Abstract
Introduction: Acute myocardial infarction (AMI) is a time-sensitive condition. Meeting guideline-recommended time metrics for these patients can be challenging in rural emergency departments (EDs). Telemedicine has been shown to improve the quality and timeliness of emergency care in rural areas. The objective of this study was to evaluate the impact of telemedicine on the timeliness of emergency AMI care for patients presenting to rural EDs with chest pain.
Methods: A prospective cohort study, conducted in six telemedicine networks, identified ED patients presenting with chest pain from November 2015 through December 2017. Primary exposure was telemedicine consultation during the ED visit. The primary outcome was time-to-electrocardiogram (ECG). For eligible AMI patients, secondary outcomes included: (1) fibrinolysis administered and (2) time-to-fibrinolysis. Analyses for multivariable models were conducted by using logistic regression, clustered at the hospital level.
Results: Overall, 1,220 patients presenting with chest pain were included in the study cohort (27.1% received telemedicine). Time-to-ECG was, on average, 0.39 times (95% confidence interval [CI] −0.26 to −0.52) faster for telemedicine cases. Among eligible patients, telemedicine was associated with higher odds of fibrinolysis administration (adjusted odds ratio 7.17, 95% CI 2.48–20.49). In a sensitivity analysis excluding patients with cardiac arrest, time-to-fibrinolysis administration did not differ when telemedicine was used.
Discussion: In telemedicine networks, telemedicine consultation during the ED visit was associated with improved timeliness of ECG evaluation and increased use of fibrinolytic reperfusion therapy for rural AMI patients. Future work should focus on the impact of telemedicine consultation on patient-centered outcomes.
Keywords: telemedicine, telehealth, cardiology/cardiovascular disease, emergency medicine/trauma
Introduction
Acute myocardial infarction (AMI) is one of the most prevalent time-sensitive conditions treated in emergency departments (EDs), affecting ∼805,000 people and leading to nearly 115,000 deaths.1,2 For AMI patients with ST elevation, rapid triage and initiation of treatment is a key determinant of short- and long-term outcomes.3 Fibrinolytic reperfusion therapy is an effective treatment to reduce mortality, and shortening time to treatment is associated with improved clinical outcomes.4,5 Approaches to health care delivery, such as the regionalization of emergency care for AMI patients to tertiary hospitals, have been implemented in an effort to reduce time-to-reperfusion.6
However, there is wide variation in treatment and outcomes of AMI across geography. Rural hospitals struggle to meet time metrics, and patients at rural hospitals are less likely to receive guideline-recommended treatments, including early fibrinolysis, than their urban counterparts.7–10 These rural–urban disparities in AMI care are especially concerning, because AMI mortality is higher in rural compared with urban areas of the United States.10–12 Further, 17% of Americans live in rural areas and rely on rural hospitals for emergency care.13
Telemedicine has been shown to improve access to high-quality emergency care. In the prehospital setting, the use of telemedicine to transmit electrocardiograms (ECGs) has been shown to improve time-to-reperfusion and reduce mortality for AMI patients.14,15 In rural critical access hospitals (CAHs), there has been rapid expansion of ED-based telemedicine networks, which are designed to deliver provider-to-provider consultation to local staff in the diagnosis and treatment of patients.16,17 Evaluation of these networks has demonstrated an association between telemedicine consultation and improved timeliness of clinical management for other conditions, such as stroke and trauma.18–20
For this study, we investigated the use of ED-based telemedicine consultation for emergency cardiac care within a set of telemedicine networks. The objective of this study was to evaluate the impact of telemedicine consultation on (1) the timeliness of ECG evaluation for patients presenting with chest pain and (2) the rate and timeliness of fibrinolysis administration for eligible AMI patients.
Methods
Study Design and Setting
This study was a prospective cohort analysis of ED patients presenting with chest pain from November 2015 through December 2017. Patients presented to an ED in a telemedicine network included in the Evidence-Based Tele-Emergency Network Grant Program (EB TNGP). Funded by the Federal Office of Rural Health Policy (FORHP) (Health Resources & Services Administration [HRSA]), the purpose of the EB TNGP was to generate data on the impact of ED telemedicine programs on rural communities. Six telemedicine networks participated in the EB TNGP to compare effectiveness of provider-to-provider telemedicine in rural EDs. The participating networks have been previously described, and briefly, participating hospitals have an annual median ED volume of 8,427 visits and are primarily rural CAHs.21 The networks are hub-and-spoke telemedicine models with spoke hospitals located in the Western, Midwestern, and Eastern United States.
The institutional review boards at each participating network and at the data analysis center (the Rural Telehealth Research Center, funded by FORHP and HRSA) approved the project. Reporting of this study adheres to the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Statement guidelines.22 This is a comparative effectiveness analysis that reports clinical effectiveness according to the National Quality Forum (NQF) recommendations for measure development in telehealth.23
Participants
Adult (≥18 years) ED patients presenting with chest pain were eligible for the study. Chest pain was defined as (1) an ICD-10-CM diagnosis code related to chest pain syndrome, angina, or acute coronary syndrome (I200, I201, I208 I209, I248, I249, I25[110, 111, 118, 119, 700, 701, 708–11, 718–21, 728–31, 738, 739, 750, 751, 758–61, 768, 769, 790, 791, 799], I237, R070, R072, R0789, R079) or (2) a presenting complaint of chest pain symptoms. Telemedicine cases and nontelemedicine controls from each network were included in the study. A sub-group analysis of subjects with AMI was performed. AMI was defined by diagnosis code (I2101, I2102, I2109, I2111, I2119, I2121, I2129, I213, I214, I220, I221, I222, I228, I229, I91191, I97190, I97191, I97790).
