To address the fear of forgetting knowledge learned after initial training |
| Scoreboard/Dashboard | Visual tracker providing trends regarding practice frequency and knowledge assessment scores |
Information to serve as an external motivator to practise regularly and perform as well if not better than peers To increase accountability for practising and increase confidence in resuscitation skills with increased practice |
Simulation mode was designed to facilitate routine practice of HBB skills, running through various scenarios that emphasize different aspects of resuscitation. Simulation mode was divided into alone mode (for individual practice) and rater mode (for group practice or peer-to-peer learning). This feature encourages and supports LDHF training. Consistent practice and increased familiarity and confidence in carrying out the steps of the Golden Minute enable HBB providers to perform all actions within one minute of a baby’s birth. To support this, timer prompts were built into simulation mode to facilitate practice of the Golden Minute. Furthermore, checklists were added at the end of every simulation to help users debrief what went well and what could be improved.
The Quizzes and knowledge check section was designed to help refresh and consolidate knowledge about the HBB algorithm and rationale for steps in resuscitation, providing real-time feedback regarding information retention.
The Scoreboard/Dashboard was created to increase accountability and motivation, encourage all users to practise HBB consistently, and foster confidence by displaying personal performance benchmarks.
Phase 1b
Table 4 summarizes the feedback that was received during Phase 1b and outlines modifications that were made, where possible, in response to the suggestions from the FGDs. Feedback about HBB Prompt was generally positive and navigation was felt to be overall intuitive. There were two iterations of Phase 1b (one with FGD1 and the other with FGD2). After suggestions were incorporated, the team was satisfied that the HBB Prompt app was ready for deployment in Phase 2 for pilot testing.
Table 4.
Summary of feedback for HBB Prompt during Phase 1b
| Feedback | Modifications made | Selected quotes |
|---|---|---|
| Likes | ||
|
Content flows well and is consistent with the HBB curriculum Can complement use of the HBB flip chart during HBB training Can serve well as a refresher training program |
Included additional practical recommendations, such as, when to refer infants for advanced care, how to cut and trim the cord length, how to keep the baby warm |
“You can use it on a daily basis and at any time. You don’t have to wait for a workshop, or organized day.” “I am satisfied that this is a dream come true. The last time we met, we had ideas but did not know how that would be incorporated in an app, and I am hoping the developers carry it farther, and avail it as quickly as they could.” |
| Training videos comprehensive, realistic and highlighted relevant materials from HBB | Supplemented training videos with text to facilitate review | |
| Demonstration in video of preparation for birth and testing of equipment in front of family—helps promote transparency and confidence in newborn resuscitation process | Kept this video as a part of the app to help encourage this process of transparency | |
|
Quizzes were useful for review, gave immediate feedback and can be useful tool for teaching Random order of questions helped users not relying on memory alone |
Some technical flaws noted that were fixed, for example unsaved answers and needing to redo the entire quiz when users tapped the screen in any incorrect place Added a review feature where answers that are correct and answers that were marked are shown to provide feedback to users |
|
|
Simulation mode was helpful for self-practice and group practice Audio and visual prompts were effective |
Fixed flaws in orientation of images and timing of prompts |
“Yes, it will help us practice with our colleagues. For instance, if you are helping someone who does not know, the video guides you and helps you know what do to next, if you forget. It also helps to time you.” “I think the videos helped us, because it directs you on what to do. Because if they kept saying the baby is not breathing, you would know what to do and keep doing it, ‘till the baby breathes.” |
| Dislikes | ||
| Lack of consistency throughout the app (e.g. how prompts are given, audio for crying, where the baby is being resuscitated in the videos) |
