Abstract
BACKGROUND:
Although single and double lung transplantation outcomes for chronic obstructive pulmonary disease (COPD) have been investigated, right and left single lung transplants have never been rigorously compared to evaluate disease-specific differences. Single lung transplants for COPD often have hyperinflation of the contralateral native lung, which may be more pronounced in left lung transplants.
METHODS:
Using the United Network for Organ Sharing registry, we conducted a retrospective cohort study of 5,585 adults who underwent lung transplantation for COPD from May 4, 2005 to June 30, 2017. Subjects were followed until March 2019. Post-transplant survival was compared using Cox proportional hazards and Royston and Parmar’s flexible parametric survival models. We adjusted for donor and recipient factors with known or plausible associations with survival.
RESULTS:
Lung transplant recipients who received a left single lung transplant for COPD had an increased risk of post-transplant death when compared with those who received a right single lung transplant for COPD (hazard ratio [HR]: 1.24, 95% CI: 1.08–1.48, p = 0.002). Survival did not differ significantly between double lung transplant and right single lung transplant recipients (HR: 0.88, 95% CI: 0.77–1.02, p = 0.086). Adjusted 5-year survival was 57.8% (95% CI: 55.7–60.1) for double lung recipients, 56.7% (95% CI: 55.4–58.0) for right single lung recipients, and 50.9% (95% CI: 47.2–55.0) for left single lung recipients.
CONCLUSIONS:
In COPD, right single lung transplantation was associated with improved post-transplant survival compared with left single lung transplantation, and no significant difference in post-transplant survival compared with double lung transplantation was found. In light of the ongoing donor lung shortage, preferential allocation of right single lungs to patients with COPD should be considered.
Keywords: lung transplant, post-transplant, survival, single lung transplant, double lung transplant, lung allocation policy
Lung transplantation may improve the quality of life and survival of patients with chronic obstructive pulmonary disease (COPD).1,2 Unfortunately, there is a shortage of donor lungs relative to the number of candidates on the lung transplant waiting list.3 Owing to the relative scarcity of available organs, donor lungs are distributed with the goal of optimizing the benefits of transplants using the lung allocation score (LAS).4 Before the LAS-based allocation system, lungs were allocated solely on the basis of waiting time and ABO blood compatibility.5 The LAS estimates medical urgency and post-transplant survival, thereby placing the emphasis on medical need and transplant benefit.4
The implementation of the LAS on May 4, 2005 had dramatic effects on the lung transplant waiting list and recipient population.3,5 Idiopathic pulmonary fibrosis replaced COPD as the primary indication for transplantation, and both age and severity of illness at the time of transplantation have risen since 2005.3,5 Whereas waiting list mortality initially improved after the advent of the LAS, it has since risen, reaching 17.2 waitlist deaths per 100 waitlist years in 2016. Solutions to address this rising mortality are needed.3
A rather simple way of maximizing organ supply is to use 1 pair of donor lungs for 2 different waitlist candidates. In COPD, survival analyses for single and double lung transplant recipients have yielded inconsistent results, and conclusions remain controversial.3,6–8 Early registry data suggested a survival benefit favoring double lung transplants for COPD.9 However, a comprehensive analysis by Schaffer et al6 in 2015 reported no significant differences in post-transplant survival between double and single lung transplant recipients when accounting for important covariates.
Single lung transplantations for COPD are often affected by hyperinflation of the contralateral native lung, which may limit the transplanted lung ventilation and gas exchange.10–12 In our center’s experience, right single lung transplant recipients for COPD develop fewer infectious complications in the early post-transplant period than recipients of left single lung transplants for COPD.13 Although single and double lung transplant outcomes have been investigated extensively, right single and left single lung transplants have never been rigorously compared to evaluate transplant-specific differences in survival.14–16 We hypothesized that for COPD, right single lung transplant recipients have superior post-transplant survival than left single lung transplant recipients.
Methods
Study design, study population, and data sources
We performed a retrospective cohort study of adults aged ≥18 years with COPD who received a lung transplant between May 4, 2005 and June 30, 2017 using data provided by the United Network of Organ Sharing. Subjects were followed through March 13, 2019. Subjects were excluded if they received a multiorgan transplant, were <18 years old, or had a lobar lung transplantation (Figure 1). This study was approved by the Columbia University Institutional Review Board and was exempt from informed consent.
Figure 1.
