Abstract
Organoids are 3D cell culture systems that mimic some of the structural and functional characteristics of an organ. Organoid cultures provide the opportunity to study organ-level biology in models that mimic human physiology more closely than 2D cell culture systems or non-primate animal models. Many organoid cultures rely on decellularized extracellular matrices as scaffolds, which are often poorly chemically defined and allow only limited tunability and reproducibility. By contrast, the biochemical and biophysical properties of engineered matrices can be tuned and optimized to support the development and maturation of organoid cultures. In this Review, we highlight how key cell-matrix interactions guiding stem-cell decisions can inform the design of biomaterials for the reproducible generation and control of organoid cultures. We survey natural, synthetic and protein-engineered hydrogels for their applicability to different organoid systems and discuss biochemical and mechanical material properties relevant for organoid formation. Finally, dynamic and cell-responsive material systems are investigated for their future use in organoid research.
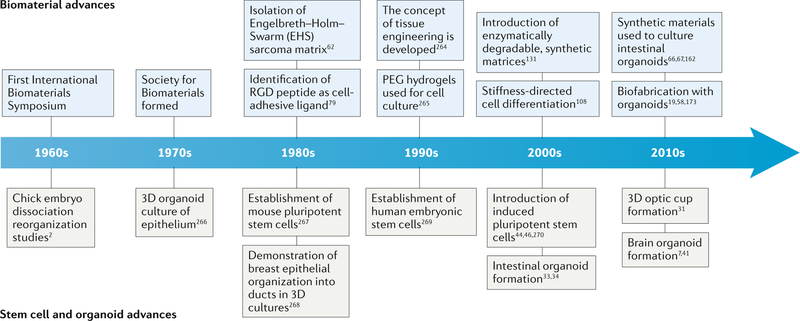
Organoids are 3D cell culture systems that are formed through cell differentiation and self-organization of pluripotent stem cells or tissue-derived progenitor cells, which can contain supporting stromal elements. The foundation of tissue culture was laid in 1907, when Harrison et al. cultured dissected frog neural tubes1. Cell culture studies were continued throughout the 20th century to describe the embryonic development of organs by observing tissue reorganization after dissociation2,3 (FIG. 1 ), which led to the identification of cell sorting and cell-fate specification during organogenesis and the powerful innate ability of cells to spontaneously organize into complex structures in vitro. Organoids are a class of microphysiological systems that provide platforms to model the features of organs and tissues in an in vitro setting4. The terminology in the field remains to be universally defined5 and terms such as organoid, organotypic culture, spheroid, enteroid and assembloid are used by different communities for different 3D cell culture systems. For example, for gastrointestinal tissues, the term organoid has been suggested for cultures that contain both epithelial and mesenchymal or stromal components, whereas the term enteroid has been used for 3D cultures that contain only epithelial cells6. By contrast, spheroid has been used to describe either aggregates of cells or region-specific brain organoids7. In this Review, the term organoid is used to describe all of these complex, multicellular systems.
Fig. 1 |. Timeline of milestones for biomaterials, organoids and stem cells.
PEG, polyethylene glycol.
Microphysiological systems usually contain two or more interacting cell types, which are in contact with each other and embedded in a matrix (either cell-secreted or externally introduced) or in a device with the aim to partially mimic cellular interactions and/or functions of a tissue or organ in vitro. These systems represent an important intermediary between conventional 2D cell culture systems and animal models, allowing the precise and reproducible investigation of the effects of experimental conditions on cell and tissue behaviour. Organoid cultures have great potential to transform drug development and disease research, as drug tests and disease studies have traditionally mostly relied on 2D in vitro cell culture assays or animal models. 2D cell culture models are simple and have a high throughput but they fail to capture the physiological complexity of entire tissues and organisms8,9. In particular, the modelling of brain development remains challenging, as this process requires months to years in humans and other primates, which is difficult to recreate in 2D in vitro cultures10. Animal models are important for basic and applied research but are time consuming, expensive and often limited by species-specific anatomy and physiology, which can make them less relevant for the investigation of human biology and pathology11,12. Advances in cell biology, biomaterials design and imaging techniques have enabled the investigation of increasingly complex biological questions; however, a gap remains between single-cell-type culture systems and actual tissues. Therefore, more sophisticated and physiologically relevant in vitro tissue models are required to study human biology and medicine13–15.
Organoids have the advantage of being based on human cells cultured in a physiologically meaningful context, that is, multiple interacting cell types with spatial organization. In contrast to other microphysiological platforms, such as organ-on-a-chip culture systems, in which cellular organization is externally imposed and nutrient supply and physiological levels of shear forces are achieved by using microfluidic chambers16, organoids are typically cultured in static 3D conditions, in which cells self-assemble into multicellular entities with an architecture similar to real tissues. By contrast, in organ-on-a-chip systems, differentiated cells are usually placed at specific regions within a device, which does not allow higher-level cell sorting or ordering16,17. However, organ-on-a-chip platforms and organoid cultures both strive to accurately model physiological behaviours that require multicellular interactions, and they can be combined by incorporating cellular spheroids and organoids into organ-on-a-chip systems18–21.
Organoid cultures typically arise from stem cells that undergo proliferation, differentiation and self-organization22,23. Organoid generation can, in principle, be scaled up, making high-throughput testing possible24,25; however, organoids are in an early stage of development and need more robust and dependable culturing practices. Therefore, to realize the full potential of organoids, technologies are required that improve organoid generation and reliability and that allow the development of key tissue-specific features26. The exploitation of specific stem-cell signalling pathways that are responsible for driving organoid formation require a precise extracellular environment. In vivo, changes in extracellular matrix (ECM) properties can have a profound influence on cellular phenotype, and abnormal ECMs are often considered a driver of disease27,28. In the absence of externally added matrices, organoids self-organize and secrete and develop their own ECM29, which has not yet been fully characterized. The development and application of well-defined 3D biomaterials that support and promote organoid formation, and that mimic the properties of healthy or diseased tissue, is an exciting research area that has the potential to greatly improve the reproducibility and human relevance of organoids. In particular, synthetic biomaterials can provide a chemically defined matrix that enables the precise tuning of matrix properties to influence and guide cellular decisions.
In this Review, the development of organoid cultures is discussed, with a focus on biomaterial properties that are crucial for 3D cell culture systems. We highlight state-of-the-art engineered material systems for culturing organoids and discuss opportunities for the development of next-generation materials systems designed with the aim to establish organoid cultures as powerful research platforms.
Organoid culture systems
From single cells to organoids
The formation of organoids requires the proliferation and reorganization of single cells, or small cell clusters, into complex and organized cell structures that mimic some of the structural and functional features of a specific organ. The generation of these structures occurs by a number of mechanisms, including physical rearrangement, spatial distribution of gene expression, cell sorting and fate specification30. A variety of organoid types and combinations have been explored thus far, including the optic cup31,32, intestine33,34, kidney35,36, lung37, pancreas38,39, thymus40 and various types of brain tissues7,41–44. Although individual organoid protocols vary and are idiosyncratic, shared culturing considerations have been developed.
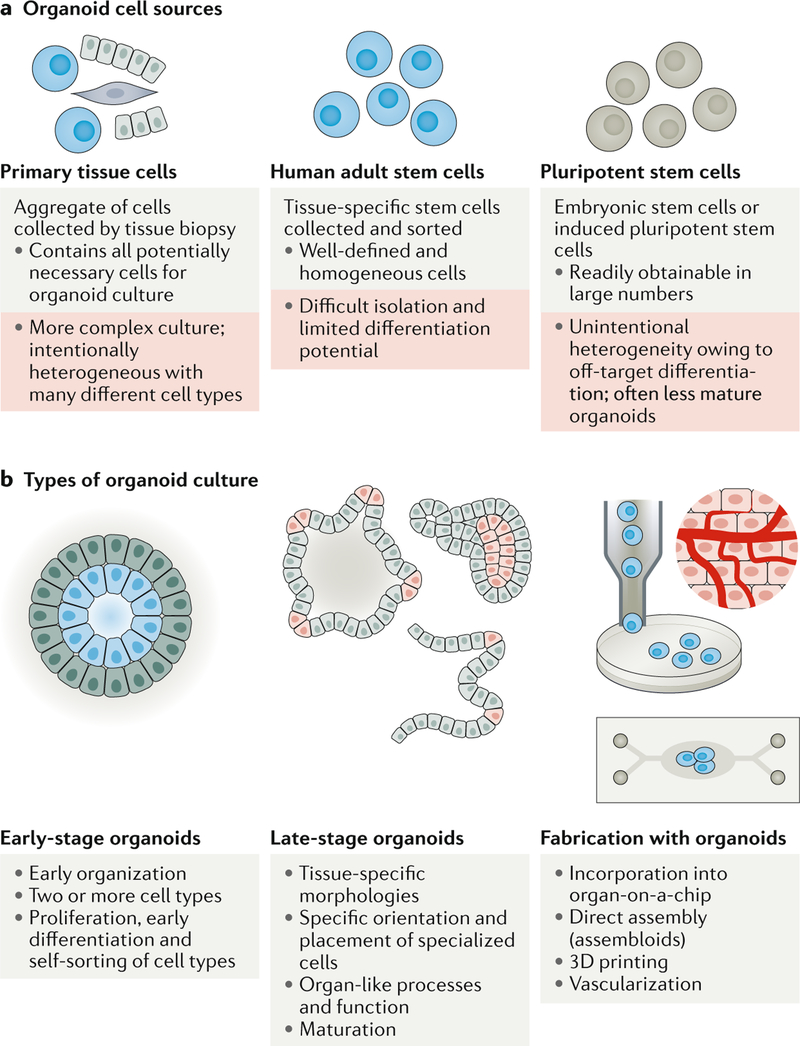
Organoids can be derived from primary tissue or differentiated from pluripotent stem cells (FIG. 2a). For example, embryonic stem cells (ESCs) or induced pluripotent stem cells (iPSCs) can be used as a cell source22. iPSCs, which are often reprogrammed from fibroblasts, have the advantage of being easy to obtain and patient specific45,46. ESCs and iPSCs are pluripotent and can differentiate into nearly any tissue type46. The resulting heterogeneity of cell types within a pluripotent stem-cell-derived organoid culture can be an advantage when trying to mimic the complexity of native tissues47–49. However, unintentional heterogeneity of pluripotent stem-cell-derived cultures50–52 and incomplete knowledge about specific differentiation signals may have undesired downstream consequences for the resulting organoids. For example, single-cell transcriptomics studies have shown that iPSC-derived and ESC-derived kidney organoids include 10–20% non-renal cells, such as brain and muscle cells53. Furthermore, pluripotent stem-cell-derived organoids can exhibit gene expression patterns that are more reminiscent of fetal tissues than of their adult counterparts15,54,55. Alternatively, excised organ tissue, which contain adult stem cells, can serve as a precursor cell source for organoids. For example, intestinal organoids can be generated through the expansion of biopsies of intestinal tissue, which contains intestinal stem cells34. These organoids provide a patient-specific cell culture of the intestinal area sampled by the biopsy, allowing the investigation of intestine pathophysiology and of potential treatments.
Fig. 2 |. Organoid cell sources and types.
a | The initial cells used for organoid culture can be human adult stem cells, pluripotent stem cells or primary tissues collected via biopsy. Each cell type has associated advantages and disadvantages as a source for organoids. b | Although each type of organoid develops with unique morphological and physiological features, a general pattern of development is followed. Different studies may desire organoids in different stages of development or fabrication platforms. The proliferation and early differentiation of single cells and cell clusters leads to the generation of early-stage organoids, sometimes referred to as spheroids. Late-stage organoids are structures that resemble native tissue morphology, contain correctly oriented and specialized cells, and display organ-like processes. Organoid cultures are often placed within a 3D matrix at the single-cell or spheroid phase. The physiological relevance and complexity of organoids can be improved by various biofabrication techniques.
The precise organoid formation process varies for each tissue type but generally follows the pattern of proliferation, differentiation, cell sorting, lineage commitment and morphogenesis, resulting in a 3D organoid structure (FIG. 2b). Organoid formation is usually guided by culturing cells in medium that contains factors that promote or inhibit specific signalling pathways, directing the culture towards the cell lineages of interest23. Some protocols also use an undirected differentiation approach that deliberately omits inductive signals41. Given that ectoderm is the default stem-cell fate, such protocols generate many cell types found in the brain41. Variation in the proliferation and differentiation of stem cells leads to a heterogeneous collection of cells. In directed-differentiation approaches, small molecules and growth factors are used to restrict cell fates, for example, for the generation of brain-region-specific organoids7. These cultures can undergo further morphogenesis to form late-stage organoids, which contain specialized cell types that give rise to organotypic structures and functions. For example, intestinal organoids show a crypt and villi-like morphology and contain specialized epithelial cells, such as goblet, Paneth and enteroendocrine cells33, which often secrete mucus into the lumina of the structure34. By contrast, opticcup organoids display characteristic inward folding31. These later-stage processes can occur over hundreds of days7,56. For example, astrocytes only begin to appear in directed brain organoids after 100 days in culture, and they switch to a postnatal gene expression profile only after 280 days in culture57. Organoids can also be combined with other organoids or cell types to generate assembloids. For example, dorsal and ventral forebrain organoids can be assembled to model the migration and functional integration of γ-aminobutyric acid (GABA) ergic interneurons and to identify defects associated with epilepsy and autism spectrum disorders58.
Organoid culture protocols
Once the cell source is selected (either primary tissue or pluripotent stem cells that have been provided with initial differentiation cues), the subsequent culture protocols are largely similar. Organoid culture protocols typically use a homogenous culture medium without any intentionally applied gradients of nutrients or gases and require the cells to be suspended or encapsulated in a 3D environment that permits the cells to freely grow and remodel their environment, and engage in self-directed cell sorting without any top-down, investigator-imposed guidance on spatial cell patterning. Uninhibited growth can be accomplished by culturing cells in low attachment conditions or in a naturally derived hydrogel, such as a reconstituted, decellularized ECM (for example, Matrigel). In low attachment conditions, stem cells, either dissociated31,59,60, in the form of colonies7 or as preaggregated clusters56, are transferred to plates with surfaces that prevent cell adhesion. Forced to float in suspension, these clumps of cells differentiate and proliferate in 3D, forming an organoid. Additionally, motion and shear forces can be applied using devices such as spinning bioreactors61.
