Abstract
Simple Summary
Lung adenocarcinoma (LUAD) is the major subtype of lung cancer and represents the deadliest human cancer, affecting current-, ex-, and even non-smokers. LUAD is driven by the accumulation of mutations in several different genes, which results in uncontrolled proliferation of the lung cells and the formation of tumors. Our immune system can recognize these transformed cancer cells and start an immune response in order to eliminate them. Unfortunately, cancer cells in turn adapt to and ultimately evade host immune defenses, fostering their growth. Current therapeutic approaches for cancer patients called “immunotherapies” aim to overcome the cancer’s ability to develop mechanisms of resistance to our immune defenses. This review summarizes the mechanisms used by LUAD cancer cells to develop immune resistance and discusses current and future therapeutic approaches in LUAD patient management.
Abstract
Lung cancer is the leading cancer killer worldwide, imposing grievous challenges for patients and clinicians. The incidence of lung adenocarcinoma (LUAD), the main histologic subtype of lung cancer, is still increasing in current-, ex-, and even non-smokers, whereas its five-year survival rate is approximately 15% as the vast majority of patients usually present with advanced disease at the time of diagnosis. The generation of novel drugs targeting key disease driver mutations has created optimism for the treatment of LUAD, but, as these mutations are not universal, this therapeutic line benefits only a subset of patients. More recently, the advent of targeted immunotherapies and their documented clinical efficacy in many different cancers, including LUAD, have started to change cancer management. Immunotherapies have been developed in order to overcome the cancer’s ability to develop mechanisms of immune resistance, i.e., to adapt to and evade the host inflammatory and immune responses. Identifying a cancer’s immune resistance mechanisms will likely advance the development of personalized immunotherapies. This review examines the key pathways of immune resistance at play in LUAD and explores therapeutic strategies which can unleash potent antitumor immune responses and significantly improve therapeutic efficacy, quality of life, and survival in LUAD.
Keywords: non-small cell lung cancer, lung adenocarcinoma, immune resistance, targeted therapies, immunotherapy
1. Introduction
Lung cancer represents one of the most challenging health problems, claiming each year more lives than breast, prostate and pancreatic cancer combined [1]. Non-small-cell lung cancer (NSCLC) accounts for approximately 85% of lung cancer incidence, and lung adenocarcinoma (LUAD), NSCLC’s most prevalent subtype, is still increasing in current-, ex-, and even non-smokers [2]. Patients with localized and early stage disease receive standard surgery, but the vast majority of patients are usually diagnosed with advanced disease, receive conventional therapies such as combination chemotherapy and radiation, and face a high mortality rate.
In the classical sense, cancer is driven by genetic and epigenetic aberrations and the complicated cross-talk between many different pathways, involving mainly mutations activating proto-oncogenes and/or suppressing tumor suppressors and resulting in uncontrolled cell proliferation. Targeted therapies have been developed for some of these genetic aberrations, rendering the molecular characterization of a patient’s tumor an imperative prerequisite for the successful design of the most efficient targeted treatment strategy. Among the most commonly found mutations in LUAD, caused spontaneously, by genetic predisposition, or by cigarette smoking and other noxious inhaled agents, are activating mutations in epidermal growth factor receptor (EGFR, 14%), Kirsten rat sarcoma virus (KRAS, 33%), mesenchymal epithelial transition factor proto-oncogene (MET, 7%), B-Raf proto-oncogene (BRAF, 10%), and Phosphatidylinositol-4,5-Bisphosphate 3-Kinase Catalytic Subunit Alpha (PIK3CA, 7%), mutations in tumor suppressor genes like tumor protein p53 (TP53, 46%) and serine/threonine kinase 11 (STK11, 17%), and translocations in anaplastic lymphoma kinase (ALK, 3–7%), ROS proto-oncogene 1(ROS1, 2%), or Ret proto-oncogene (RET, 1–2%) [3]. In the case of EGFR activating mutations, first-line treatment includes EGFR tyrosine kinase inhibitors (EGFR-TKI, like gefitinib, erlotinib, afatinib, and osimertinib), whereas BRAF-mutant tumors can be treated with dabrafenib and trametinib [4,5,6]. Encouraging results have also been demonstrated for patients harboring ALK (crizotinib, ceritinib, alectinib, brigatinib, and lorlatinib), ROS1 (crizotinib, ceritinib, and lorlatinib) or RET translocations (cabozantinib) [5,6,7,8]. Crizotinib can be also effective against MET-mutant cancers [5]. The inhibitors of PIK3CA signaling pathway, temsirolimus and everolimus, are currently under clinical trials [6]. Unfortunately, these treatments benefit only a small subset of LUAD patients, not only because all other mutated genes are not yet effectively clinically targeted, but also due to the development of primary and secondary resistance [9]. KRAS, the most commonly mutated driver oncogene in LUAD, remains notoriously untargeted. What is more, its mutations are mutually exclusive with EGFR mutations, so patients with KRAS mutations are resistant to EGFR targeted treatment and are faced with no efficient treatment options and a poor prognosis [10,11]. Encouragingly, the KRASG12C inhibitor sotorasib can potentially be the first approved targeted therapy for patients with KRASG12C-mutant NSCLC [12].
The emergence of deregulated host inflammatory pathways as an important hallmark of cancer development [13] has added great complexity to the above classical sense of cancer pathogenesis, but has also provided an alternative approach for novel therapeutic strategies. Chronic lung inflammation associated with tobacco smoking is strongly implicated in LUAD development, highlighting the dynamic communication of lung tumors with the surrounding tumor microenvironment (TME), consisting of the interface of the bronchoalveolar compartment with host immune cells, cytokines, chemokines, and other components [13]. Developing tumors can hijack and evade host immune surveillance mechanisms [13], and immunotherapies aim to stimulate the patient’s immune system to elicit a competent anti-tumor immune response. Several such approaches have been developed, including vaccine therapy [14], chimeric antigen receptor (CAR) T cells [15], and immune checkpoint inhibitors (ICI) like antibodies against cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) [16], programmed cell death 1 (PD-1) and programmed cell death ligand 1 (PD-L1) [17,18,19], and are currently used in clinical practice for the treatment of several cancers, including lung cancer [20]. Despite these encouraging results, increased immune tolerance is often documented in many cancers [21], implying that there is more to learn about the cross-talk between the developing tumors and the immune cells within the TME. Interestingly, KRAS mutations are increasingly shown to affect tumor interactions with the surrounding TME [11,22,23,24,25]. Below we will discuss the main mechanisms of tumor immune resistance, with a special emphasis on LUAD and mutant KRAS-mediated effects underlying immune resistance mechanisms.
2. Tobacco Smoke Immunomodulatory Effects
LUAD development is strongly associated with environmental exposures like cigarette smoking. Tobacco smoke contains many chemical constituents and irritant particles which are deposited on the airways and cause repeated or chronic pulmonary inflammation, sculpturing the TME [26]. The inflammatory response is initiated with the influx of neutrophils and macrophages, resulting in the secretion of signaling molecules like tumor necrosis factor (TNF) and interleukins (IL) IL-6, IL-8, and IL-1β [27,28], and in the activation of signaling cascades involving nuclear factor-κB (NF-κB), mutant RAS or ERK [29,30,31]. This ultimately leads to the secretion of immunosuppressive factors, permitting the malignant transformation of lung epithelial cells [27,30,32]. Interestingly, lung tumors of smokers and non-smokers display very distinct inflammatory signatures, with marked differences in mast cell and CD4+ T cell numbers [33]. Furthermore, it has been postulated that activated neutrophils can enhance the genomic instability caused by tobacco smoke carcinogens in lung epithelial cells, suggesting that inflammation can actually act as a tumor initiator or promoter [27,34].
3. Tumor Heterogeneity
LUAD tumors are characterized by great heterogeneity, as evidenced by the thousands of different mutations identified per cancer genome, including single nucleotide variants (SNV), copy number alterations (CNA), gene fusions, and major chromosomal events [3,35]. The differences between smokers and non-smokers in the TME described in the previous paragraph are also mirrored in the different genomic LUAD profiles between the two groups, with smokers displaying higher mutations burdens [3]. Of course, mutational hotspots are also found in LUAD, involving activating mutations in EGFR, KRAS, BRAF, and PIK3CA, deleterious mutations in tumor suppressor genes like TP53 and STK11, and balanced inversions (translocations or fusions) in ALK or RET [3]. A current mutation plot and mutual exclusivity and co-occurrence information of frequent cancer genes from the cBioportal analyzing the TCGA (The Cancer Genome Atlas) pan-cancer LUAD dataset are shown in Figure 1 and Table 1, respectively. Indicative of the bewildering tumor heterogeneity evident in the plot is also the fact that even among patients with the same smoking status or the same driver mutation, a marked intratumoral heterogeneity will be observed, as each tumor contains a plurality of populations of cancer cells, with different genetic and epigenetic features [36]. Intratumoral heterogeneity also assumes that different cell lineages can be targeted by drug treatment, as some subpopulations, containing the suitable genetic disposition, will display resistance. Under the constant pressure within the TME, tumor cells, exhibiting a remarkable plasticity, modulate their antigenic landscape, evade immune surveillance, survive and continue to propagate. These cells can then drive expression of signaling effectors which will favor tumor growth. Intratumoral heterogeneity remains a constant threat to immunotherapies.
4. Inflammatory Interactions of LUAD Cells with the Tumor Microenvironment Mediating Immune Escape
LUAD tumor cells establish a complex surrounding TME rich in inflammatory signaling, orchestrated by expression of cytokines, chemokines, and their cognate receptors by both cancer and host cells [37]. This inflammatory signaling results in the attraction of various immune cellular populations, including tumor-associated macrophages (TAMs), tumor-reactive lymphocytes, myeloid-derived suppressor cells (MDSCs), tumor-associated neutrophils and mast cells, which interact with tumor cells to ultimately shape a highly immune suppressive TME, with diminished tumor cytotoxic and enhanced tumor-promoting manifestations [38,39,40].
