Abstract
Background:
Much remains unknown about the longitudinal health and well-being of individuals with intellectual disability (ID), thus new methods to identify those with ID within nationally representative population studies are critical for harnessing these data sets to generate new knowledge.
Objective:
Our objective was to describe the development of a new method for identifying individuals with ID within large, population-level studies not targeted on ID.
Methods:
We used a secondary analysis of the de-identified, restricted-use National Longitudinal Study of Adolescent to Adult Health (Add Health) database representing 20,745 adolescents to develop a method for identifying individuals who meet the criteria of ID. The three criteria of ID (intellectual functioning, adaptive functioning, and disability originating during the developmental period) were derived from the definitions of ID used by the American Psychiatric Association and the American Association on Intellectual and Developmental Disabilities. The ID Indicator was developed from the variables indicative of intellectual and adaptive functioning limitations included in the Add Health database from Waves 1–3.
Results:
This method identified 441 adolescents who met criteria of ID and had sampling weights. At Wave 1, the mean age of this subsample of adolescents with ID was 16.1 years (range: 12, 21). About half of the adolescents were male (53.1%) and from minority racial groups. Their parents were predominately female (97.6%), married (53.2%), had less than a high school education (47.4%), and their median age was 41.62 years. The adolescents’ mean maximum abridged Peabody Picture Vocabulary Test standardized score was 69.6 (range: 7, 89), and all demonstrated at least one adaptive functioning limitation.
Discussion:
This study demonstrates the development of a data-driven method to identify individuals with ID using commonly available data elements in nationally representative population datasets. By utilizing this method, researchers can leverage existing rich data sets holding potential for answering research questions, guiding policy, and informing interventions to improve the health of the ID population.
Keywords: intellectual disability, adolescents, young adults
Health disparities researchers such as nurse scientists have a mandate to understand the deep structures underlying preventable differences in the burden of health conditions. Significant health disparities exist globally among the estimated 1% of individuals with intellectual disability (ID) (Krahn & Fox, 2014; Maulik, et al., 2011). Advances in healthcare within the United States (US) have improved survival rates for those with ID who previously may have died during childhood (Coppus, 2013); however, life expectancy remains 20 years shorter than that of the general population (Lauer & McCallion, 2015). Lower access to quality health care perpetuates health disparities (Ervin et al., 2014; Krahn & Fox, 2014) and inferior health outcomes, including higher hospitalization rates and acute care service use (Acharya et al., 2017; Anderson et al., 2013; Krahn & Fox, 2014). These trends are prominent among racial and ethnic minorities (Emerson, 2012; Mandell et al., 2009; Scott & Havercamp, 2014).
Population level study of health trajectories of individuals with ID can illuminate health needs and inform interventions. The Life Course Health Development (LCHD) framework (Halfon & Forrest, 2018), which explains how health trajectories develop over the life course, guided the conceptualization of this study. Reducing health disparities must move beyond providing better access and resources to the underserved (Halfon & Hochstein, 2002) to understanding their source. The LCHD framework focuses on the psychosocial factors contributing to disparities that are present early in life and grow synergistically across the life course. Longitudinal data sets rich in the mental and physical health, genetic, socioeconomic, and environmental data (Halfon et al., 2014) are an effective means to study life course development. The use of nationally representative longitudinal data sets is an important strategy to understand the health trajectories of individuals with ID as they often participate in these studies, but their unique experiences are left unstudied. A key barrier to knowledge development in this field is the difficulty of identifying individuals with ID within population studies not focused on disability.
The terminology used to communicate the diagnosis of ID has evolved from prior stigmatizing terms including imbecility, idiocy, mental deficiency, feeble-mindedness, and mental retardation (American Association on Intellectual and Developmental Disabilities, 2007; Schalock et al., 2010). In 2013, the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM-5) replaced mental retardation with “intellectual disability” (American Psychiatric Association, 2013), but the stigmatization, lack of recognition, and undertreatment experienced by those with ID persists and contributes to their relative invisibility within nationally representative population studies. This stigma (O’Hara, 2003; Zuckerman et al., 2014) contributes to the reticence to disclose ID (CDC, 2009; Emerson, 2011). Minority children are less likely to be diagnosed with ID and provided with special education services (Morgan et al., 2017), which contributes to educational and developmental disparities. Additionally, 85% of those with ID have mild ID (King, 2009) and are a “hidden majority” (Emerson, 2011), increasing their risk of remaining undiagnosed and without formal support.
Studying populations with ID within large, diverse, longitudinal data sets increases generalizability as large samples are more likely to include minority groups (e.g., racial/ethnic minorities), allowing for testing of within-group differences. Longitudinal designs also allow tracking of patterns of health of the ID population over time. Therefore, studying ID within longitudinal population studies allows the study of their life course development, including those who may not have had access to evaluation services and supports, and the promise of adequate sample sizes to look at within-group differences. Yet difficulty identifying those with ID have limited our ability to leverage population studies (Fox et al., 2015; Krahn et al., 2010), and understand how their health trajectories compare to those without ID. Health disparities are likely to continue in the absence of our ability to identify those with ID in population studies.
The identification of individuals with ID within nationally representative population studies is often difficult because of a lack of a widely agreed upon operational definition of ID (Fox et al., 2015). According to the leading definitions of ID by the American Psychiatric Association (APA, 2013) and the American Association on Intellectual and Developmental Disabilities (AAIDD) (Schalock et al., 2010), a conceptually valid measure of ID should include both required criteria of cognitive and adaptive function. In clinical practice, ID is diagnosed through standardized testing of both intelligence (e.g., Stanford-Binet Intelligence Scales) and the ability to perform daily activities known as adaptive functioning (e.g., Vineland Adaptive Behavior Scale). Yet researchers often use measures of cognitive function as the sole attribute to identify those with ID (e.g., Cheng & Udry, 2005; Halpern et al., 2000; Haydon et al., 2011; Kahn & Halpern, 2016). This unidimensional conceptualization is problematic as it has been shown to both under- and over-estimate the number of individuals with ID in large populations (Schalock et al., 2010; Haydon et al., 2011; Kahn & Halpern, 2016). The objective of this paper is to describe a new method for identifying individuals with ID within large, population-level studies by employing an operational definition constructed with commonly available data elements. We explicate this method by identifying individuals who meet criteria for ID (intellectual functioning, adaptive functioning, and disability originating during developmental period) within The National Longitudinal Study of Adolescent to Adult Health (Add Health), a large, nationally representative database.