Matrices are often used as a 3D culture environment that mimics the scaffolding support provided by the native ECM of the tissue, for example, hydrogels made of reconstituted decellularized ECM. The Engelbreth-Holm-Swarm (EHS) matrix, which is a reconstituted basement membrane harvested from mouse sarcoma62 and known by the trade names Matrigel, Geltrex and Cultrex BME, has been pivotal in the development of the organoid field. The EHS matrix is a mixture of many different ECM components and other biological factors62, which provide a complex environment for embedded cells (Box 1). This matrix has sufficient natural, cell-adhesive domains to promote cell attachment and can be degraded and remodelled by enzymes expressed in the developing organoid. However, the EHS matrix suffers from batch-to-batch variability, is not suitable for clinical translation and cannot be easily tailored to meet the diverse requirements of unique organoid niches.
Box 1 |. The trouble with Matrigel.
The Engelbreth-Holm-Swarm (EHS) matrix is widely used in the organoid field. However, relying on an EHS matrix likely hinders more precise studies of organoid-microenvironment interactions and creates issues with culture reproducibility and clinical translation. An EHS matrix is made of several extracellular matrix components, primarily laminin, collagen type IV and nidogen, secreted by EHS cells in mice62. Analysis of different batches of EHS matrices has identified over 1,500 unique peptides and proteins168, making careful chemical characterization of the material impractical for most users. Additionally, batch-to-batch variation of EHS matrices limits reproducibility243. Within the complex mixture of proteins in an EHS matrix, only ~53% are found consistently in each lot168. Thus, EHS matrices offer no direct control over the concentration and identity of cell-binding ligands. In addition, this complex component mixture can influence cell cultures in unexpected ways. For example, an EHS matrix contains growth-factor-binding proteins, which could lead to growth-factor sequestration and a heterogeneous cellular response168. EHS matrices are soft materials with stiffnesses of ~20–450 Pa (REFs244,245) compared with tissues, which typically have stiffnesses of ~100–100,000 Pa. Moreover, the physical properties of EHS matrices cannot be tuned. The mouse tumour origin of the material also excludes the use of EHS matrices for organoids intended to be transplanted into the body, limiting the translational potential of EHS-matrix-based cultures246. The EHS matrix is an important material for organotypic cultures that do not grow in other well-defined materials; however, the minimal matrix requirements for organoid growth and development need to be characterized to inform the design of a more reliable, tunable and clinically translatable alternative.
Cell-matrix interactions
Understanding how cells sense and respond to their surrounding matrix is crucial for the development of engineered materials for organoids. Thus far, cell-matrix interactions have mainly been investigated for single-cell-type cultures seeded on or within a matrix63. Although these homogeneously dispersed, single-cell-type cultures are simpler than organoid cultures, they, nonetheless, provide important lessons for designing matrices to direct cell behaviour in 3D.
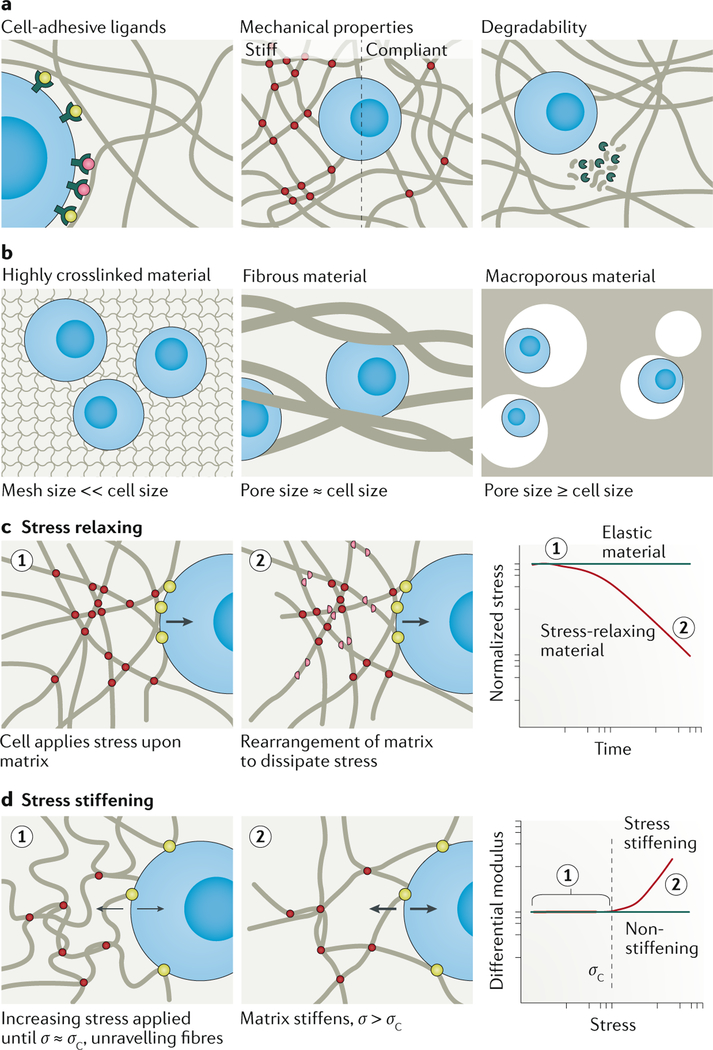
Cell-adhesive ligand presentation, mechanical properties, matrix geometry and matrix remodelling are the key parameters impacting cell culture63 (FIG. 3a,b). Although often discussed and studied individually, these properties are intrinsically intertwined. The relative influence of individual matrix properties on a cell is determined, in part, by the greater context of the entire system64. Furthermore, how the modification of a specific property impacts cell behaviour cannot necessarily be predicted a priori without considering other matrix features.
Fig. 3 |. Cell-matrix interactions.
a | The matrix microenvironment influences cellular behaviour by cell-matrix interactions established by cell-adhesive ligands bound to cell-surface receptors, by the mechanical properties of the matrix (for example, stiffness) and by the degradability of the matrix. b | The 3D geometry of the matrix can be described by the relative pore or mesh size compared with the cell size. Matrix geometry defines the nature of cell-matrix contacts and how a cell senses other matrix properties, such as cell-adhesive ligands or mechanical properties. Fibrous matrices, for example, natural extracellular matrix and biomaterials such as collagen, have a pore size on approximately the scale of cells. Highly crosslinked hydrogels, such as polyethylene glycol hydrogels, have mesh sizes much smaller than the scale of a cell, which can inhibit cell growth and migration in the absence of degradability. Macroporous materials have large pores that can be on the scale of a cell or larger. c | Viscoelastic materials, for example, native extracellular matrix, display stress-relaxation behaviour. Upon application of stress to the matrix, the molecules rearrange to dissipate the stress over time. By contrast, elastic materials cannot dissipate stress. Plotting normalized stress versus time of a stress-relaxing material and an elastic material under constant strain shows that the stress in a stress-relaxing material decreases over time, whereas it remains constant in an elastic material. d | In materials with stress-stiffening behaviour, an applied stress (σ) that is greater than the characteristic critical stress point (σc) leads to stiffening of the material, owing to local molecular stretching. The modulus of a non-stiffening material remains the same regardless of the applied stress, whereas the modulus of a stress-stiffening material increases once σ > σc.
Owing to their clinical relevance and easy accessibility, mesenchymal stem cells or mesenchymal stromal cells (MSCs) have been extensively investigated in single-cell-type cultures in or on engineered matrices. Referring to MSCs as stem cells remains controversial and is likely a historical misnomer65; however, studies with this cell type have greatly enriched the understanding of cell-matrix dynamics and provide useful information for the de novo design of matrices for organoids. Interestingly, although many organoids are formed by epithelial, as opposed to mesenchymal, stem or progenitor cells, lessons learned from MSC-matrix interaction studies could be directly applied for the development of designer matrices for intestinal epithelial organoids66,67. It will be interesting to specifically evaluate potential differences in epithelial and mesenchymal cell-matrix interactions.
Presentation of cell-adhesive ligands
The biopolymers within natural ECMs contain a multitude of cell-adhesive ligands, which provide sites for cell attachment68,69. Cell-ligand binding results in changes of the cellular cytoskeleton, which can lead to cell spreading and migration70,71. Cells can also actively pull on their surrounding environment through cell-adhesive ligands, leading to rearrangement of the ECM and clustering of cell-surface receptors. These clusters of cell-surface receptors are sites of intracellular signalling, often initiating changes in gene expression in the nucleus72,73. The extent of clustering of cell-surface receptors and cell-adhesive ligands impacts cellular behaviours, such as cell motility74, cell spreading75, cell differentiation and angiogenesis76. Therefore, the clustering of cell-adhesive ligands is a key consideration in biomaterial design77,78.
Peptides can be incorporated in engineered biomaterials to provide cell-adhesive ligands and to influence cell phenotype; for example, the fibronectin-derived peptide sequence RGD79, the collagen-derived peptide GFOGER80 or the laminin-derived peptides IKVAV81 and YIGSR82 bind to integrins and other cell-surface receptors. The concentration77,83, spacing84–86, presentation (including nuanced differences such as the identities of flanking amino acid residues)87,88, patterning89–91 and timing of ligand presentation92 impact the behaviour of cultured cells. For example, RGD ligands that are displayed as pendant groups from a polyethylene glycol (PEG) matrix lead to statistically significant improvements in MSC viability compared with RGD peptides that are constrained within the matrix87. The timing of RGD presentation is also important for MSC behaviour. For example, in a PEG hydrogel, MSCs require RGD for survival early during 3D culture; however, the removal of RGD ligands at later time points does not decrease viability but, rather, improves differentiation92.
The influence of receptor-ligand interactions has often been studied for individual receptor-ligand pairs. However, in vivo, matrices contain many different ligands with varying downstream effects on adherent cells. Moreover, cell receptor-ligand interactions are usually promiscuous and ligands (for example, RGD) can interact with various cell-surface receptors, triggering different cellular signalling pathways93. Therefore, the precise control over ligand binding is important for directing cellular behaviour in vitro. For example, scaffolds enabling α3β1 and α4β1 integrin binding rather than αvβ3 integrin binding promote endothelial cells to form a mature vasculature in vitro94. Biomaterials can also be engineered to present multiple cell-adhesive ligands95–100. Interestingly, the combination of two or more different ligands can result in non-additive and unintuitive changes in cellular behaviour and, thus, requires experimental optimization for individual cell types and cultures. For example, the optimal concentration of RGD, YIGSR and IKVAV to promote neural progenitor cell differentiation into mature neurons can be determined using response surface methods and multiple experimental iterations95, and a similar experimental approach will likely be required for engineering environments with cell-adhesive ligands for organoids.
Mechanical properties
The mechanical properties of a tissue or a biomaterial also impact cell behaviours, such as cell differentiation. Many engineered surfaces and hydrogels used for cell culture are elastic, that is, the application of force on the material results in a spontaneous proportional deformation and, upon removal of the force, the material returns to its original shape and size. However, the majority of natural tissues are viscoelastic76,101, possessing properties of both an elastic solid and a viscous liquid. The mechanical properties of tissues play a key role in guiding cellular behaviour102,103, which needs to be considered in the design of biomaterials for cell culture and organoids. In particular, material stiffness, stress relaxation rate and stress stiffening all are known to have an impact on stem-cell cultures.
Stiffness.
The stiffness of tissue microenvironments in the body ranges from compliant (often termed soft by the biomaterials community) to stiff. For example, brain and lung tissue are more compliant than bone104. Changes in tissue stiffness have been correlated with ageing105 and aberrant tissue stiffness can be both a driver and indicator of disease27,28,106,107. Cell culture has long relied on tissue culture plastic dishes with a stiffness in the gigapascal range, which is much stiffer than native tissues (~0.01 kPa to 100 kPa)104 and, thus, can influence cell behaviour in vitro. For example, 2D matrix elasticity has been shown to be sufficient to direct MSC differentiation towards tissue-specific lineages108. The cell fate of neural stem cells109,110, muscle stem cells111 and 3D cultures of MSCs112 has also been shown to be stiffness dependent in vitro. Stiffness further impacts cell proliferation110,113 and motility111,114–117.
Stress relaxation.
Physiological ECM is viscoelastic76,101. Viscoelastic materials dissipate the energy of an applied stress through time-dependent processes that result in the reorganization of the material (FIG. 3c). Therefore, stress relaxation is governed by the kinetics of matrix reorganization. Viscoelastic materials can be characterized by their stress-relaxation half-lives, that is, the time required to relax 50% of the applied stress. By contrast, elastic materials cannot dissipate the energy of an applied stress and, thus, the stress remains constant over time. Inspired by the viscoelasticity of native ECM, the influence of time-dependent mechanical properties on cellular behaviour has been explored75,76,101,118–120. MSCs cultured in 2D118,119 or 3D75,76,120 are sensitive to stress relaxation rates. In fast-relaxing, 3D hydrogels, MSCs show increased spreading, proliferation and osteogenic differentiation compared with slower relaxing matrices, independent of material stiffness76. These cellular effects may be attributed to changes in RGD ligand clustering caused by relaxation of the material; therefore, some cell types may be more responsive to stress relaxation than to stiffness in certain culture conditions.
Stress stiffening.
Fibrous ECM biopolymers often display a stress-stiffening response121,122, that is, they become stiffer once the stress applied exceeds a critical stress value (FIG. 3d). Below the critical stress value, stress on the material is compensated by the rearrangement or unravelling of bundled fibre networks. At the critical stress value, the material cannot undergo further structural rearrangement and the additional stress is distributed throughout the fibrous matrix. Most synthetic hydrogels are not stress stiffening in the biologically relevant stress regime (~0–10 Pa)122,123. However, tissue stress stiffening can be recreated in helical oligo(ethylene)glycol polyisocyanopeptide hydrogels, which can be engineered with specific stiffness and bundling characteristics123–126. Interestingly, MSCs cultured in hydrogels with an initial stiffness that usually promotes adipogenic cell fate in elastic materials preferentially undergo osteogenesis, which is normally triggered by matrices with high stiff-ness124, demonstrating that the cells can sense the high stiffness because of the stress they apply on the material. The cellular response in these hydrogels is also mediated by RGD ligand engagement124.
