Abstract
Purpose
Supportive social networks are important to the post-traumatic response process. However, the effects of social network structure may be distinct from the perceived function of those networks. The present study examined the relative importance of role diversity and perceived strength of social support in mitigating post-traumatic stress disorder (PTSD).
Methods
Data were drawn from respondents who report lifetime potentially traumatic events in the National Epidemiologic Survey on Alcohol and Related Conditions (N = 31,650). The Social Network Index (SNI) was used to measure the diversity of social connections. The Interpersonal Support Evaluation List (ISEL-12) was used to measure the perceived availability of social support within the network. Odds of current PTSD were compared among individuals representing four dichotomous types of social support: high diversity/high perceived strength, high diversity/low perceived strength, low diversity/high perceived strength, and low diversity/low perceived strength to examine which type of support is more protective against PTSD.
Results
Unadjusted odds of PTSD were 1.59 (95 % CI 1.39–1.82) for those with low versus high perceived support strength, and 1.10 (0.94–1.28) among those with non-diverse versus diverse social networks. Compared to the reference group (high diversity/high perceived strength), the adjusted odds of current PTSD were higher for two groups: low diversity/low perceived strength (OR = 1.62; 1.33–1.99), and low diversity/high perceived strength (OR = 1.57; 1.3–1.91). The high diversity/low perceived strength group had no greater odds of PTSD (OR = 1.02; 0.81–1.28).
Conclusion
The diversity of a social network is potentially more protective against PTSD than the perception of strong social support. This suggests that programs, which engage individuals in social groups and activities may effectively attenuate the risk of PTSD. A better understanding of how these networks operate with respect to PTSD prevention and mitigation holds promise for improving psychiatric health.
Keywords: PTSD, Trauma, Social support, Social networks
Background
That social support impacts psychiatric well-being, in both positive and negative ways, has been long-established [1, 2]. There are numerous mechanisms through which social relationships may influence mental health. For example, social support may promote normative behavior and may lead to either positive (e.g., regular physical activity) or negative (e.g., heavy alcohol use) health outcomes [3]; feelings of social integration may produce positive stress by catalyzing an individual’s sense of purpose, belonging, security, or self-worth, leading to increased motivation for positive self-care (e.g., healthy eating); also, access to broader support offered by community, religious, or other organizations may increase access to health-promoting resources and behaviors (e.g., completing regular physical checkups) [4].
The social support construct is generally considered to be a composite of three aspects of an individual’s life: received support (i.e., the receipt of actual help), perceived support (i.e., the belief that help is available if needed), and embedded support (i.e., the size, type, and diversity of social roles) [2, 5]. High levels of embedded support have been reliably associated with lower depression and anxiety, and less cognitive decline with aging [4, 6, 7]. There is also substantial evidence that greater perceived availability of social support buffers the rate and severity of psychological distress, depression, and anxiety which may result from exposure to a traumatic event [3, 8–10].
To better understand the distinctive relationship between trauma and social support, Cohen and Wills [3] developed a stress-buffering model, which posits that the effects of social support may be protective against potentially negative health outcomes following exposure to trauma. In this context, both perceived and embedded social support may influence an individual’s subjective appraisal and his/her negative internal or external responses to a traumatic event [11]. In fact, one large meta-analysis of risk factors for post-traumatic stress disorder (PTSD) etiology reported that the lack of social support in the aftermath of a traumatic event was one of the strongest predictors of PTSD (r = 0.40) [12].
Though studies have thoroughly investigated the relationship between social support and mental health outcomes, rarely have researchers utilized more than one aspect of social support in the same study. When using a single scale to measure social support rather than a multi-modal assessment, a non-significant finding is therefore interpreted as a global null effect, a conclusion which may overlook key unmeasured aspects of social support. The mechanisms through which perceived and embedded social support influence the post-traumatic response and subsequent psychiatric illness may operate in significantly distinct ways [7, 13]. Further, the influence of social support may confer greater risk or protection unequally within a general population. In addition to well-known risk factors such as sex and socio-economic position, [14, 15] certain stages of life may act as ‘critical periods’ during which the formation and importance of certain social relationships plays an even greater role for psychiatric well-being and resiliency to trauma (e.g., youth [16] and aging populations [17]).
The present analysis sought to examine differences in the association between PTSD and two key social network metrics, embedded social role diversity versus perceived availability of support, among individuals exposed to traumatic life events in the general US population. The primary aim was to investigate the association between social support and current PTSD among respondents who have experienced trauma, stratified by the isolated types of social support, to examine which type of support is more positively associated with PTSD. The differential effects of social support among types of trauma, as well as age at the time of trauma, were explored in concordance with previous research [18].
Methods
Data source and study population
Data were taken from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The NESARC is the largest and most comprehensive household survey ever conducted on alcohol use, alcohol use disorders, and related physical and psychiatric disabilities in the US. The study was a multistage stratified design in which primary sampling units, housing units, and group-quarter units were stratified according to certain socio-demographic criteria. Non-Hispanic Black and Hispanic housing units were selected at higher rates than other housing units. In addition, young adults (age 18–24) were oversampled, and the final data were weighted to reflect the demographic distribution of the US based on the 2000 census. Data collection spanned two waves. The first wave included 43,093 civilian non-institutionalized adult respondents in the US, interviewed from 2001–2002. Three years later, 34,653 respondents were re-interviewed [19], a follow-up rate of 80 %. Our study sample included only respondents interviewed at Wave 2, as this assessment included a module on traumatic events and post-traumatic stress disorder. Only individuals who had ever experienced a traumatic event were included in the analysis (n = 31,650, 91.3 % of the sample).