TAMs are the most crucial immune cell type of the TME, favor cancer progression, and are associated with poor prognosis [39,41]. Macrophages are generally classified into two distinct and reactive populations, perpetually changing their phenotype as they dynamically respond to environmental alterations of the TME. M1 or classically activated pro-inflammatory macrophages are typically activated by IFN-γ and lipopolysaccharide, express IL-12 and mediate anti-tumor responses. On the other hand, M2 or alternatively activated macrophages are typically activated by IL-4, IL-13 and IL-10, express IL-10 and favor wound healing as well as tumor development by suppressing anti-tumor T cell responses [40].
Pulmonary alveolar macrophages have also been implicated in lung cancer pathobiology. Resident alveolar macrophages display significant immunomodulatory properties and an M2 phenotype in the naïve state. They adopt immunosuppressive roles in preventing unwanted immune responses to environmental antigens that bombard the lungs every day. It has been postulated that these immunosuppressive functions can be hijacked by tumors to their advantage, and although the exact role of alveolar macrophages in the pathobiology of lung cancer remains controversial, recent evidence suggests that they can be preconditioned by primary tumors to suppress immune responses in the lungs, thereby facilitating cancer progression [42].
MDSCs are immune suppressive myeloid cells fostering tumor progression in many different ways, most of which result in the inhibition of activation of tumor-reactive T cells and of natural killer (NK) cell cytotoxicity [40]. Evidence supports a key role of the spleen as an intermediate organ in their phenotypic education, prior to their migration from the bone marrow to tumor sites [40] Figure 1 and Table 1.
Figure 1.
A current mutation plot of the most frequently altered genes in the TCGA pan-cancer Lung adenocarcinoma (LUAD) dataset (n = 507). Queried genes (TP53, LRP1B, KRAS, PTPRD, CDKN2A, KEAP1, PCLO, RELN, CDKN2B, STK11, EGFR, NKX2-1, TERT, MTAP, NF1, FOXA1, MCL1, ALK, ROS1, EML4) were altered in 475 (94%) of patients. Note the heterogeneity and mosaic complexity of mutations in key cancer genes. Note also the multiple mutual exclusivity and addiction patterns that are used to provide clues to which genes are candidate drivers or passengers. Data from https://www.cbioportal.org/study/summary?id=luad_tcga_pan_can_atlas_2018 [43,44].
Table 1.
Mutual exclusivity and co-occurrence of frequently altered cancer genes in the TCGA pan-cancer LUAD dataset (n = 507). Queried genes were frequently mutually exclusive (MUEX; indicating dominant oncogenes) or co-occurring (COOC; indicating oncogene addiction). p, probability, hypergeometric test; q, probability, false discovery rate. Data are from https://www.cbioportal.org/study/summary?id=luad_tcga_pan_can_atlas_2018 [43,44].
| A | B | Neither | A Not B | B Not A | Both | Log2 Odds Ratio | p-Value | q-Value | Tendency |
|---|---|---|---|---|---|---|---|---|---|
| CDKN2A | CDKN2B | 402 | 22 | 0 | 83 | >3 | <0.001 | <0.001 | COOC |
| CDKN2B | MTAP | 422 | 21 | 2 | 62 | >3 | <0.001 | <0.001 | COOC |
| CDKN2A | MTAP | 400 | 43 | 2 | 62 | >3 | <0.001 | <0.001 | COOC |
| NKX2-1 | FOXA1 | 433 | 20 | 5 | 49 | >3 | <0.001 | <0.001 | COOC |
| PCLO | RELN | 361 | 58 | 45 | 43 | 2.572 | <0.001 | <0.001 | COOC |
| KRAS | EGFR | 265 | 163 | 73 | 6 | −2.904 | <0.001 | <0.001 | MUEX |
| LRP1B | RELN | 288 | 131 | 33 | 55 | 1.873 | <0.001 | <0.001 | COOC |
| LRP1B | PCLO | 278 | 128 | 43 | 58 | 1.551 | <0.001 | <0.001 | COOC |
| TP53 | LRP1B | 179 | 142 | 64 | 122 | 1.265 | <0.001 | <0.001 | COOC |
| TP53 | PCLO | 215 | 191 | 28 | 73 | 1.553 | <0.001 | <0.001 | COOC |
| ALK | EML4 | 462 | 28 | 9 | 8 | >3 | <0.001 | <0.001 | COOC |
| KEAP1 | STK11 | 359 | 68 | 49 | 31 | 1.74 | <0.001 | <0.001 | COOC |
| TP53 | KRAS | 139 | 199 | 104 | 65 | −1.196 | <0.001 | <0.001 | MUEX |
| KRAS | STK11 | 301 | 126 | 37 | 43 | 1.473 | <0.001 | <0.001 | COOC |
| TP53 | TERT | 225 | 212 | 18 | 52 | 1.616 | <0.001 | <0.001 | COOC |
| TP53 | NF1 | 226 | 216 | 17 | 48 | 1.563 | <0.001 | 0.001 | COOC |
| LRP1B | PTPRD | 261 | 124 | 60 | 62 | 1.121 | <0.001 | 0.002 | COOC |
| CDKN2A | ROS1 | 384 | 89 | 18 | 16 | 1.939 | <0.001 | 0.003 | COOC |
| TP53 | EGFR | 219 | 209 | 24 | 55 | 1.264 | <0.001 | 0.005 | COOC |
| KRAS | NF1 | 283 | 159 | 55 | 10 | −1.628 | <0.001 | 0.005 | MUEX |
| LRP1B | EGFR | 258 | 170 | 63 | 16 | −1.375 | <0.001 | 0.005 | MUEX |
| TP53 | RELN | 215 | 204 | 28 | 60 | 1.175 | <0.001 | 0.005 | COOC |
| PTPRD | PCLO | 321 | 85 | 64 | 37 | 1.126 | 0.001 | 0.009 | COOC |
| STK11 | TERT | 360 | 77 | 67 | 3 | −2.256 | 0.002 | 0.013 | MUEX |
| PTPRD | RELN | 329 | 90 | 56 | 32 | 1.063 | 0.003 | 0.022 | COOC |
| KRAS | ROS1 | 308 | 165 | 30 | 4 | −2.006 | 0.003 | 0.022 | MUEX |
| KEAP1 | EGFR | 336 | 92 | 72 | 7 | −1.494 | 0.005 | 0.033 | MUEX |
| STK11 | EGFR | 353 | 75 | 74 | 5 | −1.653 | 0.006 | 0.041 | MUEX |
| TP53 | PTPRD | 197 | 188 | 46 | 76 | 0.792 | 0.006 | 0.041 | COOC |
| TP53 | STK11 | 194 | 233 | 49 | 31 | −0.925 | 0.007 | 0.042 | MUEX |
| LRP1B | KRAS | 227 | 111 | 94 | 75 | 0.706 | 0.007 | 0.046 | COOC |
Tumor infiltrating T cells are key players in the establishment of a favorable TME. Among them, T regulatory cells (Treg) exhibit immune suppressing functions, which, through the secretion of IL-10 and transforming growth factor (TGF)-β, help cancer cells evade the immune defensive mechanisms [45]. Lung tumor cells express immunosuppressive factors, such as IL-10 and TGFβ, contributing to the recruitment Tregs and MDSCs [46,47].
KRAS mutations are common activating mutations in LUAD (Figure 1). KRAS-mutant LUAD appear to be densely infiltrated by myeloid-derived immune cells (mainly macrophages, neutrophils and eosinophils) [48], indicating that there might be a correlation between KRAS mutations and immune cell specificity within the TME. Experimental models of LUAD formation provide a unique tool for the dissection of the mechanisms adopted by tumor cells to recruit inflammatory cells to the TME and to thereafter hijack the host immune repertoire to their advantage. By using genetically modified mice permitting the oncogenic overexpression of mutant Kras in bronchial club epithelial cells expressing Clara cell secretory protein (CC10), Ji et al. showed an overwhelming neutrophil attraction to the TME accompanying LUAD formation and identified mutant Kras tumor-elaborated CXC chemokines (and their human orthologues IL-8 and CXCL-5) as the crucial mediators for this mechanism [49]. Mutant KRAS-mediated expansion of myeloid-derived suppressor cells resulted in the suppression of the antitumor activity of CD8+ cytotoxic T cells [50].
Cross-talk within the TME between tumor and host immune cells resulting in pro-tumorigenic effects is increasingly elucidated in the context of other thoracic malignancies as well. For LUAD tumor cells with the ability to metastasize to the pleura and foster a malignant pleural effusion (MPE), it has been shown that the determining factor is the presence of KRAS activating mutations, which favor the production of CCL2 by the tumor cells. In turn, tumor-elaborated CCL2 paracrine signaling attracts CD11b+GR1+ myeloid cells to the pleural cavity [23]. This axis was further elucidated by the identification of an additional important tumor-host inflammatory circuit at play in MPE formation, which provided important insights on how an oncogene can co-opt the TME to favor tumor progression. Specifically, mutant KRAS tumor cells were shown to respond to IL-1β secretion from the CCL2-recruited myeloid cells by activating the alternative signaling cascade of NF-κB pathway, forming in this way a circuit which fuels the secretion of CXCL1 by tumor cells, enhances tumor and MPE development and drives drug resistance [25]. Additionally, LUAD tumor cells used in a model of pleural carcinomatosis were found to secrete the chemoattractant CCL2 and the protein osteopontin (SPP1) in order to mediate mast cells recruitment and degranulation [51]. In the same study, the adenocarcinoma cells were also shown to trigger myeloid cells to secrete IL-1β [51]. Mast cell-derived IL-1β was also documented as a factor fostering LUAD development in a study which utilized experimental mouse models of carcinogen-induced LUAD to show the significance of mast cells in LUAD progression [24].