Matrix geometry
Cell-adhesive ligand presentation and cell-perceived mechanical material properties are affected by the geometric structure of the material. Therefore, it is often challenging to identify individual mechanisms that are responsible for changes in cell behaviour in response to the material structure. Native ECM is composed of a fibrous network with pore sizes approximately on the scale of cells. The dimensions and structure of the void volume of a matrix are crucial parameters impacting cell migration, cell-cell interactions and the transport of growth factors and nutrients.
Materials used as matrices for 3D cell culture can be categorized by their geometric structure (FIG. 3b). Fibrous matrices, such as ECM and hydrogels composed of fibrous proteins, have pores with void volumes approximately on the size of a cell. Many highly crosslinked hydrogels have a mesh-like structure and the distance between crosslinks dictates the mesh size, which leads to void volumes that are typically much smaller than cells. By contrast, macroporous materials have pores that can be larger than the size of a cell and they are often formed through the dissolution of sacrificial porogens embedded within a highly crosslinked matrix with a very small mesh size.
The alignment and diameter of fibres within a material influence cell behaviour. For example, fibre alignment promotes fate determination in human tendon stem cells as compared with randomly aligned fibres127. Interestingly, in contrast to tendon stem cells, MSCs are more strongly directed towards tendon cell fate by fibre diameter than by fibre alignment128. However, these differences could also be caused by the differences in cell type or material chemistries. Aligned YIGSR-functionalized nanofibres promote rapid differentiation of mouse embryonic stem cells into neurons, while also guiding the direction of neurite outgrowth129. Similarly, neural stem-cell-fate determination is sensitive to fibre diameter130. Most fibrous matrices (such as the ECM) have pores that are of a similar length scale as a typical cell diameter (~1–10 μm), whereas highly crosslinked hydrogels (for example, PEG and alginate) have mesh sizes much smaller than a typical cell (commonly in the nanometre length scale). In the absence of degradation or other forms of material remodelling, this small mesh size can prohibit cell proliferation and movement131. Hydrogels can also be designed as macroporous environments by adding porogens. In response to a stimulus, porogens form pores, which are often an order of magnitude greater than typical cell diameters (~100 μm). Such macroporous hydrogels can promote neonatal bovine chondrocyte spreading and ECM deposition compared with hydrogels without macropores132. Human MSCs cultured in hydrogels composed of annealed hyaluronic acid microparticles, which enable the formation of highly controlled macropores, form interconnected cellular networks, owing to high cell infiltration and migration within the matrix; by contrast, chemically identical, non-porous gels prohibit MSC network formation133. Similarly, microribbons can be crosslinked into macroporous scaffolds to generate large macropores (~300 μm), which allow human adipose-derived stem cell (ADSC) spreading similar to that observed in 2D culture; by contrast, in scaffolds with small macropores (<100 μm), cells engage multiple microribbons at once and more direct cell-cell contacts are formed, similar to that in 3D non-porous hydrogels134.
Hydrogels are often thought of as structurally homogeneous; however, many hydrogel systems, in particular, fibrous hydrogels, have different phases and microdomains. Hydrogel systems with rapid gelation kinetics can also contain regions of high and low concentrations of crosslinking, owing to the difficulty in achieving sufficient mixing of the hydrogel precursor components135. The presence of heterogeneity within hydrogels can be explored to direct cell behaviour136,137. For example, localized differences in stiffness within a material can result in heterogeneous MSC migration and fate determination138.
Matrix degradation and remodelling
Natural ECM is constantly remodelled by highly regulated, cell-mediated processes of degradation and production of ECM components27. Cells produce ECM-digesting enzymes and rearrange their microenvironment by expressing new biopolymers. Disruption of ECM homeostasis can lead to cellular dysregulation and disease27. Biomaterials can be designed to provide a matrix that allows degradation and remodelling at a rate desirable for embedded cells139.
The degradation profile of a material is characterized by the degradation mechanism, kinetics and products of degradation. Degradation of biomaterials can occur through a single or a combination of mechanisms, which can be broadly categorized as cell-mediated or cell-independent degradation. Cell-mediated degradation is facilitated by enzymes, for example, proteases, which are produced by encapsulated cells and break down the matrix through cleavage at specific amino acid sequences. To enable cell-mediated degradation by proteases, enzyme-sensitive peptide motifs can be incorporated in the material as crosslinkers or within the polymer backbone. Matrix metalloproteinases (MMPs) are commonly exploited for enzymatic degradation because they are produced by a wide range of cell types140. Several non-protein natural biopolymers can also be enzymatically degraded by cell-produced enzymes; for example, hyaluronic acid is enzymatically degraded by hyaluro-nidases141. Cell-independent material degradation can occur through the hydrolysis of chemical bonds within the material and disruption of physical crosslinks. For example, the biopolymer alginate is ionically crosslinked by calcium ions142, and the removal of calcium can be used to disrupt and degrade the alginate matrix143.
The rate at which a biomaterial degrades can greatly influence cell behaviour. The degradation rate can be tuned by combining different protease-degradable motifs with distinct cleavage kinetics within a biomaterial scaffold144. However, the influence of degradation products on cell behaviour also has to be considered in the design of degradable materials. For example, hyaluronic acid is relatively inert in the form of a crosslinked matrix or as a high-molecular-weight polymer, but acts as a signalling molecule once degraded into low-molecular-weight fragments145. The chemical environment can also change during matrix degradation, for example, in PEG-poly(lactic acid) hydrogels146. These materials promote the proliferation of neural cells owing to the radical scavenging activity of lactic acid generated during degradation. All aspects of the degradation profile of a matrix should be considered for their potential impact on cell behaviour because matrix degradation leads to substantial changes in the cellular microenvi-ronment139, for example, changes in the presentation of cell-adhesive ligands92,147,148, mechanical properties149,150 and geometry151. Loss of matrix because of degradation can also cause an increase in void space within the scaffold, enabling cellular proliferation152,153, matrix deposition154,155 and an increase in cell-cell interactions156. Cell-cell contacts are particularly important for multicellular cultures (BOX 2) and, therefore, scaffolds for organoids and organotypic systems need to be designed to support cellular contacts.
Box 2 |. Cadherin engagement in materials.
Cell-cell adhesions are key regulators of the morphology and function of multicellular tissues in vivo and in vitro247. Numerous cell-surface proteins mediate the junctions formed between cells, of which cadherins are the best characterized248,249. Cadherins are a family of homophilic (and, in some cases, heterophilic) cell-surface proteins250,251. Although there are many types of cadherins, the influence of E-cadherin, P-cadherin, N-cadherin and VE-cadherin has been investigated in the most detail. Cells displaying a specific cadherin tend to adhere to other cells expressing the same cadherin owing to homophilic binding202, although heterophilic binding is possible in some cases250,251. This preferential cadherin binding is important in the development to drive cell junction formation and cell sorting during tissue maturation247. The identity and distribution of cadherin subtypes changes over time as the cell matures. Furthermore, cadherins play a signalling role in cells. The intracellular domain is linked to the actin cytoskeleton and has been implicated in mechanosensing252–254 and stemness maintenance156. Thus, cadherin engagement is a crucial consideration for organoid engineering. Cadherin signalling can be modified by increasing the degradability of an organoid matrix to permit cadherin-mediated cell-cell contacts, for example, to maintain stemness in neural progenitor cells156. Alternatively, synthetic cadherin interactions can be achieved through the use of engineered materials that display cadherin-mimetic peptides. For example, a hydrogel functionalized with N-cadherin-mimetic peptides promotes chondrogenesis of human mesenchymal stromal (or stem) cells and cartilage matrix deposition255. Methods to spatially and dynamically regulate cadherin interactions and to optimize the cell-cell binding within engineered biomaterials may improve the control over organoid morphogenesis.
Engineered organoid matrices
Engineered matrices are an important alternative to conventional organoid culture scaffolds, such as the EHS matrix, because they provide better tunability, are fully chemically defined and can be easily produced with conventional synthetic methods and minimal batch-to-batch variability. Therefore, a variety of engineered materials are being explored for human-derived and animal-derived organoid cultures (TABLE 1), including organotypic cultures157–160.
Table 1 |.
Materials systems for organoids
| Material class | Material | Organoid tissue | Cell origin | Refs |
|---|---|---|---|---|
| Decellularized tissues | EHS matrix | Intestine | Murine Lgr5+ cells | 33 |
| Brain | Human ESCs and iPSCs | 41 | ||
| Prostrate | Murine prostate epithelial cells | 256 | ||
| Gastric | Human ESCs and iPSCs | 55 | ||
| Brain (midbrain-like) | Human ESCs and iPSCs | 257 | ||
| Lung | Human iPSCs | 258 | ||
| Decellularized liver | Liver | HUVECs and human fetal liver cells | 259 | |
| Decellularized lung | Lung | Human ESCs and iPSCs | 37 | |
| Decellularized intestine | Intestine | Human iPSCs | 260 | |
| Natural biopolymers | Collagen | Intestine | Murine intestinal tissue | 34,162 |
| Intestine | Human intestinal epithelium | 161 | ||
| Collagen vitrigel | Intestine | Human colon carcinoma | 163 | |
| Cell-Mate3D (hyaluronic acid, chitosan and dextrose) | Brain | Human iPSCs | 164 | |
| Alginate | Intestine | Human iPSCs | 172 | |
| Alginate beads | Pulmonary | Human fetal lung fibroblasts, HUVECS, iPSCs | 165 | |
| Tubular silk sponge | Intestine | Human jejunum tissue | 173 | |
| Hyaluronic acid | Kidney | Murine kidney tissue | 261 | |
| Fibrin-laminin | Intestine, pancreas, liver | Murine intestinal tissue, human biopsy tissue | 262 | |
| Protein-engineered materials | Elastin-like protein | Intestine | Murine intestinal tissue | 178 |
| Synthetic polymers | PEG and natural biopolymers | Intestine | Isolated murine crypts/ intestinal stem cells | 66 |
| Brain (neural-tube-like) | Mouse ESCs | 26 | ||
| PEG | Pancreas | Murine embryonic pancreatic progenitor cells | 263 | |
| PEG-4MAL | Intestine | Human iPSCs | 67 | |
| Amikagel | Pancreatic islets | Human ESCs | 179 | |
| Cell foam (tantalum precipitate) | Thymus | Murine thymic stromal cells and human bone-marrow-derived progenitor cells | 40 | |
| PGA and PLLA | Intestine | Human iPSCs | 247 |
EHS, Engelbreth-Holm-Swarm; ESCs, embryonic stem cells; HUVECs, human umbilical vein endothelial cells; iPSCs, induced pluripotent stem cells; Lgr5+, leucine-rich repeat-containing G-protein-coupled receptor-5-positive; PEG, polyethylene glycol; PEG-4MAL, PEG with four thiol-reactive maleimides; PGA, polyglycolic acid; PLLA, poly-L-lactic acid.
Intestinal organoids
The use of engineered matrices has, thus far, been mostly explored for intestinal organoid cultures, in particular to provide better control of important cell niche cues. The development of intestinal organoids has greatly benefited from an in-depth understanding of the key stem-cell populations and culture conditions that are necessary for intestinal organoid formation33. In the absence of mesenchymal cells, the generation of intestinal organoids requires activation of the Wingless/integrated (Wnt) signalling pathway and can be initiated from single Wnt/R-spondin-responsive stem cells expressing leucine-rich repeat-containing G-protein-coupled receptor-5 (Lgr5)33. Cell-matrix interactions are important for controlling intestinal organoid morphology, and the removal of ECM cues causes the organoids to ‘flip’ into an apical-out morphology in a β1-integrin-dependent process13. In these reversed-polarity organoids, the luminal surface, which is usually enclosed within the organoid, becomes accessible, making these organoids powerful models for studying host-pathogen interactions.
A variety of materials have been explored for intestinal organoid cultures, including decellularized tissue matrices, single-component natural biopolymer matrices, synthetic polymer hydrogels, protein-engineered hydrogels and combinations thereof (TABLE 1). Interestingly, organoid cultures often require a period of growth and preformation in an EHS matrix prior to reseeding in an engineered material, possibly owing to specific cues present in the EHS matrix, highlighting the lack of understanding of the niche cues required for early organoid development.
Natural biopolymer materials.
Matrices composed of naturally derived, single-component biopolymers used for intestinal organoid culture include protein-based (for example, collagen34,161–163) and polysaccharide-based (for example, hyaluronic acid164 and alginate165) materials. These materials are chemically defined compared to an EHS matrix and provide opportunities to control the material properties through chemical and physical modifications142,166,167. Moreover, natural biopolymer materials do not suffer as much from batch-to-batch variability as EHS matrices168, permitting more robust experimentation.
Collagen I hydrogels exposed to an air-liquid interface can support long-term (>365 days) cultures of murine intestinal organoids34 with intrinsic stromal fibroblasts and immune components en bloc with epithelium without the need for reconstitution169,170, highlighting the importance of gas transport for organoid cultures, which is often an underappreciated parameter171. Gas transport is especially important in thick 3D cultures, which have substantial barriers to gas diffusion. Using an air-liquid interface culture rather than a conventional submerged culture improves oxygen transport and leads to improved organoid maturation, as measured by spontaneous contractility162. Organoid contractility depends on material density and geometry within collagen gel, with a narrow optimal range of approximately 20% porosity and a stiffness of 30 Pa. Importantly, such airliquid interface cultures allow en bloc culture of large tissue aggregates, which maintain native in vivo spatial relationships between epithelial cells and non-epithelial stromal cells, including fibroblasts and immune cells169,170. Alginate gels without modification with cell-adhesive ligands can support the growth of human iPSC-derived intestinal organoids in vitro for at least 90 days172, suggesting that mechanical support in the absence of other ECM cues is sufficient for some organoid cultures, possibly owing to the fact that organoids make their own niche within the culture.