Measures
Trauma and PTSD
Thirty-three different traumatic events experienced during a respondent’s lifetime were queried in the survey. Two additional binary variables were created to test for interaction by the type of traumatic experience, one grouping types of trauma as direct (e.g., personally experienced rape/assault) versus indirect (e.g., unexpected death of a loved one), and another grouping traumas experienced as a child (<18) versus as an adult.
Past-year cases of PTSD were assessed using the DSM-IV criteria using the alcohol use disorder and associated disabilities interview schedule (AUDADIS-IV)—DSM-IV version, a computerized, fully-structured diagnostic interview for use by experienced interviewers without clinical training [20]. A total of 19 dichotomous DSM-IV criterion symptoms and other criteria that define the disorder, including the subjective response to the event, duration, and impairment, were asked in connection with the worst (or single) event [21]. The test–retest reliability and internal consistency of the scales were previously determined in NESARC sub-samples, and were reported as fair to good (alpha = 0.84; κ = 0.64–0.77) [22–24]. The symptoms were grouped by three distinct factors: re-experiencing, avoidance/numbing, and arousal, in accordance with DSM-IV definitions [20].
Social network size and role diversity
The Social Network Index (SNI) is a 12-item index, which measures an individual’s quantity and type of regular social relationships (e.g., spouse, parent, friend, volunteer) [25]. The scale was designed to capture three aspects of one’s social network: the overall number of people in the network, the number of regular social roles (i.e., employed at least once every 2 weeks), and the number of different network domains in which an individual is regularly active (e.g., family, friends, work, church/temple) [26]. In concurrence with previous research that has used the SNI, this analysis focused on the number of regular social roles (between 0–12) as a measure of social role diversity [6, 24], though results were consistent when total size of the network was examined. Of the 12 potential social roles, the respondent scored 1 point for each role reported. The SNI has shown fair reliability (alpha = 0.64–0.70) [24, 27]. The SNI variable was a dichotomized score (high versus low) according to the median number of total roles reported by each respondent in the sample (median = 5).
Perceived interpersonal social support
The Interpersonal Support Evaluation List (ISEL-12) measures the perceived availability of social support [26]. Questions include both positive and negative statements about social relationships (e.g., ‘If I needed help fixing an appliance or repairing my car, there is someone who would help me’; ‘I do not often get invited to do things with others’). Responses are on a four point scale (0–3) from definitely false to definitely true. The scale has been widely used and has shown excellent reliability (alpha = 0.81–0.90) [28–30]. For this analysis, all items were coded to represent decreasing perceptions of social support availability and summed to create a composite ISEL-12 score (range = 0–36). The variable was dichotomized by dividing the total score of the overall sample into two groups (low versus high) based on the sample median (low = 0–31; high = 32–36). The score was dichotomized using the median score as a cut-off, to maintain adequate power during multivariable analysis; however, other cut-points were also explored. Sensitivity analyses were conducted using a cut-point of 17, the midpoint of the range of possible total ISEL-12 scores (low = 0–17; high = 18–36); results did not change.
As a way to isolate the association that each measure of social support may have with the outcome, the dichotomized SNI and ISEL-12 scales were combined to create four sub-types of social support: high diversity/high perceived strength, high diversity/low perceived strength, low diversity/high perceived strength, and low diversity/low perceived strength.
Covariates
The analysis tested those socio-demographic covariates that have been consistently associated with the development of social support and etiology of PTSD. If significant, the covariate was added to the final model. Categorical variables included race/ethnicity (non-Hispanic White, non-Hispanic Black, Native American/Alaska native, Asian/Pacific Islander, and Hispanic), age, education, and income; continuous variables included number of traumas; and dichotomous variables included comorbid psychiatric disorders [12]. To examine the potential for trans-generational influence of psychiatric illness, the respondent’s family history of alcohol, drug, mood, or behavioral disorders among either the respondent’s mother or biological father was also considered as a dichotomous covariate. Secondary analysis examined associations between other psychiatric disorders that have shown significant comorbidity with PTSD, including mood disorders (major depression, dysthymia mania/hypomania), anxiety disorders (generalized anxiety, social anxiety, phobia), and alcohol, and drug dependence disorders [31]. All comorbid disorders were dichotomous and were determined based on DSM-IV criteria [21] with fair to good reliability (r = 0.42–0.64) [24, 32] (κ = 0.67–0.84) [33, 34] and good to excellent validity [35, 36].
Statistical analysis
The odds of current PTSD among the four social support types were modeled using logistic regression. These measures were compared to separate crude associations between perceived support and role diversity. p values of 0.05 or less (two-sided) were considered statistically significant. All confidence intervals were calculated at a level of 95 %. The primary analysis also tested for effect modification among directly or indirectly experienced trauma, and trauma experienced as a child or as an adult. All analysis was completed using SAS® [37] and SUDAAN software [38] to adjust for the NESARC complex survey design.
