The diagnosis of Pneumocystis jirovecii pneumonia (PJP) is particularly difficult during the COVID-19 pandemic because PJP and COVID share similar symptoms and thoracic CT-scan [1]. Physicians should remember that PJP is an opportunistic infection occurring in severely immunocompromised patients. Now, in industrialised countries, most cases of PJP occur in non-HIV infected patients with secondary immunodeficiency related to treatments such as treatment for haematological malignancy [2]. The groups of patients at risk of COVID-19 pneumonia are quite different, i.e. patients with cardiovascular risk factor. We report here the case of an immunocompromised patient with concurrent COVID-19 and PJP to outline the major importance of the analysis of the immune status of patients even when COVID-19 has been diagnosed.
A 65-year-old Caucasian male was admitted to our department in June 2020 for fever, dry cough, slightly increasing dyspnoea, malaise, and weight loss. The symptoms had started 2 to 3 weeks before. He had previously received from December 2019 to March 2020 four courses of a chemotherapy regimen including fludarabine–cyclophosphamide–rituximab for a recurrent chronic lymphocytic leukaemia (CLL) diagnosed initially in 2016. Simultaneously he had monthly pentamidine aerosols as PJP prophylaxis, which were stopped in March 2020. In April 2020, he was admitted to another institution because of afebrile isolated dyspnoea. Thoracic CT-scan showed bilateral subpleural ground glass opacities predominantly in the lower lobes. Diagnosis of moderate COVID-19 was made with positive nasal SARS-CoV-2 PCR and after one week, he was discharged without specific treatment.
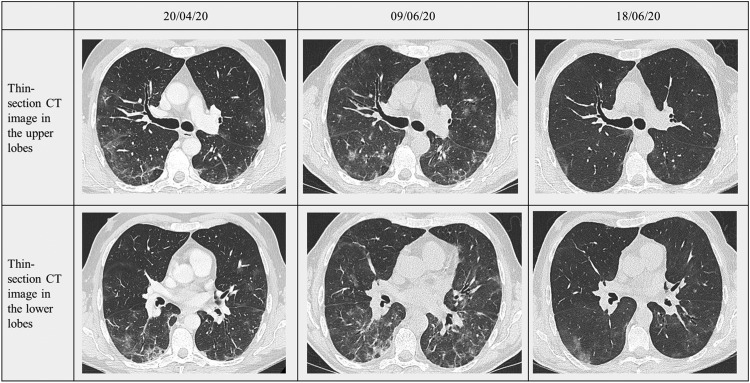
On arrival one month later, he had oxygen saturation of 94% on room air, temperature up to 38.2 °C. On examination, he had normal breath sounds and neither peripheral lymphadenopathy nor splenomegaly were detected. The white blood cell count revealed severe absolute lymphopenia of 200 lymphocytes/mm3, C-reactive protein level was 50 mg/L. HIV serological test was negative. Thoracic CT-scan disclosed increasing ground glass opacities, which were in a subpleural distribution (Fig. 1 ). Nasal swab PCR specimens were positive for SARS-CoV-2 and negative for common respiratory viruses and Chlamydia pneumoniae/Mycoplasma pneumoniae. Serum β-D-glucan level was low, below 80 pg/mL. Bronchoalveolar lavage fluid (BAL) analysis disclosed a total cell count of 468 × 103 cells/mm3 with macrophages 44%, small lymphocytes 38%, neutrophils 16%, and eosinophils 2%. Cysts of P. jirovecii were detected at direct examination on specific silver stains but not by direct immunofluorescence assay. Quantitative PCR for P. jirovecii was positive on BAL fluid (32 cycles) as was a SARS-CoV-2 PCR test. Trimethoprim–sulfamethoxazole was started intravenously then switched to orally on day 10 because of a favourable clinical course and improvement of the thoracic CT-scan (Fig. 1). He was discharged on the 14th day with 7 days more of curative treatment and later to continue PJP prophylaxis.
Fig. 1.
Radiological findings on thoracic CT-scan: at time of COVID-19 diagnosis (column 1), at time of PJP diagnosis (column 2) and at discharge (column 3).