Organoids can also be used as building blocks within single-component, biopolymer-based hydrogels (and other materials) to create complex structures173. For example, a combination of silk fibroin and collagen can be used to investigate the innate immune response of an intestinal organoid system in response to bacterial infection. The cylindrical silk scaffolds are first moulded with an internal channel, which is then seeded with primary human intestinal, organoid-derived epithelial cells. Intestinal myofibroblasts encapsulated within a collagen gel are then added to the porous bulk. The resultant culture forms an intestinal epithelium in the internal channel and bacteria, such as Escherichia coli, can be added to model pathogen attack on the intestine. The bacterial challenge leads to an upregulation of the expression of genes associated with the innate immune response to infection, including many genes implicated in inflammatory bowel disease. This approach is an excellent demonstration of how organoids can be used for the study of disease mechanisms, such as pathogen-host biology.
Synthetic polymer materials.
Matrices based entirely on synthetic polymers permit almost limitless possibilities in terms of material properties. PEG-based hydrogels are particularly useful because they resist biofouling caused by non-specific protein adsorption, which can complicate data interpretation174; they are inexpensive; they are commercially available in a range of structures (for example, linear or multi-arm star versions) and molecular weights, enabling different matrix designs; and they can be easily chemically functionalized to incorporate biological ligands, signalling molecules and points for crosslinking, allowing the precise tuning of physical and biochemical niche properties175. For example, a PEG hydrogel system with dynamic mechanical properties can support primary mouse intestinal organoid formation at early and late stages66. At early stages of culture, gels with high stiffness (~1.3 kPa) promote mouse intestinal stem-cell expansion. As the culture matures, the hydrogels become softer owing to matrix degradation, promoting intestinal stem-cell differentiation and organoid formation, which is only observed in gels with a narrow, low stiffness range (~190 Pa). This mechano-sensitivity of intestinal stem-cell organoid cultures is mediated by yes-associated protein 1 (YAP) signalling. Interestingly, matrix softening is not sufficient to enable murine organoid formation in the presence of only the RGD ligand; budding requires both RGD and laminin-111. Therefore, hydrogel systems with dynamic biochemical and mechanical properties may be needed to provide the dynamic niche requirements for the different stages of organoid development.
A modular hydrogel made of PEG with four thiol-reactive maleimides (PEG-4MAL) can also be used as a scaffold for organotypic and organoid formation67,176. Using PEG-4MAL functionalized with RGD enables the formation of human pluripotent stem-cell-derived organoids with similar organoid survival rates as in an EHS matrix67; however, the organoids first need to be formed in an EHS matrix. Replacing RGD with other cell-binding ligands, such as GFOGER and IKVAV, leads to statistically significant decreases in the survival rate of the organoids. Additionally, hydrogels with a polymer density ranging from 3.5% to 4% PEG-4MAL support early-stage to late-stage organoid transformation, whereas higher polymer density hydrogels greatly decrease culture viability. The mechanical properties of the hydrogel are the key determinants of YAP signalling-based mechanotransduction. The PEG-4MAL hydrogel has been explored as a delivery vehicle for in vivo organoid engraftment and colonic wound closure. Delivery of organoids within the hydrogel show statistically significant effectiveness in colonic wound closure compared with control therapies, in which only organoids or only hydrogels are delivered.
Protein-engineered hydrogels.
Recombinant protein-based hydrogels are composed of engineered proteins, often with specially designed sequences inspired by native proteins. Such hydrogels are easy to produce by recombinant protein expression177. Recombinantly expressed proteins are chemically well defined and have many desirable properties of natural-protein biomaterials, including cell-adhesive domains. For example, a matrix composed of a recombinant elastin-like protein can promote adult murine intestinal organoid formation178. These elastin-like proteins possess RGD in addition to a structural elastin-derived domain. Moreover, the stiffness and RGD ligand concentration can be independently tuned. More compliant matrices (~180 Pa stiffness) with higher RGD ligand concentrations (3.2 mM) more efficiently support organoid formation than stiff matrices with low RGD concentrations. Strikingly, the softest (~180 Pa) elastin-like protein hydrogel shows comparable organoid formation efficiency as collagen I hydrogels, although it is an order of magnitude stiffer than collagen. Matrix degradation by MMPs is an important requirement for organoid cultures in elastin-like protein gels. The presence of an MMP inhibitor prevents organoid growth independent of elastin-like protein matrix mechanics, an effect that is most pronounced in stiffer matrices (~1,220 Pa), highlighting the importance of determining the degradative and mechanical requirements of matrix-organoid systems.
Other organoid cultures
Although engineered materials have mostly been used for intestinal organoids thus far, they can also be applied to other organoid systems owing to the possibility to tune and optimize their biochemical modification, biomechanical properties and geometric structural features, which is not possible using an EHS matrix. For example, to optimize materials for brain organoid cultures, high-throughput screening of multiple 3D cell microenvironments has been performed to identify the factors that promote neural-tube-like morphogenesis from mouse ESCs26. PEG-based hydrogels with intermediate matrix stiffnesses (~2–4 kPa) most strongly promote apicobasal polarity and dorsal-ventral patterning as compared with hydrogels with higher (~8 kPa) or lower stiffness (~0.5 kPa). Notably, this stiffness is greater than the stiffness achievable in an EHS matrix. Interestingly, non-degradable matrices promote apicobasal polarity and dorsal-ventral patterning, whereas degradable matrices do not support dorsal-ventral patterning. The addition of laminin, which is a major component of EHS matrices, has the most beneficial impact on the generation of neural tubes compared with the addition of other ECM components. Importantly, mouse ESCs cultured in the PEG matrices optimized for mechanical properties, degradability and presence of ECM components generate more homogenous cultures of polarized neuroepithelial colonies than ESCs cultures in an EHS matrix, demonstrating that organoid cultures can be improved by carefully designing the properties of matrices.
Human iPSC-derived brain organoids spontaneously form after approximately 10 days of culture in electrostatically crosslinked hyaluronate and protonated chitosan hydrogels164. The organoids have rosettes and neural-tube-like structures, and display physiological changes in intracellular calcium concentration in response to the neurotransmitters glutamate and potassium. Using this approach, viable organoids could be formed using iPSCs from healthy or adrenoleukodystrophy patients, suggesting that this platform may be used for the modelling of neurological diseases.
In contrast to neural tissue, lung tissue has more voids, which presents a unique challenge for designing lung organoid matrices. To mimic such an environment, collagen-coated alginate beads can be mixed with human lung fibroblasts and iPSC-derived mesenchymal cells165. The surface of the alginate beads can be functionalized with collagen I to aid in cellular adhesion. Cells and beads can then be cultured in a bioreactor and rotated to coat the beads with cells. Aggregation of the alginate beads leads to the formation of a close-packed structure. This architecture restricts cellular attachment and proliferation to the interstitial space between the beads, which causes the formation of acellular regions within the culture, mimicking the alveolar architecture of lungs. This organoid system can be used to model idiopathic pulmonary fibrosis by treating the organoid with transforming growth factor β, which leads to the formation of myofibroblasts, which are thought to be responsible for an increase in fibrosis in diseased lungs.
The PEG-4MAL matrices that have been successfully applied for intestinal organoids can also be used to support human pluripotent stem-cell-derived lung organoids67. For example, human lung organoids, first formed in an EHS matrix, can be encapsulated within the PEG-4MAL system and cultured for 7 days. These organoids display the morphological organization of a lumen with lung epithelium and airway basal cells, suggesting that the PEG-4MAL system may provide a platform for a variety of human organoid types.
Synthetic biomaterials are also applicable for pancreatic islet organoids179 based on human pluripotent stem cells. Efficient production of insulin-producing pancreatic islets, which are lost in patients with type 1 diabetes, is a pressing need for the treatment of this disease. Human ESC-derived pancreatic progenitor cells can be seeded together with human endothelial cells on top of Amikagel, which is a hydrogel composed of amikacin hydrate crosslinked with PEG-diglycidyl ether (PEGDE). Cells seeded on top of stiff (Young’s modulus of ~300 kPa) hydrogels, formed with a high ratio of PEGDE to amikacin hydrate, form multicellular organoids. Compared with cultures seeded on top of an EHS matrix, Amikagel cultures show a substantial increase in the expression of the pancreatic transcription and maturation factors PDX-1 and NKX6.1, as well as glucose-dependent production of insulin.
In summary, engineered matrices can support several different types of organoid cultures. Although mainly applied for intestinal organoids thus far, various other tissue types have already been explored. Interestingly, engineered materials have almost exclusively been applied to organoids derived from pluripotent stem-cell sources or primary rodent tissue rather than from primary human tissue. However, pluripotent stem-cell-derived organoids often have limited maturity compared with tissue-derived organoids15,54 and they can include a substantial amount of contaminating cell types50–53. For the application of organoids in precision medicine and personalized drug screening, the use of primary patient-derived organoids will be essential. There are inherent differences in the niche cues required for pluripotent cells, primary rodent cells and primary human cells, which may necessitate different matrix designs, presenting an immense opportunity for the engineering of biomaterials for primary patient-derived organoids.
Opportunities for material design
Instead of naturally derived, chemically undefined matrices, well-defined, reproducible synthetic materials can be used for organoid culture. However, reproducible morphogenesis and sufficient functional maturation remain key challenges, impeding the clinical application of organoids22. To control the emergent self-organization of organoids, approaches from stem-cell biology have been explored, for example, change of media supplements over time23. Alternatively, dynamic biomaterials may provide niche cues capable of directing and responding to organoid development, for example, to achieve spatially restricted lineage commitment and cellular self-organization, which are key parameters for morphogenesis and physiologically relevant function180. Although not yet applied for organoids, various dynamic biomaterials have been developed that may be adapted for organoid culture.
Spatially restricted lineage commitment
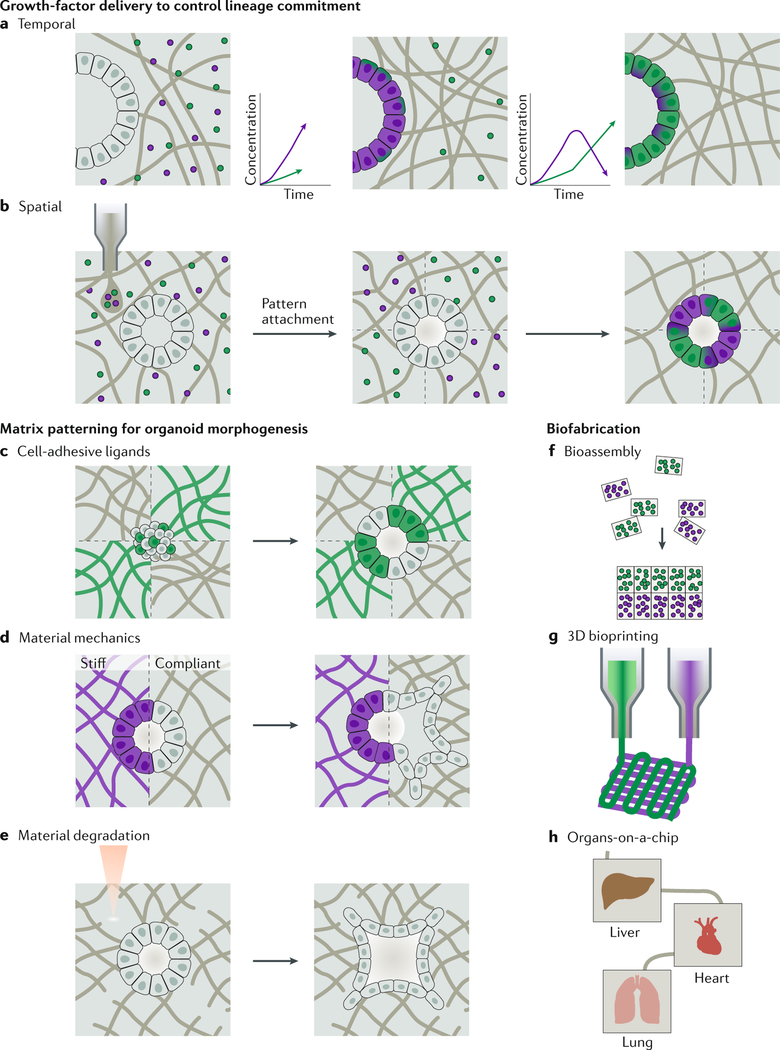
Improving the reproducibility of stem-cell differentiation and lineage commitment is crucial for the generation of organoids with reproducible emergent properties23. Biomaterials can be engineered for the spatiotemporal delivery of biochemical cues, for example, growth factors, to direct progenitor cell-fate decisions (Fig. 4a). Numerous matrix-based delivery approaches have been explored for drug delivery181, including passive drug release, cell-responsive (for example, proteolytic) drug release and user-controlled drug release. The affinity between the cargo and the biomaterial scaffold182–184 can be exploited for the simultaneous passive release of multiple growth factors, which improves the differentiation efficiency of encapsulated stem cells185. However, this approach lacks the possibility to precisely control the timing of delivery, which requires cell-triggered or user-triggered release strategies. Cell-mediated release can be achieved by using protease-cleavable peptides to tether signalling molecules to a material186. Peptide substrates have already been identified for a variety of proteases and have been used in 3D materials187–190; however, cell-mediated release in organoid systems requires thorough knowledge of the timing and specificity of pro-tease expression, which have yet to be characterized in detail. Supporting the spatiotemporally restricted lineage commitment of emergent organoid subpopulations may require direct spatial patterning of signalling molecules in addition to temporal release. Photochemistry can be used to spatially pattern peptides within 3D materials191–197 and to trigger the attachment or release of factors from a scaffold, which can be examined for user-controlled release. Thus far, fluorescent molecules or cell-adhesive peptide ligands have mostly been explored as model cargos for user-controlled release, although the controlled release of growth factors and the simultaneous, orthogonal patterning of multiple growth factors192 within scaffolds have also been investigated.
Fig. 4 |. Dynamic organoid niches.
