Abstract
Background
Interstitial pregnancy is a rare but life-threatening condition accounting for 1-4% of all types of tubal ectopic pregnancies. It can be managed by open and minimally invasive surgical techniques. Our goal was to compare laparoscopic and open surgery for managing interstitial pregnancy.
Search Strategy
We searched PubMed, Scopus, Web of Science, and Cochrane up to May 2020.
Selection Criteria
1) Women with interstitial pregnancy, 2) Intervention: laparoscopic surgery, 3) Comparator: open surgery, 4) Outcomes: Hospital stay, operation time, pain scale, blood loss. Secondary outcomes: any other reported 5) Study designs: interventional and observational.
Data collection and analysis
Data was extracted from the relevant articles and was pooled as mean difference (MD) or relative risk (RR) with a 95% confidence interval (CI).
Main Results
We included six studies, three of which provided eligible data. The duration of hospital stay was lower in the laparoscopic surgery group (MD = -1.42, 95% CI [-1.72, -0.76], P < 0.0001). There was no significant difference in operative time (MD = 5.90, 95% CI [-11.30, 23.09], P = 0.50, blood loss (MD = -9.43, 95% CI [-214.18, 195.32], P = 0.93), complications (RR = 1.54, 95% CI [0.20, 11.85], P = 0.68), or blood transfusions (RR = 0.77, 95% CI [0.50, 1.25], P = 0.30).
Conclusion
Laparoscopic surgery is associated with shorter hospital stay, with no difference in terms of blood loss, post-, and intraoperative complications, and need for blood transfusion compared with laparotomy.
Keywords: Interstitial pregnancy, cornual, ectopic, laparoscopy, laparotomy, meta-analysis
Introduction
Interstitial pregnancy is a type of ectopic pregnancy which occurs in the uterus but outside the uterine cavity, where implantation occurs in the interstitial (proximal) part of the fallopian tube at its insertion into the uterus (Moawad et al., 2010; Wai-man et al., 2001; Malinowski et al., 2006). It is a life- threatening rare condition with an incidence of about 1-4% of all types of tubal ectopic pregnancies and approximately one for every 2500-5000 live births (Rock et al., 2008). Many risk factors may predispose to interstitial pregnancy, including pelvic surgery and inflammatory diseases, tumours, anomalies of the uterus, and in-vitro fertilisation (Lau et al., 1999). Many cases can be asymptomatic or present with non-specific symptoms such as vaginal bleeding and abdominal pain; therefore diagnosis is often delayed which increases the risk of rupture (Lau et al., 1999; Habana et al., 2000; Soriano et al., 2008). Diagnosis depends on high levels of suspicion, especially in women who have any of the above risk factors. Interstitial and cornual pregnancy may be used as synonyms of each other as reported in some studies, however, the term interstitial pregnancy will be used in this text to avoid confusion with intrauterine pregnancies in one horn of a bicornuate uterus. Different definitions of cornual pregnancy are described in the literature, some of which differentiate these terms or use them as synonyms (Habana et al., 2000; Soriano et al., 2008; Faraj et al., 2007; BJOG Greentop Guideline #21, 2016).
Many modalities were used for management including medical treatment such as local and systemic methotrexate, expectant management, open and minimally invasive surgical techniques (Moawad et al., 2010). Choosing a treatment option is dependent on criteria such as the patient’s desire for future fertility and whether the rupture has occurred or not. Medical or expectant treatment are used only in asymptomatic and hemodynamically stable patient cases (Moawad et al., 2010). Surgical management is the main line of management in most cases, especially in ruptured ones. These surgical options are either laparoscopy or laparotomy depending on the patient’s condition and available resources. Traditionally, open surgery such as laparotomy with cornual resection or hysterectomy was used, but with the progression in surgical approaches, laparoscopic surgeries have shown better results compared with laparotomy (Ng et al., 2009). Laparoscopic surgery for ectopic pregnancies can be performed through different approaches, such as cornuostomy, salpingostomy, cornual resection, and mini-cornual excision (Sagiv et al., 2001; Chan et al., 2003; Tulandi et al., 1995; Vilos et al., 1995; Bremner et al., 2000). Laparoscopic surgery may have advantages over laparotomy, such as lower hospital stay duration, less postoperative pain, lower blood loss, and skin incision (Ehrenberg- Buchner et al., 2009; Marchand 2019).
Some reports have reviewed most of the treatment modalities, and described a road map for the management of ectopic pregnancies, but these reports include few or no interstitial pregnancy cases (Moawad et al., 2010; Cucinella et al., 2014) and show no clear evidence for selecting the most suitable surgical approach in interstitial pregnancy. Therefore, we aim to compare laparotomy with laparoscopic management of interstitial pregnancy, as evidenced from published studies.
Methods
This systematic review and meta-analysis was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009). We also followed the guidelines reported in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2008).