Results
Demographic frequencies of social types and PTSD in the study population
Among the study population, the distribution of social support types was 30.3 % (low diversity/low perceived strength), 18.0 % (high diversity/low perceived strength), 22.2 % (low diversity/high perceived strength), and 29.6 % (high diversity/high perceived strength). The overall prevalence of PTSD was 7.9 %, and was more than twice as high among women than men (9.5 versus 4.4 %). PTSD was most common among individuals who were aged 30–44 (7.9 %); widowed, separated, or divorced (10.4 %); with personal income<$20,000 per year (9.4 %); and with less than a high school degree (8.9 %). Non-Hispanic Black and Native American respondents reported PTSD most frequently (8.8 and 10.4 %, respectively). Prevalence of PTSD was 4.7, 5.7, 7.5, and 9.8 % for each respective support group. Frequencies of all demographic characteristics among support groups are presented in Table 1.
Table 1.
Bivariable social support type and current PTSD frequencies among socio-demographic covariates
| n (total = 31,650) | Social support type (%,SE) | PTSD (n = 2,496; 7.9 %) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [1] SNI = 0; ISEL = 0 (30.3 %) | [2] SNI = 1; ISEL = 0 (18.0 %) | [3] SNI = 0; ISEL = 1 (22.2 %) | [4] SNI = 1; ISEL = 1 (29.6 %) | χ2 | P | % | SE | χ2 | P | ||||||
| Sex | 3.5 | 0.0204 | 144.6 | <0.0001 | |||||||||||
| Men | 13,390 | 31.0 | 0.59 | 17.7 | 0.4 | 22.4 | 0.49 | 28.8 | 0.52 | 4.4 | 0.2 | ||||
| Women | 18,260 | 29.5 | 0.45 | 18.2 | 0.39 | 22.0 | 0.38 | 30.2 | 0.55 | 9.5 | 0.29 | ||||
| Age | 28.4 | <0.0001 | 29.9 | <0.0001 | |||||||||||
| 18–29 | 4,437 | 30.1 | 0.96 | 27.5 | 0.87 | 16.3 | 0.65 | 26.2 | 0.90 | 7.6 | 0.45 | ||||
| 30–44 | 9,704 | 24.1 | 0.58 | 15.9 | 0.46 | 23.7 | 0.55 | 36.3 | 0.67 | 8.0 | 0.32 | ||||
| 45–64 | 11,104 | 27.4 | 0.63 | 14.6 | 0.43 | 26.5 | 0.56 | 31.5 | 0.64 | 7.7 | 0.31 | ||||
| 65+ | 6,405 | 45.2 | 0.90 | 19.5 | 0.64 | 16.9 | 0.64 | 18.4 | 0.63 | 4.2 | 0.29 | ||||
| Race/ethnicity | 3.8 | 0.0002 | 6.8 | 0.0001 | |||||||||||
| NH White | 18,888 | 29.3 | 0.42 | 17.5 | 0.34 | 22.2 | 0.41 | 31.0 | 0.41 | 6.9 | 0.22 | ||||
| NH Black | 5,811 | 31.9 | 0.86 | 20.2 | 0.69 | 21.1 | 0.67 | 26.8 | 0.77 | 8.8 | 0.47 | ||||
| Native American/Alaska Native | 539 | 34.0 | 2.27 | 19.8 | 2.24 | 20.5 | 2.08 | 25.7 | 2.20 | 10.4 | 1.32 | ||||
| Asian/Pacific Islander | 848 | 35.0 | 2.29 | 17.6 | 1.48 | 22.7 | 2.07 | 24.7 | 1.64 | 3.8 | 0.74 | ||||
| Hispanic | 5,564 | 32.4 | 1.27 | 19.0 | 0.86 | 23.4 | 0.87 | 25.2 | 0.93 | 7.2 | 0.59 | ||||
| Current marital status | 56.1 | <0.0001 | 35.4 | <0.0001 | |||||||||||
| Married/living as if married | 17,390 | 20.3 | 0.44 | 12.1 | 0.30 | 28.8 | 0.45 | 38.9 | 0.51 | 6.1 | 0.23 | ||||
| Widowed/separated/divorced | 8,296 | 50.9 | 0.73 | 25.5 | 0.65 | 11.4 | 0.45 | 12.2 | 0.45 | 10.5 | 0.44 | ||||
| Never married | 5,964 | 45.1 | 0.91 | 32.0 | 0.83 | 9.5 | 0.54 | 13.5 | 0.56 | 7.1 | 0.38 | ||||
| Personal income | 27.0 | <0.0001 | 35.6 | <0.0001 | |||||||||||
| $0–19,999 | 13,592 | 38.3 | 0.61 | 19.0 | 0.44 | 20.0 | 0.45 | 22.6 | 0.52 | 9.4 | 0.33 | ||||