Engineered materials may enable the control of lineage commitment of stem and progenitor cells in time and space. a | The release profile of matrix-immobilized growth factors can be designed to sequentially deliver signals through growth factor-material affinity or proteolytic release, providing the appropriate biochemical cues for maturing organoids. b | Materials can be patterned with growth factors to spatially control lineage commitment and, thus, the development and maturation of organoids. c | Materials can be patterned with cell-type-specific adhesive ligands to guide cell self-sorting of early cell clusters and organoids. d | The mechanical properties of a material impact cellular migration. e | Material degradation can be designed to control cellular migration and morphogenesis of the developing organoid. f | Biofabrication techniques provide opportunities to produce spatially controlled, engineered matrices for organoid culture. Bioassembly could be used to spontaneously form microtissues with zonal organization of region-specific organoids. g | Bioprinting enables the rapid fabrication of complex tissue architectures, for example, vascularized constructs. h | Organoids can also be incorporated into organ-on-a-chip platforms. These platforms can provide powerful models of clinically relevant multi-organ interactions256–270.
A relatively unexplored area is the delivery of morphogens to establish developmentally relevant concentration gradients198. In 2D human intestinal organoid monolayer cultures, it has been shown that morphogenetic signalling circuits play a key role in regulating intestinal epithelium development199, and efforts have been made to incorporate inducible morphogenetic ‘organizers’ into organoid cultures200. Creating soluble concentration gradients within hydrogels could be used to mimic such morphogenetic gradients during organoid development201 and could enable efficient, reproducible lineage commitment in addition to morphogenesis.
Controlling cell migration and sorting
As cells commit to specialized lineages in an organoid, their spatial arrangement drastically changes owing to cell migration and self-sorting. The self-sorting of cells is crucial to developmental and in vitro morphogenesis180; however, the details and mechanisms of this cellular ‘sorting’ process are still being investigated202–205. Using engineered materials to direct self-sorting by guiding cellular migration could improve the functional maturation and reproducibility of organoids (FIG. 4b). For example, cell-adhesive islands with defined size and shape can improve organoid self-organization into physiologically relevant structures, such as neural rosettes206,207. Similarly, placing cell-adhesive ligands at specific areas in a material can flip the polarity of epithelial organoids13, demonstrating that cell-ECM contacts play an important role in cell and tissue reorganization208. Spatial patterning of a cell-adhesive ligand, for example, the RGD peptide209,210, has been applied for a variety of 3D materials to guide the migration of diverse cell types211,212. Such approaches could be modified to create ligand profiles that foster organoid self-sorting and morphogenesis (Fig. 4c). Furthermore, systems with both spatial and temporal control of cell-adhesive ligands could dynamically react in response to the progressive stages of a developing organoid.
Spatially varying the mechanical properties of a material has been widely used in 2D cell culture to reliably control cell spreading and the exertion of traction forces, which often precede migration213–216. Such strategies could also be adapted to 3D systems (FIG. 4d). In addition, user-responsive materials can be designed to alter 3D matrix mechanics over time217. Physical and mechanical cues are important parameters for biomimetic organoid morphogenesis and function. For example, the spatial patterning of mechanical cues enables asymmetric cyst formation in a model of amnio-genesis218,219. Similarly, physical confinement of developing organoids can induce a wrinkled morphology in brain organoids, which are otherwise relatively smooth in non-confining matrices. Notably, myosin disruption reduces the degree of wrinkling, demonstrating that the emergent morphology is a result of cellular physical forces20. Brain organoids can also be cultured on polymer microfilaments in a droplet of EHS matrix to generate an elongated organoid220. Thus, using materials science tools that enable spatial and temporal control of the mechanical properties of a material could be a promising avenue to promote organoid self-organization and user-defined morphologies.
Tuning the material-degradation profile may also be a strategy to promote organoid maturation (FIG. 4e). For example, proteolytic degradation could be harnessed to coordinate cellular migration131 and physiologically relevant rearrangement221,222. In particular, this may be a promising approach for organoids with a diverse expression of multiple cell-type-specific proteases. Alternatively, light-mediated material degradation could enable user-defined organoid morphologies. Photoablation has been used to guide multicellular migration of encapsulated cell aggregates in 3D223, for example, the migration of motor neurons from encapsulated embryoid bodies224. Furthermore, material designs with a combinatorial, programmable approach to matrix degradation225 could support the dynamic requirements of maturing organoids.
Building organoids by biofabrication
Organoids can also serve as the starting material for the biofabrication of larger, more complex biomimetic systems and tissues226–228. Bioassembly attempts to create complex functional structures from preformed, cell-containing building blocks, such as organoids10,229 (FIG. 4f). For example, bioassembly can be used to assemble two preformed organoids with subdomain-specific forebrain identity into a single, fused structure, termed an assembloid58. This in vitro model allows the investigation of the migration of wild-type and diseased interneurons in a process that mimics fetal development. Assembloids could also be combined with engineered materials that enable the predictive, programmed assembly of preformed microgels. 3D bioprinting can be applied to pattern ‘inks’ composed of cells and/or materials230–233 (FIG. 4g); for example, scaffold-free printing of cell aggregates similar to organoids234,235, printing of biomaterials inks with organoids as functional units or printing of an acellular ink followed by seeding with organoids. The latter strategy has been used to seed ovarian follicles on 3D-printed, microporous scaffolds. These printed ovarian follicles could restore ovarian function in a sterilized mouse model, leading to live birth of offspring236. Organoids also have the potential to be used in organ-on-a-chip devices, which often attempt to model inter-organ interactions4,18,237–239 (FIG. 4h). For example, high fluid flow rates through an organ-on-a-chip device promote the vascularization of kidney organoids adherent to a biomaterial coating19. Organoids in combination with these devices could be applied for high-throughput drug screening and personalized medicine18,240–242.
Conclusions
Organoids provide a great opportunity to study human physiology in vitro. The maturation of organoid cultures relies on the propensity of stem cells to form highly organized structures during differentiation. Although each organoid type has unique characteristics, organoid maturation shares common developmental stages and niche needs, including an ECM, which greatly influences organoid development. Engineered matrices with reproducible properties have the potential to improve the efficiency and consistency of organoid cultures compared with natural materials, such as an EHS matrix. Many material properties, including the presentation of cell-binding ligands, matrix mechanics, structural geometry and degradability, impact stem-cell activity and are crucial design parameters for organoid matrices. Engineered organoid matrices have already been explored for various organoid systems used for disease modelling and regenerative medicine. The possibility to design materials that can spatially and dynamically control the organoid microenvironment and the surrounding stromal matrix will allow the control of organoid maturation and function, as well as the inclusion of heterologous stromal cell types. Moreover, the combination of organoids with advanced materials will advance the development of biofabricated tissues for personalized medicine and drug screening.
Acknowledgements
The authors acknowledge financial support from the National Institutes of Health (R21HL138042, R01HL142718, R01EB0 2 7 666 (S.C.H.), U01DK085527 (C.J.K.), U19AI116484 (S.C.H., C.J.K.)), the National Science Foundation (DMR 1808415 (S.C.H.)), the Human Brain Organogenesis Program funded by the Wu Tsai Neurosciences Institute (S.C.H., S.P.P.), New York Stem Cell Foundation (NYSCF) Robertson Stem Cell Investigator Award (S.P.P.) and the Chan Zuckerberg Initiative (CZI) Ben Barres Award (S.P.P.). The authors thank D. Hunt, B. LaSavage, L. Marquardt and J. Roth for their helpful discussions.
Footnotes
Competing interests
The authors declare no competing interests.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harrison RG, Greenman MJ, Mall FP & Jackson CM Observations of the living developing nerve fiber. Anat. Rec 1, 116–128 (1907). [Google Scholar]
- 2.Weiss P. & Taylor AC Reconstitution of complete organs from single-cell suspensions of chick embryos in advanced stages of differentiation. Proc. Natl. Acad. Sci. USA 46, 1177–1185 (1960). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishii K. Reconstruction of dissociated chick brain cells in rotation-mediated culture. Cytologia (Tokyo) 31, 89–98 (1966). [DOI] [PubMed] [Google Scholar]
- 4.Edington CD et al. Interconnected microphysiological systems for quantitative biology and pharmacology studies. Sci. Rep 8, 4530 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simian M. & Bissell MJ Organoids: a historical perspective of thinking in three dimensions. J. Cell Biol 216, 31–40 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stelzner M. et al. A nomenclature for intestinal in vitro cultures. Am. J. Physiol. Gastrointest. Liver Physiol 302, G1359-G1363 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pasca AM et al. Functional cortical neurons and astrocytes from human pluripotent stem cells in 3D culture. Nat. Methods 12, 671–678 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.HogenEsch H. & Nikitin AY Challenges in pre-clinical testing of anti-cancer drugs in cell culture and in animal models. J. Control. Release 164, 183–186 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Horrobin DF Modern biomedical research: an internally self-consistent universe with little contact with medical reality? Nat. Rev. DrugDiscov 2, 151–154 (2003). [DOI] [PubMed] [Google Scholar]
- 10.Pasca SP Assembling human brain organoids. Science 363, 126–127 (2019). [DOI] [PubMed] [Google Scholar]
- 11.Mak IW, Evaniew N. & Ghert M. Lost in translation: animal models and clinical trials in cancer treatment. Am. J. Transl. Res 6, 114–118 (2014). [PMC free article] [PubMed] [Google Scholar]
- 12.Pound P. & Ritskes-Hoitinga M. Is it possible to overcome issues of external validity in preclinical animal research? Why most animal models are bound to fail. J. Transl. Med 16, 304 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Co JY et al. Controlling epithelial polarity: a human enteroid model for host-pathogen interactions. Cell Rep 26, 2509–2520.e4 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dang J. et al. Zika virus depletes neural progenitors in human cerebral organoids through activation of the innate immune receptor TLR3. Cell Stem Cell 19, 258–265 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Forbes TA et al. Patient-iPSC-derived kidney organoids show functional validation of a ciliopathic renal phenotype and reveal underlying pathogenetic mechanisms. Am. J. Hum. Genet 102, 816–831 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang BY, Korolj A, Lai BFL & Radisic M. Advances in organ-on-a-chip engineering. Nat. Rev. Mat 3, 257–278 (2018). [Google Scholar]
- 17.Ahadian S. et al. Organ-on-a-chip platforms: a convergence of advanced materials, cells, and microscale technologies. Adv. Healthc. Mater 7, 1700506 (2018). [DOI] [PubMed] [Google Scholar]
- 18.Bhise NS et al. A liver-on-a-chip platform with bioprinted hepatic spheroids. Biofabrication 8, 014101 (2016). [DOI] [PubMed] [Google Scholar]
- 19.Homan KA et al. Flow-enhanced vascularization and maturation of kidney organoids in vitro. Nat. Methods 16, 255–262 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Karzbrun E, Kshirsagar A, Cohen SR, Hanna JH & Reiner O. Human brain organoids on a chip reveal the physics of folding. Nat. Phys 14, 515–522 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kasendra M. et al. Development of a primary human small intestine-on-a-chip using biopsy-derived organoids. Sci. Rep 8, 2871 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rossi G, Manfrin A. & Lutolf MP Progress and potential in organoid research. Nat. Rev. Genet 19, 671–687 (2018). [DOI] [PubMed] [Google Scholar]
- 23.Lancaster MA & Knoblich JA Organogenesis in a dish: modeling development and disease using organoid technologies. Science 345, 1247125 (2014). [DOI] [PubMed] [Google Scholar]
- 24.Czerniecki SM et al. High-throughput screening enhances kidney organoid differentiation from human pluripotent stem cells and enables automated multidimensional phenotyping. Cell Stem Cell 22, 929–940.e4 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van de Wetering M. et al. Prospective derivation of a living organoid biobank of colorectal cancer patients. Cell 161, 933–945 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ranga A. et al. Neural tube morphogenesis in synthetic 3D microenvironments. Proc. Natl. Acad. Sci. USA 113, E6831-E6839 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lu P, Takai K, Weaver VM & Werb Z. Extracellular matrix degradation and remodeling in development and disease. Cold Spring Harb. Perspect. Biol 3, a005058 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levental KR et al. Matrix crosslinking forces tumor progression by enhancing integrin signaling. Cell 139, 891–906 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Simao D. et al. Recapitulation of human neural microenvironment signatures in iPSC-derived NPC 3D differentiation. Stem Cell Rep 11, 552–564 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sasai Y, Eiraku M. & Suga H. In vitro organogenesis in three dimensions: self-organising stem cells. Development 139, 4111–4121 (2012). [DOI] [PubMed] [Google Scholar]
- 31.Eiraku M. et al. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature 472, 51–56 (2011). [DOI] [PubMed] [Google Scholar]
- 32.Nakano T. et al. Self-formation of optic cups and storable stratified neural retina from human ESCs. Cell Stem Cell 10, 771–785 (2012). [DOI] [PubMed] [Google Scholar]
- 33.Sato T. et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 459, 262–265 (2009). [DOI] [PubMed] [Google Scholar]