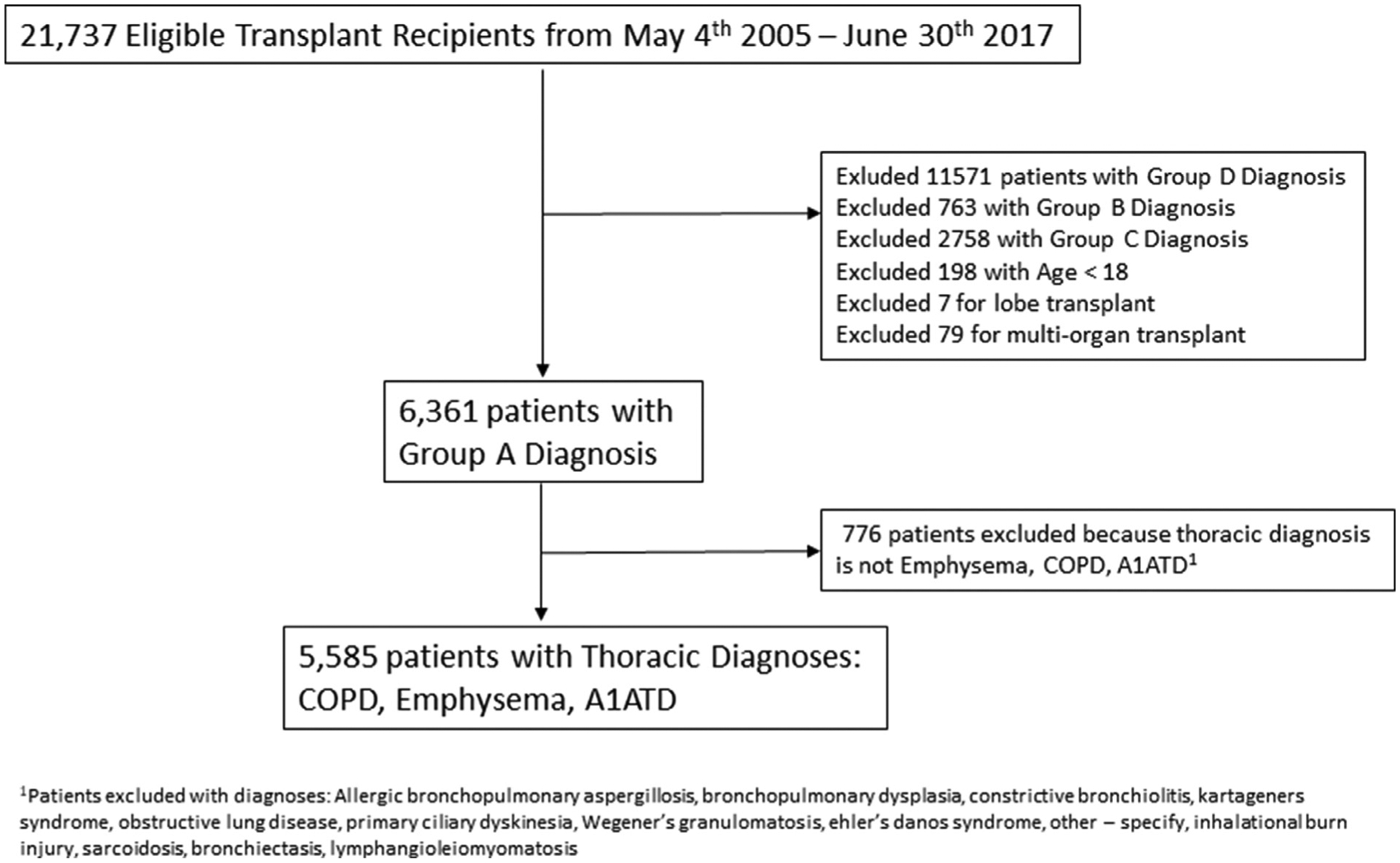
Flow chart of inclusion/exclusion criteria. A1ATD, alpha-1 antitrypsin deficiency; COPD, chronic obstructive pulmonary disease.
The COPD cohort included patients with the diagnosis of COPD, emphysema, or alpha-1 antitrypsin deficiency. Our primary predictor variables were left single, right single, and double lung transplantations. We analyzed the cohorts as 3 separate groups. The primary outcome was a composite of death or retransplantation.
Statistical analysis
Baseline characteristics were examined using the Wilcoxon rank-sum, Kruskal–Wallis, and Pearson’s chi-square tests. Post-transplant survival was analyzed using a mixed-effects (shared frailty) Cox proportional hazards model. We tested the proportional hazards assumption by regressing the Schoenfeld residuals over time. There was a violation of the proportional hazards when comparing double lung transplantation with right single lung transplantation or left single lung transplantation as has been demonstrated in previous studies comparing single and double lung transplantations.6 Our primary variables of interest (right single lung transplant compared with left single lung transplant) did not violate the proportional hazards assumption; therefore, we proceeded with a Cox proportional hazards model for our primary analysis. We selected a Cox model with shared frailty as the primary model to account for random effects of center-specific variation.
We secondarily used Royston and Parmar’s (RP) flexible parametric model using cubic splines to analyze the relationship between right single/left single lung transplantation and double lung transplantation because of the violation of the proportional hazards assumption.17,18 An RP flexible parametric model allows a covariate to have a changing hazard over time rather than assuming a proportional hazard throughout the entire analysis period. For the RP flexible parametric model, knot selection was optimized using the Akaike information criterion and Bayesian information criterion, and we designated 4 internal spline knots with 2 spline knots for the time-dependent effects for the model. A fixed-effects RP flexible parametric model was selected to compare right single/ left single lung transplantation with double lung transplantation rather than the mixed-effects models owing to the robustness of predictions permitted in the fixed-effects model.
Covariates were selected using a directed acyclic graph defined by a minimal set of variables that closed back-door paths, including age, transplant center, pulmonary hypertension, recipient–donor size mismatch, and LAS19–21 (refer to Supplementary Figure S1 available online at www.jhltonline.org). Race, sex, and ABO blood group were added in the primary analysis model as precision variables for the outcome of interest.6,7 Pulmonary artery hypertension was analyzed as a dichotomous variable above or below a mean pulmonary artery pressure of 40 mm Hg.22
Although missing data were rare (1.4% of cases) for the covariates in this model, multiple imputations were performed using chained equations approach for missing variables with 10 imputations. A priori sub-group analyses were performed to determine whether the effect was lessened or potentiated owing to the era of transplantation (2005–2010 and 2010–2018), patient age (aged <65 years and aged ≥65 years), and amount of donor–recipient size mismatch (predicted total lung capacity [pTLC] <1.1 and pTLC ≥1.16).