Data Sources and Management
All data were collected for the study by using the Tele-Emergency Performance Assessment Reporting Tool (T-PART), which has been previously reported.21 The T-PART is a standardized data abstraction form built on Microsoft Excel (Microsoft Corporation, Redmond, WA) to report on a standard set of defined measures. Exposure, outcome, and covariates were abstracted from electronic medical records by using a detailed data dictionary. Research staff at each telemedicine network abstracted data, and a central data analysis center performed validation checks for quality assurance in an iterative fashion.
Variables
The primary exposure was telemedicine consultation during the ED visit. Telemedicine consultation included a technically successful interaction with a hub site physician (i.e., an ED physician or other consultant physician) via a high-definition video conference. The primary outcome was time-to-ECG in minutes. Secondary outcomes included fibrinolysis administered and time-to-fibrinolysis in minutes, both among subjects with ST-elevated myocardial infarction (STEMI) who were fibrinolysis eligible. Fibrinolysis eligibility required an adult inpatient admission and AMI with ST-elevation on ECG closest to ED arrival. If there was a documented reason for delay of fibrinolytic therapy after the physician administering fibrinolysis arrived at the hospital, not including system-based delays (e.g., pharmacy delay, equipment malfunction), then the patient was considered not eligible for fibrinolysis. Fibrinolytic agents included alteplase, anistreplase, anisoylated plasminogen-streptokinase activator complex, reteplase, streptokinase, tenecteplase, tissue plasminogen activator, or urokinase.
Subject characteristics measured included age (categorical: 18–24, 25–44, 45–64, 65–74, or 75 or more years), sex, race (White, American Indian/Alaskan Native, Black/African American, or Other), ethnicity (Hispanic/Latinx), and primary payer (Medicare only, Private Insurance, Medicaid only, Self-Pay/Uninsured, Indian Health Service, and Other). Current Procedural Terminology code for ED Evaluation and Management (E&M) (i.e., 99281–99285, 99291, and 99292) was used as a proxy measure for severity of illness at ED arrival. ED arrival time, dichotomized as business (07:30–17:30) or nonbusiness hours, and arrival day of week (e.g., Sunday) were also recorded. Reason for ED visit was categorized into Cardiac Arrest, Chest Pain, Shortness of Breath, and Other from the recorded ED “Chief Complaint,” or the primary reason for ED visit.
Statistical Methods
Descriptive characteristics of study subjects were reported as summary statistics and compared across telemedicine exposure status with chi-square tests. Bivariate tests of association between telemedicine status and study outcomes (time-to-ECG, fibrinolytic administration, and time-to-fibrinolysis) were conducted by using proportions with chi-square tests and univariable regression. Linear and logistic regression was used for univariable and multivariable models. It was hypothesized a priori that time-to-event outcomes may have nonparametric distributions, and visualization of model residuals after linear regression demonstrated heteroskedasticity. Therefore, the logarithmic transform was used for the time-to-ECG and time-to-fibrinolysis outcomes. As the assumption of independence of observations is likely violated by treatment similarities across hospitals, robust standard errors (with an exchangeable covariance matrix) by ED facility and generalized estimating equations (Gaussian distribution/identity link and binomial distribution/logit link) were used. Model selection for the multivariable models included stepwise selection based on hypothesized confounders from previous literature and minimization of the Akaike information criterion. As care processes are systematically different for ED patients in active cardiac arrest, a sensitivity analysis was conducting while excluding subjects with a reason for ED visit of cardiac arrest. Analysis was conducted with STATA SE (version 15.0; StataCorp LP, College Station, TX).
Results
Description of Study Cohort
Overall, 1,220 patients presenting with chest pain were included in the study cohort (Fig. 1), and 331 (27.1%) received telemedicine. Of the 1,220 chest pain patients, 265 (21.7%) were diagnosed with AMI, 92 (34.7%) of whom received telemedicine. In the study cohort, the plurality of subjects was male (60%), white (90%), Medicare beneficiaries (57.9%), and had high severity current procedural terminology (CPT) codes, 99284 or 99285 (44.9%, 40.6%) (Table 1).
Fig. 1.