- 34.Ootani A. et al. Sustained in vitro intestinal epithelial culture within a Wnt-dependent stem cell niche. Nat. Med 15, 701–706 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taguchi A. & Nishinakamura R. Higher-order kidney organogenesis from pluripotent stem cells. Cell Stem Cell 21, 730–746.e6 (2017). [DOI] [PubMed] [Google Scholar]
- 36.Takasato M. et al. Kidney organoids from human iPS cells contain multiple lineages and model human nephrogenesis. Nature 526, 564–568 (2015). [DOI] [PubMed] [Google Scholar]
- 37.Dye BR et al. In vitro generation of human pluripotent stem cell derived lung organoids. Elife 4, e05098 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dorrell C. et al. The organoid-initiating cells in mouse pancreas and liver are phenotypically and functionally similar. Stem Cell Res 13, 275–283 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huch M. et al. Unlimited in vitro expansion of adult bi-potent pancreas progenitors through the Lgr5/R-spondin axis. EMBO J. 32, 2708–2721 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poznansky MC et al. Efficient generation of human T cells from a tissue-engineered thymic organoid. Nat. Biotechnol 18, 729–734 (2000). [DOI] [PubMed] [Google Scholar]
- 41.Lancaster MA et al. Cerebral organoids model human brain development and microcephaly. Nature 501, 373–379 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sakaguchi H. et al. Generation of functional hippocampal neurons from self-organizing human embryonic stem cell-derived dorsomedial telencephalic tissue. Nat. Commun 6, 8896 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kadoshima T. et al. Self-organization of axial polarity, inside-out layer pattern, and species-specific progenitor dynamics in human ES cell-derived neocortex. Proc. Natl. Acad. Sci. USA 110, 20284–20289 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qian X. et al. Brain-region-specific organoids using mini-bioreactors for modeling ZIKV exposure. Cell 165, 1238–1254 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yu J. et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 318, 1917–1920 (2007). [DOI] [PubMed] [Google Scholar]
- 46.Takahashi K. et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131, 861–872 (2007). [DOI] [PubMed] [Google Scholar]
- 47.McCracken KW et al. Wnt/beta-catenin promotes gastric fundus specification in mice and humans. Nature 541, 182–187 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Munera JO et al. Differentiation of human pluripotent stem cells into colonic organoids via transient activation of bmp signaling. Cell Stem Cell 21, 51–64.e6 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rankin SA et al. Timing is everything: reiterative Wnt, BMP and RA signaling regulate developmental competence during endoderm organogenesis. Dev. Biol 434, 121–132 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carcamo-Orive I. et al. Analysis of transcriptional variability in a large human iPSC library reveals genetic and non-genetic determinants of heterogeneity. Cell Stem Cell 20, 518–532.e9 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Graf T. & Stadtfeld M. Heterogeneity of embryonic and adult stem cells. Cell Stem Cell 3, 480–483 (2008). [DOI] [PubMed] [Google Scholar]
- 52.Narsinh KH et al. Single cell transcriptional profiling reveals heterogeneity of human induced pluripotent stem cells. J. Clin. Invest 121, 1217–1221 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wu H. et al. Comparative analysis and refinement of human PSC-derived kidney organoid differentiation with single-cell transcriptomics. Cell Stem Cell 23, 869–881.e8 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Spence JR et al. Directed differentiation of human pluripotent stem cells into intestinal tissue in vitro. Nature 470, 105–109 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McCracken KW et al. Modelling human development and disease in pluripotent stem-cell-derived gastric organoids. Nature 516, 400–404 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yoon SJ et al. Reliability of human cortical organoid generation. Nat. Methods 16, 75–78 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sloan SA et al. Human astrocyte maturation captured in 3D cerebral cortical spheroids derived from pluripotent stem cells. Neuron 95, 779–790.e6 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Birey F. et al. Assembly of functionally integrated human forebrain spheroids. Nature 545, 54–59 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eiraku M. et al. Self-organized formation of polarized cortical tissues from ESCs and its active manipulation by extrinsic signals. Cell Stem Cell 3, 519–532 (2008). [DOI] [PubMed] [Google Scholar]
- 60.Watanabe K. et al. Directed differentiation of telencephalic precursors from embryonic stem cells. Nat. Neurosci 8, 288–296 (2005). [DOI] [PubMed] [Google Scholar]
- 61.Qian X. et al. Generation of human brain region-specific organoids using a miniaturized spinning bioreactor. Nat. Protoc 13, 565–580 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kleinman HK et al. Isolation and characterization of type IV procollagen, laminin, and heparan sulfate proteoglycan from the EHS sarcoma. Biochemistry 21, 6188–6193 (1982). [DOI] [PubMed] [Google Scholar]
- 63.Huang G. et al. Functional and biomimetic materials for engineering of the three-dimensional cell microenvironment. Chem. Rev 117, 12764–12850 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Darnell M. et al. Material microenvironmental properties couple to induce distinct transcriptional programs in mammalian stem cells. Proc. Natl. Acad. Sci. USA 115, E8368-E8377 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Caplan AI Mesenchymal stem cells: time to change the name! Stem Cells Transl. Med 6, 1445–1451 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Gjorevski N. et al. Designer matrices for intestinal stem cell and organoid culture. Nature 539, 560–564 (2016). [DOI] [PubMed] [Google Scholar]
- 67.Cruz-Acuna R. et al. Synthetic hydrogels for human intestinal organoid generation and colonic wound repair. Nat. Cell Biol 19, 1326–1335 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Parsons JT, Horwitz AR & Schwartz MA Cell adhesion: integrating cytoskeletal dynamics and cellular tension. Nat. Rev. Mol. Cell Biol 11, 633–643 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hynes RO The extracellular matrix: not just pretty fibrils. Science 326, 1216–1219 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Huttenlocher A. & Horwitz AR Integrins in cell migration. Cold Spring Harb. Perspect. Biol 3, a005074 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vicente-Manzanares M, Choi CK & Horwitz AR Integrins in cell migration—the actin connection. J. Cell Sci 122, 199–206 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kim SH, Turnbull J. & Guimond S. Extracellular matrix and cell signalling: the dynamic cooperation of integrin, proteoglycan and growth factor receptor. J. Endocrinol 209, 139–151 (2011). [DOI] [PubMed] [Google Scholar]
- 73.Schwartz MA Integrins and extracellular matrix in mechanotransduction. Cold Spring Harb. Perspect. Biol 2, a005066 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Maheshwari G, Brown G, Lauffenburger DA, Wells A. & Griffith LG Cell adhesion and motility depend on nanoscale RGD clustering. J. Cell Sci 113 (10), 1677–1686 (2000). [DOI] [PubMed] [Google Scholar]
- 75.Chaudhuri O. et al. Substrate stress relaxation regulates cell spreading. Nat. Commun 6, 6364 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chaudhuri O. et al. Hydrogels with tunable stress relaxation regulate stem cell fate and activity. Nat. Mater 15, 326–334 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Benitez PL, Mascharak S, Proctor AC & Heilshorn SC Use of protein-engineered fabrics to identify design rules for integrin ligand clustering in biomaterials. Integr. Biol. (Camb.) 8, 50–61 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kong HJ, Polte TR, Alsberg E. & Mooney DJ FRET measurements of cell-traction forces and nano-scale clustering of adhesion ligands varied by substrate stiffness. Proc. Natl. Acad. Sci. USA 102, 4300–4305 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pierschbacher MD & Ruoslahti E. Cell attachment activity of fibronectin can be duplicated by small synthetic fragments of the molecule. Nature 309, 30–33 (1984). [DOI] [PubMed] [Google Scholar]
- 80.Knight CG et al. The collagen-binding A-domains of integrins alpha(1)beta(1) and alpha(2)beta(1) recognize the same specific amino acid sequence, GFOGER, in native (triple-helical) collagens. J. Biol. Chem 275, 35–40 (2000). [DOI] [PubMed] [Google Scholar]
- 81.Tashiro K. et al. A synthetic peptide containing the IKVAV sequence from the A chain of laminin mediates cell attachment, migration, and neurite outgrowth. J. Biol. Chem 264, 16174–16182 (1989). [PubMed] [Google Scholar]
- 82.Graf J. et al. Identification of an amino acid sequence in laminin mediating cell attachment, chemotaxis, and receptor binding. Cell 48, 989–996 (1987). [DOI] [PubMed] [Google Scholar]
- 83.Le Saux G, Magenau A, Bocking T, Gaus K. & Gooding JJ The relative importance of topography and RGD ligand density for endothelial cell adhesion. PLOS ONE 6, e21869 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Oria R. et al. Force loading explains spatial sensing of ligands by cells. Nature 552, 219–224 (2017). [DOI] [PubMed] [Google Scholar]
- 85.Ye K. et al. Matrix stiffness and nanoscale spatial organization of cell-adhesive ligands direct stem cell fate. Nano Lett 15, 4720–4729 (2015). [DOI] [PubMed] [Google Scholar]
- 86.Wang X. et al. Effect of RGD nanospacing on differentiation of stem cells. Biomaterials 34, 2865–2874 (2013). [DOI] [PubMed] [Google Scholar]
- 87.Salinas CN & Anseth KS The influence of the RGD peptide motif and its contextual presentation in PEG gels on human mesenchymal stem cell viability. J. Tissue Eng. Regen. Med 2, 296–304 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Koivunen E, Wang B. & Ruoslahti E. Phage libraries displaying cyclic peptides with different ring sizes: ligand specificities of the RGD-directed integrins. Biotechnology (N. Y.) 13, 265–270 (1995). [DOI] [PubMed] [Google Scholar]
- 89.Wade RJ, Bassin EJ, Gramlich WM & Burdick JA Nanofibrous hydrogels with spatially patterned biochemical signals to control cell behavior. Adv. Mater 27, 1356–1362 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Arnold M. et al. Activation of integrin function by nanopatterned adhesive interfaces. ChemPhysChem 5, 383–388 (2004). [DOI] [PubMed] [Google Scholar]
- 91.Cavalcanti-Adam EA et al. Cell spreading and focal adhesion dynamics are regulated by spacing of integrin ligands. Biophys. J. 92, 2964–2974 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kloxin AM, Kasko AM, Salinas CN & Anseth KS Photodegradable hydrogels for dynamic tuning of physical and chemical properties. Science 324, 59–63 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Campbell ID & Humphries MJ Integrin structure, activation, and interactions. Cold Spring Harb. Perspect. Biol 3, a004994 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Li S. et al. Hydrogels with precisely controlled integrin activation dictate vascular patterning and permeability. Nat. Mater 16, 953–961 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lam J, Carmichael ST, Lowry WE & Segura T. Hydrogel design of experiments methodology to optimize hydrogel for iPSC-NPC culture. Adv. Healthc. Mater 4, 534–539 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ali S, Saik JE, Gould DJ, Dickinson ME & West JL Immobilization of cell-adhesive laminin peptides in degradable PEGDA hydrogels influences endothelial cell tubulogenesis. BioRes. Open Access 2, 241–249 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Moshayedi P. et al. Systematic optimization of an engineered hydrogel allows for selective control of human neural stem cell survival and differentiation after transplantation in the stroke brain. Biomaterials 105, 145–155 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lee JW & Lee KY Dual peptide-presenting hydrogels for controlling the phenotype of PC12 cells. Colloids Surf. B Biointerfaces 152, 36–41 (2017). [DOI] [PubMed] [Google Scholar]
- 99.Huettner N, Dargaville TR & Forget A. Discovering cell-adhesion peptides in tissue engineering: beyond RGD. Trends Biotechnol 36, 372–383 (2018). [DOI] [PubMed] [Google Scholar]
- 100.Seidlits SK et al. Peptide-modified, hyaluronic acid-based hydrogels as a 3D culture platform for neural stem/progenitor cell engineering. J. Biomed. Mater. Res. A 107, 704–718 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Müller C, Müller A. & Pompe T. Dissipative interactions in cell-matrix adhesion. Soft Matter 9, 6207–6216 (2013). [Google Scholar]
- 102.Eyckmans J, Boudou T, Yu X. & Chen CS A hitchhiker’s guide to mechanobiology. Dev. Cell 21, 35–47 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Vianello S. & Lutolf MP Understanding the mechanobiology of early mammalian development through bioengineered models. Dev. Cell 48, 751–763 (2019). [DOI] [PubMed] [Google Scholar]
- 104.Butcher DT, Alliston T. & Weaver VM A tense situation: forcing tumour progression. Nat. Rev. Cancer 9, 108–122 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sherratt MJ Tissue elasticity and the ageing elastic fibre. Age 31, 305–325 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Handorf AM, Zhou Y, Halanski MA & Li WJ Tissue stiffness dictates development, homeostasis, and disease progression. Organogenesis 11, 1–15 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Lampi MC & Reinhart-King CA Targeting extracellular matrix stiffness to attenuate disease: From molecular mechanisms to clinical trials. Sci. Transl. Med 10, eaao0475 (2018). [DOI] [PubMed] [Google Scholar]
- 108.Engler AJ, Sen S, Sweeney HL & Discher DE Matrix elasticity directs stem cell lineage specification. Cell 126, 677–689 (2006). [DOI] [PubMed] [Google Scholar]
- 109.Saha K. et al. Substrate modulus directs neural stem cell behavior. Biophys. J. 95, 4426–4438 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Leipzig ND & Shoichet MS The effect of substrate stiffness on adult neural stem cell behavior. Biomaterials 30, 6867–6878 (2009). [DOI] [PubMed] [Google Scholar]
- 111.Gilbert PM, Havenstrite KL, Magnusson K. & Blau HM Substrate elasticity regulates skeletal muscle stem cell self-renewal in culture. Science 329, 1078–1081 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Huebsch N. et al. Harnessing traction-mediated manipulation of the cell/matrix interface to control stem-cell fate. Nat. Mater 9, 518–526 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Evans ND et al. Substrate stiffness affects early differentiation events in embryonic stem cells. Eur. Cell. Mater 18, 1–13; discussion 13–14 (2009). [DOI] [PubMed] [Google Scholar]
- 114.Hadden WJ et al. Stem cell migration and mechanotransduction on linear stiffness gradient hydrogels. Proc. Natl. Acad. Sci. USA 114, 5647–5652 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Lee DA, Knight MM, Campbell JJ & Bader DL Stem cell mechanobiology. J. Cell. Biochem 112, 1–9 (2011). [DOI] [PubMed] [Google Scholar]