We performed an extensive sensitivity analysis to corroborate the findings from our primary model (see Supplementary Tables S1 and S2 online). Analyses included a complete case analysis (excluding cases with missing covariate data), a fixed-effects Cox proportional hazards model clustering by transplantation center, and an analysis, including a more expansive list of covariates based on previous studies and clinical experience.6
During our analyses, we noticed that there was a trend toward improved late survival with double lung transplantation, which differed from the previous paper by Schaffer et al.6 To further validate our findings, we conducted a post-hoc analysis of single lung transplantation compared with double lung transplantation using our updated cohort from May 4, 2005 to June 30, 2017 with follow-up through March 13, 2019. We then conducted an additional analysis of single lung transplantation compared with double lung transplantation using the same study period as used by Schaffer et al,6 limiting our sample size to transplantations from May 4, 2005 to December 31, 2012 with follow-up through December 31, 2012 (see Supplementary Figure S4 online).6
All analyses were performed using Stata, version 15.1 (Stata-Corp, College Station, TX), using STCOX,23 STPM2,24 and STPM2_STANDSURV.25
Results
There were 5,585 COPD transplant recipients included in this analysis: 1,010 (18.1%) received a left single lung transplant, 995 (17.8%) received a right single lung transplant, and 3,580 (64.1%) received a double lung transplant. The median length of follow-up was similar across groups: 1,138 days (interquartile range [IQR]: 592–2,190) for left single transplants, 1,436 (IQR: 720–2,366) for right single lung transplants, and 1,361.5 (IQR: 684–2,375) for double lung transplants. Baseline characteristics were similar among the 3 cohorts; however, double lung transplant recipients were slightly younger, were more often on the ventilator before transplantation, had more pulmonary hypertension, were transplanted at centers with higher annual volume, and had better pre-transplant 6-minute walk distances (Table 1). Even though extracorporeal membrane oxygenation (ECMO) use before transplantation was rare in this cohort, the patients who required ECMO most often received a double lung transplant.
Table 1.
Baseline Characteristics for 5,585 Lung Transplant Recipients With COPD
| Characteristics | Righ single lung transplantation | Left single lung transplantation | Double lung transplantation | p-value |
|---|---|---|---|---|
| Number of transplant recipients | 995 | 1,010 | 3,580 | — |
| Age, years, median (IQR) | 63 (59–65) | 63 (59–66) | 60 (55–64) | <0.001 |
| Female, % | 53.6 | 48.8 | 45.7 | <0.001 |
| Race/ethnicity, % | ||||
| White | 92.9 | 92.2 | 90.9 | 0.41 |
| Black | 5.2 | 6.2 | 7.0 | |
| Hispanic | 1.2 | 0.9 | 1.1 | |
| Other | 0.7 | 0.7 | 1.0 | |
| BMI at listing, median (IQR) | 24.4 (21.3–27.5) | 24.6 (21.7–27.8) | 24.3 (21.3–27.4) | 0.14 |
| ABO blood type, % | ||||
| O | 41.3 | 42.7 | 42.2 | 0.092 |
| A | 45.7 | 43.6 | 41.6 | |
| B | 9.0 | 9.4 | 11.3 | |
| AB | 3.9 | 4.4 | 4.9 | |
| LAS at transplantation, median (IQR) | 33.4 (32.4–34.8) | 33.2 (32.4–34.6) | 33.6 (32.6–35.4) | <0.001 |
| O2 requirement at transplantation in liters of O2, median (IQR) | 3 (2–4) | 3 (2–4) | 3(2–4) | <0.001 |
| Mean PAP ≥ 40, % | 3.2 | 2.2 | 6.1 | <0.001 |
| ECMO before transplantation, % | 0.1 | 0.0 | 0.5 | 0.014 |
| Ventilator before transplantation, % | 1.7 | 2.2 | 3.4 | 0.006 |
| Donor age, years, median (IQR) | 32(22–47) | 30 (21–44) | 33 (23–48) | <0.001 |
| Gender mismatch between donor and recipient, % | 32.5 | 32.3 | 29.1 | 0.037 |
| Ischemic time, hours, median (IQR) | 3.9 (3.1–4.7) | 3.8 (3.0–4.6) | 5.3 (4.3–6.3) | <0.001 |
| 6-minute walk distance, feet, median (IQR) | 760 (512–965) | 738 (520–960) | 780(514.5–1,008) | 0.008 |
| pTLC ratio ≥1.1, % | 33.8 | 35.7 | 29.7 | <0.001 |
| Transplantation center volume, median (IQR) | 42.9 (21–56) | 43.3 (23–68) | 50.8 (29–74) | p < 0.001 |
| Creatinine before transplantation, median (IQR) | 0.8 (0.66–0.91) | 0.8 (0.69–0.99) | 0.8 (0.66–0.91) | 0.009 |
| Donor smoking of >20 pack per years, % | 9.2 | 8.8 | 10.0 | 0.61 |
Abbreviations: BMI, body mass index; COPD, chronic obstructive pulmonary disease; ECMO, extracorporeal membrane oxygenation; IQR, interquartile range; LAS, lung allocation score; O2, oxygen; PAP, pulmonary artery pressure; pTLC, predicted total lung capacity.