Modified videos and simulations to use the same prompts In the HBB curriculum timing of cutting the cord, and location of where the baby should be during ventilation (near mother, or on a separate surface) is left up to the discretion of the facilitators teaching in their own setting. For simplicity, decision made to only show ventilation near the mother rather than specifying location depending on the status of the baby |
|
| Some aspects of the training videos were not as realistic, such as the timing with certain actions being too slow | Modified videos to be more realistic and modified timing of transitions in simulation mode | |
| Font size and menu options at times not clear | Modified text size and colour scheme to improve visibility | |
| Navigation—suggestion for a restart button in simulation mode | Added pause button (restart feature with back button) | |
| General comments and suggestions | ||
| Using the same HBB curriculum colour scheme of Green, Yellow and Red may help reinforce learning by means of a visual prompt | Added HBB colour scheme in different parts of HBB Prompt content | |
| For training videos different viewing angles to better capture the details of the actions (e.g. mask seal in bagging) | Decision made not to re-film the videos due to time constraints in filming and editing | |
| For the Dashboard, use of real names vs. aliases was debated | Consensus was to use real names | |
| Customizability | ||
| Consideration of creating animated videos rather than filming individuals—may allow more flexibility if the app scales to different settings | Not feasible to create animations to address this need within the study time line available | |
| Including locally relevant practices even if it is not a part of the standard HBB protocol—e.g. asking birth attendants to have bed sheets available for baby in the preparation for birth section as this is common place throughout Uganda, but may not be in other settings | Decision made not to add customized recommendations and adhere to what is presented in the HBB curriculum | |
Discussion
In Phase 1 of this study, we applied a UCD framework and engaged a group of HBB trainers and providers to develop a mobile app, HBB Prompt, to improve knowledge and skills retention after initial HBB training. Many facilitators and barriers identified were feasible to address with HBB Prompt and reflected anticipated features based on prior knowledge about contributors to skills decay. Participants expressed positive perceptions of the app’s ability to help users practise and maintain HBB knowledge and skills.
Strengths
HBB Prompt is a novel mobile app that facilitates simulation of newborn resuscitation to promote deliberate practice of applying the HBB algorithm to real-life scenarios. We employed a cooperative design UCD framework, which prioritized participation from frontline end-users, both trainers and learners of HBB, since failure of adoption of healthcare technology has been attributed to absence of end-user input [40]. There are different methods to involve end-users in the design and evaluation process, with prototyping and simulation being commonly used in design, and focus groups and observations being common evaluative methods [41]. Understanding the usability of a mobile app and how it meets needs and addresses gaps to improve outcomes have been key to the successful adoption of health technologies. UCD and understanding human factors is crucial since certain ideas may not translate well into a mobile app. Understanding the needs of primary users by exploring acquisition and maintenance of skills and knowledge helped map out areas where HBB Prompt can assist and remaining gaps that need to be addressed through other means [40]. Each function of HBB Prompt was vetted during Phase 1b and largely addressed the issues that were uncovered during Phase 1a.
By iterative testing through participatory design and evaluation, we hoped to overcome the common barrier of failed interventions due to lack of user input. Since the main goal of designing HBB Prompt is to improve knowledge and skills retention after initial HBB training, the UCD process specifically focused on HBB trainer and trainee experiences regarding the process of learning HBB skills and the daily challenges of implementing those skills. We used FGDs to better understand when different cognitive processes took place, influencing our strategies for knowledge and skills retention, a method supported by the applied cognitive task analysis [42]. This strategy has been successful in developing apps for various purposes in healthcare [25, 43, 44], including those in the maternal newborn health domain [29, 32–34, 42].