Literature Search
We searched for published studies in four electronic databases: PubMed, Web of Science, Scopus, and Cochrane Central Register of Controlled Trials (CENTRAL) in June 2020. We used the following query for our search: ((Laparoscop* OR cornuostomy) AND (cornu* OR laparotomy OR “cornual evacuation” OR “cornual resection” OR “cornual excision” OR “wedge resection” OR “loop ligature” OR “Vicryl loop placement” OR “conical exeresis” OR hysterectomy OR salping* OR traditional OR classic* OR conventional)) AND (“interstitial pregnancy” OR “Cornual pregnancy” OR “cornual gestation” OR “interstitial gestation” OR “cornual ectopic”).
Eligibility criteria
We included all studies that met the following criteria: 1) Patients: women with interstitial (cornual) pregnancy, 2) Intervention: all types of laparoscopic surgeries, 3) Comparator: all types of open surgeries, 4) Outcomes: main outcomes included; hospital stay, operation time, pain on VAS scale, and blood loss. Secondary outcomes; any other reported outcome, and 5) Study design: all interventional and observational studies (Cohort, case-control, cross- sectional, case series and case report). We excluded conference abstracts, non-English language studies, reviews, and studies that report the effect of only one type of surgery. No restriction was placed on age, place, and publication date.
Screening and studies selection
Two independent authors (KW and GB) screened the search results for eligibility in two steps: title and abstracts were screened, then full-text screening occurred in which the articles were revised for all criteria to be included in our study. A third author (KS) resolved any dispute that occurred. We manually screened the references of the included studies, and previous systematic review, for additional or missed citations.
Data Extraction
After screening , two authors (AK and SH) independently extracted the following data from the eligible studies using a previous formatted data extraction sheet: (1) Summary of the included studies including study design, sites and time, participants and main inclusion criteria, total sample size, type of laparoscopic surgery, type of traditional surgery, number of patients assigned to each type, investigations, results, conclusion of each study; (2) baseline characteristics of the patients in each study including groups, cases numbers in each group, age, gestational age (days), number of symptomatic women at diagnosis, number of ruptured ectopic, parity, gravidity, and, risk factors for developing interstitial pregnancy in recruited patients; (3) any repeated outcomes (reported by two or more studies) including postoperative hospital stay (days), operative time (minutes), blood loss (ml), post- and intraoperative complications, need for blood transfusion. Data for continuous outcomes were extracted as a mean and standard deviation, and dichotomous outcomes, events and total were extracted.
Quality assessment
The quality of the included studies were assessed by quality assessment tools of the National Heart, Lung, and Blood Institute (NHLBI) (NIH Quality Assessment Tools, 2020). We used a tool for observational cohort studies and another tool for a case series study. Each tool was composed of some questions to assess the risk of bias and confounders. These questions were answered by “yes”, “no”, “not applicable”, “cannot determine”, or “not reported”, with each study then being given a score to guide the overall rating of the quality as “good”, “fair”, or “poor”. We could not assess the publication bias due to the small number of included studies according to Egger’s funnel-plot-based methodologies (Egger et al., 1997).
Data Synthesis
For continuous data, we used the inverse-variance method and the data was pooled as mean difference (MD) using Review Manager Software (version 5.3) for Windows. For dichotomous data, we used the Mantel-Hanszel method and the data was pooled as relative risk (RR) using OpenMeta [Analyst] software for windows. We assessed the heterogeneity using a Chi-square test and its extent was determined by I-square, such that values of p < 0.1 or I2>50% were significant indicators of heterogeneity. We used the random-effects model to analyse heterogeneous data and fixed-effects model for the analysis of homogeneous data, and performed a sensitivity analysis to solve the heterogeneity whenever detected.
Results
Literature search
By searching PubMed, Web of Science, Scopus, and Cochrane Central Register of Controlled Trials (CENTRAL), we identified 832 records. We removed duplicates and the remaining 505 records were screened for eligibility. Only 18 studies were further included for full-text screening. We included four studies from this step. We did not find any missing papers after screening the references of the included trials and previous systematic review (223 references). As a result, we included six studies, with four of them being eligible for meta- analysis. The literature search process is described in a PRISMA flow diagram in Figure 1.
Figure 1.