Cox proportional hazards model
In the mixed-effects Cox proportional hazards model, left single lung transplantation was associated with an increased risk of death or retransplantation compared with right single lung transplantation in both unadjusted (hazard ratio [HR]: 1.19, 95% CI: 1.07–1.32, p = 0.002) and adjusted models (HR: 1.24, 95% CI: 1.08–1.41, p = 0.002). Compared with left single lung transplantation, double lung transplantation was associated with a reduced risk of death in unadjusted (HR: 0.69, 95% CI: 0.63–0.75, p < 0.000 1) and adjusted models (HR: 0.71, 95% CI: 0.62–0.82, p < 0.001), whereas compared with right single lung transplantation, double lung transplantation was associated with a decreased risk of death in unadjusted (HR: 0.81, 95% CI: 0.74–0.89, p < 0.001) but not in an adjusted Cox model (HR: 0.88, 95% CI: 0.77–1.02, p = 0.086) (Table 2, Figure 2).
Table 2.
Cox Proportional Hazards Model
| Characteristics | Right single transplantation | Left single transplantation | Double lung transplantation |
|---|---|---|---|
| Number of events (deaths and retransplantations) | 609 | 648 | 1,700 |
| Death or retransplantation Unadjusted HR (95% CI) | 1 | 1.19 (1.07–1.32), p = 0.002 | 0.81 (0.74–0.89), p < 0.001 |
| Adjusted HRa (95% CI) | 1 | 1.24 (1.08–1.41), p = 0.002 | 0.88 (0.77–1.02), p = 0.086 |
Abbreviation: HR, hazard Ratio; LAS, lung allocation score; pTLC, predicted total lung capacity.
Covariates include age, blood type, ethnicity/race (black, white, Hispanic, other), gender, LAS at time of transplantation, pulmonary hypertension, lung listing preference, donor-to-recipient pTLC ratio (pTLC ratio ≤1.1 or >1.1), and transplantation center.
Figure 2.
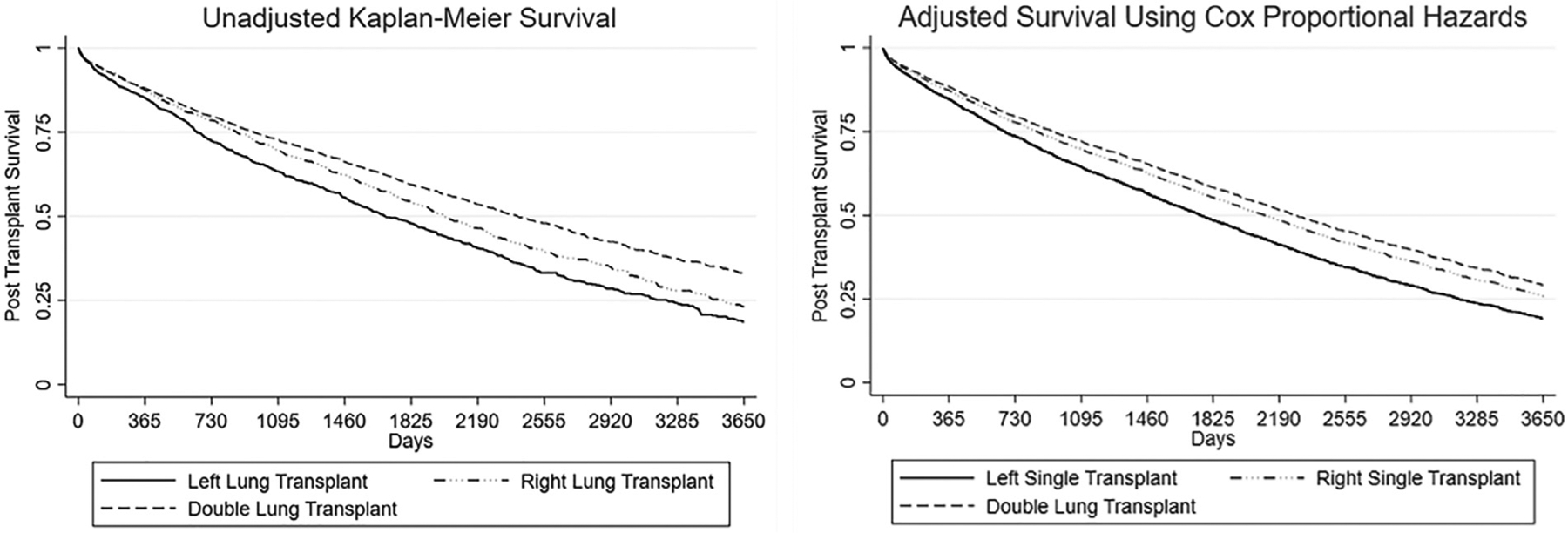
Survival post lung transplantation. (a) Kaplan–Meier unadjusted survival curve. (b) Adjusted Cox proportional hazards survival curve. Covariates include age, blood type, ethnicity/race (black, white, Hispanic, other), gender, LAS at the time of transplantation, pulmonary hypertension, lung listing preference, donor-to-recipient pTLC ratio (COPD if pTLC ratio ≥ 1.1), and transplantation center. COPD, chronic obstructive pulmonary disease; LAS, lung allocation score; pTLC, predicted total lung capacity.
Flexible parametric survival
Using the flexible parametric model and adjusting for covariates and time-dependent effects, double lung transplantation was associated with a reduced risk of death/retransplantation in the early transplant period compared with left single lung transplantation with an instantaneous HR of 0.76 (95% CI: 0.65–0.89) at 1 year after transplantation. The benefit of double lung transplantation continued to increase compared with that of left single lung transplantation at 3 and 5 years after transplantation (see Supplementary Figure S2 online). Compared with right single lung transplantation, double lung transplantation was associated with a similar risk of death/retransplantation in the early post-transplant period with an instantaneous HR of 0.95 (95% CI: 0.80–1.12) at 1 year after transplantation. Although the instantaneous hazard favored double lung transplantation at 5 years, it did not result in clinically meaningful different 5-year post-transplant survival (see Supplementary Figure S2 and Table S2 online).