Newborn health apps [28, 34] have been developed to support HBB training by provision of HBB reference material and clinical decision support. HBB Prompt builds on that foundation and adds new features including Simulation mode and the Scoreboard/Dashboard, which aim to promote LDHF practice. NeoTree [29] is a mobile application developed in a single neonatal unit in Malawi using similar methodology as HBB Prompt, but was intended for data capture of neonatal admissions and clinical decision support. The authors used focus groups to better understand acceptability and feasibility of mobile health (mHealth) solutions before and after implementation of NeoTree. The positive impact of the NeoTree app was attributed to UCD and coproduction. HBB Prompt, on the other hand, applies UCD to create and fine-tune the features deployed in the app. Finally, HBB Prompt builds on the success of the Safe Delivery App (SDA) [30]. The SDA [30] contains education material and videos based on the United Nations Basic Emergency Obstetric and Neonatal Care program (BEMONC) and was evaluated in a large cluster-randomized trial in Ethiopia, which found improved knowledge and skills retention and a statistically non-significant 24% reduction in perinatal mortality. HBB Prompt shares many features with SDA, including video and text as educational materials. HBB Prompt goes beyond the reference tool function by supporting simulation-based skills practice, an interactive feature developed with UCD based on FGD themes of the importance of simulation and peer-to-peer learning. Furthermore, HBB Prompt contains a knowledge assessment feature, which was not available in the early version of the SDA that was tested in the cluster-randomized trial.
Facilitating simulation
Our app design was informed by the principles of deliberate practice, a well-established methodology for simulation-based medical education [17]. HBB Prompt differs from available apps because it facilitates hands-on practice and simulation, which is a core component of the HBB 2.0 curriculum. While simulated resuscitation will differ from real-life scenarios, consistent practice through simulation is an effective method to maintain competency in managing high-acuity low-occurrence events, such as apnea in a newborn [16, 38]. Much of HBB Prompt’s design focus was to facilitate users’ ability to practise HBB skills in short, directed ways, either alone or with peers. LDHF practice of specific skills such as bag-mask ventilation has been shown to be effective in enhancing skills retention after training [10, 38, 45, 46]. For individuals who are unable practise skills with others, the Training mode videos serve as a guide, and the function of Simulation—alone mode provides a structure and framework whereby users can benchmark their skills and receive automated external prompts and feedback in order to retain their resuscitation skills.
Use of motivation/behaviour change strategies
The Scoreboard/Dashboard feature was designed to track trends in scores on quizzes, and participants felt it would foster confidence in knowledge retention and increase awareness of knowledge gaps. Being able to visualize frequency and practice patterns serves to increase ownership and accountability for practising as it is a visual audit, providing feedback to each user about habits of practice and where skills may be adequate or lacking [47, 48]. Besides having visual statistics that may benefit end-users, this feature was built to also track app function usage to provide insight in Phase 2 of the study to improve the app and assess which parts of the HBB 2.0 curriculum require more reinforcement. Benchmarking to help healthcare providers inform behaviour change is supported by Social Comparison Theory and Reference Group Theory and has been shown to be a successful strategy to motivate behaviour change [48]. The display of longitudinal trends provides ongoing feedback and is supported by the Feedback Intervention Theory [48]. The Scoreboard/Dashboard feature is unique to HBB Prompt compared with other apps in the newborn mHealth space and evaluating its effectiveness during Phase 2 will further enhance understanding of how audit and feedback can increase retention of knowledge and skills after training.
Limitations
Although we recruited a diverse group of participants, we may have missed some perspectives. One limitation is the absence of larger scale beta-testing prior to deployment in Phase 2. For example, Bucher et al. invited a large group of users to download and beta-test their app, and provide feedback through a UCD questionnaire [34]. However, the size of our FGDs allowed in-depth exploration and likely uncovered input to reach theme saturation. HBB Prompt’s user interface and functions may be less intuitive for potential users who are less familiar with use of technology as all but one participant (in the HBB provider group) owned a smart device and described themselves as comfortable with their use. Even though the target audience for HBB Prompt are those who were previously HBB trained, including input from first-time learners of the curriculum could have provided additional insight to the knowledge and skills acquisition and retention process. There was an intention to recruit a third focus group with naïve HBB learners; however, due to logistical constraints, we were unable to run a separate series of focus groups with pre-service trainees (medical students and nursing students). On the other hand, our in-depth FGDs solicited input from two groups of HBB users with various experiences that are representative of HBB providers in Uganda, where there is a national mandate for all frontline providers to be trained in both HBB and ECEB. Participant experiences, perceptions, and input through the UCD process were likely generalizable to HBB providers in Uganda and translatable to similar resource settings. Recent clinical and simulation experience were similarly variable across both HBB facilitators and HBB providers, which allowed us to capture opinions that would reflect those with differential exposure to deliveries requiring HBB skills.