Utilizing the Add Health Database to Study Intellectual Disability
Add Health is a well-known longitudinal database for studying developmental and health trajectories of adolescents who attended grades 7–12 in the 1994–1995 school year. The sample of 20,745 adolescents, collected over 5 waves (1994–2018), was obtained through a complex, stratified school-based sampling design (Chen, 2018). Wave 1 data were collected on 12–19 year olds using a combination of in-school interview, in-home interview, and a parent questionnaire. Subsequent waves continued with in-home interviews and added schooling, education, biomarker, and environmental data. The Add Health database provides a unique opportunity to study health trajectories of individuals with ID within context, and to make comparisons to those without ID as diverse subgroups, including individuals with physical disabilities who were oversampled (Chen, 2018).
The Add Health database contains no single variable to identify an individual with ID or capture both intellectual and adaptive limitations consistent with ID. In Wave 1, the variable “parent report of ID” asks parents to report if their child is “mentally retarded” (now obsolete language); however, not all individuals had a parent questionnaire. For those who did, accuracy of this variable hinges on access to diagnostic services in the child’s school or medical setting, parental knowledge of “mental retardation” and willingness to disclose it. Given the well-known underreporting of ID and the risk of unrecognized ID (Schalock et al., 2010; Emerson, 2011; Krahn et al., 2010), parental reporting is an insufficient single indicator.
Past studies of the ID population using the Add Health data set have used a single proxy variable, the “Add Health Picture Vocabulary Test standardized score,” an abridged Peabody Picture Vocabulary Test (aPPVT) (e.g., Cheng & Udry, 2005; Halpern et al., 2000; Haydon et al., 2011; Queiros et al., 2015). In our early exploration of this data set to study health trajectories of individuals with ID, we considered utilizing the aPPVT standardized score ≤ 79 to identify individuals with ID. Importantly, the use of this variable resulted in an unanticipated and implausible number of individuals from racial and ethnic minority groups. Similarly, Kahn & Halpern (2016) used an aPPVT ≤85 to study those with “low cognitive ability” within this data set, which resulted in a sample of 33.6% (n=742) Non-Hispanic Black, 30.2% (n=691) Hispanic, and 27.9% Non-Hispanic White (n=410). Results such as these are likely attributed to the unidimensional nature of aPPVT representing only one component of intellectual functioning, and likely reflects differences in learning experiences. Using this one indicator, aPPVT, resulted in a sample that is over-representative of racial and ethnic minority groups, raising questions about its validity as a proxy for ID. Thus, a new method of identifying individuals with ID was needed that was inclusive of both intellectual and adaptive functioning, to lower the likelihood of misclassification.
METHODS
We conceptualized ID as including disabilities in intellectual functioning, adaptive functioning, and disability present during adolescence. Add Health contains distinct variables that measure intellectual and adaptive functioning. Most of these variables were measured in Wave 1, when participants were adolescents; however, because some variables come from Wave 2 (13–19 years old), and Wave 3 (18–26 years old), we refer to the study participants as adolescents and young adults (AYAs). All AYAs within the database with an aPPVT standardized score of ≤ 79 (intellectual functioning) obtained during Wave 1 and/or Wave 3 were included. Additionally, those missing Wave 1 sampling weights were excluded as sampling weights, calculated as the inverse of the probability of each individuals selection, are required to ensure nationally representative estimates (Chen, 2018).
Variables and Procedures
We reviewed the variables collected within each Wave of Add Health data to identify those capturing a component of ID conceptually represented by the APA (2013) and AAIDD (Schalock et al., 2010) definitions. Table 1 demonstrates the similarities and differences between APA and AIDD definitions and their specific criteria. The individual variables were then examined for face validity. We sought to develop an indicator of ID that included variables of intellectual functioning (Criterion A) and adaptive functioning (Criterion B) during Wave 1 (12–18 years old) and Wave 2 (13–19 years old) to demonstrate that disability was present during the developmental period of adolescence before age 18 (Criterion C). Table 2 demonstrates the Add Health ID Indicator criteria and method used to identify those participants with functioning consistent with ID.
Table 1.
Intellectual Disability (ID) Criteria
| ID Criteria | Definitions | |
|---|---|---|
| APAa | AAIDDb | |
| Criterion A: Intellectual Functioning Limitation | “Deficits in intellectual functions such as reasoning, problem solving, planning, abstract thinking, judgement, academic learning, and learning from experience, confirmed by both clinical assessment and individualized, standardized intelligence testing” (test score ≤ 75) (p. 33). | “Significant limitations in intellectual functioning” (p. 27) including learning, reasoning, problem solving, etc. |
| IQ standardized test score cutoff approximately two standard deviations from population mean | ||
| Criterion B: Adaptive Functioning Limitation | “Deficits in adaptive functioning that result in failure to meet developmental and socio-cultural standards for personal independence and social responsibility. Without ongoing support, the adaptive deficits limit functioning in one or more activities of daily life, such as communication, social participation, and independent living, across multiple environments, such as home, school, work, and community” (p.33). | “Significant limitations in adaptive functioning” (p. 27). |
| Composed of limitations in: | ||
| • conceptual skills | ||
| • social skills | ||
| • practical skills | ||
| Standardized score of adaptive behavior approximately two standard deviations below mean on one type of adaptive skill or overall score of all three skills | ||
| Criterion C: Disability during developmental period | Onset of both intellectual and adaptive deficits during the developmental period of childhood or adolescence | Onset before age 18 |
APA (American Psychiatric Association) (American Psychiatric Association, 2013)
AAIDD (American Association on Intellectual and Developmental Disabilities) (Schalock et al., 2010)
Table 2.
Add Health Intellectual Disability (ID) Criteria and Method
| ID Criteria | Add Health Measures | Process |
|---|---|---|
| Criterion A: Intellectual Functioning Limitation | • Abridged Peabody Picture Vocabulary Test (aPPVT) Standardized Score ≤79 |
Definition • aPPVT ≤ 79 at Wave 1 and/or Wave 3 Procedures • aPPVT ≤ 79 at Wave 1 ○ If aPPVT also assessed at Wave 3, then Wave 3 aPPVT must be ≤ 89 ○ If aPPVT missing at Wave 1, then aPPVT must be ≤ 79 at Wave 3 |
| Criterion B: Adaptive Functioning Limitation | • Requires assistance with activities of daily life (eating, bathing, dressing, toileting, shopping) • Physical, learning, or emotional condition (present for > 1 year) causing limitations/difficulty with (a) attending school/work, (b) doing household chores, shopping, errands, (c) doing strenuous activities, (d) personal care • Perception of Disability (parent report): (a) parent considers child disabled, (b) parent thinks others consider child disabled • Perception of Disability (adolescent report): (a) adolescent considers self disabled, (b) adolescent thinks others consider them disabled • “Mental Retardation” • Learning Disability • Condition physical, learning, or emotional in nature • Receipt of special education or special education diploma |
Definition • Presence of 1 or more adaptive functioning limitations, reported by the parent, adolescent, or school transcripts, among those who met Criterion A Procedures • 3 categories of adaptive functioning were assessed. Each component of the category was evaluated and given a score of one when an adaptive limitation was identified. A total score was determined for each category. Categories and subcategories: ○ Activities of Daily Living (ADLs) • Parent report of AYAs ADL limitations (Wave 1) • AYA report of AYAs ADL limitations (Wave 1 & 2) ○ Perception/recognition of AYA’s Disability • Parent perception/recognition that AYA has: • disability (Wave 1) • “mental retardation” (Wave 1) • Learning disability (Wave 1) • AYA perception/recognition: • AYA has disability (Wave 1 & 2) • Condition physical, learning, or emotional in nature (Wave 2) ○ Special Education • Parent report of AYA receiving special education in last 12 months (Wave 1) • Graduated with special education diploma (Wave 3) |
| Criterion C: Disability during developmental period | • The adolescent meeting Criteria A & B during Wave 1 & Wave 2 also meets Criterion C as this demonstrates they had disability present during their developmental period |
Intellectual Functioning.