Similar to the Cox proportional hazards model, left single lung transplantation had an increased risk of death/retransplantation compared with right single lung transplantation in the RP model (HR: 1.25, 95% CI: 1.09–1.43, p = 0.001) (see Supplementary Table S1 online). Interestingly, the RP model estimated nearly identical survival between right single lung transplant and double lung transplant at 1 year (86.8%, 95% CI: 85.6–88.0 vs 86.7%, 95% CI: 85.6–88.0) with a very minimal difference in 5-year survival (56.7%, 95% CI: 55.4–58.0 vs 57.8%, 95% CI: 55.7–60.1) (see Supplementary Table S2 online).
The adjusted survival curves for right single and double lung transplant survivals do not separate until about 3 years after transplantation, whereas both survival curves separate early from that of left single lung transplant (Figure 3). Nevertheless, post-transplant survival was only modestly reduced for left single lung transplant recipients compared with both double and right single lung transplant recipients with 1-year and 5-year survivals of 84.6% (95% CI: 86.1–87.7) and 50.9% (95% CI: 47.2–55.0), respectively (see Supplementary Table S3 online).
Figure 3.
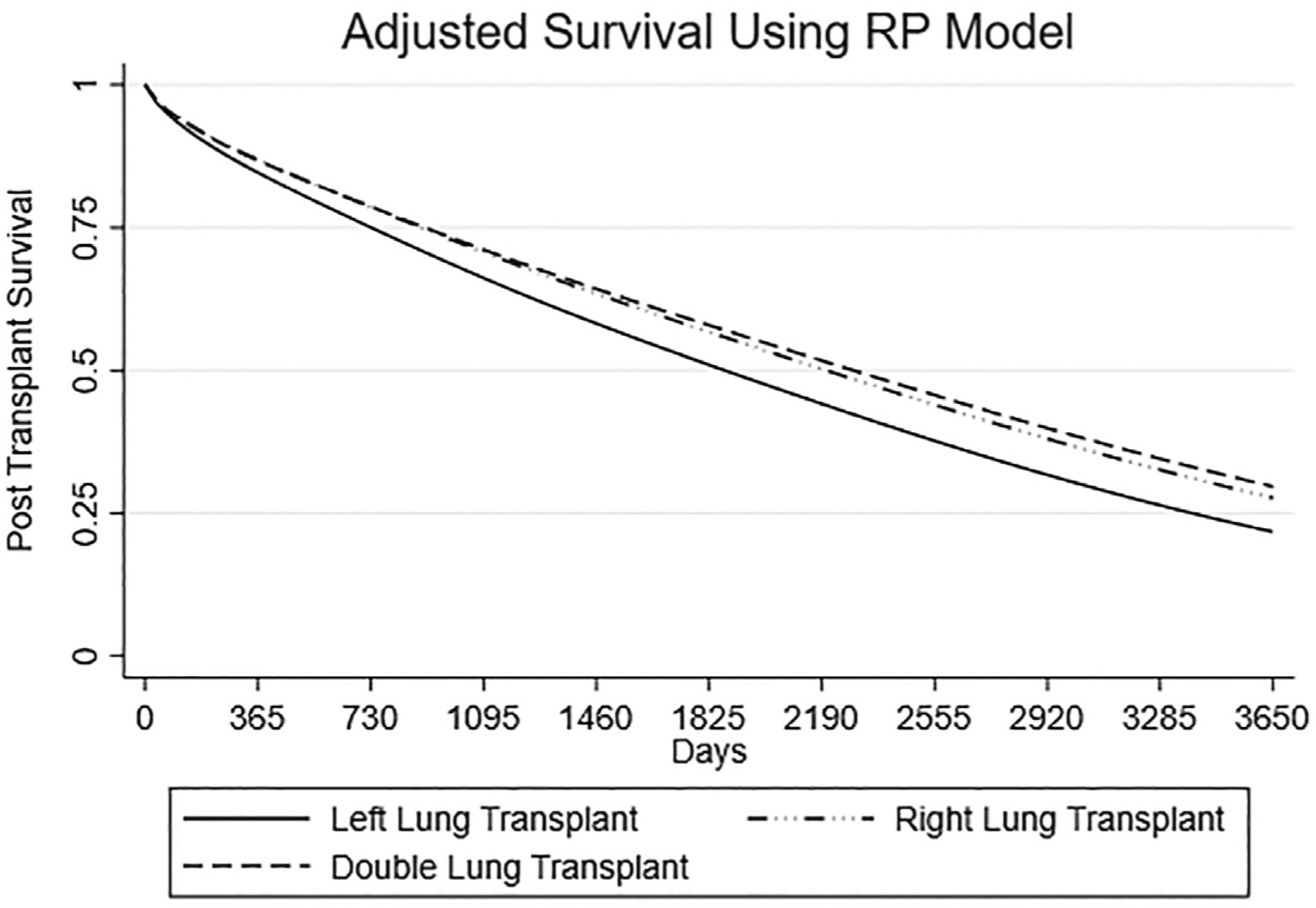
Adjusted survival for double lung, right single lung, and left single lung transplantations using flexible parametric survival model adjusting for time-dependent effects. Covariates include age, blood type, ethnicity/race (black, white, Hispanic, other), gender, LAS at the time of transplantation, pulmonary hypertension, lung listing preference, donor-to-recipient pTLC ratio (COPD if pTLC ratio ≥ 1.1), and transplantation center. COPD, chronic obstructive pulmonary disease; LAS, lung allocation score; pTLC, predicted total lung capacity; RP, Royston and Parmar.