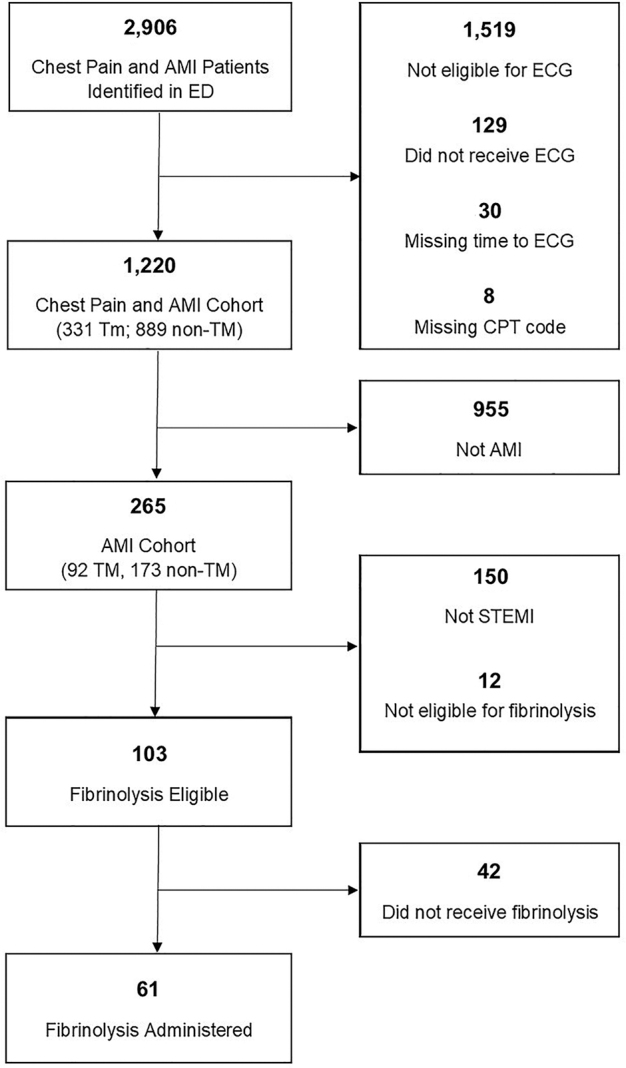
Flowchart of study subjects.
Table 1.
Demographics by TeleED Exposure for all Subjects and Acute Myocardial Infarction Subjects
| ALL CHEST PAIN AND AMI SUBJECTS |
AMI ONLY SUBJECTS |
|||||||
|---|---|---|---|---|---|---|---|---|
| TOTAL (N = 1,220), n (%) | NO teleED (N = 889), n (%) | teleED (N = 331), n (%) | p | TOTAL (N = 265), n (%) | NO teleED (N = 173), n (%) | teleED (N = 92), n (%) | p | |
| Patient age | ||||||||
| 18–24 | 10 (0.8) | 8 (0.9) | 2 (0.6) | <0.001 | 0 (0.0) | 0 (0.0) | 0 (0.0) | <0.001 |
| 25–44 | 88 (7.2) | 53 (6.0) | 35 (10.6) | 6 (2.3) | 2 (1.2) | 4 (4.3) | ||
| 45–64 | 421 (34.5) | 294 (33.1) | 127 (38.4) | 89 (33.6) | 41 (23.7) | 48 (52.2) | ||
| 65–74 | 264 (21.6) | 180 (20.2) | 84 (25.4) | 51 (19.2) | 31 (17.9) | 20 (21.7) | ||
| 75 or older | 437 (35.8) | 354 (39.8) | 83 (25.1) | 119 (44.9) | 99 (57.2) | 20 (21.7) | ||
| Patient sex | ||||||||
| Female | 488 (40.0) | 371 (41.7) | 117 (35.3) | 0.043 | 80 (30.2) | 60 (34.7) | 20 (21.7) | 0.029 |
| Male | 732 (60.0) | 518 (58.3) | 214 (64.7) | 185 (69.8) | 113 (65.3) | 72 (78.3) | ||
| Patient race | ||||||||
| White | 1,098 (90.0) | 788 (88.6) | 310 (93.7) | 247 (93.2) | 160 (92.5) | 87 (94.6) | ||
| American Indian/Alaska Native | 73 (6.0) | 63 (7.1) | 10 (3.0) | 0.035 | 8 (3.0) | 7 (4.0) | 1 (1.1) | 0.58 |
| Unknown | 40 (3.3) | 30 (3.4) | 10 (3.0) | 7 (2.6) | 4 (2.3) | 3 (3.3) | ||
| Black/African American | 9 (0.7) | 8 (0.9) | 1 (0.3) | 3 (1.1) | 2 (1.2) | 1 (1.1) | ||
| Patient ethnicity | ||||||||
| Hispanic/Latino | 16 (1.3) | 10 (1.1) | 6 (1.8) | 0.27 | 3 (1.1) | 1 (0.6) | 2 (2.2) | 0.44 |
| Not Hispanic/Latino | 1,146 (93.9) | 841 (94.6) | 305 (92.1) | 250 (94.3) | 165 (95.4) | 85 (92.4) | ||
| Unknown | 58 (4.8) | 38 (4.3) | 20 (6.0) | 12 (4.5) | 7 (4.0) | 5 (5.4) | ||
| Reason for visit—recorded data | ||||||||
| Chest pain | 772 (63.3) | 600 (67.5) | 172 (52.0) | 137 (51.7) | 91 (52.6) | 46 (50.0) | ||
| Other | 167 (13.6) | 166 (18.7) | 1 (0.3) | 26 (9.8) | 26 (15.0) | 0 (0.0) | ||
| Cardiac Arrest | 124 (10.2) | 0 (0.0) | 124 (37.5) | <0.001 | 45 (17.0) | 0 (0.0) | 45 (48.9) | <0.001 |
| Shortness of breath (dyspnea) | 53 (4.3) | 46 (5.2) | 7 (2.1) | 20 (7.5) | 20 (11.6) | 0 (0.0) | ||
| Arrival time (category) | ||||||||
| Bus hours (07.30–17.30) | 636 (52.1) | 468 (52.6) | 168 (50.8) | 0.56 | 131 (49.4) | 86 (49.7) | 45 (48.9) | 0.90 |
| Not bus hours | 584 (47.9) | 421 (47.4) | 163 (49.2) | 134 (50.6) | 87 (50.3) | 47 (51.1) | ||
| ED visit arrival day of work | ||||||||