While our goal of soliciting input from different types of end-users uncovered many themes that were feasible to address with a mobile app, there are additional limitations to consider. App features addressed intrinsic factors such as motivation and confidence, but not health system constraints, which were frequently cited as barriers. Another challenge of UCD is balancing implementation of suggestions and prolonging the timeline of app development. For example, although Simulation—rater mode was felt to work well, having the ability to link two devices so that the user and the rater could engage in the simulation on different screens would have further enhanced its function but this was technically not feasible given the time constraint of the study. Although customization was requested during feedback, it was important to consider how to be specific enough without reducing generalizability. Keeping the app content close to the HBB curriculum would allow it to scale to other settings more easily.
Conclusion
With the ubiquity of mobile devices, apps that are carefully designed and evaluated have the potential to scale rapidly and reach a broad audience to effect large scale change. HBB Prompt was developed with UCD input from HBB trainers and providers to tailor its design to support knowledge and skills maintenance after HBB training. HBB Prompt features were built to address themes uncovered, which included motivation to practise, confidence in knowledge or skills, importance of feedback and peer-to-peer learning. The iterative process of incorporating feedback further improved the features and functions of HBB Prompt as a practice tool to facilitate skills and knowledge retention. Pilot-testing of HBB Prompt in Phase 2 of this study will further evaluate the ability of this UCD process to build a mobile tool to address the important issue of increasing sustainability of HBB training.
Supplementary Information
Additional file 1. HBB Prompt Phase 1a Focus Group Guide Plan and Standard Operating Procedures. Focus group guide with operational details, questions and prompts used to conduct focus group discussions during Phase 1a.
Additional file 2. HBB Prompt Phase 1b Focus Group Guide Plan and Standard Operating Procedures. Focus group guide with operational details, questions and prompts used to conduct focus group discussions during Phase 1b.
Acknowledgements
The authors would like to acknowledge Mukama Martin and Openja Moses for their contributions as the software developers of HBB Prompt, Tumwesigye Paul for his efforts as research assistant and Dr. Diego Bassani for his assistance in study planning. Additionally, the authors acknowledge the innovation design process of the Consortium for Affordable Medical Technologies in Uganda (CAMTech Uganda) that enabled the development of the HBB Prompt App using UCD approaches. The authors acknowledge Sabrina Kernerman for her assistance in editing.
Abbreviations
- AAP
American Academy of Pediatrics
- app
Application
- BEMONC
Basic Emergency Obstetric and Neonatal Care
- CEMONC
Comprehensive Emergency Maternal and Newborn Care
- csv
Comma-separated values
- ECEB
Essential Care for Every Baby
- ECSB
Essential Care for Small Babies
- ETAT
Emergency Triage and Treatment
- FGD
Focus group discussions
- HBB
Helping Babies Breathe
- IMEI
International Mobile Equipment Identity
- LDHF
Low-dose high frequency
- mHealth
Mobile health
- MUST
Mbarara University of Science and Technology
- REC
Research Ethics Committee
- REB
Research Ethics Board
- SDA
Safe Delivery App
- UCD
User centred design
- v0
Version 0
Authors’ contributions
NC, SD, HM, and SM conceived of the study. NC drafted the manuscript. NC, SD, and RK analyzed the data. All authors participated in the design of the study, revised the manuscript critically for intellectual content, and have read and approved the final manuscript.
Funding
This study was funded by a grant from the Grand Challenges Canada Stars in Global Health program, R-ST-POC-1707-07454. The funder had no role in any aspect of the study.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was approved by the Research Ethics Board at The Hospital for Sick Children (SickKids) (REB No. 1000059992) and MUST Research Ethics Committee (REC No. 16/09-17) and registered at Clinicaltrials.gov (NCT03577054). All participants provided written informed consent for this study.