Sub-group analysis
Sub-group analysis demonstrated similar results across the eras of lung transplantation when comparing May 2005‒June 2010 era with July 2010‒June 2017 era (Table 3). Double lung transplants made up a larger portion of transplantations for COPD in the more recent era than in the older era (68.9% vs 57.3%) (Table 3). For COPD transplant recipients aged <65 years, the decreased survival associated with left single lung transplantation compared with right single lung transplantation was slightly more pronounced (HR: 1.31, 95% CI: 1.12–1.54, p = 0.001); yet, survival after right single lung transplantation was still not significantly different from survival after double lung transplantation in this sub-group (Table 3 and see Supplementary Table S2 and Figure S3 online). For COPD transplant recipients aged ≥65 years, a significant difference in post-transplant survival between right single lung transplantation and left single (1.16, 95% CI: 0.96–1.40, p = 0.13) or double lung transplantation (0.89, 95% CI: 0.75–1.05, p = 0.17) in adjusted analyses was not observed(Table 3 and see Supplementary Table S2 online). In addition, double lung transplantation did not have significantly improved long-term survival benefit compared with right and left single lung transplantations in patients with COPD aged ≥65 years (see Supplementary Figure S3 online). The results did not differ for recipients who received lungs from larger donors (donor-to-recipient pTLC ratio > 1.1) (Table 3).
Table 3.
Sub-group Analysis
| Characteristics | Right single transplantation | Left single transplantation | Double lung transplantation |
|---|---|---|---|
| Early era | |||
| May 2005-June 30, 2010 | |||
| n | 511 | 481 | 1,332 |
| Adjusted HRa (95% CI) | 1 | 1.23 (1.04–1.45), p = 0.016 | 0.86 (0.72–1.03), p = 0.101 |
| Late era | |||
| June 2010-June 30, 2017 | |||
| n | 484 | 529 | 2,248 |
| Adjusted HRa (95% CI) | 1 | 1.25 (1.0–1.57), p = 0.045 | 0.94 (0.75–1.18), p = 0.577 |
| Age <65 years | |||
| n | 643 | 640 | 2,788 |
| Adjusted HRa (95% CI) | 1 | 1.31 (1.12–1.54), p = 0.001 | 0.88 (0.75–1.04), p = 0.130 |
| Age ≥ 65 years | |||
| n | 352 | 370 | 792 |
| Adjusted HRa (95% CI) | 1 | 1.12 (0.88–1.42), p = 0.352 | 0.89 (0.68–1.17), p = 0.411 |
| Donor-to-recipient pTLC ratio of ≥1.1 | |||
| n | 336 | 361 | 1,064 |
| Adjusted HRa (95% CI) | 1 | 1.24 (1.0–1.55), p = 0.054 | 0.85 (0.67–1.08), p = 0.194 |
| Donor-to-recipient pTLC ratio of <1.1 | |||
| n | 659 | 649 | 2,516 |
| Adjusted HRa (95% CI) | 1 | 1.23 (1.04–1.46), p = 0.014 | 0.92 (0.77–1.09), p = 0.332 |
Abbreviations: HR, hazard ratio; LAS, lung allocation score; pTLC, predicted lung capacity.
Covariates include age, blood type, ethnicity/race (black, white, Hispanic, other), gender, LAS at time of transplantation, pulmonary hypertension, lung listing preference, donor-to-recipient pTLC ratio (pTLC ratio ≥1.1 or <1.1), and transplantation center.
Post-hoc analysis: Single vs double lung transplantation
In post-hoc analyses, we compared post-transplant survival of all single lung transplant recipients (right and left) with double lung transplant recipients (see Supplementary Figure S4b online). Using the adjusted RP flexible parametric model, we found that double lung transplantation has a reduced risk of death/retransplantation at both 1 and 5 years after transplantation, with an instantaneous hazard of 0.84 (95% CI: 0.73–0.98) at Year 1 and 0.74 (95% CI: 0.64–0.85) at Year 5. When the cohort and the follow-up were limited to May 4, 2005 until December 31, 2012 (identical to Schaffer et al6‘s study period), the difference in post-transplant survival between single and double lung transplantations was lessened, with an instantaneous hazard of 0.90 (95% CI: 0.73–1.11) at Year 1 and 0.80 (95% CI: 0.62–1.03) at Year 5 (see Supplementary Figure S4a online).
Discussion
We have demonstrated that right single lung transplantation is associated with a reduced risk of death/retransplantation compared with left single lung transplantation for patients with COPD. Short-term and long-term survivals are similar between single right and double lung transplant recipients, whereas left single lung transplantation has mildly worse long-term survival in recipients with COPD. In addition, for recipients aged ≥65 years with COPD, there is no difference in short-term or long-term survival between double lung, right single lung, and left single lung transplantations.
These results add to previous work evaluating single and double lung transplantations for patients with COPD.6,7 This suggests that the diminished post-transplant survival associated with single lung transplantation for COPD is largely mediated by the lower survival associated with left single lung transplantation. Unsurprisingly, the benefit of right single and double lung transplantations compared with left single lung transplantation dissipates with advancing age, which is consistent with previous work by Thabut et al.7 Interestingly, we found that despite the ongoing donor lung shortage, double lung transplants were more common over the past decade for patients with COPD than before 2010.