| Monday | 202 (16.6) | 154 (17.3) | 48 (14.5) | 36 (13.6) | 23 (13.3) | 13 (14.1) | ||
| Tuesday | 154 (12.6) | 114 (12.8) | 40 (12.1) | 35 (13.2) | 21 (12.1) | 14 (15.2) | ||
| Wednesday | 164 (13.4) | 125 (14.1) | 39 (11.8) | 32 (12.1) | 24 (13.9) | 8 (8.7) | ||
| Thursday | 172 (14.1) | 118 (13.3) | 54 (16.3) | 41 (15.5) | 22 (12.7) | 19 (20.7) | ||
| Friday | 164 (13.4) | 111 (12.5) | 53 (16.0) | 0.19 | 42 (15.8) | 25 (14.5) | 17 (18.5) | 0.10 |
| Saturday | 177 (14.5) | 123 (13.8) | 54 (16.3) | 38 (14.3) | 24 (13.9) | 14 (15.2) | ||
| Sunday | 187 (15.3) | 144 (16.2) | 43 (13.0) | 41 (15.5) | 34 (19.7) | 7 (7.6) | ||
| Primary payer—recoded data | ||||||||
| Medicare only | 706 (57.9) | 532 (59.8) | 174 (52.6) | 170 (64.2) | 131 (75.7) | 39 (42.4) | ||
| Private Insurance | 351 (28.8) | 236 (26.5) | 115 (34.7) | 67 (25.3) | 27 (15.6) | 40 (43.5) | ||
| Medicaid only | 70 (5.7) | 58 (6.5) | 12 (3.6) | 7 (2.6) | 4 (2.3) | 3 (3.3) | ||
| Self-pay/uninsured | 59 (4.8) | 33 (3.7) | 26 (7.9) | 18 (6.8) | 8 (4.6) | 10 (10.9) | ||
| Indian Health Service | 23 (1.9) | 21 (2.4) | 2 (0.6) | 3 (1.1) | 3 (1.7) | 0 (0.0) | ||
| Other | 11 (0.9) | 9 (0.8) | 2 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| CPT code | ||||||||
| 99281 | 1 (0.1) | 0 (0.0) | 1 (0.3) | <0.001 | 0 (0.0) | 0 (0.0) | 0 (0.0) | <0.001 |
| 99282 | 12 (1.0) | 10 (1.1) | 2 (0.6) | 2 (0.8) | 1 (0.6) | 1 (1.1) | ||
| 99283 | 119 (9.8) | 97 (10.9) | 22 (6.6) | 7 (2.6) | 5 (2.9) | 2 (2.2) | ||
| 99284 | 548 (44.9) | 405 (45.6) | 143 (43.2) | 74 (27.9) | 51 (29.5) | 23 (25.0) | ||
| 99285 | 495 (40.6) | 368 (41.4) | 127 (38.4) | 154 (58.1) | 111 (64.2) | 43 (46.7) | ||
| 99291 | 29 (2.4) | 6 (0.7) | 23 (6.9) | 18 (6.8) | 2 (1.2) | 16 (17.4) | ||
| 99292 | 16 (1.3) | 3 (0.3) | 13 (3.9) | 10 (3.8) | 3 (1.7) | 7 (7.6) | ||
| AMI (Y/N) | ||||||||
| No | 955 (78.3) | 716 (80.5) | 239 (72.2) | 0.002 | 0 (0.0) | 0 (0.0) | 0 (0.0) | N/A |
| Yes | 265 (21.7) | 173 (19.5) | 92 (27.8) | 265 (100.0) | 173 (100.0) | 92 (100.0) | ||
| ED discharge disposition—recoded data | ||||||||
| Admitted to local inpatient facility | 654 (53.6) | 530 (59.6) | 124 (37.5) | <0.001 | 74 (27.9) | 69 (39.9) | 5 (5.4) | <0.001 |
| Transferred to another inpatient facility | 526 (43.1) | 341 (38.4) | 185 (55.9) | 190 (71.7) | 104 (60.1) | 86 (93.5) | ||
| Routine discharge | 38 (3.1) | 18 (2.0) | 20 (6.0) | 1 (0.4) | 0 (0.0) | 1 (1.1) | ||
| Other | 2 (0.2) | 0 (0.0) | 2 (0.6) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
Data are presented as median (IQR) for continuous measures, and n (%) for categorical measures.