| $20–34,999 | 7,337 | 28.7 | 0.67 | 19.5 | 0.59 | 22.3 | 0.59 | 29.5 | 0.7 | 6.7 | 0.35 | ||||
| $35–69,999 | 7,690 | 23.2 | 0.78 | 16.5 | 0.5 | 24.4 | 0.68 | 35.9 | 0.78 | 5.1 | 0.28 | ||||
| $70,000+ | 3,031 | 18.6 | 0.85 | 14.2 | 0.76 | 25.5 | 1.01 | 41.6 | 1.06 | 3.6 | 0.39 | ||||
| Education | 44.7 | <0.0001 | 19.4 | <0.0001 | |||||||||||
| Less than high school | 4,678 | 42.8 | 0.98 | 21.8 | 0.85 | 18.5 | 0.9 | 16.9 | 0.77 | 8.9 | 0.49 | ||||
| HS graduate/GED | 15,413 | 31.8 | 0.55 | 19.3 | 0.43 | 20.8 | 0.44 | 28.2 | 0.48 | 7.5 | 0.25 | ||||
| >High school | 11,559 | 23.9 | 0.62 | 15.0 | 0.4 | 25.4 | 0.51 | 35.8 | 0.66 | 5.9 | 0.27 | ||||
| Family history of psychiatric disorder | 7.7 | 0.0002 | 119.8 | <0.0001 | |||||||||||
| No | 19,555 | 28.0 | 0.66 | 18.5 | 0.4 | 21.8 | 0.42 | 31.7 | 0.63 | 5.0 | 0.10 | ||||
| Yes | 12,095 | 29.9 | 0.58 | 17.0 | 0.48 | 24.0 | 0.56 | 29.2 | 0.62 | 10.5 | 0.15 | ||||
| Psychiatric comorbidities | 48.6 | <0.0001 | 214.9 | <0.0001 | |||||||||||
| No | 19,274 | 26.8 | 0.54 | 17.7 | 0.37 | 22.3 | 0.41 | 33.2 | 0.57 | 2.9 | 0.14 | ||||
| Yes | 12,376 | 35.6 | 0.61 | 18.5 | 0.41 | 22.1 | 0.48 | 23.9 | 0.52 | 13.5 | 0.36 | ||||
Each variable adjusted for all other covariates in the model
The unadjusted odds of PTSD among individuals with low versus high perceived support were 1.59 (95 % CI 1.39–1.82). Among individuals with low versus high network diversity, the odds of PTSD were 1.10 (CI 0.94–1.28) (Fig. 1). Only the association between perceived support strength was statistically significant, suggesting that the absence of perceived support is more strongly associated with PTSD than low network diversity.
Fig. 1.
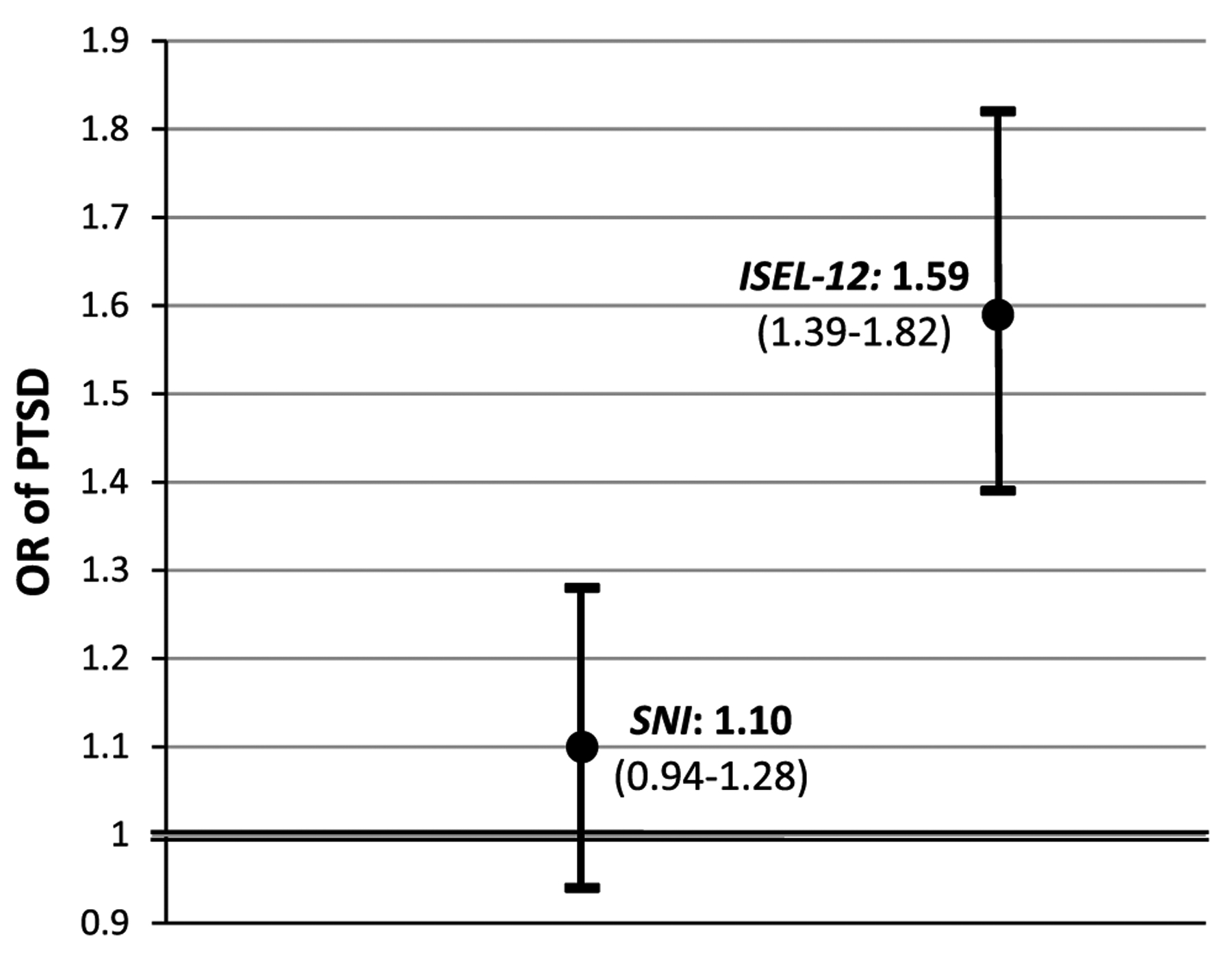
Odds ratios and 95 % CIs of PTSD among individuals with low social role diversity (SNI) and low perceived support (ISEL-12). Each measure is unadjusted for the effect of the other measure, i.e. low perceived support includes individuals with high and low social network diversity and vice versa
Odds of PTSD among social support types
As a way of isolating the effects of each aspect of social support, the odds of current PTSD were modeled for each of the four support types using logistic regression (Table 2). As predicted, those with low network diversity and low perceived availability of support had the greatest odds of ever having PTSD when compared to the reference group (high diversity/high perceived strength) (OR = 1.62, 1.33–1.99), after adjusting for sex, age, race/ethnicity, marital status, income, education, paternal or maternal history of alcohol, drug, depression, or behavioral disorder, number of traumatic events, and any comorbid mood, anxiety, or substance use disorder. Among groups with discordant support types, those with high network diversity and low perceived availability had appreciably lower odds of PTSD (OR = 1.02; 0.81–1.28) than those with low network diversity and high perceived availability (OR = 1.57; 1.3–1.91). Among these two types, the measure of effect was statistically significant (p < 0.0001) only among the latter group, suggesting that the effect of low social role diversity is more closely associated with