Abstract
Purpose:
Radiation therapy (RT) is associated with high stress levels. The role of music therapy (MT) for patients receiving RT is not well described. This study evaluates the impact of MT on anxiety and distress during simulation in patients with newly diagnosed head and neck or breast cancer.
Methods and Materials:
This institutional review board–approved randomized trial of MT versus no MT at the time of simulation included the pre–State-Trait Anxiety Inventory (STAI-S Anxiety) questionnaire and Symptom Distress Thermometer (SDT). Patients randomized to MT received a consultation with a music therapist, during which music of the patients’ choice to be played during simulation was selected. The no-MT patients did not receive the MT consultation, nor did they hear prerecorded music during simulation. Subsequent to the simulation, all patients repeated the STAI-S Anxiety questionnaire and the SDT.
Results:
Of the 78 patients enrolled (39 in MT group and 39 in no-MT group), 38 had breast cancer and 40 had head and neck cancer. The male-female ratio was 27:51. The overall mean pre- and post-simulation STAI-S scores were 38.7 (range, 20–60) and 35.2 (range, 20–72), respectively. The overall mean pre- and post-simulation SDT scores were 3.2 (range, 0–10) and 2.5 (range, 0–10), respectively. The MT group had mean pre- and post-simulation STAI-S scores of 39.1 and 31.0, respectively (P<.0001), and the mean SDT scores before and after simulation were 3.2 and 1.7, respectively (P<.0001). The no-MT group’s mean pre- and post-simulation STAI-S scores were 38.3 and 39.5, respectively (P=.46), and the mean SDT scores were 3 and 3.2, respectively (P=.51).
Conclusions:
MT significantly lowered patient anxiety and distress during the simulation procedure on the basis of the STAI-S questionnaire and SDT. Incorporating culturally centered individualized MT may be an effective intervention to reduce stressors. Continued research defining the role of MT intervention in improving the patient experience by reducing anxiety is warranted.
Summary
Music therapy’s capacity to address anxiety in cancer patients has not been well described. This institutional review board–approved study evaluated a protocolized music therapy intervention’s impact on anxiety and distress experienced by patients undergoing computed tomography simulation. The intervention significantly reduced anxiety and distress in patients with newly diagnosed head and neck or breast cancer, with a greater effect in subgroups with higher baseline levels of anxiety and distress. Continued research on music therapy’s effects in radiation oncology is warranted.
Introduction
The prospect of radiation therapy (RT) strikes fear particularly in patients with newly diagnosed cancer (1). Simulation, the first step of treatment, sets the stage for how the rest of treatment may be perceived. Although there are studies that have focused on anxiety in RT (2, 3), those measuring stress in the first step of RT, simulation, are few. Arguably, simulation—as the patients’ first experience in radiation treatment—provides the baseline and precursor to their conception of how treatment will continue. Anxiety is common prior to treatment (2), with significant levels often undetected and undertreated (3). A review of RT studies indicated 10% to 20% of patients showed clinically significant levels of anxiety at the initiation of RT (3). At the time of simulation for RT, anxiety is commonly expressed as a result of immobilization techniques including restrictions of face masking and limited movement, coupled with isolation in an unfamiliar environment.
Music therapy (MT) has been shown to be effective in reducing anxiety in hospital contexts in clinical trials (4–6), including procedures apt to be perceived as threatening such as venipuncture (7), debridement (8), and oncology treatment regimens (9). Although there are a number of recent studies examining recorded music interventions during RT (10–13), there are limited data evaluating MT at the time of simulation and virtually no research examining the use of live MT during this critical period.
The purposes of this study were to identify patients’ baseline levels of anxiety and discomfort prior to simulation and to examine the impact of MT using a multifaceted protocol designed to address preidentified anxiety triggers. Personalized medicine, as it pertains to oncology, is rooted in the idea that treatment algorithms recognize the unique features of the patient and his or her cancer. This is usually focused on genomic and molecular aspects of the tumor and host. However, we should also consider the unique emotional aspects of each patient and his or her treatment experience. Little attention has been paid to interventions that help personalize the emotional aspects of the treatment journey. This study is an initial experience aimed at improving this aspect of oncology care.
Methods and Materials
This institutional review board–approved randomized trial included patients with breast or head and neck cancer randomly assigned to MT versus a standard procedure with no MT intervention. The standard procedure for all patients included verbal instructions on what to expect during simulation provided by the department’s radiation therapists, followed by the viewing of an instructional video created by the radiation oncology department. Only subjects fluent in the English language were enrolled. Subjects were randomized following a randomization schedule generated by a biostatistician, in the order in which they were accrued into the study. No other patient condition or variable was applied to randomization (Figure 1).
Fig. 1.