Consent for publication
Not applicable.
Competing interests
Santorino Data is a co-creator of the Augmented Infant Resuscitator, which is used in Phase 2 of this study. All other authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Natalie Hoi-Man Chan, Email: natalie.chan@cw.bc.ca.
Hasan S. Merali, Email: meralih@mcmaster.ca
Niraj Mistry, Email: niraj.mistry@mail.utoronto.ca.
Ryan Kealey, Email: ryan.kealey@gmail.com.
Douglas M. Campbell, Email: Douglas.Campbell@unityhealth.to
Shaun K. Morris, Email: shaun.morris@sickkids.ca
Santorino Data, Email: sdata@must.ac.ug.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12911-021-01406-z.
Reference
- 1.UNICEF. Levels and trends in child mortality—report 2019. 2019, p. 1–52. https://childmortality.org/wp-content/uploads/2019/10/UN-IGME-Child-Mortality-Report-2019.pdf.
- 2.Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, et al. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the sustainable development goals. Lancet. 2016;388(10063):3027–3035. doi: 10.1016/S0140-6736(16)31593-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kamath-Rayne BD, Berkelhamer SK, Ashish KC, Ersdal HL, Niermeyer S. Neonatal resuscitation in global health settings: an examination of the past to prepare for the future. Pediatr Res. 2017;82(2):194–200. doi: 10.1038/pr.2017.48. [DOI] [PubMed] [Google Scholar]
- 4.Ersdal HL, Mduma E, Svensen E, Perlman JM. Early initiation of basic resuscitation interventions including face mask ventilation may reduce birth asphyxia related mortality in low-income countries: a prospective descriptive observational study. Resuscitation. 2012;83(7):869–873. doi: 10.1016/j.resuscitation.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 5.Wyckoff MH, Aziz K, Escobedo MB, Kapadia VS, Kattwinkel J, Perlman JM, et al. Part 13: neonatal resuscitation: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint) Pediatrics. 2015;136(Suppl 2):S196–S218. doi: 10.1542/peds.2015-3373G. [DOI] [PubMed] [Google Scholar]
- 6.Ariff S, Lee AC, Lawn J, Bhutta ZA. Global burden, epidemiologic trends, and prevention of intrapartum-related deaths in low-resource settings. Clin Perinatol. 2016;43(3):593–608. doi: 10.1016/j.clp.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Msemo G, Massawe A, Mmbando D, Rusibamayila N, Manji K, Kidanto HL, et al. Newborn mortality and fresh stillbirth rates in Tanzania after helping babies breathe training. Pediatrics. 2013;131(2):e353–e360. doi: 10.1542/peds.2012-1795. [DOI] [PubMed] [Google Scholar]
- 8.Goudar SS, Somannavar MS, Clark R, Lockyer JM, Revankar AP, Fidler HM, et al. Stillbirth and newborn mortality in India after helping babies breathe training. Pediatrics. 2013;131(2):e344–e352. doi: 10.1542/peds.2012-2112. [DOI] [PubMed] [Google Scholar]
- 9.Kamath-Rayne BD, Thukral A, Visick MK, Schoen E, Amick E, Deorari A, et al. Helping babies breathe, second edition: a model for strengthening educational programs to increase global newborn survival. Glob Health Sci Pract. 2018;6(3):538–551. doi: 10.9745/GHSP-D-18-00147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris SM, Fratt EM, Rodriguez J, Ruman A, Wibecan L, Nelson BD. Implementation of the helping babies breathe training program: a systematic review. Pediatrics. 2020;146(3):e20193938. doi: 10.1542/peds.2019-3938. [DOI] [PubMed] [Google Scholar]
- 11.Chaudhury S, Arlington L, Brenan S, Kairuki AK, Meda AR, Isangula KG, et al. Cost analysis of large-scale implementation of the ‘Helping Babies Breathe’ newborn resuscitation-training program in Tanzania. BMC Health Serv Res. 2016;16(1):681. doi: 10.1186/s12913-016-1924-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reisman J, Arlington L, Jensen L, Louis H, Suarez-Rebling D, Nelson BD. Newborn resuscitation training in resource-limited settings: a systematic literature review. Pediatrics. 2016;138(2):e20154490. doi: 10.1542/peds.2015-4490. [DOI] [PubMed] [Google Scholar]