PTSD than low perceived availability of support. A similar pattern was generally seen among nearly all demographic covariates (Electronic Supplementary Table 1). For every additional type of trauma an individual experienced the odds of having PTSD increased 32 % (CI 1.29–1.35). In addition, the odds of PTSD among individuals with a family history of psychiatric disorders were 1.25 times those without a family history (1.10–1.43). The final model was adjusted for those Axis I and II disorders, which were shown to have significant comorbidity with PTSD [31]. Overall, the odds of PTSD were consistent with the primary findings among nearly all disorders. Results for all comorbid disorders are presented in Table 3.
Table 2.
Adjusted odds ratios, sample frequencies, and standard errors of PTSD among four social support types
| [1] SNI = 0; ISEL = 0 | [2] SNI = 1; ISEL = 0 | [3] SNI = 0; ISEL = 1 | [4] SNI = 1; ISEL = 1 | |
|---|---|---|---|---|
| OR (95 % CI) | 1.62** (1.33–1.99) | 1.02 (0.81–1.28) | 1.57 (1.3–1.91)** | 1.00 |
| %, SE | 4.77, 0.14 | 5.58,0.15 | 8.1, 0.21 | 9.45, 0.17 |
The model is adjusted for sex, age, race/ethnicity, marital status, income, education, paternal or maternal history of alcohol, drug, depression, or behavioral disorder, number of traumatic events, age at trauma, and any comorbid mood, anxiety, or substance use disorder
p < 0.0001
Table 3.
Adjusted odds ratios of PTSD among those with comorbid disorders
| [1] SNI = 0; ISEL = 0 | [2] SNI = 1; ISEL = 0 | [3] SNI = 0; ISEL = 1 | [4] SNI = 1; ISEL = 1 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95 % CI | OR | 95 % CI | OR | 95 % CI | |||||
| Unadjusted for comorbidities | 1.9 | 1.55 | 2.33 | 1.1 | 0.88 | 1.38 | 1.71 | 1.42 | 2.06 | 1.00 |
| Any psychiatric disorder | 1.73 | 1.37 | 2.17 | 1.0 | 0.77 | 1.31 | 1.65 | 1.31 | 2.07 | 1.00 |
| Any mood disorder | 1.69 | 1.23 | 2.32 | 1.02 | 0.71 | 1.48 | 1.79 | 1.3 | 2.46 | 1.00 |
| Any anxiety disorder | 2.10 | 1.56 | 2.82 | 1.1 | 0.76 | 1.59 | 1.77 | 1.28 | 2.46 | 1.00 |
| Any substance disorder | 1.56 | 1.11 | 2.19 | 0.88 | 0.61 | 1.27 | 1.45 | 1.04 | 2.01 | 1.00 |
| >2 comorbid disorders | 1.64 | 1.48 | 1.83 | 0.94 | 0.82 | 1.06 | 1.60 | 1.42 | 1.79 | 1.00 |
| Family history | 1.57 | 1.41 | 1.75 | 0.93 | 0.84 | 1.02 | 1.60 | 1.39 | 1.73 | 1.00 |
Model adjusted for sex, age, race/ethnicity, marital status, income, education, paternal or maternal history of alcohol, drug, depression, or behavioral disorder, and number of traumatic events
Interaction by type of trauma and age at which trauma occurred
In the adjusted model, the interaction between type of trauma and social support types was not statistically significant (Wald χ2 = 0.11, df = 3; p = 0.95). Individuals who directly versus indirectly experienced traumatic events had no greater odds of PTSD among each social support type. In addition, the interaction by age at which the worst or single traumatic event was experienced trended toward statistically significant (Wald χ2 = 7.19, df = 3; p = 0.07), suggesting that there may be a meaningfully greater risk of PTSD among individuals who experience trauma as a child versus as an adult.