IL-1β is an inflammatory mediator implicated in many different malignancies. In NSCLC IL-1β has been evaluated as a prognostic marker portending poor survival [52] and the above observations clearly establish a link between IL-1β and KRAS mutant lung cancer. Tobacco smoke also causes the bronchial epithelium to produce IL-1β [53]. This link of IL-1β to lung cancer has been recently clinically tested, with fascinating results. In a clinical trial assessing the anti-inflammatory effects on cardiovascular disease of a novel inhibitor of IL-1β (Canakinumab, ACZ885, Ilaris), the Canakinumab Anti-Inflammatory Thrombosis Outcomes Study (CANTOS), the authors also documented an impressive decrease in NSCLC incidence and mortality, an outcome recognizing the potential of IL-1β inhibition in NSCLC [54,55]. At the molecular level, mitigating IL-1β signaling would prevent the oncogenic activation of the alternative pathway of NF-κB signaling in lung cancer cells, impairing in this way the cascade initiated by KRAS mutant tumor cells [25]. Enhanced IL-1β secretion by tumor-associated neutrophils has also been described as a mechanism mediating drug resistance in experimental models of lung cancer [56], raising the hope that the inhibition of IL-1β signaling could also diminish the occurrence of tumor resistance incidences.
KRAS-mutant tumors are characterized by large amount of neoantigens [22], and as such they are faced with the need to tackle the immune response mediated by tumor-specific T cells in order to sustain their growth. Along this line, it has been documented that KRAS activation downregulates expression of MHC I at the cell surface, thus impairing recognition by CD8+ T cells and promoting immune evasion [57,58]. Furthermore, KRAS mutations upregulated expression of the suppressive cytokines IL-10 and TGFβ1, which converted CD4+ T helper cells into T regulatory cells (Tregs) [59]. Tregs are immunosuppressive cells which have been identified to play important roles during KRAS mutant tumorigenesis [60]. In the lung epithelium, activating KRAS mutations resulted in elevated numbers of Th17 cells, which in turn produced high levels of IL17. This cytokine then activated a cascade involving the acceleration of cell proliferation, the production of metalloproteases (MMP-7 and MMP-12) and of additional proinflammatory cytokines like IL6, CCL2, and CXCL2, and ultimately the attraction of MDSCs to the lung [61,62]. Interestingly, differences have been documented between KRAS mutant and EGFR mutant LUAD relating to their immune content, with the former presenting increased populations of Tregs, IL17-producing lymphocytes and reduced NK cells [48]. Finally, mutant KRAS silencing led to increased expression of MHC I surface proteins on tumor cells and production of IL-18, inducing ultimately tumor regression [63].
The above observations are of particular clinical interest if KRAS activating mutations affect the response or the resistance to currently licensed immunotherapies. After all, it is well documented that immune checkpoint blockade treatment has durable beneficial effects for patients with NSCLC [12,64,65,66,67], and even more so for lung cancer patients harboring mutations in both TP53 and KRAS [68]. Supporting this notion, PD-L1 overexpression has been found to be mediated through the mutant KRAS-ERK signaling axis [69,70], and the highest level of PD-L1 expression was found in KRAS/TP53 co-mutated lung tumors [68]. Accumulating evidence suggest that KRAS mutations that coexist with wild-type STK11 co-operate for establishment of an immunosuppressive TME [71,72,73].
It is now widely accepted that KRAS extensively regulates the cross-talk between cancer and host immune cells, promoting the switch from an anti-tumor to a pro-tumor response and the development of immune escape mechanisms.
5. Adaptive Immune Resistance
Tumors are rich sources of neoantigens, formed as a sequence of their somatic mutations, which are foreign to the immune system and therefore capable of eliciting a robust antitumor immune response [74]. This indicates that tumors can progressively foster their growth by adopting mechanisms permitting tumor neoantigens to go unnoticed by the host immune defenses. The term adaptive immune resistance describes the process in which tumor cells change their phenotype, in a dynamic and reactive fashion, in order to avoid a host immune attack orchestrated by tumor neoantigen-specific cytotoxic T cells [75]. The adaptive immune resistance is the product of the cross-talk between tumor and host immune cells within the TME. Normally, T cell activation requires the interaction of antigen-specific T cells with the cognate tumor antigen. After T cell activation, signaling through the T-cell receptor (TCR) induces a robust immune response, triggered by secretion of interferon, and the expression of regulatory receptors (such as PD-1 and CTLA-4), which will act as a negative feedback mechanism. For this to happen, interferon also induces the expression of PD-L1, and the molecular interaction between the receptor and the ligand limits the inflammatory response [19]. This adaptive process is used by the tumor, which expresses PD-L1 and thereby turns off PD-1-positive T cells [76]. Usually PD-L1 expression is restricted at the invasive margin of the tumor, an area with abundant T cells, suggesting that PD-L1 expression is a counteracting mechanism adopted by tumor cells as a consequence of the presence of tumor antigen-specific T cells [77,78]. Interestingly, PD-L1 expression is not only triggered in cancer cells but also on the surface of dendritic cells, macrophages, myeloid-derived cells, TME stromal cells, and even tumor infiltrating T cells [77,79,80,81]. Another alternative is that PD-L1 overexpression is the result of gene amplification events of chromosome 9 [82]. Disruption of this negative feedback using anti-PD-1, anti-PD-L1, or anti-CTLA4 antibodies reactivates T-cell cytotoxic properties which effectively lead to tumor antigen-specific immune responses and tumor killing [16,17,18,19].
The production of proinflammatory cytokines within the TME may also result in tumor adaptive changes and immune evasion. It has been shown that tumor necrosis factor-a (TNF-α) production by infiltrating T cells promoted a dedifferentiating process in melanoma cancer cells, thereby leading to tumor antigen loss and an adaptive immune escape mechanism [83]. This process resembles the epithelial-to-mesenchymal transition (EMT), and in fact many aspects of EMT are related to inflammatory cytokines like IL6, TNFα and tumor growth factor-β TGFβ [83,84,85]. In this way, an adaptive immune resistance mechanism can even be a tumor promoting mechanism.
6. Acquired Immune Resistance
Blocking the PD-1 and CTL-4 axes with specific antibodies (like the anti-PD-1 molecules nivolumab, pembrolizumab and the emerging cemiplimab, the anti-PD-L1 antibodies atezolizumab and durvalumab, and the anti-CTL-4 antibody ipilimumab) exhibits durable beneficial effects for patients with NSCLC, with or without KRAS mutations [64,65,66,67,86,87].
Unfortunately, not all patients with LUAD can benefit from blockade of immune checkpoints, and many of the initial responders will eventually develop resistance to the therapy [88], while the mechanisms behind this phenomenon are currently under intense scrutiny.
For patients who are refractory to immune checkpoint blockade, one possible explanation is that their tumors contain low mutational load and they lack immunogenic tumor antigens, such as nonsmoker LUAD [89,90]. In conjunction with low mutation burden, the activation of MAPK in EGFR-mutant LUAD contributed in the establishment of highly immunosuppressive conditions due to increased recruitment of Tregs and TAMs [91].
For patients with acquired resistance to immunotherapies, possible explanations are the upregulation of alternative immune checkpoints, mainly T-cell immunoglobulin mucin-3 (TIM-3) [92], loss of HLA haplotypes due to rearrangement of chromosome 6 [93,94,95] and somatic mutations in interferon receptor-associated Janus kinase 1 (JAK1) or Janus kinase 2 (JAK2) and antigen-presenting protein beta-2-microglobulin [B2M, leading to loss of surface expression of major histocompatibility complex class I (MHC I)] [96,97]. Loss of tumor neoantigens through elimination of tumor subclones or chromosomal deletions has also been described as a mechanism of immune edited acquired resistance in lung cancer, in which tumors responded to the selective pressure of immune checkpoint blockade by eliminating mutations affecting MHC and TCR binding [98]. Similarly, immunoediting induced by immune checkpoint blockade transformed NSCLC to SCLC (small cell lung cancer) by selectively eliminating the treatment-sensitive tumor cells [99,100].
7. Drug Resistance
Cancer cells can become excessively dependent on specific driver mutations, a characteristic defined as “oncogene addiction” [101]. As a result, many targeted therapies have been developed aiming to inhibit these oncogenic driver mutations and genotype-directed therapy in advanced NSCLC has led to significant improvements in overall survival [102]. For patients with EGFR somatic mutations, administration of small molecule TKIs of EGFR (gefitinib, erlotinib, afatinib, and osimertinib) is the standard course of treatment, resulting in high response rates and prolonged progression-free survival [4]. Encouraging results have also been demonstrated for patients harboring ALK rearrangements, after receiving treatment with ALK-TKIs (crizotinib, ceritinib, and alectinib) [7]. The effectiveness of TKI therapy is however limited by the ability of cancer cells to evolve under the pressure of the therapy and to ultimately acquire resistance [9].
A total of 4–10% of newly diagnosed NSCLC patients will not respond to TKI therapy, exhibiting what is called primary (intrinsic) resistance [9]. One mechanism underlying intrinsic resistance could be the existence of activating yet non-sensitizing driver mutations, as has been described for the EGFR-T790M mutation with reported frequencies varying from <10% to 65% [103,104]. The combination of EGFR mutations with other genetic alterations has also been shown to contribute to intrinsic resistance to TKIs, like MET amplification and BCL2L11 mutation [104,105]. Another potential modulator conferring intrinsic resistance to EGFR-TKIs is NF-κB. It has been reported that knocking down NF-κB in EGFR-mutant lung cancer cells enhanced erlotinib sensitivity, while patient response to erlotinib was associated with high expression of the NF-κB inhibitor IκBα [106], raising hope that a combinatorial treatment targeting both EGFR and NF-κB can have beneficial responses in the clinic.