AMI, acute myocardial infarction; ED, emergency department; IQR, interquartile range
Effect of Telemedicine on Chest Pain Care Process Measures
Time-to-ECG
Of the 331 telemedicine subjects, most ECGs (64.7%) were performed before telemedicine consultations, and this did not differ between the AMI and non-AMI subjects (68.5% AMI vs. 63.2% non-AMI, p = 0.366). Subjects receiving telemedicine had shorter time-to-ECG compared with those who did not have telemedicine consults in the ED (median: telemedicine 8 min [95% confidence interval; CI: 5–15 min] vs. nontelemedicine 12 min [95% CI: 7–22 min], p < 0.001) (Table 2). Adjusting for age, sex, CPT code, and race, total time-to-ECG was, on average, 0.39 times (95% CI −0.52 to −0.26) faster for patients presenting with chest pain who received telemedicine compared with those that did not receive telemedicine consultations. Among patients diagnosed with AMI, total time-to-ECG was, on average, 0.58 times (95% CI −0.87 to −0.28) faster with the use of telemedicine (Table 3).
Table 2.
Outcomes by TeleED Exposure Status Among Chest Pain and Acute Myocardial Infarction Subjects
| ALL CHEST PAIN AND AMI SUBJECTS |
AMI ONLY SUBJECTS |
|||||||
|---|---|---|---|---|---|---|---|---|
| TOTAL (N = 1,220) | NO teleED (N = 889) | teleED (N = 331) | p | TOTAL (N = 265) | NO teleED (N = 173) | teleED (N = 92) | p | |
| Time from ED arrival to ECG (category), n (%) | ||||||||
| ≤10 Min | 572 (46.9) | 364 (40.9) | 208 (62.8) | <0.001 | 135 (50.9) | 76 (43.9) | 59 (64.1) | 0.001 |
| 11–30 Min | 479 (39.3) | 387 (43.5) | 92 (27.8) | 93 (35.1) | 64 (37.0) | 29 (31.5) | ||
| 31–60 Min | 124 (10.2) | 105 (11.8) | 19 (5.7) | 30 (11.3) | 28 (16.2) | 2 (2.2) | ||
| >60 Min | 45 (3.7) | 33 (3.7) | 12 (3.6) | 7 (2.6) | 5 (2.9) | 2 (2.2) | ||
| Time from ED arrival to ECG (min) | ||||||||
| 11 (6–21) | 12 (7–22) | 8 (5–15) | <0.001 | 10 (5–20) | 12 (6–24) | 9 (5–14) | <0.001 | |
| Fibrinolytic administered (Y/N), n (%) | ||||||||
| No | 68 (5.6) | 48 (5.4) | 20 (6.0) | 42 (15.8) | 31 (17.9) | 11 (12.0) | <0.001 | |
| Not Eligible | 165 (13.5) | 132 (14.8) | 33 (10.0) | 161 (60.8) | 128 (74.0) | 33 (35.9) | ||
| Yes | 62 (5.1) | 14 (1.6) | 48 (14.5) | 62 (23.4) | 14 (8.1) | 48 (52.2) | ||
| NA | 925 (75.8) | 695 (78.2) | 230 (69.5) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| Time from ED arrival to fibrinolytic administration (category), n (%) | ||||||||
| Missing | 203 (76.6) | 159 (91.9) | 44 (47.8) | <0.001 | ||||
| ≤30 min | 19 (7.2) | 2 (1.2) | 17 (18.5) | |||||
| 31–60 Min | 24 (9.1) | 7 (4.0) | 17 (18.5) | |||||
| 61–90 Min | 15 (5.7) | 5 (2.9) | 10 (10.9) | |||||
| 91–120 Min | 4 (1.5) | 0 (0.0) | 4 (4.3) | |||||
| Time from ED arrival to fibrinolytic administration (min) | ||||||||
| 44.5 (28–62) | 48 (37–68) | 44 (26.5–62) | 0.32 | |||||
ECG, electrocardiogram.
Table 3.
Association of TeleED Exposure with Myocardial Infarction Process Outcomes
| N | β/OR | 95% CI | p | β (adj)*/AOR* | 95% CI | p | |
|---|---|---|---|---|---|---|---|
| Time- to-ECG** (logarithmic transform) | |||||||
| AMI and chest pain | 1,220 | −0.39 | −0.51 to −0.26 | <0.001 | −0.39 | −0.52 to −0.26 | <0.001 |
| AMI-only | 265 | −0.59 | −0.85 to −0.34 | <0.001 | −0.58 | −0.87 to −0.28 | <0.001 |
| Fibrinolysis administered (yes/no) | 103a | 10.59 | 4.43 to 25.53 | <0.001 | 7.17# | 2.48 to 20.49 | <0.001 |
| Time-to-fibrinolysis** (logarithmic transform) | 61b | −0.30 | −0.60 to 0.01 | 0.054 | −0.33 | −0.62 to −0.03 | 0.030 |
Among ST-elevation myocardial infarction subjects who were fibrinolysis eligible.
Among ST-elevation myocardial infarction subjects who received fibrinolysis.
Adjusted for: age (categorical), sex, CPT code (categorical), and race.