Discussion
This study examined the differences in magnitude of the association between social role diversity versus perceived availability of social support and PTSD onset and severity among individuals exposed to traumatic life events in the general US population. Confirming previous research, we found that the overall association between perceived support and PTSD was larger than that of social network diversity and PTSD [8, 39, 40]. However, we demonstrated that the overall effect masks an important subgroup difference; after isolating the effects of each measure, low social role diversity was significantly associated with having current PTSD, whether or not perceived support was low or high.
This pattern was consistent across demographic covariates and is supported by previous studies, which have generally found that a more diverse social network is protective against a range of mental health outcomes in the context of stress [41, 42]. Our findings may also lend further support to the social capital theory of nested social support [43], which has shown that the psychiatric health impact of structural elements of social support is both directly and indirectly mediated through functional support [44]. In short, the buffering effects of perceptions of available support are contingent on an active and diverse social network structure. The practical implications of this study are as follows: first, although it would be unrealistic to provide individuals who have experienced trauma with artificial social support as a proxy for meaningful personal relationships, programs which engage individuals in church, school, volunteer, or other social groups and activities may mitigate the risk of PTSD. Community engagement programs have already been shown to help recovery among Vietnam veterans and could prove efficacious among the general population [45]. Further, our findings could inform programs to educate family members and close friends about common reactions and both immediate and long-term support needs of individuals who experience traumatic events. Such education would include emphasizing the importance of strong and readily available support, and facilitating positive social reactions regarding the traumatic event. Also, the finding that trauma experienced as a child may yield a greater risk for PTSD suggests that an even greater priority should be placed on quality social support for children who experience traumatic events. Finally, these results can also be used to inform future research endeavors. For example, understanding specific factors that moderate the effects of social support, both qualitative and quantitative, on risk for PTSD after trauma is critical to efforts at risk prediction and identification of high-risk groups. For example, the effects of social support may differ based on prior psychiatric comorbidity, trauma types, and substance use, and other characteristics of individuals [46]. Future research that tests moderated models of social support in the context of individual characteristics in longitudinal samples would build upon these results in important ways.
Study limitations are noted. First, as is a common feature and critique of investigations of the links between social support and trauma [5], this study is based on cross-sectional data absent of any pre-trauma measures of support. There is certainly potential for individuals to experience social selection, whereby traumatic experiences lead to deterioration of social support. Indeed, the significance of both pathways has been shown [18, 47]. Replicating these methods with longitudinal data would give temporal clarity to the relevant mechanisms of perceived and embedded support. Second, because of the cross-sectional study design, we were unable to ascertain the time of onset among the measured comorbid disorders. The inclusion of these other disorders was to demonstrate the robustness and specificity of the model; even after controlling for comorbid disorders, the association and pattern between social network diversity and PTSD remained significant. Third, though the analysis did include specific attention to potentially different effects of direct versus indirect trauma as well as trauma experienced as a child versus adult, there are likely meaningful differences in the odds of PTSD among individual types of trauma. For example, one meta-analysis of the risk factors for PTSD in adults noted that life-threatening traumatic events led to a greater risk of PTSD than non-life-threatening events [48]. Analyzing the relationship between social support and PTSD among each type of traumatic event could yield greater insight into when and how types of social support may buffer the effects of trauma. Fourth, the SNI scale was operationalized as only a measure of social network diversity. A similar analysis comparing the overall size of one’s network to the perceived availability of support would also provide further understanding of structural versus functional aspects of social support. Fifth, because the study sample is of the US representative population, the reported levels of perceived support were higher than we would expect in a clinical sample. Therefore, the distribution of the ISEL-12 scores was negatively skewed. We tested the main association using both survey-driven cut-off points for high/low perceived support (median = 18) and data-driven cut-off points (median = 32) and found little difference in the measures of association. Among populations with lower levels of perceived support, there may be a different relationship between role diversity and perceived support.
In conclusion, though the effect of social support on mental health outcomes has been widely investigated, the need to differentiate between functional and structural elements of social support has been recognized as priority [49]. Through our study design, we were able to identify potentially distinct psychometric characteristics in social network diversity and perceived availability. Nevertheless, it is important to recognize that both perceived support and role diversity are likely significant factors following traumatic experience [3]. It appears that the perceived availability of social support may in fact be associated with PTSD; however, those benefits appear to be conditional on a large network with diverse social roles. Clarification of these issues will allow for more meaningful selection of measures of social support in future research as well as more valid interpretation of research findings regarding the effects of support, with the potential to develop effective support interventions in both pre- and post-trauma contexts. For the large proportion of the US population who has ever experienced traumatic events, this represents a step toward a greater understanding of how social networks operate with respect to PTSD, and holds promise for prevention and mitigation of psychiatric health outcomes.