Unfortunately, even patients who initially respond positively to TKIs administration, usually develop secondary or acquired resistance to the treatment followed by disease progression. Most commonly, this is attributed to secondary somatic mutations of the target gene which hinder the binding of the drug and confer in this way resistance to treatment. In EGFR-mutant NSCLC, the dominant cause of TKI acquired resistance is the EGFR-T790M mutation, accounting for more than half of the incidences of reported resistance [105,107]. The most common secondary mutations found in ALK-mutant NSCLC are the ALK-L1196M and ALK-G1269A mutations, causing resistance by interfering with TKI binding [108,109]. Another mechanism responsible for acquired resistance to TKI therapy is gene target amplification. This has been documented with both mutant EGFR and ALK, and gene amplification can occur alone or in combination with the secondary somatic resistance mutations [107,109]. LUAD can also adapt to the pressure of TKIs by activating bypass signaling pathways, which allow cancer cells to continue to grow despite the targeting of the driver gene mutations, like PI3K/AKT or RAF/MEK/ERK pathways [3,110], or by triggered mutations activating downstream effector molecules of the targeted cascade, like MAPK activation in both EGFR- and ALK-mutant NSCLC [111,112]. NSCLC has also been shown to phenotypically transform to SCLC in order to resist TKIs treatment, resulting in the formation of an EGFR- or ALK-mutant SCLC, which is insensitive to TKIs therapy [107,113]. Finally, the notion of “drug tolerant cells” has been also suggested to explain both intrinsic and acquired resistance, which dictates that small populations of cancer cells can tolerate the drug exposure, possibly due to epigenetic changes, persist under a quiescent state and propagate until a more permanent resistance mechanism is acquired [114].
Conceptually, all resistance mechanisms can be viewed as the dynamic manifestations of cancer evolution in order to overcome the selective pressure of targeted therapies.
8. Strategies to Overcome Resistance
As cancer resistance mechanisms are under intense research scrutiny, the culprits of these endeavors have shed some light on the profound complexities of tumor biology and have guided the design of new therapeutic strategies. Immune checkpoint blockers are currently at the forefront of cancer therapeutics, with many clinical trials underway assessing the efficacy of the treatment to many solid cancers, including LUAD [115]. Significant research has also been done towards the use of CAR T cells in the very challenging context of solid tumors [15]. Despite the obstacles, the preclinical combination of CAR T cells with checkpoint immune inhibitors has demonstrated encouraging results and is now under clinical trials for EGFR mutant tumors [116]. Furthermore, strategies targeting Tregs, TAMs and MDSCs are also being evaluated [47,117], along with the development of newer generation TKIs and combinatorial drug treatments to overcome resistance [9].
Accumulating evidence supports the pivotal role of KRAS not only in governing cancer cells’ autonomous mechanisms of proliferation, but also in controlling the immune landscape within the TME and in mediating immune escape and ultimately tumor progression. Although the gene remains largely untargeted, pioneering studies have elucidated the signaling cascades originating in lung cancer cells from KRAS activating mutations and have provided the medical community with novel therapeutic targets, such as the combined KRAS/NF-κB inhibition [25]. Of note, inhibition of IL-1β, another downstream effector of mutant KRAS, is currently evaluated for NSCLC with very promising results [54,55].
9. Conclusions
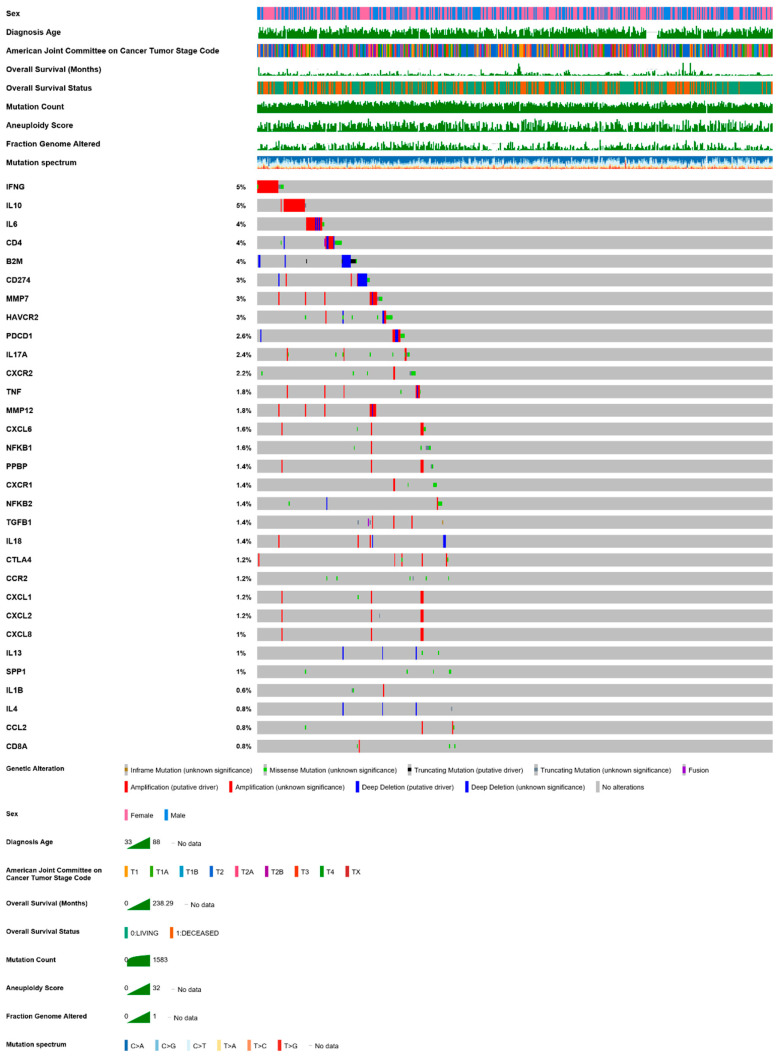
Immunotherapies hold great promise in extending the survival of patients with LUAD. Despite these significant advances, cancers still find ways to counteract any therapeutic strategy, by dynamically evolving and developing resistance mechanisms. Further and deeper understanding of the cross-talk between cancer and host immune cells within the TME will broaden our knowledge on the fundamental mechanisms of tumor escape from the immune system and will hopefully advance precision medicine and personalized combination immunotherapy. For example, the significance of the frequent co-alterations in immune genes observed in LUAD (such as the genes mentioned in this text, analyzed in Figure 2 and Table 2), have received far less attention than cancer drivers, and need to be functionally explored in the future in terms of their cellular localization and function. In conclusion, LUAD is probably one of the best studied bodily cancers and immunotherapy against this form of lung tumors has come a long way. Tackling immune resistance of this dreadful tumor will be the next great challenge for thoracic oncology.
Figure 2.
A mutation plot of altered immune genes reviewed in this text in the TCGA pan-cancer LUAD dataset (n = 507). Queried genes (IFNG, IL10, IL6, CD4, B2M, CD274, MMP7, HAVCR2, PDCD1, IL17A, CXCR2, TNF, MMP12, CXCL6, NFKB1, PPBP, CXCR1, NFKB2, TGFB1, IL18, CTLA4, CCR2, CXCL1, CXCL2, CXCL8, IL13, SPP1, IL1B, IL4, CCL2, CD8A) were altered in 135 patients (98%). Data from https://www.cbioportal.org/study/summary?id=luad_tcga_pan_can_atlas_2018 [43,44].
Table 2.
Co-occurrence of frequently altered immune genes in the TCGA pan-cancer LUAD dataset (n = 507). Queried genes (IFNG, IL10, IL6, CD4, B2M, CD274, MMP7, HAVCR2, PDCD1, IL17A, CXCR2, TNF, MMP12, CXCL6, NFKB1, PPBP, CXCR1, NFKB2, TGFB1, IL18, CTLA4, CCR2, CXCL1, CXCL2, CXCL8, IL13, SPP1, IL1B, IL4, CCL2, CD8A) were never mutually exclusive but frequently co-occurring (COOC; indicating oncogene addiction). p, probability, hypergeometric test; q, probability, false discovery rate. Data are freely available at https://www.cbioportal.org/study/summary?id=luad_tcga_pan_can_atlas_2018 [43,44].
| A | B | Neither | A Not B | B Not A | Both | Log2 Odds Ratio | p-Value | q-Value | Tendency |
|---|---|---|---|---|---|---|---|---|---|
| MMP7 | MMP12 | 492 | 6 | 0 | 9 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL1 | CXCL8 | 501 | 1 | 0 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL2 | CXCL8 | 501 | 1 | 0 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| PPBP | CXCL8 | 500 | 2 | 0 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL1 | CXCL2 | 500 | 1 | 1 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL6 | CXCL8 | 499 | 3 | 0 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| PPBP | CXCL1 | 499 | 2 | 1 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| PPBP | CXCL2 | 499 | 2 | 1 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL6 | CXCL1 | 498 | 3 | 1 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL6 | CXCL2 | 498 | 3 | 1 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| CXCL6 | PPBP | 497 | 3 | 2 | 5 | >3 | <0.001 | <0.001 | Co-occurrence |
| IL13 | IL4 | 501 | 2 | 1 | 3 | >3 | <0.001 | <0.001 | Co-occurrence |
| TGFB1 | IL18 | 496 | 4 | 4 | 3 | >3 | <0.001 | 0.002 | Co-occurrence |
| MMP12 | IL18 | 494 | 6 | 4 | 3 | >3 | <0.001 | 0.004 | Co-occurrence |
| MMP7 | IL18 | 488 | 12 | 4 | 3 | >3 | <0.001 | 0.021 | Co-occurrence |
Author Contributions
Conceptualization, M.S.; writing—original draft preparation, M.S.; writing—review and editing, G.T.S.; supervision, G.T.S.; funding acquisition, M.S., G.T.S. All authors have read and agreed to the published version of the manuscript.