- 13.Cordova E, Al-Rousan T, Castillo-Angeles M, Aftab S, Nelson BD. Effect of low-cost interventions on the retention of knowledge and skills following Helping Babies Breathe training. Int J Gynaecol Obstet. 2018;142(2):248–254. doi: 10.1002/ijgo.12512. [DOI] [PubMed] [Google Scholar]
- 14.Mduma E, Ersdal H, Svensen E, Kidanto H, Auestad B, Perlman J. Frequent brief on-site simulation training and reduction in 24-h neonatal mortality—an educational intervention study. Resuscitation. 2015;93:1–7. doi: 10.1016/j.resuscitation.2015.04.019. [DOI] [PubMed] [Google Scholar]
- 15.Bang A, Patel A, Bellad R, Gisore P, Goudar SS, Esamai F, et al. Helping Babies Breathe (HBB) training: what happens to knowledge and skills over time? BMC Pregnancy Childbirth. 2016;16(1):364. doi: 10.1186/s12884-016-1141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tabangin ME, Josyula S, Taylor KK, Vasquez JC, Kamath-Rayne BD. Resuscitation skills after Helping Babies Breathe training: a comparison of varying practice frequency and impact on retention of skills in different types of providers. Int Health. 2018;10(3):163–171. doi: 10.1093/inthealth/ihy017. [DOI] [PubMed] [Google Scholar]
- 17.Cheng A, Nadkarni VM, Mancini MB, Hunt EA, Sinz EH, Merchant RM, et al. Resuscitation education science: educational strategies to improve outcomes from cardiac arrest: a scientific statement from the American Heart Association. Circulation. 2018;138(6):e82–e122. doi: 10.1161/CIR.0000000000000583. [DOI] [PubMed] [Google Scholar]
- 18.Kak L, Johnson J, McPherson R, Keenan W, Schoen E, editors. Helping Babies Breathe—lessons learned guiding the way forward. Washington, DC: Helping Babies Breathe Global Development Alliance; 2015. pp. 1–116. [Google Scholar]
- 19.Feroz A, Jabeen R, Saleem S. Using mobile phones to improve community health workers performance in low-and-middle-income countries. BMC Public Health. 2020;20(1):49. doi: 10.1186/s12889-020-8173-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bastawrous A, Armstrong MJ. Mobile health use in low- and high-income countries: an overview of the peer-reviewed literature. J R Soc Med. 2013;106(4):130–142. doi: 10.1177/0141076812472620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Okeleke K. Uganda: Driving inclusive socio-economic progress through mobile-enabled digital transformation. London: GSMA; 2019. pp. 1–56. [Google Scholar]
- 22.Labrique AB, Vasudevan L, Kochi E, Fabricant R, Mehl G. mHealth innovations as health system strengthening tools: 12 common applications and a visual framework. Glob Health Sci Pract. 2013;1(2):160–171. doi: 10.9745/ghsp-d-13-00031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siedner MJ, Santorino D, Lankowski AJ, Kanyesigye M, Bwana MB, Haberer JE, et al. A combination SMS and transportation reimbursement intervention to improve HIV care following abnormal CD4 test results in rural Uganda: a prospective observational cohort study. BMC Med. 2015 doi: 10.1186/s12916-015-0397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siedner MJ, Santorino D, Haberer JE, Bangsberg DR. Know your audience: predictors of success for a patient-centered texting app to augment linkage to HIV care in rural Uganda. J Med Internet Res. 2015;17(3):e78–e78. doi: 10.2196/jmir.3859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewer LC, Hayes SN, Caron AR, Derby DA, Breutzman NS, Wicks A, et al. Promoting cardiovascular health and wellness among African-Americans: community participatory approach to design an innovative mobile-health intervention. PLoS ONE. 2019;14(8):e0218724. doi: 10.1371/journal.pone.0218724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krueger RA, Casey MA. Focus groups: a practical guide for applied research. 4. Los Angeles: SAGE; 2009. [Google Scholar]