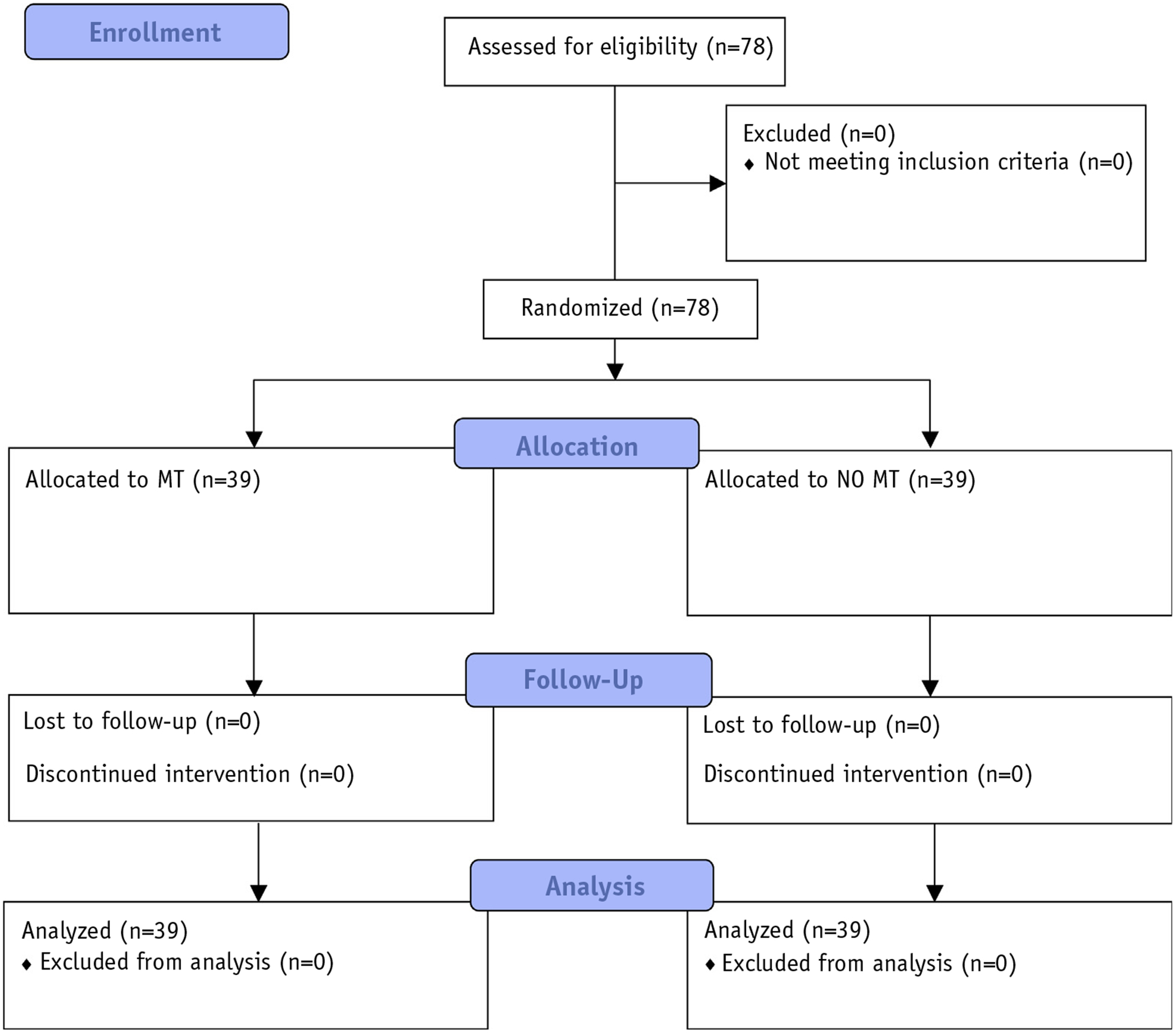
CONSORT (Consolidated Standards of Reporting Trials) diagram: patient flow through trial. Abbreviations: MT = music therapy intervention; NO MT = standard treatment alone.
MT protocol
Enrolled patients were oriented by a board-certified music therapist (MT-BC) in the simulation room before beginning the procedure. A brief assessment including an explanation of the details of the MT session ensued. The patient completed the pre–State-Trait Anxiety Inventory (STAI-S Anxiety) questionnaire with the research assistant reading the questions aloud and noting the patient’s answers, as well as a Likert-type scale, the Symptom Distress Thermometer (SDT), with the research assistant specifying that the questions on distress should be answered to describe how the patient felt in the moment, not over the past week. On the basis of the assessment, prerecorded music was prescribed for listening during the simulation procedure. The procedure for construction of the prescribed prerecorded music program involved the following: Patient-preferred music was identified and annotated, and construction of the program was carried out after the individual MT intervention. Patient-identified music was retrieved from an mp3 music file database kept on an Apple MacBook Pro (Apple, Cupertino, CA) organized in iTunes, version 12.1, containing >20,000 individual pieces spanning a broadly diverse collection of culture-centered music genres. Approximately 40 minutes of music was chosen based on each patient’s preferences and was analyzed following a “music characterization system” algorithm containing 12 musical elements and 4 nonmusical elements to identify and classify each selection numerically as having greater or lesser relaxation properties as opposed to activating properties (14). On the basis of the patient’s level of state anxiety and distress obtained during the assessment, individual pieces of music were connected in a sequence that moved progressively from pieces with higher levels of activating qualities to pieces with higher levels of relaxing qualities, based on the theories of musical entrainment (15) and music sedation (16) to increase comfort and orientation, reducing state anxiety.
On completing the questionnaire pertaining to music preference, the patient received an individual MT intervention that lasted approximately 20 minutes. The MT intervention was provided with live music played on a nylon string guitar in drop D tuning with simultaneous verbal processing. The live music played by the music therapist included an original easeful improvisational composition in D Mixolydian mode, played in such a way as to enhance entrainment with the patient and progressively deepen the relaxation response.1 The intervention is based on altered state induction to bring about a relaxed and focused state in which the patient is attuned to gentle suggestion that prompts focus while assimilating psychoeducational experience, which can be accessed and serve as a resource in both simulation and future RT treatment. Verbal direction was provided in the form of a pre-composed script2 that led the patient through 3 different psychoeducational experiences addressing 3 preidentified difficulties3 faced by patients during the simulation process. In addition to seeking a relaxation response, after the intervention, these 3 experiences were distinctly identified by the music therapist for the patient as being techniques that could be resourced during simulation to further reduce state anxiety if needed. The simulation procedure was carried out with the prescribed music lasting for the duration of the procedure time. The patient was then asked to complete the second part of the STAI-S, as well as the visual analog scale portion of the SDT.
Patients enrolled in the no-MT control group did not receive an MT intervention before simulation nor did they listen to prescribed or nonprescribed music during simulation. They received treatment as usual, which included verbal instructions of simulation and an instructional standard treatment video. These patients were offered MT interventions on their request during subsequent RT appointments.
Instruments
We used validated patient-reporting tools, that is, the STAI-S and SDT. The STAI-S is a self-report measure with 20 items to assess state anxiety, with each item evaluated on a 4-point Likert scale. A cutoff point of 39 or 40 has been suggested to detect clinically significant symptoms for the STAI-S Anxiety scale (17–19), and this was taken into consideration in further stratifying the data of 37 subjects who self-reported a State-Trait Anxiety Inventory (STAI) score ≥40.
The SDT is an 11-point scale with endpoints labeled “no distress” (0 points) and “extreme distress” (10 points) (20). Previous psychometric evaluation of the SDT indicated that a cutoff point ≥4 yielded the best sensitivity and specificity in distinguishing between individuals who were significantly distressed and those who were not, as judged by the established cutoff scores on the Hospital Anxiety and Depression Scale and Brief Symptom Inventory 18 (21). This was taken into consideration in further stratifying the data of 29 subjects identified as having SDT scores ≥4.