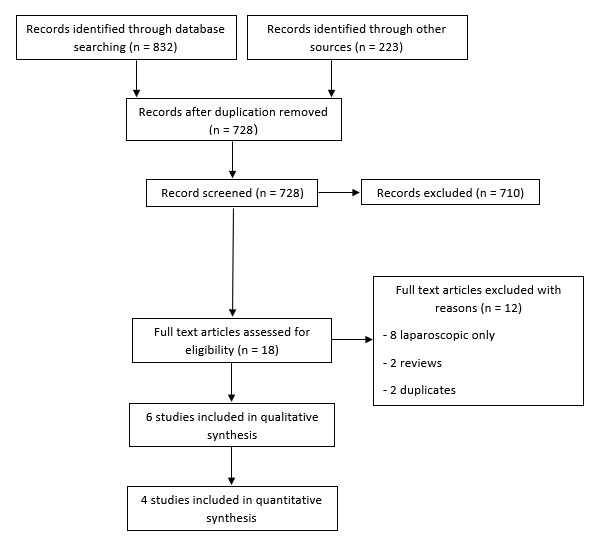
PRISMA flow chart
Characteristics of the included studies
We included one case series study, one cross- sectional, and four retrospective cohort studies with 70 cases of interstitial ectopic pregnancy in the laparoscopic surgery group and 83 cases in the open surgery group. Summary of the included studies and their results are shown in Table I and baseline characteristics of their patients are shown in Table II.
Table I.
Complete summary of the included studies and their findings (1/2).
| Study ID | Study design | Sites and time | Participants and main inclusion criteria | Total cases n | Type of Laparoscopic surgery, (n) | Type of Traditional surgery, (n) | Investigations | Results | Conclusion of the study |
|---|---|---|---|---|---|---|---|---|---|
| Jiang 2018 (32) | Retrospective analysis | Nanjing Drum Tower Hospital, China. Records from July 2010 to December 2015 | Patients with intrauterine pregnancy along with feature of a co-existing interstitial pregnancy: A gestational sac visualized high in the fundus. not surrounded by 5 mm of myometrium in all planes.a gestational sac seen separately and < 1 cm from the most lateral edge of the uterine cavity. | 17 | Laparoscopic cornual resection, (7) | Laparotomy with cornual resection, (3) | Transvaginal ultrasound scan | Compared with laparotomy, laparoscopic cornual section showed shorter operative time (median 40 vs. 70 min), less blood loss (150 vs. 400 ml) and shorter hospital stay (2 vs. 4 days). | Laparoscopic cornual resection is a feasible approach with favorable surgical and long-term pregnancy outcomes. |
| Hwang 2010 (26) | Retrospective analysis | The Korea University Medical Center, South Korea. Records from January 1998 to October 2009 | Patients with interstitial pregnancy who were treated with open cornual resection or laparoscopic cornual resection. | 88 | Laparoscopic cornual resection, (34) | Open cornual resection, (54) | Transvaginal ultrasound scan | There were no statistically significant differences between the two groups for the mean operation time, estimated blood loss, blood loss of more than 1000 mL, blood transfusion requirements, and complications. The mean number of postoperative hospital days was shorter in the laparoscopy group than in the laparotomy group (4.53 ± 1.44 days versus 5.89 ± 1.86 days, respectively; P < 0.001). | Laparoscopic cornual resection is a safe and less invasive procedure with a reasonable complication rate and shorter hospital stay. |
| Ghazali 2018 (27) | Retrospective cohort | Putrajaya Hospital, Putrajaya, Malaysia. Records from January 2005 to December 2014, | Patients with interstitial pregnancy who were treated with open cornual resection or laparoscopic cornual resection. | 14 | Laparoscopic cornuotomy, (7) | Open cornuotomy, (7) | Physical examination, transvaginal sonography, full blood count, and serum human chorionic gonadotrophin (hCG) levels. | The duration of hospitalization and mean operating time were both significantly shorter in the LC group than in the OC group (1.43 ± 0.54 versus 2.57 ± 0.79 and 61.4 ± 15.7 min versus 97.1 ± 38.2 min, respectively, P < 0.05).There were no statistically significant differences between both groups for the estimated blood loss, requirement of blood transfusion, complications, and future fertility. | Laparoscopic cornual resection (cornuotomy) is a safe and less invasive procedure with a comparable complication rate. It has shown that it is feasibility and should be considered as initial treatment in managing those cases in trained hand surgeons. |
| Sagiv 2013 (22) | Retrospective cohort | Wolfson Medical Center, Holon, and 2Sackler Faculty of Medicine, Tel-Aviv University, Tel-Aviv, Israel. Records from June 1997 to June 2007. | Patients with interstitial pregnancy who were treated with laparotomy, medical treatment with systemic methotrexate, or laparoscopy. | 14 | Laparoscopy cornuostomy, encircling, or salpingectomy, (8) | Laparotomy, (5) | Transvaginal ultrasound scan | The first four women, with significant hemoperitoneum, were treated by laparotomy. Of the next 10 women, four were selected for medical treatment with methotrexate. Only one case was treated successfully. The other six women had laparoscopic treatment. Of nine laparoscopies, one was converted to laparotomy due to excessive blood loss during the procedure. Of nine women desiring a child, three were infertile, whereas six conceived with an intrauterine pregnancy. | A change from diagnosis later in pregnancy and laparotomy to more conservative treatment, mainly by laparoscopy, suggests a possibly better subsequent pregnancy rate. |