In the current era of lung transplantation, the severity of illness at transplantation is rising and, consequently, the LAS at the time of transplantation is rising. It is difficult for a patient with COPD to achieve a high enough LAS to receive a double lung transplant, especially in areas of low-organ availability.26,27 The majority of lung transplantations for COPD in the United States are double lung transplantations. Given the national donor lung shortage, the transplantation community should consider allocating single lung transplants to most of the patients with COPD rather than double lung transplants, and this could improve organ availability and reduce the waitlist deaths.26,28 Our data support an allocation policy favoring right single lung allocation to patients with COPD when possible but not disallowing left single lung transplants.
In our center’s experience, there is an increase in post-transplant infectious complications in recipients of left single lung transplants for COPD. We previously reported reduced survival in these patients compared with recipients of right single lung transplants for COPD.13 We postulated that this occurs owing to excessive hyperinflation of the native lung on the contralateral side and that native lung hyperinflation is less severe in right single lung transplantation owing to the smaller size of the left lung and the presence of the heart-limiting excessive hyperinflation. We suspected that this might produce a survival advantage for right single lung transplants recipients who have COPD. In this cohort, there did not appear to be differences in the causes of death between the 3 groups (see Supplementary Table S4 online). Although this study does not provide a clear explanation for the differences in post-transplant survival, further prospective studies closely monitoring infectious complications and outcomes after single lung transplantation may elucidate causality.
Our post-hoc analysis comparing post-transplant survival for single and double lung transplants for COPD differs from previous results reported by Schaffer et al6 owing to the larger study size and longer study follow-up. Less than 50% of the patients in the study by Schaffer et al6 were at risk for 5 years, and the total study period was 7 years. In our study, the follow-up time for the entire cohort was 12 years, and the number of COPD cases in the analysis is nearly twice that in the study by Schaffer et al6. We were able to reproduce the results reported by Schaffer et al6 when we limited our cohort and follow-up time to the parameters of their study.6 Although the hazard of death/retransplantation beyond 5 years is higher with left single lung transplantation than with double lung transplantation, the 5-year survival estimates for left single lung transplantation is only modestly lower than the estimates of double and right single lung transplantations from a clinical perspective. A 5% lower survival at 5 years with left lung transplantation is a relatively small trade-off, and it should not preclude the allocation of left single lung transplants to patients with COPD.
Limitations
The limitations in this study include the retrospective nature of design, the potential for selection bias, missing covariates, center-specific practice patterns, and potential for incorrect data entry. We addressed these limitations as best as possible through a direct acyclic graph selection process for covariates to eliminate confounding, multivariable-adjusted Cox and RP flexible parametric analyses, extensive sensitivity analyses, and multiple imputations for missing data. Confounding by indication for either single or double lung transplantations is difficult to avoid; however, we attempted to account for this by adjusting for listing preference in our primary analysis. We further adjusted for center-specific differences by accounting for center variance in our analysis. Other important limitations in this study include the lack of quality of life information, lack of information about the surgical approach, peri-operative strategies with bypass, ECMO and selective ventilation, and lack of information on anatomic considerations for laterality, such as disease severity on a ventilation/perfusion scan. Unfortunately, these data are not reliably available in the United Network of Organ Sharing registry, but these data could be an important factor when understanding the differences in post-transplant outcomes between single and double lung transplantations.
Conclusions
There is a shortage of donor lungs, and as a result, people continue to die or deteriorate on the waiting list before undergoing lung transplantation.3 Of course, not every waiting list candidate with COPD may be a candidate for single lung transplantation owing to infectious issues, bilateral large bullae, multiple concerning lung nodules, or the occasional patient with severe secondary pulmonary hypertension. However, a straightforward way to increase the donor lung supply is to consider mandating single lung allocation to the majority of waiting list candidates with COPD, especially for those aged >65 years.
Right single lung transplantation has similar post-transplant survival compared with double lung transplantation in all transplant recipients who have COPD, and there is no difference in post-transplant survival among right single, left single, and double lung transplant recipients with COPD aged ≥65 years. Even though left single lung transplantation achieves acceptable 5-year post-transplant graft survival, preferential allocation of right single lungs to candidates with COPD should be considered.
Supplementary Material
Footnotes
Disclosure statement
The authors have no conflicts of interest to declare.
The data reported here have been supplied by the United Network of Organ Sharing as the contractor for the Organ Procurement and Transplantation Network. The datasets generated during and/or analyzed during the conduct of this study are available through the United Network of Organ Sharing or the Scientific Registry of Transplant Recipients. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as the official policy of or interpretation by the Organ Procurement and Transplantation Network or the United States government. This work was from the Columbia University Lung Transplant Program, New York.
This work was presented at the 39th International Society for Heart and Lung Transplantation annual meeting for April 2019.
Supplementary data
Supplementary data associated with this article can be found in the online version at www.jhltonline.org/.
Supplementary materials
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.healun.2020.06.009.