We report here the case of an immunocompromised patient treated for CLL who developed moderate COVID-19 and one month later a PJP of favourable course. CLL is well-known to be associated with an impaired immune response which affects mainly humoral immunity. This immune deficiency is exacerbated by an anti-leukaemia regimen such as fludarabine, which induces a profound and long CD4+ T-cell lymphocytopenia [3]. This cellular immune deficiency induces a risk of opportunistic infections as PJP. The diagnosis of PJP is more difficult in non-HIV infected people than in AIDS patients because they have less cysts of P. jirovecii detected cytologically in BAL fluid [4]. However, in our case, the diagnosis was performed by direct examination by a trained thoracic pathologist (EL), and by molecular assays. The low level of serum β-D-glucan does not rule out the diagnosis of PJP because of its low sensitivity in patients with haematological malignancies, sensitivity recently reported in a retrospective analysis at 69.8% [5].
It has been suggested that SARS-CoV-2 infection may cause an immunodeficiency state that may allow occurrence of PJP in COVID-19 patients. Following an absence of clinically significant immune deficiency induced by SARS-CoV-2, systematic P. jirovecii PCR assay performed on 423 BAL samples from 145 patients with severe COVID-19 detected only three positive results in two patients; neither of these two patients evidence of PJP [6]. Similarly, Coleman et al. reported the case of an ex-smoker HIV-patient with CD4+ cells at 422/mm3 and indetectable HIV viral load and positive SARS-CoV-2 detection by PCR who developed bilateral pulmonary ground glass changes diagnosed as PJP because P. jirovecii DNA had been detected by PCR on induced sputum [7]. It is difficult to be conclusive because PCR for P. jirovecii was not quantitative, performed on sputum and not on BAL fluid, serum β-D-glucan level was not determined and mainly because PJP in a patient with well controlled HIV infection with more than 4OO CD4+ T-cells/mm3 is an excessively rare event in adults.
Because PJP and COVID-19 share overlapping clinical and radiological manifestations, physicians need to analyse the immunological status of the patient and whether a prophylaxis had been administered. In patients with immunodeficiency, a diagnosis of COVID does not eliminate the necessity to determine the associated cause of pneumonitis. This is of major importance because failure to identify the pathogen causing pulmonary infiltrates is a well-known risk factor in haematological patients.
Disclosure of interest
The authors declare that they have no competing interest.
References
- 1.Goyal N., Chung M., Bernheim A., et al. Computed tomography features of Coronavirus disease 2019 (COVID-19) J Thorac Imaging. 2020;35:211–218. doi: 10.1097/RTI.0000000000000527. [DOI] [PubMed] [Google Scholar]
- 2.Catherinot E., Lanternier F., Bougnoux M.E., Lecuit M., Couderc L.J., Lortholary O. Pneumocystis jirovecii pneumonia. Infect Dis Clin N Am. 2010;24:107–138. doi: 10.1016/j.idc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Forconi F., Moss P. Perturbations of the normal immune system in patients with CLL. Blood. 2015;126:573–581. doi: 10.1182/blood-2015-03-567388. [DOI] [PubMed] [Google Scholar]
- 4.Azar M.M., Slotkin R., Abbi-Raad R., Liu Y., Grant M.H., Malinis M.F. Gomori methamine silver stain on bronchoalveolar lavage fluid is poorly sensitive for diagnosis of Pneumocystis jirovecii pneumonia in HIV-negative immunocompromised patients and may lead to missed or delayed diagnoses. Arch Pathol Lab Med. 2020;144:1003–1010. doi: 10.5858/arpa.2019-0394-OA. [DOI] [PubMed] [Google Scholar]
- 5.Morjaria S., Frame J., Franco-Garcia A., Geyer A., Kambol A., Badaby N.E. Clinical performance of (1,3) Beta-D-Glucan for the diagnosis of Pneumocystis Pneumonia (PCP) in cancer patients tested with polymerase chain reaction. Clin Infect Dis. 2019;69:1303–1309. doi: 10.1093/cid/ciy1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blaize M., Mayaux J., Luyt C.E., Lampros M.S., Fekkar A. COVID-19 related respiratory failure and lymphopenia do not seem associated with Pneumocystosis. Am J Respir Crit Care Med. 2020 doi: 10.1164/rccm.202007-2938LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coleman H., Snell L.B., Simons R., Douthwaite S.T., Lee M.J. COVID-19 and Pneumocystis jirovecii pneumonia: a diagnostic dilemma in HIV. AIDS. 2020;34:1258–1260. doi: 10.1097/QAD.0000000000002571. [DOI] [PMC free article] [PubMed] [Google Scholar]