Statistical methods
Group differences in posttreatment STAI anxiety levels were used for comparing outcomes of each group. On the basis of previous research (22), we estimated a medium to large effect size with Cohen d = 0.66 and used a 2-sample t test to compare average posttreatment STAI anxiety scores for each of the patient groups (MT and no MT). In addition, to consider all variables and repeated measurements from the same patients, we used a repeated-measures analysis of variance to assess treatment effects on STAI and SDT. Between-subject effects and within-subject effects were estimated for the entire cohort and separate subsets of the data. Correlation between STAI and SDT was also assessed at both time points and by group with Spearman correlation coefficients. For stratified analyses, age was divided into 4 approximately equal groups: 26 to 48 years (n=18), 49 to 58 years (n=18), 59 to 64 years (n=22), and 65 to 77 years (n=20). Data were further stratified by staging and anatomic-site cohorts. Further examination of STAI data was conducted in a cohort of patients with pre-intervention scores ≥40, as well as for SDT scores ≥4 (Table 1). Data for subjects identifying an emotional etiology for distress were also examined.
Table 1.
Patient characteristics
| Entire cohort | MT | NoMT | |
|---|---|---|---|
| Characteristic | (N=78) | (n=39) | (n=39) |
| Age, median (range), y | 58.5 (26–77) | 58 (26–71) | 60 (35–77) |
| Age by group, n (%) | |||
| 26–48 y | 18 (23.1) | 9 (23.1) | 9 (23.1) |
| 49–58 y | 18 (23.1) | 10 (25.6) | 8 (20.5) |
| 59–64 y | 22 (28.2) | 13 (33.3) | 9 (23.1) |
| 65–77 y | 20 (25.6) | 7 (18.0) | 13 (33.3) |
| Gender, n (%) | |||
| Male | 27 (34.6) | 15 (38.5) | 12 (30.8) |
| Female | 51 (65.4) | 24 (61.5) | 27 (69.2) |
| Primary cancer, n (%) | |||
| Breast | 38 (48.7) | 16 (41.0) | 22 (56.4) |
| Head and neck | 40 (51.3) | 23 (59.0) | 17 (43.6) |
| Primary cancer by stage, n(%) | |||
| Breast | |||
| 0 | 4 (10.5) | 1 (6.3) | 3 (13.6) |
| I | 14 (36.8) | 8 (50.0) | 6 (27.3) |
| II | 10 (26.3) | 4 (25.0) | 6 (27.3) |
| III | 7 (18.4) | 2 (12.5) | 5 (22.7) |
| IV | 3 (7.9) | 1 (6.3) | 2 (9.1) |
| Head and neck | |||
| I | 10 (25.0) | 5 (21.7) | 5 (29.4) |
| II | 8 (20.0) | 8 (34.8) | 0 (0) |
| III | 9 (22.5) | 5 (21.7) | 4 (23.5) |
| IV | 13 (32.5) | 5 (21.7) | 8 (47.1) |
| Higher STAI | 39 (50.0) | 20 (51.3) | 19 (48.7) |
| score: ≥40, n (%) | |||
| Higher SDT | 29 (37.2) | 17 (43.6) | 12 (30.8) |
| score: ≥4, n (%) |
Abbreviations: MT = music therapy; SDT = Symptom Distress Thermometer; STAI = State-Trait Anxiety Inventory.
Results
Patient characteristics are shown in Table 1. We enrolled 78 patients with newly diagnosed breast cancer (n=38) or head and neck cancer (n=40) in the study. The median age was 58.5 years (range, 26–77 years). There were 27 male and 51 female patients. The participants were stratified into 4 approximately equal age groups in both study arms. They were also stratified by anatomic-site staging, and both MT and no-MT groups’ anatomic-site staging.
There was a positive correlation between STAI and SDT before simulation (Spearman ρ=0.44, P<.0001) and after simulation (Spearman ρ=0.67, P<.0001) (Table 2). The correlation remained when we examined each treatment group, that is, MT participants before simulation (Spearman ρ=0.39, P=.0141) and after simulation (Spearman ρ=0.67, P<.0001) and no-MT controls before simulation (Spearman ρ=0.50, P=.0011) and after simulation (Spearman ρ=0.58, P<.0001).
Table 2.
Mean change between preand post-simulation measurements
| MT | Control | P value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Analysis group | n | Mean change | SD | n | Mean change | SD | Between subjects | Within subjects | Group × time interaction |
| STAI | |||||||||
| Entire cohort | 39 | 8.2 | 8.7 | 39 | −1.2 | 10.1 | .1006 | .002 | <.0001 |
| Higher STAI (≥40) | 18 | 10.8 | 9.5 | 19 | 0.8 | 10.4 | .1068 | .0012 | .0043 |
| Emotional block (8–12) | 18 | 10.4 | 8.9 | 19 | −2.7 | 10.3 | .0154 | .0202 | .0002 |
| Age 26–48 y | 9 | 14.7 | 10 | 9 | 2.7 | 11.5 | .4839 | .0035 | .0309 |
| Age 49–58 y | 10 | 8.6 | 7.4 | 8 | −6 | 9.3 | .2162 | .5165 | .0018 |
| Age 59–64 y | 13 | 3.5 | 7.4 | 9 | 1.8 | 8.1 | .5834 | .1303 | .6177 |
| Age 65–77 y | 7 | 7.9 | 6.5 | 13 | −3 | 10.4 | .4803 | .2778 | .0222 |
| SDT | |||||||||
| Entire cohort | 39 | 1.6 | 1.7 | 39 | −0.3 | 2.4 | .1623 | .0064 | .0002 |
| Higher SDT (≥4) | 17 | 2.8 | 1.6 | 12 | 0.75 | 3.7 | .0732 | .0016 | .0548 |
| Emotional block (8–12) | 18 | 2.3 | 1.2 | 19 | −1.2 | 2.2 | .139 | .0631 | <.0001 |
| Age 26–48 y | 9 | 0.8 | 1.5 | 9 | 0.2 | 2.3 | .4868 | .2938 | .5549 |
| Age 49–58 y | 10 | 1.7 | 1.5 | 8 | −1.1 | 1.6 | .3308 | .4487 | .0015 |
| Age 59–64 y | 13 | 1.5 | 1.9 | 9 | −0.8 | 2.8 | .8082 | .4481 | .0288 |
| Age 65–77 y | 7 | 2.6 | 1.7 | 13 | 0.3 | 2.7 | .2639 | .0201 | .0603 |
Abbreviations: MT = music therapy; SDT = Symptom Distress Thermometer; STAI = State-Trait Anxiety Inventory.