Funding
M.S. is funded by the General Secretariat for Research and Technology (GSRT) and the Hellenic Foundation for Research and Innovation (HFRI) grant #1853. G.T.S. is funded by the Graduate College (Graduiertenkolleg, GRK) #2338 of the German Research Society (Deutsche Forschungsgemeinschaft, DFG), the target validation project for pharmaceutical development ALTERNATIVE of the German Ministry for Education and Research (BundesministeriumfürBildung und Forschung, BMBF), anda Translational Research Grant by the German Center for Lung Research (DeutschesZentrumfürLungenforschung, DZL).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the writing of the manuscript.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Siegel R.L., Miller K.D., Jemal A. Cancer statistics, 2020. CA Cancer J. Clin. 2020;70:7–30. doi: 10.3322/caac.21590. [DOI] [PubMed] [Google Scholar]
- 2.Ma J., Ward E.M., Smith R., Jemal A. Annual number of lung cancer deaths potentially avertable by screening in the United States. Cancer. 2013;119:1381–1385. doi: 10.1002/cncr.27813. [DOI] [PubMed] [Google Scholar]
- 3.Cancer Genome Atlas Research Network Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–550. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dempke W.C., Suto T., Reck M. Targeted therapies for non-small cell lung cancer. Lung Cancer. 2010;67:257–274. doi: 10.1016/j.lungcan.2009.10.012. [DOI] [PubMed] [Google Scholar]
- 5.Shea M., Costa D.B., Rangachari D. Management of advanced non-small cell lung cancers with known mutations or rearrangements: Latest evidence and treatment approaches. Ther. Adv. Respir. Dis. 2016;10:113–129. doi: 10.1177/1753465815617871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yuan M., Huang L.L., Chen J.H., Wu J., Xu Q. The emerging treatment landscape of targeted therapy in non-small-cell lung cancer. Signal Transduct. Target Ther. 2019;4:61. doi: 10.1038/s41392-019-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kwak E.L., Bang Y.J., Camidge D.R., Shaw A.T., Solomon B., Maki R.G., Ou S.H., Dezube B.J., Janne P.A., Costa D.B., et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N. Engl. J. Med. 2010;363:1693–1703. doi: 10.1056/NEJMoa1006448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drilon A., Wang L., Hasanovic A., Suehara Y., Lipson D., Stephens P., Ross J., Miller V., Ginsberg M., Zakowski M.F., et al. Response to Cabozantinib in patients with RET fusion-positive lung adenocarcinomas. Cancer Discov. 2013;3:630–635. doi: 10.1158/2159-8290.CD-13-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin J.J., Shaw A.T. Resisting Resistance: Targeted Therapies in Lung Cancer. Trends Cancer. 2016;2:350–364. doi: 10.1016/j.trecan.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hames M.L., Chen H., Iams W., Aston J., Lovly C.M., Horn L. Correlation between KRAS mutation status and response to chemotherapy in patients with advanced non-small cell lung cancer. Lung Cancer. 2016;92:29–34. doi: 10.1016/j.lungcan.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dias Carvalho P., Machado A.L., Martins F., Seruca R., Velho S. Targeting the Tumor Microenvironment: An Unexplored Strategy for Mutant KRAS Tumors. Cancers. 2019;11:2010. doi: 10.3390/cancers11122010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong D.S., Fakih M.G., Strickler J.H., Desai J., Durm G.A., Shapiro G.I., Falchook G.S., Price T.J., Sacher A., Denlinger C.S., et al. KRAS(G12C) Inhibition with Sotorasib in Advanced Solid Tumors. N. Engl. J. Med. 2020;383:1207–1217. doi: 10.1056/NEJMoa1917239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hanahan D., Weinberg R.A. Hallmarks of cancer: The next generation. Cell. 2011;144:646–674. doi: 10.1016/j.cell.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 14.Wong K.K., Li W.A., Mooney D.J., Dranoff G. Advances in Therapeutic Cancer Vaccines. Adv. Immunol. 2016;130:191–249. doi: 10.1016/bs.ai.2015.12.001.S0065-2776(15)30001-8. [DOI] [PubMed] [Google Scholar]
- 15.Martinez M., Moon E.K. CAR T Cells for Solid Tumors: New Strategies for Finding, Infiltrating, and Surviving in the Tumor Microenvironment. Front. Immunol. 2019;10:128. doi: 10.3389/fimmu.2019.00128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenberg S.A. Decade in review-cancer immunotherapy: Entering the mainstream of cancer treatment. Nat. Rev. Clin. Oncol. 2014;11:630–632. doi: 10.1038/nrclinonc.2014.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dong H., Strome S.E., Salomao D.R., Tamura H., Hirano F., Flies D.B., Roche P.C., Lu J., Zhu G., Tamada K., et al. Tumor-associated B7-H1 promotes T-cell apoptosis: A potential mechanism of immune evasion. Nat. Med. 2002;8:793–800. doi: 10.1038/nm730. [DOI] [PubMed] [Google Scholar]
- 18.Curiel T.J., Wei S., Dong H., Alvarez X., Cheng P., Mottram P., Krzysiek R., Knutson K.L., Daniel B., Zimmermann M.C., et al. Blockade of B7-H1 improves myeloid dendritic cell-mediated antitumor immunity. Nat. Med. 2003;9:562–567. doi: 10.1038/nm863. [DOI] [PubMed] [Google Scholar]
- 19.Freeman G.J., Long A.J., Iwai Y., Bourque K., Chernova T., Nishimura H., Fitz L.J., Malenkovich N., Okazaki T., Byrne M.C., et al. Engagement of the PD-1 immunoinhibitory receptor by a novel B7 family member leads to negative regulation of lymphocyte activation. J. Exp. Med. 2000;192:1027–1034. doi: 10.1084/jem.192.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall R.D., Gray J.E., Chiappori A.A. Beyond the standard of care: A review of novel immunotherapy trials for the treatment of lung cancer. Cancer Control. 2013;20:22–31. doi: 10.1177/107327481302000105. [DOI] [PubMed] [Google Scholar]
- 21.Bonavida B., Chouaib S. Resistance to anticancer immunity in cancer patients: Potential strategies to reverse resistance. Ann. Oncol. 2017;28:457–467. doi: 10.1093/annonc/mdw615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dias Carvalho P., Guimaraes C.F., Cardoso A.P., Mendonca S., Costa A.M., Oliveira M.J., Velho S. KRAS Oncogenic Signaling Extends beyond Cancer Cells to Orchestrate the Microenvironment. Cancer Res. 2018;78:7–14. doi: 10.1158/0008-5472.CAN-17-2084. [DOI] [PubMed] [Google Scholar]
- 23.Agalioti T., Giannou A.D., Krontira A.C., Kanellakis N.I., Kati D., Vreka M., Pepe M., Spella M., Lilis I., Zazara D.E., et al. Mutant KRAS promotes malignant pleural effusion formation. Nat. Commun. 2017;8:15205. doi: 10.1038/ncomms15205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lilis I., Ntaliarda G., Papaleonidopoulos V., Giotopoulou G.A., Oplopoiou M., Marazioti A., Spella M., Marwitz S., Goldmann T., Bravou V., et al. Interleukin-1beta provided by KIT-competent mast cells is required for KRAS-mutant lung adenocarcinoma. Oncoimmunology. 2019;8:1593802. doi: 10.1080/2162402X.2019.1593802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marazioti A., Lilis I., Vreka M., Apostolopoulou H., Kalogeropoulou A., Giopanou I., Giotopoulou G.A., Krontira A.C., Iliopoulou M., Kanellakis N.I., et al. Myeloid-derived interleukin-1beta drives oncogenic KRAS-NF-kappaBeta addiction in malignant pleural effusion. Nat. Commun. 2018;9:672. doi: 10.1038/s41467-018-03051-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Giotopoulou G.A., Stathopoulos G.T. Effects of Inhaled Tobacco Smoke on the Pulmonary Tumor Microenvironment. Adv. Exp. Med. Biol. 2020;1225:53–69. doi: 10.1007/978-3-030-35727-6_4. [DOI] [PubMed] [Google Scholar]
- 27.Engels E.A. Inflammation in the development of lung cancer: Epidemiological evidence. Expert Rev. Anticancer. Ther. 2008;8:605–615. doi: 10.1586/14737140.8.4.605. [DOI] [PubMed] [Google Scholar]
- 28.Kode A., Yang S.R., Rahman I. Differential effects of cigarette smoke on oxidative stress and proinflammatory cytokine release in primary human airway epithelial cells and in a variety of transformed alveolar epithelial cells. Respir. Res. 2006;7:132. doi: 10.1186/1465-9921-7-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reynolds P.R., Kasteler S.D., Schmitt R.E., Hoidal J.R. Receptor for advanced glycation end-products signals through Ras during tobacco smoke-induced pulmonary inflammation. Am. J. Respir. Cell Mol. Biol. 2011;45:411–418. doi: 10.1165/rcmb.2010-0231OC. [DOI] [PubMed] [Google Scholar]
- 30.Kroening P.R., Barnes T.W., Pease L., Limper A., Kita H., Vassallo R. Cigarette smoke-induced oxidative stress suppresses generation of dendritic cell IL-12 and IL-23 through ERK-dependent pathways. J. Immunol. 2008;181:1536–1547. doi: 10.4049/jimmunol.181.2.1536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu X., Togo S., Al-Mugotir M., Kim H., Fang Q., Kobayashi T., Wang X., Mao L., Bitterman P., Rennard S. NF-kappaB mediates the survival of human bronchial epithelial cells exposed to cigarette smoke extract. Respir. Res. 2008;9:66. doi: 10.1186/1465-9921-9-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Herr C., Beisswenger C., Hess C., Kandler K., Suttorp N., Welte T., Schroeder J.M., Vogelmeier C. Suppression of pulmonary innate host defence in smokers. Thorax. 2009;64:144–149. doi: 10.1136/thx.2008.102681. [DOI] [PubMed] [Google Scholar]