A critical component of intellectual functioning is verbal comprehension, defined as the ability to understand spoken language (APA, 2013). Intellectual functioning limitation (Criterion A) for this study was represented by the aPPVT standardized score. The aPPVT, a 87-item abridged version of the Peabody Picture Vocabulary Test-Revised (Carolina Population Center, 1998), has been shown to be moderately correlated with intelligence measures, including the Wechsler Intelligence Scale for Children and Stanford-Binet Intelligence Scale (Becker, 2003; Dunn & Dunn, 1981; Wechler, 2004) and highly correlated (0.96) with the entire PPVT instrument (Halpern et al., 2000). An age-standardized score of 90–109 is classified as average, 80–89 as low average, 70–79 as borderline or very low, and 69 and below as extremely low. Given that the aPPVT does not require reading comprehension skills, it has been identified as a particularly useful cognitive ability measure for those at the lower end of the distribution (Cheng & Udry, 2005).
The aPPVT was assessed during in-home interviews at Wave 1 and repeated at Wave 3. The measurement error for the aPPVT is not known; however, full psychometric tests of intelligence generally use a score of 75 as the cut off (APA, 2013). Participants with Wave 1 aPPVT with a standardized score of ≤ 79 (identified as borderline or very low range) were considered for our ID subsample. If they also had a Wave 3 aPPVT, it must have been ≤ 89 (below average) to demonstrate consistent limitations in intellectual functioning. If a participant did not have an aPPVT completed in Wave 1 but had a Wave 3 aPPVT ≤ 79, they were also further considered for our ID subsample through analysis of their adaptive functioning.
Adaptive Functioning.
Adaptive functioning is composed of three domains: conceptual (e.g., reading, math, reasoning, language problem solving, memory); social (e.g., communication skills, social judgment, empathy); and practical (e.g., self-management across settings such as personal care, work responsibilities) (APA, 2013). To fulfill the diagnostic criteria for ID, an individual must demonstrate a deficit in at least one of these three domains at home, school, work, or in the community, and this deficit must be directly related to their intellectual functioning limitation (Criterion A) (APA, 2013). The importance of this relationship between adaptive and intellectual functioning cannot be overstated because physical disability and ID commonly co-occur (APA, 2013). For example, 45% of individuals with a physical disability of cerebral palsy also have ID, but the majority do not (Reid et al., 2018). Because physical disability does commonly co-occur, we recognized the importance of not excluding individuals based on physical disability and of identifying questions that appraise three domains of adaptive functioning among those individuals who have demonstrated Criterion A. We conducted additional analyses to determine how many individuals met criteria of physical disability, met criteria for adaptive functioning limitations based on physical disability alone, or had additional features of Criterion B captured by this ID Indicator.
Adaptive functioning was assessed by the presence of one or more adaptive functioning limitations among individuals who meet Criterion A. Adaptive functioning limitation (Criterion B) was measured by 24 components across three categories: (a) activities of daily living (b) perception/recognition of AYA disability, and (c) special education. Each component was evaluated and given a score of one when an adaptive limitation was identified. We developed a total of seven Criterion B components including parent- and AYA-reported adaptive functioning limitations Wave 1, AYA-reported adaptive functioning limitations Wave 2, parent- and AYA-reported perception of disability, history of receiving special education, and graduation with special education diploma (see Table 3).
Table 3.
Characteristics of ID Criterion Among Adolescents with ID (N = 441)
| ID Criterion | Unweighted | Weighted | ||
|---|---|---|---|---|
| N | f | % | SE | |
| Intellectual Functioning Limitations | ||||
| • Maximum aPPVT (Wave 1 or Wave 3) | ||||
| ○ 0 – 39 | 441 | 22 | 6.5% | 2.19 |
| ○ 40 – 59 | 441 | 50 | 14.0% | 3.59 |
| ○ 60 – 69 | 441 | 78 | 19.7% | 2.94 |
| ○ 70 – 79 | 441 | 229 | 46.5% | 5.55 |
| ○ 80 – 89 | 441 | 62 | 13.2% | 3.75 |
| • aPPVT Wave 1 | ||||
| ○ 0 – 39 | 424 | 21 | 6.9% | 2.25 |
| ○ 40 – 59 | 424 | 55 | 15.9% | 3.58 |
| ○ 60 – 69 | 424 | 106 | 25.9% | 2.12 |
| ○ 70 – 79 | 424 | 242 | 51.3% | 6.71 |
| • aPPVT Wave 3 | ||||
| ○ 0 – 39 | 252 | 15 | 3.9% | 2.56 |
| ○ 40 – 59 | 252 | 23 | 13.1% | 3.48 |
| ○ 60 – 69 | 252 | 41 | 14.0% | 3.24 |
| ○ 70 – 79 | 252 | 111 | 42.0% | 5.17 |
| ○ 80 – 89 | 252 | 62 | 27.0% | 5.09 |
| Adaptive Functioning Limitations | ||||
| • Requires assistance (Wave 1 parent report) | ||||
| ○ Eating | 423 | 3 | 1.7% | 1.43 |
| ○ Bathing | 423 | 6 | 2.8% | 1.97 |
| ○ Dressing | 423 | 5 | 2.4% | 2.06 |
| ○ Toileting | 423 | 3 | 1.7% | 1.43 |
| • Requires assistance (Wave 1 AYA report) | ||||
| ○ Eating | 441 | 4 | 1.8% | 1.39 |
| ○ Bathing | 441 | 5 | 2.6% | 1.92 |
| ○ Dressing | 441 | 4 | 1.9% | 1.39 |
| ○ Toileting | 441 | 5 | 2.2% | 1.30 |
| ○ Shopping | 441 | 9 | 3.7% | 2.32 |
| • Physical, learning, or emotional condition (present for > 1 year) causing (Wave 2 AYA report) | ||||
| ○ Limitations attending school or work | 319 | 104 | 33.6% | 7.07 |
| ○ Difficulty doing chores, shopping, or errands | 318 | 42 | 15.2% | 6.26 |
| ○ Limitations in doing strenuous activities | 320 | 60 | 19.9% | 4.12 |
| ○ Difficulty with personal care (bathing, dressing, eating, toileting) | 320 | 20 | 9.1% | 3.66 |
| • “Mental Retardation” (Wave 1 Parent Report) | 417 | 104 | 38.3% | 13.62 |
| • Learning Disability (Wave 1 Parent Report) | 414 | 310 | 80.5% | 4.85 |
| • Perception of Disability (Wave 1 Parent & AYA Report) | ||||
| ○ Parent considers child to be disabled | 423 | 28 | 8.7% | 1.59 |
| ○ Parent thinks others consider child disabled | 420 | 23 | 6.8% | 1.77 |
| ○ Adolescent considers self to be disabled | 440 | 13 | 3.9% | 2.22 |
| ○ Adolescent thinks others consider them disabled | 440 | 13 | 3.6% | 1.88 |
| • Condition is (Wave 2 AYA Report) | ||||
| ○ Physical | 316 | 60 | 20.4% | 4.93 |
| ○ Learning | 316 | 62 | 20.6% | 3.72 |
| ○ Emotional | 316 | 27 | 9.9% | 4.65 |