References
- 1.Thabut G, Ravaud P, Christie JD, et al. Determinants of the survival benefit of lung transplantation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2008;177:1156–63. [DOI] [PubMed] [Google Scholar]
- 2.Eskander A, Waddell TK, Faughnan ME, Chowdhury N, Singer LG. BODE index and quality of life in advanced chronic obstructive pulmonary disease before and after lung transplantation. J Heart Lung Transplant 2011;30:1334–41. [DOI] [PubMed] [Google Scholar]
- 3.Valapour M, Lehr CJ, Skeans MA, et al. OPTN/SRTR 2017 annual data report: lung. Am J Transplant 2019;19(Suppl 2):404–84. [DOI] [PubMed] [Google Scholar]
- 4.Egan TM, Murray S, Bustami RT, et al. Development of the new lung allocation system in the United States. Am J Transplant 2006;6:1212–27. [DOI] [PubMed] [Google Scholar]
- 5.Egan TM, Edwards LB. Effect of the lung allocation score on lung transplantation in the United States. J Heart Lung Transplant 2016;35: 433–9. [DOI] [PubMed] [Google Scholar]
- 6.Schaffer JM, Singh SK, Reitz BA, Zamanian RT, Mallidi HR. Single- vs double-lung transplantation in patients with chronic obstructive pulmonary disease and idiopathic pulmonary fibrosis since the implementation of lung allocation based on medical need. JAMA 2015;313: 936–48. [DOI] [PubMed] [Google Scholar]
- 7.Thabut G, Christie JD, Ravaud P, et al. Survival after bilateral versus single lung transplantation for patients with chronic obstructive pulmonary disease: a retrospective analysis of registry data. Lancet 2008;371:744–51. [DOI] [PubMed] [Google Scholar]
- 8.Hadjiliadis D, Angel LF. Controversies in lung transplantation: are two lungs better than one? Semin Respir Crit Care Med 2006;27:561–6. [DOI] [PubMed] [Google Scholar]
- 9.Trulock EP, Edwards LB, Taylor DO, Boucek MM, Keck BM, Hertz MI. Registry of the International Society for Heart and Lung Transplantation: twenty-second official adult lung and heart-lung transplant report–2005. J Heart Lung Transplant 2005;24:956–67. [DOI] [PubMed] [Google Scholar]
- 10.De Groote A, Van Muylem A, Scillia P, et al. Ventilation asymmetry after transplantation for emphysema: role of chest wall and mediastinum. Am J Respir Crit Care Med 2004;170:1233–8. [DOI] [PubMed] [Google Scholar]
- 11.Estenne M Effect of lung transplant and volume reduction surgery on respiratory muscle function. J Appl Physiol 2009;107:977–86. (1985). [DOI] [PubMed] [Google Scholar]
- 12.Loring SH, Mentzer SJ, Reilly JJ. Sources of graft restriction after single lung transplantation for emphysema. J Thorac Cardiovasc Surg 2007;134:204–9. [DOI] [PubMed] [Google Scholar]
- 13.Costa J, Piloni D, Gomez A, et al. Single vs double lung transplantation for emphysema in the lung allocation score era: a single center experience. In: Paper presented at: 26th European Conference on General Thoracic Surgery, Ljubljana, Slovenia; 2018. May 27–30. [Google Scholar]
- 14.Tsagkaropoulos S, Belmans A, Verleden GM, et al. Single-lung transplantation: does side matter? Eur J Cardiothorac Surg 2011;40:e83–92. [DOI] [PubMed] [Google Scholar]
- 15.Snell GI, Shiraishi T, Griffiths A, et al. Outcomes from paired single-lung transplants from the same donor. J Heart Lung Transplant 2000;19:1056–62. [DOI] [PubMed] [Google Scholar]
- 16.Smits JM, Melman S, Mertens BJ, et al. The Eurotransplant Study on Twin Lung Transplants (ESOTWIN): 90 paired single-lung transplants from the same donor. Transplantation 2003;76:1604–8. [DOI] [PubMed] [Google Scholar]
- 17.Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med 2002;21:2175–97. [DOI] [PubMed] [Google Scholar]
- 18.Royston P, Lambert PC. .. Flexible parametric survival analysis using Stata: beyond the Cox model. Texas: Stata Press; 2011. [Google Scholar]
- 19.Lederer DJ, Bell SC, Branson RD, et al. Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals [published correction appears in Ann Am Thorac Soc 2019;16:283]. Ann Am Thorac Soc 2019;16:22–8. [DOI] [PubMed] [Google Scholar]
- 20.Anderson MR, Tabah A, RoyChoudhury A, Lederer DJ. Procedure preference and intention-to-treat outcomes after listing for lung transplantation among U.S. adults. A cohort study. Ann Am Thorac Soc 2019;16:231–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ‘dagitty’. Int J Epidemiol 2016;45:1887–94. [DOI] [PubMed] [Google Scholar]
- 22.Nasir BS, Mulvihill MS, Barac YD, et al. Single lung transplantation in patients with severe secondary pulmonary hypertension. J Heart Lung Transplant 2019;38:939–48. [DOI] [PubMed] [Google Scholar]
- 23.StataCorp. Stata: release 16 statistical software. Texas: StataCorp LLC; 2019. [Google Scholar]
- 24.Lambert P>STPM2: “Stata module to estimate flexible parametric survival models,” Statistical software components S457128, Boston College Department of Economics. Available at: https://ideas.repec.org/c/boc/bocode/s457128.html. [Google Scholar]
- 25.Lambert P “STPM2_STANDSURV: Stata module to obtain standardized survival curves after fitting an stpm2 survival model,” statistical software components S458289, Boston College Department of Economics. Available at: https://ideas.repec.org/c/boc/bocode/s458289.html. [Google Scholar]
- 26.Ramos KJ, Harhay MO, Mulligan MS. Which shall I choose? Lung transplantation listing preference for individuals with interstitial lung disease and chronic obstructive pulmonary disease. Ann Am Thorac Soc 2019;16:193–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Benvenuto LJ, Anderson DR, Kim HP, et al. Geographic disparities in donor lung supply and lung transplant waitlist outcomes: a cohort study. Am J Transplant 2018;18:1471–80. [DOI] [PubMed] [Google Scholar]
- 28.Munson JC, Christie JD, Halpern SD. The societal impact of single versus bilateral lung transplantation for chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2011;184:1282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