- 33.Li X., Li J., Wu P., Zhou L., Lu B., Ying K., Chen E., Lu Y., Liu P. Smoker and non-smoker lung adenocarcinoma is characterized by distinct tumor immune microenvironments. Oncoimmunology. 2018;7:e1494677. doi: 10.1080/2162402X.2018.1494677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weitzman S.A., Gordon L.I. Inflammation and cancer: Role of phagocyte-generated oxidants in carcinogenesis. Blood. 1990;76:655–663. doi: 10.1182/blood.V76.4.655.655. [DOI] [PubMed] [Google Scholar]
- 35.Campbell J.D., Alexandrov A., Kim J., Wala J., Berger A.H., Pedamallu C.S., Shukla S.A., Guo G., Brooks A.N., Murray B.A., et al. Distinct patterns of somatic genome alterations in lung adenocarcinomas and squamous cell carcinomas. Nat. Genet. 2016;48:607–616. doi: 10.1038/ng.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.McGranahan N., Swanton C. Clonal Heterogeneity and Tumor Evolution: Past, Present, and the Future. Cell. 2017;168:613–628. doi: 10.1016/j.cell.2017.01.018. [DOI] [PubMed] [Google Scholar]
- 37.Allavena P., Germano G., Marchesi F., Mantovani A. Chemokines in cancer related inflammation. Exp. Cell Res. 2011;317:664–673. doi: 10.1016/j.yexcr.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 38.Bronte V., Cingarlini S., Marigo I., De Santo C., Gallina G., Dolcetti L., Ugel S., Peranzoni E., Mandruzzato S., Zanovello P. Leukocyte infiltration in cancer creates an unfavorable environment for antitumor immune responses: A novel target for therapeutic intervention. Immunol. Investig. 2006;35:327–357. doi: 10.1080/08820130600754994. [DOI] [PubMed] [Google Scholar]
- 39.Zaynagetdinov R., Sherrill T.P., Polosukhin V.V., Han W., Ausborn J.A., McLoed A.G., McMahon F.B., Gleaves L.A., Degryse A.L., Stathopoulos G.T., et al. A critical role for macrophages in promotion of urethane-induced lung carcinogenesis. J. Immunol. 2011;187:5703–5711. doi: 10.4049/jimmunol.1100558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ostrand-Rosenberg S., Sinha P., Beury D.W., Clements V.K. Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression. Semin. Cancer Biol. 2012;22:275–281. doi: 10.1016/j.semcancer.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pollard J.W. Tumour-educated macrophages promote tumour progression and metastasis. Nat. Rev. Cancer. 2004;4:71–78. doi: 10.1038/nrc1256. [DOI] [PubMed] [Google Scholar]
- 42.Sharma S.K., Chintala N.K., Vadrevu S.K., Patel J., Karbowniczek M., Markiewski M.M. Pulmonary alveolar macrophages contribute to the premetastatic niche by suppressing antitumor T cell responses in the lungs. J. Immunol. 2015;194:5529–5538. doi: 10.4049/jimmunol.1403215. [DOI] [PubMed] [Google Scholar]
- 43.Cerami E., Gao J., Dogrusoz U., Gross B.E., Sumer S.O., Aksoy B.A., Jacobsen A., Byrne C.J., Heuer M.L., Larsson E., et al. The cBio cancer genomics portal: An open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gao J., Aksoy B.A., Dogrusoz U., Dresdner G., Gross B., Sumer S.O., Sun Y., Jacobsen A., Sinha R., Larsson E., et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013;6:pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zaynagetdinov R., Stathopoulos G.T., Sherrill T.P., Cheng D.S., McLoed A.G., Ausborn J.A., Polosukhin V.V., Connelly L., Zhou W., Fingleton B., et al. Epithelial nuclear factor-kappaB signaling promotes lung carcinogenesis via recruitment of regulatory T lymphocytes. Oncogene. 2012;31:3164–3176. doi: 10.1038/onc.2011.480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shimizu K., Nakata M., Hirami Y., Yukawa T., Maeda A., Tanemoto K. Tumor-infiltrating Foxp3+ regulatory T cells are correlated with cyclooxygenase-2 expression and are associated with recurrence in resected non-small cell lung cancer. J Thorac. Oncol. 2010;5:585–590. doi: 10.1097/JTO.0b013e3181d60fd7. [DOI] [PubMed] [Google Scholar]
- 47.Srivastava M.K., Andersson A., Zhu L., Harris-White M., Lee J.M., Dubinett S., Sharma S. Myeloid suppressor cells and immune modulation in lung cancer. Immunotherapy. 2012;4:291–304. doi: 10.2217/imt.11.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Busch S.E., Hanke M.L., Kargl J., Metz H.E., MacPherson D., Houghton A.M. Lung Cancer Subtypes Generate Unique Immune Responses. J. Immunol. 2016;197:4493–4503. doi: 10.4049/jimmunol.1600576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ji H., Houghton A.M., Mariani T.J., Perera S., Kim C.B., Padera R., Tonon G., McNamara K., Marconcini L.A., Hezel A., et al. K-ras activation generates an inflammatory response in lung tumors. Oncogene. 2006;25:2105–2112. doi: 10.1038/sj.onc.1209237. [DOI] [PubMed] [Google Scholar]
- 50.Bayne L.J., Beatty G.L., Jhala N., Clark C.E., Rhim A.D., Stanger B.Z., Vonderheide R.H. Tumor-derived granulocyte-macrophage colony-stimulating factor regulates myeloid inflammation and T cell immunity in pancreatic cancer. Cancer Cell. 2012;21:822–835. doi: 10.1016/j.ccr.2012.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Giannou A.D., Marazioti A., Spella M., Kanellakis N.I., Apostolopoulou H., Psallidas I., Prijovich Z.M., Vreka M., Zazara D.E., Lilis I., et al. Mast cells mediate malignant pleural effusion formation. J. Clin. Investig. 2015;125:2317–2334. doi: 10.1172/JCI79840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim J.W., Koh Y., Kim D.W., Ahn Y.O., Kim T.M., Han S.W., Oh D.Y., Lee S.H., Im S.A., Kim T.Y., et al. Clinical Implications of VEGF, TGF-beta1, and IL-1beta in Patients with Advanced Non-small Cell Lung Cancer. Cancer Res. Treat. 2013;45:325–333. doi: 10.4143/crt.2013.45.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gagné-Ouellet V.J.É., Boucher-Lafleur A.M., Plante S., Bouchard L., Chakir J., Laprise C. Tobacco smoke induces changes in IL-1 family in bronchial epithelial cells obtained from asthmatic individuals. All Asth. Clin. Immun. 2014;10:A55. doi: 10.1186/1710-1492-10-S2-A55. [DOI] [Google Scholar]
- 54.Ridker P.M., Everett B.M., Thuren T., MacFadyen J.G., Chang W.H., Ballantyne C., Fonseca F., Nicolau J., Koenig W., Anker S.D., et al. Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N. Engl. J. Med. 2017;377:1119–1131. doi: 10.1056/NEJMoa1707914. [DOI] [PubMed] [Google Scholar]
- 55.Ridker P.M., MacFadyen J.G., Thuren T., Everett B.M., Libby P., Glynn R.J. Effect of interleukin-1beta inhibition with canakinumab on incident lung cancer in patients with atherosclerosis: Exploratory results from a randomised, double-blind, placebo-controlled trial. Lancet. 2017;390:1833–1842. doi: 10.1016/S0140-6736(17)32247-X. [DOI] [PubMed] [Google Scholar]
- 56.McLoed A.G., Sherrill T.P., Cheng D.S., Han W., Saxon J.A., Gleaves L.A., Wu P., Polosukhin V.V., Karin M., Yull F.E., et al. Neutrophil-Derived IL-1beta Impairs the Efficacy of NF-kappaB Inhibitors against Lung Cancer. Cell Rep. 2016;16:120–132. doi: 10.1016/j.celrep.2016.05.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Testorelli C., Bussini S., De Filippi R., Marelli O., Orlando L., Greiner J.W., Grohmann U., Tentori L., Giuliani A., Bonmassar E., et al. Dacarbazine-induced immunogenicity of a murine leukemia is attenuated in cells transfected with mutated K-ras gene. J. Exp. Clin. Cancer Res. 1997;16:15–22. [PubMed] [Google Scholar]
- 58.Weijzen S., Velders M.P., Kast W.M. Modulation of the immune response and tumor growth by activated Ras. Leukemia. 1999;13:502–513. doi: 10.1038/sj.leu.2401367. [DOI] [PubMed] [Google Scholar]
- 59.Zdanov S., Mandapathil M., Abu Eid R., Adamson-Fadeyi S., Wilson W., Qian J., Carnie A., Tarasova N., Mkrtichyan M., Berzofsky J.A., et al. Mutant KRAS Conversion of Conventional T Cells into Regulatory T Cells. Cancer Immunol. Res. 2016;4:354–365. doi: 10.1158/2326-6066.CIR-15-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Granville C.A., Memmott R.M., Balogh A., Mariotti J., Kawabata S., Han W., Lopiccolo J., Foley J., Liewehr D.J., Steinberg S.M., et al. A central role for Foxp3+ regulatory T cells in K-Ras-driven lung tumorigenesis. PLoS ONE. 2009;4:e5061. doi: 10.1371/journal.pone.0005061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chang S.H. Tumorigenic Th17 cells in oncogenic Kras-driven and inflammation-accelerated lung cancer. Oncoimmunology. 2015;4:e955704. doi: 10.4161/21624011.2014.955704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chang S.H., Mirabolfathinejad S.G., Katta H., Cumpian A.M., Gong L., Caetano M.S., Moghaddam S.J., Dong C. T helper 17 cells play a critical pathogenic role in lung cancer. Proc. Natl. Acad. Sci. USA. 2014;111:5664–5669. doi: 10.1073/pnas.1319051111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Smakman N., Veenendaal L.M., van Diest P., Bos R., Offringa R., Borel Rinkes I.H., Kranenburg O. Dual effect of Kras(D12) knockdown on tumorigenesis: Increased immune-mediated tumor clearance and abrogation of tumor malignancy. Oncogene. 2005;24:8338–8342. doi: 10.1038/sj.onc.1208995. [DOI] [PubMed] [Google Scholar]