Coefficients are relative time-to-ECG/fibrinolysis for teleED group compared with non-teleED group. For example, in the adjusted model for AMI and chest pain subjects, total time-to-ECG (in minutes) is, on average, 0.39 faster for teleED subjects compared with non-teleED subjects.
Adjusted for: age (categorical), sex, and CPT code (categorical).
AOR, adjusted odds ratio; CPT, current procedural terminology.
Fibrinolysis administration and timeliness
Of the 265 patients diagnosed with AMI, 103 (38.9%) were eligible for fibrinolysis. Among the eligible subjects, 62 (60.2%) received fibrinolytic therapy during their ED visit. When eligible, subjects who received telemedicine were more likely to receive fibrinolysis compared with eligible subjects without telemedicine consults (adjusted odds ratio 7.17, 95% CI 2.48–20.49). Among those who received fibrinolytic therapy, there was no difference in time-to-administration between subjects who received telemedicine and those without telemedicine consults (median: telemedicine 44 min [95% CI: 26.5–62 min] vs. nontelemedicine 48 min [95% CI: 37–68 min], p = 0.32) (Table 2). However, after adjustment for age, sex, and CPT code, time-to-fibrinolysis administration was, on average, 0.33 times (95% CI −0.62 to −0.03) faster with the use of telemedicine (Table 3).
Variations in the effects of telemedicine for groups that may experience differences in AMI treatment, including women, elderly (65+ and 75+), and nonwhite patients, were measured by using interaction terms. There were no significant differences (p > 0.05) in the magnitude of the effect of telemedicine on time-to-treatment or fibrinolysis administration for any of the groups.
Sensitivity Analysis
There were 124 subjects with cardiac arrest as the reason for ED visit. In a sensitivity analysis excluding these subjects, telemedicine remained associated with a decreased time-to-ECG compared with those who did not receive telemedicine in both the total and AMI only cohorts (Supplementary Table S1). Fibrinolysis administration also remained more likely in the telemedicine group, but there was not a difference in time-to-fibrinolysis in this restricted cohort (Supplementary Table S1).
Discussion
Achieving guideline-recommended time metrics for AMI care is a challenge, especially in rural areas. Multiple reports have suggested that prehospital telemedicine strategies can be implemented to improve the timeliness of AMI care, but a few studies have reported the value of ED-based telemedicine to further increase the proportion of rural patients receiving timely AMI care, despite rapid adoption in many rural hospitals. This study evaluated the benefit of ED-based telemedicine consultation on process outcomes for AMI care. In this cohort of telemedicine networks, telemedicine consultation during the ED visit was associated with shorter time-to-ECG for patients presenting with chest pain. In addition, when eligible, telemedicine subjects were more likely to receive fibrinolysis.
Our findings of the positive effect of telemedicine on the administration of fibrinolysis are consistent with previous findings. Multiple reports evaluating both the impact of prehospital telemedicine interventions on cardiac care (i.e., prehospital ECG transmission) and ED-based telemedicine consultation for other clinical conditions (i.e., stroke) have suggested that telemedicine can improve the use and timeliness of fibrinolysis administration.14,18,19,24 The association between telemedicine and increased use of fibrinolysis could be either causal or reverse causal. Emergency clinicians who appropriately diagnose STEMI could be selecting to use telemedicine to facilitate interhospital transfer or rapid decision making. This observation is supported by the finding that a few patients received fibrinolysis without telemedicine and that telemedicine subjects were more likely to be transferred to another inpatient facility than those who did not receive telemedicine during their ED visit. Emergency clinicians could also be utilizing telemedicine to facilitate transfer for AMI patients to receive cardiac catheterization at another hospital. In this cohort, most telemedicine patients received fibrinolysis at the index ED, suggesting that telemedicine may be used for decision support or subsequent transfer and placement for cardiac catheterization. Even if local clinicians have already selected patients for fibrinolysis, the infrequency with which these patients present in rural hospitals leads to providers' seeking additional assistance, which is highly valued during time-urgent critical cases.25
One of the most interesting findings is the robust effect of telemedicine consultation on decreased time-to-ECG for patients presenting with chest pain. This finding could be evidence of a change in provider behavior and care processes due to telemedicine interactions. We previously hypothesized that ECGs may be performed sooner if local staff prioritized the ECG earlier because they sensed that staff at the telemedicine hub expected the ECG to be performed more quickly.24 Telemedicine staff may also represent the additional resources (i.e., staff) that are necessary to streamline care in rural hospitals. Prior studies have reported that local nurses feel less stressed and burdened with the use of telemedicine. The additional monitoring and documenting by telemedicine staff may relieve nurses to perform ECGs earlier in the care of a patient.25–27
In this study, we observed that telemedicine led to a decrease in time-to-ECG. However, these observations are not consistent with our prior findings, in which telemedicine activation had no effect on time-to-ECG or time-to-fibrinolysis for AMI patients.24 One reason for these novel findings may be due to temporal changes in care processes. Earlier, CAHs were not required to report on specific quality measures, but this changed beginning in 2015, when the Federal Office of Rural Health Policy began requiring every CAH to participate in the Medicare Beneficiary Quality Improvement Project (MBQIP), an initiative designed to increase quality data reporting and improve quality of care within CAHs.28 In addition, rather than collecting data from a simple EMR query, as was previously used to collect data, data for this report were collected by trained abstractors and then processed by a central data coordinating and analysis center, which performed validation checks to ensure a high level of quality assurance. Current data benefits from both the increased quality reporting by CAHs and enhanced quality assurance, which increases confidence in the accuracy and reliability of these findings.