| • Received special education in the last 12 months (Wave 1 Parent Report) | 418 | 293 | 79.0% | 5.91 |
| • Graduated with Special Education Diploma (Wave 3 School Transcripts) | 418 | 4 | 4.9% | 3.24 |
aPPVT = Abridged Peabody Picture Vocabulary Test Standardized Score; N = unweighted ID sample; f = unweighted frequencies; weighted percent (%) after applying Wave 1 sampling weights, stratification, and cluster variables; SE = weighted standard error of the percent (%).
Parent (Wave 1) and AYA (Wave 1 & 2) reported Activities of Daily Living (ADL) were used. The in-home parent questionnaire asked parents if their child had difficulty using their hands and arms, or feet and legs. If their answers to both were “no,” skip logic was used, and further disability questions were not asked. If the parent responded yes to either, they were asked if the condition required their child to need help when eating, bathing, dressing, getting on or off the toilet. Similarly, AYAs who indicated a physical/functional limitation (difficulty using upper or lower extremity, heart problem, asthma or breathing difficulty, or adaptive equipment for ambulation) at Wave 1 were asked if their condition required help from another person when eating, when bathing, when dressing, when getting on or off the toilet, or when shopping. At Wave 2, all AYAs were asked if because of a physical, learning, or emotional condition that had lasted for at least a year, they had (a) any limitations attending school or in your ability to do regular work (b) difficulty in doing regular household chores, shopping, or errands (c) limitations in doing strenuous activities such as running, swimming, or other sports and (d) difficulty with personal care or hygiene, namely bathing, dressing, eating, or using the toilet. Each ADL component was coded 0 = no and 1 = yes at both Wave 1 and 2.
In addition to ADLs and questions about extremity function, parents and AYAs were asked about physical conditions. In Wave 1, parents were asked “Are his/her difficulties caused by a physical condition?” while AYAs were asked “Do you consider yourself to have a disability?” and “Do you think other people consider you to have a disability?” In wave 2, AYAs were asked “Is your condition physical, learning, or emotional in nature?”
To identify individuals not meeting developmental and socio-cultural standards, defined as those not meeting social responsibility and personal independence standards expected of individuals of similar age and socio-cultural background (APA, 2013), we identified variables that represent features consistent with ID. These variables include the presence of disability as evidenced by recognized ID (referred to as mental retardation in Wave 1 (1994–95)), a learning disability, and a perception of a disability according to their parents, others around them, and/or themselves. Seven questions asked parents and AYAs about their perception/recognition of the AYA’s disability category. Four questions were asked during the in-home parent questionnaire (coded 0=no and 1=yes) “Is (he/she) mentally retarded?” and “Does (he/she) have a specific learning disability, such as difficulties with attention, dyslexia, or other reading, spelling, writing, or math disability?” Parents who indicated that their child had difficulty using their upper and/or lower extremities were also asked “Do you consider [NAME] to have a disability?” and “Would other people consider [him/her] to have a disability?” We used parent report of child having learning disability as a feature of adaptive functioning limitation because it taps the conceptual and practical domains of the AAIDD and DSM criteria. It is important to note that a learning disability (e.g., dyslexia) can be present without an ID, but for this sample all AYAs demonstrated at least one low aPPVT score (≤ 79) and did not have an average or higher aPPVT at either of their aPPVT evaluations. The AYAs’ perception/recognition of their disability was assessed through three questions (coded 0=no and 1=yes): “Do you consider yourself to have a disability?” (Wave 1) and “Do you think other people consider you to have a disability?” (Wave 1); and “Is your condition physical, learning, or emotional in nature?” (Wave 2).
Lastly, we used the receipt of special education, indicating the need for support in the school setting, to assess the presence of ID. Special education is a broad umbrella term; it includes education directed to those with ID, but also to those with other impairments (e.g., vision or hearing), emotional disabilities, and specific learning disabilities (Butrymowicz & Mader, 2017). Special education was assessed by asking parents if their child had received any type of special education in the past 12 months (coded 0=no and 1=yes), and the AYAs’ high school exit status from their high school transcript. AYAs receiving special education were given one point toward adaptive functioning limitation. Those who received a special education diploma did receive an additional point for adaptive functioning limitation as it further demonstrated their difficulty in practical and conceptual domains.
Disability During the Developmental Period of Adolescence.
We identified those meeting Criteria A & B during Wave 1 and 2 when the adolescents were 12–19 years of age to demonstrate that their disability was present during the developmental period of adolescence (Criterion C). Each adolescent of this ID subsample demonstrated intellectual and adaptive functioning limitations.
Analytic Strategy
To summarize, we created an operational definition of ID that included limitations in intellectual and adaptive functioning and aligned conceptually with the DSM-5 and AAIDD ID criteria. Add Health variables that tapped our criteria for ID, limitations in intellectual and adaptive functioning originating in childhood or adolescence, were used to describe the Add Health subsample with ID, and the individual variables that composed the Add Health ID Indicator. We applied variance adjustments and the Wave 1 cross-sectional sampling weights constructed by Add Health investigators to account for the complex survey design, non-random sampling, and oversampling of certain subgroups (Chen, 2018). Analyses were conducted using the sampling weights, stratification (region of the country) and cluster (school) variables which allowed us to produce nationally representative inferences from the Add Health 1994–95 sample.