Our findings showed a strong reduction in state anxiety levels for the MT cohort, with a mean post-simulation change effect of 8.2 units (P<.0001), while state anxiety actually increased in the no-MT cohort, with a mean change effect of −1.2 units. The increase in state anxiety for this cohort was not statistically significant (P=.46). The mean pre-simulation level for both groups (N=78) was 38.7; when stratified by the MT and no-MT cohorts, the levels were 39 and 38.3, respectively. These findings represent a statistically significant 21.03% reduction in anxiety in the subjects receiving MT.
In subset analyses, among the participants reporting a high pre-STAI total score (≥40, n=37), those in the MT arm (n=18; mean, 48.2) experienced a mean decrease of 10.8 while no-MT control group participants (n=19; mean, 47.2) experienced a mean decrease of 0.8 (Figure 2). Similar to the entire cohort, there was no statistical evidence of between-subject effects (P=.11), but again, there was evidence of within-subject effects (P=.001), as well as a group × time interaction (P=.004).
Fig. 2.
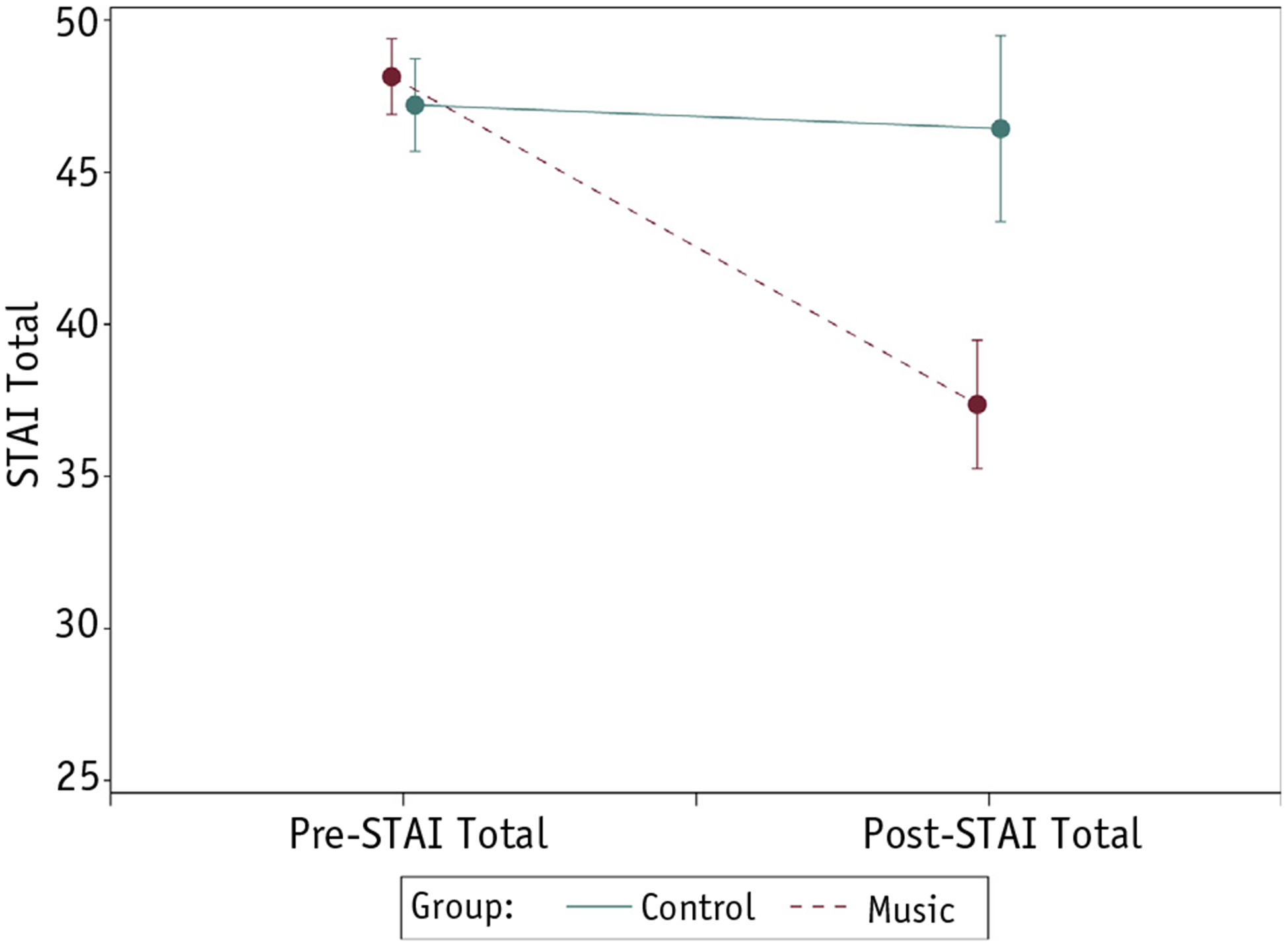
State-Trait Anxiety Inventory (STAI) scores for patients with high pre-STAI scores (≥40). Mean STAI scores with error bars (±1 standard error) are shown for the control group (solid line) and music therapy group (dashed line) at the pre– and post–music therapy time points for patients with high STAI scores.
Thirty-seven study participants indicated sources of distress related to emotional factors (emotional block 8–12). Among this cohort, 18 patients had been randomized to the MT group and 19 to the no-MT group. We observed a mean decrease in STAI score of 10.4 (SD, 8.9) and −2.7 (SD,10.3) for the MT group and no-MT control group, respectively (Figure 3). There was statistical evidence of betweensubject effects (P=.02), as well as within-subject effects (P=.02). A significant group × time interaction (P=.0002) was also observed. The mean decrease in SDT score for this subset was 2.3 (SD, 1.2) and −1.2 (SD, 2.2) for the MT group and no-MT control group, respectively (Figure 4). There was no statistical evidence of betweensubject effects (P=.14) or within-subject effects (P=.06). However, a significant group time interaction (P<.0001) was observed.