Supplementary Material
Footnotes
Conflict of interest On behalf of all authors, the corresponding author states that there is no conflict of interest.
Electronic supplementary material The online version of this article (doi:10.1007/s00127-013-0798-4) contains supplementary material, which is available to authorized users.
References
- 1.Durkheim E (1951) Suicide, a study in sociology. Glencoe, Ill.: Free Press; (Originally published in 1897) [Google Scholar]
- 2.Berkman LF, Glass T, Brisette I, Seeman TE (2000) From social integration to health: Durkheim in the New Millennium. Soc Sci Med 51:843–857 [DOI] [PubMed] [Google Scholar]
- 3.Cohen S, Wills TA (1985) Stress, social support, and the buffering hypothesis. Psychol Bull 98(2):310–357 [PubMed] [Google Scholar]
- 4.Berkman LF, Glass T (2000) Social integration, social networks, social support, and health In: Berkman LF, Kawachi I (eds) Social epidemiology. Oxford University Press, New York, pp 137–173 [Google Scholar]
- 5.Kaniasty K, Norris FH (2008) Longitudinal linkages between perceived social support and posttraumatic stress symptoms: sequential roles of social causation and social selection. J Trauma Stress 21:274–281 [DOI] [PubMed] [Google Scholar]
- 6.Berkman LF, Syme SL (1979) Social networks, host resistance and mortality: a nine year follow-up study of Alameda County residents. Am J Epidemiol 109:186–204 [DOI] [PubMed] [Google Scholar]
- 7.Cohen S, Gottlieb B, Underwood L (2000) Social relationships and health In: Cohen S, Underwood L, Gottlieb B (eds) Measuring and intervening in social support. Oxford University Press, New York, pp 3–25 [Google Scholar]
- 8.Fleming R, Baum A, Gisriel MM, Gatchel RJ (1982) Mediating influences of social support on stress at Three Mile Island. J Hum Stress 8:14–22 [DOI] [PubMed] [Google Scholar]
- 9.Joseph S (1999) Social support and mental health following trauma In: Yule W (ed) Post-traumatic stress disorders. Concepts and therapy Wiley, Chichester, pp 71–91 [Google Scholar]
- 10.Moak ZB, Agrawal A (2010) The association between perceived interpersonal social support and physical and mental health: results from the National Epidemiological Survey on Alcohol and Related Conditions. J Public Health (Oxf) 32(2):191–201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wills TA, Cleary SD (1996) How are social support effects mediated: a test for parental support and adolescent substance use. J Pers Soc Psychol 71:937–952 [DOI] [PubMed] [Google Scholar]
- 12.Brewin CR, Andrews B, Valentine JD (2000) Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol 68(5):748–766 [DOI] [PubMed] [Google Scholar]
- 13.Cohen S (1988) Psychosocial models of social support in the etiology of physical disease. Health Psychol 7:269–297 [DOI] [PubMed] [Google Scholar]
- 14.Wethington E, McLeod JD, Kessler RC (1987) The importance of life events for explaining sex differences in psychological distress In: Barnett RC, Biener L, Baruch GK (eds) Gender and stress. The Free Press, New York, pp 144–156 [Google Scholar]
- 15.Belle D (1987) Gender differences in the social moderators of stress In: Barnett RC, Biener L, Baruch GK (eds) Gender and stress. The Free Press, New York, pp 257–277 [Google Scholar]
- 16.Bowlby J (1973) Attachment and loss. Hogarth Press, London [Google Scholar]
- 17.Oxman TE, Berkman LF, Kasl S, Freeman DH Jr, Barrett J (1992) Social support and depressive symptoms in the elderly. Am J Epidemiol 135(4):356–368 [DOI] [PubMed] [Google Scholar]
- 18.Ozer EJ, Best SR, Lipsey TL, Weiss DS (2003) Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull 129(1):52–73 [DOI] [PubMed] [Google Scholar]
- 19.Chen CM, Yi H, Falk DE, Stinson FS, Dawson DA, Grant BF (2010) Alcohol use and alcohol use disorders in the United States, a 3-year follow-up: main findings from the 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism, Bethesda [Google Scholar]
- 20.American Psychiatric Association (2001) Diagnostic and statistical manual of mental disorders, 4th edn American Psychiatric Association, Washington [Google Scholar]
- 21.Grant BF, Dawson DA, Hasin DS (2004) The Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions Alcohol Use Disorder and Associated Disabilities Interview Schedule DSM-IV Version National Institute on Alcohol Abuse and Alcoholism, Bethesda [Google Scholar]
- 22.Bohnert KM, Breslau N (2011) Assessing the performance of the short screening scale for post-traumatic stress disorder in a large nationally-representative survey. Int J Methods Psychiatr Res 20(1):E1–E5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Uddin M, Aiello AE, Wildman DE, Koenen KC, Pawelec G, de los Santos R, Galea S (2010) Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proc Natl Acad Sci USA 107(20):9470–9475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Grant BF (2008) The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend 92(27):1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen S (1991) Social supports and physical health In: Greene AL, Cummings M, Karraker KH (eds) Life-span developmental psychology: perspectives on stress and coping. Erlbaum Associates, Hillsdale, pp 213–234 [Google Scholar]