RESULTS
Process to Obtain Final Sample
Our consort flow diagram (see Figure 1) demonstrates the progression from the total Add Health sample to the final Add Health ID subsample (N = 441), including how participants exited. Based on this process, adolescents met Criterion A in one of four ways: (a) Wave 1 aPPVT missing and Wave 3 aPPVT ≤ 79 (n = 76), ( b) Wave 1 aPPVT ≤ 79 and Wave 3 aPPVT missing (n = 668), (c) Wave 1 and Wave 3 aPPVT ≤ 79 (n = 565), (d) Wave 1 aPPVT ≤ 79 and Wave 3 aPPVT 80 – 89 (n = 258). After meeting Criterion A, the remaining 1,567 AYAs were evaluated for Criterion B. Based on the Criterion B 1,048 adolescents exited who lacked a single adaptive functioning limitation. There were 519 AYAs who met Criterion A and B, and therefore C; however, given our aim to make nationally representative inferences, adolescents without sampling weights (n=78) (i.e., those not part of the original sampling frame who were enrolled in the field (e.g., twin)) were exited. This process resulted in a final sample of 441.
Figure 1.
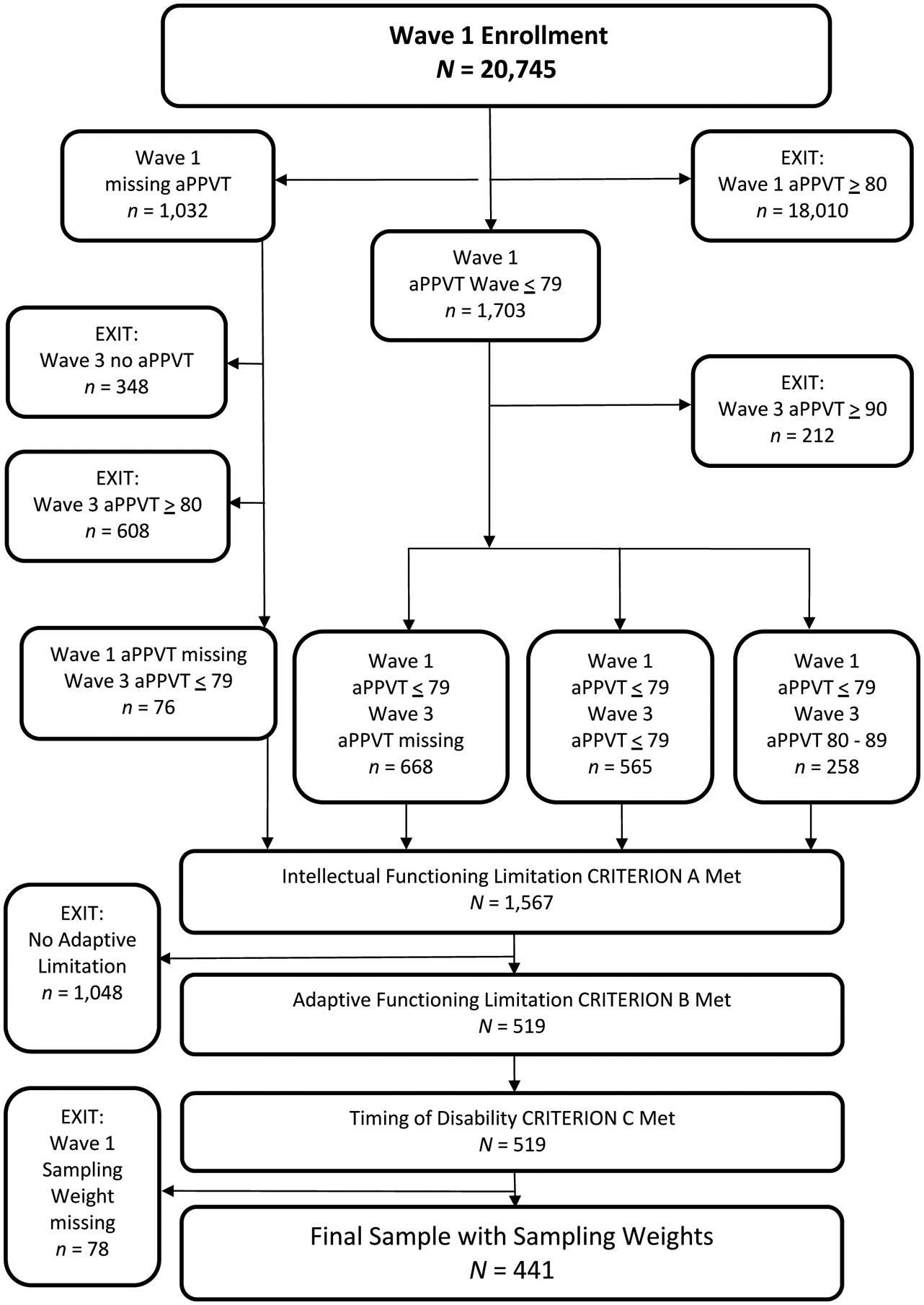
Consort Diagram Demonstrating Progression to the final Add Health ID Subsample.
Characteristics of ID Subpopulation and ID Criterion
Demographic characteristics of the AYAs (n=441) and parents (one per family), are presented in Table 4. The AYAs’ mean age was 16.1 years (range: 12, 21) and mean maximum aPPVT was 69.6 (range: 7, 89). The weighted characteristics of the ID criterion are displayed in Table 3. There were 62 participants of the 441 with an aPPVT at Wave 1 who scored ≤ 79 and then at Wave 3 had a score ≥ 80 and ≤ 89. Otherwise, those who had a Wave 1 aPPVT scored ≤ 79, and if they had a Wave 3 aPPVT, it was also remained ≤ 79.
Table 4.