| Tulandi 2004 (23) | Cross sectional | Cases from 1999 to 2002. | Patients with interstitial pregnancy who were treated with laparotomy, methotrexate, or laparoscopy. | 32 | Laparoscopy, (11) | Laparotomy, (13) | Transvaginal ultrasound scan and diagnostic laparoscopy and laparotomy. | Persistently elevated serum human chorionic gonadotropin levels were found in one patient after laparoscopic cornual excision, and she was successfully treated with methotrexate. Fourteen cases (43.7%) of rupture of interstitial pregnancy were found. This included five cases (15.6%) of heterotopic pregnancy; all were the results of in vitro fertilization, and all ruptured at the time of diagnosis. Subsequent pregnancy was achieved in ten patients. No uterine rupture was encountered during pregnancy or labor | Ipsilateral salpingectomy, previous ectopic pregnancy, and in vitro fertilization are predisposing factors for interstitial pregnancy. Contrary to previous belief, rupture of interstitial pregnancy occurs relatively early in pregnancy. In selected patients, laparoscopic cornual excision is a viable treatment option. |
| Warda 2014 (24) | Case series | N/A | Cases of interstitial ectopic pregnancy | 4 | Laparoscopic cornuostomy and removal of products of conception, (3) | Cornuostomy by laparotomy, (1) | Transvaginal ultrasound scan and diagnostic laparoscopy | Subsequent successful reproductive outcomes are presented. | Progressively conservative surgical measures are being used to treat interstitial pregnancy successfully, with no negative impact on subsequent pregnancies. |
Table II.
Baseline characteristics of enrolled patients in the included studies.
| Article ID | Groups | Cases, n | Age, mean (SD) | Gestational age (days), mean (SD) | Symptomatic, number (%) | Ruptured ectopic, number (%) | Parity, mean (SD) | Gravidity, mean (SD) | Ovulation induction number (%) | Sexually transmitted disease, number (%) | Previous laparotomy, number (%) | Previous D & C, number (%) | Previous other tubal pregnancy, number (%) | Previous ectopic pregnancy, number (%) | Previous pelvic surgery, number (%) | Spontaneous conception, number (%) | In vitro fertilization, number (%) | laparoscopic salpingectomy, number (%) | left tubal litigation, number (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jiang 2018 (24) | laparoscopic cornual resection | 7 | 30.71 (3.04) | 52.71 (13.78) | 4 (57.14) | - | 0 | 4.25 (4.83) | - | - | - | - | - | - | - | - | 7 (100) | 5 (71.43) | 1 (14.29) |
| Laparotomy with cornual resection | 3 | 27.67 (2.52) | 46.33 (7.51) | 1 (33.33) | 0 | 2.33 (2.31) | 3 (100) | 2 (66.67) | 1 (33.33) | ||||||||||
| Hwang 2010 (30) | laparoscopic cornual resection | 34 | 31.12 (5.99) | 55.87 (13.08) | 70 (79.5) | 8 (23.5) | 0.82 (0.9) | - | - | - | 34 (38.6) | 66 (75.0) | 14 (15.9) | 1 (1.1) | - | - | 1 (1.1) | - | - |
| Open cornual resection | 54 | 32.74 (5.11) | 54.41 (10.61) | 19 (35.2) | 0.98 (0.74) | ||||||||||||||
| Ghazali 2018 (31) | Laparoscopic cornuotomy | 7 | 29.3 (5.9) | - | 6 (85.7) | 5 (71.4) | - | 2.9 (0.7) | - | - | - | - | 3 (42.9) | 4 (57.1) | 6 (85.7) | 1 (14.3) | - | - | |
| Open cornuotomy | 7 | 31.4 (7.3) | 7 (100) | 6 (85.7) | 2.7 (1.5) | 1 (14.3) | 3 (42.9) | 7 (100) | 0 (0) | ||||||||||
| Sagiv 2013 (22) | Laparoscopy | 8 | 34.38 (5.83) | 49 (5.29) | 3 (21.4) | 7 (50) | 2.5 (1.2) | 4.25 (1.58) | - | - | - | - | 5 (35.7) | - | - | - | 4 (28.6) | - | |
| Laparotomy | 5 | 31.8 (6.91) | 78.4 (34.79) | 1.8 (1.92) | 5.2 (2.59) | ||||||||||||||
| Tulandi 2004 (23) | Laparoscopy | 11 | 32.6 (5.66) | 37.8 (23.24) | - | 5 (45.4) | - | - | 1 (3.1) | 8 (25.0) | - | - | 13 (40.6) | - | - | 11 (34.4) | 12 (37.5) | ||
| Laparotomy | 13 | 51.1 (10.08) | 9 (69.2) | ||||||||||||||||
| Warda 2014 (27) | Laparoscopic cornuostomy and removal of products of conception. | 3 | 32 (3.46) | - | - | - | - | - | - | - | - | - | - | - | - | 1 (33.33) | 2 (66.67) | 1 (33.33) | - |
| Cornuostomy by laparotomy | 1 | 36 | 1 (100) |
Results of Risk of Bias Assessment
Two cohort studies had a fair quality according to the NIH quality assessment tool for Observational Cohort and Cross-Sectional Studies. The other two cohort studies and the only cross-sectional study were poor quality. The case series study was fair in quality according to the NIH quality assessment tool for case series studies. For more details and answers to all assessment questions in each study, see supplementary Table I for cohort studies and Table II for a case series study.