Fig. 3.
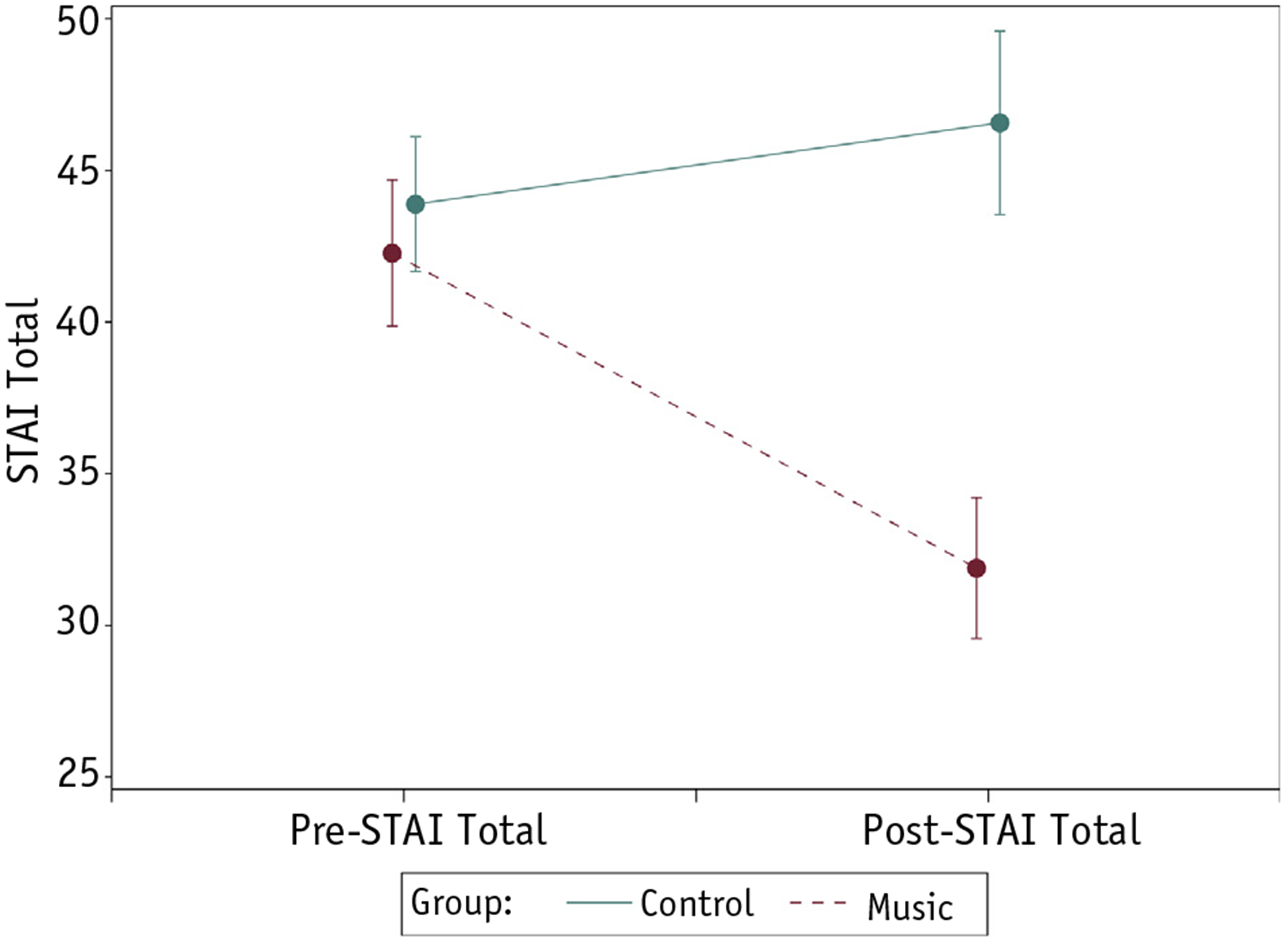
State-Trait Anxiety Inventory (STAI) scores for patients with distress related to high emotional factors. Mean STAI scores with error bars (±1 standard error) are shown for the control group (solid line) and music therapy group (dashed line) at the pre– and post–music therapy time points for patients with high pre-emotional distress (emotional block 8–12).