Demographic Characteristics of Adolescents with ID and Parents at Wave 1 (N = 441)
| Unweighted N | Unweighted f | Weighted % | Weighted SE | |
|---|---|---|---|---|
| Adolescents with ID | ||||
| Male | 441 | 232 | 53.1% | 3.68 |
| Race (may identify 1 or more) | ||||
| White | 433 | 175 | 44.0% | 3.29 |
| Black/African American | 433 | 164 | 35.9% | 5.88 |
| American Indian/Native | 433 | 13 | 2.4% | 1.18 |
| American | ||||
| Asian or Pacific Islander | 433 | 29 | 4.1% | 1.41 |
| Other | 433 | 65 | 15.9% | 3.87 |
| Hispanic/Latinx | 437 | 144 | 28.0% | 3.60 |
| Parent Characteristics | ||||
| Female | 403 | 388 | 97.6% | 0.94 |
| Race (may identify 1 or more) | ||||
| White | 415 | 181 | 44.3% | 5.03 |
| Black/African American | 415 | 158 | 35.7% | 5.62 |
| American Indian/Native | 415 | 14 | 3.7% | 1.82 |
| American | ||||
| Asian or Pacific Islander | 415 | 24 | 3.6% | 1.29 |
| Other | 415 | 54 | 16.0 | 2.05 |
| Hispanic/Latinx | 414 | 133 | 26.2% | 3.56 |
| Marital Status | ||||
| Single, Never Married | 414 | 56 | 13.0% | 2.31 |
| Married | 414 | 213 | 53.2% | 4.36 |
| Widowed | 414 | 22 | 4.7% | 1.51 |
| Divorced | 414 | 72 | 17.9% | 2.25 |
| Separated | 414 | 51 | 11.1% | 1.89 |
| Highest Education Completed | ||||
| Less than high school | 414 | 200 | 47.4% | 4.62 |
| High School Graduate/GED | 414 | 111 | 28.6% | 2.74 |
| Some College | 414 | 81 | 19.2% | 3.10 |
| College Graduate | 414 | 15 | 3.6% | 1.01 |
| Graduate Training | 414 | 7 | 1.2% | 0.52 |
| Employed Outside Home | 414 | 210 | 50.8% | 4.15 |
| Employed Full Time | 406 | 154 | 35.5% | 3.45 |
| Annual Household Income | ||||
| Less than $14,999 | 347 | 150 | 42.1% | 4.85 |
| $15,000–$34,999 | 347 | 111 | 29.4% | 2.69 |
| $35,000–$49,999 | 347 | 52 | 15.6% | 3.17 |
| $50,000–$74,999 | 347 | 21 | 8.0% | 2.06 |
| $75,000–$99,999 | 347 | 7 | 3.3% | 1.68 |
| $100,000 and more | 347 | 6 | 1.5% | 0.72 |
N = unweighted ID sample; f = unweighted frequencies; weighted percent (%) after applying Wave sampling weights, stratification, and cluster variables; SE = weighted standard error of the percent (%).
The rate of ADL limitation at Wave 1, representing adaptive functioning limitations attributed to physical conditions, was low (6.6%). There were 6 AYAs who had at least one parent-reported adaptive functioning limitation at Wave 1, yet 12 AYAs self-reported having at least one adaptive functioning limitation. Requiring assistance with shopping was the most reported need (3.7%). At Wave 2, when the question was not limited to those who reported physical limitations, many more adolescents reported adaptive functioning limitations. There were 137 AYAs who had at least 1 adaptive functioning limitation at Wave 2. Of the 310 AYAs whose parents reported they had a learning disability, 248 had other indicators of adaptive functioning limitation (range 1 – 19 indicators). Sixty-two AYA’s (20%) who already met the aPPVT criterion met the adaptive functioning criterion based on learning disability alone. When asked about their perception of disability, more parents (n=324) than adolescents (n=143) considered the adolescent disabled.
Additional Characteristics of Adolescents and Young Adults with ID
High school transcripts were available for 211 AYAs; 71.8% graduated with a standard high school diploma, dropped out (10.7%), were identified as other non-graduate (10.5%), or received a certificate of completion (2.1%). To capture adolescent self-reported physical disability involving extremities on the in-school questionnaire at Wave 1, the original Add Health Study team flagged 589 students from the full sample who self-reported physical disability. Among our subsample, 8 AYAs (0.4%) had the Wave 1 flag. The majority (86.4%) of the 20 parents who attributed their child’s difficulties to their physical condition indicated that this physical condition was present at birth while 10.8% reported that it was due to an accident.
DISCUSSION
While there is a critical need to use large population data sets to understand the health needs of individuals with ID, challenges remain in their identification. We present here a method for identifying individuals who meet conceptually grounded criteria for ID using nationally representative databases. The model can be used to evaluate the presence of similar variables in other datasets and to guide decisions on their usefulness for identifying and studying individuals with intellectual disabilities.
Our method for identifying AYAs meeting criteria for ID was grounded in the use of leading ID definitions (APA, 2013; Schalock et al., 2010). In order to make nationally representative inferences, we retained 441 AYAs who met the criteria for ID and had valid sampling weights. We developed the Add Health ID Indicator to capture both intellectual and adaptive functioning to prevent the inclusion of an AYA with an aPPVT ≤ 79 at one time point but with no other features of ID, as could occur in the case of an AYA with low academic opportunity or short term cause for low aPPVT (e.g., intoxication) (Haydon et al., 2011; Kahn & Halpern, 2016).
The intellectual functioning of the majority (46.5%) of AYAs (maximum aPPVT scores), was borderline or very low (between 70–79; mean maximum 69.6). This was expected, as previous literature demonstrates that 85% of those with ID have mild severity (King, 2009). Studies using the PPVT with samples with ID have found mean standardized scores of 82 (Williams syndrome; Mervis & John, 2010) and 53 (Autism; Krasileva et al., 2017). Because the abridged version of the PPVT measures receptive vocabulary ability alone rather than all components of intelligence, we are not able to further differentiate among severity based on the aPPVT score.
Features of adaptive functioning limitations, specifically physical disability and learning disability, if taken alone, can present risks to the validity of this ID Indicator. Thus, it is important that they be considered in combination with other core domains of ID. A minority of parents (6.6%) attributed their adolescents’ difficulties to a physical condition during Wave 1. And only 0.4% of the sample were flagged as those AYAs who had self-reported physical disability. This finding reveals that many with physical disability did not demonstrate functioning consistent with ID. Caution is needed in this interpretation as this identification relied on the ability of AYA to self-report, which may have been difficult for those with significant ID, and may also indicate adolescents’ reluctance to report differences or disabilities. In contrast, 80.5% of participants had a learning disability based on parent report. Parents might have been (a) informed that their child had a learning disability when they really had ID, (b) been more comfortable communicating that their child had a learning disability, or (c) been unaware that their child had ID but recognized that their child had difficulty learning.