- 27.Øksnebjerg L, Woods B, Waldemar G. Designing the ReACT app to support self-management of people with dementia: an iterative user-involving process. Gerontology. 2019;65(6):673–685. doi: 10.1159/000500445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Prakash V, Thukral A, Sankar MJ, Agarwal RK, Paul VK, Deorari AK. Efficacy and acceptability of an ‘App on sick newborn care’ in physicians from newborn units. BMC Med Educ. 2016;16(1):84. doi: 10.1186/s12909-016-0579-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Crehan C, Kesler E, Nambiar B, Dube Q, Lufesi N, Giaccone M, et al. The NeoTree application: developing an integrated mHealth solution to improve quality of newborn care and survival in a district hospital in Malawi. BMJ Glob Health. 2019;4(1):e000860–e912. doi: 10.1136/bmjgh-2018-000860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lund S, Boas IM, Bedesa T, Fekede W, Nielsen HS, Sørensen BL. Association between the safe delivery app and quality of care and perinatal survival in Ethiopia. JAMA Pediatr. 2016;170(8):765–767. doi: 10.1001/jamapediatrics.2016.0687. [DOI] [PubMed] [Google Scholar]
- 31.Chan NH, Mistry N, Campbell DM. A simulation-based pilot study of a mobile application (NRP prompt) as a cognitive aid for neonatal resuscitation training. Simul Healthc J Soc Simul Healthc. 2019;14(3):146–156. doi: 10.1097/SIH.0000000000000353. [DOI] [PubMed] [Google Scholar]
- 32.Amoakoh HB, Klipstein-Grobusch K, Ansah EK, Grobbee DE, Yveoo L, Agyepong I. How and why front-line health workers (did not) use a multifaceted mHealth intervention to support maternal and neonatal healthcare decision-making in Ghana. BMJ Glob Health. 2019;4(2):e001153–e1214. doi: 10.1136/bmjgh-2018-001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schaeffer LE, Ahmed S, Rahman M, Whelan R, Rahman S, Roy AD, et al. Development and evaluation of a mobile application for case management of small and sick newborns in Bangladesh. BMC Med Inform Decis Mak. 2019;19(1):116. doi: 10.1186/s12911-019-0835-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bucher S, Meyers E, Kshatriya BSA, Avanigadda PC, Purkayastha S. Development of an innovative mobile phone-based newborn care training application. In: Abraham A, Gandhi N, Pant M, editors. innovations in bio-inspired computing and applications. Cham: Springer; 2019. pp. 361–374. [Google Scholar]
- 35.Schnall R, Rojas M, Bakken S, Brown W, Carballo-Dieguez A, Carry M, et al. A user-centered model for designing consumer mobile health (mHealth) applications (apps) J Biomed Inform. 2016;60:243–251. doi: 10.1016/j.jbi.2016.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Couture B, Lilley E, Chang F, DeBord SA, Cleveland J, Ergai A, et al. Applying user-centered design methods to the development of an mHealth application for use in the hospital setting by patients and care partners. Appl Clin Inform. 2018;09(02):302–312. doi: 10.1055/s-0038-1645888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merali HS, Chan NH-M, Mistry N, Kealey R, Campbell D, Morris SK, et al. Designing and evaluating a novel mobile application for Helping Babies Breathe skills retention in Uganda: comparative study protocol. BMJ Paediatr Open. 2019;3(1):e00561. doi: 10.1136/bmjpo-2019-000561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ugwa E, Kabue M, Otolorin E, Yenokyan G, Oniyire A, Orji B, et al. Simulation-based low-dose, high-frequency plus mobile mentoring versus traditional group-based trainings among health workers on day of birth care in Nigeria; a cluster randomized controlled trial. BMC Health Serv Res. 2020;20(1):586. doi: 