Analysis of Outcomes
1. Postoperative hospital stay (days)
Three studies reported postoperative hospital stay (days) (Ghazali et al., 2018; Hwang et al., 2011; Jiang et al., 2018). The pooled mean difference (MD) showed that laparoscopic surgery was significantly associated with less hospital stay duration than open surgery (MD = -1.42 days, 95% CI [-1.72, -0.76], P > 0.0001); Fig.2. Pooled results were homogenous (P = 0.88, I2 = 0%).
Figure 2.
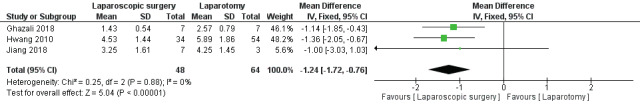
Mean difference (MD) in Postoperative hospital stay.
2. Operation time (minutes)
Three studies reported operation time (minutes) (Ghazali et al., 2018; Hwang et al., 2011; Jiang et al., 2018). The pooled effect estimate revealed no significant difference between laparoscopic surgery and open surgery in terms of operative time (MD = -11.22 minutes, 95% CI [-42.44, 20], P = 0.48); Fig.3 (A). Pooled results were heterogeneous (P = 0.03, I2 = 73%) and the detected heterogeneity was best resolved after excluding Ghazali et al 2018 (P = 0.29). Homogeneous results also did not favour either group (MD = 5.90, 95% CI [-11.30, 23.09], P = 0.50; Fig.3 (B).
Figure 3.
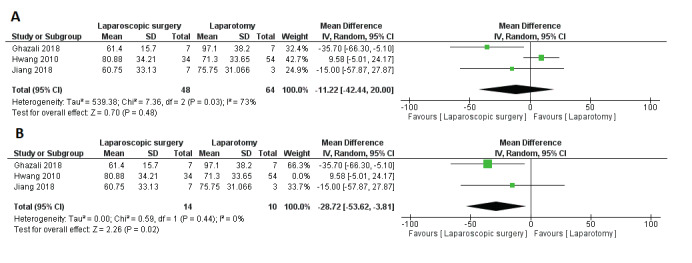
Mean difference (MD) in Operative Time .
3. Blood loss (ml)
Blood loss (ml) was reported by three studies (Ghazali et al., 2018; Hwang et al., 2011; Jiang et al., 2018). The pooled mean difference (MD) showed no significant difference between laparoscopic surgery and open surgery in terms of blood loss (MD = -9.43, 95% CI [-214.18, 195.32], P = 0.93); Fig.4. Pooled results were homogenous (P = 0.39, I2 = 0%).
Figure 4.
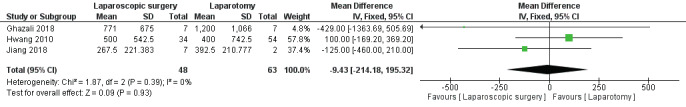
Mean difference (MD) in Blood loss.
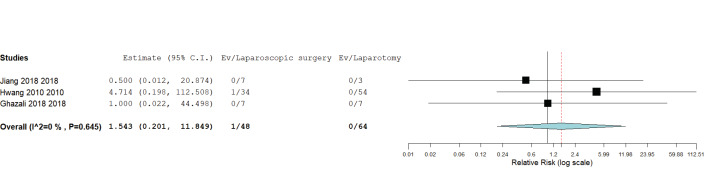
4. Post- and intraoperative complications
Three studies reported post- and intraoperative complications (Ghazali et al., 2018; Hwang et al., 2011; Jiang et al., 2018). The pooled relative risk (RR) revealed no significant difference between laparoscopic surgery and open surgery in terms of post- and intraoperative complications (RR = 1.54, 95% CI [0.20, 11.85], P = 0.68); Fig.5. Pooled results were homogenous (P = 0.65, I2 = 0%).
Figure 5.
Postoperative and intraoperative complications.