- 64.Borghaei H., Paz-Ares L., Horn L., Spigel D.R., Steins M., Ready N.E., Chow L.Q., Vokes E.E., Felip E., Holgado E., et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015;373:1627–1639. doi: 10.1056/NEJMoa1507643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Garon E.B., Rizvi N.A., Hui R., Leighl N., Balmanoukian A.S., Eder J.P., Patnaik A., Aggarwal C., Gubens M., Horn L., et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N. Engl. J. Med. 2015;372:2018–2028. doi: 10.1056/NEJMoa1501824. [DOI] [PubMed] [Google Scholar]
- 66.Brahmer J., Reckamp K.L., Baas P., Crino L., Eberhardt W.E., Poddubskaya E., Antonia S., Pluzanski A., Vokes E.E., Holgado E., et al. Nivolumab versus Docetaxel in Advanced Squamous-Cell Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2015;373:123–135. doi: 10.1056/NEJMoa1504627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rittmeyer A., Barlesi F., Waterkamp D., Park K., Ciardiello F., von Pawel J., Gadgeel S.M., Hida T., Kowalski D.M., Dols M.C., et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): A phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–265. doi: 10.1016/S0140-6736(16)32517-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dong Z.Y., Zhong W.Z., Zhang X.C., Su J., Xie Z., Liu S.Y., Tu H.Y., Chen H.J., Sun Y.L., Zhou Q., et al. Potential Predictive Value of TP53 and KRAS Mutation Status for Response to PD-1 Blockade Immunotherapy in Lung Adenocarcinoma. Clin Cancer Res. 2017;23:3012–3024. doi: 10.1158/1078-0432.CCR-16-2554. [DOI] [PubMed] [Google Scholar]
- 69.Huynh T.G., Morales-Oyarvide V., Campo M.J., Gainor J.F., Bozkurtlar E., Uruga H., Zhao L., Gomez-Caraballo M., Hata A.N., Mark E.J., et al. Programmed Cell Death Ligand 1 Expression in Resected Lung Adenocarcinomas: Association with Immune Microenvironment. J. Thorac. Oncol. 2016;11:1869–1878. doi: 10.1016/j.jtho.2016.08.134. [DOI] [PubMed] [Google Scholar]
- 70.Chen N., Fang W., Lin Z., Peng P., Wang J., Zhan J., Hong S., Huang J., Liu L., Sheng J., et al. KRAS mutation-induced upregulation of PD-L1 mediates immune escape in human lung adenocarcinoma. Cancer Immunol. Immunother. 2017;66:1175–1187. doi: 10.1007/s00262-017-2005-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Skoulidis F., Byers L.A., Diao L., Papadimitrakopoulou V.A., Tong P., Izzo J., Behrens C., Kadara H., Parra E.R., Canales J.R., et al. Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer Discov. 2015;5:860–877. doi: 10.1158/2159-8290.CD-14-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Koyama S., Akbay E.A., Li Y.Y., Aref A.R., Skoulidis F., Herter-Sprie G.S., Buczkowski K.A., Liu Y., Awad M.M., Denning W.L., et al. STK11/LKB1 Deficiency Promotes Neutrophil Recruitment and Proinflammatory Cytokine Production to Suppress T-cell Activity in the Lung Tumor Microenvironment. Cancer Res. 2016;76:999–1008. doi: 10.1158/0008-5472.CAN-15-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Herter-Sprie G.S., Koyama S., Korideck H., Hai J., Deng J., Li Y.Y., Buczkowski K.A., Grant A.K., Ullas S., Rhee K., et al. Synergy of radiotherapy and PD-1 blockade in Kras-mutant lung cancer. JCI Insight. 2016;1:e87415. doi: 10.1172/jci.insight.87415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Schumacher T.N., Schreiber R.D. Neoantigens in cancer immunotherapy. Science. 2015;348:69–74. doi: 10.1126/science.aaa4971. [DOI] [PubMed] [Google Scholar]
- 75.Ribas A. Adaptive Immune Resistance: How Cancer Protects from Immune Attack. Cancer Discov. 2015;5:915–919. doi: 10.1158/2159-8290.CD-15-0563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pardoll D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tumeh P.C., Harview C.L., Yearley J.H., Shintaku I.P., Taylor E.J., Robert L., Chmielowski B., Spasic M., Henry G., Ciobanu V., et al. PD-1 blockade induces responses by inhibiting adaptive immune resistance. Nature. 2014;515:568–571. doi: 10.1038/nature13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Taube J.M., Anders R.A., Young G.D., Xu H., Sharma R., McMiller T.L., Chen S., Klein A.P., Pardoll D.M., Topalian S.L., et al. Colocalization of inflammatory response with B7-h1 expression in human melanocytic lesions supports an adaptive resistance mechanism of immune escape. Sci. Transl. Med. 2012;4:127ra137. doi: 10.1126/scitranslmed.3003689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Herbst R.S., Soria J.C., Kowanetz M., Fine G.D., Hamid O., Gordon M.S., Sosman J.A., McDermott D.F., Powderly J.D., Gettinger S.N., et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515:563–567. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mayoux M., Roller A., Pulko V., Sammicheli S., Chen S., Sum E., Jost C., Fransen M.F., Buser R.B., Kowanetz M., et al. Dendritic cells dictate responses to PD-L1 blockade cancer immunotherapy. Sci. Transl. Med. 2020;12 doi: 10.1126/scitranslmed.aav7431. [DOI] [PubMed] [Google Scholar]
- 81.Oh S.A., Wu D.C., Cheung JNavarro A., Xiong H., Cubas R., Totpal K., Chiu H., Wu Y., Comps-Agrar L., Leader A.M., et al. PD-L1 expression by dendritic cells is a key regulator of T-cell immunity in cancer. Nat. Cancer. 2020:681–691. doi: 10.1038/s43018-020-0075-x. [DOI] [PubMed] [Google Scholar]
- 82.Green M.R., Monti S., Rodig S.J., Juszczynski P., Currie T., O’Donnell E., Chapuy B., Takeyama K., Neuberg D., Golub T.R., et al. Integrative analysis reveals selective 9p24.1 amplification, increased PD-1 ligand expression, and further induction via JAK2 in nodular sclerosing Hodgkin lymphoma and primary mediastinal large B-cell lymphoma. Blood. 2010;116:3268–3277. doi: 10.1182/blood-2010-05-282780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Landsberg J., Kohlmeyer J., Renn M., Bald T., Rogava M., Cron M., Fatho M., Lennerz V., Wolfel T., Holzel M., et al. Melanomas resist T-cell therapy through inflammation-induced reversible dedifferentiation. Nature. 2012;490:412–416. doi: 10.1038/nature11538. [DOI] [PubMed] [Google Scholar]
- 84.Knutson K.L., Lu H., Stone B., Reiman J.M., Behrens M.D., Prosperi C.M., Gad E.A., Smorlesi A., Disis M.L. Immunoediting of cancers may lead to epithelial to mesenchymal transition. J. Immunol. 2006;177:1526–1533. doi: 10.4049/jimmunol.177.3.1526. [DOI] [PubMed] [Google Scholar]
- 85.Santisteban M., Reiman J.M., Asiedu M.K., Behrens M.D., Nassar A., Kalli K.R., Haluska P., Ingle J.N., Hartmann L.C., Manjili M.H., et al. Immune-induced epithelial to mesenchymal transition in vivo generates breast cancer stem cells. Cancer Res. 2009;69:2887–2895. doi: 10.1158/0008-5472.CAN-08-3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mok T.S.K., Wu Y.L., Kudaba I., Kowalski D.M., Cho B.C., Turna H.Z., Castro G., Jr., Srimuninnimit V., Laktionov K.K., Bondarenko I., et al. Pembrolizumab versus chemotherapy for previously untreated, PD-L1-expressing, locally advanced or metastatic non-small-cell lung cancer (KEYNOTE-042): A randomised, open-label, controlled, phase 3 trial. Lancet. 2019;393:1819–1830. doi: 10.1016/S0140-6736(18)32409-7. [DOI] [PubMed] [Google Scholar]
- 87.Gandhi L., Rodriguez-Abreu D., Gadgeel S., Esteban E., Felip E., De Angelis F., Domine M., Clingan P., Hochmair M.J., Powell S.F., et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018;378:2078–2092. doi: 10.1056/NEJMoa1801005. [DOI] [PubMed] [Google Scholar]
- 88.Gettinger S.N., Horn L., Gandhi L., Spigel D.R., Antonia S.J., Rizvi N.A., Powderly J.D., Heist R.S., Carvajal R.D., Jackman D.M., et al. Overall Survival and Long-Term Safety of Nivolumab (Anti-Programmed Death 1 Antibody, BMS-936558, ONO-4538) in Patients with Previously Treated Advanced Non-Small-Cell Lung Cancer. J. Clin. Oncol. 2015;33:2004–2012. doi: 10.1200/JCO.2014.58.3708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Rizvi N.A., Hellmann M.D., Snyder A., Kvistborg P., Makarov V., Havel J.J., Lee W., Yuan J., Wong P., Ho T.S., et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348:124–128. doi: 10.1126/science.aaa1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Alexandrov L.B., Nik-Zainal S., Wedge D.C., Aparicio S.A., Behjati S., Biankin A.V., Bignell G.R., Bolli N., Borg A., Borresen-Dale A.L., et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415–421. doi: 10.1038/nature12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kinoshita T., Kudo-Saito C., Muramatsu R., Fujita T., Saito M., Nagumo H., Sakurai T., Noji S., Takahata E., Yaguchi T., et al. Determination of poor prognostic immune features of tumour microenvironment in non-smoking patients with lung adenocarcinoma. Eur. J. Cancer. 2017;86:15–27. doi: 10.1016/j.ejca.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 92.Koyama S., Akbay E.A., Li Y.Y., Herter-Sprie G.S., Buczkowski K.A., Richards W.G., Gandhi L., Redig A.J., Rodig S.J., Asahina H., et al. Adaptive resistance to therapeutic PD-1 blockade is associated with upregulation of alternative immune checkpoints. Nat. Commun. 2016;7:10501. doi: 10.1038/ncomms10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Maeurer M.J., Gollin S.M., Storkus W.J., Swaney W., Karbach J., Martin D., Castelli C., Salter R., Knuth A., Lotze M.T. Tumor escape from immune recognition: Loss of HLA-A2 melanoma cell surface expression is associated with a complex rearrangement of the short arm of chromosome 6. Clin. Cancer Res. 1996;2:641–652. [PubMed] [Google Scholar]