This study provides novel insight into the benefits of telemedicine consultation in the clinical management of ED AMI care. Although previous studies have indicated that telemedicine interventions in the prehospital setting can improve the timeliness of AMI care,14 this study evaluates ED-based telemedicine networks to provide a broader analysis of telemedicine strategies in AMI. This is the first study to evaluate the impact of telemedicine for AMI care within multiple telemedicine networks to estimate the real-world effect of telemedicine use on clinical care. The findings of the benefit of telemedicine consultation on both the rate and timeliness of critical actions in AMI care support the value of telemedicine in changing care processes and improving the quality of rural AMI care. Further, the impact of telemedicine on timeliness suggests that telemedicine networks may be a resource to improve quality-of-care metrics for rural EDs.
Our study has several limitations. First, data were collected prospectively from ED medical records. Although this design allowed for robust measurement of time-based metrics, it also restricted the available measures of disease severity. Quantitative information about the severity of AMI would be an ideal measure. As this was not available, the CPT code for ED Evaluation and Management was used as a proxy measure for severity of illness at ED arrival.29,30 To limit the influence of selection bias, estimates were adjusted for CPT code as well as patient-level characteristics, but residual bias may still remain in the reported estimates. In addition, this study was limited to data collected during the ED encounter and, therefore, does not include long-term clinical or functional outcomes. The impact of telemedicine consultation on these patient- and policy-relevant outcomes remains an important question.
In conclusion, the use of ED-based telemedicine consultation improved the timeliness of evaluation and treatment for rural patients with AMI. Telemedicine was also associated with a higher proportion of fibrinolytic reperfusion therapy among eligible patients. These data support previous research that telemedicine can improve the quality of time-sensitive care in rural hospitals. Future work should focus on evaluating the effects of telemedicine on patient-centered outcomes.
Supplementary Material
Acknowledgments
The authors thank Amanda Bell (PI), Luke Mack, Amy Wittrock from Avera Health; Eric Pollard (PI), Martha Nikides from St. Vincent Healthcare; Stephanie Laws (PI), Hicham Rahmouni, Daniel Hardesty, and Amanda O'Brien from Union Hospital; James Marcin (PI), Jamie Mouzoon from University of California-Davis; Roger Humphries (PI), Brian Dennis, Theresa Mims, and Rob Sprang from University of Kentucky; and Nina Solenski (PI), Tracy Blount from University of Virginia for contributing data for these analyses.
Disclaimer
The findings and conclusions are those of the author(s), who are responsible for its content, and do not necessarily represent the views of Agency for Health care Research and Quality (AHRQ).
Disclosure Statement
No competing financial interests exist.
Funding Information
This study was supported by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) to the Rural Telehealth Research Center under cooperative agreement #UICRH29074. The Evidence-Based Tele-Emergency Network Grant Program provided funding for delivering teleED services to grantees—Avera Health (PI: Amanda Bell, Grant No. GO1RH27868), Saint Vincent Health care (PI: Eric Pollard, Grant No. G01RH27870), Union Hospital (PI: Stephanie Laws, Grant No. G01RH27871), University of California, Davis (PI: James Marcin, Grant No. G01RH27872), University of Kentucky (PI: Roger Humphries, Grant No. G01RH27873), and University of Virginia (PI: Nina Solenski, Grant No. G01RH27869). The information, conclusions, and opinions expressed are those of the authors and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred. Dr. Mohr is additionally supported by grant K08 HS025753 from the Agency for Health care Research and Quality (AHRQ).