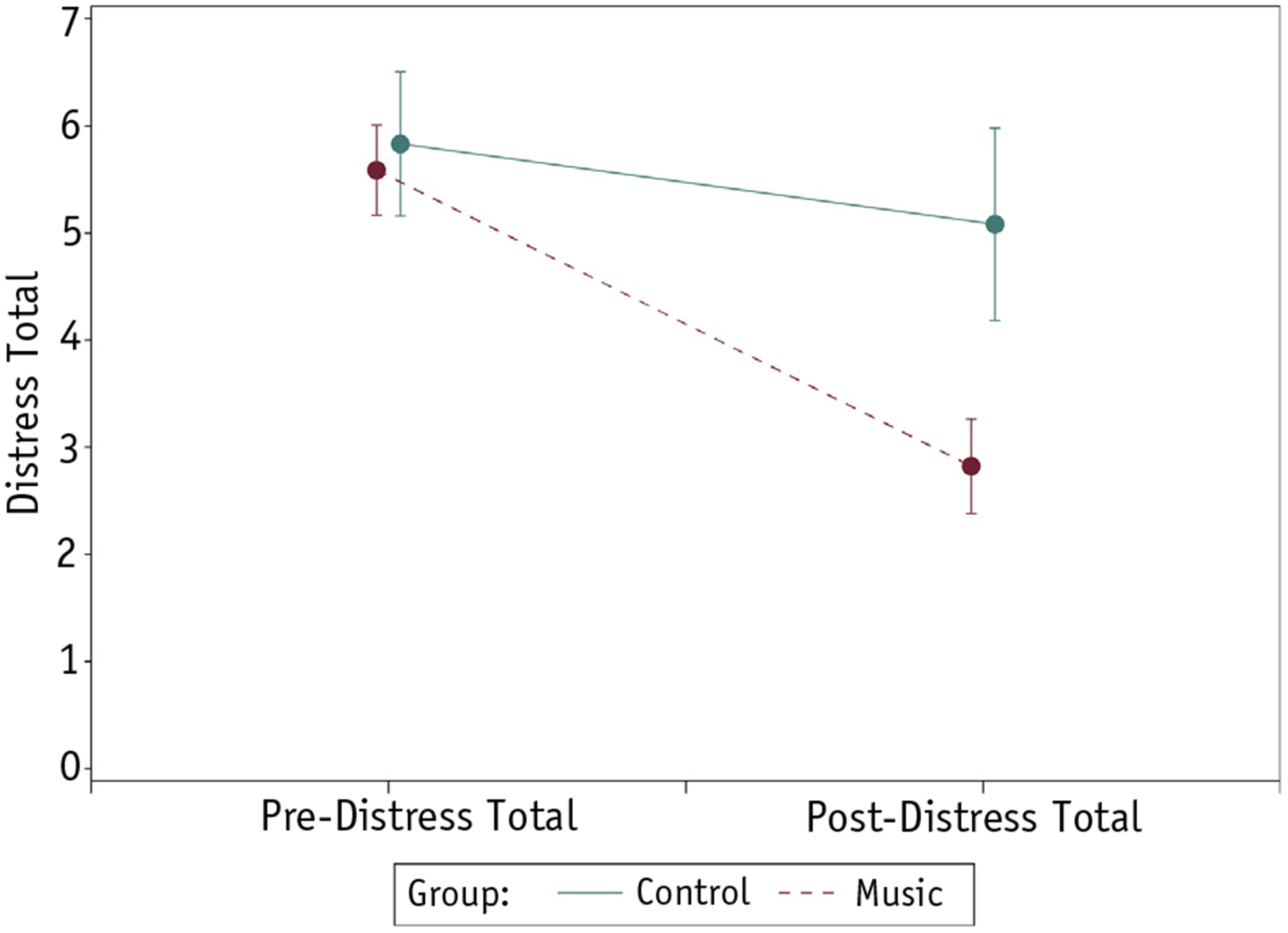
Fig. 4.
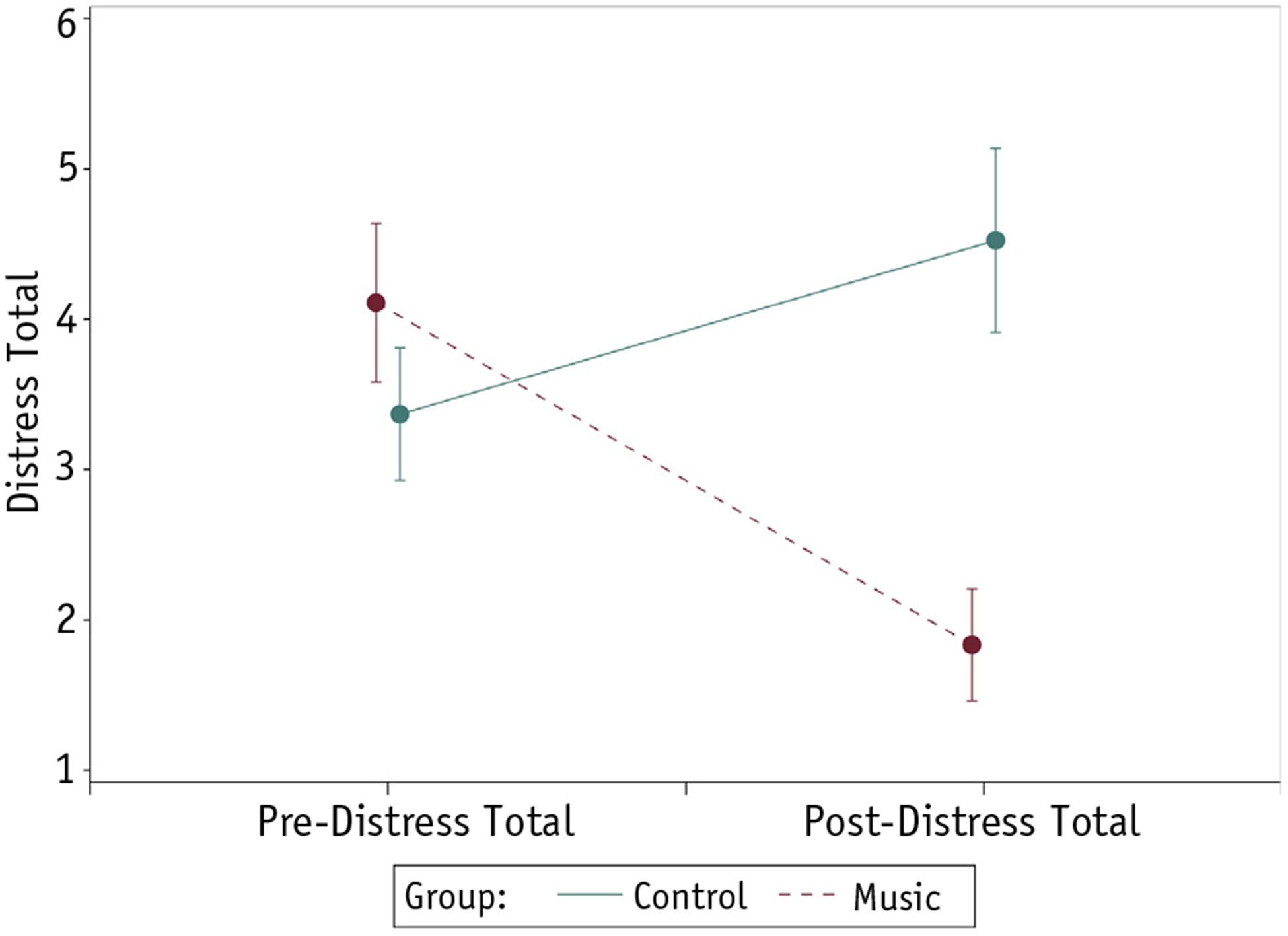
Mean distress scores with error bars (±1 standard error) for control group (solid line) and music therapy group (dashed line) at pre– and post–music therapy time points for subgroup of patients with high pre-simulation emotional distress (emotional block 8–12).