- 116.Vining KH & Mooney DJ Mechanical forces direct stem cell behaviour in development and regeneration. Nat. Rev. Mol. Cell Biol 18, 728–742 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Wang N. Review of cellular mechanotransduction. J. Phys. D Appl. Phys 50, 233002 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cameron AR, Frith JE & Cooper-White JJ The influence of substrate creep on mesenchymal stem cell behaviour and phenotype. Biomaterials 32, 5979–5993 (2011). [DOI] [PubMed] [Google Scholar]
- 119.Cameron AR, Frith JE, Gomez GA, Yap AS & Cooper-White JJ The effect of time-dependent deformation of viscoelastic hydrogels on myogenic induction and Rac1 activity in mesenchymal stem cells. Biomaterials 35, 1857–1868 (2014). [DOI] [PubMed] [Google Scholar]
- 120.Nam S, Stowers R, Lou J, Xia Y. & Chaudhuri O. Varying PEG density to control stress relaxation in alginate-PEG hydrogels for 3D cell culture studies. Biomaterials 200, 15–24 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Rudnicki MS et al. Nonlinear strain stiffening is not sufficient to explain how far cells can feel on fibrous protein gels. Biophys. J. 105, 11–20 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Storm C, Pastore JJ, MacKintosh FC, Lubensky TC & Janmey PA Nonlinear elasticity in biological gels. Nature 435, 191–194 (2005). [DOI] [PubMed] [Google Scholar]
- 123.Jaspers M. et al. Ultra-responsive soft matter from strain-stiffening hydrogels. Nat. Commun 5, 5808 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Das RK, Gocheva V, Hammink R, Zouani OF & Rowan AE Stress-stiffening-mediated stem-cell commitment switch in soft responsive hydrogels. Nat. Mater 15, 318–325 (2016). [DOI] [PubMed] [Google Scholar]
- 125.de Almeida P. et al. Cytoskeletal stiffening in synthetic hydrogels. Nat. Commun 10, 609 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Kouwer PH et al. Responsive biomimetic networks from polyisocyanopeptide hydrogels. Nature 493, 651–655 (2013). [DOI] [PubMed] [Google Scholar]
- 127.Yin Z. et al. The regulation of tendon stem cell differentiation by the alignment of nanofibers. Biomaterials 31, 2163–2175 (2010). [DOI] [PubMed] [Google Scholar]
- 128.Cardwell RD, Dahlgren LA & Goldstein AS Electrospun fibre diameter, not alignment, affects mesenchymal stem cell differentiation into the tendon/ ligament lineage. J. Tissue Eng. Regen. Med 8, 937–945 (2014). [DOI] [PubMed] [Google Scholar]
- 129.Silantyeva EA et al. Accelerated neural differentiation of mouse embryonic stem cells on aligned GYIGSR-functionalized nanofibers. Acta Biomater 75, 129–139 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Christopherson GT, Song H. & Mao HQ The influence of fiber diameter of electrospun substrates on neural stem cell differentiation and proliferation. Biomaterials 30, 556–564 (2009). [DOI] [PubMed] [Google Scholar]
- 131.Lutolf MP et al. Synthetic matrix metalloproteinase-sensitive hydrogels for the conduction of tissue regeneration: engineering cell-invasion characteristics. Proc. Natl. Acad. Sci. USA 100, 5413–5418 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Han LH, Lai JH, Yu S. & Yang F. Dynamic tissue engineering scaffolds with stimuli-responsive macroporosity formation. Biomaterials 34, 4251–4258 (2013). [DOI] [PubMed] [Google Scholar]
- 133.Nih LR, Sideris E, Carmichael ST & Segura T. Injection of microporous annealing particle (MAP) hydrogels in the stroke cavity reduces gliosis and inflammation and promotes NPC migration to the lesion. Adv. Mater 29, 1606471 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Han LH, Tong X. & Yang F. Photo-crosslinkable PEG-based microribbons for forming 3D macroporous scaffolds with decoupled niche properties. Adv. Mater 26, 1757–1762 (2014). [DOI] [PubMed] [Google Scholar]
- 135.Darling NJ, Hung YS, Sharma S. & Segura T. Controlling the kinetics of thiol-maleimide Michaeltype addition gelation kinetics for the generation of homogenous poly(ethylene glycol) hydrogels. Biomaterials 101, 199–206 (2016). [DOI] [PubMed] [Google Scholar]
- 136.Wang H, Cai L, Paul A, Enejder A. & Heilshorn SC Hybrid elastin-like polypeptide-polyethylene glycol (ELP-PEG) hydrogels with improved transparency and independent control of matrix mechanics and cell ligand density. Biomacromolecules 15, 3421–3428 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Zhao H. et al. Microengineered in vitro model of cardiac fibrosis through modulating myofibroblast mechanotransduction. Biofabrication 6, 045009 (2014). [DOI] [PubMed] [Google Scholar]
- 138.Tse JR & Engler AJ Stiffness gradients mimicking in vivo tissue variation regulate mesenchymal stem cell fate. PLOS ONE 6, e15978 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Kharkar PM, Kiick KL & Kloxin AM Designing degradable hydrogels for orthogonal control of cell microenvironments. Chem. Soc. Rev 42, 7335–7372 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Giambernardi TA et al. Overview of matrix metalloproteinase expression in cultured human cells. Matrix Biology 16, 483–496 (1998). [DOI] [PubMed] [Google Scholar]
- 141.Girish KS & Kemparaju K. The magic glue hyaluronan and its eraser hyaluronidase: a biological overview. Life Sci 80, 1921–1943 (2007). [DOI] [PubMed] [Google Scholar]
- 142.Lee KY & Mooney DJ Alginate: properties and biomedical applications. Prog. Polym. Sci 37, 106–126 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kong HJ, Smith MK & Mooney DJ Designing alginate hydrogels to maintain viability of immobilized cells. Biomaterials 24, 4023–4029 (2003). [DOI] [PubMed] [Google Scholar]
- 144.Parmar PA et al. Temporally degradable collagen¬mimetic hydrogels tuned to chondrogenesis of human mesenchymal stem cells. Biomaterials 99, 56–71 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Stern R, Asari AA & Sugahara KN Hyaluronan fragments: an information-rich system. Eur. J. Cell Biol 85, 699–715 (2006). [DOI] [PubMed] [Google Scholar]
- 146.Lampe KJ, Bjugstad KB & Mahoney MJ Impact of degradable macromer content in a poly(ethylene glycol) hydrogel on neural cell metabolic activity, redox state, proliferation, and differentiation. Tissue Eng. Part A 16, 1857–1866 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Khetan S. et al. Degradation-mediated cellular traction directs stem cell fate in covalently crosslinked three-dimensional hydrogels. Nat. Mater 12, 458–465 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Salinas CN & Anseth KS The enhancement of chondrogenic differentiation of human mesenchymal stem cells by enzymatically regulated RGD functionalities. Biomaterials 29, 2370–2377 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ehrbar M. et al. Elucidating the role of matrix stiffness in 3D cell migration and remodeling. Biophys. J. 100, 284–293 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Khetan S. & Burdick JA Patterning network structure to spatially control cellular remodeling and stem cell fate within 3-dimensional hydrogels. Biomaterials 31, 8228–8234 (2010). [DOI] [PubMed] [Google Scholar]
- 151.Kloxin AM et al. Responsive culture platform to examine the influence of microenvironmental geometry on cell function in 3D. Integr. Biol. (Camb.) 4, 1540–1549 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Anderson SB, Lin CC, Kuntzler DV & Anseth KS The performance of human mesenchymal stem cells encapsulated in cell-degradable polymer-peptide hydrogels. Biomaterials 32, 3564–3574 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Ashton RS, Banerjee A, Punyani S, Schaffer DV & Kane RS Scaffolds based on degradable alginate hydrogels and poly(lactide-co-glycolide) microspheres for stem cell culture. Biomaterials 28, 5518–5525 (2007). [DOI] [PubMed] [Google Scholar]
- 154.Bryant SJ & Anseth KS Controlling the spatial distribution of ECM components in degradable PEG hydrogels for tissue engineering cartilage. J. Biomed. Mater Res. A 64, 70–79 (2003). [DOI] [PubMed] [Google Scholar]
- 155.Chung C, Beecham M, Mauck RL & Burdick JA The influence of degradation characteristics of hyaluronic acid hydrogels on in vitro neocartilage formation by mesenchymal stem cells. Biomaterials 30, 4287–4296 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Madl CM et al. Maintenance of neural progenitor cell stemness in 3D hydrogels requires matrix remodelling. Nat. Mater 16, 1233–1242 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Purwada A. et al. Ex vivo engineered immune organoids for controlled germinal center reactions. Biomaterials 63, 24–34 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Purwada A, Shah SB, Beguelin W, Melnick AM & Singh A. Modular immune organoids with integrin ligand specificity differentially regulate ex vivo B cell activation. ACS Biomater. Sci. Eng 3, 214–225 (2017). [DOI] [PubMed] [Google Scholar]
- 159.McGuigan AP & Sefton MV Vascularized organoid engineered by modular assembly enables blood perfusion. Proc. Natl. Acad. Sci. USA 103, 11461–11466 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Weber RJ et al. Rapid organoid reconstitution by chemical micromolding. ACS Biomater. Sci. Eng 2, 1851–1855 (2016). [DOI] [PubMed] [Google Scholar]
- 161.Jabaji Z. et al. Type I collagen as an extracellular matrix for the in vitro growth of human small intestinal epithelium. PLOS ONE 9, e107814 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.DiMarco RL et al. Engineering of three-dimensional microenvironments to promote contractile behavior in primary intestinal organoids. Integr. Biol. (Camb.) 6, 127–142 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Takezawa T, Ozaki K, Nitani A, Takabayashi C. & Shimo-Oka T. Collagen vitrigel: a novel scaffold that can facilitate a three-dimensional culture for reconstructing organoids. Cell Transplant 13, 463–473 (2004). [DOI] [PubMed] [Google Scholar]
- 164.Lindborg BA et al. Rapid induction of cerebral organoids from human induced pluripotent stem cells using a chemically defined hydrogel and defined cell culture medium. Stem Cells Transl. Med 5, 970–979 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wilkinson DC et al. Development of a three-dimensional bioengineering technology to generate lung tissue for personalized disease modeling. Stem Cells Transl. Med 6, 622–633 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Wolf KJ & Kumar S. Hyaluronic acid: incorporating the bio into the material. ACS Biomater. Sci. Eng 10.1021/acsbiomaterials.8b01268 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Antoine EE, Vlachos PP & Rylander MN Review of collagen I hydrogels for bioengineered tissue microenvironments: characterization of mechanics, structure, and transport. Tissue Eng. Part B Rev 20, 683–696 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hughes CS, Postovit LM & Lajoie GA Matrigel: a complex protein mixture required for optimal growth of cell culture. Proteomics 10, 1886–1890 (2010). [DOI] [PubMed] [Google Scholar]
- 169.Li X. et al. Oncogenic transformation of diverse gastrointestinal tissues in primary organoid culture. Nat. Med 20, 769–777 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Neal JT et al. Organoid modeling of the tumor immune microenvironment. Cell 175, 1972–1988. e16 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Giandomenico SL et al. Cerebral organoids at the air-liquid interface generate diverse nerve tracts with functional output. Nat. Neurosci 22, 669–679 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Capeling MM et al. Nonadhesive alginate hydrogels support growth of pluripotent stem cell-derived intestinal organoids. Stem Cell Rep 12, 381–394 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Chen Y, Zhou W, Roh T, Estes MK & Kaplan DL In vitro enteroid-derived three-dimensional tissue model of human small intestinal epithelium with innate immune responses. PLOS ONE 12, e0187880 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Banerjee I, Pangule RC & Kane RS Antifouling coatings: recent developments in the design of surfaces that prevent fouling by proteins, bacteria, and marine organisms. Adv. Mater 23, 690–718 (2011). [DOI] [PubMed] [Google Scholar]
- 175.Zhu J. Bioactive modification of poly(ethylene glycol) hydrogels for tissue engineering. Biomaterials 31, 4639–4656 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Enemchukwu NO et al. Synthetic matrices reveal contributions of ECM biophysical and biochemical properties to epithelial morphogenesis. J. Cell Biol 212, 113–124 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sengupta D. & Heilshorn SC Protein-engineered biomaterials: highly tunable tissue engineering scaffolds. Tissue Eng. Part B Rev 16, 285–293 (2010). [DOI] [PubMed] [Google Scholar]
- 178.DiMarco RL, Dewi RE, Bernal G, Kuo C. & Heilshorn SC Protein-engineered scaffolds for in vitro 3D culture of primary adult intestinal organoids. Biomater. Sci 3, 1376–1385 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Candiello J. et al. 3D heterogeneous islet organoid generation from human embryonic stem cells using a novel engineered hydrogel platform. Biomaterials 177, 27–39 (2018). [DOI] [PubMed] [Google Scholar]
- 180.Sasai Y. Cytosystems dynamics in self-organization of tissue architecture. Nature 493, 318–326 (2013). [DOI] [PubMed] [Google Scholar]
- 181.Li J. & Mooney DJ Designing hydrogels for controlled drug delivery. Nat. Rev. Mater. 1, 16071 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Liang Y. & Kiick KL Heparin-functionalized polymeric biomaterials in tissue engineering and drug delivery applications. Acta Biomater 10, 1588–1600 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sakiyama-Elbert SE Incorporation of heparin into biomaterials. Acta Biomater 10, 1581–1587 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Vulic K. & Shoichet MS Affinity-based drug delivery systems for tissue repair and regeneration. Biomacromolecules 15, 3867–3880 (2014). [DOI] [PubMed] [Google Scholar]
- 185.Willerth SM, Rader A. & Sakiyama-Elbert SE The effect of controlled growth factor delivery on embryonic stem cell differentiation inside fibrin scaffolds. Stem Cell Res 1, 205–218 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Guo C. et al. Bio-orthogonal conjugation and enzymatically triggered release of proteins within multi-layered hydrogels. Acta Biomater 56, 80–90 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Straley KS & Heilshorn SC Independent tuning of multiple biomaterial properties using protein engineering. Soft Matter 5, 114–124 (2009). [Google Scholar]
- 188.Patterson J. & Hubbell JA Enhanced proteolytic degradation of molecularly engineered PEG hydrogels in response to MMP-1 and MMP-2. Biomaterials 31, 7836–7845 (2010). [DOI] [PubMed] [Google Scholar]
- 189.Kukreja M. et al. High-throughput multiplexed peptide-centric profiling illustrates both substrate cleavage redundancy and specificity in the MMP family. Chem. Biol 22, 1122–1133 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kwon MY et al. Dose and timing of N-cadherin mimetic peptides regulate MSC chondrogenesis within hydrogels. Adv. Healthc. Mater 7, 1701199 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Ruskowitz ER & DeForest CA Photoresponsive biomaterials for targeted drug delivery and 4D cell culture. Nat. Rev. Mater 3, 17087–17017 (2018). [Google Scholar]
- 192.Wylie RG et al. Spatially controlled simultaneous patterning of multiple growth factors in three-dimensional hydrogels. Nat. Mater 10, 799–806 (2011) [DOI] [PubMed] [Google Scholar]