Supplementary Material
References
- 1. Benjamin EJ, Virani SS, Callaway CW, et al. Heart disease and stroke statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67.–e492. [DOI] [PubMed] [Google Scholar]
- 2. Rui P, Kang K, Ashman JJ National Hospital Ambulatory Medical Care Survey: 2016. emergency department summary tables. Available at https://www.cdc.gov/nchs/data/nhamcs/web_tables/2016_ed_web_tables.pdf (last accessed June15, 2019)
- 3. Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction). Circulation 2004;110:e82.–e292. [PubMed] [Google Scholar]
- 4. Boersma E, Maas AC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: Reappraisal of the golden hour. Lancet 1996;348:771.–775. [DOI] [PubMed] [Google Scholar]
- 5. Baigent C, Collins R, Appleby P, et al. ISIS-2: 10 year survival among patients with suspected acute myocardial infarction in randomised comparison of intravenous streptokinase, oral aspirin, both, or neither. The ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. BMJ 1998;316:1337.–1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jollis JG, Al-Khalidi HR, Roettig ML, et al. Impact of regionalization of ST-segment-elevation myocardial infarction care on treatment times and outcomes for emergency medical services-transported patients presenting to hospitals with percutaneous coronary intervention: Mission: Lifeline Accelerator-2. Circulation 2018;137:376.–387. [DOI] [PubMed] [Google Scholar]
- 7. McMullan JT, Hinckley W, Bentley J, et al. Ground emergency medical services requests for helicopter transfer of ST-segment elevation myocardial infarction patients decrease medical contact to balloon times in rural and suburban settings. Acad Emerg Med 2012;19:153.–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baldwin LM, MacLehose RF, Hart LG, et al. Quality of care for acute myocardial infarction in rural and urban US hospitals. J Rural Health 2004;20:99.–108. [DOI] [PubMed] [Google Scholar]
- 9. Sheikh K, Bullock C. Urban-rural differences in the quality of care for medicare patients with acute myocardial infarction. Arch Intern Med 2001;161:737.–743. [DOI] [PubMed] [Google Scholar]
- 10. Abrams TE, Vaughan-Sarrazin M, Kaboli PJ. Mortality and revascularization following admission for acute myocardial infarction: Implication for rural veterans. J Rural Health 2010;26:310.–317. [DOI] [PubMed] [Google Scholar]
- 11. Bhuyan SS, Wang Y, Opoku S, Lin G. Rural-urban differences in acute myocardial infarction mortality: Evidence from Nebraska. J Cardiovasc Dis Res 2013;4:209.–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rosenberg BL, Kellar JA, Labno A, et al. Quantifying geographic variation in health care outcomes in the United States before and after risk-adjustment. PLoS One 2016;11:e0166762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Health Resources and Services Administration, Department of Health and Human Services. Rockville, MD, Area Resource File (ARF), 2012
- 14. Marcolino MS, Maia LM, Oliveira JAQ, et al. Impact of telemedicine interventions on mortality in patients with acute myocardial infarction: A systematic review and meta-analysis. Heart 2019;105:1479.–1486. [DOI] [PubMed] [Google Scholar]
- 15. de Waure C, Cadeddu C, Gualano MR, Ricciardi W. Telemedicine for the reduction of myocardial infarction mortality: A systematic review and a meta-analysis of published studies. Telemed J E Health 2012;18:323.–328. [DOI] [PubMed] [Google Scholar]
- 16. Ward MM, Jaana M, Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform 2015;84:601.–616. [DOI] [PubMed] [Google Scholar]
- 17. Mohr NM, Harland K, Chrischilles E, Donner J, Bell A, Shane DM, Ward MM. Telemedicine penetration and consultation among rural trauma patients in critical access hospital emergency departments in North Dakota. Res Policy Brief 2016:1–4 [Google Scholar]
- 18. Müller-Barna P, Hubert GJ, Boy S, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke 2014;45:2739.–2744. [DOI] [PubMed] [Google Scholar]
- 19. Nguyen-Huynh MN, Klingman JG, Avins AL, et al. Novel Telestroke Program improves thrombolysis for acute stroke across 21 hospitals of an Integrated Healthcare System. Stroke 2018;49:133.–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mohr NM, Vakkalanka JP, Harland KK, et al. Telemedicine use decreases rural emergency department length of stay for transferred North Dakota Trauma Patients. Telemed J E Health 2018;24:194.–202. [DOI] [PubMed] [Google Scholar]
- 21. Heppner S, Mohr N, Carter K, Ullrich F, Merchant KAS, Ward MM. HRSA's Evidence-Based Tele-Emergency Network Grant Program: Multi-site prospective cohort analysis across six rural tele-emergency networks. PLoS Med 2019. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344.–349. [DOI] [PubMed] [Google Scholar]
- 23. Creating a Framework to Support Measure Development for Telehealth: National Quality Forum 2017. www.qualityforum.org/publications/2017/08/creating_a_Framework_to_support_measure_development_for_telehealth.aspx (last accessed February21, 2020)
- 24. Mohr NM, Young T, Harland KK, et al. Telemedicine is associated with faster diagnostic imaging in stroke patients: A Cohort Study. Telemed J E Health 2019;25:93.–100. [DOI] [PubMed] [Google Scholar]
- 25. Ward MM, Ullrich F, MacKinney AC, et al. Tele-emergency utilization: In what clinical situations is tele-emergency activated? J Telemed Telecare 2016;22:25.–31. [DOI] [PubMed] [Google Scholar]
- 26. Ward MM, Ullrich F, Potter AJ, et al. Factors affecting staff perceptions of Tele-ICU Service in rural hospitals. Telemed J E Health 2015;21:459.–466. [DOI] [PubMed] [Google Scholar]
- 27. Westbrook JI, Coiera EW, Brear M, et al. Impact of an ultrabroadband emergency department telemedicine system on the care of acutely ill patients and clinicians' work. Med J Aust 2008;188:704.–708. [DOI] [PubMed] [Google Scholar]
- 28. MBQIP Fundamentals Guide for State Flex Programs: Rural Quality Improvement Technical Assistance, 2019
- 29. Mohr NM, Dick-Perez R, Ahmed A, et al. Emergency department charges may be associated with mortality in patients with severe sepsis and septic shock: A cohort study. BMC Emerg Med 2018;18:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Alessandrini EA, Alpern ER, Chamberlain JM, et al. Developing a diagnosis-based severity classification system for use in emergency medical services for children. Acad Emerg Med 2012;19:70.–78. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