The data in our study show the entire cohort’s mean pre-simulation distress scores for both the MT and no-MT groups to be <4 (a generally accepted clinically significant cutoff level), at 3.1 and 3.5, respectively. The mean decrease in SDT score was 1.6 (SD, 1.7) and −0.3 (SD, 2.4) for the MT and control groups, respectively. There was no statistical evidence of between-subject effects (P=.16); however, there was evidence of within-subject effects (P=.006). A significant group × time interaction (P=.0002) was also observed. We identified 29 subjects as having distress scores ≥4; 12 belonged to the randomized no-MT group and 17 to the MT group. In the MT group, the mean pre-simulation score was 5.6 and the mean post-simulation score was 2.8 (P=.0016), which represents a 50% reduction in distress, bringing the level to a subsymptomal 2.8 (Figure 5). The no-MT group’s mean pre-simulation score of 5.8 and post-simulation score of 5.08 represent a negligible effect. Examining a subset of subjects receiving MT who identified emotional factors (block 8–12 on SDT) as the cause of distress, we found a 2.3-unit reduction in distress (interaction P<.0001).
Fig. 5.
Mean distress scores with error bars (±1 standard error) for control group (solid line) and music therapy group (dashed line) at pre– and post–music therapy time points for subgroup of patients with pre-simulation distress scores ≥4.
The age subsets yielded no statistically significant results with the exception of the group aged 26 to 48 years, whose MT arm (before simulation, 42.4; after simulation,27.8) experienced a mean reduction in anxiety of 14.6 units (P=.0035, interaction P=.0309). Because of the resulting small sample sizes, the subset analyses of participants stratified by anatomic-site staging provided exploratory results that may provide a basis for further study.
Discussion
This is the first clinical trial that measures a multilevel MT intervention using both live and prerecorded music to treat state anxiety and distress in patients undergoing simulation for RT. Our data strongly suggest that MT can significantly reduce both in this cohort. The prevalence of patient anxiety severe enough to cause session disruption indicates that initial interventions are well warranted and furthermore may have the potential to shift future perceived patient distress and enhance comfort factors (23). Decreasing emotional distress during simulation will likely result in successful completion of simulation with relative comfort, as well as a less traumatizing first encounter with the RT process. MT, provided by a board-certified music therapist, may offer a safe, cost-effective means of alleviating patient anxiety and distress. This study further validates its efficacy and impact and may serve as an incentive for treatment inclusion among radiation oncology treatment teams.
Optimal cancer care integrates both physical and psychosocial aspects of treatment to improve a patient’s sense of general well-being. Psychological support is warranted from the very beginning of physical and psychologically invasive treatments for cancer (24), particularly as an alarming number of patients undergoing RT for head and neck cancer show symptoms of emotional distress even before beginning treatment and this proportion increases significantly during RT (23).
The STAI-S is not a stand-alone diagnostic instrument and is meant to reflect the influence of whatever transient situational factors exist at the time of testing. Although the STAI manual itself does not indicate cutoff levels or significance of unit variation (25), a cutoff of 39 or 40 has been used in prior studies (26, 27).
We found a robust mean effect that represents a statistically significant reduction in anxiety in those subjects receiving MT. Further examination of the data identified subsets of patients in a highly fragile condition who showed a greater reduction of anxiety. This finding suggests that the MT intervention showed greater clinical efficacy for patients with higher levels of anxiety and that the reduction in the mean level in the MT group reached subclinical values after intervention.
Significantly, as with distress scores, the cohort that had identified emotional factors (block 8–12 on SDT) as the cause of distress also experienced greater anxiety, as well as a greater reduction. This finding suggests that people with distress related to emotional factors appear to also have higher anxiety levels prior to simulation and that the MT intervention was highly effective in reducing such anxiety.
Although mean pre-simulation distress scores for the entire cohort’s MT and no-MT groups are lower than symptomal levels, there was a significant reduction in distress. An important finding was that the subset of subjects with clinically significant distress scores ≥4 receiving pre-simulation MT showed a strong reduction in distress that resulted in subsymptomal distress levels.
It is important to recognize that “subclinical” levels of distress weigh heavily on patients. Subclinical emotional distress is common in cancer populations (28) and, although not pathologic, can cause “significant islands of life disruption” (29). Subclinical levels of distress associated with cancer symptoms had a profound impact on the quality of life of 243 cancer patients in a landmark study by Portenoy et al (30).
Any reduction in the distress experienced by cancer patients likely contributes to a better patient experience, especially when that experience is the first to be encountered in a radiation oncology unit. It may enhance patient perception of his or her remaining treatment experience, leading to better tolerance of the course of treatment and enhanced quality of life. The MT group experienced a robust mean reduction distress, and an important finding was that the subset of patients receiving MT who identified emotional factors as the cause of distress experienced an even greater reduction in distress after MT than the entire MT group. This larger effect suggests that MT in this context may be more effective in addressing the emotional domain of distress than logistic or purely physiological domains.
Conclusions
A multilevel protocolized MT intervention using biopsychosocial constructs was effective in reducing the level of presented ubiquitous state anxiety experienced by patients with breast or head and neck cancer undergoing simulation for RT. Our results suggest that the intervention was effective in reducing clinically significant levels of distress. Further studies examining the impact of such interventions on the patients’ experience during simulation and MT’s impact on the trajectory of their experience for the subsequent treatments delivered on a daily basis are warranted. Future studies should include further examination of the mechanisms that enhance our understanding of such clinical changes. Inclusion of a third arm consisting of attentive interactive discussion of the simulation procedure with nursing or medical staff may enhance findings. Researchers may also want to include more rigorous examination of time allotment in their control and/or treatment arms. RT units often grapple with waiting times and unpredictable scheduling concerns, which without question affect patients’ perception of treatment. Best practices in designing future studies should include team input in devising a plan of care inclusive of the ideal timing of the intervention as well as the development of scripted language that meets the unique needs of individual simulation units. This will provide a meaningful entry point for defining the most effective way MT interventions can be used.
Footnotes
Conflict of interest: none.
A recorded example of a section of the intervention is available by contacting the first author.
A copy of the scripted induction is available by contacting the first author.