10.1186/s12913-020-05450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eblovi D, Kelly P, Afua G, Agyapong S, Dante S, Pellerite M. Retention and use of newborn resuscitation skills following a series of helping babies breathe trainings for midwives in rural Ghana. Glob Health Act. 2017;10(1):1–6. doi: 10.1080/16549716.2017.1387985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kushniruk A, Nøhr C. Participatory design, user involvement and health IT evaluation. In: Ammenwerth E, Rigby M, editors. Evidence-based health informatics: promoting safety and efficiency through scientific methods and ethical policy. Amsterdam: IOS Press; 2016. pp. 139–151. [PubMed] [Google Scholar]
- 41.Scott PJ. Mixed methods: a paradigm for holistic evaluation of health IT. In: Ammenwerth E, Rigby M, editors. Evidence-based health informatics: promoting safety and efficiency through scientific methods and ethical policy. Amsterdam: IOS Press; 2016. pp. 102–113. [PubMed] [Google Scholar]
- 42.Pickup L, Lang A, Shipley L, Henry C, Carpenter J, McCartney D, et al. Development of a clinical interface for a novel newborn resuscitation device: human factors approach to understanding cognitive user requirements. JMIR Hum Factors. 2019;6(2):e12055–e12113. doi: 10.2196/12055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stinson JN, Lalloo C, Harris L, Isaac L, Campbell F, Brown S, et al. iCanCope with PainTM: user-centred design of a web- and mobile-based self-management program for youth with chronic pain based on identified health care needs. Pain Res Manag. 2014;19(5):257–265. doi: 10.1155/2014/935278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Simpson AJ, Honkoop PJ, Kennington E, Snoeck-Stroband JB, Smith I, East J, et al. Perspectives of patients and healthcare professionals on mHealth for asthma self-management. Eur Respir J. 2017;49(5):1601966. doi: 10.1183/13993003.01966-2016. [DOI] [PubMed] [Google Scholar]
- 45.Gomez PP, Nelson AR, Asiedu A, Addo E, Agbodza D, Allen C, et al. Accelerating newborn survival in Ghana through a low-dose, high-frequency health worker training approach: a cluster randomized trial. BMC Pregnancy Childbirth. 2018;18(1):72–83. doi: 10.1186/s12884-018-1705-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Evans CL, Bazant E, Atukunda I, Williams E, Niermeyer S, Hiner C, et al. Peer-assisted learning after onsite, low-dose, high-frequency training and practice on simulators to prevent and treat postpartum hemorrhage and neonatal asphyxia: a pragmatic trial in 12 districts in Uganda. PLoS ONE. 2018;13(12):e0207909–e0207917. doi: 10.1371/journal.pone.0207909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gude WT, Roos-Blom M-J, van der Veer SN, Dongelmans DA, de Jonge E, Francis JJ, et al. Health professionals' perceptions about their clinical performance and the influence of audit and feedback on their intentions to improve practice: a theory-based study in Dutch intensive care units. Implement Sci. 2018;13(1):33. doi: 10.1186/s13012-018-0727-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gude WT, Brown B, van der Veer SN, Colquhoun HL, Ivers NM, Brehaut JC, et al. Clinical performance comparators in audit and feedback: a review of theory and evidence. Implement Sci. 2019;14(1):39. doi: 10.1186/s13012-019-0887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. HBB Prompt Phase 1a Focus Group Guide Plan and Standard Operating Procedures. Focus group guide with operational details, questions and prompts used to conduct focus group discussions during Phase 1a.
Additional file 2. HBB Prompt Phase 1b Focus Group Guide Plan and Standard Operating Procedures. Focus group guide with operational details, questions and prompts used to conduct focus group discussions during Phase 1b.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.