Implications for Research, Policy, and Nursing Practice
Add Health is an example of a large data set that holds potential to learn more about the health of the ID population. Additional strategies could improve the utility of Add Health and other data sets. Self-report from AYAs with ID is important, but care needs to be taken in assessing the comprehension level of standardized questions. A mixed method study with primary data collection that includes qualitative interviews with AYAs and parents may help to overcome this challenge and assess questions of validity and reliability for this population. Because of skip logic, parents and AYAs in Wave 1 were only asked ADL questions if they indicated upper or lower extremity problems or other physical/functional limitations of physical origin. ADLs can be impacted by ID, and not just by physical disability, and thus it is important to structure studies to ask ADL questions of all individuals. Lastly, interviewer observation-based variables could be leveraged in future waves and within other studies to allow for improved triangulation of data. Other population-based health related datasets may contain other variables that allow for operationalizing the three criteria used in this study to identify the ID subpopulation.
The approach developed in this paper can be used to identify the strengths and weaknesses of using the best available variables in each dataset and to inform a decision on the usefulness of the dataset for studying the ID subpopulation. Future research leveraging other large population-based health related data sets and merging data sources is needed to address knowledge gaps of this adolescent to young adulthood period as well as across the life course for the ID population.
Policies to promote effective data exchange across systems (e.g., medical, education) are crucial for understanding life course development and their related impact. For example, intellectual, adaptive, and other types of cognitive testing results are used to determine eligibility for supplemental security income but are not currently accessible to merge with other data sources. The ability to connect this information with data sources as we have described could improve tracking of health outcomes, inform policy, and guide efforts to improve the health and well-being of the population with ID. Given the need for robust data, the expense of conducting population studies, and the current funding environment, secondary data analysis of existing data and strategies to identify ID subsamples is important to uncover and address disparities, drive clinical improvement, and inform nursing practice.
Study Limitations
The aPPVT may not be equivalent across cultures, and AYAs with reduced educational opportunities may have poorer performance than those with better opportunities. Secondly, a limited range of variables were available in Add Health to assess components of ID. Third, it is possible that this method results in a conservative identification of those with ID and may result in false negatives given that those without adaptive functioning limitations but with aPPVT ≤ 79 (n = 1,048) were excluded. Future studies using this method could compare this group to those that (n = 1,048) exited to see how they differ over time in outcomes and whether they should be further classified.
Conclusion
In the absence of appropriate ways to identify and study individuals with ID and their health trajectories in population studies, health disparities are likely to continue unnoticed, untracked, and unaddressed. This study demonstrates a feasible methodology for identifying individuals with ID within a large data set. By doing so we can learn more about their unique experiences and needs including those of racial minority and mild ID who are generally underrepresented in clinical studies, and at additional risk due to having multiple minority identities.
Acknowledgement:
This research was supported by the Margolis Scholar Award from the Duke-Margolis Center for Health Policy. This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain the Add Health data files is available on the Add Health website (http://www.cpc.unc.edu/addhealth). No direct support was received from grant P01-HD31921 for this analysis.
Ethical Conduct of Research: This research study was approved by the Duke University Health System Institutional Review Board (Study Number: 00101050). All study activities were conducted according to this approved review and met ethical conduct of research standards.
Footnotes
The authors have no conflicts of interest to report.
Contributor Information
Susan G. Silva, Duke University School of Nursing, Durham, NC.
Gary R. Maslow, Duke University School of Medicine, Durham, NC.
Carolyn T. Halpern, University of North Carolina at Chapel Hill Gillings School of Global Public Health, Chapel Hill, NC.
Elizabeth I. Merwin, University of Texas Arlington College of Nursing and Health Innovation, Arlington, Texas.
Sharron L. Docherty, Duke University School of Nursing, Durham, NC.
References
- Acharya K, Meza R, & Msall ME (2017). Disparities in life course outcomes for transition-aged youth with disabilities. Pediatric Annals, 46(10), e371–e376 10.3928/19382359-20170918-01 [DOI] [PubMed] [Google Scholar]
- American Association on Intellecual and Developmental Disabilities. (2007). Mental retardation is no more - new name is intellecual and developmental disabilities [Press release]. Retrieved from http://sath.org/page/Mental_Retardation_Is_No_More151New_Name_Is_Intellectual_and_Developmental_Disabilities/10130/741/
- American Psychiatric Association. (2013). Neurodevelopmental Disorders In Diagnostic and statistical manual of mental disorders (5th ed.). http//doi.org/10.1176appi.books.9780890425596.dsm05 [Google Scholar]
- Anderson LL, Humphries K, McDermott S, Marks B, Sisirak J, & Larson S (2013). The state of the science of health and wellness for adults with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 51(5), 385–398. 10.1352/1934-9556-51.5.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker KA (2003). History of the Stanford-Binet Intelligence Scales: Content and psychometrics (Stanford-Binet Intelligence Scales, Fifth Edition Assessment Service Bulletin No. 1). Itasca, IL: Riverside Publishing. [Google Scholar]
- Butrymowicz S, & Mader J (2017). Almost all students with disabilites are capable of graduating on time. Here’s why they’re not. The Hechinger Report. Retrieved from https://hechingerreport.org/high-schools-fail-provide-legally-required-education-students-disabilities/ [Google Scholar]
- Carolina Population Center (1998). National Longitudinal Study of Adolescent Health: Wave 1 adolescent in-home questionnaire code book, introductory guides. Retrieved from http://www.cpc.unc.edu/projects/addhealth/documentation/restricteduse/datasets?b_start:int=0
- Centers for Disease Control and Prevention (CDC), National Center on Birth Defects and Developmental Disabilities Health Surveillance Work Group. (2009). U.S. surveillance of health of people with intellectual disabilites: A white paper. Retrieved from https://www.cdc.gov/ncbddd/disabilityandhealth/pdf/209537-A_IDmeeting%20short%20version12-14-09.pdf
- Chen P (2018). Appropriate analysis in Add Health: Correcting for design effects & selecting weights. Retrieved from https://www.cpc.unc.edu/projects/addhealth/events/Appropriate_Analysis_in_Add_Health_Correcting_for_Design_Effects_and_Selecting_Weights_Chen.pdf