The 3 difficulties faced by patients specific to the simulation experience were determined through consultation with oncology attending physicians, nurse practitioners, and radiation therapists, as well as through conversations with patients undergoing RT. Those chosen as the most salient aspects of the procedure were as follows: physical discomfort from maintaining a prolonged prone or supine position on an unpadded surface, sensitivity to experiencing claustrophobic events because of the inherent isolation and restraint during simulation, and the distressing somatic “body experience” related to state anxiety in relation to the burden of illness.
References
- 1.Peck A, Boland J. Emotional reactions to radiation treatment. Cancer 1977;40:180–184. [DOI] [PubMed] [Google Scholar]
- 2.Andersen BL, Karlsson JA, Anderson B, et al. Anxiety and cancer treatment: Response to stressful radiotherapy. Health Psychol 1984;3: 535–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stiegelis HE, Ranchor AV, Sanderman R. Psychological functioning in cancer patients treated with radiotherapy. Patient Educ Couns 2004; 52:131–141. [DOI] [PubMed] [Google Scholar]
- 4.Chlan L Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart Lung 1998;27:169–176. [DOI] [PubMed] [Google Scholar]
- 5.Horne-Thompson A, Grocke DJ. The effect of music therapy on anxiety in patients who are terminally ill. J Palliat Med 2008;11:582–590. [DOI] [PubMed] [Google Scholar]
- 6.Han L, Li JP, Sit JW, et al. Effects of music intervention on physiological stress response and anxiety level of mechanically ventilated patients in China: A randomized controlled trial. J Clin Nurs 2010;19: 978–987. [DOI] [PubMed] [Google Scholar]
- 7.Malone AB. The effects of live music on the distress of pediatric patients receiving intravenous starts, venipunctures, injections, and heel sticks. J Music Ther 1996;33:19–33. [Google Scholar]
- 8.Fratianne RB, Prensner JD, Huston MJ, et al. The effect of music-based imagery and musical alternate engagement on the burn debridement process. J Burn Care Rehabil 2001;22:47–53. [DOI] [PubMed] [Google Scholar]
- 9.Ferrer AJ. The effect of live music on decreasing anxiety in patients undergoing chemotherapy treatment. J Music Ther 2007;44: 242–255. [DOI] [PubMed] [Google Scholar]
- 10.Clark M, Isaacks-Downton G, Wells N, et al. Use of preferred music to reduce emotional distress and symptom activity during radiation therapy. J Music Ther 2006;43:247–265. [DOI] [PubMed] [Google Scholar]
- 11.O’Callaghan C, Sexton M, Wheeler G. Music therapy as a non-pharmacological anxiolytic for paediatric radiotherapy patients. Australas Radiol 2007;51:159–162. [DOI] [PubMed] [Google Scholar]
- 12.Smith M, Casey L, Johnson D, et al. Music as a therapeutic intervention for anxiety in patients receiving radiation therapy. Oncol Nurs Forum 2001;28:855–862. [PubMed] [Google Scholar]
- 13.Chen C, Tze-Fang W, Yi-Nuo S, et al. Fifteen-minute music intervention reduces pre-radiotherapy anxiety in oncology patients. Eur J Oncol Nurs 2013;17:436–441. [DOI] [PubMed] [Google Scholar]
- 14.Rossetti A Towards prescribing music in clinical contexts: More than words. Music Med 2014;6:70–77. [Google Scholar]
- 15.Bradt J The effects of music entrainment on postoperative pain perception in pediatric patients. Music Med 2010;2:150–157. [Google Scholar]
- 16.Loewy J, Hallan C, Friedman E, et al. Sleep/sedation in children undergoing EEG testing: A comparison of chloral hydrate and music therapy. Am J Electroneurodiagnostic Technol 2006;46:343–355. [PubMed] [Google Scholar]
- 17.Julian LJ. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res (Hoboken) 2011; 63(Suppl. 11):S467–S472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knight RG, Waal-Manning HJ, Spears GF. Some norms and reliability data for the State-Trait Anxiety Inventory and the Zung Self-Rating Depression scale. Br J Clin Psychol 1983;22(Pt. 4):245–249. [DOI] [PubMed] [Google Scholar]
- 19.Addolorato G, Ancona C, Capristo E, et al. State and trait anxiety in women affected by allergic and vasomotor rhinitis. J Psychosom Res 1999;46:283–289. [DOI] [PubMed] [Google Scholar]
- 20.National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw 2003;1:344–374. [DOI] [PubMed] [Google Scholar]
- 21.Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer 2005;103:1494–1502. [DOI] [PubMed] [Google Scholar]
- 22.Bradt J, Dileo C, Grocke D, et al. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst Rev 2011;CD006911. [DOI] [PubMed] [Google Scholar]
- 23.Clover K, Oultram S, Adams C, et al. Disruption to radiation therapy sessions due to anxiety among patients receiving radiation therapy to the head and neck area can be predicted using patient self-report measures. Psychooncology 2011;20:1334–1341. [DOI] [PubMed] [Google Scholar]
- 24.Greer JA, Pirl WF, Park ER, et al. Behavioral and psychological predictors of chemotherapy adherence in patients with advanced non-small cell lung cancer. J Psychosom Res 2008;65:549–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spielberger CD, Gorsuch RL, Lushene R, et al. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 26.Kvaal K, Macijauskiene J, Engedal K, et al. High prevalence of anxiety symptoms in hospitalized geriatric patients. Int J Geriatr Psychiatry 2001;16:690–693. [DOI] [PubMed] [Google Scholar]
- 27.Clements A The relationship between temperament and anxiety phase I in the development of a risk screening model to predict stress-related health problems. J Health Psychol 2010;15:515–525. [DOI] [PubMed] [Google Scholar]
- 28.Saleeba AK, Weitzner MA, Meyers CA. Subclinical psychological distress in long-term survivors of breast cancer. J Psychosoc Oncol 1996;14:83–93. [Google Scholar]
- 29.Tope DM, Ahles TA, Silberfarb PM. Psycho-oncology: Psychological well-being as one component of quality of life. Psychother Psychosom 1993;60:129–147. [DOI] [PubMed] [Google Scholar]
- 30.Portenoy RK, Thaler HT, Kornblith AB, et al. Symptom prevalence, characteristics and distress in a cancer population. Qual Life Res 1994; 3:183–189. [DOI] [PubMed] [Google Scholar]