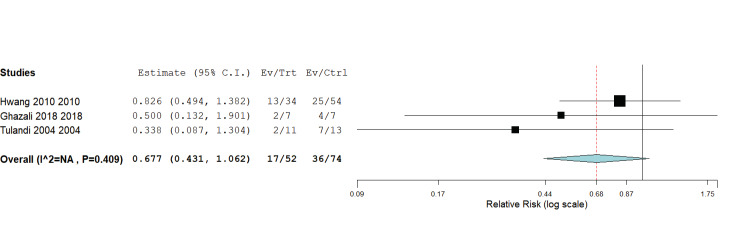
5. Need for blood transfusion
Two studies reported the need for blood transfusion (Ghazali et al., 2018; Hwang et al., 2011; Jiang et al., 2018). The pooled mean difference (MD) showed no significant difference between laparoscopic surgery and open surgery in terms of need for blood transfusion (RR = 0.68, 95% CI [0.43, 1.062], P = 0.09); Fig.6. Pooled results were homogenous (P = 0.41, I2 = 0%).
Figure 6.
Blood Transfusion.
Miscellaneous outcomes
For pregnancy outcome as reported by Sagiv et. al (2013), three out of five women undergoing laparotomy became infertile, one underwent a tubal ligation, and only one woman became pregnant and delivered by cesarean section. But out of eight women managed by laparoscopy, three women were undesirable for pregnancy, one outcome was not reported, one had an early miscarriage, and three became pregnant and delivered by cesarean section.
Tulandi et al. (2004) reported that in patients managed by laparoscopy, the hemoperitoneum encountered was 1385.7 ± 978.8 mL in the laparotomy group and 460.0 ± 70.7 mL in the laparoscopy group. In the laparotomy group, no patient needed any subsequent treatment but in the laparoscopy group, the first treatment failed in one patient and needed methotrexate as a subsequent treatment.
Warda et. al (2014) presented four cases of interstitial pregnancy; the first case was a 36-year-old woman treated with cornuostomy by laparotomy and then received a third intracytoplasmic sperm injection cycle, subsequently delivering an intact female after a pregnancy period devoid of any complications. The other three cases ( two aged 30, 30, and one 36 ) were treated with laparoscopic cornuostomy and removal of products of conception. They also underwent another in-vitro fertilisation cycle, then delivering without any complications and with no adverse neonatal outcomes.
Discussion
We found that laparoscopic surgery was significantly associated with less postoperative hospital stay period and less operation time than open surgery. However, we found no difference between both types in terms of blood loss, post- and intraoperative complications, and need for blood transfusion.
Our results were consistent with other studies published in the literature. Laparoscopic surgery has many advantages such as minimal skin incision and a shorter hospital stay period, preserves the uterus for future fertility, and is associated with improved and fast recovery and less postoperative pain (Soriano et al., 2008; Ng et al., 2009), but also has some minor disadvantages such as hematomas of the abdominal wall occurring near the incisions, some abdominal or pelvic infections, although serious laparoscopy complications are rare (Rempen et al. 1999).
Laparotomy is the second line of management when there is no laparoscopic expertise or when adequate closure or hemostasis cannot be achieved by laparoscopic surgery. However, it has a lot of risks, ranging from the general risks of anesthesia and surgery to incisional hernia, infections, bleeding, and injury of pelvic or abdominal organs. Also, it is associated with longer hospital stay periods as reported in some studies (Hwang et al., 2011; Ghazali et al., 2018).
Two previous systematic reviews have described a roadmap for nearly all medical and surgical options, and both recommended using laparoscopic surgery in most conditions (Moawad et al., 2010; Cucinella et al., 2014).
A previous meta-analysis compared laparoscopy against laparotomy for ectopic pregnancy and concluded that laparoscopy is better than laparotomy. However, contrary to our results, they found no difference between laparoscopy and laparotomy in terms of operation time, which we found was lower in the laparoscopic group. Additionally, they found that intraoperative blood loss was lower in the laparoscopy arm compared with laparotomy (Gao et al., 2009).
Some studies compared different laparoscopic approaches; the study by Lee et al. (2016) compared laparoscopic cornual resection and laparoscopic cornuotomy, and found no significant difference between them in haemoglobin levels after the operation, persistent interstitial pregnancy and incidence of major complications, though the operation time was significantly shorter for cornuotomy than that for cornual resection. Also, Gasparria et al. (2018) compared conventional versus single port laparoscopy, and found no difference between them in terms of haemoglobin levels, need for blood transfusions, operation time, length of hospital stay period, and post- and intra- operative complications.
In a cost-effectiveness comparison between laparoscopic and laparotomy, Gray et. al in 1995 showed that at lower costs, laparoscopy produced final outcomes comparable to those of laparotomy. Also, Ghazali et. al (2018) stated that laparoscopy was associated with financial savings.
We included all studies comparing laparoscopic surgery with laparotomy in interstitial ectopic pregnancy patients. Additionally, most of our results were homogenous and we managed to solve the heterogeneity detected among studies.
However, we have some limitations in our study such as: 1- Small number of the included studies and small sample size with the absence of clinical trials; 2- lack of data about long term effects; 3- all of the included studies were observational which are considered a low level of evidence; 4- we only included English studies; only three studies with 112 cases were eligible for analysis, which might have an influence on our results in situations where the laparoscopic approach is not applicable.