- Cheng MM, & Udry JR (2005). Sexual experiences of adolescents with low cognitive abilities in the U.S. Journal of Developmental & Physical Disabilities, 17(2), 155–172. 10.1007/s10882-005-3666-3 [DOI] [Google Scholar]
- Coppus AM (2013). People with intellectual disability: What do we know about adulthood and life expectancy? Developmental Disabilities Research Reviews, 18(1), 6–16. 10.1002/ddrr.1123 [DOI] [PubMed] [Google Scholar]
- Dunn L, & Dunn LM (1981). Peabody Picture Vocabulary Test- Revised manual. Circle Pines, MN: American Guidance Service. [Google Scholar]
- Emerson E (2011). Health status and health risks of the “hidden majority” of adults with intellectual disability. Intellectual and Developmental Disabilities, 49(3), 155–165. 10.1352/1934-9556-49.3.155 [DOI] [PubMed] [Google Scholar]
- Emerson E (2012). Deprivation, ethnicity and the prevalence of intellectual and developmental disabilities. Journal of Epidemiology and Community Health, 66(3), 218–224. 10.1136/jech.2010.111773 [DOI] [PubMed] [Google Scholar]
- Ervin DA, Hennen B, Merrick J, & Morad M (2014). Healthcare for persons with intellectual and developmental disability in the community. Frontiers in Public Health, 2(83), 1–8. 10.3389/fpubh.2014.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox MH, Bonardi A, & Krahn GL (2015). Expanding public health surveillance for people with intellectual and developmental disabilities in the United States. International Review of Research in Developmental Disabilities, 48(4), 73–114. [PMC free article] [PubMed] [Google Scholar]
- Halfon N, Larson K, Lu M, Tullis E, & Russ S (2014). Lifecourse Health Development: Past, Present and Future. Maternal and Child Health Journal, 18(2), 344–365. doi.org/10.1007/s10995-013-1346-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halfon N, & Forrest CB (2018). The Emerging Theoretical Framework of Life Course Health Development In Halfon N, Forrest CB, Lerner R, & Faustman E (Eds.), Handbook of Life Course Health Development (pp. 19–43). doi.org/10.1007/978-3-319-47143-3 [Google Scholar]
- Halfon N, & Hochstein M (2002). Life Course Health Development: An integrated framework for developing health, policy, and research. Milbank Quarterly, 80(3), 433–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern CT, Joyner K, Udry JR, & Suchindran C (2000). Smart teens don’t have sex (or kiss much either). Journal of Adolescent Health, 26(3), 213–225. 10.1016/s1054-139x(99)00061-0 [DOI] [PubMed] [Google Scholar]
- Harris KM (2009). The National Longitudinal Study of Adolescent to Adult Health (Add Health), Wave I & II, 1996–1996; Wave III, 2001–2002; Wave IV, 2007–2009 [machine-readable data file and documentation].
- Haydon AA, McRee AL, & Tucker Halpern C (2011). Unwanted sex among young adults in the United States: The role of physical disability and cognitive performance. Journal of Interpersonal Violence, 26(17), 3476–3493. 10.1177/0886260511403756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahn NF, & Halpern CT (2016). The relationship between cognitive ability and experiences of vaginal, oral, and anal sex in the United States. The Journal of Sex Research. 10.1080/00224499.2016.1247149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King BH, Toth KE, Hodapp RM, & Dykens EM (2009). Intellectual disability In Sadock BJ, Sadock VA, & Ruiz P (Eds.). Comprehensive textbook of psychiatry (9th ed., pp. 3444–3474). Philadelphia: Lippincott Williams & Wilkins. [Google Scholar]
- Krahn G, Fox M, Campbell V, Ramon I Jesien G (2010). Developing a health surveillance system for people with intellectual disabilites in the United States. Journal of Policy and Practice in Intellectual Disabilities, 7(3), 155–166. [Google Scholar]
- Krahn GL, & Fox MH (2014). Health disparities of adults with intellectual disabilities: What do we know? What do we do? Journal of Applied Research in Intellect Disabilities, 27(5), 431–446. 10.1111/jar.12067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krasileva KE, Sanders SJ, & Bal VH (2017). Peabody picture vocabulary test: Proxy for verbal IQ in genetic studies of autism spectrum disorder. Journal of Autism and Developmental Disorders, 47(4), 1073–1085. 10.1007/s10803-017-3030-7 [DOI] [PubMed] [Google Scholar]
- Lauer E, & McCallion P (2015). Mortality of people with intellectual and developmental disabilities from select US state disability service systems and medical claims data. Journal of Applied Research in Intellectual Disabilities, 28(5), 394–405. 10.1111/jar.12191 [DOI] [PubMed] [Google Scholar]
- Mandell DS, Wiggins LD, Carpenter LA, Daniels J, DiGuiseppi C, Durkin MS, … Kirby RS (2009). Racial/ethnic disparities in the identification of children with autism spectrum disorders. American Journal of Public Health, 99(3), 493–498. 10.2105/AJPH.2007.131243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, & Saxena S (2011). Prevalence of intellectual disability: A meta-analysis of population-based studies. Research in Developmental Disabilities, 32(2), 419–436. 10.1016/j.ridd.2010.12.018 [DOI] [PubMed] [Google Scholar]
- Mervis CB, & John AE (2010). Cognitive and behavioral characteristics of children with Williams syndrome: implications for intervention approaches. American Journal of Medical Genetics. Part C: Seminars in Medical Genetics, 154c(2), 229–248. 10.1002/ajmg.c.30263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan PL, Farkas G, Hillemeier MM, & Maczuga S (2017). Replicated evidence of racial and ethnic disparities in disability identification in US schools. Educational Researcher, 46(6), 305–322. 10.3102/0013189X17726282 [DOI] [Google Scholar]
- O’Hara J (2003). Learning disabilites and ethnicity: Achieving cultural competence. Advances in Psychiatric Treatment, 9, 166–174. 10.1192/apt.93.166 [DOI] [Google Scholar]
- Queiros FC, Wehby GL, & Halpern CT (2015). Developmental disabilities and socioeconomic outcomes in young adulthood. Public Health Reports, 130(3), 213–221. 10.1177/003335491513000308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid SM, Meehan EM, Arnup SJ, & Reddihough DS (2018). Intellectual disability in cerebral palsy: A population-based retrospective study. Developmental Medicine and Child Neurology, 60(7), 687–694. 10.1111/dmcn.13773 [DOI] [PubMed] [Google Scholar]
- Schalock RL, Borthwick-Duffy SA, Bradley VJ, Buntinx WHE, Coulter DL, Craig EM Yeager MH (2010). Intellectual disability: Definition, classification, and systems of supports (11th edition). Washington, DC: American Association on Intellectual and Developmental Disabilities. [Google Scholar]
- Scott HM, & Havercamp SM (2014). Race and health disparities in adults with intellectual and developmental disabilities living in the United States. Intellectual and Developmental Disabilities, 52(6), 409–418. 10.1352/1934-9556-52.6.409 [DOI] [PubMed] [Google Scholar]
- Wechsler D (2004). The Wechsler Intelligence Scale for Children (4th ed.). London, UK: Pearson Assessment. [Google Scholar]
- Zuckerman KE, Sinche B, Meijia A, Cobian M, Becker T, & Nicolaidis C (2014). Latino parents’ perspectives on barriers to autism diagnosis. Academic Pediatrics, 14, 301–308. 10.1016/j.acap.2013.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]