- 193.DeForest CA & Tirrell DA A photoreversible protein-patterning approach for guiding stem cell fate in three-dimensional gels. Nat. Mater 14, 523–531 (2015). [DOI] [PubMed] [Google Scholar]
- 194.Grim JC et al. A reversible and repeatable thiol-ene bioconjugation for dynamic patterning of signaling proteins in hydrogels. ACS Cent. Sci 4, 909–916 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Jeon O, Lee K. & Alsberg E. Spatial micropatterning of growth factors in 3D hydrogels for location-specific regulation of cellular behaviors. Small 14, 1800579 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Hoffmann JC & West JL Three-dimensional photolithographic patterning of multiple bioactive ligands in poly(ethylene glycol) hydrogels. Soft Matter 6, 5056–5063 (2010). [Google Scholar]
- 197.Shadish JA, Benuska GM & DeForest CA Bioactive site-specifically modified proteins for 4D patterning of gel biomaterials. Nat. Mater 10.1038/s41563-019-0367-7 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Attayek PJ et al. In vitro polarization of colonoids to create an intestinal stem cell compartment. PLOS ONE 11, e0153795 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Thorne CA et al. Enteroid monolayers reveal an autonomous WNT and BMP circuit controlling intestinal epithelial growth and organization. Dev. Cell 44, 624–633.e4 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Cederquist GY et al. Specification of positional identity in forebrain organoids. Nat. Biotechnol 37, 436–444 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Nguyen EH, Schwartz MP & Murphy WL Biomimetic approaches to control soluble concentration gradients in biomaterials. Macromol. Biosci 11, 483–492 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Foty RA & Steinberg MS The differential adhesion hypothesis: a direct evaluation. Dev. Biol 278, 255–263 (2005). [DOI] [PubMed] [Google Scholar]
- 203.Brodland GW The differential interfacial tension hypothesis (DITH): a comprehensive theory for the self-rearrangement of embryonic cells and tissues. J. Biomech. Eng 124, 188–197 (2002). [DOI] [PubMed] [Google Scholar]
- 204.Fagotto F. The cellular basis of tissue separation. Development 141, 3303–3318 (2014). [DOI] [PubMed] [Google Scholar]
- 205.Canty L, Zarour E, Kashkooli L, Francois P. & Fagotto F. Sorting at embryonic boundaries requires high heterotypic interfacial tension. Nat. Commun 8, 157 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Knight GT et al. Engineering induction of singular neural rosette emergence within hPSC-derived tissues. Elife 7, e37549 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Knight GT, Sha J. & Ashton RS Micropatterned, clickable culture substrates enable in situ spatiotemporal control of human PSC-derived neural tissue morphology. Chem. Commun 51, 5238–5241 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Cerchiari AE et al. A strategy for tissue self-organization that is robust to cellular heterogeneity and plasticity. Proc. Natl. Acad. Sci. USA 112, 2287–2292 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.DeForest CA, Polizzotti BD & Anseth KS Sequential click reactions for synthesizing and patterning three-dimensional cell microenvironments. Nat. Mater 8, 659–664 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Pedron S. et al. Patterning three-dimensional hydrogel microenvironments using hyperbranched polyglycerols for independent control of mesh size and stiffness. Biomacromolecules 18, 1393–1400 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Luo Y. & Shoichet MS A photolabile hydrogel for guided three-dimensional cell growth and migration. Nat. Mater 3, 249–253 (2004). [DOI] [PubMed] [Google Scholar]
- 212.Lee SH, Moon JJ & West JL Three-dimensional micropatterning of bioactive hydrogels via two-photon laser scanning photolithography for guided 3D cell migration. Biomaterials 29, 2962–2968 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Guvendiren M. & Burdick JA Stiffening hydrogels to probe short-and long-term cellular responses to dynamic mechanics. Nat. Commun 3, 792 (2012). [DOI] [PubMed] [Google Scholar]
- 214.Marklein RA & Burdick JA Spatially controlled hydrogel mechanics to modulate stem cell interactions. Soft Matter 6, 136–143 (2010). [Google Scholar]
- 215.Doyle AD, Wang FW, Matsumoto K. & Yamada KM One-dimensional topography underlies three-dimensional fibrillar cell migration. J. Cell Biol 184, 481–490 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Plotnikov SV, Pasapera AM, Sabass B. & Waterman CM Force fluctuations within focal adhesions mediate ECM-rigidity sensing to guide directed cell migration. Cell 151, 1513–1527 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Brown TE et al. Photopolymerized dynamic hydrogels with tunable viscoelastic properties through thioester exchange. Biomaterials 178, 496–503 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Shao Y. et al. Self-organized amniogenesis by human pluripotent stem cells in a biomimetic implantation-like niche. Nat. Mater 16, 419–425 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Shao Y. et al. A pluripotent stem cell-based model for post-implantation human amniotic sac development. Nat. Commun 8, 208 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lancaster MA et al. Guided self-organization and cortical plate formation in human brain organoids. Nat. Biotechnol 35, 659–666 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Madl CM, Katz LM & Heilshorn SC Tuning bulk hydrogel degradation by simultaneous control of proteolytic cleavage kinetics and hydrogel network architecture. ACS Macro. Lett 7, 1302–1307 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Mori H, Gjorevski N, Inman JL, Bissell MJ & Nelson CM Self-organization of engineered epithelial tubules by differential cellular motility. Proc. Natl. Acad. Sci. USA 106, 14890–14895 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Sarig-Nadir O, Livnat N, Zajdman R, Shoham S. & Seliktar D. Laser photoablation of guidance microchannels into hydrogels directs cell growth in three dimensions. Biophys. J. 96, 4743–4752 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.McKinnon DD, Brown TE, Kyburz KA, Kiyotake E. & Anseth KS Design and characterization of a synthetically accessible, photodegradable hydrogel for user-directed formation of neural networks. Biomacromolecules 15, 2808–2816 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Badeau BA, Comerford MP, Arakawa CK, Shadish JA & DeForest CA Engineered modular biomaterial logic gates for environmentally triggered therapeutic delivery. Nat. Chem 10, 251–258 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Moroni L. et al. Biofabrication strategies for 3D in vitro models and regenerative medicine. Nat. Rev. Mater 3, 21–37 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Workman MJ et al. Engineered human pluripotent-stem-cell-derived intestinal tissues with a functional enteric nervous system. Nat. Med 23, 49–59 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Xiang Y. et al. hESC-derived thalamic organoids form reciprocal projections when fused with cortical organoids. Cell Stem Cell 24, 487–497.e7 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Du Y, Lo E, Ali S. & Khademhosseini A. Directed assembly of cell-laden microgels for fabrication of 3D tissue constructs. Proc. Natl. Acad. Sci. USA 105, 9522–9527 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Kang HW et al. A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat. Biotechnol 34, 312–319 (2016). [DOI] [PubMed] [Google Scholar]
- 231.Groll J. et al. A definition of bioinks and their distinction from biomaterial inks. Biofabrication 11, 013001 (2018). [DOI] [PubMed] [Google Scholar]
- 232.Jia W. et al. Direct 3D bioprinting of perfusable vascular constructs using a blend bioink. Biomaterials 106, 58–68 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Zhang YS et al. Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials 110, 45–59 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Mironov V. et al. Organ printing: tissue spheroids as building blocks. Biomaterials 30, 2164–2174 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Yu Y. et al. Three-dimensional bioprinting using self-assembling scalable scaffold-free “tissue strands” as a new bioink. Sci. Rep 6, 28714 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Laronda MM et al. A bioprosthetic ovary created using 3D printed microporous scaffolds restores ovarian function in sterilized mice. Nat. Commun 8, 15261 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Chen HJ, Miller P. & Shuler ML A pumpless body-on-a-chip model using a primary culture of human intestinal cells and a 3D culture of liver cells. Lab Chip 18, 2036–2046 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Chen WLK et al. Integrated gut/liver microphysiological systems elucidates inflammatory inter-tissue crosstalk. Biotechnol. BioEng 114, 2648–2659 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Esch MB, Ueno H, Applegate DR & Shuler ML Modular, pumpless body-on-a-chip platform for the co-culture of GI tract epithelium and 3D primary liver tissue. Lab Chip 16, 2719–2729 (2016). [DOI] [PubMed] [Google Scholar]
- 240.Benam KH et al. Matched-comparative modeling of normal and diseased human airway responses using a microengineered breathing lung chip. Cell Systems 3, 456–466.e4 (2016). [DOI] [PubMed] [Google Scholar]
- 241.Barrile R. et al. Organ-on-chip recapitulates thrombosis induced by an anti-CD154 monoclonal antibody: translational potential of advanced microengineered systems. Clin. Pharmacol. Ther 104, 1240–1248 (2018). [DOI] [PubMed] [Google Scholar]
- 242.Figtree GA, Bubb KJ, Tang O, Kizana E. & Gentile C. Vascularized cardiac spheroids as novel 3D in vitro models to study cardiac fibrosis. Cells Tissues Organs 204, 191–198 (2017). [DOI] [PubMed] [Google Scholar]
- 243.Nguyen EH et al. Versatile synthetic alternatives to Matrigel for vascular toxicity screening and stem cell expansion. Nat. Biomed. Eng 1, 0096 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Soofi SS, Last JA, Liliensiek SJ, Nealey PF & Murphy CJ The elastic modulus of Matrigel as determined by atomic force microscopy. J. Struct. Biol 167, 216–219 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Chaudhuri O. et al. Extracellular matrix stiffness and composition jointly regulate the induction of malignant phenotypes in mammary epithelium. Nat. Mater 13, 970–978 (2014). [DOI] [PubMed] [Google Scholar]
- 246.Villa-Diaz LG, Ross AM, Lahann J. & Krebsbach PH Concise review: the evolution of human pluripotent stem cell culture: from feeder cells to synthetic coatings. Stem Cells 31, 1–7 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Halbleib JM & Nelson WJ Cadherins in development: cell adhesion, sorting, and tissue morphogenesis. Genes Dev 20, 3199–3214 (2006). [DOI] [PubMed] [Google Scholar]
- 248.Takeichi M. Cadherins: a molecular family important in selective cell-cell adhesion. Annu. Rev Biochem 59, 237–252 (1990). [DOI] [PubMed] [Google Scholar]
- 249.Steinberg MS & McNutt PM Cadherins and their connections: adhesion junctions have broader functions. Curr. Opin. Cell Biol 11, 554–560 (1999). [DOI] [PubMed] [Google Scholar]
- 250.Katsamba P. et al. Linking molecular affinity and cellular specificity in cadherin-mediated adhesion. Proc. Natl. Acad. Sci. USA 106, 11594–11599 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Vendome J. et al. Structural and energetic determinants of adhesive binding specificity in type I cadherins. Proc. Natl. Acad. Sci. USA 111, E4175-E4184 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.le Duc Q. et al. Vinculin potentiates E-cadherin mechanosensing and is recruited to actin-anchored sites within adherens junctions in a myosin II-dependent manner. J. Cell Biol 189, 1107–1115 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Leckband DE, le Duc Q, Wang N. & de Rooij J. Mechanotransduction at cadherin-mediated adhesions. Curr. Opin. Cell Biol 23, 523–530 (2011). [DOI] [PubMed] [Google Scholar]
- 254.Cosgrove BD et al. N-cadherin adhesive interactions modulate matrix mechanosensing and fate commitment of mesenchymal stem cells. Nat. Mater 15, 1297–1306 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Bian L, Guvendiren M, Mauck RL & Burdick JA Hydrogels that mimic developmentally relevant matrix and N-cadherin interactions enhance MSC chondrogenesis. Proc. Natl. Acad. Sci. USA 110, 10117–10122 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Karthaus WR et al. Identification of multipotent luminal progenitor cells in human prostate organoid cultures. Cell 159, 163–175 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Jo J. et al. Midbrain-like organoids from human pluripotent stem cells contain functional dopaminergic and neuromelanin-producing neurons. Cell Stem Cell 19, 248–257 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Miller AJ et al. Generation of lung organoids from human pluripotent stem cells in vitro. Nat. Protoc 14, 518–540 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Baptista PM et al. The use of whole organ decellularization for the generation of a vascularized liver organoid. Hepatology 53, 604–617 (2011). [DOI] [PubMed] [Google Scholar]
- 260.Finkbeiner SR et al. Generation of tissue-engineered small intestine using embryonic stem cell-derived human intestinal organoids. Biol. Open 4, 1462–1472 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Astashkina AI, Mann BK, Prestwich GD & Grainger DWA 3-D organoid kidney culture model engineered for high-throughput nephrotoxicity assays. Biomaterials 33, 4700–4711 (2012). [DOI] [PubMed] [Google Scholar]
- 262.Broguiere N. et al. Growth of epithelial organoids in a defined hydrogel. Adv. Mater 30, 1801621 (2018). [DOI] [PubMed] [Google Scholar]
- 263.Greggio C. et al. Artificial three-dimensional niches deconstruct pancreas development in vitro. Development 140, 4452–4462 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Langer R. & Vacanti JP Tissue engineering. Science 260, 920–926 (1993). [DOI] [PubMed] [Google Scholar]
- 265.Drumheller PD & Hubbell JA Densely crosslinked polymer networks of poly(ethylene glycol) in trimethylolpropane triacrylate for cell-adhesion-resistant surfaces. J. Biomed. Mater. Res 29, 207–215 (1995). [DOI] [PubMed] [Google Scholar]
- 266.Rheinwald JG & Green H. Formation of a keratinizing epithelium in culture by a cloned cell line derived from a teratoma. Cell 6, 317–330 (1975). [DOI] [PubMed] [Google Scholar]
- 267.Martin GR Isolation of a pluripotent cell line from early mouse embryos cultured in medium conditioned by teratocarcinoma stem cells. Proc. Natl. Acad. Sci. USA 78, 7634–7638 (1981). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Li ML et al. Influence of a reconstituted basement membrane and its components on casein gene expression and secretion in mouse mammary epithelial cells. Proc. Natl. Acad. Sci. USA 84, 136–140 (1987). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Thomson JA et al. Embryonic stem cell lines derived from human blastocysts. Science 282, 1145–1147 (1998). [DOI] [PubMed] [Google Scholar]
- 270.Takahashi K. & Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006). [DOI] [PubMed] [Google Scholar]