Conclusion
Our analysis shows that in women with interstitial ectopic pregnancy, management with laparoscopic surgery is associated with reduced postoperative hospital stay duration. There was no difference in terms of operation time, blood loss, post- and intraoperative complications, and need for blood transfusion.
Further studies, especially interventional studies with longer follow up duration and larger sample sizes, are needed to produce more valid results and until that we recommend using laparoscopic surgery if available as it has some advantages over open surgery.
Footnotes
Conflicts of Interest:Authors declare no conflicts of interest.
Contributions to authorship: Greg Marchand gathered the idea and reviewed the whole work starting from search to final writing. Ahmed Taher Masoud performed statistical analysis and wrote the statistical part of the results as well as reviewing the writing process. Katelyn Sainz, Ali Azadi, and Kelly Ware searched all databases for possible included studies and screened the retrieved results. Janelle Vallejo, Sienna Anderson, and Alexa King performed the data extraction and risk of bias assessment for included studies. Asya Osborn and Stacy Ruther wrote the introduction section. Giovanna Brazil wrote the methods section. Kaitlynne Cieminski, and Sophia Hopewell wrote the results section and served as the second team for screening and data extraction of outcomes and baseline tables, Lisa Rials1. Danielle Jenks, Jennifer Love, and Allison Steele assisted with both rounds of revisions and reformatting.
Ethical approval: This Manuscript has been reviewed by the institutional IRB board at Marchand Institute and was found to be exempt from IRB review. (May 2020)
Financial disclosures: All authors have no disclosures. No authors received any funding for this review.
Prosper Registration Number: CRD42020185248
References
- 1.Bremner T, Cela V, Luciano AA. Surgical management of interstitial pregnancy. J Minim Invasive Gynecol. 2000;7(3):387–389. doi: 10.1016/s1074-3804(05)60483-5. [DOI] [PubMed] [Google Scholar]
- 2.Chan LY-S, Yuen PM. Successful treatment of ruptured interstitial pregnancy with laparoscopic surgery: A report of 2 cases. J REPROD MED. 2003;48:569–571. [PubMed] [Google Scholar]
- 3.Cucinella G, Calagna G, Rotolo S, et al. Interstitial pregnancy: A ‘Road Map’ of surgical treatment based on a systematic review of the literature. Gynecol Obstet Invest. 2014;78:141–149. doi: 10.1159/000364869. [DOI] [PubMed] [Google Scholar]
- 4.Diagnosis and Management of Ectopic Pregnancy: Green-top Guideline No. 21. BJOG. 2016;123:15–55. doi: 10.1111/1471-0528.14189. [DOI] [PubMed] [Google Scholar]
- 5.Egger M, Smith GD, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrenberg-Buchner S, Sandadi S, Moawad NS, et al. Ectopic pregnancy: Role of laparoscopic treatment. Clin Obstet Gynecol. 2009;52:372–379. doi: 10.1097/GRF.0b013e3181b0be24. [DOI] [PubMed] [Google Scholar]
- 7.Faraj R, Steel M. Management of cornual (interstitial) pregnancy. Obstet Gynaecol. 2007;9:249–255. [Google Scholar]
- 8.Gao MX, Gao Q, Jia J, et al. Laparoscopy versus laparotomy for ectopic pregnancy: A systematic review. J Minim Invasive Gynecol. 2009;9:994–1000. [Google Scholar]
- 9.Gasparri ML, Mueller MD, Taghavi K, et al. Conventional versus single port laparoscopy for the surgical treatment of ectopic pregnancy: A meta-analysis. Gynecol Obstet Invest. 2018;83:329–337. doi: 10.1159/000487944. [DOI] [PubMed] [Google Scholar]
- 10.Ghazali WAHW, Abidin NHZ, Muda AM, et al. Comparative study on surgical outcomes between laparoscopic and open cornuotomy in Urban Tertiary Center of Malaysia. Gynecol Minim Invasive Ther. 2018;7:22–26. doi: 10.4103/GMIT.GMIT_7_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gray DT, Gray DT, Thorburn J, et al. A cost-effectiveness study of a randomised trial of laparoscopy versus laparotomy for ectopic pregnancy. Lancet. 1995;345:1139–1143. doi: 10.1016/s0140-6736(95)90977-x. [DOI] [PubMed] [Google Scholar]
- 12.Habana A, Dokras A, Giraldo JL, et al. Cornual heterotopic pregnancy: contemporary management options. Am J Obstet. 2000;182:1264–1270. doi: 10.1067/mob.2000.103620. [DOI] [PubMed] [Google Scholar]