- 26.Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM Jr (1997) Social ties and susceptibility to the common cold. JAMA 277(24):1940–1944 [PubMed] [Google Scholar]
- 27.Cohen S (2004) Social relationships and health. Am Psychol 59(8):676–684 [DOI] [PubMed] [Google Scholar]
- 28.Brookings JB, Bolton B (1988) Confirmatory factor analysis of the Interpersonal Support Evaluation List. Am J Community Psychol 16(1):137–147 [DOI] [PubMed] [Google Scholar]
- 29.Hall LA, Sachs B, Rayens MK (1998) Mother’s potential for child abuse: the roles of childhood abuse and social resources. Nurs Res 47:87–95 [DOI] [PubMed] [Google Scholar]
- 30.Cohen S, Mermelstein R, Kamarck T, Hoberman H (1985) Measuring the functional components of social support In: Sarason IG, Sarason BR (eds) Social support: theory, research and application. Martinus Nijhoff, The Hague, pp 73–94 [Google Scholar]
- 31.Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF (2005) Prevalence, correlates, and comorbidity of DSM-IV anti-social personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry 66:677–685 [DOI] [PubMed] [Google Scholar]
- 32.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R (2003) The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend 71:7–16 [DOI] [PubMed] [Google Scholar]
- 33.Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF (1997) The alcohol use disorder and associated disabilities interview schedule (AUDADIS): reliability of alcohol and drug modules in a clinical sample. Drug Alcohol Depend 44:133–141 [DOI] [PubMed] [Google Scholar]
- 34.Chatterji S, Saunders JB, Vrasti R, Grant BF, Hasin D, Mager D (1997) Reliability of the alcohol and drug modules of the alcohol use disorder and associated disabilities interview schedule–alcohol/drug-revised (AUDADIS-ADR): an international comparison. Drug Alcohol Depend 47:171–185 [DOI] [PubMed] [Google Scholar]
- 35.Hasin DS, Paykin A (1999) Alcohol dependence and abuse diagnoses: concurrent validity in a nationally representative sample. Alcohol Clin Exp Res 23:144–150 [PubMed] [Google Scholar]
- 36.Hasin DS, Muthuen B, Wisnicki KS, Grant BF (1994) Validity of the bi-axial dependence concept: a test in the US general population. Addiction 89:573–579 [DOI] [PubMed] [Google Scholar]
- 37.SAS Institute Inc, SAS 9.1.3 (2000–2004) Help and Documentation, Cary, NC: SAS Institute Inc [Google Scholar]
- 38.Research Triangle Institute (2008) Software for Survey Data Analyses (SUDAAN) 10, Research Triangle Park, NC: RTI [Google Scholar]
- 39.Eriksson CB, Van De Kemp H, Gorsuch R, Hoke S, Foy DW (2001) Trauma exposure and PTSD symptoms in international relief and development personnel. J Trauma Stress 14:205–219 [Google Scholar]
- 40.Ozer EJ, Weinstein RS (2004) Urban adolescents’ exposure to community violence: the role of support, school safety, and social constraints in a school-based sample of boys and girls. J Clin Child Adolesc Psychol 33:463–476 [DOI] [PubMed] [Google Scholar]
- 41.George LK (1989) Stress, social support, and depression over the life-course In: Markides K, Cooper C (eds) Aging, stress, social support, and health. Wiley, London, pp 241–267 [Google Scholar]
- 42.Johnson TP (1991) Mental health, social relations, and social selection: a longitudinal analysis. J Health Soc Behav 32(4):408–423 [PubMed] [Google Scholar]
- 43.Kawachi I, Berkman LF (2000) Social cohesion, social capital, and health In: Berkman LF, Kawachi I (eds) Social epidemiology. Oxford University Press, New York, pp 174–190 [Google Scholar]
- 44.Lin N, Ye X, Ensel WM (1999) Social support and depressed mood: a structural analysis. J Health Soc Behav 40(4):344–359 [PubMed] [Google Scholar]
- 45.Koenen KC, Stellman JM, Stellman SD, Jr Sommer JF (2003) Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. J Consult Clin Psychol 71:980–986 [DOI] [PubMed] [Google Scholar]
- 46.Galea S, Ahern J, Tracy M, Hubbard A, Cerda M, Goldmann E, Vlahov D (2008) Longitudinal determinants of posttraumatic stress in a population-based cohort study. Epidemiology 19(1):47–54 [DOI] [PubMed] [Google Scholar]
- 47.King DW, Taft C, King LA, Hammond C, Stone ER (2006) Directionality of the association between social support and posttraumatic stress disorder: a longitudinal investigation. J Appl Soc Psychol 36:2980–2992 [Google Scholar]
- 48.Cohen J, Cohen P (1983) Applied multiple regression/correlation analysis for the behavioral sciences, 2nd edn Erlbaum, Hillsdale [Google Scholar]
- 49.Guay S, Billette V, Marchand A (2006) Exploring the links between posttraumatic stress disorder and social support: processes and potential research avenues. J Trauma Stress 19:327–338 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