- 94.McGranahan N., Rosenthal R., Hiley C.T., Rowan A.J., Watkins T.B.K., Wilson G.A., Birkbak N.J., Veeriah S., Van Loo P., Herrero J., et al. Allele-Specific HLA Loss and Immune Escape in Lung Cancer Evolution. Cell. 2017;171:1259–1271.e1211. doi: 10.1016/j.cell.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Montesion M., Murugesan K., Jin D.X., Sharaf R., Sanchez N., Guria A., Minker M., Li G., Fisher V., Sokol E.S., et al. Somatic HLA class I loss is a widespread mechanism of immune evasion which refines the use of tumor mutational burden as a biomarker of checkpoint inhibitor response. Cancer Discov. 2020 doi: 10.1158/2159-8290.CD-20-0672. [DOI] [PubMed] [Google Scholar]
- 96.Zaretsky J.M., Garcia-Diaz A., Shin D.S., Escuin-Ordinas H., Hugo W., Hu-Lieskovan S., Torrejon D.Y., Abril-Rodriguez G., Sandoval S., Barthly L., et al. Mutations Associated with Acquired Resistance to PD-1 Blockade in Melanoma. N. Engl. J. Med. 2016;375:819–829. doi: 10.1056/NEJMoa1604958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gettinger S., Choi J., Hastings K., Truini A., Datar I., Sowell R., Wurtz A., Dong W., Cai G., Melnick M.A., et al. Impaired HLA Class I Antigen Processing and Presentation as a Mechanism of Acquired Resistance to Immune Checkpoint Inhibitors in Lung Cancer. Cancer Discov. 2017;7:1420–1435. doi: 10.1158/2159-8290.CD-17-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Anagnostou V., Smith K.N., Forde P.M., Niknafs N., Bhattacharya R., White J., Zhang T., Adleff V., Phallen J., Wali N., et al. Evolution of Neoantigen Landscape during Immune Checkpoint Blockade in Non-Small Cell Lung Cancer. Cancer Discov. 2017;7:264–276. doi: 10.1158/2159-8290.CD-16-0828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Bar J., Ofek E., Barshack I., Gottfried T., Zadok O., Kamer I., Urban D., Perelman M., Onn A. Transformation to small cell lung cancer as a mechanism of resistance to immunotherapy in non-small cell lung cancer. Lung Cancer. 2019;138:109–115. doi: 10.1016/j.lungcan.2019.09.025. [DOI] [PubMed] [Google Scholar]
- 100.Imakita T., Fujita K., Kanai O., Terashima T., Mio T. Small cell lung cancer transformation during immunotherapy with nivolumab: A case report. Respir. Med. Case Rep. 2017;21:52–55. doi: 10.1016/j.rmcr.2017.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Weinstein I.B. Cancer. Addiction to oncogenes--the Achilles heal of cancer. Science. 2002;297:63–64. doi: 10.1126/science.1073096. [DOI] [PubMed] [Google Scholar]
- 102.Barlesi F., Mazieres J., Merlio J.P., Debieuvre D., Mosser J., Lena H., Ouafik L., Besse B., Rouquette I., Westeel V., et al. Routine molecular profiling of patients with advanced non-small-cell lung cancer: Results of a 1-year nationwide programme of the French Cooperative Thoracic Intergroup (IFCT) Lancet. 2016;387:1415–1426. doi: 10.1016/S0140-6736(16)00004-0. [DOI] [PubMed] [Google Scholar]
- 103.Costa C., Molina M.A., Drozdowskyj A., Gimenez-Capitan A., Bertran-Alamillo J., Karachaliou N., Gervais R., Massuti B., Wei J., Moran T., et al. The impact of EGFR T790M mutations and BIM mRNA expression on outcome in patients with EGFR-mutant NSCLC treated with erlotinib or chemotherapy in the randomized phase III EURTAC trial. Clin. Cancer Res. 2014;20:2001–2010. doi: 10.1158/1078-0432.CCR-13-2233. [DOI] [PubMed] [Google Scholar]
- 104.Turke A.B., Zejnullahu K., Wu Y.L., Song Y., Dias-Santagata D., Lifshits E., Toschi L., Rogers A., Mok T., Sequist L., et al. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell. 2010;17:77–88. doi: 10.1016/j.ccr.2009.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Arcila M.E., Oxnard G.R., Nafa K., Riely G.J., Solomon S.B., Zakowski M.F., Kris M.G., Pao W., Miller V.A., Ladanyi M. Rebiopsy of lung cancer patients with acquired resistance to EGFR inhibitors and enhanced detection of the T790M mutation using a locked nucleic acid-based assay. Clin. Cancer Res. 2011;17:1169–1180. doi: 10.1158/1078-0432.CCR-10-2277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bivona T.G., Hieronymus H., Parker J., Chang K., Taron M., Rosell R., Moonsamy P., Dahlman K., Miller V.A., Costa C., et al. FAS and NF-kappaB signalling modulate dependence of lung cancers on mutant EGFR. Nature. 2011;471:523–526. doi: 10.1038/nature09870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sequist L.V., Waltman B.A., Dias-Santagata D., Digumarthy S., Turke A.B., Fidias P., Bergethon K., Shaw A.T., Gettinger S., Cosper A.K., et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci. Transl. Med. 2011;3:75ra26. doi: 10.1126/scitranslmed.3002003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Choi Y.L., Soda M., Yamashita Y., Ueno T., Takashima J., Nakajima T., Yatabe Y., Takeuchi K., Hamada T., Haruta H., et al. EML4-ALK mutations in lung cancer that confer resistance to ALK inhibitors. N. Engl. J. Med. 2010;363:1734–1739. doi: 10.1056/NEJMoa1007478. [DOI] [PubMed] [Google Scholar]
- 109.Doebele R.C., Pilling A.B., Aisner D.L., Kutateladze T.G., Le A.T., Weickhardt A.J., Kondo K.L., Linderman D.J., Heasley L.E., Franklin W.A., et al. Mechanisms of resistance to crizotinib in patients with ALK gene rearranged non-small cell lung cancer. Clin. Cancer Res. 2012;18:1472–1482. doi: 10.1158/1078-0432.CCR-11-2906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Engelman J.A., Zejnullahu K., Mitsudomi T., Song Y., Hyland C., Park J.O., Lindeman N., Gale C.M., Zhao X., Christensen J., et al. MET amplification leads to gefitinib resistance in lung cancer by activating ERBB3 signaling. Science. 2007;316:1039–1043. doi: 10.1126/science.1141478. [DOI] [PubMed] [Google Scholar]
- 111.Crystal A.S., Shaw A.T., Sequist L.V., Friboulet L., Niederst M.J., Lockerman E.L., Frias R.L., Gainor J.F., Amzallag A., Greninger P., et al. Patient-derived models of acquired resistance can identify effective drug combinations for cancer. Science. 2014;346:1480–1486. doi: 10.1126/science.1254721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Tricker E.M., Xu C., Uddin S., Capelletti M., Ercan D., Ogino A., Pratilas C.A., Rosen N., Gray N.S., Wong K.K., et al. Combined EGFR/MEK Inhibition Prevents the Emergence of Resistance in EGFR-Mutant Lung Cancer. Cancer Discov. 2015;5:960–971. doi: 10.1158/2159-8290.CD-15-0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Miyamoto S., Ikushima S., Ono R., Awano N., Kondo K., Furuhata Y., Fukumoto K., Kumasaka T. Transformation to small-cell lung cancer as a mechanism of acquired resistance to crizotinib and alectinib. Jpn. J. Clin. Oncol. 2016;46:170–173. doi: 10.1093/jjco/hyv173. [DOI] [PubMed] [Google Scholar]
- 114.Sharma S.V., Lee D.Y., Li B., Quinlan M.P., Takahashi F., Maheswaran S., McDermott U., Azizian N., Zou L., Fischbach M.A., et al. A chromatin-mediated reversible drug-tolerant state in cancer cell subpopulations. Cell. 2010;141:69–80. doi: 10.1016/j.cell.2010.02.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tartour E., Zitvogel L. Lung cancer: Potential targets for immunotherapy. Lancet Respir. Med. 2013;1:551–563. doi: 10.1016/S2213-2600(13)70159-0. [DOI] [PubMed] [Google Scholar]
- 116.Yoon D.H., Osborn M.J., Tolar J., Kim C.J. Incorporation of Immune Checkpoint Blockade into Chimeric Antigen Receptor T Cells (CAR-Ts): Combination or Built-In CAR-T. Int. J. Mol. Sci. 2018;19:340. doi: 10.3390/ijms19020340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Arce Vargas F., Furness A.J.S., Solomon I., Joshi K., Mekkaoui L., Lesko M.H., Miranda Rota E., Dahan R., Georgiou A., Sledzinska A., et al. Fc-Optimized Anti-CD25 Depletes Tumor-Infiltrating Regulatory T Cells and Synergizes with PD-1 Blockade to Eradicate Established Tumors. Immunity. 2017;46:577–586. doi: 10.1016/j.immuni.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.