- 13. Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: cochrane book series. Chichester, UK: John Wiley & Sons, Ltd; 2008. [Google Scholar]
- 14.Hwang JH, Lee JK, Lee NW, et al. Open cornual resection versus laparoscopic cornual resection in patients with interstitial ectopic pregnancies. Eur J Obstet. 2011;156:78–82. doi: 10.1016/j.ejogrb.2010.12.014. [DOI] [PubMed] [Google Scholar]
- 15.Jiang Y, Chen J, Zhou H, et al. Management and obstetric outcomes of 17 heterotopic interstitial pregnancies. BMC Pregnancy Childbirth. 2018;18:78. doi: 10.1186/s12884-018-1700-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lau S, Tulandi T. Conservative medical and surgical management of interstitial ectopic pregnancy. Fertil Steril. 1999;72:207–215. doi: 10.1016/s0015-0282(99)00242-3. [DOI] [PubMed] [Google Scholar]
- 17.Lee MH, Im SY, Kim MK, et al. Comparison of laparoscopic cornual resection and cornuotomy for interstitial pregnancy. J Minim Invasive Gynecol. 2017;24:397–401. doi: 10.1016/j.jmig.2016.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Malinowski A, Bates SK. Semantics and pitfalls in the diagnosis of cornual/interstitial pregnancy. Fertil Steril. 2006;86:1764–1811. doi: 10.1016/j.fertnstert.2006.03.073. [DOI] [PubMed] [Google Scholar]
- 19.Marchand G. Single port advanced laparoscopic hysterectomy: An advanced ultra-minimally invasive surgical technique - (LESS-11mm Hysterectomy). Marchand Institute for Minimally Invasive Surgery; 2019. [Google Scholar]
- 20.Moawad NS, Mahajan ST, Moniz NH, et al. Current diagnosis and treatment of interstitial pregnancy. Am J Obstet Gynecol. 2010;2020:15–29. doi: 10.1016/j.ajog.2009.07.054. [DOI] [PubMed] [Google Scholar]
- 21.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Institute of Health. National Heart, Lung and Blood Institute Quality Assessment Tools. (https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. ).
- 23.Ng S, Hamontri S, Chua I, et al. Laparoscopic management of 53 cases of cornual ectopic pregnancy. Fertil Steril. 2009;92:448–452. doi: 10.1016/j.fertnstert.2008.08.072. [DOI] [PubMed] [Google Scholar]
- 24.Rempen A, Dietl J. Complication rates after surgical treatment of ectopic pregnancy. Hum Reprod. 1999;14:1401–1403. doi: 10.1093/humrep/14.5.1401. [DOI] [PubMed] [Google Scholar]
- 25.Rock JA, Jones HW TLRW. 10th ed. Philadelphia: Lippincott-Raven; 2008. Te Linde’s operative gynecology. [Google Scholar]
- 26.Sagiv R, Debby A, Keidar R, et al. Interstitial pregnancy management and subsequent pregnancy outcome. Acta Obstet Gynecol Scand. 2013;92:1327–1330. doi: 10.1111/aogs.12239. [DOI] [PubMed] [Google Scholar]
- 27.Sagiv R, Golan A, Arbel-Alon S, et al. Three conservative approaches to treatment of interstitial pregnancy. J Minim Invasive Gynecol. 2001;8:154–158. doi: 10.1016/s1074-3804(05)60567-1. [DOI] [PubMed] [Google Scholar]
- 28.Soriano D, Vicus D, Mashiach R, et al. Laparoscopic treatment of cornual pregnancy: a series of 20 consecutive cases. Fertil Steril. 2008;90:839–843. doi: 10.1016/j.fertnstert.2007.07.1288. [DOI] [PubMed] [Google Scholar]
- 29.Tulandi T, Al-Jaroudi D. Interstitial pregnancy: Results generated from the society of reproductive surgeons registry. Obstet Gynecol. 2004;103:47–50. doi: 10.1097/01.AOG.0000109218.24211.79. [DOI] [PubMed] [Google Scholar]
- 30.Tulandi T, Vilos G, Gomel V. Laparoscopic treatment of interstitial pregnancy. Obstet Gynecol. 1995;85:465–467. doi: 10.1016/0029-7844(94)00423-B. [DOI] [PubMed] [Google Scholar]
- 31.Vilos GA. Laparoscopic resection of a heterotopic cornual pregnancy followed by term vaginal delivery. American Association of Gynecologic Laparoscopists. 1995;2:471–473. doi: 10.1016/s1074-3804(05)80073-8. [DOI] [PubMed] [Google Scholar]
- 32.Wai-man KN, Wai-kit TG. On the look out for a rarity - interstitial/cornual pregnancy. Eur J Emerg Med. 2001;8:147–150. doi: 10.1097/00063110-200106000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Warda H, Mamik MM, Ashraf M, et al. Interstitial ectopic pregnancy: Conservative surgical management. JSLS. 2014;18:197–203. doi: 10.4293/108680813X13753907292836. [DOI] [PMC free article] [PubMed] [Google Scholar]